- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Preparation and Procedures Involved in Gender Affirmation Surgeries
If you or a loved one are considering gender affirmation surgery , you are probably wondering what steps you must go through before the surgery can be done. Let's look at what is required to be a candidate for these surgeries, the potential positive effects and side effects of hormonal therapy, and the types of surgeries that are available.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender.
A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery.
The term "transexual" was previously used by the medical community to describe people who undergo gender affirmation surgery. The term is no longer accepted by many members of the trans community as it is often weaponized as a slur. While some trans people do identify as "transexual", it is best to use the term "transgender" to describe members of this community.
Transitioning
Transitioning may involve:
- Social transitioning : going by different pronouns, changing one’s style, adopting a new name, etc., to affirm one’s gender
- Medical transitioning : taking hormones and/or surgically removing or modifying genitals and reproductive organs
Transgender individuals do not need to undergo medical intervention to have valid identities.
Reasons for Undergoing Surgery
Many transgender people experience a marked incongruence between their gender and their assigned sex at birth. The American Psychiatric Association (APA) has identified this as gender dysphoria.
Gender dysphoria is the distress some trans people feel when their appearance does not reflect their gender. Dysphoria can be the cause of poor mental health or trigger mental illness in transgender people.
For these individuals, social transitioning, hormone therapy, and gender confirmation surgery permit their outside appearance to match their true gender.
Steps Required Before Surgery
In addition to a comprehensive understanding of the procedures, hormones, and other risks involved in gender-affirming surgery, there are other steps that must be accomplished before surgery is performed. These steps are one way the medical community and insurance companies limit access to gender affirmative procedures.
Steps may include:
- Mental health evaluation : A mental health evaluation is required to look for any mental health concerns that could influence an individual’s mental state, and to assess a person’s readiness to undergo the physical and emotional stresses of the transition.
- Clear and consistent documentation of gender dysphoria
- A "real life" test : The individual must take on the role of their gender in everyday activities, both socially and professionally (known as “real-life experience” or “real-life test”).
Firstly, not all transgender experience physical body dysphoria. The “real life” test is also very dangerous to execute, as trans people have to make themselves vulnerable in public to be considered for affirmative procedures. When a trans person does not pass (easily identified as their gender), they can be clocked (found out to be transgender), putting them at risk for violence and discrimination.
Requiring trans people to conduct a “real-life” test despite the ongoing violence out transgender people face is extremely dangerous, especially because some transgender people only want surgery to lower their risk of experiencing transphobic violence.
Hormone Therapy & Transitioning
Hormone therapy involves taking progesterone, estrogen, or testosterone. An individual has to have undergone hormone therapy for a year before having gender affirmation surgery.
The purpose of hormone therapy is to change the physical appearance to reflect gender identity.
Effects of Testosterone
When a trans person begins taking testosterone , changes include both a reduction in assigned female sexual characteristics and an increase in assigned male sexual characteristics.
Bodily changes can include:
- Beard and mustache growth
- Deepening of the voice
- Enlargement of the clitoris
- Increased growth of body hair
- Increased muscle mass and strength
- Increase in the number of red blood cells
- Redistribution of fat from the breasts, hips, and thighs to the abdominal area
- Development of acne, similar to male puberty
- Baldness or localized hair loss, especially at the temples and crown of the head
- Atrophy of the uterus and ovaries, resulting in an inability to have children
Behavioral changes include:
- Aggression
- Increased sex drive
Effects of Estrogen
When a trans person begins taking estrogen , changes include both a reduction in assigned male sexual characteristics and an increase in assigned female characteristics.
Changes to the body can include:
- Breast development
- Loss of erection
- Shrinkage of testicles
- Decreased acne
- Decreased facial and body hair
- Decreased muscle mass and strength
- Softer and smoother skin
- Slowing of balding
- Redistribution of fat from abdomen to the hips, thighs, and buttocks
- Decreased sex drive
- Mood swings
When Are the Hormonal Therapy Effects Noticed?
The feminizing effects of estrogen and the masculinizing effects of testosterone may appear after the first couple of doses, although it may be several years before a person is satisfied with their transition. This is especially true for breast development.
Timeline of Surgical Process
Surgery is delayed until at least one year after the start of hormone therapy and at least two years after a mental health evaluation. Once the surgical procedures begin, the amount of time until completion is variable depending on the number of procedures desired, recovery time, and more.
Transfeminine Surgeries
Transfeminine is an umbrella term inclusive of trans women and non-binary trans people who were assigned male at birth.
Most often, surgeries involved in gender affirmation surgery are broken down into those that occur above the belt (top surgery) and those below the belt (bottom surgery). Not everyone undergoes all of these surgeries, but procedures that may be considered for transfeminine individuals are listed below.
Top surgery includes:
- Breast augmentation
- Facial feminization
- Nose surgery: Rhinoplasty may be done to narrow the nose and refine the tip.
- Eyebrows: A brow lift may be done to feminize the curvature and position of the eyebrows.
- Jaw surgery: The jaw bone may be shaved down.
- Chin reduction: Chin reduction may be performed to soften the chin's angles.
- Cheekbones: Cheekbones may be enhanced, often via collagen injections as well as other plastic surgery techniques.
- Lips: A lip lift may be done.
- Alteration to hairline
- Male pattern hair removal
- Reduction of Adam’s apple
- Voice change surgery
Bottom surgery includes:
- Removal of the penis (penectomy) and scrotum (orchiectomy)
- Creation of a vagina and labia
Transmasculine Surgeries
Transmasculine is an umbrella term inclusive of trans men and non-binary trans people who were assigned female at birth.
Surgery for this group involves top surgery and bottom surgery as well.
Top surgery includes :
- Subcutaneous mastectomy/breast reduction surgery.
- Removal of the uterus and ovaries
- Creation of a penis and scrotum either through metoidioplasty and/or phalloplasty
Complications and Side Effects
Surgery is not without potential risks and complications. Estrogen therapy has been associated with an elevated risk of blood clots ( deep vein thrombosis and pulmonary emboli ) for transfeminine people. There is also the potential of increased risk of breast cancer (even without hormones, breast cancer may develop).
Testosterone use in transmasculine people has been associated with an increase in blood pressure, insulin resistance, and lipid abnormalities, though it's not certain exactly what role these changes play in the development of heart disease.
With surgery, there are surgical risks such as bleeding and infection, as well as side effects of anesthesia . Those who are considering these treatments should have a careful discussion with their doctor about potential risks related to hormone therapy as well as the surgeries.
Cost of Gender Confirmation Surgery
Surgery can be prohibitively expensive for many transgender individuals. Costs including counseling, hormones, electrolysis, and operations can amount to well over $100,000. Transfeminine procedures tend to be more expensive than transmasculine ones. Health insurance sometimes covers a portion of the expenses.
Quality of Life After Surgery
Quality of life appears to improve after gender-affirming surgery for all trans people who medically transition. One 2017 study found that surgical satisfaction ranged from 94% to 100%.
Since there are many steps and sometimes uncomfortable surgeries involved, this number supports the benefits of surgery for those who feel it is their best choice.
A Word From Verywell
Gender affirmation surgery is a lengthy process that begins with counseling and a mental health evaluation to determine if a person can be diagnosed with gender dysphoria.
After this is complete, hormonal treatment is begun with testosterone for transmasculine individuals and estrogen for transfeminine people. Some of the physical and behavioral changes associated with hormonal treatment are listed above.
After hormone therapy has been continued for at least one year, a number of surgical procedures may be considered. These are broken down into "top" procedures and "bottom" procedures.
Surgery is costly, but precise estimates are difficult due to many variables. Finding a surgeon who focuses solely on gender confirmation surgery and has performed many of these procedures is a plus. Speaking to a surgeon's past patients can be a helpful way to gain insight on the physician's practices as well.
For those who follow through with these preparation steps, hormone treatment, and surgeries, studies show quality of life appears to improve. Many people who undergo these procedures express satisfaction with their results.
Bizic MR, Jeftovic M, Pusica S, et al. Gender dysphoria: Bioethical aspects of medical treatment . Biomed Res Int . 2018;2018:9652305. doi:10.1155/2018/9652305
American Psychiatric Association. What is gender dysphoria? . 2016.
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender-nonconforming people . 2012.
Tomlins L. Prescribing for transgender patients . Aust Prescr . 2019;42(1): 10–13. doi:10.18773/austprescr.2019.003
T'sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine . Endocr Rev . 2019;40(1):97-117. doi:10.1210/er.2018-00011
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877-884. doi:10.21037/tau.2016.09.04
Seal LJ. A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria . Ann Clin Biochem . 2016;53(Pt 1):10-20. doi:10.1177/0004563215587763
Schechter LS. Gender confirmation surgery: An update for the primary care provider . Transgend Health . 2016;1(1):32-40. doi:10.1089/trgh.2015.0006
Altman K. Facial feminization surgery: current state of the art . Int J Oral Maxillofac Surg . 2012;41(8):885-94. doi:10.1016/j.ijom.2012.04.024
Therattil PJ, Hazim NY, Cohen WA, Keith JD. Esthetic reduction of the thyroid cartilage: A systematic review of chondrolaryngoplasty . JPRAS Open. 2019;22:27-32. doi:10.1016/j.jpra.2019.07.002
Top H, Balta S. Transsexual mastectomy: Selection of appropriate technique according to breast characteristics . Balkan Med J . 2017;34(2):147-155. doi:10.4274/balkanmedj.2016.0093
Chan W, Drummond A, Kelly M. Deep vein thrombosis in a transgender woman . CMAJ . 2017;189(13):E502-E504. doi:10.1503/cmaj.160408
Streed CG, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: A narrative review . Ann Intern Med . 2017;167(4):256-267. doi:10.7326/M17-0577
Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: A review of guidelines and literature . Fed Pract . 2018;35(7):30-37.
Van de grift TC, Elaut E, Cerwenka SC, Cohen-kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming aurgery: A follow-up atudy . J Sex Marital Ther . 2018;44(2):138-148. doi:10.1080/0092623X.2017.1326190
American Society of Plastic Surgeons. Gender confirmation surgeries .
American Psychological Association. Transgender people, gender identity, and gender expression .
Colebunders B, Brondeel S, D'Arpa S, Hoebeke P, Monstrey S. An update on the surgical treatment for transgender patients . Sex Med Rev . 2017 Jan;5(1):103-109. doi:10.1016/j.sxmr.2016.08.001
- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
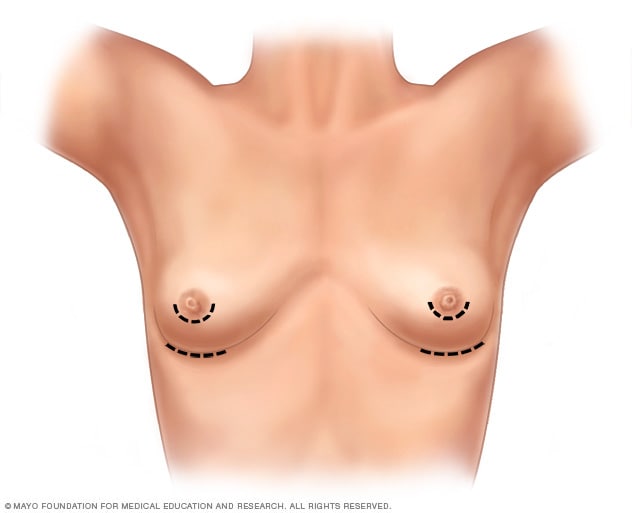
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
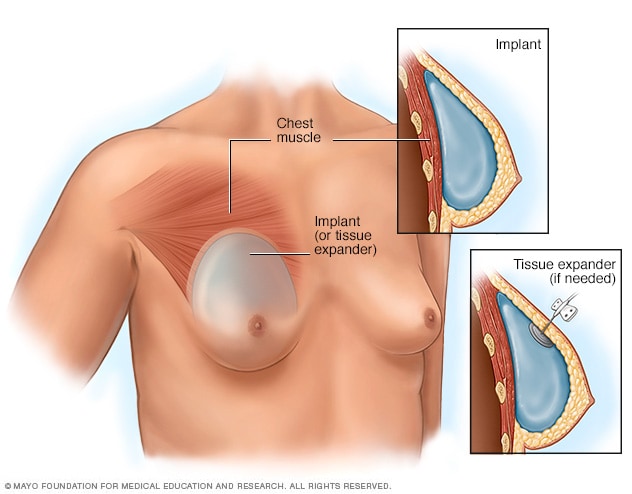
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
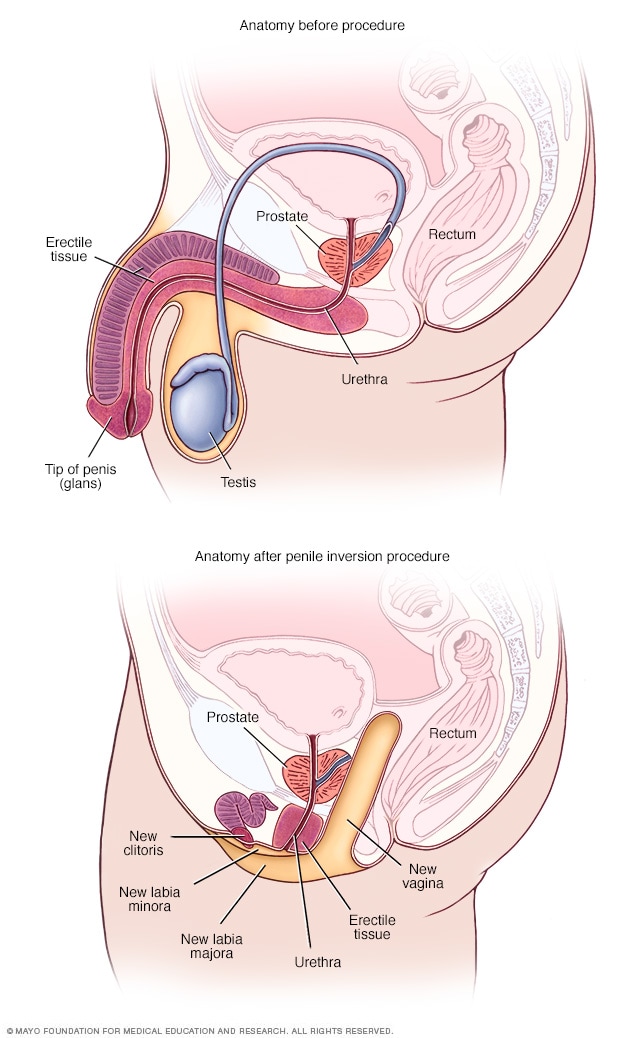
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
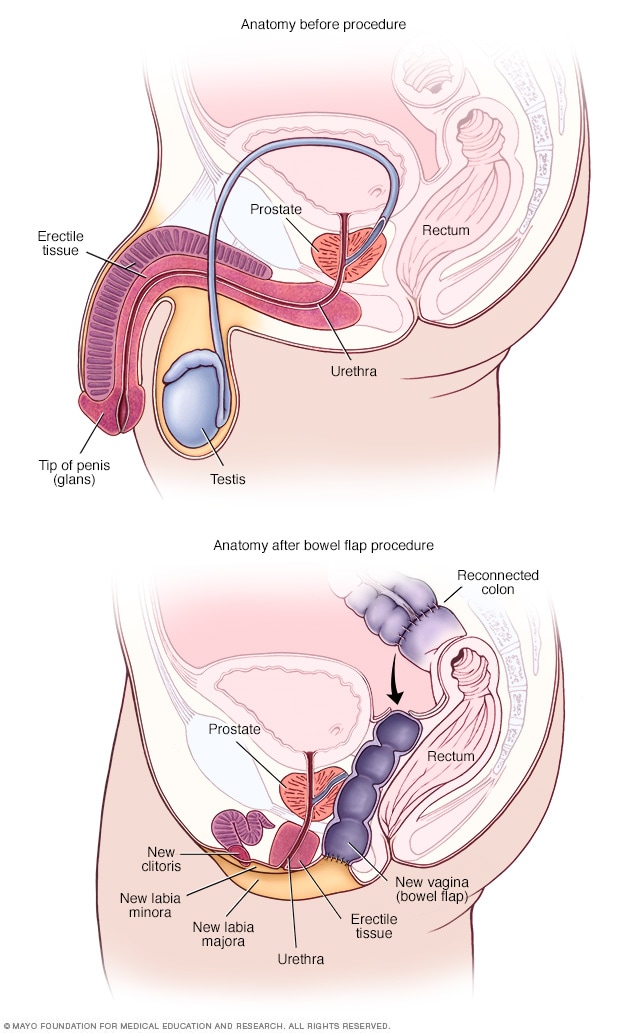
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Search the site GO Please fill out this field.
- Newsletters
- Mental Health
- Social and Public Health
What Is Gender Affirmation Surgery?
:max_bytes(150000):strip_icc():format(webp)/KP-Headshot-IMG_1661-0d48c6ea46f14ab19a91e7b121b49f59.jpg)
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary, to change one or more of their sex characteristics. This type of procedure offers a person the opportunity to have features that align with their gender identity.
For example, this type of surgery may be a transgender surgery like a male-to-female or female-to-male surgery. Read on to learn more about what masculinizing, feminizing, and gender-nullification surgeries may involve, including potential risks and complications.
Why Is Gender Affirmation Surgery Performed?
A person may have gender affirmation surgery for different reasons. They may choose to have the surgery so their physical features and functional ability align more closely with their gender identity.
For example, one study found that 48,019 people underwent gender affirmation surgeries between 2016 and 2020. Most procedures were breast- and chest-related, while the remaining procedures concerned genital reconstruction or facial and cosmetic procedures.
In some cases, surgery may be medically necessary to treat dysphoria. Dysphoria refers to the distress that transgender people may experience when their gender identity doesn't match their sex assigned at birth. One study found that people with gender dysphoria who had gender affirmation surgeries experienced:
- Decreased antidepressant use
- Decreased anxiety, depression, and suicidal ideation
- Decreased alcohol and drug abuse
However, these surgeries are only performed if appropriate for a person's case. The appropriateness comes about as a result of consultations with mental health professionals and healthcare providers.
Transgender vs Nonbinary
Transgender and nonbinary people can get gender affirmation surgeries. However, there are some key ways that these gender identities differ.
Transgender is a term that refers to people who have gender identities that aren't the same as their assigned sex at birth. Identifying as nonbinary means that a person doesn't identify only as a man or a woman. A nonbinary individual may consider themselves to be:
- Both a man and a woman
- Neither a man nor a woman
- An identity between or beyond a man or a woman
Hormone Therapy
Gender-affirming hormone therapy uses sex hormones and hormone blockers to help align the person's physical appearance with their gender identity. For example, some people may take masculinizing hormones.
"They start growing hair, their voice deepens, they get more muscle mass," Heidi Wittenberg, MD , medical director of the Gender Institute at Saint Francis Memorial Hospital in San Francisco and director of MoZaic Care Inc., which specializes in gender-related genital, urinary, and pelvic surgeries, told Health .
Types of hormone therapy include:
- Masculinizing hormone therapy uses testosterone. This helps to suppress the menstrual cycle, grow facial and body hair, increase muscle mass, and promote other male secondary sex characteristics.
- Feminizing hormone therapy includes estrogens and testosterone blockers. These medications promote breast growth, slow the growth of body and facial hair, increase body fat, shrink the testicles, and decrease erectile function.
- Non-binary hormone therapy is typically tailored to the individual and may include female or male sex hormones and/or hormone blockers.
It can include oral or topical medications, injections, a patch you wear on your skin, or a drug implant. The therapy is also typically recommended before gender affirmation surgery unless hormone therapy is medically contraindicated or not desired by the individual.
Masculinizing Surgeries
Masculinizing surgeries can include top surgery, bottom surgery, or both. Common trans male surgeries include:
- Chest masculinization (breast tissue removal and areola and nipple repositioning/reshaping)
- Hysterectomy (uterus removal)
- Metoidioplasty (lengthening the clitoris and possibly extending the urethra)
- Oophorectomy (ovary removal)
- Phalloplasty (surgery to create a penis)
- Scrotoplasty (surgery to create a scrotum)
Top Surgery
Chest masculinization surgery, or top surgery, often involves removing breast tissue and reshaping the areola and nipple. There are two main types of chest masculinization surgeries:
- Double-incision approach : Used to remove moderate to large amounts of breast tissue, this surgery involves two horizontal incisions below the breast to remove breast tissue and accentuate the contours of pectoral muscles. The nipples and areolas are removed and, in many cases, resized, reshaped, and replaced.
- Short scar top surgery : For people with smaller breasts and firm skin, the procedure involves a small incision along the lower half of the areola to remove breast tissue. The nipple and areola may be resized before closing the incision.
Metoidioplasty
Some trans men elect to do metoidioplasty, also called a meta, which involves lengthening the clitoris to create a small penis. Both a penis and a clitoris are made of the same type of tissue and experience similar sensations.
Before metoidioplasty, testosterone therapy may be used to enlarge the clitoris. The procedure can be completed in one surgery, which may also include:
- Constructing a glans (head) to look more like a penis
- Extending the urethra (the tube urine passes through), which allows the person to urinate while standing
- Creating a scrotum (scrotoplasty) from labia majora tissue
Phalloplasty
Other trans men opt for phalloplasty to give them a phallic structure (penis) with sensation. Phalloplasty typically requires several procedures but results in a larger penis than metoidioplasty.
The first and most challenging step is to harvest tissue from another part of the body, often the forearm or back, along with an artery and vein or two, to create the phallus, Nicholas Kim, MD, assistant professor in the division of plastic and reconstructive surgery in the department of surgery at the University of Minnesota Medical School in Minneapolis, told Health .
Those structures are reconnected under an operative microscope using very fine sutures—"thinner than our hair," said Dr. Kim. That surgery alone can take six to eight hours, he added.
In a separate operation, called urethral reconstruction, the surgeons connect the urinary system to the new structure so that urine can pass through it, said Dr. Kim. Urethral reconstruction, however, has a high rate of complications, which include fistulas or strictures.
According to Dr. Kim, some trans men prefer to skip that step, especially if standing to urinate is not a priority. People who want to have penetrative sex will also need prosthesis implant surgery.
Hysterectomy and Oophorectomy
Masculinizing surgery often includes the removal of the uterus (hysterectomy) and ovaries (oophorectomy). People may want a hysterectomy to address their dysphoria, said Dr. Wittenberg, and it may be necessary if their gender-affirming surgery involves removing the vagina.
Many also opt for an oophorectomy to remove the ovaries, almond-shaped organs on either side of the uterus that contain eggs and produce female sex hormones. In this case, oocytes (eggs) can be extracted and stored for a future surrogate pregnancy, if desired. However, this is a highly personal decision, and some trans men choose to keep their uterus to preserve fertility.
Feminizing Surgeries
Surgeries are often used to feminize facial features, enhance breast size and shape, reduce the size of an Adam’s apple , and reconstruct genitals. Feminizing surgeries can include:
- Breast augmentation
- Facial feminization surgery
- Penis removal (penectomy)
- Scrotum removal (scrotectomy)
- Testicle removal (orchiectomy)
- Tracheal shave (chondrolaryngoplasty) to reduce an Adam's apple
- Vaginoplasty
- Voice feminization
Breast Augmentation
Top surgery, also known as breast augmentation or breast mammoplasty, is often used to increase breast size for a more feminine appearance. The procedure can involve placing breast implants, tissue expanders, or fat from other parts of the body under the chest tissue.
Breast augmentation can significantly improve gender dysphoria. Studies show most people who undergo top surgery are happier, more satisfied with their chest, and would undergo the surgery again.
Most surgeons recommend 12 months of feminizing hormone therapy before breast augmentation. Since hormone therapy itself can lead to breast tissue development, transgender women may or may not decide to have surgical breast augmentation.
Facial Feminization and Adam's Apple Removal
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers, botox, fat grafting, and liposuction may also be used to create a more feminine appearance.
Some trans women opt for chondrolaryngoplasty, also known as a tracheal shave. The procedure reduces the size of the Adam's apple, an area of cartilage around the larynx (voice box) that tends to be larger in people assigned male at birth.
Vulvoplasty and Vaginoplasty
As for bottom surgery, there are various feminizing procedures from which to choose. Vulvoplasty (to create external genitalia without a vagina) or vaginoplasty (to create a vulva and vaginal canal) are two of the most common procedures.
Dr. Wittenberg noted that people might undergo six to 12 months of electrolysis or laser hair removal before surgery to remove pubic hair from the skin that will be used for the vaginal lining.
Surgeons have different techniques for creating a vaginal canal. A common one is a penile inversion, where the masculine structures are emptied and inverted into a created cavity, explained Dr. Kim. Vaginoplasty may be done in one or two stages, said Dr. Wittenberg, and the initial recovery is three months—but it will be a full year until people see results.
Surgical removal of the penis or penectomy is sometimes used in feminization treatment. This can be performed along with an orchiectomy and scrotectomy.
However, a total penectomy is not commonly used in feminizing surgeries . Instead, many people opt for penile-inversion surgery, a technique that hollows out the penis and repurposes the tissue to create a vagina during vaginoplasty.
Orchiectomy and Scrotectomy
An orchiectomy is a surgery to remove the testicles —male reproductive organs that produce sperm. Scrotectomy is surgery to remove the scrotum, that sac just below the penis that holds the testicles.
However, some people opt to retain the scrotum. Scrotum skin can be used in vulvoplasty or vaginoplasty, surgeries to construct a vulva or vagina.
Other Surgical Options
Some gender non-conforming people opt for other types of surgeries. This can include:
- Gender nullification procedures
- Penile preservation vaginoplasty
- Vaginal preservation phalloplasty
Gender Nullification
People who are agender or asexual may opt for gender nullification, sometimes called nullo. This involves the removal of all sex organs. The external genitalia is removed, leaving an opening for urine to pass and creating a smooth transition from the abdomen to the groin.
Depending on the person's sex assigned at birth, nullification surgeries can include:
- Breast tissue removal
- Nipple and areola augmentation or removal
Penile Preservation Vaginoplasty
Some gender non-conforming people assigned male at birth want a vagina but also want to preserve their penis, said Dr. Wittenberg. Often, that involves taking skin from the lining of the abdomen to create a vagina with full depth.
Vaginal Preservation Phalloplasty
Alternatively, a patient assigned female at birth can undergo phalloplasty (surgery to create a penis) and retain the vaginal opening. Known as vaginal preservation phalloplasty, it is often used as a way to resolve gender dysphoria while retaining fertility.
The recovery time for a gender affirmation surgery will depend on the type of surgery performed. For example, healing for facial surgeries may last for weeks, while transmasculine bottom surgery healing may take months.
Your recovery process may also include additional treatments or therapies. Mental health support and pelvic floor physiotherapy are a few options that may be needed or desired during recovery.
Risks and Complications
The risk and complications of gender affirmation surgeries will vary depending on which surgeries you have. Common risks across procedures could include:
- Anesthesia risks
- Hematoma, which is bad bruising
- Poor incision healing
Complications from these procedures may be:
- Acute kidney injury
- Blood transfusion
- Deep vein thrombosis, which is blood clot formation
- Pulmonary embolism, blood vessel blockage for vessels going to the lung
- Rectovaginal fistula, which is a connection between two body parts—in this case, the rectum and vagina
- Surgical site infection
- Urethral stricture or stenosis, which is when the urethra narrows
- Urinary tract infection (UTI)
- Wound disruption
What To Consider
It's important to note that an individual does not need surgery to transition. If the person has surgery, it is usually only one part of the transition process.
There's also psychotherapy . People may find it helpful to work through the negative mental health effects of dysphoria. Typically, people seeking gender affirmation surgery must be evaluated by a qualified mental health professional to obtain a referral.
Some people may find that living in their preferred gender is all that's needed to ease their dysphoria. Doing so for one full year prior is a prerequisite for many surgeries.
All in all, the entire transition process—living as your identified gender, obtaining mental health referrals, getting insurance approvals, taking hormones, going through hair removal, and having various surgeries—can take years, healthcare providers explained.
A Quick Review
Whether you're in the process of transitioning or supporting someone who is, it's important to be informed about gender affirmation surgeries. Gender affirmation procedures often involve multiple surgeries, which can be masculinizing, feminizing, or gender-nullifying in nature.
It is a highly personalized process that looks different for each person and can often take several months or years. The procedures also vary regarding risks and complications, so consultations with healthcare providers and mental health professionals are essential before having these procedures.
American Society of Plastic Surgeons. Gender affirmation surgeries .
Wright JD, Chen L, Suzuki Y, Matsuo K, Hershman DL. National estimates of gender-affirming surgery in the US . JAMA Netw Open . 2023;6(8):e2330348-e2330348. doi:10.1001/jamanetworkopen.2023.30348
Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8 . Int J Transgend Health . 2022;23(S1):S1-S260. doi:10.1080/26895269.2022.2100644
Chou J, Kilmer LH, Campbell CA, DeGeorge BR, Stranix JY. Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria . Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX.0000944280.62632.8c
Human Rights Campaign. Get the facts on gender-affirming care .
Human Rights Campaign. Transgender and non-binary people FAQ .
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877–84. doi:10.21037/tau.2016.09.04
Richards JE, Hawley RS. Chapter 8: Sex Determination: How Genes Determine a Developmental Choice . In: Richards JE, Hawley RS, eds. The Human Genome . 3rd ed. Academic Press; 2011: 273-298.
Randolph JF Jr. Gender-affirming hormone therapy for transgender females . Clin Obstet Gynecol . 2018;61(4):705-721. doi:10.1097/GRF.0000000000000396
Cocchetti C, Ristori J, Romani A, Maggi M, Fisher AD. Hormonal treatment strategies tailored to non-binary transgender individuals . J Clin Med . 2020;9(6):1609. doi:10.3390/jcm9061609
Van Boerum MS, Salibian AA, Bluebond-Langner R, Agarwal C. Chest and facial surgery for the transgender patient . Transl Androl Urol . 2019;8(3):219-227. doi:10.21037/tau.2019.06.18
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):248–53. doi:10.21037/tau.2019.06.12
Bordas N, Stojanovic B, Bizic M, Szanto A, Djordjevic ML. Metoidioplasty: surgical options and outcomes in 813 cases . Front Endocrinol . 2021;12:760284. doi:10.3389/fendo.2021.760284
Al-Tamimi M, Pigot GL, van der Sluis WB, et al. The surgical techniques and outcomes of secondary phalloplasty after metoidioplasty in transgender men: an international, multi-center case series . The Journal of Sexual Medicine . 2019;16(11):1849-1859. doi:10.1016/j.jsxm.2019.07.027
Waterschoot M, Hoebeke P, Verla W, et al. Urethral complications after metoidioplasty for genital gender affirming surgery . J Sex Med . 2021;18(7):1271–9. doi:10.1016/j.jsxm.2020.06.023
Nikolavsky D, Hughes M, Zhao LC. Urologic complications after phalloplasty or metoidioplasty . Clin Plast Surg . 2018;45(3):425–35. doi:10.1016/j.cps.2018.03.013
Nota NM, den Heijer M, Gooren LJ. Evaluation and treatment of gender-dysphoric/gender incongruent adults . In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext . MDText.com, Inc.; 2000.
Carbonnel M, Karpel L, Cordier B, Pirtea P, Ayoubi JM. The uterus in transgender men . Fertil Steril . 2021;116(4):931–5. doi:10.1016/j.fertnstert.2021.07.005
Miller TJ, Wilson SC, Massie JP, Morrison SD, Satterwhite T. Breast augmentation in male-to-female transgender patients: Technical considerations and outcomes . JPRAS Open . 2019;21:63-74. doi:10.1016/j.jpra.2019.03.003
Claes KEY, D'Arpa S, Monstrey SJ. Chest surgery for transgender and gender nonconforming individuals . Clin Plast Surg . 2018;45(3):369–80. doi:10.1016/j.cps.2018.03.010
De Boulle K, Furuyama N, Heydenrych I, et al. Considerations for the use of minimally invasive aesthetic procedures for facial remodeling in transgender individuals . Clin Cosmet Investig Dermatol . 2021;14:513-525. doi:10.2147/CCID.S304032
Asokan A, Sudheendran MK. Gender affirming body contouring and physical transformation in transgender individuals . Indian J Plast Surg . 2022;55(2):179-187. doi:10.1055/s-0042-1749099
Sturm A, Chaiet SR. Chondrolaryngoplasty-thyroid cartilage reduction . Facial Plast Surg Clin North Am . 2019;27(2):267–72. doi:10.1016/j.fsc.2019.01.005
Chen ML, Reyblat P, Poh MM, Chi AC. Overview of surgical techniques in gender-affirming genital surgery . Transl Androl Urol . 2019;8(3):191-208. doi:10.21037/tau.2019.06.19
Wangjiraniran B, Selvaggi G, Chokrungvaranont P, Jindarak S, Khobunsongserm S, Tiewtranon P. Male-to-female vaginoplasty: Preecha's surgical technique . J Plast Surg Hand Surg . 2015;49(3):153-9. doi:10.3109/2000656X.2014.967253
Okoye E, Saikali SW. Orchiectomy . In: StatPearls [Internet] . Treasure Island (FL): StatPearls Publishing; 2022.
Salgado CJ, Yu K, Lalama MJ. Vaginal and reproductive organ preservation in trans men undergoing gender-affirming phalloplasty: technical considerations . J Surg Case Rep . 2021;2021(12):rjab553. doi:10.1093/jscr/rjab553
American Society of Plastic Surgeons. What should I expect during my recovery after facial feminization surgery?
American Society of Plastic Surgeons. What should I expect during my recovery after transmasculine bottom surgery?
de Brouwer IJ, Elaut E, Becker-Hebly I, et al. Aftercare needs following gender-affirming surgeries: findings from the ENIGI multicenter European follow-up study . The Journal of Sexual Medicine . 2021;18(11):1921-1932. doi:10.1016/j.jsxm.2021.08.005
American Society of Plastic Surgeons. What are the risks of transfeminine bottom surgery?
American Society of Plastic Surgeons. What are the risks of transmasculine top surgery?
Khusid E, Sturgis MR, Dorafshar AH, et al. Association between mental health conditions and postoperative complications after gender-affirming surgery . JAMA Surg . 2022;157(12):1159-1162. doi:10.1001/jamasurg.2022.3917
Related Articles
Jump to content
Updated visitor policies
Other michigan medicine sites.
- About Michigan Medicine
- UofMHealth.org
- Medical School
- Find a Clinical Trial

Michigan Medicine
Federated search page form block, quick links.
- Patient Portal Login
- For Health Providers
- Maps & Directions
Gender Confirmation Surgery
The University of Michigan Health System offers procedures for surgical gender transition. Working together, the surgical team of the Comprehensive Gender Services Program, which includes specialists in plastic surgery, urology and gynecology, bring expertise, experience and safety to procedures for our transgender patients.
Access to gender-related surgical procedures for patients is made through the University of Michigan Health System Comprehensive Gender Services Program .
The Comprehensive Gender Services Program adheres to the WPATH Standards of Care , including the requirement for a second-opinion prior to genital sex reassignment.
Available surgeries:
Male-to-Female: Tracheal Shave Breast Augmentation Facial Feminization Male-to-Female genital sex reassignment
Female-to-Male: Hysterectomy, oophorectomy, vaginectomy Chest Reconstruction Female-to-male genital sex reassignment
Sex Reassignment Surgeries (SRS)
At the University of Michigan Health System, we are dedicated to offering the safest proven surgical options for sex reassignment (SRS.) Because sex reassignment surgery is just one step for transitioning people, the Comprehensive Gender Services Program has access to providers for mental health services, hormone therapy, pelvic floor physiotherapy, and speech therapy. Surgical procedures are done by a team that includes, as appropriate, gynecologists, urologists, pelvic pain specialists and a reconstructive plastic surgeon. A multi-disciplinary team helps to best protect the health of the patient.
For patients receiving mental health and medical services within the University of Michigan Health System, the UMHS-CGSP will coordinate all care including surgical referrals. For patients who have prepared for surgery elsewhere, the UMHS-CGSP will help organize the needed records, meet WPATH standards, and coordinate surgical referrals. Surgical referrals are made through Sara Wiener the Comprehensive Gender Services Program Director.
Male-to-female sex reassignment surgery
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a male-to-female sex reassignment surgery will be offered a penile inversion vaginoplasty with a neurovascular neoclitoris.
During this procedure, a surgeon makes “like become like,” using parts of the original penis to create a sensate neo-vagina. The testicles are removed, a procedure called orchiectomy. The skin from the scrotum is used to make the labia. The erectile tissue of the penis is used to make the neoclitoris. The urethra is preserved and functional.
This procedure provides for aesthetic and functional female genitalia in one 4-5 hour operation. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation. What to Expect: Vaginoplasty at Michigan Medicine .
Female-to-male sex reassignment
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a female-to-male sex reassignment surgery will be offered a phalloplasty, generally using the radial forearm flap method.
This procedure, which can be done at the same time as a hysterectomy/vaginectomy, creates an aesthetically appropriate phallus and creates a urethera for standing urination. Construction of a scrotum with testicular implants is done as a second stage. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation.
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected] . W e will assist you in obtaining what you need to qualify for surgery.
How Gender Reassignment Surgery Works (Infographic)
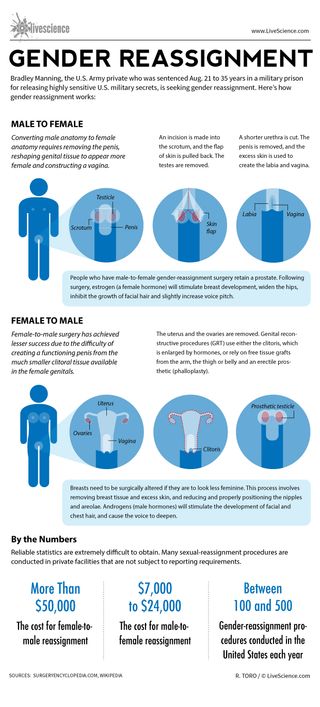
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Man's years of premature ejaculation had a rare cause
Viagra alternatives? Study of mouse erections hints at new ways to treat erectile dysfunction
Pet fox with 'deep relationship with the hunter-gatherer society' buried 1,500 years ago in Argentina
Most Popular
By Anna Gora December 27, 2023
By Anna Gora December 26, 2023
By Anna Gora December 25, 2023
By Emily Cooke December 23, 2023
By Victoria Atkinson December 22, 2023
By Anna Gora December 16, 2023
By Anna Gora December 15, 2023
By Anna Gora November 09, 2023
By Donavyn Coffey November 06, 2023
By Anna Gora October 31, 2023
By Anna Gora October 26, 2023
- 2 How and where to watch the April 8 solar eclipse online for free
- 3 NASA engineers discover why Voyager 1 is sending a stream of gibberish from outside our solar system
- 4 Giant coyote killed in southern Michigan turns out to be a gray wolf — despite the species vanishing from region 100 years ago
- 5 When is the next total solar eclipse after 2024 in North America?
- 2 Giant 'toe biter' water bugs discovered in Cyprus for the 1st time
- 3 Watch live! The total solar eclipse has begun over North America.
- 4 8,200-year-old campsite of 'Paleo-Archaic' peoples discovered on US Air Force base in New Mexico
- Follow us on Facebook
- Follow us on Twitter
- Criminal Justice
- Environment
- Politics & Government
- Race & Gender
Expert Commentary
What the research says about hormones and surgery for transgender youth
Researchers and physicians point to a growing body of peer-reviewed academic scholarship in support of gender-affirming medical treatment for transgender youth.

Republish this article

This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License .
by Chloe Reichel, The Journalist's Resource August 7, 2019
This <a target="_blank" href="https://journalistsresource.org/politics-and-government/gender-confirmation-surgery-transgender-youth-research/">article</a> first appeared on <a target="_blank" href="https://journalistsresource.org">The Journalist's Resource</a> and is republished here under a Creative Commons license.<img src="https://journalistsresource.org/wp-content/uploads/2020/11/cropped-jr-favicon-150x150.png" style="width:1em;height:1em;margin-left:10px;">
In the interest of examining this important news topic through a research lens, Journalist’s Resource collaborated on this story with The Burlington Free Press, where it first appeared . This piece is part of the newspaper’s series of stories about transgender youth in the state.
As Vermont regulators consider changes to Medicaid that would expand access to gender confirmation surgery for transgender youth, researchers and physicians point to a growing body of peer-reviewed academic scholarship in support of the new proposal.
Among other changes, the proposed rules would eliminate the requirement that transgender individuals on Medicaid must wait until the age of 21 to receive surgery. Individuals over the age of 18 and minors — with informed parental consent — would be eligible.
Such changes are in line with current thinking among academics and physicians in the field. It’s still a fledgling field, as Marci Bowers, a California-based gynecologist and surgeon who specializes in gender confirmation and serves as a professorial lecturer at the Icahn School of Medicine at Mount Sinai points out.
“Kids are coming out very young. A generation ago, they were driven into the closet,” Bowers said. “It’s only these last 20 years or so where instead of that happening, people are getting professional help.”
How common are gender confirmation surgeries in the U.S.?
Estimates suggest that in the U.S., between 2000 and 2014, 10.9% of inpatient visits for transgender people involved gender confirmation surgery. This figure comes from an analysis of inpatient visits for a nationally representative sample that includes, but is not limited to, transgender patients, which was published in 2018 in the medical journal JAMA Surgery . Over the study period, the number of patients who sought gender confirmation surgery increased annually.
Further, the percentage of gender confirmation surgeries that are “genital surgeries” — commonly referred to as bottom surgeries — has increased over time. Between 2000 and 2005, 72% of gender confirmation surgeries were bottom surgeries; from 2006 to 2011, that number increased to 84%. And the number of patients insured by Medicare or Medicaid seeking these procedures increased threefold between 2012-2013 and 2014.
As societal acceptance of gender diversity has grown, medical thinking has changed, too, Bowers notes.
“At least in the academic circles, in the medical circles, we realize that yes, it’s valid, that yes, kids do better after treatment, yes, surgery is appropriate, and why wait till 21?” Bowers said. “That’s really completely arbitrary. In fact, it’s probably cruel.”
“Most of the research is on older patients,” Elizabeth Boskey, a social worker at the Center for Gender Surgery at Boston Children’s Hospital and co-author of several research papers on gender confirmation gender-affirming surgery in youth, notes. “But there is evidence in the literature about just overall improved health, reduced anxiety, increased ability to function, for individuals after they have these gender-affirming surgeries.”
What does research say about treatment of transgender youth?
A review of the latest research on gender-affirming hormones and surgery in transgender youth , published in a June 2019 edition of The Lancet Diabetes & Endocrinology , supports Bowers’ assertions that gender confirmation surgery benefits adolescents, though it does not go as far as to recommend specific age guidelines.
“Several preliminary studies have shown benefits of gender-affirming surgery in adolescents, particularly regarding bilateral mastectomy in transgender adolescent males, but there is a scarcity of literature to guide clinical practice for surgical vaginoplasty in transgender adolescent females,” the authors write. “The optimal age and developmental stage for initiating [cross sex hormones] and performing gender-affirming surgeries remains to be clarified.”
The World Professional Association for Transgender Health (WPATH), a leading organization for transgender health worldwide whose membership consists of physicians and educators, publishes Standards of Care and Ethical Guidelines for the treatment of transgender patients.
Though WPATH’s Standards of Care was last updated in 2011 and is under revision, even the current standards suggest that individuals at the age of majority in a given country (for the United States, that’s 18) who have lived for at least 12 months in accordance with their gender identity should be eligible for genital surgery, and that chest surgeries can be done earlier.
“I think it’s important to recognize for all of these standards of care, these are flexible guidelines,” says Loren Schechter, director of the Center for Gender Confirmation Surgery at Weiss Memorial Hospital , clinical professor of surgery at the University of Illinois at Chicago, and co-lead for the revision of the WPATH standards of care surgery chapter for adolescents and adults. “It is not necessarily uncommon that we will currently perform bottom surgeries under the legal age of majority now.”
Schechter also indicated that the revision of the standards will likely include lowered age guidelines.

One reason to give transgender youth access to surgery
Schechter maintains that there are many reasons why minors should be eligible to receive gender confirmation surgery.
“One of them is that post-operative care in a supportive environment is very important,” Schechter said. “So, for example, for those individuals going off to college, the ability to recuperate while at home in a supportive environment and parents during that post-operative period is quite important. Trying to have your post-operative care in a dorm room after surgery is it is not necessarily an ideal scenario.”
This reasoning was echoed in a paper published in the Journal of Sexual Medicine in April 2017 . For the study, researchers asked 20 WPATH-affiliated surgeons practicing in the U.S. about whether and why they performed genital surgery on transgender female minors.
Respondents noted the beneficial recovery environment some minor patients may have.
“Some surgeons viewed timing the procedure before college attendance as a harm reduction measure: Younger patients who have the support of their families, support of their parents, and can have the operation while they are still at home, as opposed to being alone at school or at work, anecdotally tend to do much better than someone who is alone and doesn’t have appropriate support.”
Others suggest that receiving surgery as a minor might allow the patient to “fully socially transition” in their next phase, such as in college.
Who is ready for surgery? Considerations beyond age
Physicians involved in the study also noted that while the number of minors requesting information about genital surgery had increased, psychological maturity is their main criteria for approval.
As one interviewed surgeon put it, “Age is arbitrary. The true measures of how well a patient will do are based on maturity, discipline and support.”
Eleven of the 20 surgeons interviewed had performed such surgeries. Minors ranged in age from 15 to “a day before 18.” About two-thirds of surgeons interviewed believe that such decisions should be made on a case-by-case basis rather than in strict adherence with current WPATH guidelines, which advises to wait until 18 in the U.S.
Boskey, who works for the Center for Gender Surgery at Boston Children’s Hospital, notes: “Just setting the age guidelines in place doesn’t remove the need to appropriately assess whether the surgery is something that should be happening,” she said.
“They’re going to need to make certain that the patient is appropriate for that surgery, that they are being diagnosed with gender dysphoria, that they are taking hormones as appropriate, that they are living in their affirmed gender, that they are aware of all of the life-changing nature of these surgeries,” she said. “These are surgeries that require pretty intense assessment to make certain that they’re appropriate. But that needs to come from the clinical side, rather than the insurance side.”
Will trans youth regret surgery? What the research says
Research supports the benefits of early interventions.
A 2018 study published in JAMA Pediatrics of 136 transmasculine youth and young adults between the ages of 13 and 25 receiving care at Children’s Hospital of Los Angeles finds that, on average, chest dysphoria, or distress caused by one’s chest, was significantly higher among participants who had not received chest reconstruction surgery as compared with those who did .
Serious complications among the surgery group were rare, and only one of the 68 patients who received surgery reported experiencing regret sometimes, with the other 67 reporting no regret over the procedure. The time that had elapsed between surgery and the survey ranged from less than 1 year to 5 years.
“Given these findings,” the authors conclude, “professional guidelines and clinical practice should consider patients for chest surgery based on individual need rather than chronologic age.”
Those who study the impact of early access to gender confirming surgeries often point to research from the Netherlands, home to one of the earliest comprehensive gender clinics.
“[T]hey’ve probably got the most data on transgender, gender non-conforming adolescents, who have been followed longitudinally, prospectively in the most rigorous way — that data indicates that people do well with early access and early interventions,” Schechter says. “By early, I mean late adolescence — we’re not, of course, talking about operating on children.”
Adolescents who were the first 22 people to receive gender confirming surgery at the clinic in the Netherlands showed after surgery that they no longer experienced distress over their gender, according to a 1997 publication in the Journal of the American Academy of Child & Adolescent Psychiatry .
The study also showed that the 22 adolescents scored within the normal range for a number of psychological measures.
Further, the authors note, “Not a single subject expressed feelings of regret concerning the decision to undergo sex reassignment.”
A follow-up study, published four years later, of another group of 20 adolescents receiving surgery after the first group of 22 confirmed the initial findings .
Another, later study in the Netherlands focused on the outcomes of 55 transgender young adults who received gender confirmation surgery between 2004 and 2011. The participants all “were generally satisfied with their physical appearance and none regretted treatment.”
Moreover, gender dysphoria was alleviated, mental health improved, and well-being among those studied was similar to or better than their peers in the general population.
About The Author
Chloe Reichel
Long-term Outcomes After Gender-Affirming Surgery: 40-Year Follow-up Study
Affiliations.
- 1 From the Department of Plastic and Reconstructive Surgery.
- 2 School of Medicine.
- 3 Department of Obstetrics and Gynecology.
- 4 Department of Urology.
- 5 Department of Psychiatry and Neurobehavioral Sciences, University of Virginia, Charlottesville, VA.
- PMID: 36149983
- DOI: 10.1097/SAP.0000000000003233
Background: Gender dysphoria is a condition that often leads to significant patient morbidity and mortality. Although gender-affirming surgery (GAS) has been offered for more than half a century with clear significant short-term improvement in patient well-being, few studies have evaluated the long-term durability of these outcomes.
Methods: Chart review identified 97 patients who were seen for gender dysphoria at a tertiary care center from 1970 to 1990 with comprehensive preoperative evaluations. These evaluations were used to generate a matched follow-up survey regarding their GAS, appearance, and mental/social health for standardized outcome measures. Of 97 patients, 15 agreed to participate in the phone interview and survey. Preoperative and postoperative body congruency score, mental health status, surgical outcomes, and patient satisfaction were compared.
Results: Both transmasculine and transfeminine groups were more satisfied with their body postoperatively with significantly less dysphoria. Body congruency score for chest, body hair, and voice improved significantly in 40 years' postoperative settings, with average scores ranging from 84.2 to 96.2. Body congruency scores for genitals ranged from 67.5 to 79 with free flap phalloplasty showing highest scores. Long-term overall body congruency score was 89.6. Improved mental health outcomes persisted following surgery with significantly reduced suicidal ideation and reported resolution of any mental health comorbidity secondary to gender dysphoria.
Conclusion: Gender-affirming surgery is a durable treatment that improves overall patient well-being. High patient satisfaction, improved dysphoria, and reduced mental health comorbidities persist decades after GAS without any reported patient regret.
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
- Follow-Up Studies
- Gender Dysphoria* / surgery
- Sex Reassignment Surgery*
- Transgender Persons* / psychology
- Transsexualism* / psychology
- Introduction
- Conclusions
- Article Information
Error bars represent 95% CIs. GAS indicates gender-affirming surgery.
Percentages are based on the number of procedures divided by number of patients; thus, as some patients underwent multiple procedures the total may be greater than 100%. Error bars represent 95% CIs.
eTable. ICD-10 and CPT Codes of Gender-Affirming Surgery
eFigure. Percentage of Patients With Codes for Gender Identity Disorder Who Underwent GAS
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Wright JD , Chen L , Suzuki Y , Matsuo K , Hershman DL. National Estimates of Gender-Affirming Surgery in the US. JAMA Netw Open. 2023;6(8):e2330348. doi:10.1001/jamanetworkopen.2023.30348
Manage citations:
© 2024
- Permissions
National Estimates of Gender-Affirming Surgery in the US
- 1 Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, New York, New York
- 2 Department of Obstetrics and Gynecology, University of Southern California, Los Angeles
Question What are the temporal trends in gender-affirming surgery (GAS) in the US?
Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
Meaning These findings suggest that there will be a greater need for clinicians knowledgeable in the care of transgender individuals with the requisite expertise to perform gender-affirming procedures.
Importance While changes in federal and state laws mandating coverage of gender-affirming surgery (GAS) may have led to an increase in the number of annual cases, comprehensive data describing trends in both inpatient and outpatient procedures are limited.
Objective To examine trends in inpatient and outpatient GAS procedures in the US and to explore the temporal trends in the types of GAS performed across age groups.
Design, Setting, and Participants This cohort study includes data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. Patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified, and the performance of GAS, including breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures, were identified.
Main Outcome Measures Weighted estimates of the annual number of inpatient and outpatient procedures performed and the distribution of each class of procedure overall and by age were analyzed.
Results A total of 48 019 patients who underwent GAS were identified, including 25 099 (52.3%) who were aged 19 to 30 years. The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years. When stratified by the type of procedure performed, breast and chest procedures made up a greater percentage of the surgical interventions in younger patients, while genital surgical procedures were greater in older patients.
Conclusions and Relevance Performance of GAS has increased substantially in the US. Breast and chest surgery was the most common group of procedures performed. The number of genital surgical procedures performed increased with increasing age.
Gender dysphoria is characterized as an incongruence between an individual’s experienced or expressed gender and the gender that was assigned at birth. 1 Transgender individuals may pursue multiple treatments, including behavioral therapy, hormonal therapy, and gender-affirming surgery (GAS). 2 GAS encompasses a variety of procedures that align an individual patient’s gender identity with their physical appearance. 2 - 4
While numerous surgical interventions can be considered GAS, the procedures have been broadly classified as breast and chest surgical procedures, facial and cosmetic interventions, and genital reconstructive surgery. 2 , 4 Prior studies 2 - 7 have shown that GAS is associated with improved quality of life, high rates of satisfaction, and a reduction in gender dysphoria. Furthermore, some studies have reported that GAS is associated with decreased depression and anxiety. 8 Lastly, the procedures appear to be associated with acceptable morbidity and reasonable rates of perioperative complications. 2 , 4
Given the benefits of GAS, the performance of GAS in the US has increased over time. 9 The increase in GAS is likely due in part to federal and state laws requiring coverage of transition-related care, although actual insurance coverage of specific procedures is variable. 10 , 11 While prior work has shown that the use of inpatient GAS has increased, national estimates of inpatient and outpatient GAS are lacking. 9 This is important as many GAS procedures occur in ambulatory settings. We performed a population-based analysis to examine trends in GAS in the US and explored the temporal trends in the types of GAS performed across age groups.
To capture both inpatient and outpatient surgical procedures, we used data from the Nationwide Ambulatory Surgery Sample (NASS) and the National Inpatient Sample (NIS). NASS is an ambulatory surgery database and captures major ambulatory surgical procedures at nearly 2800 hospital-owned facilities from up to 35 states, approximating a 63% to 67% stratified sample of hospital-owned facilities. NIS comprehensively captures approximately 20% of inpatient hospital encounters from all community hospitals across 48 states participating in the Healthcare Cost and Utilization Project (HCUP), covering more than 97% of the US population. Both NIS and NASS contain weights that can be used to produce US population estimates. 12 , 13 Informed consent was waived because data sources contain deidentified data, and the study was deemed exempt by the Columbia University institutional review board. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We selected patients of all ages with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision ( ICD-10 ) diagnosis codes for gender identity disorder or transsexualism ( ICD-10 F64) or a personal history of sex reassignment ( ICD-10 Z87.890) from 2016 to 2020 (eTable in Supplement 1 ). We first examined all hospital (NIS) and ambulatory surgical (NASS) encounters for patients with these codes and then analyzed encounters for GAS within this cohort. GAS was identified using ICD-10 procedure codes and Common Procedural Terminology codes and classified as breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures. 2 , 4 Breast and chest surgical procedures encompassed breast reconstruction, mammoplasty and mastopexy, or nipple reconstruction. Genital reconstructive procedures included any surgical intervention of the male or female genital tract. Other facial and cosmetic procedures included cosmetic facial procedures and other cosmetic procedures including hair removal or transplantation, liposuction, and collagen injections (eTable in Supplement 1 ). Patients might have undergone procedures from multiple different surgical groups. We measured the total number of procedures and the distribution of procedures within each procedural group.
Within the data sets, sex was based on patient self-report. The sex of patients in NIS who underwent inpatient surgery was classified as either male, female, missing, or inconsistent. The inconsistent classification denoted patients who underwent a procedure that was not consistent with the sex recorded on their medical record. Similar to prior analyses, patients in NIS with a sex variable not compatible with the procedure performed were classified as having undergone genital reconstructive surgery (GAS not otherwise specified). 9
Clinical variables in the analysis included patient clinical and demographic factors and hospital characteristics. Demographic characteristics included age at the time of surgery (12 to 18 years, 19 to 30 years, 31 to 40 years, 41 to 50 years, 51 to 60 years, 61 to 70 years, and older than 70 years), year of the procedure (2016-2020), and primary insurance coverage (private, Medicare, Medicaid, self-pay, and other). Race and ethnicity were only reported in NIS and were classified as White, Black, Hispanic and other. Race and ethnicity were considered in this study because prior studies have shown an association between race and GAS. The income status captured national quartiles of median household income based of a patient’s zip code and was recorded as less than 25% (low), 26% to 50% (medium-low), 51% to 75% (medium-high), and 76% or more (high). The Elixhauser Comorbidity Index was estimated for each patient based on the codes for common medical comorbidities and weighted for a final score. 14 Patients were classified as 0, 1, 2, or 3 or more. We separately reported coding for HIV and AIDS; substance abuse, including alcohol and drug abuse; and recorded mental health diagnoses, including depression and psychoses. Hospital characteristics included a composite of teaching status and location (rural, urban teaching, and urban nonteaching) and hospital region (Northeast, Midwest, South, and West). Hospital bed sizes were classified as small, medium, and large. The cutoffs were less than 100 (small), 100 to 299 (medium), and 300 or more (large) short-term acute care beds of the facilities from NASS and were varied based on region, urban-rural designation, and teaching status of the hospital from NIS. 8 Patients with missing data were classified as the unknown group and were included in the analysis.
National estimates of the number of GAS procedures among all hospital encounters for patients with gender identity disorder were derived using discharge or encounter weight provided by the databases. 15 The clinical and demographic characteristics of the patients undergoing GAS were reported descriptively. The number of encounters for gender identity disorder, the percentage of GAS procedures among those encounters, and the absolute number of each procedure performed over time were estimated. The difference by age group was examined and tested using Rao-Scott χ 2 test. All hypothesis tests were 2-sided, and P < .05 was considered statistically significant. All analyses were conducted using SAS version 9.4 (SAS Institute Inc).
A total of 48 019 patients who underwent GAS were identified ( Table 1 ). Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged 12 to 18 years. Private insurance coverage was most common in 29 064 patients (60.5%), while 12 127 (25.3%) were Medicaid recipients. Depression was reported in 7192 patients (15.0%). Most patients (42 467 [88.4%]) were treated at urban, teaching hospitals, and there was a disproportionate number of patients in the West (22 037 [45.9%]) and Northeast (12 396 [25.8%]). Within the cohort, 31 668 patients (65.9%) underwent 1 procedure while 13 415 (27.9%) underwent 2 procedures, and the remainder underwent multiple procedures concurrently ( Table 1 ).
The overall number of health system encounters for gender identity disorder rose from 13 855 in 2016 to 38 470 in 2020. Among encounters with a billing code for gender identity disorder, there was a consistent rise in the percentage that were for GAS from 4552 (32.9%) in 2016 to 13 011 (37.1%) in 2019, followed by a decline to 12 818 (33.3%) in 2020 ( Figure 1 and eFigure in Supplement 1 ). Among patients undergoing ambulatory surgical procedures, 37 394 (80.3%) of the surgical procedures included gender-affirming surgical procedures. For those with hospital admissions with gender identity disorder, 10 625 (11.8%) of admissions were for GAS.
Breast and chest procedures were most common and were performed for 27 187 patients (56.6%). Genital reconstruction was performed for 16 872 patients (35.1%), and other facial and cosmetic procedures for 6669 patients (13.9%) ( Table 2 ). The most common individual procedure was breast reconstruction in 21 244 (44.2%), while the most common genital reconstructive procedure was hysterectomy (4489 [9.3%]), followed by orchiectomy (3425 [7.1%]), and vaginoplasty (3381 [7.0%]). Among patients who underwent other facial and cosmetic procedures, liposuction (2945 [6.1%]) was most common, followed by rhinoplasty (2446 [5.1%]) and facial feminizing surgery and chin augmentation (1874 [3.9%]).
The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020 ( Figure 1 ). Similar trends were noted for breast and chest surgical procedures as well as genital surgery, while the rate of other facial and cosmetic procedures increased consistently from 2016 to 2020. The distribution of the individual procedures performed in each class were largely similar across the years of analysis ( Table 3 ).
When stratified by age, patients 19 to 30 years had the greatest number of procedures, 25 099 ( Figure 2 ). There were 10 476 procedures performed in those aged 31 to 40 years and 4359 in those aged 41 to 50 years. Among patients younger than 19 years, 3678 GAS procedures were performed. GAS was less common in those cohorts older than 50 years. Overall, the greatest number of breast and chest surgical procedures, genital surgical procedures, and facial and other cosmetic surgical procedures were performed in patients aged 19 to 30 years.
When stratified by the type of procedure performed, breast and chest procedures made up the greatest percentage of the surgical interventions in younger patients while genital surgical procedures were greater in older patients ( Figure 2 ). Additionally, 3215 patients (87.4%) aged 12 to 18 years underwent GAS and had breast or chest procedures. This decreased to 16 067 patients (64.0%) in those aged 19 to 30 years, 4918 (46.9%) in those aged 31 to 40 years, and 1650 (37.9%) in patients aged 41 to 50 years ( P < .001). In contrast, 405 patients (11.0%) aged 12 to 18 years underwent genital surgery. The percentage of patients who underwent genital surgery rose sequentially to 4423 (42.2%) in those aged 31 to 40 years, 1546 (52.3%) in those aged 51 to 60 years, and 742 (58.4%) in those aged 61 to 70 years ( P < .001). The percentage of patients who underwent facial and other cosmetic surgical procedures rose with age from 9.5% in those aged 12 to 18 years to 20.6% in those aged 51 to 60 years, then gradually declined ( P < .001). Figure 2 displays the absolute number of procedure classes performed by year stratified by age. The greatest magnitude of the decline in 2020 was in younger patients and for breast and chest procedures.
These findings suggest that the number of GAS procedures performed in the US has increased dramatically, nearly tripling from 2016 to 2019. Breast and chest surgery is the most common class of procedure performed while patients are most likely to undergo surgery between the ages of 19 and 30 years. The number of genital surgical procedures performed increased with increasing age.
Consistent with prior studies, we identified a remarkable increase in the number of GAS procedures performed over time. 9 , 16 A prior study examining national estimates of inpatient GAS procedures noted that the absolute number of procedures performed nearly doubled between 2000 to 2005 and from 2006 to 2011. In our analysis, the number of GAS procedures nearly tripled from 2016 to 2020. 9 , 17 Not unexpectedly, a large number of the procedures we captured were performed in the ambulatory setting, highlighting the need to capture both inpatient and outpatient procedures when analyzing data on trends. Like many prior studies, we noted a decrease in the number of procedures performed in 2020, likely reflective of the COVID-19 pandemic. 18 However, the decline in the number of procedures performed between 2019 and 2020 was relatively modest, particularly as these procedures are largely elective.
Analysis of procedure-specific trends by age revealed a number of important findings. First, GAS procedures were most common in patients aged 19 to 30 years. This is in line with prior work that demonstrated that most patients first experience gender dysphoria at a young age, with approximately three-quarters of patients reporting gender dysphoria by age 7 years. These patients subsequently lived for a mean of 23 years for transgender men and 27 years for transgender women before beginning gender transition treatments. 19 Our findings were also notable that GAS procedures were relatively uncommon in patients aged 18 years or younger. In our cohort, fewer than 1200 patients in this age group underwent GAS, even in the highest volume years. GAS in adolescents has been the focus of intense debate and led to legislative initiatives to limit access to these procedures in adolescents in several states. 20 , 21
Second, there was a marked difference in the distribution of procedures in the different age groups. Breast and chest procedures were more common in younger patients, while genital surgery was more frequent in older individuals. In our cohort of individuals aged 19 to 30 years, breast and chest procedures were twice as common as genital procedures. Genital surgery gradually increased with advancing age, and these procedures became the most common in patients older than 40 years. A prior study of patients with commercial insurance who underwent GAS noted that the mean age for mastectomy was 28 years, significantly lower than for hysterectomy at age 31 years, vaginoplasty at age 40 years, and orchiectomy at age 37 years. 16 These trends likely reflect the increased complexity of genital surgery compared with breast and chest surgery as well as the definitive nature of removal of the reproductive organs.
This study has limitations. First, there may be under-capture of both transgender individuals and GAS procedures. In both data sets analyzed, gender is based on self-report. NIS specifically makes notation of procedures that are considered inconsistent with a patient’s reported gender (eg, a male patient who underwent oophorectomy). Similar to prior work, we assumed that patients with a code for gender identity disorder or transsexualism along with a surgical procedure classified as inconsistent underwent GAS. 9 Second, we captured procedures commonly reported as GAS procedures; however, it is possible that some of these procedures were performed for other underlying indications or diseases rather than solely for gender affirmation. Third, our trends showed a significant increase in procedures through 2019, with a decline in 2020. The decline in services in 2020 is likely related to COVID-19 service alterations. Additionally, while we comprehensively captured inpatient and ambulatory surgical procedures in large, nationwide data sets, undoubtedly, a small number of procedures were performed in other settings; thus, our estimates may underrepresent the actual number of procedures performed each year in the US.
These data have important implications in providing an understanding of the use of services that can help inform care for transgender populations. The rapid rise in the performance of GAS suggests that there will be a greater need for clinicians knowledgeable in the care of transgender individuals and with the requisite expertise to perform GAS procedures. However, numerous reports have described the political considerations and challenges in the delivery of transgender care. 22 Despite many medical societies recognizing the necessity of gender-affirming care, several states have enacted legislation or policies that restrict gender-affirming care and services, particularly in adolescence. 20 , 21 These regulations are barriers for patients who seek gender-affirming care and provide legal and ethical challenges for clinicians. As the use of GAS increases, delivering equitable gender-affirming care in this complex landscape will remain a public health challenge.
Accepted for Publication: July 15, 2023.
Published: August 23, 2023. doi:10.1001/jamanetworkopen.2023.30348
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Wright JD et al. JAMA Network Open .
Corresponding Author: Jason D. Wright, MD, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, 161 Fort Washington Ave, 4th Floor, New York, NY 10032 ( [email protected] ).
Author Contributions: Dr Wright had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Wright, Chen.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Wright.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Wright, Chen.
Administrative, technical, or material support: Wright, Suzuki.
Conflict of Interest Disclosures: Dr Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Plast Reconstr Surg Glob Open
- v.9(3); 2021 Mar
Regret after Gender-affirmation Surgery: A Systematic Review and Meta-analysis of Prevalence
Valeria p. bustos.
From the * Division of Plastic and Reconstructive Surgery, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Mass.
Samyd S. Bustos
† Department of Plastic Surgery, University of Pittsburgh, Pittsburgh, Pa.
Andres Mascaro
‡ Department of Plastic and Reconstructive Surgery, Cleveland Clinic, Weston, Fla.
Gabriel Del Corral
§ Department of Plastic and Reconstructive Surgery, MedStar Georgetown University Hospital, Washington, D.C.
Antonio J. Forte
¶ Division of Plastic and Reconstructive Surgery, Mayo Clinic, Jacksonville, Fla.
Pedro Ciudad
∥ Department of Plastic, Reconstructive and Burn Surgery, Arzobispo Loayza National Hospital, Lima, Peru
Esther A. Kim
** Division of Plastic and Reconstructive Surgery, University of California, San Francisco, Calif.
Howard N. Langstein
†† Division of Plastic and Reconstructive Surgery, University of Rochester Medical Center, Strong Memorial Hospital, Rochester, N.Y.
Oscar J. Manrique
Associated data.
Supplemental Digital Content is available in the text.
Background:
There is an unknown percentage of transgender and gender non-confirming individuals who undergo gender-affirmation surgeries (GAS) that experiences regret. Regret could lead to physical and mental morbidity and questions the appropriateness of these procedures in selected patients. The aim of this study was to evaluate the prevalence of regret in transgender individuals who underwent GAS and evaluate associated factors.
A systematic review of several databases was conducted. Random-effects meta-analysis, meta-regression, and subgroup and sensitivity analyses were performed.
A total of 27 studies, pooling 7928 transgender patients who underwent any type of GAS, were included. The pooled prevalence of regret after GAS was 1% (95% CI <1%–2%). Overall, 33% underwent transmasculine procedures and 67% transfemenine procedures. The prevalence of regret among patients undergoing transmasculine and transfemenine surgeries was <1% (IC <1%–<1%) and 1% (CI <1%–2%), respectively. A total of 77 patients regretted having had GAS. Twenty-eight had minor and 34 had major regret based on Pfäfflin’s regret classification. The majority had clear regret based on Kuiper and Cohen-Kettenis classification.
Conclusions:
Based on this review, there is an extremely low prevalence of regret in transgender patients after GAS. We believe this study corroborates the improvements made in regard to selection criteria for GAS. However, there is high subjectivity in the assessment of regret and lack of standardized questionnaires, which highlight the importance of developing validated questionnaires in this population.
Introduction
Discordance or misalignment between gender identity and sex assigned at birth can translate into disproportionate discomfort, configuring the definition of gender dysphoria. 1 – 3 This population has increased risk of psychiatric conditions, including depression, substance abuse disorders, self-injury, and suicide, compared with cis-gender individuals. 4 , 5 Approximately 0.6% of adults in the United States identify themselves as transgenders. 6 Despite advocacy to promote and increase awareness of the human rights of transgender and gender non-binary (TGNB) individuals, discrimination continue to afflict the daily life of these individuals. 4 , 7
Gender-affirmation care plays an important role in tackling gender dysphoria. 5 , 8 – 10 Gender-affirmation surgeries (GAS) aim to align the patients’ appearance with their gender identity and help achieve personal comfort with one-self, which will help decrease psychological distress. 5 , 10 These interventions should be addressed by a multidisciplinary team, including psychiatrists, psychologists, endocrinologists, physical therapists, and surgeons. 1 , 9 The number of GAS has consistently increased during the last years. In the United States, from 2017 to 2018, the number of GAS increased to 15.3%. 8 , 11 , 12
Significant improvement in the quality of life, body image/satisfaction, and overall psychiatric functioning in patients who underwent GAS has been well documented. 5 , 13 – 19 However, despite this, there is a minor population that experiences regret, occasionally leading to de-transition surgeries. 20 Both regret and de-transition may add an important burden of physical, social, and mental distress, which raises concerns about the appropriateness and effectiveness of these procedures in selected patients. Special attention should be paid in identifying and recognizing the prevalence and factors associated with regret. In the present study, we hypothesized that the prevalence of regret is less than the last estimation by Pfafflin in 1993, due to improvements in standard of care, patient selection, surgical techniques, and gender confirmation care. Therefore, the aim of this study was to evaluate the prevalence of regret and assess associated factors in TGNB patients 13-years-old or older who underwent GAS. 20
Search Methodology
Following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines, a comprehensive research of several databases from each database’s inception to May 11, 2020, for studies in both English and Spanish languages, was conducted. 21 The databases included Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations, and Daily, Ovid EMBASE, Ovid Cochrane Central Register of Controlled Trials, Ovid Cochrane Database of Systematic Reviews, and Scopus. The search strategy was designed and conducted by an experienced librarian, with input from the study’s principal investigator. Controlled vocabulary supplemented with keywords was used to search for studies of de-transition and regret in adult patients who underwent gender confirmation surgery. The actual strategy listing all search terms used and how they are combined is available in Supplemental Digital Content 1. ( See Supplemental Digital Content 1, which displays the search strategy. http://links.lww.com/PRSGO/B598 .)
Study Selection
Search results were exported from the database into XML format and then uploaded to Covidence. 22 The study selection was performed in a 2-stage screening process. The first step was conducted by 2 screeners (V.P.B. and S.S.B.), who reviewed titles and abstracts and selected those of relevance to the research question. Then, the same 2 screeners reviewed full text of the remaining articles and selected those eligible according to the inclusion and exclusion criteria (Fig. (Fig.1). 1 ). If disagreements were encountered, a third reviewer (O.J.M.) moderated a discussion, and a joint decision between the 3 reviewers was made for a final determination. Inclusion criteria were all the articles that included patients aged 13 years or more who underwent GAS and report regret or de-transition rates, and observational or interventional studies in English or Spanish language. Exclusion criteria were letter to the editors, case series with <10 patients, case reports correspondences, and animal studies.

PRISMA flow diagram for systematic reviews.
Data Extraction/Synthesis
After selecting the articles, we assessed study characteristics. We identified year of publication, country in which the study was conducted, population size, and number of transmasculine and transfemenine patients with their respective mean age (expressed with SD, range, or interquartile range if included in the study). In addition, we extracted information of the method of data collection (interviews versus questionnaires), number of regrets following GAS, as well as the type of surgery, time of follow-up, and de-transition procedures. We classified the type of regret based on the patient’s reasons for regret if they were mentioned in the studies. We used the Pfäfflin and Kuiper and Cohen-Kettenis classifications of regret (Table (Table1 1 ). 20 , 23
Pfäfflin and Kuiper and Cohen-Kettenis Categories of Regret
Quality Assessment
To assess the risk of bias within each study, the National Institute of Health (NIH) quality assessment tool was used. 24 This tool ranks each article as “good,” “fair,” or “poor,” and with this, we categorized each article into “low risk,” “moderate risk,” or “high risk” of bias, respectively.
Our primary outcome of interest was the prevalence of regret of transgender patients who underwent any type of GAS. Secondary outcomes of interest were discriminating the prevalence of regrets by type gender transition (transfemenine and transmasculine), and type of surgery.
Data Analysis and Synthesis
The binominal data were analyzed, and the pooled prevalence of regret was estimated using proportion meta-analysis with Stata Software/IC (version 16.1). 25 Given the heterogeneity between studies, we conducted a logistic-normal-random-effect model. The study-specific proportions with 95% exact CIs and overall pooled estimates with 95% Wald CIs with Freeman-Turkey double arcsine transformation were used. The effect size and percentage of weight were presented for each individual study. 25 , 26
To evaluate heterogeneity, I 2 statistics was used. If P < 0.05 or I 2 > 50%, significant heterogeneity was considered. A univariate meta-regression analysis was performed to assess the significance in country of origin, tools of measurement, and quality of the studies.
To assess publication bias, we used funnel plot graphic and the Egger test. If this test showed us no statistical significance ( P > 0.05), we assumed that the publication bias had a low impact on the results of our metanalysis. To assess the impact of the publication bias on our missing studies, we used the trim-and-fill method.
A sensitivity analysis was conducted to assess the influence of certain characteristics in the magnitude and precision of the overall prevalence of regret. The following characteristics were excluded: <10 participants included, and the presence of a high risk of bias.
A total of 74 articles were identified in the search, and 2 additional records were identified through other sources. After the first-step screening process, 39 articles were relevant based on the information provided in their titles and abstracts. After the second-step process, a total of 27 articles were included in the systematic review and metanalysis (Fig. (Fig.1 1 ).
Based on the NIH quality assessment tool, the majority of article ranged between “poor” and “fair” categories. 24 ( See Supplemental Digital Content 2, which displays the score of each reviewed study. http://links.lww.com/PRSGO/B599 .)
Study Characteristics
In total, the included studies pooled 7928 cases of transgender individuals who underwent any type of GAS. A total of 2578 (33%) underwent transmasculine procedures, 5136 (67%) underwent transfemenine surgeries, and 1 non-binary patient underwent surgery. In Table Table2 2 characteristics of studies are listed. Without discriminating type of surgical technique, from all transfemenine surgeries included, 772 (39.3%) were vaginoplasty, 260 (13.3%) were clitoroplasty, 107 (5.5%) were breast augmentation, 72 (3.7%) were labioplasty and vulvoplasty, and a small minority were facial feminization surgery, vocal cord surgery, thyroid cartilage reduction, and oophorectomy surgery. The rest did not specify type of surgery. In regard to transmasculine surgeries, 297 (12.4%) were mastectomies, 61 (2.6%) were phalloplasties, and 51 (2.1%) hysterectomies (Table (Table3 3 and and4). 4 ). Overall, follow-up time from surgery to the time of regret assessment ranged from 0.8 to 9 years (Table (Table2 2 ).
*Reflects the mean of both transmasculine and transfemenine.
†Includes both scheduled and completed surgery.
‡Includes both surgery and no surgery patients.
H, High; He, Heterosexual; Ho, Homosexual; I, Interview; IQR, Interquartile Range; L, Low; M, Moderate; Me, Median; NA, Not applicable; NS: Not specified, Q: Questionnaire; RAP: Radial Arterial Forearm-Flap Phalloplasty without or with cutaneous nerve to clitoral nerve anastomosis; SP: Suprapubic Pedicle-Flap Phalloplasty.
Studies Differentiating Type of Surgery among Transfemenine Patients
Studies Differentiating the Type of Surgery among Transmasculine Patients
Regrets and De-transition
Almost all studies conducted non-validated questionnaires to assess regret due to the lack of standardized questionnaires available in this topic. 15 , 19 – 33 Most of the questions evaluating regret used options such as, “ yes,” “sometimes,” “no” or “ all the time,” “sometimes,” “never,” or “most certainly, ” “very likely,” “maybe,” “rather not,” or “definitely not.” 14 , 18 , 19 , 23 , 27 – 38 Other studies used semi-structured interviews. 34 , 37 , 39 – 43 However, in both circumstances, some studies provided further specific information on reasons for regret. 14 , 20 , 23 , 29 , 32 , 36 , 41 , 44 – 46 Of the 7928 patients, 77 expressed regret (12 transmen, 57 transwomen, 8 not specified), understood by those who had “sometimes” or “always” felt it.
Reasons for Regret
The most prevalent reason for regret was the difficulty/dissatisfaction/acceptance in life with the new gender role. 23 , 29 , 32 , 36 , 44 Other less prevalent reasons were “failure” of surgery to achieve their surgical goals in an aesthetic level and psychological level. 29 , 32 , 36 , 47 Based on the reasons presented, we classified the types of regrets according to Pfäfflin’s types of regret and Kuiper and Cohen-Kettenis classification. According to Pfäfflin’s types, 28 patients had minor regret, and 34 patients had major regret. 14 , 20 , 23 , 29 , 32 , 36 , 41 , 44 , 45 Based on the Kuiper and Cohen-Kettenis regret classification, 35 patients had clear regret, 26 uncertain regret, 1 regret, and none presented with regret assumed by others. 23 In Table Table5 5 and and6, 6 , the reasons and classifications are shown.
Type of Regret
*8 mastectomies, 2 vaginectomies, 2 phalloplasties, 2 testicular implants removal, and 1 breast augmentation.
N, no; NS, not specified; Y, Yes.
Causes of Regret
NS, not specified.
Prevalence of Regret
The pooled prevalence of regret among the TGNB population after GAS was 1% (95% Confidence interval [CI] <1%–2%; I 2 = 75.1%) (Fig. (Fig.2). 2 ). The prevalence for transmasculine surgeries was <1% (CI <1%–<1%, I 2 = 28.8%), and for transfemenine surgeries, it was 1% (CI <1%–2%, I 2 = 75.5%) (Fig. (Fig.3). 3 ). The prevalence of regret after vaginoplasty was of 2% (CI <1%–4%, I 2 = 41.5%) and that after mastectomy was <1% (CI <1–<1%, I 2 = 21.8%) (Fig. (Fig.4 4 ).

Pooled prevalence of regret among TGNB individuals after gender confirmation surgery. Heterogeneity χ 2 = 104.31 (d.f. = 26), P = 0.00, I 2 [variation in effect size (ES) attributable to heterogeneity] = 75.08%, Estimate of between-study variance Ʈ 2 = 0.02, Test of ES = 0, z = 4.22, P = 0.00.

Subgroup analysis of the prevalence of regret among TGNB individuals after gender confirmation surgery based on gender. ES, effect size.

Subgroup analysis of the prevalence of regret among TGNB individuals after gender confirmation surgery based on the type of surgery. ES, effect size.
Meta-regression and Publication Bias
No covariates analyzed affected the pooled endpoint in this metanalysis. The Funnel Plot shows asymmetry between studies (Fig. (Fig.5). 5 ). The Egger test resulted in a P value of 0.0271, which suggests statistical significance for publication bias. The Trim & Fill method imputed 14 approximated studies, with limited impact of the adjusted results. The change in effect size was from 0.010 to 0.005 with no statistical significance (Fig. (Fig.6 6 ).

Funnel plot.

Funnel plot of the Trim & Fill method.
Sensitivity Analysis
When excluding studies with sample sizes less than 10 and high-risk biased studies, the pooled prevalence was similar 1% (CI <1%–3%) compared with the pooled prevalence when those studies were included 1% (CI <1%–2%).
The prevalence of regret in the TGNB population after GAS was of 1% (CI <1%–2%). The prevalence of regret for transfemenine surgeries was 1% (CI <1%–2%), and the prevalence for transmasculine surgeries was <1% (CI <1%–<1%). Traditionally, the landmark reference of regret prevalence after GAS has been based on the study by Pfäfflin in 1993, who reported a regret rate of 1%–1.5%. In this study, the author estimated the regret prevalence by analyzing two sources: studies from the previous 30 years in the medical literature and the author’s own clinical practice. 20 In the former, the author compiled a total of approximately 1000–1600 transfemenine, and 400–550 transmasculine. In the latter, the author included a total of 196 transfemenine, and 99 transmasculine patients. 20 In 1998, Kuiper et al followed 1100 transgender subjects that underwent GAS using social media and snowball sampling. 23 Ten experienced regret (9 transmasculine and 1 transfemenine). The overall prevalence of regret after GAS in this study was of 0.9%, and 3% for transmasculine and <0.12% for transfemenine. 23 Because these studies were conducted several years ago and were limited to specific countries, these estimations may not be generalizable to the entire TGNB population. However, a clear trend towards low prevalences of regret can be appreciated.
The causes and types of regrets reported in the studies are specified and shown in Table Table5 5 and and6. 6 . Overall, the most common reason for regret was psychosocial circumstances, particularly due to difficulties generated by return to society with the new gender in both social and family enviroments. 23 , 29 , 32 , 33 , 36 , 44 In fact, some patients opted to reverse their gender role to achieve social acceptance, receive better salaries, and preserve relatives and friends relationships. These findings are in line with other studies. Laden et al performed a logistic regression analysis to assess potential risk factors for regret in this population. 46 They found that the two most important risk factors predicting regret were “poor support from the family” and “belonging to the non-core group of transsexuals.” 46 In addition, a study in Italy hypothesized that the high percentage of regret was attributed to social experience when they return after the surgery. 33
Another factor associated with regret (although less prevalent) was poor surgical outcomes. 20 , 23 , 36 Loss of clitoral sensation and postoperative chronic abdominal pain were the most common reported factors associated with surgical outcomes. 14 , 36 In addition, aesthetic outcomes played an important role in regret. Two studies mentioned concerns with aesthetic outcomes. 14 , 47 Only one of them quoted a patient inconformity: “body doesn’t meet the feminine ideal.” 14 Interestingly, Lawrence et al demonstrated in their study that physical results of surgery are by far the most influential in determining satisfaction or regret after GAS than any preoperative factor. 36 Concordantly, previous studies have shown absence of regret if sensation in clitoris and vaginal is achieved and if satisfaction with vaginal width is present. 36
Other factors associated to regret were identified. Blanchard et al in 1989 noted a strong positive correlation between heterosexual preference and postoperative regret. 32 All patients in this study who experienced regret were heterosexual transmen. 32 On the contrary, Lawrence et al in 2003 did not find such correlation and attributed their findings to the increase in social tolerance in North American and Western European societies. 36 Bodlund et al found that clinically evident personality disorder was a negative prognostic factor for regret in patients undergoing GAS. 48 On the other hand, Blanchard et al did not find a correlation among patient’s education, age at surgery, and gender assigned at birth. 32
In the present review, nearly half of the patients experienced major regret (based on Pfäfflin classification), meaning that they underwent or desire de-transition surgery, that will never pass through the same process again, and/or experience increase of gender dysphoria from the new gender. One study found that 10 of 14 patients with regret underwent de-transition surgeries (8 mastectomies, 2 vaginectomies, 2 phalloplasties, 2 testicular implants removal, and 1 breast augmentation) for reasons of social regret, true regret or feeling non-binary. 23 On the other hand, based on the Kuiper and Cohen Kettenis’ classification, half of the patients in this review had clear regret and uncertain regret . This means that they freely expressed their regret toward the procedure, but some had role reversal to the former gender and others did not. Interestingly, Pfäfflin concluded that from a clinical standpoint, trangender patients suffered from many forms of minor regrets after GAS, all of which have a temporary course. 20 This is an important consideration meaning that the actual true regret rate will always remain uncertain, as temporarity and types of regret can bring a huge challenge for assessment.
Regret after GAS may result from the ongoing discrimination that afflicts the TGNB population, affecting their freely expression of gender identity and, consequently feeling regretful from having had surgery. 15 Poor social and group support, late-onset gender transition, poor sexual functioning, and mental health problems are factors associated with regret. 15 Hence, assessing all these potential factors preoperatively and controlling them if possible could reduce regret rates even more and increase postoperative patient satisfaction.
Regarding transfemenine surgery, vaginoplasty was the most prevalent. 14 , 19 , 23 , 30 – 33 , 35 , 36 , 44 , 45 Interesintgly, regret rates were higher in vaginoplasties. 14 , 36 , 44 In this study, we estimated that the overall prevalence of regret after vaginoplasty was 2% (from 11 studies reviewed). This result is slightly higher than a metanalysis of 9 studies from 2017 that reported a prevalence of 1%. 13 Moreover, vaginoplasty has shown to increase the quality of life in these patients. 13 Mastectomy was the most prevalent transmasculine surgery. Also, it showed a very low prevalence of regret after mastectomy (<1%). Olson-Kennedy et al demonstrated that chest surgery decreases chest dysphoria in both minors and young adults, which might be the major reason behind our findings. 38
In the current study, we identified a total of 7928 cases from 14 different countries. To the best of our knowledge, this is the largest attempt to compile the information on regret rates in this population. However, limitations such as significant heterogeneity among studies and among instruments used to assess regret rates, and moderate-to-high risk of bias in some studies represent a big barrier for generalization of the results of this study. The lack of validated questionnaires to evaluate regret in this population is a significant limiting factor. In addition, bias can occur because patients might restrain from expressing regrets due to fear of being judged by the interviewer. Moreover, the temporarity of the feeling of regret in some patients and the variable definition of regret may underestimate the real prevalence of “true” regret.
Based on this meta-analysis, the prevalence of regret is 1%. We believe this reflects and corroborates the increased in accuracy of patient selection criteria for GAS. Efforts should be directed toward the individualization of the patient based on their goals and identification of risk factors for regrets. Surgeons should continue to rigorously follow the current Standard of Care guidelines of the World Professional Association for Transgender Health (WATH). 49
CONCLUSIONS
Our study has shown a very low percentage of regret in TGNB population after GAS. We consider that this is a reflection on the improvements in the selection criteria for surgery. However, further studies should be conducted to assess types of regret as well as association with different types of surgical procedure.
Acknowledgments
All the authors have completed the ICMJE uniform disclosure form. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Supplementary Material
Published online 19 March 2021
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com .

Pope blasts transgender surgery as it represents 'grave threat to the DIGNITY of a person'
The Pope has condemned gender reassignment surgery, saying it represents a “grave threat to the dignity of a person”.
In a text dubbed “Dignitas Infinita” (Infinite Dignity), the Vatican said that “any sex change intervention, as a rule, risks threatening the unique dignity the person has received from the moment of conception”.
The 20-page declaration, which was signed by Pope Francis, reaffirmed the Catholic Church’s long-held opposition to abortion and euthanasia, as well as stressed its rejection of gender theory.
It said God created man and woman as biologically different and that people must not interfere with that plan or try to “make oneself God”.
The declaration, which took five years to draw up, said that surgery to resolve “genital abnormalities” was permissible, however emphasised that “such a medical procedure would not constitute a sex change in the sense intended here”.
The Pope has previously been criticised by Catholic conservatives for his apparent liberal stance on gender issues.
In December, Pope Francis approved new rules to allow priests to bless same-sex couples, a significant advance for LGBT people in the Roman Catholic Church. The ruling was seen as the Vatican taking a more liberal stance towards gay Catholics, which has been adopted by Pope Francis since his election in 2013.
Some have argued that the milestone decision by the Vatican directly contradicted the church’s stance on gay marriage and homosexuality, and the ruling showed that the Catholic Church was softening its position on the matter.
LATEST DEVELOPMENTS:
・ Ukraine slams Pope for urging country to raise 'white flag' with Russia
・ ‘He’s done wonderfully well’: Queen’s ex-chaplain praises under-fire Pope for ‘white flag’ Ukraine comment
・ Traditional Catholics ‘persecuted’ as Pope Francis clamps down on ‘loyal’ Church-goers
In the document published on April 8, the Vatican comes to the defence of gay Catholics and criticises the criminalisation of homosexuality in some countries.
“It should be denounced as contrary to human dignity the fact that, in some places, not a few people are imprisoned, tortured, and even deprived of the good of life solely because of their sexual orientation,” it said.
Last year, the Pope also said that transgender people could be baptised in the Catholic Church as long as doing so did not cause scandal or “confusion”.
However, the Pope has previously called gender theory an “ugly ideology” that is the “worst danger” facing humanity today.
The Catholic Church also reiterated its tough stance on the topics of surrogacy, abortion and euthanasia. The declaration said surrogate parenting violates the dignity of both the surrogate mother and the child, urging a global ban.
Their gender theory stance was slammed by some LGBT groups. Francis DeBernardo, the executive director of New Ways Ministry, an American organisation that campaigns for gay Catholics, said: “The Vatican is again supporting and propagating ideas that lead to real physical harm to transgender, non-binary and other LGBTQ+ people.”
He added that the text demonstrated a “stunning lack of awareness of the actual lives of transgender and non-binary people”.
Mara Klein, a nonbinary, transgender activist, said: “The suggestion that gender-affirming healthcare — which has saved the lives of so many wonderful trans people and enabled them to live in harmony with their bodies, their communities and (God) — might risk or diminish trans people’s dignity is not only hurtful but dangerously ignorant.”

Wednesday, April 10, 2024
Military doctor: transgender surgery uptick paid for with us tax dollars.
- by: Tracy Beanz

Read our latest news on any of these social networks!
Get the latest news delivered daily!
We will send you breaking news right to your inbox
Recent Articles
Recommended
Critics blast ny’s proposed ‘equal rights amendment’ they say strips parents of their rights over kids’ transgender surgery.
- View Author Archive
- Email the Author
- Get author RSS feed
Contact The Author
Thanks for contacting us. We've received your submission.
Thanks for contacting us. We've received your submission.
Critics are raging against New York’s proposed “Equal Rights Amendment,” claiming the Nov. 5 ballot measure could curb the rights of parents when it comes to allowing minors to undergo gender reassignment surgery.
New York voters don’t yet know much about the particulars of the ERA, which could codify abortion rights in the state constitution — advanced by Gov. Kathy Hochul and Democrats who run the state legislature.
The broad language of the proposal — dubbed Proposition One — has sparked a fierce debate over what could happen if it gets passed, with opponents claiming it’ll lead to kids possibly being able to get serious medical procedures without their parents’ OK and allow transgender females to compete in women’s sports.
“Proposition One would strip the legal rights of parents with school age children to know about crucially important things happening with their kids, including controversial gender transformation procedures” the Coalition to Protect Kids said in a statement.
“Schools would be required to permit biological males to compete on girls’ sports teams if voters approve this amendment.”
The proposal asks voters whether they support or oppose adding language to the constitution that people cannot be denied rights based on their “ethnicity, national origin, age, and disability” or “sex, including sexual orientation, gender identity, gender expression, pregnancy, pregnancy outcomes, and reproductive healthcare and autonomy.”
Coalition to Protect Kids NY Executive Director Greg Garvey said the ERA should instead be called “The Parent Replacement Act,” because it “opens the floodgates” for the government wielding more authority over children than their parents on some of the most important decisions of their lives.
“Any decent lawyer will take one look at the Proposition One language and say, ‘you’ve got to be kidding me,’” said Garvey.

“This ballot initiative is written so broadly and so poorly that it could cause irreparable harm to children and families,” he added.
“Governor Hochul and her woke Albany colleagues have a lot of explaining to do.”
The group’s website includes a video saying a school could help a 7-year-old girl “try life as a boy” and help her transition without her mother “ever knowing” under the amendment, adding, “Do you think that’s OK?”
The Coalition to Protect Kids also claims that laws that determine the legal age to purchase and/or consume alcohol or cannabis, elder abuse and statutory rape could all be weakened because they might arguably “‘discriminate’ based on age.”
The group New Yorkers for Equal Rights denied that the amendment strips parents of their rights.
“These claims simply aren’t true. This amendment is about making sure our fundamental rights and reproductive freedoms are protected and never at risk of becoming a political football,” said Sasha Ahuja, campaign director of New Yorkers for Equal Rights.

The pro-amendment group, in a statement Monday, also said, “If passed, the NY ERA would provide the most comprehensive list of protected categories of any state in the country — safeguarding New Yorkers’ rights, as well as serving as a model for other states.”
Members of the pro-ERA group include 1199SEIU United Healthcare Workers East, Planned Parenthood, North Star, New York Immigration Coalition, the Civil Liberties Union, NEW Pride Agenda, National Institute for Reproductive Health Action Fund, NAACP, Make the Road New York and New York State United Teachers.
New York already has among the strongest abortion laws in the country and long been a pro-choice, with critics questioning whether such a controversial issue belongs in the constitution.
“It’s an ‘anything goes’ amendment,” said state Conservative Party chairman Gerard Kassar, whose party will campaign against the ERA.
He also said Democrats are looking to “change the conversation” away from problems they own — such as the migrant crisis and crime.

A lawsuit has been filed in Livingston County Supreme Court claiming that the legislature approved the proposed amendment going to the voters before getting a legal opinion from state Attorney General Letitia James’ Office.
There’s also been a recent public backlash in New York against permitting trans females from competing in women’s sports, leading to a controversial ban in some sporting venues in Nassau County.
Even one of the world’s most famous transgender females — Caitlyn Jenner — the former 1976 Olympic decathlon champion as Bruce Jenner — is opposed.
Additional reporting by Vaughn Golden
Share this article:

Advertisement

Bangkok, Thailand – Thanadech Jandee is thrilled that Thailand’s marriage equality bill, allowing same-sex couples to marry, is moving closer to becoming law.
Thanadech, who was born biologically female and had gender reassignment surgery to identify as male last year, lives with his girlfriend and her son from a previous relationship.
Keep reading
Uganda’s constitutional court rejects petition against anti-gay law, trump, biden clash over transgender day of visibility falling on easter, thai parliament passes same-sex marriage bill, two bar workers arrested in russia’s first lgbtq ‘extremism’ case.
“I want the equal marriage law to be passed. It will make my family complete like any other family of men and women,” the 34-year-old Grab delivery driver in Bangkok told Al Jazeera.
But along with many LGBTQ activists, Thanadech worries about the bill’s terminology.
Activists say using “parents” and “mother and father” in legal terms will affirm those who identify as LGBTQ on equal terms with other couples.
But efforts to get the wording into the bill have so far been unsuccessful.
The proposed marriage equality law will label marriage as a partnership between two individuals, instead of a man and a woman or a husband and a wife. Couples will have full rights, including receiving medical treatment, tax initiatives, inheritance rights and the right to adopt children.
“I just want to do whatever it takes to have rights that normal men and women have,” Thanadech said.
Thailand’s parliament moved closer to legalising same-sex marriage after the Senate approved the bill at its first hearing on Tuesday. The previous week, Thailand’s lower house approved the bill nearly unanimously – only 10 of the 415 sitting lawmakers did not vote in its favour.

The bill will be examined by the Senate vetting committee before two more readings, scheduled for July. The final step is for Thailand’s king to sign and approve it.
“It’s a cause for celebration,” Mookdapa Yangyuenpradorn, a Thailand human rights associate at Fortify Rights, told Al Jazeera.
“[But] it is important to ensure that the more inclusive and gender-neutral language “parents” is included in future revisions to prevent any discriminatory application of the Civil and Commercial Code. We remain steadfast in our call for full protection and recognition of LGBTI+ rights,” Mookdapa added.
In contrast to many other Asian countries, Thailand has long allowed for same-sex celebrations , including Pride. It also holds international transgender beauty pageants and is a global leader in gender reassignment surgery. In 2015, it passed the Gender Equality Act, aiming to protect all people from gender-based discrimination.
But despite having one of the most open LGBTQ communities in the Asian region, Thailand still provides no legal protection to transgender people.
Ariya Milintanapa was born biologically male but identifies as a trans woman. The 40-year-old is a parent to two boys with her husband Lee, whom she married in the United States in 2019. Ariya was the guardian for her younger brother and because of her birth gender as male, was allowed to adopt her now eight-year-old brother as his “uncle”. Their eldest son is a 10-year-old from her husband’s previous relationship.
She says the law makes it “difficult” for them to live as a family.
“It causes a lot of problems like travelling and insurance. We applied for one school but they kept asking for [legal proof] that we were “mum” and “dad”. Even bullies say [to our children] that their mum is different,” Ariya told Al Jazeera.
“We hope to hear the next move where the focus is mainly about the child’s benefit more than the concern of birth gender,” Ariya added.
Bullying risk
Without identifying same-sex and LGBTQ couples as “parents”, there could be a rise in discrimination and bullying between children, according to Nada Chaiyajit, a LGBTQ advocate and law lecturer at Mae Fah Luang University.
“If the law does not recognise “parents” status, it would potentially create discrimination in a form of social bullying,” Nada told Al Jazeera. “Your mother is not your real mother and is a f*****, something like that.”
Nada says it is unclear what other legal rights those who identify as LGBTQ will receive if they are not legally identified as parents and campaigners remain determined the term be described in the law.
“A lot of work is needed to be done. At least we still have some chances to work with the Senate to bring back the word “parents” to complete our rights to family establishment. We will keep pushing,” Nada added.

Emilie Palamy Pradichit, the founder of the Manushya Foundation, a human rights organisation in Bangkok, say the wording means the proposed law is not truly for marriage equality.
“It means only people of the same sex recognised as father or mothers will be allowed to marry, because it is a same-sex bill, not a truly marriage equality bill. For example, if a transgender woman wants to marry a non-binary person… they won’t be able to. Thailand does not have a legal gender identity law – that’s a core issue,” she told Al Jazeera.
That could change in the future though. According to one Thai MP, a draft gender recognition law is in the works.
“Draft gender recognition law… Intentional gender identity… I’m working on it. To allow people to define themselves in various ways to define their own gender. It is something that must be continuously pushed forward,” Tunyawaj Kamolwongwat, a lawmaker with the Move Forward Party posted on the X platform.
For now, Thailand’s focus remains on the marriage equality bill.
It has taken more than a decade of campaigning to get to this point and the draft legislation holds widespread political support. Prime Minister Srettha Thavisin, who became leader after elections last year has championed it.
“It is considered the pride of Thai society that together [we] walk towards a society of equality and respect diversity,” the Thai Prime Minister wrote on Twitter, formerly X, last week.
If the bill does become law, Thailand will become the first country in Southeast Asia to legalise same-sex marriage – and the third in the wider Asian region after Taiwan and Nepal.
Thailand has a population of more than 71 million people and market research firm Ipsos Group says about 9 percent of Thai people identify as LGBTQ.
Since the first reading of the law in December, enquiries about wedding ceremonies by the community have surged.
“There’s definitely an increase of interest. So that would be about like 25 percent of all the bookings. A lot of couples are looking to celebrate,” Wannida Kasiwong, the owner of Wonders and Weddings in Thailand, told Al Jazeera earlier this year.

IMAGES
VIDEO
COMMENTS
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
Nicolas AsfouriAFP/Getty Images. N early 60 years ago, Johns Hopkins Hospital opened a first-of-its-kind clinic to provide gender-affirming surgery. The Gender Identity Clinic blazed a new trail ...
Development. Gender-affirming surgeries were performed during the 1920s and '30s, primarily in Europe. These procedures were experimental and not extensively accepted by the medical community. At the time, it was widely believed that gender identity was immutable and that surgery could not alter it.
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
Overview. Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender. A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery. The term "transexual" was previously used by the medical community to ...
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria. Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX ...
Because sex reassignment surgery is just one step for transitioning people, the Comprehensive Gender Services Program has access to providers for mental health services, hormone therapy, pelvic floor physiotherapy, and speech therapy. Surgical procedures are done by a team that includes, as appropriate, gynecologists, urologists, pelvic pain ...
This procedure involves changing the clitoris into a penis. A person will receive hormone therapy before the surgery to enlarge the clitoris for this purpose. During the procedure, the surgeon ...
His confidence in this new approach is the result of nearly three decades of expertise and innovation in SRS and urogenital reconstructive surgery, which includes 600 male-to-female vaginoplasties, 900 female-to-male metoidioplasties, 300 female-to-male phalloplasties, and the co-development of a penile disassembly technique for epispadias repair.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed. A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia ...
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
Among other changes, the proposed rules would eliminate the requirement that transgender individuals on Medicaid must wait until the age of 21 to receive surgery. Individuals over the age of 18 and minors — with informed parental consent — would be eligible. Such changes are in line with current thinking among academics and physicians in ...
Factors that have been found to contribute to "minor regret" after gender-affirming surgery include postsurgical factors such as pain during and after surgery, surgical complications, poor surgical results, loss of partners, loss of job, conflict with family, and disappointments that various expectations linked to surgery were not fulfilled ...
Long-term overall body congruency score was 89.6. Improved mental health outcomes persisted following surgery with significantly reduced suicidal ideation and reported resolution of any mental health comorbidity secondary to gender dysphoria. Conclusion: Gender-affirming surgery is a durable treatment that improves overall patient well-being ...
Sex and sexual health tips for transgender women after gender-affirming surgery. Sex after surgery. Achieving orgasm. Libido. Vaginal depth and lubrication. Aftercare. Contraceptions and STIs ...
Key Points. Question What are the temporal trends in gender-affirming surgery (GAS) in the US?. Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
1. Introduction. Transgender and gender non-binary individuals are a growing demographic worldwide (See Appendix A for glossary of terms). An estimated 0.7% of the youth in the United States (ages 13-17) identify as transgender [].Over the last decade, access to gender-affirming specialized surgical care has increased among adolescents and young adults.
In addition, bias can occur because patients might restrain from expressing regrets due to fear of being judged by the interviewer. Moreover, the temporarity of the feeling of regret in some patients and the variable definition of regret may underestimate the real prevalence of "true" regret. ... Male-to-female sex reassignment surgery ...
Patients who undergo gender-affirming genital surgeries may present to the emergency department for their postsurgical complications. In this paper, we briefly describe the transfeminine and transmasculine genital procedures, review the diagnosis and management of both common and potentially life-threatening complications, and discuss the criteria for hospitalization and time frame for ...
The Pope has condemned gender reassignment surgery, saying it represents a "grave threat to the dignity of a person". In a text dubbed "Dignitas Infinita" (Infinite Dignity), the Vatican ...
However, understand this: with increasing frequency, the US Military is performing gender reassignment surgery—up to and including the removal of genitals and the creation of fake ones- on active duty military, and you are paying for it. Not only that, but they are also covering what would be considered "elective" cosmetic procedures for all ...
Critics are raging against New York's proposed "Equal Rights Amendment," claiming the measure will curb the rights of parents when it comes to allowing minors to undergo gender reassignment surgery.
The Vatican's declaration that gender-affirming surgery and what it calls gender "ideologies" violate human dignity is disappointing and "deeply harmful," LGBTQ+ rights advocates in Canada say. The Vatican's doctrine office issued a 20-page declaration Monday that describes "gender theory" and surrogacy as "grave violations of human dignity" that are on par with abortion, euthanasia, war and ...
Puberty blockers and hormones were given to children as young as 12. Once they were 17, many were then transferred to adult services for gender reassignment surgery, such as breast removal.
It also holds international transgender beauty pageants and is a global leader in gender reassignment surgery. In 2015, it passed the Gender Equality Act, aiming to protect all people from gender ...