- Open access
- Published: 19 June 2020

Well-being is more than happiness and life satisfaction: a multidimensional analysis of 21 countries
- Kai Ruggeri 1 , 2 ,
- Eduardo Garcia-Garzon 3 ,
- Áine Maguire 4 ,
- Sandra Matz 5 &
- Felicia A. Huppert 6 , 7
Health and Quality of Life Outcomes volume 18 , Article number: 192 ( 2020 ) Cite this article
257k Accesses
216 Citations
366 Altmetric
Metrics details
Recent trends on measurement of well-being have elevated the scientific standards and rigor associated with approaches for national and international comparisons of well-being. One major theme in this has been the shift toward multidimensional approaches over reliance on traditional metrics such as single measures (e.g. happiness, life satisfaction) or economic proxies (e.g. GDP).
To produce a cohesive, multidimensional measure of well-being useful for providing meaningful insights for policy, we use data from 2006 and 2012 from the European Social Survey (ESS) to analyze well-being for 21 countries, involving approximately 40,000 individuals for each year. We refer collectively to the items used in the survey as multidimensional psychological well-being (MPWB).
The ten dimensions assessed are used to compute a single value standardized to the population, which supports broad assessment and comparison. It also increases the possibility of exploring individual dimensions of well-being useful for targeting interventions. Insights demonstrate what may be masked when limiting to single dimensions, which can create a failure to identify levers for policy interventions.
Conclusions
We conclude that both the composite score and individual dimensions from this approach constitute valuable levels of analyses for exploring appropriate policies to protect and improve well-being.
What is well-being?
Well-being has been defined as the combination of feeling good and functioning well; the experience of positive emotions such as happiness and contentment as well as the development of one’s potential, having some control over one’s life, having a sense of purpose, and experiencing positive relationships [ 23 ]. It is a sustainable condition that allows the individual or population to develop and thrive. The term subjective well-being is synonymous with positive mental health. The World Health Organization [ 45 ] defines positive mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community”. This conceptualization of well-being goes beyond the absence of mental ill health, encompassing the perception that life is going well.
Well-being has been linked to success at professional, personal, and interpersonal levels, with those individuals high in well-being exhibiting greater productivity in the workplace, more effective learning, increased creativity, more prosocial behaviors, and positive relationships [ 10 , 27 , 37 ]. Further, longitudinal data indicates that well-being in childhood goes on to predict future well-being in adulthood [ 39 ]. Higher well-being is linked to a number of better outcomes regarding physical health and longevity [ 13 ] as well as better individual performance at work [ 30 ], and higher life satisfaction has been linked to better national economic performance [ 9 ].
Measurement of well-being
Governments and researchers have attempted to assess the well-being of populations for centuries [ 2 ]. Often in economic or political research, this has ended up being assessed using a single item about life satisfaction or happiness, or a limited set of items regarding quality of life [ 3 ]. Yet, well-being is a multidimensional construct, and cannot be adequately assessed in this manner [ 14 , 24 , 29 ]. Well-being goes beyond hedonism and the pursuit of happiness or pleasurable experience, and beyond a global evaluation (life satisfaction): it encompasses how well people are functioning, known as eudaimonic, or psychological well-being. Assessing well-being using a single subjective item approach fails to offer any insight into how people experience the aspects of their life that are fundamental to critical outcomes. An informative measure of well-being must encompass all the major components of well-being, both hedonic and eudaimonic aspects [ 2 ], and cannot be simplified to a unitary item of income, life satisfaction, or happiness.
Following acknowledgement that well-being measurement is inconsistent across studies, with myriad conceptual approaches applied [ 12 ], Huppert and So [ 27 ] attempted to take a systematic approach to comprehensively measure well-being. They proposed that positive mental health or well-being can be viewed as the complete opposite to mental ill health, and therefore attempted to define mental well-being in terms of the opposite of the symptoms of common mental disorders. Using the DSM-IV and ICD-10 symptom criteria for both anxiety and depression, ten features of psychological well-being were identified from defining the opposite of common symptoms. The features encompassed both hedonic and eudaimonic aspects of well-being: competence, emotional stability, engagement, meaning, optimism, positive emotion, positive relationships, resilience, self-esteem, and vitality. From these ten features an operational definition of flourishing, or high well-being, was developed using data from Round 3 of the European Social Survey (ESS), carried out in 2006. The items used in the Huppert and So [ 27 ] study were unique to that survey, which reflects a well-being framework based on 10 dimensions of good mental health. An extensive discussion on the development and validation of these measures for the framework is provided in this initial paper [ 27 ].
As this was part of a major, multinational social survey, each dimension was measured using a single item. As such, ‘multidimensional’ in this case refers to using available measures identified for well-being, but does not imply a fully robust measure of these individual dimensions, which would require substantially more items that may not be feasible for population-based work related to policy development. More detailed and nuanced approaches might help to better capture well-being as a multidimensional construct, and also may consider other dimensions. However, brief core measures such as the one implemented in the ESS are valuable as they provide a pragmatic way of generating pioneering empirical evidence on well-being across different populations, and help direct policies as well as the development of more nuanced instruments. While this naturally would benefit from complementary studies of robust measurement focused on a single topic, appropriate methods for using sprawling social surveys remain critical, particularly through better standardization [ 6 ]. While this paper will overview those findings, we strongly encourage more work to that end, particularly in more expansive measures to support policy considerations.
General approach and key questions
The aim of the present study was to develop a more robust measurement of well-being that allows researchers and policymakers to measure well-being both as a composite construct and at the level of its fundamental dimensions. Such a measure makes it possible to study overall well-being in a manner that goes beyond traditional single-item measures, which capture only a fraction of the dimensions of well-being, and because it allows analysts to unpack the measure into its core components to identify strengths and weaknesses. This would produce a similar approach as the most common reference for policy impacts: Gross Domestic Product (GDP), which is a composite measure of a large number of underlying dimensions.
The paper is structured as follows: in the first step, data from the ESS are used to develop a composite measure of well-being from the items suggested by Huppert & So [ 27 ] using factor analysis. In the second step, the value of the revised measure is demonstrated by generating insights into the well-being of 21 European countries, both at the level of overall well-being and at the level of individual dimensions.
The European social survey
The ESS is a biannual survey of European countries. Through comprehensive measurement and random sampling techniques, the ESS provides a representative sample of the European population for persons aged 15 and over [ 38 ]. Both Round 3 (2006–2007) and Round 6 (2012–2013) contained a supplementary well-being module. This module included over 50 items related to all aspects of well-being including psychological, social, and community well-being, as well as incorporating a brief measure of symptoms of psychological distress. As summarized by Huppert et al. [ 25 ], of the 50, only 30 items relate to personal well-being, of which only 22 are positive measures. Of those remaining, not all relate to the 10 constructs identified by Huppert and So [ 27 ], so only a single item could be used, or else the item that had the strongest face validity and distributional items were chosen.
Twenty-two countries participated in the well-being modules in both Round 3 and Round 6. As this it within a wider body of analyses, it was important to focus on those initially. Hungary did not have data for the vitality item in Round 3 and was excluded from the analysis, as appropriate models would not have been able to reliably resolve a missing item for an entire country. To be included in the analysis and remain consistent, participants therefore had to complete all 10 items used and have the age, gender, employment, and education variables completed. Employment was classified into four groups: students, employed, unemployed, retired; other groups were excluded. Education was classified into three groups: low (less than secondary school), middle (completed secondary school), and high (postsecondary study including any university and above). Using these criteria, the total sample for Round 6 was 41,825 people from 21 countries for analysis. The full sample was 52.6% female and ranged in age from 15 to 103 (M = 47.9; SD = 18.9). Other details about participation, response rates, and exclusion have been published elsewhere [ 38 ].
Huppert & So [ 27 ] defined well-being using 10 items extracted from the Round 3 items, which represent 10 dimensions of well-being. However, the items used in Round 3 to represent positive relationships and engagement exhibited ceiling effects and were removed from the questionnaire in Round 6. Four alternatives were available to replace each question. Based on their psychometric properties (i.e., absence of floor effects and wider response distributions), two new items were chosen for positive relationships and engagement (one item for each dimension). The new items and those they replaced can be seen in Table 1 (also see Supplement ).
Development of a composite measure of psychological well-being (MPWB)
A composite measure of well-being that yields an overall score for each individual was developed. From the ten indicators of well-being shown in Table 1 , a single factor score was calculated to represent MPWB. This overall MPWB score hence constitutes a summary of how an individual performs across the ten dimensions, which is akin to a summary score such as GDP, and will be of general value to policymakers. Statistical analysis was performed in R software, using lavaan [ 40 ] and lavaan.survey [ 35 ] packages. The former is a widely-used package for the R software designed for computing structural equation models and confirmatory factor analyses (CFA). The latter allows introducing complex survey design weights (combination of design and population size weights) when estimating confirmatory factor analysis models with lavaan, which ensures that MPWB scoring followed ESS guidelines regarding both country-level and survey specific weights [ 17 ]. Both packages have been previously tested and validated in various analyses using ESS data (as explained in detail in lavaan.survey documentation).
It should be noted that Round 6 was treated as the focal point of these efforts before repeating for Round 3, primarily due to the revised items that were problematic in Round 3, and considering that analyses of the 2006 data are already widely available.
Prior to analysis, all items were coded such that higher scores were more positive and lower scores more negative. Several confirmatory factor analysis models were performed in order to test several theoretical conceptualizations regarding MPWB. Finally, factor scores (expected a posteriori [ 15 ];) were calculated for the full European sample and used for descriptive purposes. The approach and final model are presented in supplemental material .
Factor scores are individual scores computed as weighted combinations of each person’s response on a given item and the factor scoring coefficients. This approach is to be preferred to using raw or sum scores: sum or raw scores fail to consider how well a given item serves as an indicator of the latent variable (i.e., all items are unrealistically assumed to be perfect and equivalent measures of MPWB). They also do not take into account that different items could present different variability, which is expected to occur if items present different scales (as in our case). Therefore, the use of such simple methods results in inaccurate individual rankings for MPWB. To resolve this, factor scores are both more informative and more accurate, as they avoid the propagation of measurement error in subsequent analyses [ 19 ].
Not without controversy (see Supplement ), factor scores are likely to be preferable to sum scores when ranking individuals on unobservable traits that are expected to be measured with noticeable measurement error (such as MPWB [ 32 ];). Similar approaches based on factor scoring have been successfully applied in large international assessment research [ 21 , 34 ]. With the aim of developing a composite well-being score, it was necessary to provide a meaningful representation of how the different well-being indicators are reflected in the single measure. A hierarchical model with one higher-order factor best approximated MPWB along with two first-order factors (see supplement Figure S 1 ). This model replicates the factor structure reported for Round 3 by Huppert & So [ 27 ]. The higher-order factor explained the relationship between two first-order factors (positive functioning and positive characteristics showed a correlation of ρ = .85). In addition, modelling standardized residuals showed that the items representing vitality and emotional stability and items representing optimism and self-esteem were highly correlated. The similarities in wording in both pairs of items (see Table 1 ) are suspected to be responsible for such high residual correlations. Thus, those correlations were included in the model. As presented in Table 2 , the hierarchical model was found to fit the data better than any other model but a bi-factor model including these correlated errors. The latter model resulted in collapsed factor structure with a weak, bi-polar positive functioning factor. However, this bi-factor model showed a problematic bi-polar group factor with weak loadings. Whether this group factor was removed (resulting in a S-1 bi-factor model, as in [ 16 ]), model fit deteriorated. Thus, neither bi-factor alternative was considered to be acceptable.
To calculate the single composite score representing MPWB, a factor scoring approach was used rather than a simplistic summing of raw scores on these items. Factor scores were computed and standardized for the sample population as a whole, which make them suitable for broad comparison [ 8 ]. This technique was selected for two reasons. First, it has the ability to take into account the different response scales used for measuring the items included in the multidimensional well-being model. The CFA model, from which MPWB scores were computed, was defined such that the metric of the MPWB was fixed, which results in a standardized scale. Alternative approaches, such as sum or raw scores, would result in ignoring the differential variability across items, and biased individual group scores. Our approach, using factor scoring, resolves this issue by means of standardization of the MPWB scores. The second reason for this technique is that it could take account of how strongly each item loaded onto the MPWB factor. It should be noted that by using only two sub-factors, the weight applied to the general factor is identical within the model for each round. This model was also checked to ensure it also was a good fit for different groups based on gender, age, education and employment.
Separate CFA analyses per each country indicate that the final model fit the data adequately in all countries (.971 < CFI < .995; .960 < TFI < .994; .020 < RMSEA < .05; 0,023 < SRMR < 0,042). All items presented substantive loadings on their respective factors, and structures consistently replicated across all tested countries. Largest variations were found when assessing the residual items’ correlations (e.g., for emotional stability and vitality correlation, values ranged from 0,076 to .394). However, for most cases, residuals correlations were of similar size and direction (for both cases, the standard deviation of estimated correlations was close of .10). Thus, strong evidence supporting our final model was systematically found across all analyzed countries. Full results are provided in the supplement (Tables S 2 -S 3 ).
Model invariance
In order to establish meaningful comparisons across groups within and between each country, a two-stage approach was followed, resulting in a structure that was successfully found to be similar across demographics. First, a descriptive comparison of the parameter estimates unveiled no major differences across groups. Second, factor scores were derived for the sample, employing univariate statistics to compare specific groups within country and round. In these analyses, neither traditional nor modern approaches to factor measurement invariance were appropriate given the large sample and number of comparisons at stake ([ 8 ]; further details in Supplement ).
From a descriptive standpoint, the hierarchical structure satisfactorily fit both Round 3 and Round 6 data. All indicators in both rounds had substantial factor loadings (i.e., λ > .35). A descriptive comparison of parameter estimates produced no major differences across the two rounds. The lack of meaningful differences in the parameter estimates confirms that this method for computing MPWB can be used in both rounds.
As MPWB scores from both rounds are obtained from different items that have different scales for responses, it is necessary to transform individual scores obtained from both rounds in order to be aligned. To do this between Round 3 and Round 6 items, a scaling approach was used. To produce common metrics, scores from Round 3 were rescaled using a mean and sigma transformation (Kolen & Brennan 2010) to align with Round 6 scales. This was used as Round 6 measures were deemed to have corrected some deficiencies found in Round 3 items. This does not change outcomes in either round but simply makes the scores match in terms of distributions relative to their scales, making them more suitable for comparison.
As extensive descriptive insights on the sample and general findings are already available (see [ 41 ]), we focus this section on the evidence derived directly from the proposed approach to MPWB scores. For the combined single score for MPWB, the overall mean (for all participants combined) is fixed to zero, and the scores represent deviation from the overall mean. In 2012 (Round 6), country scores on well-being ranged from − 0.41 in Bulgaria to 0.46 in Denmark (Fig. 1 ). There was a significant, positive relationship between national MPWB mean scores and national life satisfaction means ( r = .56 (.55–.57), p < .001). In addition, MPWB was negatively related with depression scores and positively associated with other well-being measurements (see Supplement ).
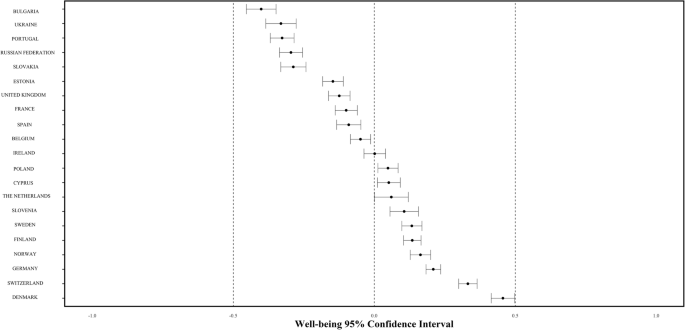
Distribution of national MPWB means and confidence intervals across Europe
Denmark having the highest well-being is consistent with many studies [ 4 , 18 ] and with previous work using ESS data [ 27 ]. While the pattern is typically that Nordic countries are doing the best and that eastern countries have the lowest well-being, exceptions exist. The most notable exception is Portugal, which has the third-lowest score and is not significantly higher than Ukraine, which is second lowest. Switzerland and Germany are second and third highest respectively, and show generally similar patterns to the Scandinavian countries (see Fig. 1 ). It should be noted that, for Figs. 1 , 2 , 3 , 4 , 5 , countries with the lowest well-being are at the top. This is done to highlight the greatest areas for potential impact, which are also the most of concern to policy.
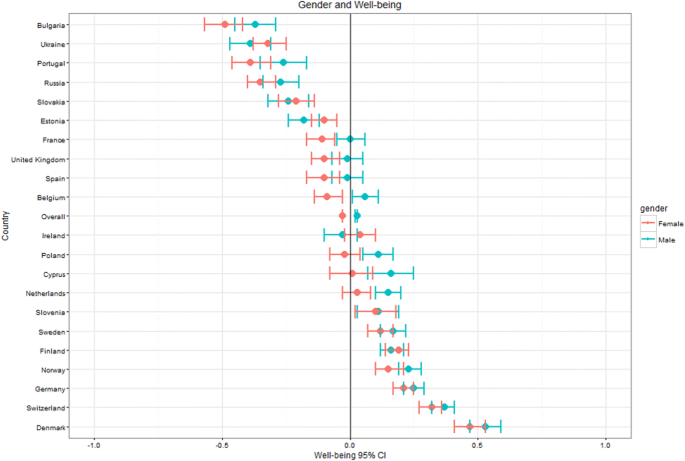
Well-being by country and gender
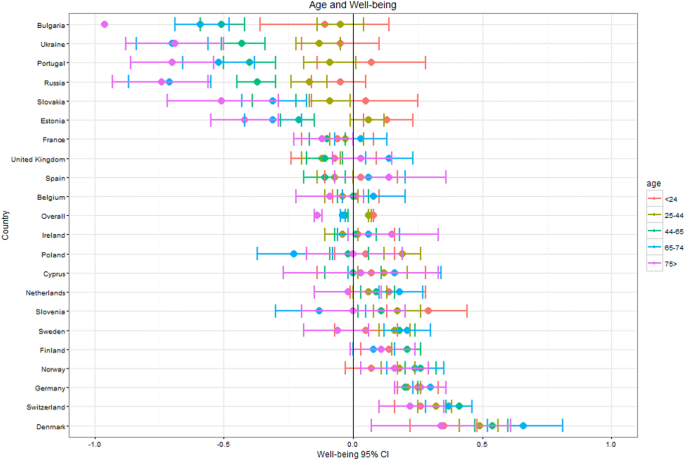
Well-being by country and age

Well-being by country and employment
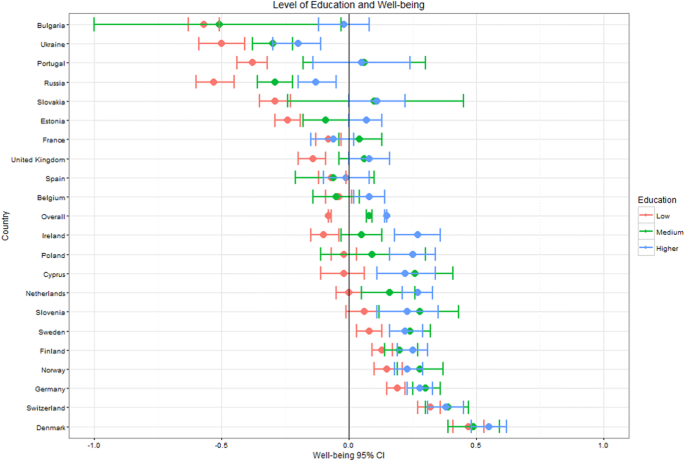
Well-being by country and education
General patterns across the key demographic variables – gender, age, education, employment – are visible across countries as seen in Figs. 1 , 2 , 3 , 4 , 5 (see also Supplement 2 ). These figures highlight patterns based on overall well-being as well as potential for inequalities. The visualizations presented here, though univariate, are for the purpose of understanding broad patterns while highlighting the need to disentangle groups and specific dimensions to generate effective policies.
For gender, women exhibited lower MPWB scores than men across Europe (β = −.09, t (36508) = − 10.37; p < .001). However, these results must be interpreted with caution due to considerable overlap in confidence intervals for many of the countries, and greater exploration of related variables is required. This also applies for the five countries (Estonia, Finland, Ireland, Slovakia, Ukraine) where women have higher means than men. Only four countries have significant differences between genders, all of which involve men having higher scores than women: the Netherlands (β = −.12, t (1759) = − 3.24; p < .001), Belgium (β = −.14, t (1783) = − 3.94; p < .001), Cyprus (β = −.18, t (930) = − 2.87; p < .001) and Portugal (β = −.19, t (1847) = − 2.50; p < .001).
While older individuals typically exhibited lower MPWB scores compared to younger age groups across Europe (β 25–44 = −.05, t (36506) = − 3.686, p < .001; β 45–65 = −.12, t (36506) = − 8.356, p < .001; β 65–74 = −.16, t (36506) = − 8.807, p < .001; β 75+ = −.28, t (36506) = − 13.568, p < .001), the more compelling pattern shows more extreme differences within and between age groups for the six countries with the lowest well-being. This pattern is most pronounced in Bulgaria, which has the lowest overall well-being. For the three countries with the highest well-being (Denmark, Switzerland, Germany), even the mean of the oldest age group was well above the European average, while for the countries with the lowest well-being, it was only young people, particularly those under 25, who scored above the European average. With the exception of France and Denmark, countries with higher well-being typically had fewer age group differences and less variance within or between groups. Only countries with the lowest well-being showed age differences that were significant with those 75 and over showing the lowest well-being.
MPWB is consistently higher for employed individuals and students than for retired (β = −.31, t (36506) = − 21.785; p < .00) or unemployed individuals (β = −.52, t (36556) = − 28.972; p < .001). Unemployed groups were lowest in nearly all of the 21 countries, though the size of the distance from other groups did not consistently correlate with national MPWB mean. Unemployed individuals in the six countries with the lowest well-being were significantly below the mean, though there is little consistency across groups and countries by employment beyond that. In countries with high well-being, unemployed, and, in some cases, retired individuals, had means below the European average. In countries with the lowest well-being, it was almost exclusively students who scored above the European average. Means for retired groups appear to correlate most strongly with overall well-being. There is minimal variability for employed groups in MPWB means within and between countries.
There is a clear pattern of MPWB scores increasing with education level, though the differences were most pronounced between low and middle education groups (β = .12, t (36508) = 9.538; p < .001). Individuals with high education were significantly higher on MPWB than those in the middle education group (β = .10, t (36508) =11.06; p < .001). Differences between groups were noticeably larger for countries with lower overall well-being, and the difference was particularly striking in Bulgaria. In Portugal, medium and high education well-being means were above the European average (though 95% confidence intervals crossed 0), but educational attainment is significantly lower in the country, meaning the low education group represents a greater proportion of the population than the other 21 countries. In the six countries with the highest well-being, mean scores for all levels of education were above the European mean.
Utilizing ten dimensions for superior understanding of well-being
It is common to find rankings of national happiness and well-being in popular literature. Similarly, life satisfaction is routinely the only measure reported in many policy documents related to population well-being. To demonstrate why such limited descriptive approaches can be problematic, and better understood using multiple dimensions, all 21 countries were ranked individually on each of the 10 indicators of well-being and MPWB in Round 6 based on their means. Figure 6 demonstrates the variations in ranking across the 10 dimensions of well-being for each country.
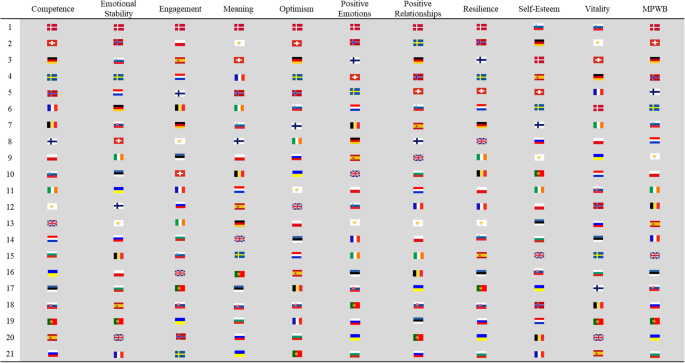
Country rankings in 2012 on multidimensional psychological well-being and each of its 10 dimensions
The general pattern shows typically higher rankings for well-being dimensions in countries with higher overall well-being (and vice-versa). Yet countries can have very similar scores on the composite measure but very different underlying profiles in terms of individual dimensions. Figure 7 a presents this for two countries with similar life satisfaction and composite well-being, Belgium and the United Kingdom. Figure 7 b then demonstrates this even more vividly for two countries, Finland and Norway, which have similar composite well-being scores and identical mean life satisfaction scores (8.1), as well as have the highest two values for happiness of all 21 countries. In both pairings, the broad outcomes are similar, yet countries consistently have very different underlying profiles in individual dimensions. The results indicate that while overall scores can be useful for general assessment, specific dimensions may vary substantially, which is a relevant first step for developing interventions. Whereas the ten items are individual measures of 10 areas of well-being, had these been limited to a single domain only, the richness of the underlying patterns would have been lost, and the limitation of single item approaches amplified.
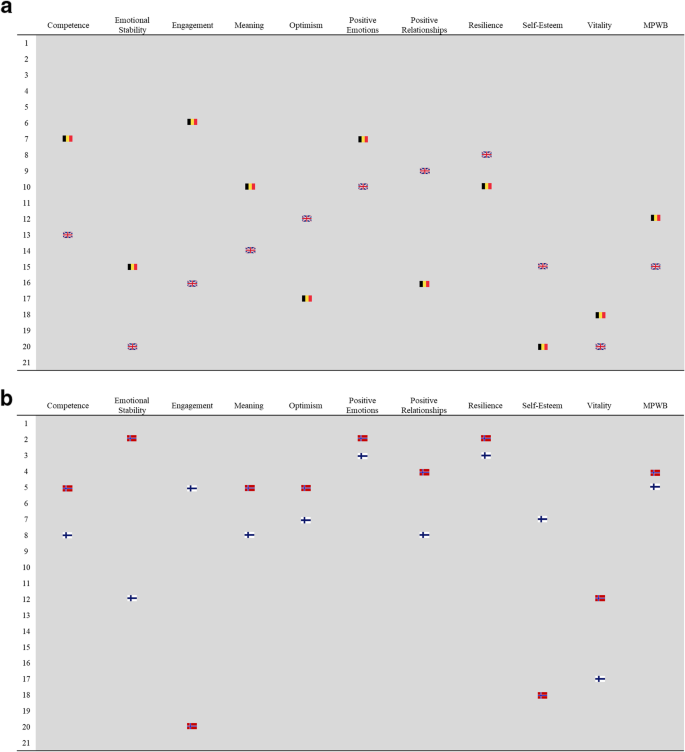
a Comparison of ranks for dimensions of well-being between two different countries with similar life satisfaction in 2012: Belgium and United Kingdom. b Comparison of ranks for dimensions of well-being between two similar countries with identical life satisfaction and composite well-being scores in 2012: Finland and Norway
The ten-item multidimensional measure provided clear patterns for well-being across 21 countries and various groups within. Whether used individually or combined into a composite score, this approach produces more insight into well-being and its components than a single item measure such as happiness or life satisfaction. Fundamentally, single items are impossible to unpack in reverse to gain insights, whereas the composite score can be used as a macro-indicator for more efficient overviews as well as deconstructed to look for strengths and weaknesses within a population, as depicted in Figs. 6 and 7 . Such deconstruction makes it possible to more appropriately target interventions. This brings measurement of well-being in policy contexts in line with approaches like GDP or national ageing indexes [ 7 ], which are composite indicators of many critical dimensions. The comparison with GDP is discussed at length in the following sections.
Patterns within and between populations
Overall, the patterns and profiles presented indicate a number of general and more nuanced insights. The most consistent among these is that the general trend in national well-being is usually matched within each of the primary indicators assessed, such as lower well-being within unemployed groups in countries with lower overall scores than in those with higher overall scores. While there are certainly exceptions, this general pattern is visible across most indicators.
The other general trend is that groups with lower MPWB scores consistently demonstrate greater variability and wider confidence intervals than groups with higher scores. This is a particularly relevant message for policymakers given that it is an indication of the complexity of inequalities: improvements for those doing well may be more similar in nature than for those doing poorly. This is particularly true for employment versus unemployment, yet reversed for educational attainment. Within each dimension, the most critical pattern is the lack of consistency for how each country ranks, as discussed further in other sections.
Examining individual dimensions of well-being makes it possible to develop a more nuanced understanding of how well-being is impacted by societal indicators, such as inequality or education. For example, it is possible that spending more money on education improves well-being on some dimensions but not others. Such an understanding is crucial for the implementation of targeted policy interventions that aim at weaker dimensions of well-being and may help avoid the development of ineffective policy programs. It is also important to note that the patterns across sociodemographic variables may differ when all groups are combined, compared to results within countries. Some effects may be larger when all are combined, whereas others may have cancelling effects.
Using these insights, one group that may be particularly important to consider is unemployed adults, who consistently have lower well-being than employed individuals. Previous research on unemployment and well-being has often focused on mental health problems among the unemployed [ 46 ] but there are also numerous studies of differences in positive aspects of well-being, mainly life satisfaction and happiness [ 22 ]. A large population-based study has demonstrated that unemployment is more strongly associated with the absence of positive well-being than with the presence of symptoms of psychological distress [ 28 ], suggesting that programs that aim to increase well-being among unemployed people may be more effective than programs that seek to reduce psychological distress.
Certainly, it is well known that higher income is related to higher subjective well-being and better health and life expectancy [ 1 , 42 ], so reduced income following unemployment is likely to lead to increased inequalities. Further work would be particularly insightful if it included links to specific dimensions of well-being, not only the comprehensive scores or overall life satisfaction for unemployed populations. As such, effective responses would involve implementation of interventions known to increase well-being in these groups in times of (or in spite of) low access to work, targeting dimensions most responsible for low overall well-being. Further work on this subject will be presented in forthcoming papers with extended use of these data.
This thinking also applies to older and retired populations in highly deprived regions where access to social services and pensions are limited. A key example of this is the absence in our data of a U-shaped curve for age, which is commonly found in studies using life satisfaction or happiness [ 5 ]. In our results, older individuals are typically lower than what would be expected in a U distribution, and in some cases, the oldest populations have the lowest MPWB scores. While previous studies have shown some decline in well-being beyond the age of 75 [ 20 ], our analysis demonstrates quite a severe fall in MPWB in most countries. What makes this insight useful – as opposed to merely unexpected – is the inclusion of the individual dimensions such as vitality and positive relationships. These dimensions are clearly much more likely to elicit lower scores than for younger age groups. For example, ageing beyond 75 is often associated with increased loneliness and isolation [ 33 , 43 ], and reduction in safe, independent mobility [ 31 ], which may therefore correspond with lower scores on positive relationships, engagement, and vitality, and ultimately lower scores on MPWB than younger populations. Unpacking the dimensions associated with the age-related decline in well-being should be the subject of future research. The moderate positive relationship of MPWB scores with life satisfaction is clear but also not absolute, indicating greater insights through multidimensional approaches without any obvious loss of information. Based on the findings presented here, it is clearly important to consider ensuring the well-being of such groups, the most vulnerable in society, during periods of major social spending limitations.
Policy implications
Critically, Fig. 6 represents the diversity of how countries reach an overall MPWB score. While countries with overall high well-being have typically higher ranks on individual items, there are clearly weak dimensions for individual countries. Conversely, even countries with overall low well-being have positive scores on some dimensions. As such, the lower items can be seen as potential policy levers in terms of targeting areas of concern through evidence-based interventions that should improve them. Similarly, stronger areas can be seen as learning opportunities to understand what may be driving results, and thus used to both sustain those levels as well as potentially to translate for individuals or groups not performing as well in that dimension. Collectively, we can view this insight as a message about specific areas to target for improvement, even in countries doing well, and that even countries doing poorly may offer strengths that can be enhanced or maintained, and could be further studied for potential applications to address deficits. We sound a note of caution however, in that these patterns are based on ranks rather than actual values, and that those ranks are based on single measures.
Figure 7 complements those insights more specifically by showing how Finland and Norway, with a number of social, demographic, and economic similarities, plus identical life satisfaction scores (8.1) arrive at similar single MPWB scores with very different profiles for individual dimensions. By understanding the levers that are specific to each country (i.e. dimensions with the lowest well-being scores), policymakers can respond with appropriate interventions, thereby maximizing the potential for impact on entire populations. Had we restricted well-being measurement to a single question about happiness, as is commonly done, we would have seen both countries had similar and extremely high means for happiness. This might have led to the conclusion that there was minimal need for interventions for improving well-being. Thus, in isolation, using happiness as the single indicator would have masked the considerable variability on several other dimensions, especially those dimensions where one or both had means among the lowest of the 21 countries. This would have resulted in similar policy recommendations, when in fact, Norway may have been best served by, for example, targeting lower dimensions such as Engagement and Self-Esteem, and Finland best served by targeting Vitality and Emotional Stability.
Targeting specific groups and relevant dimensions as opposed to comparing overall national outcomes between countries is perhaps best exemplified by Portugal, which has one of the lowest educational attainment rates in OECD countries, exceeded only by Mexico and Turkey [ 36 ]. This group thus skews the national MPWB score, which is above average for middle and high education groups, but much lower for those with low education. Though this pattern is not atypical for the 21 countries presented here, the size of the low education group proportional to Portugal’s population clearly reduces the national MPWB score. This implies that the greatest potential for improvement is likely to be through addressing the well-being of those with low education as a near-term strategy, and improving access to education as a longer-term strategy. It will be important to analyze this in the near future, given recent reports that educational attainment in Portugal has increased considerably in recent years (though remains one of the lowest in OECD countries) [ 36 ].
One topic that could not be addressed directly is whether these measures offer value as indicators of well-being beyond the 21 countries included here, or even beyond the countries included in ESS generally. In other words, are these measures relevant only to a European population or is our approach to well-being measurement translatable to other regions and purposes? Broadly speaking, the development of these measures being based on DSM and ICD criteria should make them relevant beyond just the 21 countries, as those systems are generally intended to be global. However, it can certainly be argued that these methods for designing measures are heavily influenced by North American and European medical frameworks, which may limit their appropriateness if applied in other regions. Further research on these measures should consider this by adding potential further measures deemed culturally appropriate and seeing if comparable models appear as a result.
A single well-being score
One potential weakness remains the inconsistency of scaling between ESS well-being items used for calculating MPWB. However, this also presents an opportunity to consider the relative weighting of each item within the current scales, and allow for the development of a more consistent and reliable measure. These scales could be modified to align in separate studies with new weights generated – either generically for all populations or stratified to account for various cultural or other influences. Using these insights, scales could alternatively be produced to allow for simple scoring for a more universally accessible structure (e.g. 1–100) but with appropriate values for each item that represents the dimensions, if this results in more effective communication with a general public than a standardized score with weights. Additionally, common scales would improve on attempts to use rankings for presenting national variability within and between dimensions. Researchers should be aware that factor scores are sample-dependent (as based on specific factor model parameters such as factor loadings). Nevertheless, future research focused on investigating specific item differential functioning (by means of multidimensional item response functioning or akin techniques) of these items across situations (i.e., rounds) and samples (i.e., rounds and countries) should be conducted in order to have a more nuanced understanding of this scale functioning.
What makes this discussion highly relevant is the value of a more informed measure to replace traditional indicators of well-being, predominantly life satisfaction. While life satisfaction may have an extensive history and present a useful metric for comparisons between major populations of interest, it is at best a corollary, or natural consequence, of other indicators. It is not in itself useful for informing interventions, in the same way limiting to a single item for any specific dimension of well-being should not alone inform interventions.
By contrast, a validated and standardized multidimensional measure is exceptionally useful in its suitability to identify those at risk, as well as its potential for identifying areas of strengths and weaknesses within the at-risk population. This can considerably improve the efficiency and appropriateness of interventions. It identifies well-understood dimensions (e.g. vitality, positive emotion) for direct application of evidence-based approaches that would improve areas of concern and thus overall well-being. Given these points, we strongly argue for the use of multidimensional approaches to measurement of well-being for setting local and national policy agenda.
There are other existing single-score approaches for well-being addressing its multidimensional nature. These include the Warwick-Edinburgh Mental Well-Being Scale [ 44 ] and the Flourishing Scale [ 11 ]. In these measures, although the single score is derived from items that clearly tap a number of dimensions, the dimensions have not been systematically derived and no attempt is made to measure the underlying dimensions individually. In contrast, the development approach used here – taking established dimensions from DSM and ICD – is based on years of international expertise in the field of mental illness. In other words, there have long been adequate measures for identifying and understanding illness, but there is room for improvement to better identify and understand health. With increasing support for the idea of these being a more central focus of primary outcomes within economic policies, such approaches are exceptionally useful [ 13 ].
Better measures, better insights
Naturally, it is not a compelling argument to simply state that more measures present greater information than fewer or single measures, and this is not the primary argument of this manuscript. In many instances, national measures of well-being are mandated to be restricted to a limited set of items. What is instead being argued is that well-being itself is a multidimensional construct, and if it is deemed a critical insight for establishing policy agenda or evaluating outcomes, measurements must follow suit and not treat happiness and life satisfaction values as universally indicative. The items included in ESS present a very useful step to that end, even in a context where the number of items is limited.
As has been argued by many, greater consistency in measurement of well-being is also needed [ 26 ]. This may come in the form of more consistency regarding dimensions included, the way items are scored, the number of items representing each dimension, and changes in items over time. While inconsistency may be prevalent in the literature to date for definitions and measurement, the significant number of converging findings indicates increasingly robust insights for well-being relevant to scientists and policymakers. Improvements to this end would support more systematic study of (and interventions for) population well-being, even in cases where data collection may be limited to a small number of items.
The added value of MPWB as a composite measure
While there are many published arguments (which we echo) that measures of well-being must go beyond objective features, particularly related to economic indicators such as GDP, this is not to say one replaces the other. More practically, subjective and objective approaches will covary to some degree but remain largely distinct. For example, GDP presents a useful composite of a substantial number of dimensions, such as consumption, imports, exports, specific market outcomes, and incomes. If measurement is restricted to a macro-level indicator such as GDP, we cannot be confident in selecting appropriate policies to implement. Policies are most effective when they target a specific component (of GDP, in this instance), and then are directly evaluated in terms of changes in that component. The composite can then be useful for comprehensive understanding of change over time and variation in circumstances. Specific dimensions are necessary for identifying strengths and weaknesses to guide policy, and examining direct impacts on those dimensions. In this way, a composite measure in the form of MPWB for aggregate well-being is also useful, so long as the individual dimensions are used in the development and evaluation of policies. Similar arguments for other multidimensional constructs have been made recently, such as national indexes of ageing [ 7 ].
In the specific instance of MPWB in relation to existing measures of well-being, there are several critical reasons to ensure a robust approach to measurement through systematic validation of psychometric properties. The first is that these measures are already part of the ESS, meaning they are being used to study a very large sample across a number of social challenges and not specifically a new measure for well-being. The ESS has a significant influence on policy discussions, which means the best approaches to utilizing the data are critical to present systematically, as we have attempted to do here. This approach goes beyond existing measures such as Gallup or the World Happiness Index to broadly cover psychological well-being, not individual features such as happiness or life satisfaction (though we reiterate: as we demonstrate in Fig. 7 a and b, these individual measures can and should still covary broadly with any multidimensional measure of well-being, even if not useful for predicting all dimensions). While often referred to as ‘comprehensive’ measurement, this merely describes a broad range of dimensions, though more items for each dimension – and potentially more dimensions – would certainly be preferable in an ideal scenario.
These dimensions were identified following extensive study for flourishing measures by Huppert & So [ 27 ], meaning they are not simply a mix of dimensions, but established systematically as the key features of well-being (the opposite of ill-being). Furthermore, the development of the items is in line with widely validated and practiced measures for the identification of illness. The primary adjustment has simply been the emphasis on health, but otherwise maintains the same principles of assessment. Therefore, the overall approach offers greater value than assessing only negative features and inferring absence equates to opposite (positives), or that individual measures such as happiness can sufficiently represent a multidimensional construct like well-being. Collectively, we feel the approach presented in this work is therefore a preferable method for assessing well-being, particularly on a population level, and similar approaches should replace single items used in isolation.
While the focus of this paper is on the utilization of a widely tested measure (in terms of geographic spread) that provides for assessing population well-being, it is important to provide a specific application for why this is relevant in a policy context. Additionally, because the ESS itself is a widely-recognized source of meaningful information for policymakers, providing a robust and comprehensive exploration of the data is necessary. As the well-being module was not collected in recent rounds, these insights provide clear reasoning and applications for bringing them back in the near future.
More specifically, it is critical that this approach be seen as advantageous both in using the composite measure for identifying major patterns within and between populations, and for systematically unpacking individual dimensions. Using those dimensions produces nuanced insights as well as the possibility of illuminating policy priorities for intervention.
In line with this, we argue that no composite measure can be useful for developing, implementing, or evaluating policy if individual dimensions are not disaggregated. We are not arguing that MPWB as a single composite score, nor the additional measures used in ESS, is better than other existing single composite scoring measures of well-being. Our primary argument is instead that MPWB is constructed and analyzed specifically for the purpose of having a robust measure suitable for disaggregating critical dimensions of well-being. Without such disaggregation, single composite measures are of limited use. In other words, construct a composite and target the components.
Well-being is perhaps the most critical outcome measure of policies. Each individual dimension of well-being as measured in this study represents a component linked to important areas of life, such as physical health, financial choice, and academic performance [ 26 ]. For such significant datasets as the European Social Survey, the use of the single score based on the ten dimensions included in multidimensional psychological well-being gives the ability to present national patterns and major demographic categories as well as to explore specific dimensions within specific groups. This offers a robust approach for policy purposes, on both macro and micro levels. This facilitates the implementation and evaluation of interventions aimed at directly improving outcomes in terms of population well-being.
Availability of data and materials
The datasets analysed during the current study are available in the European Social Survey repository, http://www.europeansocialsurvey.org/data/country_index.html
Abbreviations
Diagnostic and Statistical Manual of Mental Disorders
European Social Survey
Gross Domestic Product
International Classification of Disease
Multidimensional psychological well-being
Adler NE, Rehkopf DH. US disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235–52.
PubMed Google Scholar
Allin P, Hand DJ. New statistics for old?—measuring the wellbeing of the UK. J Royal Stat Soc Ser A. 2017;180(1):3–43.
Google Scholar
Arechavala NS, Espina PZ, Trapero BP. The economic crisis and its effects on the quality of life in the European Union. Soc Indic Res. 2015;120(2):323–43.
Biswas-Diener R, Vittersø J, Diener E. The Danish effect: beginning to explain high well-being in Denmark. Soc Indic Res. 2010;97(2):229–46.
Blanchflower DG, Oswald AJ. Is well-being U-shaped over the life cycle? Soc Sci Med. 2008;66(8):1733–49.
Carreira H, Williams R, Strongman H, Bhaskaran K. Identification of mental health and quality of life outcomes in primary care databases in the UK: a systematic review. BMJ Open. 2019;9(7):e029227.
PubMed PubMed Central Google Scholar
Chen C, Goldman DP, Zissimopoulos J, Rowe JW. Multidimensional comparison of countries’ adaptation to societal aging. Proc Natl Acad Sci. 2018;115(37):9169–74.
CAS PubMed PubMed Central Google Scholar
Cieciuch J, Davidov E, Schmidt P, Algesheimer R, Schwartz SH. Comparing results of exact vs. an approximate (Bayesian) measurement invariance test: a cross-country illustration with a scale to measure 19 human values. Front Psychol. 2014;8(5):982.
Deaton A. Income, health and wellbeing around the world: evidence from the Gallup world poll. J Econ Perspect. 2008;22(2):53–72.
Diener E. New findings and future directions for subjective well-being research. Am Psychol. 2012;67(8):590.
Diener E, Wirtz D, Tov W, Kim-Prieto C, Choi D, Oishi S, Biswas-Diener R. New measures of well-being: flourishing and positive and negative feelings. Soc Indic Res. 2009;39:247–66.
Diener E, Seligman ME. Beyond money toward an economy of well-being. Psychol Sci Public Interest. 2004;5(1):1–31.
Diener E, Pressman S, Hunter J, Chase D. If, why, and when subjective well-being influences health, and future needed research. Appl Psychol Health Well Being. 2017;9(2):133–67.
Dolan P, White MP. How can measures of subjective well-being be used to inform public policy? Perspect Psychol Sci. 2007;2(1):71–85.
Eastbrook R, Neale M. A comparison of factor score estimation methods in presence of missing data: reliability and an application to nicotine dependence. Multivar Behav Res. 2012;48(1):1–27.
Eid M, Krumm S, Koch T, Schulze J. Bifactor models for predicting criteria by general and specific factors: problems of Nonidentiability and alternative solutions. Journal of Intelligence. 2018;6(3):42.
European Social Survey (2014). Weighting European Social Survey Data. Retrieved from https://www.europeansocialsurvey.org/docs/methodology/ESS_weighting_data_1.pdf .
Farver-Vestergaard I, Ruggeri K. Setting National Policy Agendas in Light of the Denmark Results for Well-being. JAMA Psychiatry. 2017;74(8):773–4.
Ferrando PJ, Lorenzo-Seva U. A note on improving EAP trait estimation in oblique factor-analytic and item response theory models. Psicologica. 2016;37(2):235–47.
Gerstorf D, Hoppmann CA, Löckenhoff CE, Infurna FJ, Schupp J, Wagner GG, Ram N. Terminal decline in well-being: the role of social orientation. Psychol Aging. 2016;31(2):149.
Grundke, R., et al. Skills and global value chains: A characterisation, OECD Science, Technology and Industry Working Papers, No. 2017/05, OECD Publishing. 2017. https://doi.org/10.1787/cdb5de9b-en .
Gudmundsdottir DG. The impact of economic crisis on happiness. Soc Indic Res. 2013;110(3):1083–101.
Huppert FA. Psychological well-being: evidence regarding its causes and consequences†. Appl Psychol Health Well Being. 2009;1(2):137–64. https://doi.org/10.1111/j.1758-0854.2009.01008.x .
Article Google Scholar
Huppert FA. The state of well-being science: concepts, measures, interventions and policies. In: Huppert FA, Cooper CL, editors. Interventions and policies to enhance well-being. Oxford: Wiley-Blackwell; 2014.
Huppert FA, Marks N, Clark A, Siegrist J, Stutzer A, Vitterso J, Wahrendorf M. Measuring well-being across Europe: description of the ESS well-being module and preliminary findings. Soc Indic Res. 2009;91(3):301–15.
Huppert F, Ruggeri K. 15. Policy challenges: well-being as a priority in public mental health. In: Bhugra D, Bhui K, Wong S, Gilman S, editors. Oxford textbook of public mental health. Oxford: Oxford University Press; 2018.
Huppert FA, So TT. Flourishing across Europe: application of a new conceptual framework for defining well-being. Soc Indic Res. 2013;110(3):837–61.
Huppert FA, Whittington JE. Evidence for the independence of positive and negative well-being: implications for quality of life assessment. Br J Health Psychol. 2003;8(1):107–22.
Kahneman D, Krueger AB. Developments in the measurement of subjective well-being. J Econ Perspect. 2006;20(1):3–24.
Knapp M, McDaid D, Parsonage M. Mental health promotion and mental illness prevention: the economic case. London: London School of Economics; 2011.
Lihavainen K, Sipilä S, Rantanen T, Kauppinen M, Sulkava R, Hartikainen S. Effects of comprehensive geriatric assessment and targeted intervention on mobility in persons aged 75 years and over: a randomized controlled trial. Clin Rehabil. 2012;26(4):314–26.
McNeish, D., & Wolf, M. G. (2019). Sum Scores Are Factor Scores. https://doi.org/10.31234/osf.io/3wy47 .
Nicolaisen M, Thorsen K. Who are lonely? Loneliness in different age groups (18–81 years old), using two measures of loneliness. Int J Aging Hum Dev. 2014;78(3):229–57.
Nicoletti, G., Scarpetta, S., & Boylaud, O. Summary indicators of product market regulation with an extension to employment protection legislation, OECD Economics Department Working Paper s , no. 226, OECD publishing, Paris. 2000. https://doi.org/10.1787/215182844604 .
Oberski D. Lavaan.Survey: an R package for complex survey analysis of structural equation models. J Stat Softw. 2014;57(1):1–27.
OECD. Education at a glance 2014: OECD indicators. Portugal. Retrieved on January 28, 2016 at http://bit.ly/2wqZweh . 2014.
Oishi S, Diener E, Lucas RE. The optimum level of well-being: can people be too happy? Perspect Psychol Sci. 2007;2(4):346–60.
Reibling N, Beckfield J, Huijts T, Schmidt-Catran A, Thomson KH, Wendt C. Depressed during the depression: has the economic crisis affected mental health inequalities in Europe? Findings from the European social survey (2014) special module on the determinants of health. Eur J Public Health. 2017;27:47–54.
Richards M, Huppert FA. Do positive children become positive adults? Evidence from a longitudinal birth cohort study. J Posit Psychol. 2011;6(1):75–87.
Roseel Y. Lavaan: an R package for structural equation modeling. J Stat Softw. 2012;48(2):1–36.
Ruggeri K, Garcia Garzon E, Maguire Á, Huppert F. Chapter 1: comprehensive psychological well-being. In: Looking through the wellbeing kaleidoscope: Results from the European Social Survey. London: New Economics Foundation; 2016.
Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2015;385(9968):640–8.
Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci. 2013;110(15):5797–801.
Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Outcomes. 2007;5(1):63.
World Health Organization. The world health report 2001: mental health: new understanding, new hope. Geneva: World Health Organization; 2001.
Young C. Losing a job: the nonpecuniary cost of unemployment in the United States. Soc Forces. 2012;91(2):609–6.
Download references
Acknowledgements
The authors would like to thank Ms. Sara Plakolm, Ms. Amel Benzerga, and Ms. Jill Hurson for assistance in proofing the final draft. We would also like to acknowledge the general involvement of the Centre for Comparative Social Surveys at City University, London, and the Centre for Wellbeing at the New Economics Foundation.
This work was supported by a grant from the UK Economic and Social Research Council (ES/LO14629/1). Additional support was also provided by the Isaac Newton Trust, Trinity College, University of Cambridge, and the UK Economic and Social Research Council (ES/P010962/1).
Author information
Authors and affiliations.
Columbia University Mailman School of Public Health, New York, USA
Kai Ruggeri
Policy Research Group, Centre for Business Research, Judge Business School, University of Cambridge, Cambridge, UK
Universidad Camilo José Cela, Madrid, Spain
Eduardo Garcia-Garzon
Trinity College Dublin, Dublin, Ireland
Áine Maguire
Columbia Business School, New York, USA
Sandra Matz
University of New South Wales, Sydney, Australia
Felicia A. Huppert
Well-being Institute, University of Cambridge, Cambridge, UK
You can also search for this author in PubMed Google Scholar
Contributions
KR is the lead author and researcher on the study, responsible for all materials start to finish. FH was responsible for the original grant award and the general theory involved in the measurement approaches. ÁM was responsible for broad analysis and writing. EGG was responsible for psychometric models and the original factor scoring approach, plus writing the supplementary explanations. SM provided input on later drafts of the manuscript as well as the auxiliary analyses. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Kai Ruggeri .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
All authors declare they have no competing interests in the dissemination of this work. While all authors receive funding and conduct various research on the topic in academic and consultant capacities, this work is free from any interests and has no direct link to work that would influence any outputs or conclusions.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: figure s1.
. Hierarchical approach to modelling comprehensive psychological well-being. Table S1 . Confirmatory Factor Structure for Round 6 and 3. Figure S2 . Well-being by country and gender. Figure S3 . Well-being by country and age. Figure S4 . Well-being by country and employment. Figure S5 . Well-being by country and education. Table S2 . Item loadings for Belgium to Great Britain. Table S3 . Item loadings for Ireland to Ukraine.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ruggeri, K., Garcia-Garzon, E., Maguire, Á. et al. Well-being is more than happiness and life satisfaction: a multidimensional analysis of 21 countries. Health Qual Life Outcomes 18 , 192 (2020). https://doi.org/10.1186/s12955-020-01423-y
Download citation
Received : 03 May 2019
Accepted : 28 May 2020
Published : 19 June 2020
DOI : https://doi.org/10.1186/s12955-020-01423-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Composite measures
- Economic policy
- Exploratory structural equation models
Health and Quality of Life Outcomes
ISSN: 1477-7525
- Submission enquiries: [email protected]
Advertisement
Determinants of wellbeing in university students: The role of residential status, stress, loneliness, resilience, and sense of coherence
- Open access
- Published: 26 April 2022
- Volume 42 , pages 19699–19708, ( 2023 )
Cite this article
You have full access to this open access article
- Caroline E. Brett ORCID: orcid.org/0000-0002-5680-2948 1 ,
- Michelle L. Mathieson ORCID: orcid.org/0000-0002-3147-3228 1 &
- Avril M. Rowley ORCID: orcid.org/0000-0003-3107-9500 2
11k Accesses
5 Citations
9 Altmetric
Explore all metrics
Maintaining wellbeing in university students is a government priority, but robust evidence has been lacking. Higher wellbeing is associated with better mental and physical health, higher self-esteem, self-efficacy, and effective coping strategies. This study aimed to identify, through an online survey in 2018, key determinants of wellbeing amongst a sample of 574 (65.5% female) students across all levels of study at a university in the UK. Most respondents (526 (91.8%)) reported feeling unusually stressed or overwhelmed at university. Residential students reported higher loneliness and number of stressors than commuter students, and postgraduate students reported higher wellbeing, resilience, and sense of coherence, and lower perceived stress and loneliness. Hierarchical regression analyses showed that 71.8% of the variance in wellbeing was predicted by a model containing demographics (age/gender, level of study, number of stressors), psychosocial variables, and perceived stress, with perceived stress, sense of coherence, loneliness, and resilience the strongest predictors. The findings suggest that interventions designed to improve resilience and sense of coherence, and reduce loneliness and perceived stress are likely to be effective in enhancing wellbeing in a student population.
Similar content being viewed by others

Exploring loneliness and students’ sense of coherence (S-SoC) in the university setting
Andrea Limarutti, Marco Johannes Maier & Eva Mir

The impact of lockdown stress and loneliness during the COVID-19 pandemic on mental health among university students in Germany
Antonia M. Werner, Ana N. Tibubos, … Manfred E. Beutel

Student Subjective Wellbeing amidst the Covid-19 Pandemic in Iran: Role of Loneliness, Resilience and Parental Involvement
Faramarz Asanjarani, Aneesh Kumar & Simindokht Kalani
Avoid common mistakes on your manuscript.
Introduction
Mental health and wellbeing in university students is of increasing concern throughout the world (Royal College of Psychiatrists, 2011 ; Brown, 2018 ; Hughes & Spanner, 2019 ). Increasing numbers of students are reporting and seeking support for mental health difficulties (Auerbach et al., 2018 ), possibly due to a number of factors including increasing financial pressures, uncertain future career prospects, widening participation, and an increased awareness of the signs and symptoms of mental health difficulties (Pollard et al., 2019 ; Royal College of Psychiatrists, 2011 ). Although this trend is reflected in the general population – mental health difficulties have increased in young people aged 16–24 across a similar timescale (Johnson & Crenna-Jennings, 2018 ) – students have in recent years scored lower than their non-student counterparts on a number of measures of wellbeing (Neves & Hillman, 2019 ). Students attending university for the first time at this age are vulnerable to mental health difficulties, with evidence suggesting that the majority of mental illnesses develop by the time an individual reaches their mid-20 s (Kessler et al., 2007 ).
The transition to university is often a time of great upheaval requiring rapid adjustment and considerable personal resources (Lipson & Eisenberg, 2018 ). During this period, students may not only need to move home, often to a new place away from friends and family, but also need to make new social connections, manage finances, manage a household and manage their own time, which can be frightening new experiences for them. Many students also have to juggle academic study with paid work and other commitments, alongside an increasingly busy social life. Combined with the transition towards academic autonomy, the requirement for considerable independent study, and constant assessment deadlines with reduced support from tutors compared to their previous school experience, the university experience itself can be a source of stress and has been associated with increased mental health difficulties (Cleary et al., 2011 ). However, little published research exists on how the university experience affects student wellbeing (Barkham et al., 2019 ), and how individual psychological characteristics, such as personality, outlook, and coping resources, might influence students’ ability to maintain their wellbeing in the face of personal and academic stressors. Thus, understanding the determinants of student wellbeing across all levels of study and personal circumstances is vital to enable universities to help support students and prevent the development of mental health difficulties that may continue throughout their lives.
University-Related Factors
The university experience is changing. Financial pressures and widening participation initiatives have resulted in greater numbers of students remaining in the family home while undertaking their university studies (Pollard et al., 2019 ). This is particularly the case in city-based universities, where strong transport links facilitate commuting to the university campus, enabling more students to study from home in their local area. These ‘commuter’ or ‘stay-at-home’ students, who constitute as much as 90% of the student population at some universities (Jones, 2020 ), experience university in a qualitatively different way to ‘residential’ students who live in halls or shared accommodation, and are more likely to come from underrepresented groups and experience lower progression rates than their peers (Office for Students, 2020a ). Lower achievement can lead to negative impacts on mental health and wellbeing, which for commuter students is compounded by the challenge of developing social connections with fellow students, particularly when social events are held on campus during the evenings or weekends. In addition, commuter students are often overlooked by student societies or support services. Evidence suggests that commuter students fare less well than their residential counterparts in terms of academic achievement (Office for Students, 2020a ) and satisfaction with life (Blackman, 2020 ; Office for Students, 2020b ).
Although there is a paucity of longitudinal research on student wellbeing, one such study demonstrated that psychological wellbeing and anxiety levels fluctuated across the three-year undergraduate degree, and across the academic year (Bewick et al., 2010 ). Macaskill ( 2013 ) reported increased psychiatric symptoms amongst second year undergraduates, although the reasons for this warrant further investigation. High levels of mental distress and low wellbeing have also been reported amongst postgraduate research students (Byrom et al., 2020 ). Understanding the predictors of wellbeing at different stages of the university experience is vital for ensuring student support services are tailored appropriately.
University students experience many stressors including assessments, financial difficulties, relationship and family difficulties, and job insecurity. Lazarus and Folkman’s ( 1984 ) transactional model of stress conceptualises perceived stress as an individual’s appraisal of their circumstances as stressful in relation to their ability to cope. High perceived stress has been associated with higher levels of mental health difficulties, including anxiety and depression (Stowell et al., 2021 ). Perceived stress, particularly relating to assessment, has been shown to be a strong predictor of student mental health and wellbeing (Denovan & Macaskill, 2017 ; McIntyre et al., 2018 ; Neves & Hillman, 2019 ).
Psychosocial Resources
Research into the determinants of wellbeing has emphasised the importance of psychosocial factors and resources in underpinning an individual’s approach and response to life circumstances, which in turn influences their outlook and mental wellbeing (Diener et al., 1999 ). Three such factors are loneliness, resilience and sense of coherence.
Loneliness has also been shown to be an important determinant of student wellbeing and mental distress (McIntyre et al., 2018 ). Although – and possibly because – university is often championed as a time of increased social connectedness, where students will meet life-long friends or romantic partners, increasing numbers of students report feeling lonely (Diehl et al., 2018 ). This issue is especially acute for commuter students who remain more connected to their family and childhood friendships than their academic peers (Office for Students, 2020a ). This can also create a disconnect for these students both socially and intellectually when ‘transitioning’ back into their home lives and mixing with family and peers who may not have attended university themselves (Office for Students, 2020b ).
Resilience is here conceptualised as a process by which an individual ‘bounces back’ from adversity (Fletcher and Sarkar, 2013 ; Windle, 2011 ), enabling them to respond to stressful situations in a positive way and both maintain their wellbeing and/or use the experience to flourish by developing their personal skills and resources. Resilience has been strongly associated with subjective and psychological wellbeing, including mental health difficulties, in a variety of populations (Smith et al., 2008 ; Windle, 2011 ), including young adults (Campbell-Sills et al., 2006 ). Understanding and supporting the development of resilience has been highlighted as a key priority within higher education policy and practice (McIntosh & Shaw, 2017 ).
Sense of coherence (SOC) stems from Antonovsky’s ( 1987 ) salutogenic approach to stress and health – focussing on the factors and resources that help people maintain their health and wellbeing in the face of life’s challenges. SOC is thought to develop in early adulthood and remain stable across the life course (Antonovsky, 1987 ; Hakanen et al., 2007 ). It incorporates three dimensions: meaningfulness (whether one’s life conveys purpose and meaning), comprehensibility (whether the circumstances of one’s life make sense and are understandable), and manageability (whether a person feels they can cope with the circumstances of their life). There are similarities between these dimensions and other psychological constructs, most notably purpose and meaning (Ryff & Keyes, 1995 ), self-determination theory (Ryan & Deci, 2000 ), and self-efficacy (Bandura, 1977 ). SOC is theorised to play a mediating role, enabling individuals to mobilise psychosocial resources such as personality and social support to ensure successful coping and adaptation in response to adversity. This theory has been confirmed empirically in adults (Gana, 2001 ), and older adults (Wiesmann & Hannich, 2013 ). Sense of coherence has been strongly associated with both physical and mental health (Eriksson, 2022 ). However, very little research has hitherto investigated its role in facilitating student wellbeing.
Drawing together the theory and evidence presented, we propose the model of wellbeing in students outlined in Fig. 1 . In essence, how a student feels (particularly how stressed they feel) will influence how they rate their wellbeing. A student’s perceived stress will be influenced by what is happening to them (including background demographics and current circumstances) and their ability to cope with challenges (represented by psychosocial resources such as resilience, sense of coherence, and social support). Overall, a student’s wellbeing will be influenced by a combination of these three—circumstances, psychosocial resources, and perceived stress.
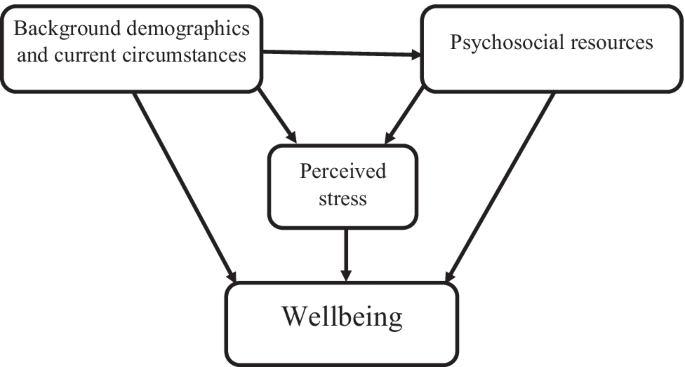
Proposed model of wellbeing in students
The current study aimed to test this model of wellbeing in a student population at a large, city-based university in the UK. We adopted a salutogenic approach, focussing on the factors that enhance positive mental wellbeing in students, in contrast to the pathogenic approach adopted by most previous research on the wellbeing of students, which focusses on mental health and illness (Hernández-Torrance et al., 2020). The study was innovative in both the salutogenic approach and in comparing wellbeing and its determinants across all levels and subjects of university study, whereas much previous research has focussed on individual year groups or subjects.
Based on previous literature, and the proposed model of wellbeing, the study aimed to address the following hypotheses:
1. Commuter and residential students will differ on measures of wellbeing, perceived stress, and psychosocial resources.
2. Scores on measures of wellbeing, perceived stress, and psychosocial resources will differ across different levels of study.
3. A significant amount of variance in wellbeing will be explained by a model containing background demographics / circumstances, psychosocial resources (resilience, sense of coherence, and loneliness) and perceived stress.
4. Each component or step of the model will explain a significant amount of variance in wellbeing.
A cross-sectional correlational design was conducted with mental wellbeing as the dependent variable and demographics (age, gender, residential status, level of study, number of stressors), psychosocial resources (resilience, sense of coherence, loneliness) and perceived stress as predictor variables.
Participants
All students currently registered at a large post-92 university in the north west of England, UK (N = ~ 20,000), were invited via email to participate in the study, which was conducted online in February-April 2018. Due to the success of widening participation initiatives, the student population at this university is diverse and includes a good balance of commuter and residential students. It is, therefore, well placed to provide a representative sample of university students in the UK. 574 students (mean age = 24.51, s.d. = 8.39, range 17–67) completed at least part of the online questionnaire. 376 (65.5%) were female, 112 (19.5%) male, 4 (0.7%) other, 2 (0.3%) prefer not to say, and 80 (13.9%) did not answer the gender question.
Demographics
Participants were asked to give their gender and age in years, the main subject area of their degree (based on the university’s administrative structure), and their level of study from 3 (foundation year) through 4–6 (undergraduate 1 st to 3 rd year) up to 7 (postgraduate masters level) and 8 (doctorate). Due to small numbers of students from level 3, levels 3 and 4 were collapsed into one category for statistical analysis.
Residential status
Participants were asked to indicate whether their living status was “at home, commuting into university” or “living with other students in halls or shared accommodation”. If neither of these, they were asked to provide more details. The responses were grouped into four categories: commuter, residential, postgrad/mature (incorporating students who owned their own home or lived alone AND were at level 7 or 8), and other. Only one student fell into the ‘Other’ category – they reported living in halls during the week and returning home at weekends for paid work purposes.
Experiences and Causes of Stress
Participants were asked to indicate whether, during their time at university, they had ever felt unusually stressed or overwhelmed. They were then asked to indicate their primary sources of stress using the following question: “If you have felt or think you ever would feel increased stress or pressure, what would be the main trigger?”. Response options were pre-determined based on previous literature and student consultation and included managing university workload, personal problems outside of university work, social worries, money worries, concerns about finding a job after university, difficulty settling into Liverpool, loneliness, and other. Further information given in the ‘other’ category was used to further categorise common stressors. The total number of stressors (or potential stressors) reported was calculated for each participant.
Mental Wellbeing
The Warwick Edinburgh Mental Wellbeing Scale (Tennant et al., 2007 ) was used to measure mental wellbeing. Participants were asked to indicate, on a Likert-type scale of 1–5, the extent to which they had experienced 14 positively-worded statements during the last 2 weeks. Possible scores range from 14–70, with high scores indicating greater mental wellbeing.
Sense of Coherence
The 13-item Orientation to Life Scale (Antonovsky, 1987 ) was used to measure SOC. Participants were asked to respond to a series of statements covering the three dimensions of meaningfulness (SOC Me), comprehensibility (SOC Co), and manageability (SOC Ma), on a Likert-type scale of 1–7. After reversal of appropriate items, scores are calculated for each of the dimensions and the total (range 13–91), with higher scores indicating a higher sense of coherence.
The Brief Resilience Scale (BRS; Smith et al., 2008 ) was used to measure resilience. This consists of 6 items, on a scale of 1–5. After reversal of three items, the mean score of all 6 items was calculated, with higher scores indicating higher resilience.
Perceived Stress
The Perceived Stress Scale (PSS; Cohen et al., 1983 ) was used. Participants were asked to read a series of 10 statements and indicate, on a four-point scale from 0–4 from Never to Very often, the extent to which this was true of them over the last month. After appropriate reversals, scores are summed to give a total perceived stress with a range of 0–40, higher scores indicating greater stress.
This was measured using a single item: “Loneliness can be a serious problem for some people and not for others. At the present moment do you feel lonely?” This item has been used in a number of longitudinal cohort studies and has been shown to be strongly associated with measures of subjective wellbeing (Gow et al., 2007 ). Participants provided their response on a five point scale from Most of the time (1) to None of the time (5), with higher scores indicating lower loneliness.
Participants were presented with the participant information sheet online. Consent was implied by completion of the study questionnaire. Participants were then invited to complete the questionnaires, which took an average of 23 minutes. All participants were fully debriefed on completion of the study.
Ethical Considerations
Ethical approval for the study was granted by the appropriate university Research Ethics Committee (REF: 18/NSP/0008). Participants were informed of the purpose and nature of the study in the participant information sheet. Consent was implied by completion of the study questionnaire. All data was fully anonymous at the point of collection and participants were debriefed at the end of the study.
Statistical Analysis
Independent sample t-tests were used to compare commuter and residential students and one-way ANOVA to investigate the effect of level of study on resilience, SOC, loneliness, perceived stress, number of stressors, and wellbeing.
Pearson bivariate correlations were calculated to investigate associations between all the predictor variables and mental wellbeing.
Hierarchical linear regression analysis was then conducted to test the effect of the predictor variables on mental wellbeing. Level of study was recoded as dummy variables, with level 3–4 as the reference, in order to ascertain differences in wellbeing across levels. Variables were entered into the model based on the proposed model of wellbeing. Age, gender, level of study dummy variables and number of stressors were entered at the first step, resilience, SOC and loneliness at the second, and perceived stress at the third step.
Summary demographics, including experiences of stress and number of stressors, for all participants are presented in Table 1 .
Due to small numbers in level 3 (foundation year), levels 3 and 4 were collapsed into one category for all inferential analyses. Overall, 526 (91.6%) participants reported having felt unusually stressed or overwhelmed since starting university, citing a mean number of 3.17 (S.D. = 1.51) stressors. Chi squared tests indicated significant differences between levels of study (X 2 (4, N = 494) = 15.274, p < 0.01), with students at levels 5, 6, and 8 more likely to report having experienced stress while at university – this was echoed in the number of stressors reported (F(4,489) = 11.341, p < 0.001).
Descriptive statistics for all psychological variables for all participants, and divided by gender, residential status, and level of study, are shown in Table 2 . Independent samples t-tests indicated that females reported significantly higher perceived stress (t(476) = -3.145, p < 0.01), lower resilience (t(486) = 2.912, p < 0.01), and lower SOC manageability (t(481) = 2.746, p < 0.01) than males.
Residential Status
Independent samples t-tests indicated that residential students reported significantly higher loneliness (t(452) = 3.580, p < 0.001) and a greater number of stressors (t(451.353) = -5.820, p < 0.001) than commuter students. No other differences were significant at the p < 0.01 level.
Level of Study
One-way ANOVAs indicated significant differences in scores between students at different levels of study, with post-hoc tests suggesting greater wellbeing (F(4,475) = 8.109, p < 0.001), resilience (F(4,489) = 5.521, p < 0.001), lower perceived stress (F(4,479) = 6.511, p < 0.001), and lower loneliness (F(4,489) = 6.103, p < 0.001) amongst the two postgraduate groups (levels 7 and 8, masters and PhD) compared to the three undergraduate groups.
Postgraduate students at level 7 and 8 also reported greater scores on the measure of sense of coherence (F(4,466) = 8.781, p < 0.001) and its subscales: meaningfulness (F(4,484) = 9.240, p < 0.001), comprehensibility (F(4,475) = 6.981, p < 0.001), and manageability (F(4,484) = 6.508, p < 0.001).
Determinants of Wellbeing
Bivariate correlations (Table 3 ) showed significant associations between mental wellbeing and all the predictor variables. All were in the expected direction: higher resilience, higher SOC, lower perceived stress, and lower loneliness were all associated with higher wellbeing. Older age and higher year of study were also associated with higher wellbeing. The strongest associations were between wellbeing and perceived stress and SOC.
The hierarchical linear regression analysis results are shown in Table 4 . All three models significantly predicted wellbeing. Demographics explained 17.5% of the variance (model F(7, 425) = 14.13, p < 0.001), psychosocial resources explained an additional 44.1% (model F(10, 422) = 71.94, p < 0.001) and perceived stress explained an additional 9.4% (model F(11, 421) = 100.78, p < 0.001). The final model explained 71.8% of the variance in wellbeing. The strongest predictors were perceived stress, SOC, loneliness, and resilience. Age, gender, level of study, and number of stressors all did not reach significance in the final model. All assumptions of linear regression were met.
The findings show that commuter and residential students did not differ significantly on measures of wellbeing or psychosocial resources, although residential students did report greater loneliness and a higher number of stressors. Postgraduate students reported greater wellbeing, resilience, and SOC, and lower perceived stress and loneliness than undergraduate students. In terms of determinants of wellbeing, over 70% of the variance in wellbeing was explained by the final model, with SOC, perceived stress, loneliness, and resilience all making significant independent contributions and each model component predicting significant variance in wellbeing.
The observed differences between commuter and residential students were, perhaps, encouraging. While the findings contrast with previous research (Neves & Hillman, 2019 ) and our first hypothesis, they are not altogether surprising. Commuter students are often living within the family home, providing them with greater access to companionship and support and removing the personal stressors associated with transition to university such as the need to make new social connections and manage one’s own household and finances. Postgraduate and mature students – who are often more settled in their residential status – reported better outcomes on all measures, although this again is unsurprising given the considerable differences in life circumstances between this group and other students.
Level of study appears to have had a significant impact on experiences of stress, mental wellbeing, and all psychosocial variables. Postgraduate students in general reported higher levels of wellbeing, resilience, and SOC, and lower loneliness and perceived stress, which contrasts with previous research (Byrom et al., 2020 ) – although doctoral students were more likely to report having experienced stress. Undergraduates in their 2 nd and 3 rd year reported a greater number of stressors, lower wellbeing, and higher perceived stress than the other groups, which is in keeping with previous research (Bewick et al., 2010 ; Macaskill, 2013 ).
The data support our proposed model of wellbeing, with each component of the model explaining significant variance in wellbeing. Psychosocial resources contributed the greatest amount of variance, which is in keeping with previous research (Brett et al., 2012 ; Diener et al., 1999 ; McIntyre et al., 2018 ).
Perceived stress was the strongest predictor of wellbeing in this study. The number of stressors reported, while significantly associated with wellbeing in univariate analyses and in step 1 of the hierarchical regression, did not reach significance in the final model, suggesting that how stressors are perceived by students is more important than the number of stressors experienced. This is in keeping with previous studies and the conceptualisation of perceived stress (Denovan & Macaskill, 2017 ; Lazarus & Folkman, 1984 ).
The finding that SOC and resilience were both significant predictors of wellbeing – even after controlling for the more proximal measures of perceived stress and loneliness – suggests these more stable psychological variables have a role to play in enabling students to maintain their wellbeing in the face of stress and adversity, and supports the adoption of a salutogenic approach to wellbeing in students, focussing on the factors that help students manage their stress and maintain their wellbeing, rather than mental health and illness (Antonovsky, 1987 ; Chu et al., 2016 ; Hernández-Torrano et al., 2020 ). Indeed, there is increasing awareness of the importance of resilience and interventions to enhance resilience amongst young people, including students, has become a key priority in higher education (McIntosh & Shaw, 2017 ) and public health (Association for Young People’s Health, 2016 ). Multi-faceted, skills-based interventions have been shown to be effective in a variety of populations, with interventions combining Cognitive Behavioural Therapy techniques and mindfulness training proving effective in universities (Joyce et al., 2018 ). In contrast, despite its importance in promoting optimal functioning and wellbeing, there is a paucity of literature on the development of SOC (Joseph & Sagy, 2017 ). This is particularly the case in young people, with much research on SOC focussing on its role in promoting wellbeing in older adults.
Limitations
The current study has a number of limitations which affect the generalisability of its findings. The study took place within a single, city-based, higher education institution in a city in northwest England. Although the city is culturally and socioeconomically diverse, the findings may not be generalisable to other student populations. In particular, the experience of residential students on campus-based universities may be qualitatively different, with greater opportunities to meet other students and make friends. However, the study findings suggest – contrary to previous research – that residential status did not have an impact on wellbeing, although loneliness and perceived stress – two significant predictors of wellbeing – were higher amongst residential students.
A further limitation is the possibility of sample bias. The sample size of 574 represents only a small proportion (2.87%) of the 20,000 active students at the institution. Practical factors likely influenced this low response rate: the study invitation originated from an academic unknown to the majority of students, and via a generic student mailing list. However, it is also possible that participation was influenced by psychological factors that might have had a confounding effect on the study findings. First, although the male:female ratio at the institution is roughly 50:50, females were overrepresented in the study sample. Second, participating in a study on wellbeing might appeal more to students who are interested in this topic, either on a personal or academic level. Third, the survey invitation was sent out towards the end of semester two of the academic year, which can be a time of high stress due to the large number of assessment deadlines, resulting in low engagement with activities unrelated to assessment. Indeed, in Bewick et al.’s ( 2010 ) study, wellbeing was lowest and anxiety highest during semester two. However, as this was a cross-sectional study with all participants completing the survey during the same time period, the impact of this on the study findings will have been attenuated.
The final, key, limitation is that this study did not measure any potential mediating or moderating factors that might explain the relationship between the predictor variables and wellbeing. For example, personality traits are likely to contribute to students’ susceptibility to experience stress, while understanding students’ social connectedness – including social networks and social support – might further explain the observed differences in loneliness between residential and commuter students.
Implications and Conclusion
It is well documented that university can be a time of great stress for students (Neves & Hillman, 2019 ), which can lead to high levels of mental health difficulties among the student population (Royal College of Psychiatrists, 2011 ; Brown, 2018 ; Hughes & Spanner, 2019 ). This study found support for a new model of wellbeing which emphasises the importance of perceived stress and psychosocial resources including resilience, sense of coherence, and loneliness in determining wellbeing in students – over and above demographic variables, current circumstances, and the number of stressors experienced. It may be well-nigh impossible for universities to reduce the stressors experienced by students due to the difficulties of balancing assessment demands and student wellbeing (Jones et al., 2021 ), and the financial pressures resulting from government policy (Johnson & Crenna-Jennings, 2018 ). However, adopting a salutogenic approach by prioritising interventions to enhance students’ ability to cope with stressors might, therefore, help them maintain or improve their wellbeing and prevent the development of mental health difficulties. The results also suggest that reducing loneliness – for example by facilitating social connectedness amongst students – might also help improve wellbeing, particularly amongst residential students.
Further research is needed to fully understand the development of resilience and sense of coherence within the student population, and the mechanisms underlying their relationship with wellbeing. The model of wellbeing proposed here could be further developed to incorporate additional psychosocial factors such as personality, social support, optimism, and current mood. Finally, longitudinal research is needed to identify and understand the changes in wellbeing and its determinants that occur throughout the university journey.
Antonovsky, A. (1987). Unraveling the mystery of health . Jossey-Bass.
Google Scholar
Association for Young People’s Health. (2016). A public health approach to promoting young people’s resilience : A guide to resources for policy makers, commissioners, and service planners and providers . https://www.youngpeopleshealth.org.uk/wp-content/uploads/2016/03/resilience-resource-15-march-version.pdf .
Auerbach, R. P., Mortier, P., Bruffaerts, R., Alonso, J., Benjet, C., Cuijpers, P., Demyttenaere, K., Ebert, D. D., Green, J. G., Hasking, P., Murray, E., Nock, M. K., Pinder-Amaker, S., Sampson, N. A., Stein, D. J., Vilagut, G., Zaslavsky, A. M., Kessler, R. C., WHO WMH-ICS Collaborators. (2018). WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. Journal of Abnormal Psychology, 127 (7), 623–638. https://doi.org/10.1037/abn0000362
Article PubMed PubMed Central Google Scholar
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioural change. Psychological Review , 84 , 191–215. https://doi.org/10.1037/0033-295X.84.2.191
Barkham, M., Broglia, E., Dufour, G., Fudge, M., Knowles, L., Percy, A., Turner, A., Williams, C., SCORE Consortium. (2019). Towards an evidence-base for student wellbeing and mental health: Definitions, developmental transitions and data sets. Counselling and Psychotherapy Research, 19 (4), 351–357. https://doi.org/10.1002/capr.12227
Article Google Scholar
Bewick, B., Koutsopoulou, G., Miles, J., Slaa, E., & Barkham, M. (2010). Changes in undergraduate students’ psychological well-being as they progress through university. Studies in Higher Education, 35 , 633–645. https://doi.org/10.1080/03075070903216643
Blackman, T. (2020). What affects student wellbeing? Health Education Policy Institute Policy Note 21.
Brett, C. E., Gow, A. J., Corley, J., Pattie, A., Starr, J. M., & Deary, I. J. (2012). Psychosocial factors and health as determinants of quality of life in community-dwelling older adults. Quality of Life Research, 21 , 505–516. https://doi.org/10.1007/s11136-011-9951-2
Article PubMed Google Scholar
Brown, J. S. L. (2018). Student mental health: Some answers and more questions. Journal of Mental Health, 27 (3), 193–196. https://doi.org/10.1080/09638237.2018.1470319
Byrom, N. C., Dinu, L., Kirkman, A., & Hughes, G. (2020). Predicting stress and mental wellbeing among doctoral researchers. Journal of Mental Health . https://doi.org/10.1080/09638237.2020.1818196 .
Campbell-Sills, L., Cohan, S. L., & Stein, M. B. (2006). Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behaviour Research and Therapy , 44 (4), 585–599. https://doi.org/10.1016/j.brat.2005.05.001
Chu, J. J., Khan, M. H., Jahn, H. J., & Kraemer, A. (2016). Sense of coherence and associated factors among university students in China: Cross-sectional evidence. BMC Public Health, 16 , 336. https://doi.org/10.1186/s12889-016-3003-3
Cleary, M., Walter, G., & Jackson, D. (2011). Not always smooth sailing: mental health issues associated with the transition from high school to college. Issues in Mental Health Nursing, 32 , 250–254. https://doi.org/10.3109/01612840.2010.548906
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24 , 385–396. https://doi.org/10.2307/2136404
Denovan, A., & Macaskill, A. (2017). Stress and subjective wellbeing among first year UK undergraduate students. Journal of Happiness Studies, 18 , 505–525. https://doi.org/10.1007/s10902-016-9736-y
Diehl, K., Jansen, C., Ishchanova, K., & Hilger-Kolb, J. (2018). Loneliness at universities: determinants of emotional and social loneliness among students. International Journal of Environmental Research and Public Health, 15 (9), 1865. https://doi.org/10.3390/ijerph15091865
Diener, E., Suh, E. M., Lucas, R. E., & Smith, H. L. (1999). Subjective well-being: Three decades of progress. Psychological Bulletin, 125 , 276–302. https://doi.org/10.1037/0033-2909.125.2.276
Eriksson, M. (2022). The sense of coherence: The concept and its relationship to health. In M. B. Mittelmark M. B. Mittelmark, G. F. Bauer, L. Vaandrager, J. M. Pelikan, S. Sagy, M. Eriksson, B. Lindström, & C. M. Magistretti (Eds.) The Handbook of Salutogenesis (2nd ed). Springer. https://doi.org/10.1007/978-3-030-79515-3_9 .
Fletcher, D., & Sarkar, M. (2013). Psychological resilience: A review and critique of definitions, concepts, and theory. European Psychologist, 18 (1), 12. https://doi.org/10.1027/1016-9040/a000124
Gana, K. (2001). Is sense of coherence a mediator between adversity and psychological well-being in adults? Stress and Health: Journal of the International Society for the Investigation of Stress, 17 , 77–83. https://doi.org/10.1002/smi.882
Gow, A. J., Pattie, A., Whiteman, M. C., Whalley, L. J., & Deary, I. J. (2007). Social support and successful aging: Investigating the relationship between lifetime cognitive change and life satisfaction. Journal of Individual Differences, 28 , 103–115. https://doi.org/10.1027/1614-0001.28.3.103
Hakanen, J. J., Feldt, T., & Leskinen, E. (2007). Change and stability of sense of coherence in adulthood: Longitudinal evidence from the Healthy Child study. Journal of Research in Personality, 41 , 602–617. https://doi.org/10.1016/j.jrp.2006.07.001
Hernández-Torrano, D., Ibrayeva, L., Sparks, J., Lim, N., Clementi, A., Alumkhambetova, A., Nurtayev, Y., & Muratkyzy, A. (2020). Mental health and wellbeing of university students: A bibliometric mapping of the literature. Frontiers in Psychology, 11 , 1226. https://doi.org/10.3389/fpsyg.2020.01226
Hughes, G., & Spanner, L. (2019). The University Mental Health Charter . Student Minds.
Johnson, K. & Crenna-Jennings, W. (2018). Prevalence of mental health issues within the student-aged population. https://epi.org.uk/publications-and-research/prevalence-of-mental-health-issues-within-the-student-aged-population/ .
Jones, S. (2020) If more students choose home over halls, it's time to celebrate . The Guardian. https://www.theguardian.com/education/2020/jun/30/if-more-students-choose-home-over-halls-its-time-to-celebrate .
Jones, E., Priestley, M., Brewster, L., Wilbraham, S. J., Hughes, G., & Spanner, L. (2021). Student wellbeing and assessment in higher education: The balancing act. Assessment & Evaluation in Higher Education, 46 (3), 438–450. https://doi.org/10.1080/02602938.2020.1782344
Joseph, S., & Sagy, S. (2017). Positive psychology in the context of salutogenesis. In M. B. Mittelmark, S. Sagy, M. Eriksson, G. F. Bauer, J. M. Pelikan, B. Lindström, G. A. Espnes, (Eds). The Handbook of Salutogenesis (pp. 83–88). Springer. https://doi.org/10.1007/978-3-319-04600-6 .
Joyce, S., Shand, F., Tighe, J., Lauren, S. J., Bryant, R. A., & Harvey, S. B. (2018). Road to resilience: A systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open, 8 , e017858. https://doi.org/10.1136/bmjopen-2017-017858
Kessler, R. C., Amminger, G. P., Aguilar-Gaxiola, S., Alonso, J., Lee, S., & Ustun, T. B. (2007). Age of onset of mental disorders: A review of recent literature. Current Opinions in Psychiatry, 20 (4), 359–364. https://doi.org/10.1097/YCO.0b013e32816ebc8c
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping . Springer publishing company.
Lipson, S. K., & Eisenberg, D. (2018). Mental health and academic attitudes and expectations in university populations: results from the healthy minds study. Journal of Mental Health, 27 (3), 205–213. https://doi.org/10.1080/09638237.2017.1417567
Macaskill, A. (2013). The mental health of university students in the United Kingdom. British Journal of Guidance & Counselling, 41 (4), 426–441. https://doi.org/10.1080/03069885.2012.743110
McIntosh, E. & Shaw, J. (2017) Student Resilience: Exploring the Positive Case for Resilience (Unite Group). www.unite-group.co.uk/sites/default/files/2017-05/student-resilience.pdf .
McIntyre, J. C., Worsley, J., Corcoran, R., Harrison Woods, P., & Bentall, R. P. (2018). Academic and non-academic predictors of student psychological distress: The role of social identity and loneliness. Journal of Mental Health, 27 (3), 230–239. https://doi.org/10.1080/09638237.2018.1437608
Neves, J., & Hillman, N. (2019). Student academic experience survey 2019 . Health Education Policy Institute and Advance HE.
Office for Students (2020a) Local and commuter students: challenges and opportunities https://www.officeforstudents.org.uk/advice-and-guidance/promoting-equal-opportunities/effective-practice/local-and-commuter-students/ .
Office for Students (2020b) Update to associations between characteristics of students (ABCS). How do outcomes differ when accounting for multiple student characteristics? https://www.officeforstudents.org.uk/media/1bbaaa77-b9e9-4110-b778-19c0b5201805/abcs_2020b_update_final_for_web_2021.pdf .
Pollard, E. H. C., Martin, A., Takala, H., & Byford, M. (2019). Impact of the student finance system on participation, experience and outcomes of disadvantaged young people Literature review . Department of Education.
Royal College of Psychiatrists. (2011). The mental health of students in higher education . Royal College of Psychiatrists.
Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55 , 68–78. https://doi.org/10.1037//0003-066x.55.1.68
Ryff, C. D., & Keyes, C. L. (1995). The structure of psychological well-being revisited. Journal of Personality and Social Psychology, 69 , 719–727. https://doi.org/10.1037//0022-3514.69.4.719
Smith, B. W., Dalen, J., Wiggins, K., Tooley, E., Christopher, P., & Bernard, J. (2008). The Brief Resilience Scale: Assessing the ability to bounce back. International Journal of Behavioural Medicine, 15 , 194–200. https://doi.org/10.1080/10705500802222972
Stowell, D., Lewis, R. K., & Brooks, K. (2021). Perceived stress, substance use, and mental health issues among college students in the Midwest. Journal of Prevention & Intervention in the Community, 49 (3), 221–234. https://doi.org/10.1080/10852352.2019.1654263
Tennant, R., Hiller, L., Fishwick, R., Platt, S., Joseph, S., Weich, S., Parkinson, J., Secker, J., & Stewart-Brown, S. (2007). The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health and Quality of Life Outcomes, 5 , 63. https://doi.org/10.1186/1477-7525-5-63
Wiesmann, U., & Hannich, H.-J. (2013). The contribution of resistance resources and sense of coherence to life satisfaction in older age. Journal of Happiness Studies, 14 , 911–928. https://doi.org/10.1007/s10902-012-9361-3
Windle, G. (2011). What is resilience? A review and concept analysis. Reviews in Clinical Gerontology, 21 (2), 152–169. https://doi.org/10.1017/S0959259810000420
Download references
Author information
Authors and affiliations.
School of Psychology, Liverpool John Moores University, Byrom Street, Liverpool, L3 3AF, UK
Caroline E. Brett & Michelle L. Mathieson
School of Education, Liverpool John Moores University, Liverpool, UK
Avril M. Rowley
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by MLM and CEB. First and subsequent drafts of the manuscript were written by CEB and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Caroline E. Brett .
Ethics declarations
This work was funded by a Curriculum Enhancement grant from Liverpool John Moores University awarded to CEB and AMR and on which MLM was employed.
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
The questionnaire and methodology for this study was approved by the Research Ethics Committee of Liverpool John Moores University (REF: 18/NSP/0008).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Data availability
The datasets generated during and/or analysed during the current study are available in the LJMU Data Repository, https://opendata.ljmu.ac.uk/ .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Brett, C.E., Mathieson, M.L. & Rowley, A.M. Determinants of wellbeing in university students: The role of residential status, stress, loneliness, resilience, and sense of coherence. Curr Psychol 42 , 19699–19708 (2023). https://doi.org/10.1007/s12144-022-03125-8
Download citation
Accepted : 15 April 2022
Published : 26 April 2022
Issue Date : August 2023
DOI : https://doi.org/10.1007/s12144-022-03125-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sense of coherence
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 28 March 2024
Medical student wellbeing during COVID-19: a qualitative study of challenges, coping strategies, and sources of support
- Helen M West ORCID: orcid.org/0000-0001-8712-5890 1 ,
- Luke Flain ORCID: orcid.org/0000-0001-7296-6304 2 ,
- Rowan M Davies 3 , 4 ,
- Benjamin Shelley 3 , 5 &
- Oscar T Edginton ORCID: orcid.org/0000-0001-5298-9402 3 , 6
BMC Psychology volume 12 , Article number: 179 ( 2024 ) Cite this article
245 Accesses
Metrics details
Medical students face challenges to their mental wellbeing and have a high prevalence of mental health problems. During training, they are expected to develop strategies for dealing with stress. This study investigated factors medical students perceived as draining and replenishing during COVID-19, using the ‘coping reservoir’ model of wellbeing.
In synchronous interactive pre-recorded webinars, 78 fourth-year medical students in the UK responded to reflective prompts. Participants wrote open-text comments on a Padlet site. Responses were analysed using reflexive thematic analysis.
Analysis identified five themes. COVID-19 exacerbated academic pressures, while reducing the strategies available to cope with stress. Relational connections with family and friends were affected by the pandemic, leading to isolation and reliance on housemates for informal support. Relationships with patients were adversely affected by masks and telephone consultations, however attending placement was protective for some students’ wellbeing. Experiences of formal support were generally positive, but some students experienced attitudinal and practical barriers.
Conclusions
This study used a novel methodology to elicit medical students’ reflections on their mental wellbeing during COVID-19. Our findings reinforce and extend the ‘coping reservoir’ model, increasing our understanding of factors that contribute to resilience or burnout. Many stressors that medical students typically face were exacerbated during COVID-19, and their access to coping strategies and support were restricted. The changes to relationships with family, friends, patients, and staff resulted in reduced support and isolation. Recognising the importance of relational connections upon medical students’ mental wellbeing can inform future support.
Peer Review reports
Medical students are known to experience high levels of stress, anxiety, depression and burnout due to the nature, intensity and length of their course [ 1 ]. Medical students are apprehensive about seeking support for their mental wellbeing due to perceived stigma and concerns about facing fitness to practice proceedings [ 2 ], increasing their vulnerability to poor mental health.
Research has identified that the stressors medical students experience include a demanding workload, maintaining work–life balance, relationships, personal life events, pressure to succeed, finances, administrative issues, career uncertainty, pressure around assessments, ethical concerns, and exposure to patient death [ 3 , 4 ]. In March 2020, the COVID-19 pandemic introduced additional stressors into medical students’ lives. These included sudden alterations to clinical placements, the delivery of online teaching, uncertainty around exams and progression, ambiguity regarding adequate Personal Protective Equipment (PPE), fear of infection, and increased exposure to death and dying [ 5 , 6 ]. Systematic reviews have reported elevated levels of anxiety, depression and stress among medical students during COVID-19 [ 7 ] and that the prevalence of depression and anxiety during COVID-19 was higher among medical students than in the general population or healthcare workers [ 8 ].
While training, medical students are expected to develop awareness of personal mental wellbeing and learn healthy coping strategies for dealing with stress [ 9 ]. Developing adaptive methods of self-care and stress reduction is beneficial both while studying medicine, and in a doctor’s future career. Protecting and promoting psychological wellbeing has the potential to improve medical students’ academic attainment, as well as their physical and mental wellbeing [ 10 ], and it is therefore important for medical educators to consider how mental wellbeing is fostered. Feeling emotionally supported while at medical school reduces the risk of psychological distress and burnout, and is related to whether students contemplate dropping out of medical training [ 11 ]. In their systematic narrative review of support systems for medical students during COVID-19, Ardekani et al. [ 12 ] propose a framework incorporating four levels: policies that promote a supportive culture and environment, active support for students at higher risk of mental health problems, screening for support needs, and provision for students wishing to access support. This emphasis on preventative strategies aligns with discussions of trauma-informed approaches to medical education, which aim to support student learning and prevent harm to mental wellbeing [ 13 ]. Dunn et al. [ 14 ] proposed a ‘coping reservoir’ model to conceptualise the factors that deplete and restore medical students’ mental wellbeing (Fig. 1 ). This reservoir is drained and filled repeatedly, as a student faces demands for their time, energy, and cognitive and emotional resources. This dynamic process leads to positive or negative outcomes such as resilience or burnout.
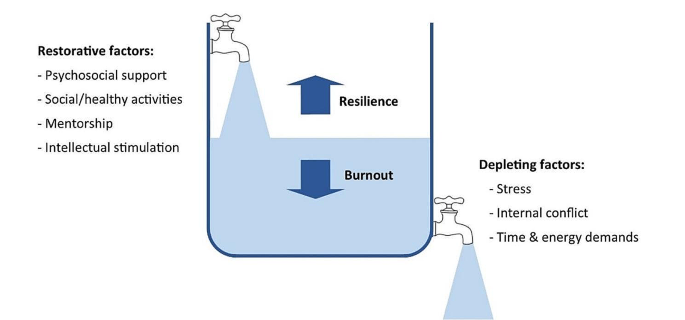
Coping reservoir model– adapted from Dunn et al. [ 14 ], with permission from the authors and Springer Nature
At present we have limited evidence to indicate why medical students’ mental wellbeing was so profoundly affected by COVID-19 and whether students developed coping strategies that enhanced their resilience, as suggested by Kelly et al. [ 15 ]. This study therefore sought to conceptualise the challenges medical students experienced during COVID-19, the coping strategies they developed in response to these stressors, and the supportive measures they valued. The ‘coping reservoir’ model [ 14 ] was chosen as the conceptual framework for this study because it includes both restorative and depleting influences. Understanding the factors that mediate medical students’ mental wellbeing will enable the development of interventions and support that are effective during crises such as the pandemic and more generally.
Methodology
This research study is based on a critical realist paradigm, recognising that our experience of reality is socially located [ 16 ]. Participant responses were understood to represent a shared understanding of that reality, acknowledging the social constructivist position that subjective meanings are formed through social norms and interactions with others, including while participating in this study. It also draws on hermeneutic phenomenology in aiming to interpret everyday experienced meanings for medical students during COVID-19 [ 17 ]. The use of an e-learning environment demonstrates an application of connectivism [ 18 ], a learning theory in which students participate in technological enabled networks. We recognise that meaning is co-constructed by the webinar content, prompts, ‘coping reservoir’ framework and through the process of analysis.
The multidisciplinary research team included a psychologist working in medical education, two medical students, and two Foundation level doctors. The team’s direct experience of the phenomenon studied was an important resource throughout the research process, and the researchers regularly reflected on how their subjective experiences and beliefs informed their interpretation of the data. Reflexive thematic analysis was chosen because it provides access to a socially contextualised reality, encompasses both deductive and inductive orientations so that analysis could be informed by the ‘coping reservoir’ while also generating unanticipated insights, and enables actionable outcomes to be produced [ 19 ].
Ethical approval
Approval was granted by the University of Liverpool Institute of Population Health Research Ethics Committee (Reference: 8365).
Participants
Fourth-year medical students at the University of Liverpool were invited to participate in the study during an online webinar in their Palliative Medicine placement. During six webinars between November 2020 and June 2021, 78 out of 113 eligible students participated, giving a response rate of 69%. This was a convenience sample of medical students who had a timetabled session on mental wellbeing. At the time, these medical students were attending clinical placements, however COVID-19 measures in the United Kingdom meant that academic teaching and support was conducted online, travel was limited, and contact with family and friends was restricted.
Students were informed about the study prior to the synchronous interactive pre-recorded webinar and had an opportunity to ask questions. Those who consented to participate accessed a Padlet ( www.padlet.com ) site during the webinar that provided teaching on mental wellbeing, self-care and resilience in the context of palliative medicine. Padlet is a collaborative online platform that hosts customisable virtual bulletin boards. During this recording, participants were asked to write anonymous open-text responses to reflective prompts developed from reviewing the literature (Appendix 1 ), and post these on Padlet. The Padlet board contained an Introduction to the webinar, sections for each prompt, links to references, and signposting to relevant support services. Data files were downloaded to Excel and stored securely, in line with the University of Liverpool Research Data Management Policy.
The research team used the six steps of reflexive thematic analysis to analyse the dataset. This process is described in Table 1 , and the four criteria for trustworthiness in qualitative research proposed by Lincoln and Guba [ 20 ] are outlined in Table 2 . We have used the purposeful approach to reporting thematic analysis recommended by Nowell et al. [ 21 ] and SRQR reporting standards [ 22 ] (Appendix 2 ).
Five themes were identified from the analysis:
COVID-19 exacerbated academic pressures.
COVID-19 affected students’ lifestyles and reduced their ability to cope with stress.
COVID-19 changed relationships with family and friends, which affected mental wellbeing.
COVID-19 changed interactions with patients, with positive and negative effects.
Formal support was valued but seeking it was perceived as more difficult during COVID-19.
COVID-19 exacerbated academic pressures
‘Every day feels the same, it’s hard to find motivation to do anything.’
Many participants reported feeling under chronic academic pressure due to studying medicine. Specific stressors reported were exams, revision, deadlines, workload, specific course requirements, timetables, online learning, placement, and communication from University. Some participants also reported negative effects on their mental wellbeing from feelings of comparison and competition, feeling unproductive, and overthinking.
Massive amounts of work load that feels unachievable.
COVID-19 exacerbated these academic stresses, with online learning and monotony identified as particularly draining. However, other students found online learning beneficial, due to reduced travelling.
I miss being able to see people face to face and zoom is becoming exhausting. My mental wellbeing hasn’t been great recently and I think the effects of the pandemic are slowly beginning to affect me.
I also prefer zoom as it is less tiring than travelling to campus/placement.
Clinical placements provided routine and social interaction. However, with few social interactions outside placement, this became monotonous. A reduction in other commitments helped some students to focus on their academic requirements.
Most social activity only taking place on placement has made every day feel the same.
Some students placed high value on continuing to be productive and achieve academically despite the disruption of a pandemic, potentially to the detriment of their mental wellbeing. Time that felt unproductive was frustrating and draining.
Having a productive day i.e. going for a run and a good amount of work completed in the day.
Unproductive days of revision or on placement.
COVID-19 affected students’ lifestyles and reduced their ability to cope with stress
‘Everyone’s mental well-being decreased as things they used for mental health were no longer available’.
Students often found it difficult to sustain motivation for academic work without the respite of their usual restorative activities challenging.
Not being able to balance work and social life to the same extent makes you resent work and placement more.
The competing demands medical students encounter for their time and energy were repeatedly reported by participants.
Sometimes having to go to placement + travel + study + look after myself is really tough to juggle!
However, removing some of the boundaries around academic contact and structure of extracurricular activities heightened the impact of stressors. Many participants focused on organising and managing their time to cope with this. Students were aware that setting time aside for relaxation, enjoyment, creativity, and entertainment would be beneficial for their wellbeing.
Taking time off on the weekends to watch movies.
However, they found it difficult to prioritise these without feeling guilty or believing they needed to ‘earn’ them, and academic commitments were prioritised over mental wellbeing.
Try to stop feeling guilty for doing something that isn’t medicine. Would like to say I’d do more to increase my mental wellbeing but finals are approaching and that will probably have to take priority for the next few months.
Medical students were generally aware that multiple factors such as physical activity, time with loved ones, spiritual care, nourishment and hobbies had a positive impact on their mental wellbeing. During COVID-19, many of the coping strategies that students had previously found helpful were unavailable.
Initially it improved my mental well-being as I found time to care for myself, but with time I think everyone’s mental well-being decreased as things they used for mental health were no longer available e.g. gym, counselling, seeing friends.
Participants adapted to use coping strategies that remained available during the pandemic. These included walks and time spent outdoors, exercise, journaling, reflection, nutrition, and sleep.
'Running’. ‘Yoga’. ‘Fresh air and walks'.
A few students also reported that they tried to avoid unhelpful coping strategies, such as social media and alcohol.
Not reading the news, not using social media.
Avoiding alcohol as it leads to poor sleep and time wasted.
Many participants commented on increased loneliness, anxiety, low mood, frustration, and somatic symptoms.
Everyone is worn out and demotivated. Feel that as I am feeling low I don’t want to bring others down. ‘Feel a lot more anxious than is normal and also easily annoyed and irritable.’
However, not all students reported that COVID-19 had a negative effect on wellbeing. A small minority responded that their wellbeing had improved in some way.
I think covid-19 has actually helped me become more self reliant in terms of well-being.
COVID-19 changed relationships with family and friends, which affected mental wellbeing
‘Family are a huge support for me and I miss seeing them and the lack of human contact.’
Feeling emotionally supported by family and friends was important for medical students to maintain good mental wellbeing. However, COVID-19 predominantly had a negative impact on these relationships. Restrictions, such as being unable to socialise or travel during lockdowns, led to isolation and poor mental wellbeing.
Not being able to see friends or travel back home to see friends/family there.
Participants frequently reported that spending too much time with people, feeling socially isolated, being unable to see people, or having negative social experiences had an adverse effect on their mental wellbeing. Relationships with housemates were a key source of support for some students. However, the increased intensity in housemate relationships caused tension in some cases, which had a particularly negative effect.
Much more difficult to have relationships with peers and began feeling very isolated. Talk about some of the experiences I’ve had on placement with my housemates. Added strain on my housemates to be the only ones to support me.
Knowing that their peers were experiencing similar stressors helped to normalise common difficulties. The awareness that personal contacts were also struggling sometimes curtailed seeking informal support to avoid being a burden.
Actually discussing difficulties with friends has been most helpful, as it can sometimes feel like you’re the only one struggling, when actually most people are finding this year really difficult. Family and friends, but also don’t want to burden them as I know I can feel overwhelmed if people are always coming to me for negative conversations.
COVID-19 changed interactions with patients, with positive and negative effects
‘With patients there has been limited contact and I miss speaking to patients.’
Some students reported positive effects on relationships with patients, and feeling a sense of purpose in talking to patients when their families were not allowed to visit. Medical students felt a moral responsibility to protect patients and other vulnerable people from infection, which contributed to a reduction in socialising even when not constrained by lockdown.
Talking to patients who can’t get visitors has actually made me feel more useful. Anxiety over giving COVID-19 to patients or elderly relatives.
Students occasionally reported that wearing PPE made interactions with patients more challenging. Students’ contact with patients changed on some placements due to COVID-19, for example replacing in-person appointments with telephone consultations, and they found this challenging and disappointing.
Masks are an impediment to meaningful connections with new people. GP block when I saw no patients due to it all being on the telephone.
Formal support was valued but seeking it was perceived as more difficult during COVID-19
‘Feel a burden on academic and clinical staff/in the way/annoying so tend to just keep to myself.’
Many participants emphasised the primary importance of support from family and friends, and their responses indicated that most had not sought formal support. While staff remained available and created opportunities for students to seek support, factors such as online learning and increased clinical workloads meant that some students found it harder to build supportive relationships with academic and placement staff and felt disconnected from them, which was detrimental for wellbeing and engagement.
Staff have been really helpful on placement but it was clear that in some cases, staff were overwhelmed with the workload created by COVID. Even though academic staff are available having to arrange meetings over zoom rather than face to face to discuss any problem is off putting.
A few students described difficulty knowing what support was available, and identifying when they needed it.
It’s difficult to access support when you’re not sure what is available. Also you may feel your problems aren’t as serious as other people’s so hold off on seeking support.
Formal support provided within the University included meetings with Academic Advisors, the School of Medicine wellbeing team, and University counselling service and mental health advisory team. It was also available from NHS services, such as GPs and psychological therapies. Those who had accessed formal support mostly described positive experiences with services. However, barriers to seeking formal support, such as perceived stigma, practicalities, waiting times for certain services, and concern that it may impact their future career were reported by some participants.
It is good that some services offer appointments that are after 5pm- this makes it more accessible to healthcare students. Had good experience with GPs about mental health personally. Admitting you need help or asking for help would make you look weak. Reassurance should be provided to medical students that accessing the wellbeing team is not detrimental to their degree. If anything it should be marketed as a professional and responsible thing to do.
Some students preferred the convenience of remote access, others found phone or video impersonal and preferred in-person contact.
Students expressed that it was helpful when wellbeing support was integrated with academic systems, for example Academic Advisors or placement supervisors.
My CCT [primary-care led small group teaching] makes sure to ask how we are getting on and how our placements are going, so I think small groups of people with more contact with someone are more useful then large groups over zoom. Someone to speak to on palliative care placement, individual time with supervisor to check how we are doing (wellbeing, mental health) - would be a nice quick checkup.
Participants typically felt able to share openly in an anonymous forum. Reading peers’ comments helped them to see that other students were having similar experiences and challenged unhealthy comparisons.
I definitely shared more than I would have done on a zoom call. I loved this session as it makes you feel like you’re not alone. Reassuring to know that there are others going through similar things as you.
Our findings demonstrate that the COVID-19 pandemic exacerbated the stressors medical students experience, and removed some rewarding elements of learning, while reducing access to pre-existing coping strategies. The results support many aspects of the ‘coping reservoir’ framework [ 14 ]. Findings corroborate the restorative effects of psychosocial support and social/healthy activities such as sleep and physical activity, and the depletion of wellbeing due to time and energy demands, stress, and disruptions relating to the pandemic such as online teaching and limited social interaction. Feeling a sense of purpose, from continuing studying or interactions with patients for example, was restorative for wellbeing. Mentorship and intellectual stimulation were present in the responses, but received less attention than psychosocial support and social/healthy activities. Internal conflict is primarily characterised by Dunn et al. [ 14 ] as ambivalence about pursuing a career in medicine, which was not expressed by participants during the study. However, participants identified that their wellbeing was reduced by feeling unproductive and lacking purpose, feeling guilty about taking time for self-care, competing priorities, and comparison with peers, all of which could be described as forms of internal conflict. Different restorative and draining factors appeared to not be equally weighted by the participants responding to the prompts: some appear to be valued more highly, or rely on other needs being met. Possible explanations are that students may be less likely to find intellectual stimulation and mentorship beneficial if they are experiencing reduced social support or having difficulty sleeping, and internal conflict about pursuing a career in medicine might be overshadowed by more immediate concerns, for example about the pandemic. This prioritisation resembles the relationship between physiological and psychological needs being met and academic success [ 23 ], based on Maslow’s hierarchy of needs [ 24 ]. A revised ‘coping reservoir’ model is shown in Fig. 2 .
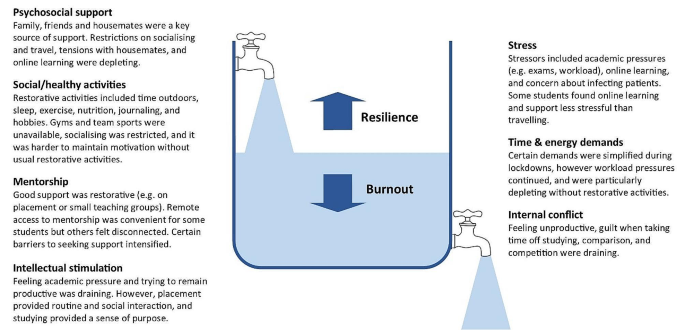
Coping reservoir model - the effects of COVID-19 on restorative and depleting factors for medical students, adapted from Dunn et al. [ 14 ], with permission from the authors and Springer Nature
Relational connections with family, friends, patients, and staff were protective factors for mental wellbeing. Feeling emotionally supported by family and friends is considered especially important for medical students to maintain good mental wellbeing [ 11 ]. These relationships usually mitigate the challenges of medical education [ 25 ], however they were fundamentally affected by the pandemic. Restrictions affecting support from family and friends, and changes to contact with patients on placement, had a negative effect on many participants’ mental wellbeing. Wellbeing support changed during the pandemic, with in-person support temporarily replaced by online consultations due to Government guidelines. Barriers to seeking formal support, such as perceived stigma, practicalities, and concern that it may impact their future career were reported by participants, reflecting previous research [ 26 ]. Despite initiatives to increase and publicise formal support, some students perceived that this was less available and accessible during COVID-19, due to online learning and awareness of the increased workload of clinicians, as described by Rich et al. [ 27 ]. These findings provide further support for the job demand-resources theory [ 28 , 29 ] where key relationships and support provide a protective buffer against the negative effects of challenging work.
In line with previous research, many participants reported feeling under chronic academic pressure while studying medicine [ 3 ]. Our findings indicate that medical students often continued to focus on achievement, productivity and competitiveness, despite the additional pressures of the pandemic. Remaining productive in their studies might have protected some students’ mental wellbeing by providing structure and purpose, however students’ responses primarily reflected the adverse effect this mindset had upon their wellbeing. Some students felt guilty taking time away from studying to relax, which contributes to burnout [ 30 ] , and explicitly prioritised academic achievement over their mental wellbeing.
Students were aware of the factors that have a positive impact on their mental wellbeing, such as physical activity, time with loved ones, spiritual care, nourishment and hobbies [ 31 ]. However, COVID-19 restrictions affected many replenishing factors, such as socialising, team sports, and gyms, and intensified draining factors, such as academic stressors. Students found ways to adapt to the removal of most coping strategies, for example doing home workouts instead of going to the gym, showing how they developed coping strategies that enhanced their resilience [ 15 ]. However, they found it more difficult to mitigate the effect of restrictions on relational connections with peers, patients and staff, and this appears to have had a particularly negative impact on mental wellbeing. While clinical placements provided helpful routine, social interaction and a sense of purpose, some students reported that having few social interactions outside placement became monotonous.
Our findings show that medical students often felt disconnected from peers and academic staff, and reported loneliness, isolation and decreased wellbeing during COVID-19. This corresponds with evidence that many medical students felt isolated [ 32 ], and students in general were at higher risk of loneliness than the general population during COVID-19 lockdowns [ 33 ]. Just as ‘belongingness’ mediates subjective wellbeing among University students [ 34 ], feeling connected and supported acts as a protective buffer for medical students’ psychological wellbeing [ 25 ].
Translation into practice
Based on the themes identified in this study, specific interventions can be recommended to support medical students’ mental wellbeing, summarised in Table 3 . This study provides evidence to support the development of interventions that increase relational connections between medical students, as a method of promoting mental wellbeing and preventing burnout. Our findings highlight the importance of interpersonal relationships and informal support mechanisms, and indicate that medical student wellbeing could be improved by strengthening these. Possible ways to do this include encouraging collaboration over competition, providing sufficient time off to visit family, having a peer mentor network, events that encourage students to meet each other, and wellbeing sessions that combine socialising with learning relaxation and mindfulness techniques. Students could be supported in their interactions with patients and peers by embedding reflective practice such as placement debrief sessions, Schwartz rounds [ 35 ] or Balint groups [ 36 ], and simulated communication workshops for difficult situations.
Experiencing guilt [ 30 ] and competition [ 4 ] while studying medicine are consistently recognised as contributing to distress and burnout, so interventions targeting these could improve mental wellbeing. Based on the responses from students, curriculum-based measures to protect mental wellbeing include manageable workloads, supportive learning environments, cultivating students’ sense of purpose, and encouraging taking breaks from studying without guilt. Normalising sharing of difficulties and regularly including content within the curriculum on self-care and stress reduction would improve mental wellbeing.
In aiming to reduce psychological distress among medical students, it is important that promotion of individual self-care is accompanied by reducing institutional stressors [ 11 , 29 ]. While the exploration of individual factors is important, such as promoting healthy lifestyle habits, reflection, time management, and mindset changes, this should not detract from addressing factors within the culture, learning and work environment that diminish mental wellbeing [ 37 ]. Heath et al. [ 38 ] propose a pro-active, multi-faceted approach, incorporating preventative strategies, organisational justice, individual strategies and organisational strategies to support resilience in healthcare workers. Similarly, trauma-informed medical education practices [ 13 ] involve individual and institutional strategies to promote student wellbeing.
Students favoured formal support that was responsive, individualised, and accessible. For example, integrating conversations about wellbeing into routine academic systems, and accommodating in-person and remote access to support. There has been increased awareness of the wellbeing needs of medical students in recent years, especially since the start of the pandemic, which has led to improvements in many of these areas, as reported in reviews by Ardekani et al. [ 12 ] and Klein and McCarthy [ 39 ]. Continuing to address stigma around mental health difficulties and embedding discussions around wellbeing in the curriculum are crucial for medical students to be able to seek appropriate support.
Strengths & limitations
By using qualitative open-text responses, rather than enforcing preconceived categories, this study captured students’ lived experience and priorities [ 4 , 31 ]. This increased the salience and depth of responses and generated categories of responses beyond the existing evidence, which is particularly important given the unprecedented experiences of COVID-19. Several strategies were used to establish rigour and trustworthiness, based on the four criteria proposed by Lincoln and Guba [ 20 ] (Table 2 ). These included the active involvement of medical students and recent medical graduates in data analysis and the development of themes, increasing the credibility of the research findings.
Potential limitations of the study are that participants may have been primed to think about certain aspects of wellbeing due to data being collected during a webinar delivered by medical educators including the lead author at the start of their palliative medicine placement, and the choice of prompts. Data was collected during the COVID-19 pandemic, and therefore represents fourth year medical students’ views in specific and unusual circumstances. Information on this context is provided to enable the reader to evaluate whether the findings have transferability to their setting. Responses were visible to others in the group, so participants may have influenced each other to give socially acceptable responses. This process of forming subjective meanings through social interactions is recognised as part of the construction of a shared understanding of reality, and we therefore view it as an inherent feature of this methodology rather than a hindrance. Feedback on the webinar indicated that students benefitted from this process of collective meaning-making. Similarly, researcher subjectivity is viewed as a contextual resource for knowledge generation in reflexive thematic analysis, rather than a limitation to be managed [ 19 ]. The study design meant that different demographic groups could not be compared.
Padlet provided a novel and acceptable method of data collection, offering researchers and educators the potential benefits of an anonymous forum in which students can see their peers’ responses. The use of an interactive webinar demonstrated a potential application of connectivist pedagogical principles [ 18 ]. Researchers are increasingly using content from online forums for qualitative research [ 40 ], and Padlet has been extensively used as an educational tool. However, to the authors’ knowledge, Padlet has not previously been used as a data collection platform for qualitative research. Allowing anonymity carried the risk of students posting comments that were inappropriate or unprofessional. However, with appropriate guidance it appeared to engender honesty and reflection, provided a safe and collaborative learning environment, and student feedback was overwhelmingly positive. It would be useful to evaluate the effects of this reflective webinar on medical students’ mental wellbeing, given that it acted as an intervention in addition to a teaching session and research study.
Students were prompted to plan what they would do following the webinar to improve their mental wellbeing. A longitudinal study to determine how students enacted these plans would allow a more detailed investigation of students’ self-care behaviour.
While we hope that the stressors of COVID-19 will not be repeated, this study provides valuable insight into medical students’ mental wellbeing, which can inform support beyond this exceptional time. The lasting impact of the pandemic upon medical education and mental wellbeing remains to be seen. Nevertheless, our findings reinforce and extend the coping reservoir model proposed by Dunn et al. [ 14 ], adding to our understanding of the factors that contribute to resilience or burnout. In particular, it provides evidence for the development of interventions that increase experiences of relational connectedness and belonging, which are likely to act as a buffer against emotional distress among medical students.
Data availability
The datasets generated and analysed during the study are available from the corresponding author on reasonable request.
Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students. JAMA. 2016;316(21):2214.
Article PubMed PubMed Central Google Scholar
Awad F, Awad M, Mattick K, Dieppe P. Mental health in medical students: time to act. Clin Teach. 2019;16(4):312–6.
Article PubMed Google Scholar
Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80(12):1613–22.
Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Med Educ Online. 2018;23(1):1530558.
Papapanou M, Routsi E, Tsamakis K, Fotis L, Marinos G, Lidoriki I, et al. Medical education challenges and innovations during COVID-19 pandemic. Postgrad Med J. 2021;0:1–7.
Google Scholar
De Andres Crespo M, Claireaux H, Handa AI. Medical students and COVID-19: lessons learnt from the 2020 pandemic. Postgrad Med J. 2021;97(1146):209–10.
Paz DC, Bains MS, Zueger ML, Bandi VR, Kuo VY, Cook K et al. COVID-19 and mental health: a systematic review of international medical student surveys. Front Psychol. 2022;(November):1–13.
Jia Q, Qu Y, Sun H, Huo H, Yin H, You D. Mental health among medical students during COVID-19: a systematic review and meta-analysis. Front Psychol. 2022;13:846789.
General Medical Council. Outcomes for Graduates. London; 2020 https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates [accessed 13 Feb 2024].
Shiralkar MT, Harris TB, Eddins-Folensbee FF, Coverdale JH. A systematic review of stress-management programs for medical students. Acad Psychiatry. 2013;37(3):158–64.
McLuckie A, Matheson KM, Landers AL, Landine J, Novick J, Barrett T, et al. The relationship between psychological distress and perception of emotional support in medical students and residents and implications for educational institutions. Acad Psychiatry. 2018;42(1):41–7.
Ardekani A, Hosseini SA, Tabari P, Rahimian Z, Feili A, Amini M. Student support systems for undergraduate medical students during the COVID-19 pandemic: a systematic narrative review of the literature. BMC Med Educ. 2021;21:352.
Brown T, Berman S, McDaniel K, Radford C, Mehta P, Potter J, et al. Trauma-informed medical education (TIME): advancing curricular content and educational context. Acad Med. 2021;96(5):661–7.
Dunn LB, Iglewicz A, Moutier C. Promoting resilience and preventing burnout. Acad Psychiatry. 2008;32(1):44–53.
Kelly EL, Casola AR, Smith K, Kelly S, Syl M, Cruz D, De. A qualitative analysis of third-year medical students ’ reflection essays regarding the impact of COVID-19 on their education. BMC Med Educ. 2021;21(481).
Pilgrim D. Some implications of critical realism for mental health research. Soc Theory Heal. 2014;12:1–21.
Article Google Scholar
Henriksson C, Friesen N. Introduction. In: Friesen N, Henriksson C, Saevi T, editors. Hermeneutic phenomenology in education. Sense; 2012. pp. 1–17.
Goldie JGS, Connectivism. A knowledge learning theory for the digital age? Med Teach. 2016;38(10):1064–9.
Braun V, Clarke V. Thematic analysis: a practical guide. SAGE Publications Ltd; 2021.
Lincoln YS, Guba EG. Naturalistic inquiry. Beverly Hills, California: SAGE; 1985.
Book Google Scholar
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving tomeet thetrustworthiness criteria. 2017;16:1–13.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for Reporting Qualitative Research: Acad Med. 2014;89(9):1245–51.
PubMed Google Scholar
Freitas FA, Leonard LJ. Maslow’s hierarchy of needs and student academic success. Teach Learn Nurs. 2011;6(1):9–13.
Maslow AH. Motivation and personality. 3rd ed. New York: Longman; 1954.
MacArthur KR, Sikorski J. A qualitative analysis of the coping reservoir model of pre-clinical medical student well-being: human connection as making it worth it. BMC Med Educ. 2020;20(1):1–11.
Simpson V, Halpin L, Chalmers K, Joynes V. Exploring well-being: medical students and staff. Clin Teach. 2019;16(4):356–61.
Rich A, Viney R, Silkens M, Griffin A, Medisauskaite A. UK medical students ’ mental health during the COVID-19 pandemic: a qualitative interview study. BMJ Open. 2023;13:e070528.
Bakker AAB, Demerouti E. Job demands-resources theory: taking stock and looking forward. J Occup Health Psychol. 2017;22(3):273–85.
Riley R, Kokab F, Buszewicz M, Gopfert A, Van Hove M, Taylor AK et al. Protective factors and sources of support in the workplace as experienced by UK foundation and junior doctors: a qualitative study. BMJ Open. 2021;11(6).
Greenmyer JR, Montgomery M, Hosford C, Burd M, Miller V, Storandt MH, et al. Guilt and burnout in medical students. Teach Learn Med. 2021;34(1):69–77.
Ayala EE, Omorodion AM, Nmecha D, Winseman JS, Mason HRC. What do medical students do for self-care? A student-centered approach to well-being. Teach Learn Med. 2017;29(3):237–46.
Wurth S, Sader J, Cerutti B, Broers B, Bajwa MN, Carballo S, et al. Medical students’ perceptions and coping strategies during the first wave of the COVID-19 pandemic: studies, clinical implication, and professional identity. BMC Med Educ. 2021;21(1):620.
Bu F, Steptoe A, Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31–4.
Arslan G, Loneliness C, Belongingness. Subjective vitality, and psychological adjustment during coronavirus pandemic: development of the college belongingness questionnaire. J Posit Sch Psychol. 2021;5(1):17–31.
Maben J, Taylor C, Dawson J, Leamy M, McCarthy I, Reynolds E et al. A realist informed mixed-methods evaluation of Schwartz center rounds in England. Heal Serv Deliv Res. 2018;6(37).
Monk A, Hind D, Crimlisk H. Balint groups in undergraduate medical education: a systematic review. Psychoanal Psychother. 2018;8734:1–26.
Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50(1):132–49.
Heath C, Sommerfield A, Von Ungern-Sternberg BS. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: a narrative review. Anaesthesia. 2020;75(10):1364–71.
Klein HJ, McCarthy SM. Student wellness trends and interventions in medical education: a narrative review. Humanit Soc Sci Commun. 2022;9(92).
Smedley RM, Coulson NS. A practical guide to analysing online support forums. Qual Res Psychol. 2021;18(1):76–103.
Download references
Acknowledgements
We would like to thank Dr P Byrne for providing guidance, Mrs A Threlfall and Professor VCT Goddard-Fuller for commenting on drafts, and the medical students who participated in the webinars.
This study was unfunded.
Author information
Authors and affiliations.
Department of Psychology, University of Liverpool, Eleanor Rathbone Building, Bedford Street South, Liverpool, L69 7ZA, UK
Helen M West
Liverpool University Hospitals NHS Foundation Trust, Liverpool, UK
School of Medicine, University of Liverpool, Liverpool, UK
Rowan M Davies, Benjamin Shelley & Oscar T Edginton
Salford Royal NHS Foundation Trust, Manchester, UK
Rowan M Davies
Calderdale and Huddersfield NHS Foundation Trust, West Yorkshire, UK
Benjamin Shelley
Leeds Teaching Hospitals NHS Foundation Trust, Leeds, UK
Oscar T Edginton
You can also search for this author in PubMed Google Scholar
Contributions
HMW conceptualised the study and collected the data. HMW, LF, RMD, BS and OTE conducted data analysis. HMW, LF, RMD and OTE wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Correspondence to Helen M West .
Ethics declarations
Ethical approval and consent to participate.
Approval was granted by the University of Liverpool Institute of Population Health Research Ethics Committee (Reference: 8365). Students were fully informed about the study prior to the workshop and had an opportunity to ask questions. Participants provided informed consent, completing an electronic consent form before responding to prompts. The study was conducted in accordance with relevant guidelines and regulations, including the University of Liverpool Research Ethics and Research Data Management Policies, and the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
West, H.M., Flain, L., Davies, R.M. et al. Medical student wellbeing during COVID-19: a qualitative study of challenges, coping strategies, and sources of support. BMC Psychol 12 , 179 (2024). https://doi.org/10.1186/s40359-024-01618-8
Download citation
Received : 12 December 2023
Accepted : 22 February 2024
Published : 28 March 2024
DOI : https://doi.org/10.1186/s40359-024-01618-8

Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Mental wellbeing
- Medical student
- Student doctor
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
- Open access
- Published: 12 December 2023
Examining the role of community resilience and social capital on mental health in public health emergency and disaster response: a scoping review
- C. E. Hall 1 , 2 ,
- H. Wehling 1 ,
- J. Stansfield 3 ,
- J. South 3 ,
- S. K. Brooks 2 ,
- N. Greenberg 2 , 4 ,
- R. Amlôt 1 &
- D. Weston 1
BMC Public Health volume 23 , Article number: 2482 ( 2023 ) Cite this article
1752 Accesses
21 Altmetric
Metrics details
The ability of the public to remain psychologically resilient in the face of public health emergencies and disasters (such as the COVID-19 pandemic) is a key factor in the effectiveness of a national response to such events. Community resilience and social capital are often perceived as beneficial and ensuring that a community is socially and psychologically resilient may aid emergency response and recovery. This review presents a synthesis of literature which answers the following research questions: How are community resilience and social capital quantified in research?; What is the impact of community resilience on mental wellbeing?; What is the impact of infectious disease outbreaks, disasters and emergencies on community resilience and social capital?; and, What types of interventions enhance community resilience and social capital?
A scoping review procedure was followed. Searches were run across Medline, PsycInfo, and EMBASE, with search terms covering both community resilience and social capital, public health emergencies, and mental health. 26 papers met the inclusion criteria.
The majority of retained papers originated in the USA, used a survey methodology to collect data, and involved a natural disaster. There was no common method for measuring community resilience or social capital. The association between community resilience and social capital with mental health was regarded as positive in most cases. However, we found that community resilience, and social capital, were initially negatively impacted by public health emergencies and enhanced by social group activities.
Several key recommendations are proposed based on the outcomes from the review, which include: the need for a standardised and validated approach to measuring both community resilience and social capital; that there should be enhanced effort to improve preparedness to public health emergencies in communities by gauging current levels of community resilience and social capital; that community resilience and social capital should be bolstered if areas are at risk of disasters or public health emergencies; the need to ensure that suitable short-term support is provided to communities with high resilience in the immediate aftermath of a public health emergency or disaster; the importance of conducting robust evaluation of community resilience initiatives deployed during the COVID-19 pandemic.
Peer Review reports
For the general population, public health emergencies and disasters (e.g., natural disasters; infectious disease outbreaks; Chemical, Biological, Radiological or Nuclear incidents) can give rise to a plethora of negative outcomes relating to both health (e.g. increased mental health problems [ 1 , 2 , 3 , 4 ]) and the economy (e.g., increased unemployment and decreased levels of tourism [ 4 , 5 , 6 ]). COVID-19 is a current, and ongoing, example of a public health emergency which has affected over 421 million individuals worldwide [ 7 ]. The long term implications of COVID-19 are not yet known, but there are likely to be repercussions for physical health, mental health, and other non-health related outcomes for a substantial time to come [ 8 , 9 ]. As a result, it is critical to establish methods which may inform approaches to alleviate the longer-term negative consequences that are likely to emerge in the aftermath of both COVID-19 and any future public health emergency.
The definition of resilience often differs within the literature, but ultimately resilience is considered a dynamic process of adaptation. It is related to processes and capabilities at the individual, community and system level that result in good health and social outcomes, in spite of negative events, serious threats and hazards [ 10 ]. Furthermore, Ziglio [ 10 ] refers to four key types of resilience capacity: adaptive, the ability to withstand and adjust to unfavourable conditions and shocks; absorptive, the ability to withstand but also to recover and manage using available assets and skills; anticipatory, the ability to predict and minimize vulnerability; and transformative, transformative change so that systems better cope with new conditions.
There is no one settled definition of community resilience (CR). However, it generally relates to the ability of a community to withstand, adapt and permit growth in adverse circumstances due to social structures, networks and interdependencies within the community [ 11 ]. Social capital (SC) is considered a major determinant of CR [ 12 , 13 ], and reflects strength of a social network, community reciprocity, and trust in people and institutions [ 14 ]. These aspects of community are usually conceptualised primarily as protective factors that enable communities to cope and adapt collectively to threats. SC is often broken down into further categories [ 15 ], for example: cognitive SC (i.e. perceptions of community relations, such as trust, mutual help and attachment) and structural SC (i.e. what actually happens within the community, such as participation, socialising) [ 16 ]; or, bonding SC (i.e. connections among individuals who are emotionally close, and result in bonds to a particular group [ 17 ]) and bridging SC (i.e. acquaintances or individuals loosely connected that span different social groups [ 18 ]). Generally, CR is perceived to be primarily beneficial for multiple reasons (e.g. increased social support [ 18 , 19 ], protection of mental health [ 20 , 21 ]), and strengthening community resilience is a stated health goal of the World Health Organisation [ 22 ] when aiming to alleviate health inequalities and protect wellbeing. This is also reflected by organisations such as Public Health England (now split into the UK Health Security Agency and the Office for Health Improvement and Disparities) [ 23 ] and more recently, CR has been targeted through the endorsement of Community Champions (who are volunteers trained to support and to help improve health and wellbeing. Community Champions also reflect their local communities in terms of population demographics for example age, ethnicity and gender) as part of the COVID-19 response in the UK (e.g. [ 24 , 25 ]).
Despite the vested interest in bolstering communities, the research base establishing: how to understand and measure CR and SC; the effect of CR and SC, both during and following a public health emergency (such as the COVID-19 pandemic); and which types of CR or SC are the most effective to engage, is relatively small. Given the importance of ensuring resilience against, and swift recovery from, public health emergencies, it is critically important to establish and understand the evidence base for these approaches. As a result, the current review sought to answer the following research questions: (1) How are CR and SC quantified in research?; (2) What is the impact of community resilience on mental wellbeing?; (3) What is the impact of infectious disease outbreaks, disasters and emergencies on community resilience and social capital?; and, (4) What types of interventions enhance community resilience and social capital?
By collating research in order to answer these research questions, the authors have been able to propose several key recommendations that could be used to both enhance and evaluate CR and SC effectively to facilitate the long-term recovery from COVID-19, and also to inform the use of CR and SC in any future public health disasters and emergencies.
A scoping review methodology was followed due to the ease of summarising literature on a given topic for policy makers and practitioners [ 26 ], and is detailed in the following sections.
Identification of relevant studies
An initial search strategy was developed by authors CH and DW and included terms which related to: CR and SC, given the absence of a consistent definition of CR, and the link between CR and SC, the review focuses on both CR and SC to identify as much relevant literature as possible (adapted for purpose from Annex 1: [ 27 ], as well as through consultation with review commissioners); public health emergencies and disasters [ 28 , 29 , 30 , 31 ], and psychological wellbeing and recovery (derived a priori from literature). To ensure a focus on both public health and psychological research, the final search was carried across Medline, PsycInfo, and EMBASE using OVID. The final search took place on the 18th of May 2020, the search strategy used for all three databases can be found in Supplementary file 1 .
Selection criteria
The inclusion and exclusion criteria were developed alongside the search strategy. Initially the criteria were relatively inclusive and were subject to iterative development to reflect the authors’ familiarisation with the literature. For example, the decision was taken to exclude research which focused exclusively on social support and did not mention communities as an initial title/abstract search suggested that the majority of this literature did not meet the requirements of our research question.
The full and final inclusion and exclusion criteria used can be found in Supplementary file 2 . In summary, authors decided to focus on the general population (i.e., non-specialist, e.g. non-healthcare worker or government official) to allow the review to remain community focused. The research must also have assessed the impact of CR and/or SC on mental health and wellbeing, resilience, and recovery during and following public health emergencies and infectious disease outbreaks which affect communities (to ensure the research is relevant to the review aims), have conducted primary research, and have a full text available or provided by the first author when contacted.
Charting the data
All papers were first title and abstract screened by CH or DW. Papers then were full text reviewed by CH to ensure each paper met the required eligibility criteria, if unsure about a paper it was also full text reviewed by DW. All papers that were retained post full-text review were subjected to a standardised data extraction procedure. A table was made for the purpose of extracting the following data: title, authors, origin, year of publication, study design, aim, disaster type, sample size and characteristics, variables examined, results, restrictions/limitations, and recommendations. Supplementary file 3 details the charting the data process.
Analytical method
Data was synthesised using a Framework approach [ 32 ], a common method for analysing qualitative research. This method was chosen as it was originally used for large-scale social policy research [ 33 ] as it seeks to identify: what works, for whom, in what conditions, and why [ 34 ]. This approach is also useful for identifying commonalities and differences in qualitative data and potential relationships between different parts of the data [ 33 ]. An a priori framework was established by CH and DW. Extracted data was synthesised in relation to each research question, and the process was iterative to ensure maximum saturation using the available data.
Study selection
The final search strategy yielded 3584 records. Following the removal of duplicates, 2191 records remained and were included in title and abstract screening. A PRISMA flow diagram is presented in Fig. 1 .
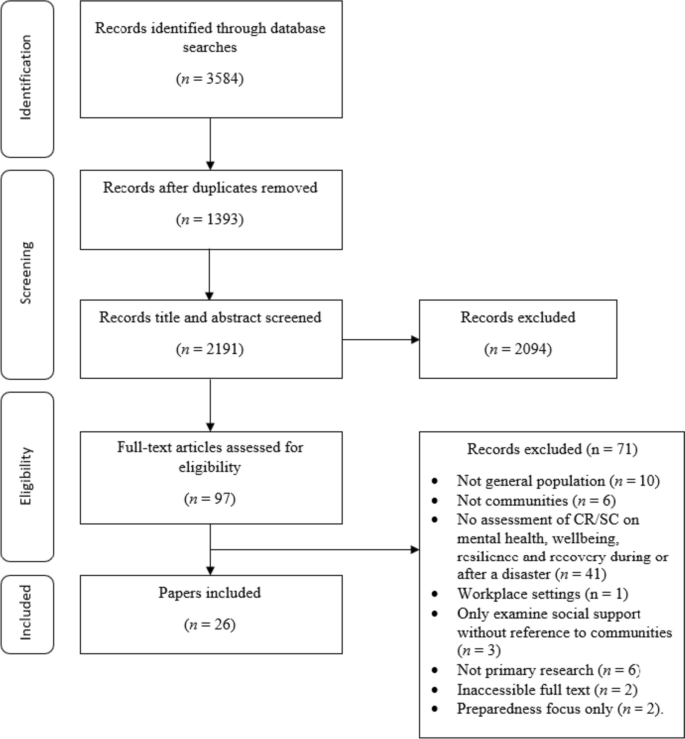
PRISMA flow diagram
At the title and abstract screening stage, the process became more iterative as the inclusion criteria were developed and refined. For the first iteration of screening, CH or DW sorted all records into ‘include,’ ‘exclude,’ and ‘unsure’. All ‘unsure’ papers were re-assessed by CH, and a random selection of ~ 20% of these were also assessed by DW. Where there was disagreement between authors the records were retained, and full text screened. The remaining papers were reviewed by CH, and all records were categorised into ‘include’ and ‘exclude’. Following full-text screening, 26 papers were retained for use in the review.
Study characteristics
This section of the review addresses study characteristics of those which met the inclusion criteria, which comprises: date of publication, country of origin, study design, study location, disaster, and variables examined.
Date of publication
Publication dates across the 26 papers spanned from 2008 to 2020 (see Fig. 2 ). The number of papers published was relatively low and consistent across this timescale (i.e. 1–2 per year, except 2010 and 2013 when none were published) up until 2017 where the number of papers peaked at 5. From 2017 to 2020 there were 15 papers published in total. The amount of papers published in recent years suggests a shift in research and interest towards CR and SC in a disaster/ public health emergency context.
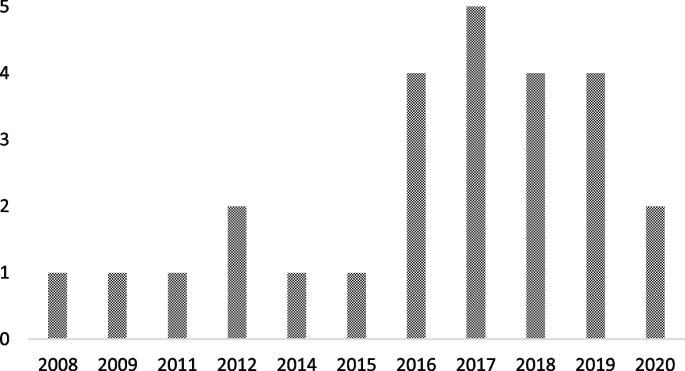
Graph to show retained papers date of publication
Country of origin
The locations of the first authors’ institutes at the time of publication were extracted to provide a geographical spread of the retained papers. The majority originated from the USA [ 35 , 36 , 37 , 38 , 39 , 40 , 41 ], followed by China [ 42 , 43 , 44 , 45 , 46 ], Japan [ 47 , 48 , 49 , 50 ], Australia [ 51 , 52 , 53 ], The Netherlands [ 54 , 55 ], New Zealand [ 56 ], Peru [ 57 ], Iran [ 58 ], Austria [ 59 ], and Croatia [ 60 ].
There were multiple methodological approaches carried out across retained papers. The most common formats included surveys or questionnaires [ 36 , 37 , 38 , 42 , 46 , 47 , 48 , 49 , 50 , 53 , 54 , 55 , 57 , 59 ], followed by interviews [ 39 , 40 , 43 , 51 , 52 , 60 ]. Four papers used both surveys and interviews [ 35 , 41 , 45 , 58 ], and two papers conducted data analysis (one using open access data from a Social Survey [ 44 ] and one using a Primary Health Organisations Register [ 56 ]).
Study location
The majority of the studies were carried out in Japan [ 36 , 42 , 44 , 47 , 48 , 49 , 50 ], followed by the USA [ 35 , 37 , 38 , 39 , 40 , 41 ], China [ 43 , 45 , 46 , 53 ], Australia [ 51 , 52 ], and the UK [ 54 , 55 ]. The remaining studies were carried out in Croatia [ 60 ], Peru [ 57 ], Austria [ 59 ], New Zealand [ 56 ] and Iran [ 58 ].
Multiple different types of disaster were researched across the retained papers. Earthquakes were the most common type of disaster examined [ 45 , 47 , 49 , 50 , 53 , 56 , 57 , 58 ], followed by research which assessed the impact of two disastrous events which had happened in the same area (e.g. Hurricane Katrina and the Deepwater Horizon oil spill in Mississippi, and the Great East Japan earthquake and Tsunami; [ 36 , 37 , 38 , 42 , 44 , 48 ]). Other disaster types included: flooding [ 51 , 54 , 55 , 59 , 60 ], hurricanes [ 35 , 39 , 41 ], infectious disease outbreaks [ 43 , 46 ], oil spillage [ 40 ], and drought [ 52 ].
Variables of interest examined
Across the 26 retained papers: eight referred to examining the impact of SC [ 35 , 37 , 39 , 41 , 46 , 49 , 55 , 60 ]; eight examined the impact of cognitive and structural SC as separate entities [ 40 , 42 , 45 , 48 , 50 , 54 , 57 , 59 ]; one examined bridging and bonding SC as separate entities [ 58 ]; two examined the impact of CR [ 38 , 56 ]; and two employed a qualitative methodology but drew findings in relation to bonding and bridging SC, and SC generally [ 51 , 52 ]. Additionally, five papers examined the impact of the following variables: ‘community social cohesion’ [ 36 ], ‘neighbourhood connectedness’ [ 44 ], ‘social support at the community level’ [ 47 ], ‘community connectedness’ [ 43 ] and ‘sense of community’ [ 53 ]. Table 1 provides additional details on this.
How is CR and SC measured or quantified in research?
The measures used to examine CR and SC are presented Table 1 . It is apparent that there is no uniformity in how SC or CR is measured across the research. Multiple measures are used throughout the retained studies, and nearly all are unique. Additionally, SC was examined at multiple different levels (e.g. cognitive and structural, bonding and bridging), and in multiple different forms (e.g. community connectedness, community cohesion).
What is the association between CR and SC on mental wellbeing?
To best compare research, the following section reports on CR, and facets of SC separately. Please see Supplementary file 4 for additional information on retained papers methods of measuring mental wellbeing.
- Community resilience
CR relates to the ability of a community to withstand, adapt and permit growth in adverse circumstances due to social structures, networks and interdependencies within the community [ 11 ].
The impact of CR on mental wellbeing was consistently positive. For example, research indicated that there was a positive association between CR and number of common mental health (i.e. anxiety and mood) treatments post-disaster [ 56 ]. Similarly, other research suggests that CR is positively related to psychological resilience, which is inversely related to depressive symptoms) [ 37 ]. The same research also concluded that CR is protective of psychological resilience and is therefore protective of depressive symptoms [ 37 ].
- Social capital
SC reflects the strength of a social network, community reciprocity, and trust in people and institutions [ 14 ]. These aspects of community are usually conceptualised primarily as protective factors that enable communities to cope and adapt collectively to threats.
There were inconsistencies across research which examined the impact of abstract SC (i.e. not refined into bonding/bridging or structural/cognitive) on mental wellbeing. However, for the majority of cases, research deems SC to be beneficial. For example, research has concluded that, SC is protective against post-traumatic stress disorder [ 55 ], anxiety [ 46 ], psychological distress [ 50 ], and stress [ 46 ]. Additionally, SC has been found to facilitate post-traumatic growth [ 38 ], and also to be useful to be drawn upon in times of stress [ 52 ], both of which could be protective of mental health. Similarly, research has also found that emotional recovery following a disaster is more difficult for those who report to have low levels of SC [ 51 ].
Conversely, however, research has also concluded that when other situational factors (e.g. personal resources) were controlled for, a positive relationship between community resources and life satisfaction was no longer significant [ 60 ]. Furthermore, some research has concluded that a high level of SC can result in a community facing greater stress immediately post disaster. Indeed, one retained paper found that high levels of SC correlate with higher levels of post-traumatic stress immediately following a disaster [ 39 ]. However, in the later stages following a disaster, this relationship can reverse, with SC subsequently providing an aid to recovery [ 41 ]. By way of explanation, some researchers have suggested that communities with stronger SC carry the greatest load in terms of helping others (i.e. family, friends and neighbours) as well as themselves immediately following the disaster, but then as time passes the communities recover at a faster rate as they are able to rely on their social networks for support [ 41 ].
Cognitive and structural social capital
Cognitive SC refers to perceptions of community relations, such as trust, mutual help and attachment, and structural SC refers to what actually happens within the community, such as participation, socialising [ 16 ].
Cognitive SC has been found to be protective [ 49 ] against PTSD [ 54 , 57 ], depression [ 40 , 54 ]) mild mood disorder; [ 48 ]), anxiety [ 48 , 54 ] and increase self-efficacy [ 59 ].
For structural SC, research is again inconsistent. On the one hand, structural SC has been found to: increase perceived self-efficacy, be protective of depression [ 40 ], buffer the impact of housing damage on cognitive decline [ 42 ] and provide support during disasters and over the recovery period [ 59 ]. However, on the other hand, it has been found to have no association with PTSD [ 54 , 57 ] or depression, and is also associated with a higher prevalence of anxiety [ 54 ]. Similarly, it is also suggested by additional research that structural SC can harm women’s mental health, either due to the pressure of expectations to help and support others or feelings of isolation [ 49 ].
Bonding and bridging social capital
Bonding SC refers to connections among individuals who are emotionally close, and result in bonds to a particular group [ 17 ], and bridging SC refers to acquaintances or individuals loosely connected that span different social groups [ 18 ].
One research study concluded that both bonding and bridging SC were protective against post-traumatic stress disorder symptoms [ 58 ]. Bridging capital was deemed to be around twice as effective in buffering against post-traumatic stress disorder than bonding SC [ 58 ].
Other community variables
Community social cohesion was significantly associated with a lower risk of post-traumatic stress disorder symptom development [ 35 ], and this was apparent even whilst controlling for depressive symptoms at baseline and disaster impact variables (e.g. loss of family member or housing damage) [ 36 ]. Similarly, sense of community, community connectedness, social support at the community level and neighbourhood connectedness all provided protective benefits for a range of mental health, wellbeing and recovery variables, including: depression [ 53 ], subjective wellbeing (in older adults only) [ 43 ], psychological distress [ 47 ], happiness [ 44 ] and life satisfaction [ 53 ].
Research has also concluded that community level social support is protective against mild mood and anxiety disorder, but only for individuals who have had no previous disaster experience [ 48 ]. Additionally, a study which separated SC into social cohesion and social participation concluded that at a community level, social cohesion is protective against depression [ 49 ] whereas social participation at community level is associated with an increased risk of depression amongst women [ 49 ].
What is the impact of Infectious disease outbreaks / disasters and emergencies on community resilience?
From a cross-sectional perspective, research has indicated that disasters and emergencies can have a negative effect on certain types of SC. Specifically, cognitive SC has been found to be impacted by disaster impact, whereas structural SC has gone unaffected [ 45 ]. Disaster impact has also been shown to have a negative effect on community relationships more generally [ 52 ].
Additionally, of the eight studies which collected data at multiple time points [ 35 , 36 , 41 , 42 , 47 , 49 , 56 , 60 ], three reported the effect of a disaster on the level of SC within a community [ 40 , 42 , 49 ]. All three of these studies concluded that disasters may have a negative impact on the levels of SC within a community. The first study found that the Deepwater Horizon oil spill had a negative effect on SC and social support, and this in turn explained an overall increase in the levels of depression within the community [ 40 ]. A possible explanation for the negative effect lays in ‘corrosive communities’, known for increased social conflict and reduced social support, that are sometimes created following oil spills [ 40 ]. It is proposed that corrosive communities often emerge due to a loss of natural resources that bring social groups together (e.g., for recreational activities), as well as social disparity (e.g., due to unequal distribution of economic impact) becoming apparent in the community following disaster [ 40 ]. The second study found that SC (in the form of social cohesion, informal socialising and social participation) decreased after the 2011 earthquake and tsunami in Japan; it was suggested that this change correlated with incidence of cognitive decline [ 42 ]. However, the third study reported more mixed effects based on physical circumstances of the communities’ natural environment: Following an earthquake, those who lived in mountainous areas with an initial high level of pre-community SC saw a decrease in SC post disaster [ 49 ]. However, communities in flat areas (which were home to younger residents and had a higher population density) saw an increase in SC [ 49 ]. It was proposed that this difference could be due to the need for those who lived in mountainous areas to seek prolonged refuge due to subsequent landslides [ 49 ].
What types of intervention enhance CR and SC and protect survivors?
There were mixed effects across the 26 retained papers when examining the effect of CR and SC on mental wellbeing. However, there is evidence that an increase in SC [ 56 , 57 ], with a focus on cognitive SC [ 57 ], namely by: building social networks [ 45 , 51 , 53 ], enhancing feelings of social cohesion [ 35 , 36 ] and promoting a sense of community [ 53 ], can result in an increase in CR and potentially protect survivors’ wellbeing and mental health following a disaster. An increase in SC may also aid in decreasing the need for individual psychological interventions in the aftermath of a disaster [ 55 ]. As a result, recommendations and suggested methods to bolster CR and SC from the retained papers have been extracted and separated into general methods, preparedness and policy level implementation.
General methods
Suggested methods to build SC included organising recreational activity-based groups [ 44 ] to broaden [ 51 , 53 ] and preserve current social networks [ 42 ], introducing initiatives to increase social cohesion and trust [ 51 ], and volunteering to increase the number of social ties between residents [ 59 ]. Research also notes that it is important to take a ‘no one left behind approach’ when organising recreational and social community events, as failure to do so could induce feelings of isolation for some members of the community [ 49 ]. Furthermore, gender differences should also be considered as research indicates that males and females may react differently to community level SC (as evidence suggests males are instead more impacted by individual level SC; in comparison to women who have larger and more diverse social networks [ 49 ]). Therefore, interventions which aim to raise community level social participation, with the aim of expanding social connections and gaining support, may be beneficial [ 42 , 47 ].
Preparedness
In order to prepare for disasters, it may be beneficial to introduce community-targeted methods or interventions to increase levels of SC and CR as these may aid in ameliorating the consequences of a public health emergency or disaster [ 57 ]. To indicate which communities have low levels of SC, one study suggests implementing a 3-item scale of social cohesion to map areas and target interventions [ 42 ].
It is important to consider that communities with a high level of SC may have a lower level of risk perception, due to the established connections and supportive network they have with those around them [ 61 ]. However, for the purpose of preparedness, this is not ideal as perception of risk is a key factor when seeking to encourage behavioural adherence. This could be overcome by introducing communication strategies which emphasise the necessity of social support, but also highlights the need for additional measures to reduce residual risk [ 59 ]. Furthermore, support in the form of financial assistance to foster current community initiatives may prove beneficial to rural areas, for example through the use of an asset-based community development framework [ 52 ].
Policy level
At a policy level, the included papers suggest a range of ways that CR and SC could be bolstered and used. These include: providing financial support for community initiatives and collective coping strategies, (e.g. using asset-based community development [ 52 ]); ensuring policies for long-term recovery focus on community sustainable development (e.g. community festival and community centre activities) [ 44 ]; and development of a network amongst cooperative corporations formed for reconstruction and to organise self-help recovery sessions among residents of adjacent areas [ 58 ].
This scoping review sought to synthesise literature concerning the role of SC and CR during public health emergencies and disasters. Specifically, in this review we have examined: the methods used to measure CR and SC; the impact of CR and SC on mental wellbeing during disasters and emergencies; the impact of disasters and emergencies on CR and SC; and the types of interventions which can be used to enhance CR. To do this, data was extracted from 26 peer-reviewed journal articles. From this synthesis, several key themes have been identified, which can be used to develop guidelines and recommendations for deploying CR and SC in a public health emergency or disaster context. These key themes and resulting recommendations are summarised below.
Firstly, this review established that there is no consistent or standardised approach to measuring CR or SC within the general population. This finding is consistent with a review conducted by the World Health Organization which concludes that despite there being a number of frameworks that contain indicators across different determinants of health, there is a lack of consensus on priority areas for measurement and no widely accepted indicator [ 27 ]. As a result, there are many measures of CR and SC apparent within the literature (e.g., [ 62 , 63 ]), an example of a developed and validated measure is provided by Sherrieb, Norris and Galea [ 64 ]. Similarly, the definitions of CR and SC differ widely between researchers, which created a barrier to comparing and summarising information. Therefore, future research could seek to compare various interpretations of CR and to identify any overlapping concepts. However, a previous systemic review conducted by Patel et al. (2017) concludes that there are nine core elements of CR (local knowledge, community networks and relationships, communication, health, governance and leadership, resources, economic investment, preparedness, and mental outlook), with 19 further sub-elements therein [ 30 ]. Therefore, as CR is a multi-dimensional construct, the implications from the findings are that multiple aspects of social infrastructure may need to be considered.
Secondly, our synthesis of research concerning the role of CR and SC for ensuring mental health and wellbeing during, or following, a public health emergency or disaster revealed mixed effects. Much of the research indicates either a generally protective effect on mental health and wellbeing, or no effect; however, the literature demonstrates some potential for a high level of CR/SC to backfire and result in a negative effect for populations during, or following, a public health emergency or disaster. Considered together, our synthesis indicates that cognitive SC is the only facet of SC which was perceived as universally protective across all retained papers. This is consistent with a systematic review which also concludes that: (a) community level cognitive SC is associated with a lower risk of common mental disorders, while; (b) community level structural SC had inconsistent effects [ 65 ].
Further examination of additional data extracted from studies which found that CR/SC had a negative effect on mental health and wellbeing revealed no commonalities that might explain these effects (Please see Supplementary file 5 for additional information)
One potential explanation may come from a retained paper which found that high levels of SC result in an increase in stress level immediately post disaster [ 41 ]. This was suggested to be due to individuals having greater burdens due to wishing to help and support their wide networks as well as themselves. However, as time passes the levels of SC allow the community to come together and recover at a faster rate [ 41 ]. As this was the only retained paper which produced this finding, it would be beneficial for future research to examine boundary conditions for the positive effects of CR/SC; that is, to explore circumstances under which CR/SC may be more likely to put communities at greater risk. This further research should also include additional longitudinal research to validate the conclusions drawn by [ 41 ] as resilience is a dynamic process of adaption.
Thirdly, disasters and emergencies were generally found to have a negative effect on levels of SC. One retained paper found a mixed effect of SC in relation to an earthquake, however this paper separated participants by area in which they lived (i.e., mountainous vs. flat), which explains this inconsistent effect [ 49 ]. Dangerous areas (i.e. mountainous) saw a decrease in community SC in comparison to safer areas following the earthquake (an effect the authors attributed to the need to seek prolonged refuge), whereas participants from the safer areas (which are home to younger residents with a higher population density) saw an increase in SC [ 49 ]. This is consistent with the idea that being able to participate socially is a key element of SC [ 12 ]. Overall, however, this was the only retained paper which produced a variable finding in relation to the effect of disaster on levels of CR/SC.
Finally, research identified through our synthesis promotes the idea of bolstering SC (particularly cognitive SC) and cohesion in communities likely to be affected by disaster to improve levels of CR. This finding provides further understanding of the relationship between CR and SC; an association that has been reported in various articles seeking to provide conceptual frameworks (e.g., [ 66 , 67 ]) as well as indicator/measurement frameworks [ 27 ]. Therefore, this could be done by creating and promoting initiatives which foster SC and create bonds within the community. Papers included in the current review suggest that recreational-based activity groups and volunteering are potential methods for fostering SC and creating community bonds [ 44 , 51 , 59 ]. Similarly, further research demonstrates that feelings of social cohesion are enhanced by general social activities (e.g. fairs and parades [ 18 ]). Also, actively encouraging activities, programs and interventions which enhance connectedness and SC have been reported to be desirable to increase CR [ 68 ]. This suggestion is supported by a recent scoping review of literature [ 67 ] examined community champion approaches for the COVID-19 pandemic response and recovery and established that creating and promoting SC focused initiatives within the community during pandemic response is highly beneficial [ 67 ]. In terms of preparedness, research states that it may be beneficial for levels of SC and CR in communities at risk to be assessed, to allow targeted interventions where the population may be at most risk following an incident [ 42 , 44 ]. Additionally, from a more critical perspective, we acknowledge that ‘resilience’ can often be perceived as a focus on individual capacity to adapt to adversity rather than changing or mitigating the causes of adverse conditions [ 69 , 70 ]. Therefore, CR requires an integrated system approach across individual, community and structural levels [ 17 ]. Also, it is important that community members are engaged in defining and agreeing how community resilience is measured [ 27 ] rather than it being imposed by system leads or decision-makers.
In the aftermath of the pandemic, is it expected that there will be long-term repercussions both from an economic [ 8 ] and a mental health perspective [ 71 ]. Furthermore, the findings from this review suggest that although those in areas with high levels of SC may be negatively affected in the acute stage, as time passes, they have potential to rebound at a faster rate than those with lower levels of SC. Ongoing evaluation of the effectiveness of current initiatives as the COVID-19 pandemic progresses into a recovery phase will be invaluable for supplementing the evidence base identified through this review.
- Recommendations
As a result of this review, a number of recommendations are suggested for policy and practice during public health emergencies and recovery.
Future research should seek to establish a standardised and validated approach to measuring and defining CR and SC within communities. There are ongoing efforts in this area, for example [ 72 ]. Additionally, community members should be involved in the process of defining how CR is measured.
There should be an enhanced effort to improve preparedness for public health emergencies and disasters in local communities by gauging current levels of SC and CR within communities using a standardised measure. This approach could support specific targeting of populations with low levels of CR/SC in case of a disaster or public health emergency, whilst also allowing for consideration of support for those with high levels of CR (as these populations can be heavily impacted initially following a disaster). By distinguishing levels of SC and CR, tailored community-centred approaches could be implemented, such as those listed in a guide released by PHE in 2015 [ 73 ].
CR and SC (specifically cognitive SC) should be bolstered if communities are at risk of experiencing a disaster or public health emergency. This can be achieved by using interventions which aim to increase a sense of community and create new social ties (e.g., recreational group activities, volunteering). Additionally, when aiming to achieve this, it is important to be mindful of the risk of increased levels of CR/SC to backfire, as well as seeking to advocate an integrated system approach across individual, community and structural levels.
It is necessary to be aware that although communities with high existing levels of resilience / SC may experience short-term negative consequences following a disaster, over time these communities might be able to recover at a faster rate. It is therefore important to ensure that suitable short-term support is provided to these communities in the immediate aftermath of a public health emergency or disaster.
Robust evaluation of the community resilience initiatives deployed during the COVID-19 pandemic response is essential to inform the evidence base concerning the effectiveness of CR/ SC. These evaluations should continue through the response phase and into the recovery phase to help develop our understanding of the long-term consequences of such interventions.
Limitations
Despite this review being the first in this specific topic area, there are limitations that must be considered. Firstly, it is necessary to note that communities are generally highly diverse and the term ‘community’ in academic literature is a subject of much debate (see: [ 74 ]), therefore this must be considered when comparing and collating research involving communities. Additionally, the measures of CR and SC differ substantially across research, including across the 26 retained papers used in the current review. This makes the act of comparing and collating research findings very difficult. This issue is highlighted as a key outcome from this review, and suggestions for how to overcome this in future research are provided. Additionally, we acknowledge that there will be a relationship between CR & SC even where studies measure only at individual or community level. A review [ 75 ] on articulating a hypothesis of the link to health inequalities suggests that wider structural determinants of health need to be accounted for. Secondly, despite the final search strategy encompassing terms for both CR and SC, only one retained paper directly measured CR; thus, making the research findings more relevant to SC. Future research could seek to focus on CR to allow for a comparison of findings. Thirdly, the review was conducted early in the COVID-19 pandemic and so does not include more recent publications focusing on resilience specifically in the context of COVID-19. Regardless of this fact, the synthesis of, and recommendations drawn from, the reviewed studies are agnostic to time and specific incident and contain critical elements necessary to address as the pandemic moves from response to recovery. Further research should review the effectiveness of specific interventions during the COVID-19 pandemic for collation in a subsequent update to this current paper. Fourthly, the current review synthesises findings from countries with individualistic and collectivistic cultures, which may account for some variation in the findings. Lastly, despite choosing a scoping review method for ease of synthesising a wide literature base for use by public health emergency researchers in a relatively tight timeframe, there are disadvantages of a scoping review approach to consider: (1) quality appraisal of retained studies was not carried out; (2) due to the broad nature of a scoping review, more refined and targeted reviews of literature (e.g., systematic reviews) may be able to provide more detailed research outcomes. Therefore, future research should seek to use alternative methods (e.g., empirical research, systematic reviews of literature) to add to the evidence base on CR and SC impact and use in public health practice.
This review sought to establish: (1) How CR and SC are quantified in research?; (2) The impact of community resilience on mental wellbeing?; (3) The impact of infectious disease outbreaks, disasters and emergencies on community resilience and social capital?; and, (4) What types of interventions enhance community resilience and social capital?. The chosen search strategy yielded 26 relevant papers from which we were able extract information relating to the aims of this review.
Results from the review revealed that CR and SC are not measured consistently across research. The impact of CR / SC on mental health and wellbeing during emergencies and disasters is mixed (with some potential for backlash), however the literature does identify cognitive SC as particularly protective. Although only a small number of papers compared CR or SC before and after a disaster, the findings were relatively consistent: SC or CR is negatively impacted by a disaster. Methods suggested to bolster SC in communities were centred around social activities, such as recreational group activities and volunteering. Recommendations for both research and practice (with a particular focus on the ongoing COVID-19 pandemic) are also presented.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Social Capital
Zortea TC, Brenna CT, Joyce M, McClelland H, Tippett M, Tran MM, et al. The impact of infectious disease-related public health emergencies on suicide, suicidal behavior, and suicidal thoughts. Crisis. 2020;42(6):474–87.
Article PubMed PubMed Central Google Scholar
Davis JR, Wilson S, Brock-Martin A, Glover S, Svendsen ER. The impact of disasters on populations with health and health care disparities. Disaster Med Pub Health Prep. 2010;4(1):30.
Article Google Scholar
Francescutti LH, Sauve M, Prasad AS. Natural disasters and healthcare: lessons to be learned. Healthc Manage Forum. 2017;30(1):53–5.
Article PubMed Google Scholar
Jones L, Palumbo D, Brown D. Coronavirus: How the pandemic has changed the world economy. BBC News; 2021. Accessible at: https://www.bbc.co.uk/news/business-51706225 .
Below R, Wallemacq P. Annual disaster statistical review 2017. Brussels: CRED, Centre for Research on the Epidemiology of Disasters; 2018.
Google Scholar
Qiu W, Chu C, Mao A, Wu J. The impacts on health, society, and economy of SARS and H7N9 outbreaks in China: a case comparison study. J Environ Public Health. 2018;2018:2710185.
Worldometer. COVID-19 coronavirus pandemic. 2021.
Harari D, Keep M. Coronavirus: economic impact house of commons library. Briefing Paper (Number 8866); 2021. Accessible at: https://commonslibrary.parliament.uk/research-briefings/cbp-8866/ .
Nabavi N. Covid-19: pandemic will cast a long shadow on mental health, warns England’s CMO. BMJ. 2021;373:n1655.
Ziglio E. Strengthening resilience: a priority shared by health 2020 and the sustainable development goals. No. WHO/EURO: 2017-6509-46275-66939. World Health Organization; Regional Office for Europe; 2017.
Asadzadeh A, Kotter T, Salehi P, Birkmann J. Operationalizing a concept: the systematic review of composite indicator building for measuring community disaster resilience. Int J Disaster Risk Reduct. 2017;25:147.
Sherrieb K, Norris F, Galea S. Measuring capacities for community resilience. Soc Indicators Res. 2010;99(2):227.
Poortinga W. Community resilience and health: the role of bonding, bridging, and linking aspects of social capital. Health Place. 2011;18(2):286–95.
Ferlander S. The importance of different forms of social capital for health. Acta Sociol. 2007;50(2):115–28.
Nakagawa Y, Shaw R. Social capital: a missing link to disaster recovery. Int J Mass Emerge Disasters. 2004;22(1):5–34.
Grootaert C, Narayan D, Jones VN, Woolcock M. Measuring social capital: an integrated questionnaire. Washington, DC: World Bank Working Paper, No. 18; 2004.
Adler PS, Kwon SW. Social capital: prospects for a new concept. Acad Manage Rev. 2002;27(1):17–40.
Aldrich DP, Meyer MA. Social capital and community resilience. Am Behav Sci. 2015;59(2):254–69.
Rodriguez-Llanes JM, Vos F, Guha-Sapir D. Measuring psychological resilience to disasters: are evidence-based indicators an achievable goal? Environ Health. 2013;12(1):115.
De Silva MJ, McKenzie K, Harpham T, Huttly SR. Social capital and mental Illness: a systematic review. J Epidemiol Community Health. 2005;59(8):619–27.
Bonanno GA, Galea S, Bucciarelli A, Vlahov D. Psychological resilience after disaster: New York City in the aftermath of the september 11th terrorist attack. Psychol Sci. 2006;17(3):181.
World Health Organization. Health 2020: a European policy framework and strategy for the 21st century. World Health Organization. Regional Office for Europe; 2013.
Public Health England. Community-Centred Public Health: Taking a Whole System Approach. 2020.
SPI-B. The role of Community Champion networks to increase engagement in the context of COVID19: Evidence and best practice. 2021.
Public Health England. Community champions: A rapid scoping review of community champion approaches for the pandemic response and recovery. 2021.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
World Health Organisation. WHO health evidence network synthesis report: what quantitative and qualitative methods have been developed to measure health-related community resilience at a national and local level. 2018.
Hall C, Williams N, Gauntlett L, Carter H, Amlôt R, Peterson L et al. Findings from systematic review of public perceptions and responses. PROACTIVE EU. Deliverable 1.1. 2019. Accessible at: https://proactive-h2020.eu/wp-content/uploads/2021/04/PROACTIVE_20210312_D1.1_V5_PHE_Systematic-Review-of-Public-Perceptions-and-Responses_revised.pdf .
Weston D, Ip A, Amlôt R. Examining the application of behaviour change theories in the context of Infectious disease outbreaks and emergency response: a review of reviews. BMC Public Health. 2020;20(1):1483.
Article PubMed PubMed Central CAS Google Scholar
Patel SS, Rogers MB, Amlôt R, Rubin GJ. What do we mean by ‘community resilience’? A systematic literature review of how it is defined in the literature. PLoS Curr. 2017;9:ecurrents.dis.db775aff25efc5ac4f0660ad9c9f7db2.
PubMed PubMed Central Google Scholar
Brooks SK, Weston D, Wessely S, Greenberg N. Effectiveness and acceptability of brief psychoeducational interventions after potentially traumatic events: a systematic review. Eur J Psychotraumatology. 2021;12(1):1923110.
Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review-a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy. 2005;10(1_suppl):21–34.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:1–8.
Bearman M, Dawson P. Qualitative synthesis and systematic review in health professions education. Med Educ. 2013;47(3):252–60.
Heid AR, Pruchno R, Cartwright FP, Wilson-Genderson M. Exposure to Hurricane Sandy, neighborhood collective efficacy, and post-traumatic stress symptoms in older adults. Aging Ment Health. 2017;21(7):742–50.
Hikichi H, Aida J, Tsuboya T, Kondo K, Kawachi I. Can community social cohesion prevent posttraumatic stress disorder in the aftermath of a disaster? A natural experiment from the 2011 Tohoku Earthquake and tsunami. Am J Epidemiol. 2016;183(10):902–10.
Lee J, Blackmon BJ, Cochran DM, Kar B, Rehner TA, Gunnell MS. Community resilience, psychological resilience, and depressive symptoms: an examination of the Mississippi Gulf Coast 10 years after Hurricane Katrina and 5 years after the Deepwater Horizon oil spill. Disaster med. 2018;12(2):241–8.
Lee J, Blackmon BJ, Lee JY, Cochran DM Jr, Rehner TA. An exploration of posttraumatic growth, loneliness, depression, resilience, and social capital among survivors of Hurricane Katrina and the deepwater Horizon oil spill. J Community Psychol. 2019;47(2):356–70.
Lowe SR, Sampson L, Gruebner O, Galea S. Psychological resilience after Hurricane Sandy: the influence of individual- and community-level factors on mental health after a large-scale natural disaster. PLoS One. 2015;10(5):e0125761.
Rung AL, Gaston S, Robinson WT, Trapido EJ, Peters ES. Untangling the disaster-depression knot: the role of social ties after deepwater Horizon. Soc Sci Med. 2017;177:19–26.
Weil F, Lee MR, Shihadeh ES. The burdens of social capital: how socially-involved people dealt with stress after Hurricane Katrina. Soc Sci Res. 2012;41(1):110–9.
Hikichi H, Aida J, Matsuyama Y, Tsuboya T, Kondo K, Kawachi I. Community-level social capital and cognitive decline after a Natural Disaster: a natural experiment from the 2011 Great East Japan Earthquake and Tsunami. Soc Sci Med. 2018;257:111981.
Lau AL, Chi I, Cummins RA, Lee TM, Chou KL, Chung LW. The SARS (severe acute respiratory syndrome) pandemic in Hong Kong: effects on the subjective wellbeing of elderly and younger people. Aging Ment Health. 2008;12(6):746–60.
Sun Y, Yan T. The use of public health indicators to assess individual happiness in post-disaster recovery. Int J Environ Res Public Health. 2019;16(21):4101.
Wong H, Huang Y, Fu Y, Zhang Y. Impacts of structural social capital and cognitive social capital on the psychological status of survivors of the yaan Earthquake. Appl Res Qual Life. 2018;14:1411–33.
Xiao H, Zhang Y, Kong D, Li S, Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit. 2020;26:e923921.
PubMed PubMed Central CAS Google Scholar
Matsuyama Y, Aida J, Hase A, Sato Y, Koyama S, Tsuboya T, et al. Do community- and individual-level social relationships contribute to the mental health of disaster survivors? A multilevel prospective study after the great East Japan earthquake. Soc Sci Med. 2016;151:187–95.
Ozaki A, Horiuchi S, Kobayashi Y, Inoue M, Aida J, Leppold C, Yamaoka K. Beneficial roles of social support for mental health vary in the Japanese population depending on disaster experience: a nationwide cross-sectional study. Tohoku J Exp Med. 2018;246(4):213–23.
Sato K, Amemiya A, Haseda M, Takagi D, Kanamori M, Kondo K, et al. Post-disaster changes in Social Capital and Mental Health: a natural experiment from the 2016 Kumamoto Earthquake. Am J Epidemiol. 2020;189(9):910–21.
Tsuchiya N, Nakaya N, Nakamura T, Narita A, Kogure M, Aida J, Tsuji I, Hozawa A, Tomita H. Impact of social capital on psychological distress and interaction with house destruction and displacement after the great East Japan earthquake of 2011. J Neuropsychiatry Clin Neurosci. 2017;71(1):52–60.
Brockie L, Miller E. Understanding older adults’ resilience during the Brisbane floods: social capital, life experience, and optimism. Disaster Med Pub Health Prep. 2017;11(1):72–9.
Caldwell K, Boyd CP. Coping and resilience in farming families affected by drought. Rural Remote Health. 2009;9(2):1088.
PubMed Google Scholar
Huang Y, Tan NT, Liu J. Support, sense of community, and psychological status in the survivors of the Yaan earthquake. J Community Psychol. 2016;44(7):919–36.
Wind T, Fordham M, Komproe H. Social capital and post-disaster mental health. Glob Health Action. 2011;4(1):6351.
Wind T, Komproe IH. The mechanisms that associate community social capital with post-disaster mental health: a multilevel model. Soc Sci Med. 2012;75(9):1715–20.
Hogg D, Kingham S, Wilson TM, Ardagh M. The effects of spatially varying earthquake impacts on mood and anxiety symptom treatments among long-term Christchurch residents following the 2010/11 Canterbury Earthquakes, New Zealand. Health Place. 2016;41:78–88.
Flores EC, Carnero AM, Bayer AM. Social capital and chronic post-traumatic stress disorder among survivors of the 2007 earthquake in Pisco, Peru. Soc Sci Med. 2014;101:9–17.
Rafiey H, Alipour F, LeBeau R, Salimi Y, Ahmadi S. Exploring the buffering role of social capital in the development of posttraumatic stress symptoms among Iranian earthquake survivors. Psychol Trauma. 2019;14(6):1040–6.
Babcicky P, Seebauer S. The two faces of social capital in private Flood mitigation: opposing effects on risk perception, self-efficacy and coping capacity. J Risk Res. 2017;20(8):1017–37.
Bakic H, Ajdukovic D. Stability and change post-disaster: dynamic relations between individual, interpersonal and community resources and psychosocial functioning. Eur J Psychotraumatol. 2019;10(1):1614821.
Rogers RW. A protection motivation theory of fear appeals and attitude change. J Psychol. 1975;91(1):93–114.
Lindberg K, Swearingen T. A reflective thrive-oriented community resilience scale. Am J Community Psychol. 2020;65(3–4):467–78.
Leykin D, Lahad M, Cohen O, Goldberg A, Aharonson-Daniel L. Conjoint community resiliency assessment measure-28/10 items (CCRAM28 and CCRAM10): a self-report tool for assessing community resilience. Am J Community Psychol. 2013;52:313–23.
Sherrieb K, Norris FH, Galea S. Measuring capacities for community resilience. Soc Indic Res. 2010;99:227–47.
Ehsan AM, De Silva MJ. Social capital and common mental disorder: a systematic review. J Epidemiol Community Health. 2015;69(10):1021–8.
Pfefferbaum B, Van Horn RL, Pfefferbaum RL. A conceptual framework to enhance community resilience using social capital. Clin Soc Work J. 2017;45(2):102–10.
Carmen E, Fazey I, Ross H, Bedinger M, Smith FM, Prager K, et al. Building community resilience in a context of climate change: the role of social capital. Ambio. 2022;51(6):1371–87.
Humbert C, Joseph J. Introduction: the politics of resilience: problematising current approaches. Resilience. 2019;7(3):215–23.
Tanner T, Bahadur A, Moench M. Challenges for resilience policy and practice. Working paper: 519. 2017.
Vadivel R, Shoib S, El Halabi S, El Hayek S, Essam L, Bytyçi DG. Mental health in the post-COVID-19 era: challenges and the way forward. Gen Psychiatry. 2021;34(1):e100424.
Article CAS Google Scholar
Pryor M. Social Capital Harmonised Standard. London: Government Statistical Service. 2021. Accessible at: https://gss.civilservice.gov.uk/policystore/social-capital/ .
Public Health England NE. A guide to community-centred approaches for health and wellbeing. 2015.
Hawe P. Capturing the meaning of ‘community’ in community intervention evaluation: some contributions from community psychology. Health Promot Int. 1994;9(3):199–210.
Uphoff EP, Pickett KE, Cabieses B, Small N, Wright J. A systematic review of the relationships between social capital and socioeconomic inequalities in health: a contribution to understanding the psychosocial pathway of health inequalities. Int J Equity Health. 2013;12:1–12.
Download references
Acknowledgements
Not applicable.
This study was supported by the National Institute for Health Research Research Unit (NIHR HPRU) in Emergency Preparedness and Response, a partnership between Public Health England, King’s College London and the University of East Anglia. The views expressed are those of the author(s) and not necessarily those of the NIHR, Public Health England, the UK Health Security Agency or the Department of Health and Social Care [Grant number: NIHR20008900]. Part of this work has been funded by the Office for Health Improvement and Disparities, Department of Health and Social Care, as part of a Collaborative Agreement with Leeds Beckett University.
Author information
Authors and affiliations.
Behavioural Science and Insights Unit, Evaluation & Translation Directorate, Science Group, UK Health Security Agency, Porton Down, Salisbury, SP4 0JG, UK
C. E. Hall, H. Wehling, R. Amlôt & D. Weston
Health Protection Research Unit, Institute of Psychology, Psychiatry and Neuroscience, King’s College London, 10 Cutcombe Road, London, SE5 9RJ, UK
C. E. Hall, S. K. Brooks & N. Greenberg
School of Health and Community Studies, Leeds Beckett University, Portland Building, PD519, Portland Place, Leeds, LS1 3HE, UK
J. Stansfield & J. South
King’s Centre for Military Health Research, Institute of Psychology, Psychiatry and Neuroscience, King’s College London, 10 Cutcombe Road, London, SE5 9RJ, UK
N. Greenberg
You can also search for this author in PubMed Google Scholar
Contributions
DW, JSo and JSt had the main idea for the review. The search strategy and eligibility criteria were devised by CH, DW, JSo and JSt. CH conducted the database searches. CH and DW conducted duplicate, title and abstract and full text screening in accordance with inclusion criteria. CH conducted data extraction, CH and DW carried out the analysis and drafted the initial manuscript. All authors provided critical revision of intellectual content. All authors approved the final manuscript.
Authors’ information
Corresponding author.
Correspondence to D. Weston .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., additional file 2., additional file 3., additional file 4., additional file 5., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hall, C.E., Wehling, H., Stansfield, J. et al. Examining the role of community resilience and social capital on mental health in public health emergency and disaster response: a scoping review. BMC Public Health 23 , 2482 (2023). https://doi.org/10.1186/s12889-023-17242-x
Download citation
Received : 04 April 2022
Accepted : 16 November 2023
Published : 12 December 2023
DOI : https://doi.org/10.1186/s12889-023-17242-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Community cohesion
- Public health emergency
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- COVID-19 and your mental health
Worries and anxiety about COVID-19 can be overwhelming. Learn ways to cope as COVID-19 spreads.
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020.
Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19. And you're not alone if you've coped with the stress in less than healthy ways, such as substance use.
But healthier self-care choices can help you cope with COVID-19 or any other challenge you may face.
And knowing when to get help can be the most essential self-care action of all.
Recognize what's typical and what's not
Stress and worry are common during a crisis. But something like the COVID-19 pandemic can push people beyond their ability to cope.
In surveys, the most common symptoms reported were trouble sleeping and feeling anxiety or nervous. The number of people noting those symptoms went up and down in surveys given over time. Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well.
The first step is to notice how often you feel helpless, sad, angry, irritable, hopeless, anxious or afraid. Some people may feel numb.
Keep track of how often you have trouble focusing on daily tasks or doing routine chores. Are there things that you used to enjoy doing that you stopped doing because of how you feel? Note any big changes in appetite, any substance use, body aches and pains, and problems with sleep.
These feelings may come and go over time. But if these feelings don't go away or make it hard to do your daily tasks, it's time to ask for help.
Get help when you need it
If you're feeling suicidal or thinking of hurting yourself, seek help.
- Contact your healthcare professional or a mental health professional.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
If you are worried about yourself or someone else, contact your healthcare professional or mental health professional. Some may be able to see you in person or talk over the phone or online.
You also can reach out to a friend or loved one. Someone in your faith community also could help.
And you may be able to get counseling or a mental health appointment through an employer's employee assistance program.
Another option is information and treatment options from groups such as:
- National Alliance on Mental Illness (NAMI).
- Substance Abuse and Mental Health Services Administration (SAMHSA).
- Anxiety and Depression Association of America.
Self-care tips
Some people may use unhealthy ways to cope with anxiety around COVID-19. These unhealthy choices may include things such as misuse of medicines or legal drugs and use of illegal drugs. Unhealthy coping choices also can be things such as sleeping too much or too little, or overeating. It also can include avoiding other people and focusing on only one soothing thing, such as work, television or gaming.
Unhealthy coping methods can worsen mental and physical health. And that is particularly true if you're trying to manage or recover from COVID-19.
Self-care actions can help you restore a healthy balance in your life. They can lessen everyday stress or significant anxiety linked to events such as the COVID-19 pandemic. Self-care actions give your body and mind a chance to heal from the problems long-term stress can cause.
Take care of your body
Healthy self-care tips start with the basics. Give your body what it needs and avoid what it doesn't need. Some tips are:
- Get the right amount of sleep for you. A regular sleep schedule, when you go to bed and get up at similar times each day, can help avoid sleep problems.
- Move your body. Regular physical activity and exercise can help reduce anxiety and improve mood. Any activity you can do regularly is a good choice. That may be a scheduled workout, a walk or even dancing to your favorite music.
- Choose healthy food and drinks. Foods that are high in nutrients, such as protein, vitamins and minerals are healthy choices. Avoid food or drink with added sugar, fat or salt.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to manage how you feel can make matters worse and reduce your coping skills. Avoid taking illegal drugs or misusing prescriptions to manage your feelings.
Take care of your mind
Healthy coping actions for your brain start with deciding how much news and social media is right for you. Staying informed, especially during a pandemic, helps you make the best choices but do it carefully.
Set aside a specific amount of time to find information in the news or on social media, stay limited to that time, and choose reliable sources. For example, give yourself up to 20 or 30 minutes a day of news and social media. That amount keeps people informed but not overwhelmed.
For COVID-19, consider reliable health sources. Examples are the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Other healthy self-care tips are:
- Relax and recharge. Many people benefit from relaxation exercises such as mindfulness, deep breathing, meditation and yoga. Find an activity that helps you relax and try to do it every day at least for a short time. Fitting time in for hobbies or activities you enjoy can help manage feelings of stress too.
- Stick to your health routine. If you see a healthcare professional for mental health services, keep up with your appointments. And stay up to date with all your wellness tests and screenings.
- Stay in touch and connect with others. Family, friends and your community are part of a healthy mental outlook. Together, you form a healthy support network for concerns or challenges. Social interactions, over time, are linked to a healthier and longer life.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel sad, hurt and angry when people in their community avoid them for fear of getting COVID-19. People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers and people with COVID-19.
Treating people differently because of their medical condition, called medical discrimination, isn't new to the COVID-19 pandemic. Stigma has long been a problem for people with various conditions such as Hansen's disease (leprosy), HIV, diabetes and many mental illnesses.
People who experience stigma may be left out or shunned, treated differently, or denied job and school options. They also may be targets of verbal, emotional and physical abuse.
Communication can help end stigma or discrimination. You can address stigma when you:
- Get to know people as more than just an illness. Using respectful language can go a long way toward making people comfortable talking about a health issue.
- Get the facts about COVID-19 or other medical issues from reputable sources such as the CDC and WHO.
- Speak up if you hear or see myths about an illness or people with an illness.
COVID-19 and health
The virus that causes COVID-19 is still a concern for many people. By recognizing when to get help and taking time for your health, life challenges such as COVID-19 can be managed.
- Mental health during the COVID-19 pandemic. National Institutes of Health. https://covid19.nih.gov/covid-19-topics/mental-health. Accessed March 12, 2024.
- Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1. Accessed March 12, 2024.
- Mental health and the pandemic: What U.S. surveys have found. Pew Research Center. https://www.pewresearch.org/short-reads/2023/03/02/mental-health-and-the-pandemic-what-u-s-surveys-have-found/. Accessed March 12, 2024.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed March 12, 2024.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed March 12, 2024.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed March 12, 2024.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- COVID-19 and substance abuse. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/covid-19-substance-use#health-outcomes. Accessed March 12, 2024.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed March 15, 2024.
- Negative coping and PTSD. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/gethelp/negative_coping.asp. Accessed March 15, 2024.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed March 15, 2024.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed March 15, 2024.
- World leprosy day: Bust the myths, learn the facts. Centers for Disease Control and Prevention. https://www.cdc.gov/leprosy/world-leprosy-day/. Accessed March 15, 2024.
- HIV stigma and discrimination. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/hiv-stigma/. Accessed March 15, 2024.
- Diabetes stigma: Learn about it, recognize it, reduce it. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html. Accessed March 15, 2024.
- Phelan SM, et al. Patient and health care professional perspectives on stigma in integrated behavioral health: Barriers and recommendations. Annals of Family Medicine. 2023; doi:10.1370/afm.2924.
- Stigma reduction. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/od2a/case-studies/stigma-reduction.html. Accessed March 15, 2024.
- Nyblade L, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Medicine. 2019; doi:10.1186/s12916-019-1256-2.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed March 15, 2024.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Sawchuk CN (expert opinion). Mayo Clinic. March 25, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 drugs: Are there any that work?
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to take your pulse
- How to measure your respiratory rate
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Mental health: What's normal, what's not - Related information Mental health: What's normal, what's not
- Mental illness - Related information Mental illness
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
The independent source for health policy research, polling, and news.
The Implications of COVID-19 for Mental Health and Substance Use
Nirmita Panchal , Heather Saunders , Robin Rudowitz , and Cynthia Cox Published: Mar 20, 2023
Note: This brief was updated on March 20, 2023 to incorporate the latest available data. Concerns about mental health and substance use remain elevated three years after the onset of the COVID-19 pandemic, with 90% of U.S. adults believing that the country is facing a mental health crisis, according to a recent KFF/CNN survey. The pandemic has affected the public’s mental health and well-being in a variety of ways, including through isolation and loneliness, job loss and financial instability, and illness and grief.
Over the course of the pandemic, many adults reported symptoms consistent with anxiety and depression, with approximately four in ten adults reporting these symptoms by early 2021, before declining to approximately three in ten adults as the pandemic continued (Figure 1). Additionally, drug overdose deaths have sharply increased – largely due to fentanyl – and after a brief period of decline, suicide deaths are once again on the rise. These negative mental health and substance use outcomes have disproportionately affected some populations, particularly communities of color and youth. As the end of the declaration of the public health emergency nears – on May 11, 2023 – many people continue to grapple with worsened mental health and well-being and face barriers to care.
This brief explores mental health and substance use during, and prior to, the COVID-19 pandemic. We highlight populations that were more likely to experience worse mental health and substance use outcomes during the pandemic and discuss some innovations in the delivery of services. We analyze and present findings using the most recent data available at the time of this publication – including the Household Pulse Survey and the CDC WONDER database . Key takeaways include:
- Symptoms of anxiety and depression increased during the pandemic and are more pronounced among individuals experiencing household job loss, young adults, and women. Adolescent females have also experienced increased feelings of hopelessness and sadness compared to their male peers.
- Deaths due to drug overdose increased sharply across the total population coinciding with the pandemic – and more than doubled among adolescents. Drug overdose death rates are highest among American Indian and Alaska Native people and Black people.
- Alcohol-induced death rates increased substantially during the pandemic, with rates increasing the fastest among people of color and people living in rural areas.
- After briefly decreasing, suicide deaths are on the rise again as of 2021. From 2019 to 2021, many communities of color experienced a larger growth in suicide death rates compared to their White counterparts. Additionally, self-harm and suicidal ideation has increased faster among adolescent females compared to their male peers.
- Several changes have been implemented in the delivery of mental health and substance use services since the onset of the pandemic, including the utilization of telehealth, steps to improve access to treatment for opioid use disorders, expansion of school-based mental health care, and the rollout of the 988 crisis line. As the public health emergency declaration comes to an end, it is possible that some of these changes will be interrupted.
Prevalence of Mental Illness and Substance Use During the Pandemic
Anxiety and depression.
The pandemic was associated with a high prevalence of anxiety and depression symptoms in adults. Research suggests that these symptoms increased during the pandemic, but the extent of this increase is unclear . 1 Throughout the pandemic, symptoms of anxiety and depression have been more pronounced among several populations.
For example, individuals experiencing household job loss were more likely than their counterparts to report symptoms of anxiety and/or depression (53% vs. 30%) in February 2023 (Figure 2). Job loss and unemployment – which have long been associated with adverse mental health outcomes – increased substantially early on in the pandemic .
Fifty percent of young adults (ages 18-24) reported anxiety and depression symptoms in 2023, making them more likely than older adults to experience mental health symptoms (Figure 2). Young adults have experienced a number of pandemic-related consequences – such as closures of universities, transitioning to remote work, and loss of income or employment – that may contribute to poor mental health. Additionally, young adults in college settings may encounter increased difficulty accessing treatment .
Symptoms of anxiety and/or depression were also elevated among women (36%) compared to men (28%) in February 2023 (Figure 2). Even before the pandemic, women were more likely than men to report mental health disorders, including serious mental illness.
Concerns about youth mental health further increased with the onset of the pandemic and the recent uptick in gun violence . In a recent KFF/CNN survey , roughly half of parents (47%) said the pandemic had a negative impact on their child’s mental health, including 17% who said it had a “major negative impact”. Poor mental health has been more pronounced among adolescent females in particular. As shown in Figure 3, the gap in the share of adolescent females and males reporting feelings of hopelessness and sadness – symptoms indicative of depressive disorder – widened from 2019 (47% vs. 27%, respectively) to 2021 (57% vs. 29%, respectively). Many female adolescents also reported adverse experiences in 2021, which can negatively impact mental health.
Substance use and deaths
The pandemic has coincided with an increase in substance use and increased death rates due to substances. In 2021, there were over 106,600 deaths due to drug overdose in the U.S. – the highest on record. This spike in deaths has primarily been driven by substances laced with synthetic opioids, including illicitly manufactured fentanyl .
Further, the overall drug overdose death rate rose by 50% during the pandemic (Figure 4), but varied across states . While drug overdose death rates increased across all racial and ethnic groups, the increases were larger for people of color compared to White people. White people continue to account for the largest share of deaths due to drug overdose per year, but people of color are accounting for a growing share of these deaths over time. In 2021, the highest drug overdose death rates were among American Indian Alaska Native (AIAN) people (56.6 per 100,000), Black people (44.2 per 100,000), and White people (36.8 per 100,000) (Figure 4). Differences in drug overdose deaths by sex were also exacerbated during the pandemic. As shown in Figure 4, the gap in the drug overdose death rates between males and females increased from 2019 (29.6 vs. 13.7 per 100,000, respectively) to 2021 (45.1 vs. 19.6 per 100,000, respectively).
Research suggests that substance use among adolescents has declined, yet drug overdose deaths have sharply increased among this population, primarily due to fentanyl-laced substances . Among adolescents, drug overdose deaths have more than doubled from 2019 (282 deaths) to 2021 (637 deaths) following a period of relative stability. 2 Male, Black, and Hispanic youth have experienced the highest increases in deaths due to drug overdose.
During the pandemic, excessive drinking increased along with alcohol-induced deaths. Alcohol-induced death rates increased by 38% during the pandemic, with rates the highest and increasing the fastest among AIAN people. AIAN people died of alcohol-induced causes at a rate of 91.7 per 100,000 in 2021, six times more than the next highest group – Hispanic people at a rate of 13.6. Black people also experienced significant increases in alcohol-induced deaths during COVID, with rates increasing more than 45% (Figure 5). Both rural and metropolitan areas experienced an increase in alcohol-induced deaths during the pandemic, but rural areas saw the largest increase (46% increase compared to 36%).
Suicidal ideation and deaths
Concerns about suicidal ideation and suicide deaths have also grown during the pandemic. Notably, self-harm and suicidal ideation has increased among adolescent females. Thirty percent of adolescent females seriously considered attempting suicide in 2021 compared to 14% of their male peers (Figure 6). Other analyses found that as the pandemic progressed, emergency department visits for suicide attempts increased among adolescents, primarily driven by females.
Suicide deaths in the U.S. began to increase in 2021 after briefly slowing in 2019 and 2020 , although some research suggests that some suicides may be misclassified as drug overdose deaths since it can be difficult to determine whether drug overdoses are intentional . From 2019 to 2021, many communities of color experienced a larger growth in suicide death rates compared to their White counterparts. 3 In 2021, suicide deaths by firearm accounted for more than half ( 55% ) of all suicides in the U.S., but varied greatly across states .
The pandemic has also raised concerns about mental illness, suicide, and substance use among other populations. Essential workers and people with chronic health conditions may have experienced worsened mental health due to increased risk of contracting or becoming severely ill from COVID-19. Many of these individuals, particularly those with chronic conditions , were already at-risk of experiencing poor mental health outcomes prior to the pandemic. LBGT+ people have historically faced mental health problems at higher rates than their non-LGBT+ peers. The pandemic has continued to negatively impact LBGT+ people’s mental health in disproportionate ways. In addition, people experiencing prolonged COVID-19 symptoms, or long COVID , may be more likely to develop new mental health conditions or to experience worsening of existing ones.
Changes in the Delivery of Mental Health and Substance Use Disorder Services
Leading up to the pandemic, many people faced barriers accessing mental health and substance use disorder services for reasons including costs, not knowing where to obtain care, limited provider options, and low rates of insurance acceptance. Young adults, Black adults, men, and uninsured people were less likely to receive services compared to their peers.
In recent years, access to care barriers may have worsened due to pandemic disruptions and closures, workforce shortages, and increased demand for services. In response to growing need, some policies and strategies were implemented to address access challenges, such as growth of telehealth, improved access to opioid use disorder treatment, the expansion of school-based mental health services, and the rollout of 988; however, challenges remain.
The delivery of mental health and substance use disorder services via telehealth grew sharply during the pandemic. By 2021, nearly 40% of all mental health and substance use disorder outpatient visits were delivered through telehealth. These behavioral health services via telehealth have also been more utilized in rural areas than urban areas during the pandemic. This underscores the role telehealth can play in improving access to behavioral health services in rural areas, which often face additional provider and resource shortages . Further, community health centers – which serve low-income and medically underserved communities, including communities of color and those in rural areas – experienced a large increase in behavioral health visits in 2021, largely driven by telehealth. During the pandemic, many state Medicaid programs expanded coverage of behavioral health telehealth services. This includes broadening the range of behavioral health services offered virtually and allowing for more provider types to be reimbursed for telehealth services. Many state Medicaid programs reported that telehealth has helped maintain and expand access to behavioral services during the pandemic. Some private payers have also improved coverage for mental health and substance use services by removing pre-pandemic telehealth coverage restrictions. Although telehealth can broaden access to care, in-person care may be necessary or preferred for some or for those experiencing challenges with technology and digital literacy.
As opioid-related overdose deaths have sharply increased, measures to improve access to treatment have been implemented. Following the onset of the pandemic , the federal government allowed for new flexibilities in opioid use disorder (OUD) treatment to ease access barriers, for example allowing for take-home methadone doses and covering telehealth treatment, and the Biden administration has proposed making these flexibilities permanent. Further, the 2023 Consolidated Appropriations Act eliminated the X-waiver requirement for prescribing buprenorphine, which substantially increases the number of providers who are authorized to prescribe buprenorphine to treat OUD. Voluntary guidelines for providers have also been issued to help reduce opioid overprescribing and misuse. At the same time, the Drug Enforcement Agency recently proposed returning to previous rules that required in-person visits before prescribing controlled substances to patients via telehealth, though there are some exceptions.
In response to growing mental health concerns among youth, integration of mental health services in school-based settings became a priority. Recent legislation aims to expand mental health care in schools – a setting that is easily accessible by children and adolescents. Specifically, legislation provides funding to expand and train mental health providers in schools; implement suicide, drug, and violence prevention programs; and provide trauma support services, among others. Further, recognizing Medicaid’s importance in covering and financing behavioral health care for children , CMS is now required to provide updated guidance on how to support and expand school-based behavioral health services. The recently passed Consolidated Appropriations Act (CAA) continues to build on prior pandemic-era legislation that promotes access to behavioral health care for children. For example, to ensure more stable coverage for low-income children the CAA requires states to provide 12 months of continuous eligibility for children in Medicaid and CHIP.
An easy-to-remember number for the suicide and behavioral health crisis hotline, 988, was launched in 2022 . On July 16, 2022, the federally mandated crisis number , 988 , became available to all landline and cell phone users , providing a single three-digit number to access a network of over 200 local and state funded crisis centers where those in need may receive crisis counseling, resources and referrals. After 988 implementation, national answer rates increased alongside increases in call volume. Long-term sustainable funding of local 988 crisis call centers remains uncertain in many states. In addition to 988, some states are developing behavioral health crisis response systems, such as mobile crisis or crisis stabilization units, which will enable a specialized behavioral health response for behavioral health crises that require intervention. The CAA included provisions aimed at strengthening and evaluating 988 and the developing behavioral health crisis continuum.
Despite steps taken to improve the delivery of mental health and substance use services, challenges remain. Provider workforce challenges are widespread, with nearly half of the U.S. population ( 47% ) living in a mental health workforce shortage area . Shortages may contribute to access challenges and contribute to increases in psychiatric boarding in emergency rooms. Additionally, provider network directories are often outdated, further contributing to access challenges. While recent legislation has taken steps in response – including funding for at least 100 new psychiatry residency positions, grants for mental health peer support providers, and improvements to provider directories through the CAA – these are relatively small measures in the face of big access challenges. The lack of a diverse mental health care workforce may contribute to limited mental health treatment among people of color. Separately, even with insurance coverage, individuals with mental health needs face challenges accessing care. While Medicaid enrollees have limited out-of-pocket costs there is variation in who is eligible and the range of services covered across states . Additionally, the end of Medicaid’s continuous enrollment provision – on March 31, 2023 – could result in millions of disenrollments over the next year which could disrupt access to behavioral health services. Among private insurance enrollees, enrollees, with mental illness face high out-of-pocket costs; and these costs vary substantially across states . While most adults with mental illness have private insurance, rates of mental illness and substance use disorders are most prevalent among nonelderly adults with Medicaid.
Looking Ahead
Although steps have been taken to address negative mental health impacts stemming from the pandemic, mental health and substance use concerns remain elevated. Heightened racism and increasing gun violence may also contribute to poor mental health outcomes. Further, negative mental health impacts have been more pronounced among several populations, including communities of color, young adults and children – populations which have historically experienced increased barriers to care. Additionally, despite renewed discussions and new federal grants for state parity enforcement under the CAA, challenges with mental health parity persist – including lack of clarity on specific protections, low compliance rates, and slow federal enforcement. Finally, the COVID-19 public health emergency will end in May 2023, which may at least partially unravel steps taken toward delivering mental health services via telehealth and improving access to substance use disorder services.
History has shown that the mental health impact of disasters outlasts the physical impact, suggesting today’s elevated mental health needs will continue well beyond the coronavirus outbreak itself. As we emerge from the COVID-19 pandemic and the federal public health emergency draws to an end, it will be important to consider how the increased need for mental health and substance use services may persist long term, even as new cases and deaths due to COVID-19 hopefully subside.
This work was supported in part by Well Being Trust. KFF maintains full editorial control over all of its policy analysis, polling, and journalism activities.
The Household Pulse Survey (HPS) is a rapid response survey that has provided real-time data during the pandemic and includes a 4-item Patient Health Questionnaire (PHQ-4) anxiety and depression screening scale. In order to understand how the prevalence of anxiety and depression may have shifted in the adult population during the onset of the pandemic, mental health estimates from HPS were compared against pre-pandemic data from the National Health Interview Survey, which also includes the 4-item PHQ scale. However, recent research finds that these comparisons may not be reliable given lower response rates and over estimation in HPS; and are no longer included in this brief.
← Return to text
KFF analysis of Centers for Disease Control and Prevention, Wide-ranging Online Data for Epidemiologic Research (WONDER). Accessed at: https://wonder.cdc.gov/mcd-icd10-expanded.html
- Mental Health
- Coronavirus (COVID-19)
- Affordable Care Act
- Access to Care
- Adolescents
- Tracking Poll
- Race/Ethnicity
news release
- Latest Federal Data Show That Young People Are More Likely Than Older Adults to Be Experiencing Symptoms of Anxiety or Depression
Also of Interest
- Medicaid Coverage of Behavioral Health Services in 2022: Findings from a Survey of State Medicaid Programs
- Mental Health and Substance Use State Fact Sheets
- Mental Health and Substance Use Considerations Among Children During the COVID-19 Pandemic
- Mental Health Impact of the COVID-19 Pandemic: An Update
- Mental Illnesses May Soon Be the Most Common Pre-Existing Conditions
- State Data on Mental Health and Substance Abuse
- April 2022 Web Event: The Future of Mental Health Coverage & Access
- Medicaid Behavioral Health Services: Data Collection

Title: Supporting digital key workers: addressing the challenges faced by content moderators during and after the COVID-19 pandemic
Authors : Elena Martellozzo; Paul Bleakley; Paula Bradbury; Ruth Spence; Jeffrey DeMarco
Addresses : Department of Criminology and Sociology, Middlesex University, London, NW4 4BT, UK ' Henry C. Lee College of Criminal Justice and Forensic Sciences, University of New Haven, West Haven, 06516, USA ' Middlesex University, London, NW4 4BT, UK ' Middlesex University, London, NW4 4BT, UK ' Middlesex University, London, NW4 4BT, UK
Abstract : Content moderators (CMs) are private or state sector professionals responsible for inspecting user-generated content and applying policies to decide whether contentious content should remain online or be removed. CMs were required to review an unprecedented increase in illegal content during the COVID-19 pandemic. The existing evidence, although mostly anecdotal, suggests that frequent exposure to such content affects CM's well-being, mental health, and quality of life, as well as their work competence, satisfaction, and productivity. This study utilises (N = 9) in-depth qualitative interviews with CMs, which explored the impact of this work in the exceptional and challenging period of the COVID-19 pandemic. The aim of this paper is to critically explore what lessons can be learned from CM's experiences at work and how they coped with the difficulties created by COVID-19. This research will in turn assist organisations in identifying what is needed to improve conditions and mental well-being in the workplace.
Keywords : content moderators; social media; tech industry; labour conditions; digital first-responders; COVID-19; CSAM; lockdown; work-from-home; mental well-being.
DOI : 10.1504/IJTPM.2024.137818
International Journal of Technology, Policy and Management, 2024 Vol.24 No.2, pp.212 - 228
Received: 11 Apr 2023 Accepted: 06 Jul 2023 Published online: 05 Apr 2024 *
Keep up-to-date
- Our Newsletter ( subscribe for free )
- New issue alerts
- Inderscience is a member of publishing organisations including:
Read our research on: Gun Policy | International Conflict | Election 2024
Regions & Countries
What public k-12 teachers want americans to know about teaching.
Illustrations by Hokyoung Kim

At a time when most teachers are feeling stressed and overwhelmed in their jobs, we asked 2,531 public K-12 teachers this open-ended question:
If there’s one thing you’d want the public to know about teachers, what would it be?
We also asked Americans what they think about teachers to compare with teachers’ perceptions of how the public views them.
Related: What’s It Like To Be a Teacher in America Today?
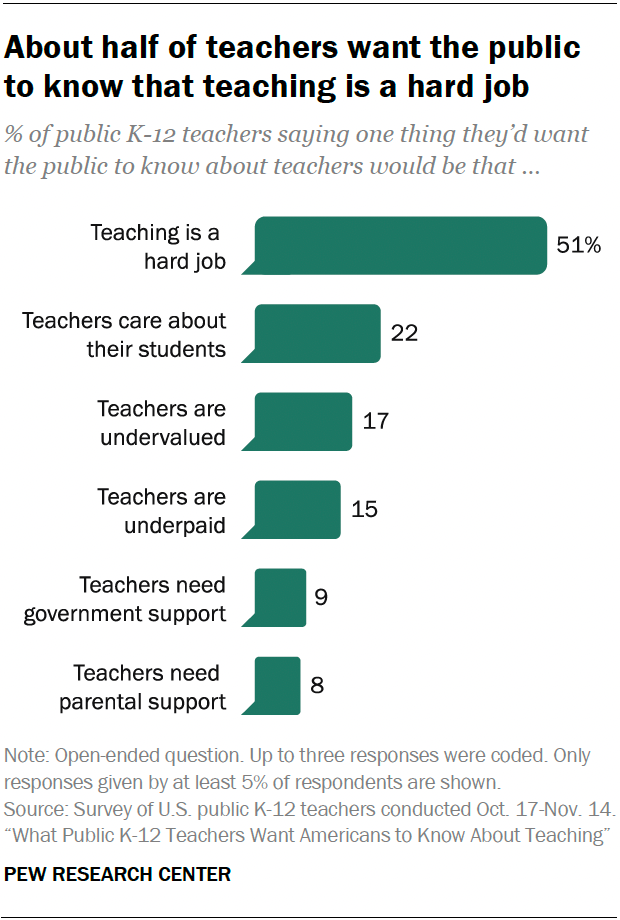
Pew Research Center conducted this analysis to better understand what public K-12 teachers would like Americans to know about their profession. We also wanted to learn how the public thinks about teachers.
For the open-end question, we surveyed 2,531 U.S. public K-12 teachers from Oct. 17 to Nov. 14, 2023. The teachers surveyed are members of RAND’s American Teacher Panel, a nationally representative panel of public K-12 school teachers recruited through MDR Education. Survey data is weighted to state and national teacher characteristics to account for differences in sampling and response to ensure they are representative of the target population.
Overall, 96% of surveyed teachers provided an answer to the open-ended question. Center researchers developed a coding scheme categorizing the responses, coded all responses, and then grouped them into the six themes explored in the data essay.
For the questions for the general public, we surveyed 5,029 U.S. adults from Nov. 9 to Nov. 16, 2023. The adults surveyed are members of the Ipsos KnowledgePanel, a nationally representative online survey panel. Panel members are randomly recruited through probability-based sampling, and households are provided with access to the Internet and hardware if needed. To ensure that the results of this survey reflect a balanced cross section of the nation, the data is weighted to match the U.S. adult population by gender, age, education, race and ethnicity and other categories.
Here are the questions used for this analysis , along with responses, the teacher survey methodology and the general public survey methodology .
Most of the responses to the open-ended question fell into one of these six themes:
Teaching is a hard job
About half of teachers (51%) said they want the public to know that teaching is a difficult job and that teachers are hardworking. Within this share, many mentioned that they have roles and responsibilities in the classroom besides teaching, which makes the job stressful. Many also talked about working long hours, beyond those they’re contracted for.
“Teachers serve multiple roles other than being responsible for teaching curriculum. We are counselors, behavioral specialists and parents for students who need us to fill those roles. We sacrifice a lot to give all of ourselves to the role as teacher.”
– Elementary school teacher
“The amount of extra hours that teachers have to put in beyond the contractual time is ridiculous. Arriving 30 minutes before and leaving an hour after is just the tip of the iceberg. … And as far as ‘having summers off,’ most of August is taken up with preparing materials for the upcoming school year or attending three, four, seven days’ worth of unpaid development training.”
– High school teacher
Teachers care about their students
The next most common theme: 22% of teachers brought up how fulfilling teaching is and how much teachers care about their students. Many gave examples of the hardships of teaching but reaffirmed that they do their job because they love the kids and helping them succeed.

“We are passionate about what we do. Every child we teach is important to us and we look out for them like they are our own.”
– Middle school teacher
“We are in it for the kids, and the most incredible moments are when children make connections with learning.”
Teachers are undervalued and disrespected
Some 17% of teachers want the public to know that they feel undervalued and disrespected, and that they need more public support. Some mentioned that they are well-educated professionals but are not treated as such. And many teachers in this category responded with a general plea for support from the public, which they don’t feel they’re getting now.
“We feel undervalued. The public and many parents of my students treat me and my peers as if we do not know as much as they do, as if we are uneducated.”
“The public attitudes toward teachers have been degrading, and it is making it impossible for well-qualified teachers to be found. People are simply not wanting to go into the profession because of public sentiments.”
Teachers are underpaid
A similar share of teachers (15%) want the public to know that teachers are underpaid. Many teachers said their salary doesn’t account for the effort and care they put into their students’ education and believe that their pay should reflect this.
“We are sorely underpaid for the amount of hours we work and the education level we have attained.”
Teachers need support and resources from government and administrators
About one-in-ten teachers (9%) said they need more support from the government, their administrators and other key stakeholders. Many mentioned working in understaffed schools, not having enough funding and paying for supplies out of pocket. Some teachers also expressed that they have little control over the curriculum that they teach.
“The world-class education we used to be proud of does not exist because of all the red tape we are constantly navigating. If you want to see real change in the classroom, advocate for smaller class sizes for your child, push your district to cap class sizes at a reasonable level and have real, authentic conversations with your child’s teacher about what is going on in the classroom if you’re curious.”
Teachers need more support from parents
Roughly the same share of teachers (8%) want the public to know that teachers need more support from parents, emphasizing that the parent-teacher relationship is strained. Many view parents as partners in their child’s education and believe that a strong relationship improves kids’ overall social and emotional development.

“Teachers help students to reach their potential. However, that job is near impossible if parents/guardians do not take an active part in their student’s education.”
How the U.S. public views teachers
While the top response from teachers in the open-ended question is that they want the public to know that teaching is a hard job, most Americans already see it that way. Two-thirds of U.S. adults say being a public K-12 teacher is harder than most other jobs, with 33% saying it’s a lot harder.
And about three-quarters of Americans (74%) say teachers should be paid more than they are now, including 39% who say teachers should be paid a lot more.
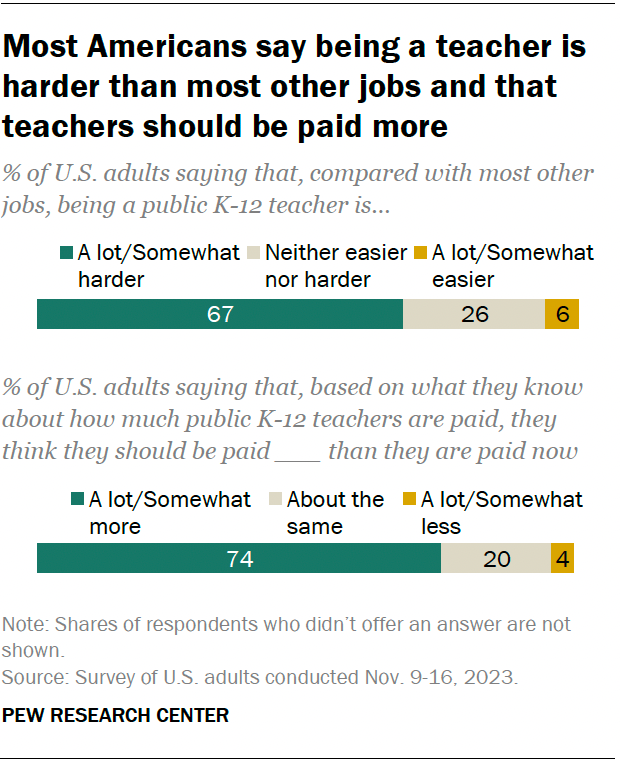
Americans are about evenly divided on whether the public generally looks up to (32%) or down on (30%) public K-12 teachers. Some 37% say Americans neither look up to or down on public K-12 teachers.
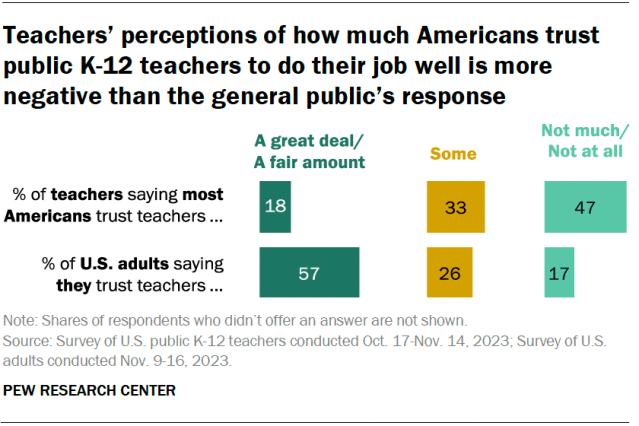
In addition to the open-ended question about what they want the public to know about them, we asked teachers how much they think most Americans trust public K-12 teachers to do their job well. We also asked the public how much they trust teachers. Answers differ considerably.
Nearly half of public K-12 teachers (47%) say most Americans don’t trust teachers much or at all. A third say most Americans trust teachers some, and 18% say the public trusts teachers a great deal or a fair amount.
In contrast, a majority of Americans (57%) say they do trust public K-12 teachers to do their job well a great deal or a fair amount. About a quarter (26%) say they trust teachers some, and 17% say they don’t trust teachers much or at all.
Related: About half of Americans say public K-12 education is going in the wrong direction
How the public’s views differ by party
There are sizable party differences in Americans’ views of teachers. In particular, Democrats and Democratic-leaning independents are more likely than Republicans and Republican leaners to say:
- They trust teachers to do their job well a great deal or a fair amount (70% vs. 44%)
- Teaching is a lot or somewhat harder when compared with most other jobs (77% vs. 59%)
- Teachers should be paid a lot or somewhat more than they are now (86% vs. 63%)
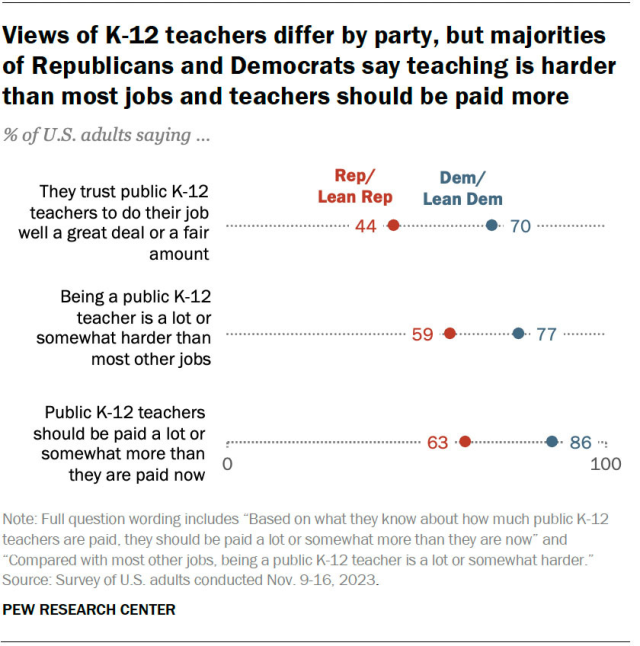
In their own words
Below, we have a selection of quotes that describe what teachers want the public to know about them and their profession.
Social Trends Monthly Newsletter
Sign up to to receive a monthly digest of the Center's latest research on the attitudes and behaviors of Americans in key realms of daily life
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Sports (Basel)
Physical Activity and Sports—Real Health Benefits: A Review with Insight into the Public Health of Sweden
Christer malm.
1 Sports Medicine Unit, Department of Community Medicine and Rehabilitation, Umeå University, 901 87 Umeå, Sweden; [email protected]
Johan Jakobsson
Andreas isaksson.
2 Department of Molecular Medicine and Surgery, Karolinska Institutet, 171 77 Solna, Sweden; [email protected]
Positive effects from sports are achieved primarily through physical activity, but secondary effects bring health benefits such as psychosocial and personal development and less alcohol consumption. Negative effects, such as the risk of failure, injuries, eating disorders, and burnout, are also apparent. Because physical activity is increasingly conducted in an organized manner, sport’s role in society has become increasingly important over the years, not only for the individual but also for public health. In this paper, we intend to describe sport’s physiological and psychosocial health benefits, stemming both from physical activity and from sport participation per se. This narrative review summarizes research and presents health-related data from Swedish authorities. It is discussed that our daily lives are becoming less physically active, while organized exercise and training increases. Average energy intake is increasing, creating an energy surplus, and thus, we are seeing an increasing number of people who are overweight, which is a strong contributor to health problems. Physical activity and exercise have significant positive effects in preventing or alleviating mental illness, including depressive symptoms and anxiety- or stress-related disease. In conclusion, sports can be evolving, if personal capacities, social situation, and biological and psychological maturation are taken into account. Evidence suggests a dose–response relationship such that being active, even to a modest level, is superior to being inactive or sedentary. Recommendations for healthy sports are summarized.
1. Introduction
Sport is a double-edged sword regarding effects on health. Positive effects are achieved primarily through physical activity, which is the main part of most sports. Many secondary effects of sport also bring health benefits, such as psychosocial development of both young [ 1 ] and old [ 2 ], personal development [ 3 ], later onset, and less consumption of alcohol [ 4 , 5 ]. Finally, those who play sports have a higher level of physical activity later in life [ 6 ], and through sport, knowledge of nutrition, exercise, and health can be developed [ 7 ]. Negative effects include the risk of failure leading to poor mental health [ 8 , 9 ], risk of injury [ 10 , 11 ], eating disorders [ 12 ], burnout [ 13 ], and exercise-induced gastrointestinal tract discomfort [ 14 ]. In sport, there are unfortunately also reports of physical and psychological abuse [ 15 ]. Negative aspects are more common in elite-level sports, where there is a fine balance between maximum performance and negative health. A somewhat unexpected effect of sport participation is that people submitting to planned training in some cases perform less physical activity compared to those who are exercising without a set schedule. One explanation can be a reduced spontaneous physical activity in the latter group [ 16 ]. Because physical activity is increasingly executed in an organized manner [ 17 , 18 , 19 ], sport’s role in society has become increasingly important over the years, not only for the individual but also for public health.
In this paper, we describe the health effects of sport from a physiological and psychological perspective, related both to physical activity and added values of sport per se. Initially, brief definitions of various concepts related to physical activity and health are given. This is then followed by: (1) A brief description of how physical activity and training affect our body from a physiological perspective; (2) a report on the health effects of physical activity and training; and (3) sport’s specific influences on the various dimensions of health. We chose to discuss the subject from an age-related perspective, separating children/adolescents, adults, and the elderly, as well as separating for sex in each age group.
2. Definitions of Physical Activity, Exercise, Training, Sport, and Health
Definitions and terms are based on “Physical activity in the prevention and treatment of disease” (FYSS, www.fyss.se [Swedish] [ 20 ]), World Health Organization (WHO) [ 21 ] and the US Department of Human Services [ 22 ]. The definition of physical activity in FYSS is: “Physical activity is defined purely physiologically, as all body movement that increases energy use beyond resting levels”. Health is defined according to the World Health Organization (WHO) as: “[…] a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity” [ 21 ].
Physical activity can occur spontaneously (leisure/work/transport) or organized and be divided according to purpose: Physical exercise is aimed primarily at improving health and physical capacity. Physical training is aimed primarily at increasing the individual’s maximum physical capacity and performance [ 23 ]. Physical inactivity is described as the absence of body movement, when energy consumption approximates resting levels. People who do not meet recommendations for physical activity are considered physically inactive and are sometimes called “sedentary”. Sport can be organized by age, sex, level of ambition, weight or other groupings [ 24 ]. Sport can also be spontaneous [ 7 , 17 ] and defined as a subset of exercises undertaken individually or as a part of a team, where participants have a defined goal [ 7 ]. General recommendations for physical activity are found in Table 1 , not considering everyday activities. One can meet the daily recommendations for physical activity by brief, high-intensity exercise, and remaining physically inactive for the rest of the day, thereby creating a “polarization” of physical activity: Having a high dose of conscious physical training, despite having a low energy expenditure in normal life due to high volumes of sedentary time. Polarization of physical activity may lead to increased risk of poor health despite meeting the recommendations for physical activity [ 25 , 26 , 27 ]. During most of our lives, energy expenditure is greater in normal daily life than in sport, physical training, and exercise, with the exceptions of children and the elderly, where planned physical activity is more important [ 28 ].
Recommendations regarding physical activity for different target groups. Note that additional health effects can be achieved if, in addition to these recommendations, the amount of physical activity increases, either by increasing the intensity or duration or a combination of both.
Compiled from FYSS 2017 ( www.fyss.se ) and WHO 2017 ( www.who.int ).
3. Aerobic and Muscle-Strengthening Physical Activity
Physical activity is categorized according to FYSS as: (1) Aerobic physical activity and (2) muscle-strengthening physical activity. Physical activity in everyday life and exercise training is mainly an aerobic activity, where a majority of energy production occurs via oxygen-dependent pathways. Aerobic physical activity is the type of activity typically associated with stamina, fitness, and the biggest health benefits [ 29 , 30 , 31 ]. Muscle-strengthening physical activity is referred to in everyday language as “strength training” or “resistance training” and is a form of physical exercise/training that is primarily intended to maintain or improve various forms of muscle strength and increase or maintain muscle mass [ 32 ]. Sometimes, another category is defined: Muscle-enhancing physical activity, important for maintenance or improvement of coordination and balance, especially in the elderly [ 33 ]. According to these definitions, muscle-strengthening activities primarily involve the body’s anaerobic (without oxygen) energy systems, proportionally more as intensity increases.
Exercise intensity can be expressed in absolute or relative terms. Absolute intensity means the physical work (for example; Watts [W], kg, or metabolic equivalent [MET]), while relative intensity is measured against the person’s maximum capacity or physiology (for example; percentage of maximum heart rate (%HR), rate of perceived exhaustion (RPE), W·kg −1 or relative oxygen uptake in L·min −1 ·kg −1 (VO 2 )). In terms of recommendations to the public, as in Table 1 , the intensity is often described in subjective terms (“makes you breathe harder” for moderate intensity, and “makes you puff and pant” for vigorous intensity) [ 27 ]. While objective criteria such as heart rate and accelerometry will capture the intensity of activity, they may not distinguish between different types of physical activity behaviors [ 34 ]. FYSS defines low intensity as 20%–39% of VO 2 max, <40 %HR, 1.5–2.9 METs; moderate intensity as 40%–59% of VO 2 max, 60–74 %HR, 3.0–5.9 METs, and vigorous intensity as 60%–89% of VO 2 max, 75–94 %HR, 6.0–8.9 METs. Absolute intensity, however, can vary greatly between individuals where a patient with heart disease may have a maximal capacity of <3 MET, and an elite athlete >20 MET [ 35 ].
4. How does the Body Adapt to Physical Activity and Training?
Adaption to physical activity and training is a complex physiological process, but may, in the context of this paper, be simplified by a fundamental basic principle:” The general adaptation syndrome (GAS)” [ 36 , 37 , 38 ]. This principle assumes that physical activity disturbs the body’s physiological balance, which the body then seeks to restore, all in a dose-related response relationship. The overload principle states that if exercise intensity is too low, overload is not reached to induce desired physiological adaptations, whereas an intensity too high will result in fatigue and possibly overtraining. Thus, for adaptation to occur, greater than normal stress must be induced, interspersed with sufficient recovery periods for restoration of physiological balance [ 39 ]. During and immediately after physical exercise/training, functions of affected tissues and systems are impaired, manifested as temporarily decreased performance. You feel tired. In order to gradually improve performance capacity, repeated cycles of adequate overload and recovery are required [ 40 ]. In practice, positive effects can be seen after a relatively short period of a few weeks, but more substantial improvements if the training is maintained for a longer period.
As a rule of thumb, it is assumed that all people can adapt to physical activity and exercise, but the degree of adaptation depends on many factors, including age, heredity, the environment, and diet [ 41 , 42 , 43 , 44 ]. The hereditary factor (genetics) may be the most critical for adaptation [ 45 ]. The degree of adaptation also depends on how the person in question trained previously; a well-trained athlete usually does not have the same relative improvement as an untrained one. Even if training is thought to be specific to mode, intensity, and duration, there are some overlaps. For example, it has been found that strength training in some individuals contributes to a relatively large positive impact on health and endurance, effects previously associated primarily with aerobic exercise [ 46 , 47 ]. The overload principle may, if applied too vigorously in relation to a person’s individual adaptation ability, have detrimental effects, including reduced performance, injury, overtraining, and disease [ 10 ]. Training is a commodity that must be renewed; otherwise, you gradually lose achieved performance improvements [ 48 ], although some capacities, such as muscle memory, seem to persist for life [ 49 ].
General recommendations for health may be stated, but individual predispositions make general training schedules for specific performance effects unpredictable. All exercise training should be adjusted to individual purposes, goals, and circumstances.
5. Health Effects of Physical Activity and Training
Human biology requires a certain amount of physical activity to maintain good health and wellbeing. Biological adaption to life with less physical activity would take many generations. People living today have, more or less, the same requirements for physical activity as 40,000 years ago [ 50 , 51 ]. For an average man with a body weight of 70 kg, this corresponds to about 19 km daily walking in addition to everyday physical activity [ 52 ]. For most people, daily physical activity decreases, while planned, conscious exercise and training increases [ 19 , 53 ]. Unfortunately, average daily energy intake is increasing more than daily energy output, creating an energy surplus. This is one reason for the increasing number of overweight people, and a strong contributor to many health problems [ 54 ]. More sedentary living (not reaching recommended level of physical activity), combined with increased energy intake, impairs both physical and mental capabilities and increases the risk of disease. Despite this, Swedes (as an example) seemed to be as physically active and stressed but had better general health in 2015, compared to 2004 ( Figure 1 ). Compared to 2004–2007, the Swedish population in 2012–2015 reported better overall health (more county-dots are blue) and less fatigue (smaller county-dots) with similar level of physical activity (~65% indicated at least 30 min daily physical activity) and stress (~13% were stressed).

Selected physical and mental health indicators of a Sweden cohort, in relation to the degree of physical activity for the period of years 2004–2007 ( N = 29,254) and years 2012–2015 ( N = 38,553). Surveyed subjects are age 16 to 84 years old, with data representing median scores of four years, not normalized for age. Y-axis: Percentage of subjects reporting “stressed”; X-axis: Percentage of subjects indicating physical active at least 30 minutes each day. Each dot represents one County (Län), dot-size indicates self-reported fatigue, and color self-reported healthiness of the County. If 70% of the population states they are having “Good/Very good” health, the dot is blue. If less than 70% states they are having good/very good health, the dot is red. The circle indicated with a black arrow corresponds to nation median. The black line connected to the nation circle represents the movement in the X–Y plane from the year 2004 to 2007, and from 2012 to 2015, respectively. Data retrieved from the Public Health Agency of Sweden 2019-04-22 ( www.folkhalsomyndigheten.se ).
Results in Figure 1 may in part be explained by a polarization of who is physically active: Some individuals are extremely active, others very inactive, giving a similar central tendency (mean/median). As physical activity and mental stress are not changed, but health is, the figure indicates that other factors must be more important to our overall health and fatigue. Recently, a national study of Swedish 11- to 15-year-olds concluded that this age group is inactive for most of their time awake, that is, sitting, standing or moving very little [ 55 ]. Time as inactive increased with age, from 67 percent for 11-year-olds to 75 percent for 15-year-olds. The study states that in all age groups, the inactive time is evenly distributed over the week, with school time, leisure time, and weekend. Further, those who feel school-related stress have more inactive time, both overall and during school hours, than those who have less school-related stress.
People active in sports have, in general, better health than those who do not participate in sports, because they are physically and mentally prepared for the challenges of sports, abilities that in many cases can be transferred to other parts of life [ 56 ].
However, there is a certain bias in this statement. Sport practitioners are already positively selected, because sickness and injury may prevent participation. As many health benefits of sport are related to the level of physical activity, separation of sport and physical exercise may be problematic. Regardless, societal benefits of these health effects can be seen in lower morbidity, healthier elderly, and lower medical costs [ 7 , 57 , 58 ].
Health effects of physical activity in many cases follow a dose–response relationship; dose of physical activity is in proportion to the effect on health [ 59 , 60 ]. Figure 2 depicts the relationship between risk of death and level of physical activity, in a Finnish twin cohort, adjusted for smoking, occupational group, and alcohol consumption [ 59 ]. Odds ratio (OR) for the risk of all-cause mortality in a larger sample in the same study was 0.80 for occasional exercisers ( p = 0.002, 95% CI = 0.69–0.91). This dose–response relationship between risk of all-cause mortality and physical activity is evident in several extensive studies [ 60 , 61 , 62 ]. The total dose is determined by the intensity (how strenuous), duration (duration), and frequency (how often). While Figure 2 shows sex differences in death rates, it is likely that sedentary behavior is equally hazardous for men and women, but inconsistent results sometime occur due to inadequate assessment measures, or low statistical power [ 59 , 63 ]. To obtain the best possible development due to physical exercise/training, both for prevention and treatment purposes, a basic understanding of how these variables affect the dose of activity is required, as well as understanding how they can be modified to suit individual requirements. A physically active population is important for the health of both the individual and society, with sport participation being one, increasingly important, motivator for exercise.

Relative risk (odds ratio; OR) of premature death in relationship to level of physical activity, in 286 male and 148 female twin pairs, adjusted for smoking, occupational group, and use of alcohol [ 59 ].
There is strong scientific evidence supporting an association between physical exercise/training and good physical and mental health. For example: A reduction in musculoskeletal disorders and reduced disability due to chronic disease [ 27 , 64 ], better mental health with reduced anxiety [ 65 , 66 ], insomnia [ 67 ], depression [ 31 ], stress [ 68 ], and other psychological disorders [ 69 ]. Physical and mental health problems are related to an increased risk of developing a number of our major public health diseases and may contribute to premature death ( Table 2 ).
Health-related physiological effects of aerobic and muscle strengthening physical activity. Green circle indicates that the activity contributes with an effect, whereas a red circle indicates that the activity has no proven effect. Orange circle indicates that the activity may in some cases be effective.
5.1. Effects on Physical Health
The effects of physical activity and exercise are both acute (during and immediately after) and long-lasting. Effects remaining after a long period of regular physical activity have far-reaching consequences for health and are described below. For example, some muscle enzymes’ activity can be quickly increased by physical exercise/training but just as quickly be lost when idle [ 118 ]. Other changes remain for months or years even if training ends—for instance, increased number and size of muscle fibers and blood vessels [ 49 , 119 , 120 ]. Good health, therefore, requires physical activity to be performed with both progression and continuity. Most of the conducted physical exercise/training is a combination of both aerobic and muscle strengthening exercise, and it can be difficult to distinguish between their health effects ( Table 2 ).
To describe ill-health, indicators of life expectancy, disease incidence (number), and prevalence (how often) are used [ 121 ]. In describing the relationship between physical activity and falling ill with certain diseases, the dose–response relationship, the effect size (the risk reduction that is shown in studies), and the recommended type and dose of physical activity are considered [ 122 ]. Table 3 shows the relative effects of regular physical activity ton the risk of various diseases (US Department of Human Services, 2009). The greatest health gains are for people who move from completely sedentary to moderately active lifestyles, with health effects seen before measurable improvements in physical performance. Previously, most scientific studies collected data only on aerobic physical activity. However, resistance exercise also shows promising health (mental and physical) and disease-prevention effects [ 123 , 124 , 125 , 126 , 127 ].
Disease prevention effects of regular physical activity.
Compiled from US Department of Health and Human Service, https://health.gov/paguidelines/report/ [ 62 , 146 ] 1 : Risk reduction refers to the relative risk in physically active samples in comparison to a non-active sample, i.e., a risk reduction of 20% means that the physically active sample has a relative risk of 0.8, compared to the non-active sample, which has 1.0. 2 : In general, general recommendations for PA that are described and referred to herein apply to most conditions. However, in some cases, more specific recommendations exist, more in depth described by the US Department of Health and Human Service, amongst others [ 62 ]. 3 : Evidence is dependent on cancer subtype; refer to US Department of Health and Human Service [ 62 ] for in-depth guidance. PA = Physical.
Aerobic physical activity has been shown to benefit weight maintenance after prior weight loss, reduce the risk of metabolic syndrome, normalize blood lipids, and help with cancer/cancer-related side effects ( Table 2 and Table 3 ), while effects on chronic pain are not as clear [ 29 ].
Muscle-strengthening physical activity has, in contrast to aerobic exercise, been shown to reduce muscle atrophy [ 128 ], risk of falling [ 75 ], and osteoporosis [ 74 ] in the elderly. Among the elderly, both men and women adapt positively to strength training [ 129 ]. Strength training also prevents obesity [ 130 ], enhances cognitive performance if done alongside aerobic exercise [ 131 ], counteracts the development of neurodegenerative diseases [ 132 , 133 , 134 ], reduces the risk of metabolic syndrome [ 135 ], counteracts cancer/cancer-related side effects [ 135 , 136 ], reduces pain and disability in joint diseases [ 137 ], and enhances bone density [ 137 , 138 ]. The risk of falling increases markedly with age and is partly a result of reduced muscle mass, and reduced coordination and balance [ 76 , 139 , 140 ]. A strong correlation between physical performance, reduced risk of falls, and enhanced quality of life is therefore, not surprisingly, found in older people [ 141 ]. Deterioration in muscle strength, but not muscle mass, increases the risk of premature death [ 142 ] but can be counteracted by exercise as a dose–response relationship describes the strength improvement in the elderly [ 122 , 143 ]. Recommendations state high-intensity strength training (6–8 repetitions at 80% of 1-repetition maximum) as most effective [ 144 ]. Muscle strengthening physical activity for better health is recommended as a complement to aerobic physical activity [ 29 ]. Amongst the elderly, vibration training can be an alternative to increase strength [ 145 ].
5.2. Effects on Mental Health
Mental illness is a global problem affecting millions of people worldwide [ 147 ]. Headache, stress, insomnia, fatigue, and anxiety are all measures of mental ill health. The term “ ill health ” constitutes a collection of several mental health problems and symptoms with various levels of seriousness. Studies have compared expected health benefits from regular physical activity for improvement of mental health with other treatments, for example, medication. Most recent studies show that physical activity and exercise used as a primary, or secondary, processing method have significant positive effects in preventing or alleviating depressive symptoms [ 31 , 148 , 149 , 150 , 151 ] and have an antidepressant effect in people with neurological diseases [ 152 ]. Training and exercise improve the quality of life and coping with stress and strengthen self-esteem and social skills [ 69 , 153 ]. Training and exercise also lessen anxiety in people who are diagnosed with an anxiety- or stress-related disease [ 68 ], improve vocabulary learning [ 154 ], memory [ 155 , 156 ], and creative thinking [ 157 ].
The same Swedish data as used in Figure 1 show that between the years 2004–2007 and 2012–2015 anxiety, worry, and insomnia decreased but were not obviously correlated to the slightly increased level of physical activity in the population during the same period. Thus, in a multifactorial context, the importance of physical exercise alone cannot be demonstrated in this dataset.
Some of the suggested physiological explanations for improved mental health with physical activity and exercise are greater perfusion and increased brain volume [ 107 , 158 ], increased volume of the hippocampus [ 106 ], and the anti-inflammatory effects of physical activity, reducing brain inflammation in neurological diseases [ 159 ]. Physical exercise may also mediate resilience to stress-induced depression via skeletal muscle peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α), enhancing kynurenine conversion to kynurenine acid, which in turn protects the brain and reduces the risk for stress-induced depression [ 153 ]. Further, increased release of growth factors, endorphins, and signaling molecules are other exercise-induced enhancers of mental health [ 69 ].
6. How Sport Affects Health
Sport’s main purposes are to promote physical activity and improve motor skills for health and performance and psychosocial development [ 56 ]. Participants also gain a chance to be part of a community, develop new social circles, and create social norms and attitudes. In healthy individuals, and patients with mental illness, sport participation has been shown to provide individuals with a sense of meaning, identity, and belonging [ 160 , 161 ]. Whether the sport movement exists or not, training and competition including physical activity will happen. Sport’s added values, in addition to the health benefits of physical activity, are therefore of interest. Some argue that it is doubtful, or at least not confirmed, that health development can come from sport, while others believe that healthy sport is something other than health, reviewed in depth by Coakley [ 162 ]. In a sporting context, health is defined as subjective (e.g., one feels good), biological (e.g., not being sick), functional (e.g., to perform), and social (e.g., to collaborate) [ 163 ]. Holt [ 56 ] argued that the environment for positive development in young people is distinctly different from an environment for performance, as the latter is based on being measured and assessed. That said, certain skills (goal setting, leadership, etc.) can be transferred from a sporting environment to other areas of life. The best way to transfer these abilities is, at the moment, unclear.
Having the goal to win at all costs can be detrimental to health. This is especially true for children and adolescents, as early engagement in elite sports increases the risk of injury, promotes one-dimensional functional development, leads to overtraining, creates distorted social norms, risks psychosocial disorders, and has the risk of physical and psychological abuse [ 15 , 164 ]. Of great importance, therefore, is sport’s goal of healthy performance development, starting at an early age. For older people, a strong motivating factor to conduct physical activity is sports club membership [ 165 ]. One can summarize these findings by stating sport’s utility at the transition between different stages of the life; from youth to adulthood and from adulthood to old age. There, sports can be a resource for good physical and mental health [ 166 ].
Today, a higher proportion of the population, compared to 50 years ago, is engaged in organized sports, and to a lesser extent performs spontaneous sports ( Figure 3 ), something that Engström showed in 2004 [ 17 ] and is confirmed by data from The Swedish Sports Confederation ( www.rf.se ). Of the surveyed individuals in 2001, 50%–60% of children and young people said they were active in a sports club. The trend has continued showing similar progression to 2011, with up to 70% of school students playing sports in a club. Furthermore, the study shows that those active in sport clubs also spontaneously do more sports [ 167 ]. Similar data from the years 2007–2018, compiled from open sources at The Swedish Sports Confederation, confirm the trend with an even higher share of youths participating in organized sports, compared to 1968 and 2001 ( Figure 4 ).

Spontaneous sport has decreased over the last decades, to the advantage of organized sport. Data compiled from Engström, 2004, The Swedish Research Council for Sport Science.

Data compiled from open sources report Sport Statistics (Idrotten i siffror) at The Swedish Sports Confederation for the year 2011 ( www.rf.se ).
Taking part in sports can be an important motivator for physical activity for older people [ 165 , 166 ]. With aging, both participation in sports ( Figure 4 ) and physical activity in everyday life [ 168 ] decreases. At the same time, the number of people who are physically active both in leisure and in organized sports increases (The Public Health Agency of Sweden 2017; www.folkhalsomyndigheten.se ). Consequently, among elderly people, a greater proportion of the physical activity occurs within the context of sport [ 8 , 28 ]. Together, research shows that organized sports, in clubs or companies, are more important for people’s overall physical activity than ever before. Groups that are usually less physically active can be motivated through sport—for example, elderly men in sport supporters’ clubs [ 169 ], people in rural areas [ 170 ], migrants [ 171 ], and people with alternative physical and mental functions [ 172 ]. No matter how you get your sporting interest, it is important to establish a physical foundation at an early age to live in good health when you get older ( Figure 5 ). As seen in Figure 5 , a greater sport habitus at age 15 results in higher physical activity at 53 years of age. Early training and exposure to various forms of sports are therefore of great importance. Participation creates an identity, setting the stage for a high degree of physical activity later in life [ 173 ].

Odds ratio (OR) of physical activity at age 53 in relation to Sport habitus at age 15. Sport habitus (“the total physical capital"), including cultural capital, athletic diversity, and grades in physical education and health are, according to Engström [ 173 ], the factors most important for being physically active in later life. For a further discussion on sport habitus, the readers are referred to Engström, 2008 [ 173 ]. Numbers above bar show the 95% confidence interval. ** = significant difference from “Very low”, p < 0.01. *** = p < 0.001.
7. Sport’s Effects on the Health of Children and Young People
The effects of participation in organized sports for children and young people are directly linked to physical activity, with long term secondary effects; an active lifestyle at a young age fosters a more active lifestyle as an adult. As many diseases that are positively affected by physical activity/exercise appear later in life, continued participation in sport as an adult will reduce morbidity and mortality.
It must be emphasized that good physical and mental health of children and young people participating in sport requires knowledge and organization based on everyone’s participation. Early specialization counteracts, in all regards, both health and performance development [ 174 , 175 ].
7.1. Positive Aspects
According to several reviews, there is a correlation between high daily physical activity in children and a low risk for obesity, improved development of motor and cognitive skills, as well as a stronger skeleton [ 176 , 177 ]. Positive effects on lipidemia, blood pressure, oxygen consumption, body composition, metabolic syndrome, bone density and depression, increased muscle strength, and reduced damage to the skeleton and muscles are also described [ 178 , 179 ]. If many aspects are merged in a multidimensional analysis [ 8 , 173 ], the factors important for future good health are shown to be training in sports, broad exposure to different sports, high school grades, cultural capital, and that one takes part in sport throughout childhood ( Table 4 ).
Compiled health profiles for men and women at the age of 20 years, depending on participation in organized sports at the age of 5, 7, 8, 10, 14, and 17 years.
Classification with repeated latent class analysis creates three groups for girls and boys, respectively: Children who never participated (girls only), participated, quit prematurely, or began late (only boys) in sports. Arrows indicate whether participation in sports at young age has an effect on health at 20 years of age. Green up arrow is positive, red down arrow negative, and a horizontal black double arrow shows that sport had no significant effect. Modified from Howie et. al., 2016 [ 8 ].
Psychological benefits of sports participation of young people were compiled by Eime et al. [ 1 ], where the conclusion was that sporting children have better self-esteem, less depression, and better overall psychosocial health. One problem with most of these studies, though, is that they are cross-sectional studies, which means that no cause–effect relationship can be determined. As there is a bias for participating children towards coming from socially secure environments, the results may be somewhat skewed.
7.2. Negative Aspects
As Table 4 and Table 5 show, there are both positive and negative aspects of sports. Within children’s and youth sports, early specialization to a specific sport is a common phenomenon [ 175 ]. There is no scientific evidence that early specialization would have positive impact, neither for health nor for performance later in life [ 175 ]. No model or method including performance at a young age can predict elite performance as an adult. By contrast, specialization and competitiveness can lead to injury, overtraining, increased psychological stress, and reduced training motivation, just to mention a few amongst many negative aspects [ 174 , 175 ]. Another important aspect is that those who are excluded from sports feel mentally worse [ 8 ]. As there is a relationship between depressive episodes in adolescence, and depression as adults [ 116 ], early exclusion has far-reaching consequences. Therefore, sports for children and young people have future health benefits by reducing the risk of developing depression and depressive symptoms, as well as improved wellbeing throughout life.
Positive and negative aspects with sport (at young age).
While some degree of sport specialization is necessary to develop elite-level athletes, research shows clear adverse health effects of early specialization and talent selection [ 180 ]. More children born during the fall and winter (September–December) are excluded [ 181 ], and as a group, they are less physically active than spring (January–April) children, both in sports and leisure ( Figure 6 ). In most sports and in most countries, there is a skewed distribution of participants when sorted by birth-date, and there are more spring children than fall children among those who are involved in sport [ 182 , 183 , 184 , 185 , 186 ]. Because a large part of the physical activity takes place in an organized form, this leads to lower levels of physical activity for late-born persons (Malm, Jakobsson, and Julin, unpublished data). Early orientation and training in physical activity and exercise will determine how active you are later in life. Greater attention must be given to stimulating as many children and young people as possible to participate in sport as long as possible, both in school and on their leisure time. According to statistics from the Swedish Sports Confederation in 2016, this relative-age effect persists throughout life, despite more starting than ending with sport each year [ 18 ].

The figure shows the distribution of 7597 children aged 10 years and younger who in 2014 were registered as active in one particular, individual sport in Sweden (data compiled from the Swedish Sport Confederation, www.rf.se ). Spring, Summer, and Fall represent January–April, May–August, and September–December, respectively.
When summarize, the positive and negative aspects of sport at a young age can be divided into three categories: (1) Personal identification, (2) social competence, and (3) physiological capacity, briefly summarized in Table 5 . A comprehensive analysis of what is now popularly known as “physical literacy” has recently been published [ 187 ].
7.3. Relevance of Sports
Sports can make children and young people develop both physically and mentally and contribute with health benefits if planned and executed exercise/training considers the person’s own capacities, social situation, and biological as well as psychological maturation. In children and adolescents, it is especially important to prevent sports-related injuries and health problems, as a number of these problems are likely to remain long into adulthood, sometimes for life. Comprehensive training is recommended, which does not necessarily mean that you have to participate in various sports. What is required is diverse training within every sport and club. Research shows that participation in various sports simultaneously during childhood and adolescence is most favorable for healthy and lifelong participation [ 8 , 173 , 188 , 189 ].
8. Sport’s Effects on the Health of Adults and the Elderly
Adults who stop participating in sports reduce their physical activity and have health risks equal to people who have neither done sports nor been physical [ 190 , 191 ]. Lack of adherence to exercise programs is a significant hindrance in achieving health goals and general physical activity recommendations in adults and the elderly [ 192 ]. While several socioeconomic factors are related to exercise adherence, it is imperative that trainers and health care providers are informed about factors that can be modulated, such as intervention intensity (not to high), duration (not too long), and supervision, important for higher adherence, addressed more in depth by Rivera-Torres, Fahey and Rivera [ 192 ].
Healthy aging is dependent on many factors, such as the absence of disease, good physical and mental health, and social commitment (especially through team sports or group activities) [ 193 ]. Increased morbidity with age may be partly linked to decreased physical activity. Thus, remaining or becoming active later in life is strongly associated with healthy aging [ 194 ]. With increased age, there is less involvement in training and competition ( Figure 4 ), and only 20% of adults in Sweden are active, at least to some extent, in sports clubs, and the largest proportion of adults who exercise do it on their own. The following sections describes effects beyond what is already provided for children and youths.
8.1. Positive Aspects
Participation in sports, with or without competition, promotes healthy behavior and a better quality of life [ 166 ]. Exclusion from sports at a young age appears to have long-term consequences, as the previously described relative age effect ( Figure 6 ) remains even for master athletes (Malm, Jakobsson, and Julin, unpublished data). Because master athletes show better health than their peers [ 95 ], actions should be taken to include adults and elderly individuals who earlier in life were excluded from, or never started with sport [ 195 ]. As we age, physical activity at a health-enhancing intensity is not enough to maintain all functions. Higher intensity is required, best comprising competition-oriented training [ 196 , 197 ]. One should not assume that high-intensity exercise cannot be initiated by the elderly [ 198 ]. Competitive sports, or training like a competitive athlete as an adult, can be one important factor to counter the loss of physical ability with aging [ 199 ]. In this context, golf can be one example of a safe form of exercise with high adherence for older adults and the elderly, resulting in increased aerobic performance, metabolic function, and trunk strength [ 200 , 201 ].
8.2. Negative Aspects
Increased morbidity (e.g., cardiovascular disease) with aging is seen also among older athletes [ 202 ] and is associated with the same risk factors as in the general population [ 203 ]. An increased risk of cardiovascular disease among adults (master) compared to other populations has been found [ 204 ]. Unfortunately, the designs and interpretations of these studies have been criticized, and the incidence of cardiac arrest in older athletes is unclear [ 205 ]. In this context, the difference between competitive sports aiming to optimize performance and recreational sports has to be taken into account, where the former is more likely to induce negative effects due to high training loads and/or impacts during training and games. Although high-intensity training even for older athletes is positive for aerobic performance, it does not prevent the loss of motor units [ 206 ].
Quality of life is higher in sporting adults compared to those who do not play sports, but so is the risk of injury. When hit by injury, adults and young alike may suffer from psychological disorders such as depression [ 207 ], but with a longer recovery time in older individuals [ 208 ]. As with young athletes, secession of training at age 50 years and above reduces blood flow in the brain, including the hippocampus, possibly related to long-term decline in mental capacity [ 209 ].
8.3. Relevance of Sport
As for children and young people, many positive health aspects come through sport also for adults and the elderly [ 210 ]. Sport builds bridges between generations, a potential but not elucidated drive for adults’ motivation for physical activity. The percentage of adults participating in competitive sports has increased in Sweden since 2010, from about 20 percent to 30 percent of all of those who are physically active [ 18 ], a trend that most likely provides better health for the group in the 30–40 age group and generations to come.
9. Recommendations for Healthy Sport
- 1. Plan exercise, rest, and social life. For health-promoting and healthy-aging physical activity, refer to general guidelines summarized in this paper: Aerobic exercise three times a week, muscle-strengthening exercise 2–3 times a week.
- 2. Set long-term goals.
- 3. Adopt a holistic performance development including physiological, medical, mental, and psychosocial aspects.
- ○ a. Exercise load (time, intensity, volume);
- ○ b. Recovery (sleep, resting heart rate, appetite, estimated fatigue, etc.);
- ○ c. Sickness (when–where–how, type of infections, how long one is ill, etc.);
- ○ d. Repeat type- and age-specific physical tests with relevant evaluation and feedback;
- ○ e. Frequency of injuries and causes.
- ○ a. Motivation for training, competition, and socializing;
- ○ b. Personal perception of stress, anxiety, depression, alienation, and self-belief;
- ○ c. Repeat type- and age-specific psychological tests with relevant evaluation and feedback.
- 6. Register and interpret signs of overtraining, such as reduced performance over time, while maintaining or increasing exercise load.
Author Contributions
C.M. and A.J. conceived and designed the review. C.M., A.J., J.J. and interpreted the data and drafted the manuscript. J.J. edited the manuscript, tables, and figures. All authors approved the final version.
This work was supported by the Swedish Sports Confederation.
Conflicts of Interest
The authors declare no conflict of interest.

IMAGES
VIDEO
COMMENTS
Background Recent trends on measurement of well-being have elevated the scientific standards and rigor associated with approaches for national and international comparisons of well-being. One major theme in this has been the shift toward multidimensional approaches over reliance on traditional metrics such as single measures (e.g. happiness, life satisfaction) or economic proxies (e.g. GDP ...
Implementation of Healthy People 2030 will by strengthened by engaging users from many sectors and ensuring the effective use and alignment of resources. Promoting the nation's health and well-being is a shared responsibility—at the national, state, territorial, tribal, and community levels. It requires involving the public, private, and not ...
Introduction. The existing definitions of happiness, subjective well-being, and health related quality of life and the main components assigned to these constructs in the research literature (see Table 1) suggest conceptual overlap between these dimensions (Camfield & Skevington, 2008).Quality of life was defined in the cross-cultural project of the World Health Organization (WHO) as:
PDF | On May 23, 2021, Gerard Bodeker and others published Well-Being and Mental Wellness Well-Being and Mental Wellness | Find, read and cite all the research you need on ResearchGate
Abstract. It is known that the concept of wellbeing is closely related to health and to the quality of life. Thus, the wellbeing exists within two dimensions, a subjective one and an objective one ...
Introduction. Although the influence of work on occupational health and safety has been long recognized (), importance of work for well-being has been gaining scientific attention only recently (2-6).The impact of employee health on work has been traditionally examined through the lenses of physical and mental disabilities that limit chances for performing certain jobs (7-9).
The purpose of this paper is to present an expanded conceptual model, grounded in the conditions of work, ... health and wellbeing: Future research will need to move beyond traditional occupational health outcomes of reducing work-related injuries and illnesses and towards examining ways work determines and shapes positive health and wellbeing ...
1. Introduction. Mental health is broadly described as a state of well-being where an individual recognizes their capabilities to cope with normal stresses of life, work effectively and contribute to the society (WHO, 2001).It is a significant issue for employees, workplaces, and societies and the fifth most significant cause of disability in the Organization for Economic Cooperation and ...
Maintaining wellbeing in university students is a government priority, but robust evidence has been lacking. Higher wellbeing is associated with better mental and physical health, higher self-esteem, self-efficacy, and effective coping strategies. This study aimed to identify, through an online survey in 2018, key determinants of wellbeing amongst a sample of 574 (65.5% female) students across ...
The paper first critically reviews the theoretical approaches and challenges for operationalizing the concept of wellbeing in both research and policy. We then present a framework of the spaces of ...
On well-being research and TWB. An early contribution regarding the importance of well-being was provided by the World Health Organization (WHO). By 1946, the WHO had already defined health as a state of complete physical, mental, and social well-being, as opposed to the mere absence of disease or infirmity.
The field's scope has broadened with time to include the concept of worker well-being, or the ability of people to address normal stresses, work productively, and achieve their highest potential. 5, 6. Well-being is closely linked with health and productivity. Research shows that employees who are in good physical, mental, and emotional ...
Background Medical students face challenges to their mental wellbeing and have a high prevalence of mental health problems. During training, they are expected to develop strategies for dealing with stress. This study investigated factors medical students perceived as draining and replenishing during COVID-19, using the 'coping reservoir' model of wellbeing. Methods In synchronous ...
The World Health Organization defines mental well-being as an individual's ability to develop their potential, work productively and creatively, build strong and positive relationships with others and contribute to their community. 1 This view distinguishes subjective happiness or life satisfaction (hedonic well-being) from positive psychological functioning (eudaimonic well-being).
Modern wellbeing research has largely been undertaken within the field of psychology with a Western focus and many subjective measures of wellbeing. ... The example of well-being indicators in the WHO "Health 2020 ... (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine, 41 (10), 1403-1409. 10.1016/0277 ...
INTRODUCTION. Sleep is vital for health and well-being in children, adolescents, and adults. 1-3 Healthy sleep is important for cognitive functioning, mood, mental health, and cardiovascular, cerebrovascular, and metabolic health. 4 Adequate quantity and quality of sleep also play a role in reducing the risk of accidents and injuries caused by sleepiness and fatigue, including workplace ...
There has been a recent interest in how architecture affects mental health and psychological well-being, motivated by the fact that we spend the majority of our waking time inside and interacting with built environments. Some studies have investigated the psychological responses to indoor design parameters; for instance, contours, and proposed that curved interiors, when compared to angular ...
The research must also have assessed the impact of CR and/or SC on mental health and wellbeing, resilience, and recovery during and following public health emergencies and infectious disease outbreaks which affect communities (to ensure the research is relevant to the review aims), have conducted primary research, and have a full text available ...
The differences between wellbeing components and determinants and the terms used interchangeably with wellbeing, such as health, are considered from the perspective of a doctor. The philosophies underpinning wellbeing and modern wellbeing research theories are discussed in terms of their appropriateness in an inclusive definition.
Recently, the United-Nations adopted 17 sustainable development goals for the 2030 Agenda. The Sustainable Development Goal (SDG) 3 "Ensuring a healthy life and promoting well-being for all ages ...
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help. Worldwide ...
Research suggests that substance use among adolescents has declined, yet drug overdose deaths have sharply increased among this population, primarily due to fentanyl-laced substances.Among ...
Abstract. In addition to the apparent physical health benefits, physical activity also affects mental health positively. Physically inactive individuals have been reported to have higher rates of morbidity and healthcare expenditures. Commonly, exercise therapy is recommended to combat these challenges and preserve mental wellness.
41%. Percentage of teens with the highest social media use who rate their overall mental health as poor or very poor, compared with 23% of those with the lowest use. For example, 10% of the highest use group expressed suicidal intent or self-harm in the past 12 months compared with 5% of the lowest use group, and 17% of the highest users expressed poor body image compared with 6% of the lowest ...
A working paper from University of Pennsylvania and Columbia University researchers identifies key themes in the challenges learners at two-year institutions face and how it impacts their enrollment and degree progression in the first year. Community college students make up 41 percent of undergraduates and, among students who completed a degree in 2015-16, 49 percent have enrolled at a ...
The aim of this paper is to critically explore what lessons can be learned from CM's experiences at work and how they coped with the difficulties created by COVID-19. This research will in turn assist organisations in identifying what is needed to improve conditions and mental well-being in the workplace.
3. To us this is consistent with considerations of wellbeing, co mpri sing five factors: 1) security, 2) the basic materials for a good life, 3) health, 4) good social relations and 5) freedom of ...
Pew Research Center conducted this analysis to better understand what public K-12 teachers would like Americans to know about their profession. ... and then grouped them into the six themes explored in the data essay. For the questions for the general public, we surveyed 5,029 U.S. adults from Nov. 9 to Nov. 16, 2023. ... get to know them and ...
2. Definitions of Physical Activity, Exercise, Training, Sport, and Health. Definitions and terms are based on "Physical activity in the prevention and treatment of disease" (FYSS, www.fyss.se [Swedish] []), World Health Organization (WHO) [] and the US Department of Human Services [].The definition of physical activity in FYSS is: "Physical activity is defined purely physiologically, as ...