- Reference Manager
- Simple TEXT file

People also looked at
Editorial article, editorial: doing critical health communication: a forum on methods.

- 1 Department of Communication, University of Cincinnati, Cincinnati, OH, United States
- 2 Department of Communication, University of South Florida, Tampa, FL, United States
Editorial on the Research Topic “Doing” Critical Health Communication. A Forum on Methods
The assumed premise of health communication research is straightforward: improving communication processes across all health-related domains. Communication between providers and patients, public health messaging, health literacy training, culturally competent healthcare, health status sharing in families, workplaces, and small groups can all fit within the broad definition of health communication. However, philosophical differences in what communication means–or for that matter, what health means–result in a complex, multi-paradigmatic field of study. For instance, viewing communication primarily as information transfer leads to a different trajectory of research and scholarship than a view of communication as the constitutive process of meaning making. Similarly, conceptualizing health as a means of achieving social concordance or even control vs. as a site of social struggle leads us different places.
Within the well-established field of health communication, a preponderance of published research continues to be rooted in communication models that derive from social psychology and information science. Consequently, emerging issues, new theoretical and methodological directions, and ethical challenges define the landscape of the field. For instance, we have witnessed a significant rise in interpretive research focusing on the social construction of meaning. However, we believe there is more work to do in nurturing critical health communication [CHC] perspectives.
The primary rationale for this research topic was to describe multiple ways to engage in CHC methodologies through a set of short, “how-to” articles. The original impetus were two roundtable panels (convened at successive National Communication Association conventions) to gauge the trajectory of CHC in the decade after Zoller and Kline’s review of the contributions of interpretive/critical health communication research in the Annals of Communication (then called Communication Yearbook). One of the things we recognized in those panel discussions was that CHC was still considered a niche sub-discipline or area within health communication, and consequently, students and young scholars who were interested in CHC often did not receive formal guidance in this area, notwithstanding the dramatic increases in CHC-fueled work being published in our disciplinary journals, and/or presented at conferences. Even for scholars familiar with the intellectual terrains of poststructuralism, postcolonialism, the “linguistic turn,” hermeneutics, phenomenology and critical theory, there was a gap in documenting these theoretical concepts into concrete ways of “doing” health communication research.
In calling for papers, we urged potential authors to ask, “What makes your work critical?” How do methodological practices illuminate the role of critique? What are the ontological and epistemological implications of doing CHC? How is CHC related to critical praxis? How does “doing” critical work engage with/deviate from the broader interpretive move toward discourses/texts? What do recent provocations around the “return to the material” in Communication scholarship mean for CHC researchers? How is CHC situated to respond to widening racial, gendered and other social disparities in health across the globe? Finally, how do CHC researchers situate their own privilege and conceptualize embodied risk through their work? The fourteen articles that comprise this collection, selected from the 30 + abstracts submitted for consideration, and shortlisted from 19 full-text article submissions) respond to this prompt in unique, individual ways.
Of the fourteen articles, five report on new/original research, four offer ‘Conceptual Analysis’ or brief essays on a particular concept. Another four are short “Perspectives” on varying issues concerning CHC, and one is a Brief Research Report. As to our remit of a “how to” for CHC, the articles offer pedagogical insights on CHC methods in a variety of ways.
Zoller and Kline’s 2008 drew attention to both shared attributes and key points of difference in interpretive and critical health communication. One of our goals for this topic was to theorize their differences as well as their “blurry edges.” Anne Kerber’s essay addresses longstanding conflicts between a critical “hermeneutic” of suspicion that interrogates relations of power and an affirmative stance that seeks positive models of critical social change.
A second rationale for this collection was to re-establish the disciplinary history of the efforts of CHC scholars. At the abovementioned conference panel discussions and through our own anecdotal experience, we have learnt that the multi-decade project to critique, de-parochialize, globalize and queer the body of the discipline (and consequently, its journals and editorial boards), led by women, scholars of color, LGBTQ scholars, and scholars from the Global South, has not been documented or set into the received intellectual history of the field (in contrast to cognate areas, like critical organizational or critical management studies). This absence influences the diffusion of our work. It also makes it possible for other scholarly collectives, notably our colleagues who coalesce under the “Rhetoric of Health and Medicine” or RHM, whose work we admire, review and support, to largely ignore this history and the contributions of CHC scholars in opening up space for critical/humanist inquiry in this area. In that sense, we seek to make explicit the politics, the pragmatics and the real-life implications of doing CHC work. As a foundational scholar in the area, Heather Zoller’s essay derives from her extensive work in the field, and outlines how the politics of academic training, visibility, and publishing intersect in pursuing a trajectory of critical health communication research. This essay is an excellent entry point for this research topic.
Essays in this collection model different forms of critical analysis. For instance, Carter and Alexander’s original research is an exemplar for connecting race, class, historical positioning, and health communication practices. Their interview-based original research highlights the voices of African American farmers, revealing how their issues and interests have been silenced in discussions about United States farming. They connect these erasures with broader political discourses about diet and health disparities.
Khan et al model critical ethnographic analysis through their study of Ashodaya Samithi , a sex worker collective in Mysore, India. They offer narratives that highlight resistance and alliance building that are imperative in order to invert dominant discriminatory notions of nationhood and citizenship that have and continue to violate health and rights of marginalized communities. Much of the critical work in health communication has emerged from the global South, espousing a critique of the West-dominated nature of communication theorizing and global health policies.
Dutta and his team provide a primer in a Marxist approach to critical theorizing, with attention to the global subaltern. The authors draw from their embodied culture-centered research engaging in activist interventions that aim to disrupt Whiteness and associated capitalist and colonial logics. The authors challenge us to consider what counts as resistance organizing in ways that provide an interesting counterpoint to Kerber’s essay. Such tensions in what counts as “critical” research in health communication continues to be an important fault line in our field. Metatheoretical differences in conceptualizing the role of the critic in health communication manifest in methodological and pragmatic differences in what research looks like. One such difference is in the practice of what some scholas call ‘critical reflexivity’
Critical reflexivity–or the continual introspection of how analysis reveals the motivations of the analyst as much as it says something about that which is analyzed–is a governing principle guiding the ethical conduct of critical research. Rebecca de Souza’s essay interrogates how the literature on critical reflexivity–what she calls the “self-other” hyphen—predicates a white researcher introspecting on their ethical analytical practices as they work in communities of color. However, flipping the trope, de Souza’s essay offers a fascinating look at what happens when a person of color navigates analysis of predominantly white spaces. Through an analysis of the responses and challenges to her work by peer reviewers, commentators and colleagues, de Souza offers a window into the “micro-politics” of knowledge production. Her work offers practical suggestions for scholars of color to challenge the hegemonic assumptions that emerge from working in white spaces.
Similarly, Leandra Hernandez and Sarah De Los Santos Upton provide an exemplar of the power of critical reflexivity and the need for critical praxis through social justice activism. The essay blends discussion of their research and activist work, describing the intersectional approach they have taken to health communication research at the United States-Mexico border. Situated as Chicana feminists, they have investigated gendered, racial and class constructions in the context of reproductive justice, violence, and immigration. The authors describe how their work has necessitated a blending of theoretical and methodological approaches.
Critical reflexivity is also an important tool in Smita Misra’s essay , which centers around the concept of migrant trauma. As encapsulated by their experiences in a participatory theater project that purportedly allowed for refugees to cope with trauma, Misra offers a critical reflexive account of how well-meaning, “participatory”/critical projects can offer limited/constraining understanding of the lives of the vulnerable populations they serve.
Nicole Hudak’s essay discusses challenges in publishing research that does not fit within post-positivism, calling for more advocacy of qualitative and critical research. In addition, the essay challenges all of us to interrogate reviewer practices that reinforce heteronormativity and create barriers to research addressing LGBTQ + health care experiences. This turn to embodied identity is further crystallized in Ellingson’s work, which theorizes embodiment more centrally.
Embodiment becomes sensorial in Laura Ellingson’s essay. Sensual intersubjectivities that blend the senses, the motors, and the material, Ellingson explains, are crucial to critical health communication research methods because interrupting discourses on/of what makes certain bodies/citizens ‘healthy’ and ‘normal’ calls for a sustained practice of sensorial reflexivity.
If critical reflexivity is one way to redefine the “blurry edges” between interpretive and critical approaches, then Sastry and Basu’s essay offers a methodological warrant to use critical reflexivity as a practicable method for analysis in health communication. The essay elucidates an approach blending culture-centered analysis, abductive analysis, and critical reflexivity in a post-COVID world. Departing from their ethnographic work in the culture-centered tradition, the authors offer a framework to analyze health discourses using the early responses to COVID-19 as an exemplar.
Several essays offer methodological innovations in the doing of critical health research. Sarah MacLean and Simon Hatcher write about the walkthrough method in their essay. The walkthrough method offers a viable process to scrutinize the architecture of a health technology tools –- the BEACON Rx Platform in their case –in terms of expected use and consequent implications of access and equity. This method also creates spaces for questioning the discourses inherent in health technologies that frame dominant understandings of how to be in “good” health.
Wendy Pringle provides a new methodological tool for critical health communication scholars, particularly those interested in textual/rhetorical analysis and policy discourses. She adapts the “What's the Problem Represented to be?” (WPR) approach from the field of discursive policy analysis. The paper uses the illustrative example of the legalization of medical assistance in dying in Canada. The WPR method facilitates attention to evolving discourses of problem constructions, and she describes the implications for people with disabilities, including what is said and what is left unspoken. The method addresses social change, including policy critique, and advocacy as a form of resistance.
In our call for papers, we hoped to collectively articulate (and complicate) what exactly we mean by “critical” in CHC. In addition to the models we have discussed, Kim Kline and Shamshad Khan call attention to the need for CHC scholars to speak to both internal and external stakeholders. Their essay signposts the possibilities and challenges for CHC scholars to engage in “transdisciplinary” collaborations within and without the discipline of health communication.
Speaking of collaborations, this research topic would not have been realized without the collaborative efforts between the contributing authors, the editorial team, and most importantly, the large number of reviewers who volunteered their time and intellectual commitment to this cause–not to mention adapting their reviewing practices for Frontiers. While open-access, transparency, and publication of reviewers’ names with published articles signals the timely democratization of the publication process, the concomitant “bot-tification” of the process was a learning curve for several Communication scholars–us included.
As we conclude this editorial, the United States has more than 13 million confirmed cases of COVID-19, and some estimates suggest that the death toll might reach 5,00,000 by the summer of 2021. Debates around masks, vaccines, technology transfers, economic impacts and racial and income inequalities related to the pandemic continue, painfully demonstrate the need for more research in how mechanisms of power/control/inequality shape individual and collective experiences of health and illness.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Keywords: health communication, critical health studies, research methods, reflexivity, critical health communication
Citation: Sastry S, Zoller HM and Basu A (2021) Editorial: Doing Critical Health Communication: A Forum on Methods. Front. Commun. 5:637579. doi: 10.3389/fcomm.2020.637579
Received: 03 December 2020; Accepted: 24 December 2020; Published: 25 January 2021.
Edited and reviewed by:
Copyright © 2021 Sastry, Zoller and Basu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shaunak Sastry, [email protected]
This article is part of the Research Topic
'Doing' Critical Health Communication: A Forum on Methods
Health Communication Research Paper Topics

Community Health Issues
- Change Agency
- Collective Efficacy
- Community Mobilization
- Community Organizing as a Research Approach
- Community Participation
- Community-Based Participatory Research
- Comprehensive Community Initiatives
- Conflict Management: Health Professionals
- Cultural Differences
- Health Activism and Public Health
- Immigrant Families
- Media Literacy
- Nature, Environment, and Sustainability
- Organizational and Public Policy Barriers
- Readiness Assessments
- Rural Health Communication
- Sex Workers
- Social Action, Types of
- Social Aggregates
- Social Capital
- Social Determinants of Health
- University–Community Relationships
End-of-Life Issues
- Advance Directives
- Advanced Aging Communities
- Bereavement
- Communicating Bad News
- Death and Dying
- Family Communication and End of Life
- Final Conversations
- Palliative Care
- Pediatric Hospice Care
- Rhetoric: Death with Dignity
- Staff Communication in Nursing Homes
- Terminality
Evaluation of Health Intervention, Education, and Communication
- Content Analysis
- Data Mining
- Focus Groups
- Logic Models and Program Evaluation
- Measurement Problems
- Message Quality Measurement
- Mixed Methods of Evaluation
- Modeling Development and Testing
- New Technologies and Intervention Evaluation Methodology
- Qualitative Methods of Evaluation
- Quantitative Methods of Evaluation
- Risk Communication
- Risk Society
- Setting Objectives in Health Communication and Intervention
- Statistical Challenges in Evaluation
Everyday and Family Health Communication Issues
- Adolescent Substance Abuse Prevention
- Alcohol and Health Decision Making
- Childhood Injury Prevention
- Communication with Families
- Consequences of Health Literacy
- Consequences of Stigmatization
- Coping with Stigmatization
- Courtesy Stigma
- Cross-Generational Health Communication
- Decision Making
- Disabilities and Family Relationships
- Everyday Health Communication
- Familial Roles in Health Communication
- Family Caregiving
- Family Meeting
- Family Planning
- Family Relationship to Health
- Grief and Loss
- Health Communication with Children
- Health Education
- Health Literacy and Numeracy
- Health Transition and Family Communication
- Illness Identity
- Improving Health Literacy
- Integrating Health Literacy into Health Care Systems
- Measurement of Health Literacy
- Model of Health Literacy
- Mother–Daughter Dyad Communication
- Online Health Literacy
- Religion and Spirituality
- Social Construction of Disability
- Social Identity
- Social Influence of Everyday Health Communication
- Social Norms
- Social Support and Cardiovascular Health
- Social Support and Health
- Social Support and Support Groups
- Social Support Interventions
- Stigma Reduction
- Stigmatization
- Stigmatization, Labels, Marks, and Peril
- Surrogate Decision Makers
- Teen Pregnancy
- Types of Social Support
- Unintended Effects of Health Communication
- Health Campaigns
- Advertising of Dietary Supplements
- Advertising of Food
- Advertising of Over-the-Counter Drugs
- Advertising of Prescription Drugs
- Affordable Care Act
- Assessment of Health Campaigns
- Awareness and Instruction Strategies
- Campaign Effects Versus Effectiveness
- Campaigns in Developing Countries
- Channels and Formats
- Communication Complex
- Communication for Behavioral Impact
- Crisis Communication
- Disease Prevention
- Dissemination
- Emotion Appraisals Regarding Risk
- Evidence Role in Health Campaigns
- Formative Evaluation
- Governmental Regulation of Advertising
- Incentive Appeals
- Influential Source Messengers
- Integrated Marketing Mix
- Interpersonal Communication and Mass Media Health Campaigns
- Message Design
- Message Sidedness
- Message Tailoring
- Optimistic Bias
- Perceived Threat
- Program Strategies: Campaigns
- Public Service Announcements
- Risk Communication and Food Safety
- Risk Perceptions
- Risk-Taking Behavior
- Segmentation of Health Campaigns
- Sensation-Seeking Targeting
- Social Marketing
International and Diversity Issues in Health Communication
- Conflict and Negative Health Effects
- Cultural Sensitivity
- Discrimination or Bias in Health Care
- Disenfranchised Populations
- Ethnic Diversity in Health Care Settings
- Health Disparities in Clinical Interactions
- Health Disparities on Communal Level
- Human Rights
- Immigrant Populations
- Intercultural Health Communication
- Islamic Healing
- LGBT Issues
- Marginalized Populations
- Overall Health Disparities
- Personal Influences on Health Disparities
- Public Health Intervention in Multicultural Communities
- Relational Influences on Health Disparities
- Solutions for Health Disparities
- Structure-Centered Approach
Health Information
- Defensive Reactions to Health Messages
- Digital Divide
- Disclosure and Family Health History
- Disclosure and Medical Errors
- Disclosure and Providers and Patients
- Emotion and Information Seeking
- Explaining Illness
- Expressive Writing and Health
- Health Citizenship
- Health Communication Curricula
- Information Nonseeking
- Information Seeking
- Information Sharing
- Need for Explaining Illness
- Online Health Information Seeking
- Online Health Information Sharing
- Opinion Leaders
- Psychosocial Determinants of Health Information-Seeking Behavior
- Social Determinants of Health Information-Seeking Behavior
- History of Health Communication
- Basic Concepts of Communication
- Communication Across the Lifespan
- Communication Networks
- E-Health Defined
- Evolution of Medicine as Business
- Health Information Channels
- Patient and Relationship-Centered Communication and Medicine
- Personalized Medicine
- Postcolonial Studies and Health
- Premises of Health Communication
- Science Communication
- Translational Research
Media Content
- Advertising Unhealthy Foods to Children
- Body Images and Portrayals
- Celebrity Cancer Announcements
- Celebrity Endorsements
- Critical Analysis of Media and Health
- Digital Media
- Entertainment–Education
- European Approach to Entertainment–Education
- Health Blogging
- Health Consequences of Pornography
- Health Journalism
- Health Promotion
- Hollywood and Public Relations Approach to Entertainment–Education
- Ideological Hegemony
- Impact of Media Content
- Institutional Processes and Competing Agendas
- Interpretation and Effects of Disclaimers
- Media and Health Disparities
- Media and Quality of Health Information
- Media Content: Magazines
- Media Content: Newspapers
- Media Content: Other Print
- Media Content: Televised Entertainment
- Media Content: Televised News
- Media Coverage of Genetically Modified Organisms
- Media Depictions of Disability
- Media Depictions of Medical Workers
- Media Depictions of Mental Illnesses
- Moderating Variables and Audience Effects
- Music in Health Behavior
- Obesity and Mass Media
- Pathways to Change Tool
- Public Relations and Health Journalism
- Public Relations and Health Promotion
- Public Relations and Social Media
- Reaching Audiences
- Role of Involvement in Entertainment–Education
- Social Marketing and Community Change Perspective
- Twitter and Public Health
Organizational Issues and Health Policy
- Adult Children of Alcoholics
- American Medical Association
- Conflict Management and Health Professionals
- Department of Health and Human Services
- Health Care Teams
- Health Policy
- Healthy People Initiative
- Hospital Governance Culture
- Informed Consent
- Interdisciplinary Health Services Research
- Mediated Health Campaigns
- Multicultural Campaigns
- National Action Plan to Improve Health Literacy
- National Cancer Institute
- National Institutes of Health
- National Library of Medicine
- National Medical Association
- Organizations and Health
- Patient Privacy
- Politics and Political Complexities
- Public Relations and Health Care Organizations
- Role Stress
- Segmentation and Public Relations
- Stress and Burnout
- Stress and Burnout: Emotional Labor
- Stress and Burnout: Home–Work Conflict
- Three Community and Five Cities Projects
- S. Centers for Disease Control and Prevention
- Working Well
- World Health Organization
Provider–Patient Interaction
- Adherence to Medical Regimens
- Anger Appeals
- Clinical Trial Participation
- Coding Health Interaction
- Collaborative Decision Making
- Contested Illnesses
- Conversation Analysis
- Decision Making Between Support Providers and Persons with Disabilities
- Dependent Variables Derived from Critical Health Outcomes
- Difficult Patients
- Discourse and Health
- Doctor–Patient Communication
- Emergency Rooms
- Emotions and the Medical Care Process
- Face and Politeness
- Health Care Environment
- HIV Test Counseling
- Identification
- Interactional Context and Intervention
- Interpersonal Communication Skills
- Interpreters and Language
- Interviewing in the Health Care Context
- Language and Negation Bias in Doctor–Patient Interaction
- Language Brokering
- Listening in Health Care Interactions
- Malpractice Litigation
- Medical Outcomes
- Nonverbal Communication in Health Care Settings
- Open Dialogue Approach
- Overtreatment and Overreliance on Diagnostic Testing
- Pathways to Health Outcomes
- Patient Activation
- Patient Education and Hospital Discharge and Readmission
- Patient Empowerment
- Patient Navigators and Family Advisors
- Patient Safety
- Patients and Communication Skills Training:
- Prescribing Medications
- Providers and Communication Skills Training and Assessment
- Quality of Life as a Health Outcome
- Satisfaction
- Shared Mind in Collaborative Decision Making:
- Supportive Listening
- Uncertainty in Collaborative Decision Making
- Public Health Communication
- Biopreparedness and Biosecurity
- Climate Change
- Communication of Scientific Complexity
- Developmental Health
- Disaster Relief
- Emergency Preparedness and Response
- Environmental Health
- Evolution of Public Health Communication
- Flu Vaccine Rhetoric
- HIV/AIDS Prevention
- Immunizations
- Memorable Messages
- Mother-to-Child HIV/AIDS Transmission
- Newborn Care
- Online Health Information Credibility
- Priming in Health Campaign Messages
- Public Engagement and Science Policy
- Public Health and Academic Partnerships
- Public Understanding of Research
- Public Understanding of Science
- Research in Environmental Health
- School Health
- Science Literacy
- Sexual Health
- Warning Labels
- Warning Labels on Alcohol
- Warning Labels on Cigarettes
- Warning Labels on Prescription Drugs
- Women’s Health
- Work Site Safety
Specific Health Issues/Providers
- Child and Spousal Abuse
- Acupuncture
- Age-Related Hearing Loss
- Alternative and Complementary Medicine
- Alzheimer’s Disease
- Ayurveda, Yoga, and Meditation
- Bioterrorism
- Birth Control and Contraception
- Breast Cancer
- Breastfeeding
- Bullying and Cyberbullying
- Cancer Risk Communication
- Cancer Survivorship
- Chronic Diseases
- Communication Interventions
- Contraception
- Dialectical Behavioral Therapy
- Distance Caregiving
- Drug and Alcohol Abuse Minimization
- Eating Disorders
- Emergency Health Communication
- Enhancement
- Gambling Addiction
- Heart Health
- HIV/AIDS and Disclosure Dilemmas
- HIV/AIDS Treatment
- HIV/AIDS, Condom Use, and Meanings
- Holistic Medicine
- Human Papillomavirus
- Influenza A Virus Subtype H1N1
- Integrative Medicine
- Internet Addiction
- Language, Metaphors, and Social Construction of HIV/AIDS
- Malaria and Mosquito Nets
- Male Circumcision
- Mammography
- Meanings of HIV/AIDS Test
- Mental Health
- Military Health
- Military Sexual Assault
- Multilevel Interventions
- Neurorhetoric
- Nutrition and Diet
- Oral Health and Dentistry
- Organ Donation
- Pharmacists
- Physical Activity and Weight
- Post-Traumatic Stress Disorder
- Prenatal Health Promotion
- Prostate Cancer
- Responses to Slow-Motion Technological Disaster
- Severe Acute Respiratory Syndrome
- Sex Education
- Sexual Assault
- Sexually Transmitted Disease Prevention
- Skin Cancer and Sun Safety
- Skin Cancer and Tanning
- Social Determinants of Disparities in HIV/AIDS
- Transitions, Health Effects, and Support
- Traumatic Brain Injury
- Tuberculosis
- Vaccinations
Technology and Health Communication
- Biomedical and Health Informatics
- Bundled Interventions
- Communication Technology Theoretical Frameworks
- Computer-Tailored Interventions
- Customization as Tailoring 2.0
- Digital Personal Health Records
- Electronic Medical Records
- Free-Standing Computer Kiosks
- Geographic Information Systems Technology
- Internet and Information Acquisition
- Medical Body Implants
- Mobile Health
- New Reproductive Technologies
- Online Focus Groups
- Online Health Information Exchange and Privacy
- Online Support Groups
- Online Support Groups Advantages and Disadvantages
- Persuasive Technologies for Health
- Secondary Data Analysis
- Social Media
- Technology and Health Outcomes
- Technology Impact on Physician–Patient Dialogue
- Telemedicine
- Virtual Reality Environments
- Weak Tie/Strong Tie Network Support
- Web-Based Delivery
Health Communication Theories, Ethics, and Philosophy
- Acculturation
- Action Tendency Emotions
- Acute Versus Preventive Care
- Affection Exchange Theory
- Agenda Setting
- Amputee Wannabes
- Attribution Theory and Attribution Error
- Biological Citizenship
- Biopower and Biopolitics
- Care Model and Productive Interaction
- Change Approaches
- Communication Accommodation Theory
- Communication Privacy Management Theory
- Communication Theory of Identity
- Community Resilience
- Control Theory
- Critical Approaches
- Cultivation Theory
- Cultural Variance Model
- Culture-Centered Approaches
- Cyberchondria
- Diffusion of Innovations Model
- Double ABC-X Model of Family Stress and Coping
- Dual-Processing Models
- Ecological Perspectives
- Encoded Exposure and Aided Versus Unaided Awareness
- Ethic of Care
- Ethics and Health Campaigns
- Ethics and Health Communication Strategies
- Ethics and New Technologies
- Ethics of Provider–Patient Interaction
- Ethnography
- Ethnomethodology
- Fear Appeals and the Extended Parallel Process Model
- Generative Tensions in Health Communication Theory
- Globalization Theory
- Grounded Theory
- Harm Reduction Theory
- Health Belief Model
- Health Communication Ethics
- Health Locus of Control
- Hofstede’s Dimensions of Culture
- Inconsistent Nurturing as Control Theory
- Inoculation Effects
- Instructional Principles of Risk Communication
- Invisible Disabilities
- Loose Versus Tight Coupling
- Measurement of Social Networks
- Media Complementarity Theory
- Medicalization
- Message Sensation Value
- Meta-Analysis
- Motivational Interviewing
- Multilevel Modeling
- Narrative Engagement Theory
- Narrative Medicine
- Narratives and Barrier Reduction
- Narratives and Health Campaigns
- Narratives and Social Marketing
- Negotiated Morality Theory
- Olson’s Circumplex Model of Marital and Family Systems
- Organization–Public Relations Theory
- O-S-O-R Model
- Perceived Effectiveness
- Phenomenology
- Placebo Effects
- Problematic Integration Theory
- Problem-Based Learning
- Psychological Reactance
- Psychometric Theory and Reliability/Validity of Measures
- Reconceptualized Health Belief Model
- Relational Dialectics Theory
- Relational Health Communication Competence Model
- Rhetoric, Health, and Medicine
- Risk Information Seeking and Processing Model
- Risk Perception Attitude Framework
- Self-Determination Theory
- Self-Efficacy
- Situational Theory and Communication Behaviors
- Social Cognitive Theory
- Social Comparison Theory
- Social Construction of Reality
- Social Construction Perspective on Risk Communication
- Social Judgment Theory
- Social Networks
- Social Networks and Message Delivery
- Societal Risk Reduction Motivation Model
- Sociometric Social Networks
- Structural Violence and Health
- Systems Theory
- Theory of Motivated Information Management
- Theory of Normative Social Behavior
- Theory of Planned Behavior
- Theory of Reasoned Action
- Traditions of Health Communication Theory
- Trait Approaches
- Uncertainty Management Theory
- Uses and Gratifications Theory
- Weick’s Model of Organizing
Organization of the Field
There is no simple or complete way to organize the field of health communication, though several sub-fields have existed depending on one’s research interests, as well as adventitious and historical circumstances. At the individual level, the focus is twofold: (1) how health cognitions affect, and behaviors influence and are influenced by, health communications; and (2) how interpersonal interactions between patients, family members, and providers, and with members of their social network, influence health outcomes. At the organizational level, some have studied the role of communication within health-care systems and how organization of the media and the practices of media professionals may influence population and individual health.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code.
Finally, at the societal level, the focus is on large-scale social changes and the role of communication with such changes. For example, one might examine how strategic communications as well as natural diffusion of information impact individual and population health; or how communication mediates and is influenced by social determinants such as social class, neighborhood, social cohesion and conflict, social and economic policies, and how that impacts individual and population health.
Even as these levels provide a useful organizing framework, two caveats are warranted. First, policymaking and research related to health may affect more than one level. Second, interest in a level of analysis and pursuit of work at one level is not inconsequential. Locating a problem at one level, and studying it at that level, have implications for the kind of policy or practice that is likely to emerge from that research.
Interpersonal Communication
Extensive attention has been given to understanding the consequences of communication between physicians and patients on patient satisfaction, adherence, and quality of life. One theme is who controls the interaction between providers and patients, known as ‘relational control.’ A second theme focuses on the outcomes of patient– provider interactions. Extensive research has documented that patient–provider communication influences patient satisfaction which, in turn, is related to patient adherence and compliance to treatment regimens, ease of distress, physiological response, length of stay in the hospital, quality of life, and health status, among others. Third, researchers have documented stark differences in patient preparation and access, and in care received and health outcomes, between social classes as well as racial and ethnic groups.
The implications of interpersonal interaction in the context of families, friends, co-workers, and voluntary associations on health outcomes have become one of the most dynamic areas of research in health communication. This topic has been pursued from diverse theoretical viewpoints by researchers focusing on social networks, social support, family communications, and social capital based on the researcher’s disciplinary origins and research interests. In addition to social support, social networks can accelerate or decelerate diffusion of new information, and also influence how it is interpreted (Himelboim & Han 2014). Members within networks can serve as role models for lifestyle behaviors such as smoking and obesity. The emergence and spread of the Internet have broadened the scope of interpersonal interaction and its influence in health communication by moderating the limits of geography.
Mass Media and Health
The incidental and routine use of media for news and entertainment serves four functions in health. (1) The informational function is served when casual use of media for news or other purposes may expose the audience to developments on new treatments or new drugs, alert them to risk factors, or warn them of impending threats such as avian flu; (2) media serve an instrumental function by providing information that facilitates action; e.g., in times of natural disasters the audience may learn about places where they should take shelter, and information of this kind allows for practical action; (3) media defines what is acceptable and legitimate, performing a social control function; (4) the communal function is served when media provide social support, generate social capital, and connect people to social institutions and groups.
Information seeking, as a construct, has gained greater currency in recent times as more information on health has become routinely available because of greater coverage of health in the media, the spread of health-related content on the world wide web, or the consumerist movement in health that promotes informed or shared decision-making. It is widely assumed that under certain conditions some people actively look for health information to seek a second opinion, make a more informed choice on treatments, and learn in greater depth about a health problem that afflicts them or their friends or family members.
The most visible and popular means of strategic communications is through health campaigns which have become a critical arsenal in health promotion. A typical health campaign attempts to promote change by increasing the amount of information on the health topic, and by defining the issue of interest in such a way as to promote health or prevent disease. Recent reviews of the vast literature on health campaigns have identified conditions under which health campaigns can be successful (e.g. Noar 2006; Randolph & Viswanath 2004).
Emerging Challenges/Dimensions
First, the combined impact of computers and telecommunications on society has been transformative, impinging on almost every facet of human life including art, culture, science, and education. Consumer informatics integrates consumer information needs and preferences with clinical systems to empower patients to take charge of their healthcare, bring down costs, and improve quality of care. For example, the integration of electronic medical records with communications should facilitate communications between patients and providers, send automatic reminders to patients to stay on schedule, and help patients navigate the health-care system. Second, technological developments are coinciding with the consumerist movement in health-care. The paternalistic model that characterized the physician–patient relationship is slowly being complemented by alternative models such as shared/informed decisionmaking models (SDM/IDM) or patient-centered communication (PCC). Third, the significant investments in biomedical research enterprise in the developing world, and movement toward more evidence- based medicine, have led to calls for translation of the knowledge from the laboratory to the clinic and the community. Lastly, an urgent and a moral imperative in health is addressing the profound inequities in access to health-care and the disproportionate burden of disease faced by certain groups.
References:
- Epstein, R. M. & Street, R. L., Jr. (2007). Patient-centered communication in cancer care: Promoting healing and reducing suffering. NIH Publication no. 07–6225. Bethesda, MD: National Cancer Institute.
- Glanz, K., Rimer, B., & Viswanath, K. (eds.) (2008). Health behavior and health education: Theory, research, and practice. 4th ed. San Francisco, CA: Jossey-Bass.
- Himelboim, I. & Han, J. Y. (2014). Cancer talk on twitter: Community structure and information sources in breast and prostate cancer social networks. Journal of Health Communication: International Perspectives, 19(2), 210–225.
- Hornik, R. (ed.) (2002). Public health communication: Evidence for behavior change. Mahwah, NJ: Lawrence Erlbaum.
- McCauley, M., Blake, K., Meissner, H., & Viswanath, K. (2013). The social group influences of U.S. health journalists and their impact on the newsmaking process. Health Education Research, 28(20), 339–51.
- Noar, S. M. (2006). A 10-year retrospective of research in health mass media campaigns: Where do we go from here? Journal of Health Communication, 11, 21–42.
- Obregon, R. & Waisbord, S. (eds.) (2012). The handbook of global health communication. Oxford: Wiley Blackwell.
- Parker, J. C. & Thorson, E. (2008). Health communication in the new media landscape. New York: Springer.
- Randolph, W. & Viswanath, K. (2004). Lessons learned from public health mass media campaigns: Marketing health in a crowded media world. Annual Review of Public Health, 25, 419–37.
- Snyder, L. B. & Hamilton, M. A. (2002). A meta-analysis of U.S. health campaign effects on behavior: Emphasize enforcement, exposure, and new information, and beware of secular trend. In R. Hornik (ed.), Public health communication: Evidence for behavior change. Mahwah, NJ: Lawrence Erlbaum, pp. 357–383.
- Viswanath, K. (2005). The communications revolution and cancer control. Nature Reviews Cancer, 5(10), 828–835.
Back to Communication Research Paper Topics .
ORDER HIGH QUALITY CUSTOM PAPER

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 May 2024
Long-term weight loss effects of semaglutide in obesity without diabetes in the SELECT trial
- Donna H. Ryan 1 ,
- Ildiko Lingvay ORCID: orcid.org/0000-0001-7006-7401 2 ,
- John Deanfield 3 ,
- Steven E. Kahn 4 ,
- Eric Barros ORCID: orcid.org/0000-0001-6613-4181 5 ,
- Bartolome Burguera 6 ,
- Helen M. Colhoun ORCID: orcid.org/0000-0002-8345-3288 7 ,
- Cintia Cercato ORCID: orcid.org/0000-0002-6181-4951 8 ,
- Dror Dicker 9 ,
- Deborah B. Horn 10 ,
- G. Kees Hovingh 5 ,
- Ole Kleist Jeppesen 5 ,
- Alexander Kokkinos 11 ,
- A. Michael Lincoff ORCID: orcid.org/0000-0001-8175-2121 12 ,
- Sebastian M. Meyhöfer 13 ,
- Tugce Kalayci Oral 5 ,
- Jorge Plutzky ORCID: orcid.org/0000-0002-7194-9876 14 ,
- André P. van Beek ORCID: orcid.org/0000-0002-0335-8177 15 ,
- John P. H. Wilding ORCID: orcid.org/0000-0003-2839-8404 16 &
- Robert F. Kushner 17
Nature Medicine ( 2024 ) Cite this article
30k Accesses
1 Citations
2154 Altmetric
Metrics details
- Health care
- Medical research
In the SELECT cardiovascular outcomes trial, semaglutide showed a 20% reduction in major adverse cardiovascular events in 17,604 adults with preexisting cardiovascular disease, overweight or obesity, without diabetes. Here in this prespecified analysis, we examined effects of semaglutide on weight and anthropometric outcomes, safety and tolerability by baseline body mass index (BMI). In patients treated with semaglutide, weight loss continued over 65 weeks and was sustained for up to 4 years. At 208 weeks, semaglutide was associated with mean reduction in weight (−10.2%), waist circumference (−7.7 cm) and waist-to-height ratio (−6.9%) versus placebo (−1.5%, −1.3 cm and −1.0%, respectively; P < 0.0001 for all comparisons versus placebo). Clinically meaningful weight loss occurred in both sexes and all races, body sizes and regions. Semaglutide was associated with fewer serious adverse events. For each BMI category (<30, 30 to <35, 35 to <40 and ≥40 kg m − 2 ) there were lower rates (events per 100 years of observation) of serious adverse events with semaglutide (43.23, 43.54, 51.07 and 47.06 for semaglutide and 50.48, 49.66, 52.73 and 60.85 for placebo). Semaglutide was associated with increased rates of trial product discontinuation. Discontinuations increased as BMI class decreased. In SELECT, at 208 weeks, semaglutide produced clinically significant weight loss and improvements in anthropometric measurements versus placebo. Weight loss was sustained over 4 years. ClinicalTrials.gov identifier: NCT03574597 .
Similar content being viewed by others

Effects of a personalized nutrition program on cardiometabolic health: a randomized controlled trial

Two-year effects of semaglutide in adults with overweight or obesity: the STEP 5 trial

What is the pipeline for future medications for obesity?
The worldwide obesity prevalence, defined by body mass index (BMI) ≥30 kg m − 2 , has nearly tripled since 1975 (ref. 1 ). BMI is a good surveillance measure for population changes over time, given its strong correlation with body fat amount on a population level, but it may not accurately indicate the amount or location of body fat at the individual level 2 . In fact, the World Health Organization defines clinical obesity as ‘abnormal or excessive fat accumulation that may impair health’ 1 . Excess abnormal body fat, especially visceral adiposity and ectopic fat, is a driver of cardiovascular (CV) disease (CVD) 3 , 4 , 5 , and contributes to the global chronic disease burden of diabetes, chronic kidney disease, cancer and other chronic conditions 6 , 7 .
Remediating the adverse health effects of excess abnormal body fat through weight loss is a priority in addressing the global chronic disease burden. Improvements in CV risk factors, glycemia and quality-of-life measures including personal well-being and physical functioning generally begin with modest weight loss of 5%, whereas greater weight loss is associated with more improvement in these measures 8 , 9 , 10 . Producing and sustaining durable and clinically significant weight loss with lifestyle intervention alone has been challenging 11 . However, weight-management medications that modify appetite can make attaining and sustaining clinically meaningful weight loss of ≥10% more likely 12 . Recently, weight-management medications, particularly those comprising glucagon-like peptide-1 receptor agonists, that help people achieve greater and more sustainable weight loss have been developed 13 . Once-weekly subcutaneous semaglutide 2.4 mg, a glucagon-like peptide-1 receptor agonist, is approved for chronic weight management 14 , 15 , 16 and at doses of up to 2.0 mg is approved for type 2 diabetes treatment 17 , 18 , 19 . In patients with type 2 diabetes and high CV risk, semaglutide at doses of 0.5 mg and 1.0 mg has been shown to significantly lower the risk of CV events 20 . The SELECT trial (Semaglutide Effects on Heart Disease and Stroke in Patients with Overweight or Obesity) studied patients with established CVD and overweight or obesity but without diabetes. In SELECT, semaglutide was associated with a 20% reduction in major adverse CV events (hazard ratio 0.80, 95% confidence interval (CI) 0.72 to 0.90; P < 0.001) 21 . Data derived from the SELECT trial offer the opportunity to evaluate the weight loss efficacy, in a geographically and racially diverse population, of semaglutide compared with placebo over 208 weeks when both are given in addition to standard-of-care recommendations for secondary CVD prevention (but without a focus on targeting weight loss). Furthermore, the data allow examination of changes in anthropometric measures such as BMI, waist circumference (WC) and waist-to-height ratio (WHtR) as surrogates for body fat amount and location 22 , 23 . The diverse population can also be evaluated for changes in sex- and race-specific ‘cutoff points’ for BMI and WC, which have been identified as anthropometric measures that predict cardiometabolic risk 8 , 22 , 23 .
This prespecified analysis of the SELECT trial investigated weight loss and changes in anthropometric indices in patients with established CVD and overweight or obesity without diabetes, who met inclusion and exclusion criteria, within a range of baseline categories for glycemia, renal function and body anthropometric measures.
Study population
The SELECT study enrolled 17,604 patients (72.3% male) from 41 countries between October 2018 and March 2021, with a mean (s.d.) age of 61.6 (8.9) years and BMI of 33.3 (5.0) kg m − 2 (ref. 21 ). The baseline characteristics of the population have been reported 24 . Supplementary Table 1 outlines SELECT patients according to baseline BMI categories. Of note, in the lower BMI categories (<30 kg m − 2 (overweight) and 30 to <35 kg m − 2 (class I obesity)), the proportion of Asian individuals was higher (14.5% and 7.4%, respectively) compared with the proportion of Asian individuals in the higher BMI categories (BMI 35 to <40 kg m − 2 (class II obesity; 3.8%) and ≥40 kg m − 2 (class III obesity; 2.2%), respectively). As the BMI categories increased, the proportion of women was higher: in the class III BMI category, 45.5% were female, compared with 20.8%, 25.7% and 33.0% in the overweight, class I and class II categories, respectively. Lower BMI categories were associated with a higher proportion of patients with normoglycemia and glycated hemoglobin <5.7%. Although the proportions of patients with high cholesterol and history of smoking were similar across BMI categories, the proportion of patients with high-sensitivity C-reactive protein ≥2.0 mg dl −1 increased as the BMI category increased. A high-sensitivity C-reactive protein >2.0 mg dl −1 was present in 36.4% of patients in the overweight BMI category, with a progressive increase to 43.3%, 57.3% and 72.0% for patients in the class I, II and III obesity categories, respectively.
Weight and anthropometric outcomes
Percentage weight loss.
The average percentage weight-loss trajectories with semaglutide and placebo over 4 years of observation are shown in Fig. 1a (ref. 21 ). For those in the semaglutide group, the weight-loss trajectory continued to week 65 and then was sustained for the study period through week 208 (−10.2% for the semaglutide group, −1.5% for the placebo group; treatment difference −8.7%; 95% CI −9.42 to −7.88; P < 0.0001). To estimate the treatment effect while on medication, we performed a first on-treatment analysis (observation period until the first time being off treatment for >35 days). At week 208, mean weight loss in the semaglutide group analyzed as first on-treatment was −11.7% compared with −1.5% for the placebo group (Fig. 1b ; treatment difference −10.2%; 95% CI −11.0 to −9.42; P < 0.0001).
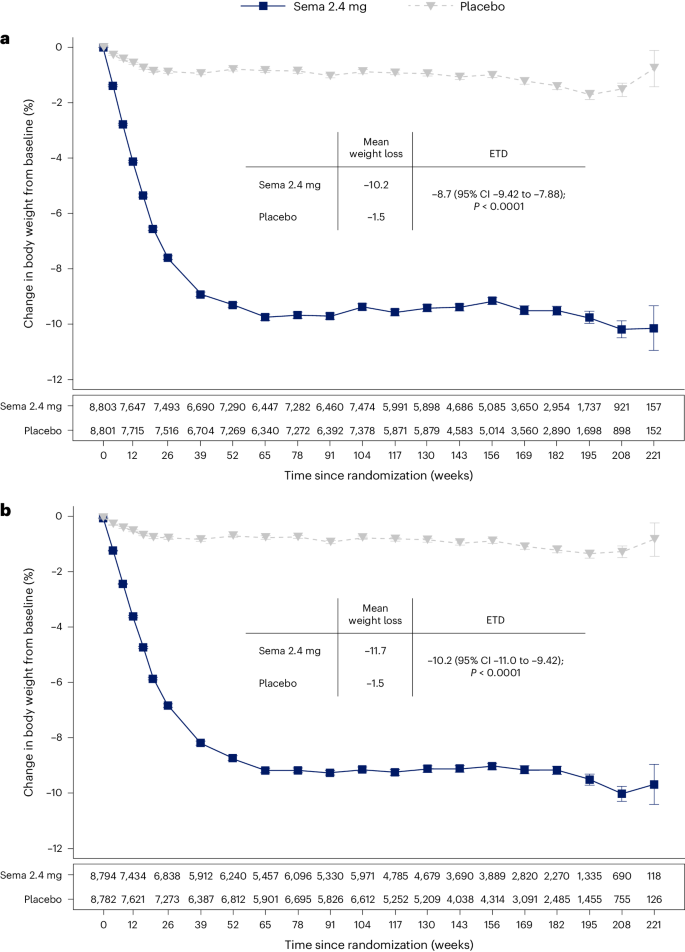
a , b , Observed data from the in-trial period ( a ) and first on-treatment ( b ). The symbols are the observed means, and error bars are ±s.e.m. Numbers shown below each panel represent the number of patients contributing to the means. Analysis of covariance with treatment and baseline values was used to estimate the treatment difference. Exact P values are 1.323762 × 10 −94 and 9.80035 × 10 −100 for a and b , respectively. P values are two-sided and are not adjusted for multiplicity. ETD, estimated treatment difference; sema, semaglutide.
Categorical weight loss and individual body weight change
Among in-trial (intention-to-treat principle) patients at week 104, weight loss of ≥5%, ≥10%, ≥15%, ≥20% and ≥25% was achieved by 67.8%, 44.2%, 22.9%, 11.0% and 4.9%, respectively, of those treated with semaglutide compared with 21.3%, 6.9%, 1.7%, 0.6% and 0.1% of those receiving placebo (Fig. 2a ). Individual weight changes at 104 weeks for the in-trial populations for semaglutide and placebo are depicted in Fig. 2b and Fig. 2c , respectively. These waterfall plots show the variation in weight-loss response that occurs with semaglutide and placebo and show that weight loss is more prominent with semaglutide than placebo.
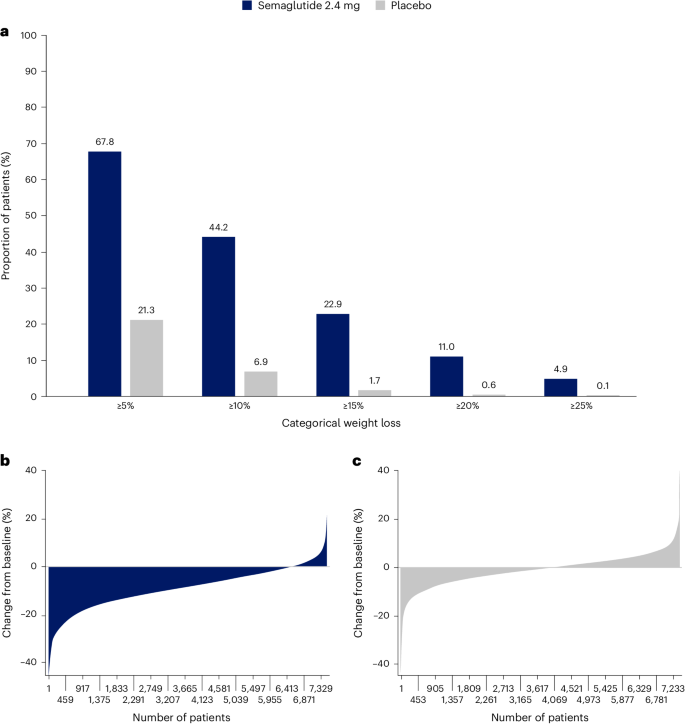
a , Categorical weight loss from baseline at week 104 for semaglutide and placebo. Data from the in-trial period. Bars depict the proportion (%) of patients receiving semaglutide or placebo who achieved ≥5%, ≥10%, ≥15%, ≥20% and ≥25% weight loss. b , c , Percentage change in body weight for individual patients from baseline to week 104 for semaglutide ( b ) and placebo ( c ). Each patient’s percentage change in body weight is plotted as a single bar.
Change in WC
WC change from baseline to 104 weeks has been reported previously in the primary outcome paper 21 . The trajectory of WC change mirrored that of the change in body weight. At week 208, average reduction in WC was −7.7 cm with semaglutide versus −1.3 cm with placebo, with a treatment difference of −6.4 cm (95% CI −7.18 to −5.61; P < 0.0001) 21 .
WC cutoff points
We analyzed achievement of sex- and race-specific cutoff points for WC by BMI <35 kg m − 2 or ≥35 kg m − 2 , because for BMI >35 kg m − 2 , WC is more difficult technically and, thus, less accurate as a risk predictor 4 , 25 , 26 . Within the SELECT population with BMI <35 kg m − 2 at baseline, 15.0% and 14.3% of the semaglutide and placebo groups, respectively, were below the sex- and race-specific WC cutoff points. At week 104, 41.2% fell below the sex- and race-specific cutoff points for the semaglutide group, compared with only 18.0% for the placebo group (Fig. 3 ).
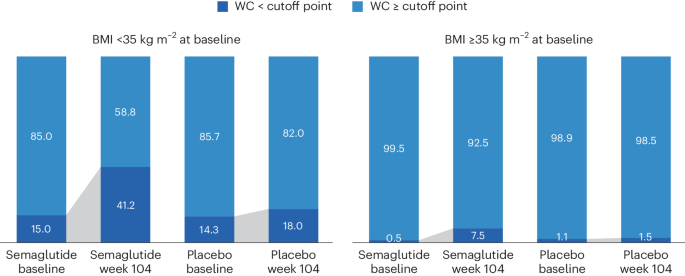
WC cutoff points; Asian women <80 cm, non-Asian women <88 cm, Asian men <88 cm, non-Asian men <102 cm.
Waist-to-height ratio
At baseline, mean WHtR was 0.66 for the study population. The lowest tertile of the SELECT population at baseline had a mean WHtR <0.62, which is higher than the cutoff point of 0.5 used to indicate increased cardiometabolic risk 27 , suggesting that the trial population had high WCs. At week 208, in the group randomized to semaglutide, there was a relative reduction of 6.9% in WHtR compared with 1.0% in placebo (treatment difference −5.87% points; 95% CI −6.56 to −5.17; P < 0.0001).
BMI category change
At week 104, 52.4% of patients treated with semaglutide achieved improvement in BMI category compared with 15.7% of those receiving placebo. Proportions of patients in the BMI categories at baseline and week 104 are shown in Fig. 4 , which depicts in-trial patients receiving semaglutide and placebo. The BMI category change reflects the superior weight loss with semaglutide, which resulted in fewer patients being in the higher BMI categories after 104 weeks. In the semaglutide group, 12.0% of patients achieved a BMI <25 kg m − 2 , which is considered the healthy BMI category, compared with 1.2% for placebo; per study inclusion criteria, no patients were in this category at baseline. The proportion of patients with obesity (BMI ≥30 kg m − 2 ) fell from 71.0% to 43.3% in the semaglutide group versus 71.9% to 67.9% in the placebo group.
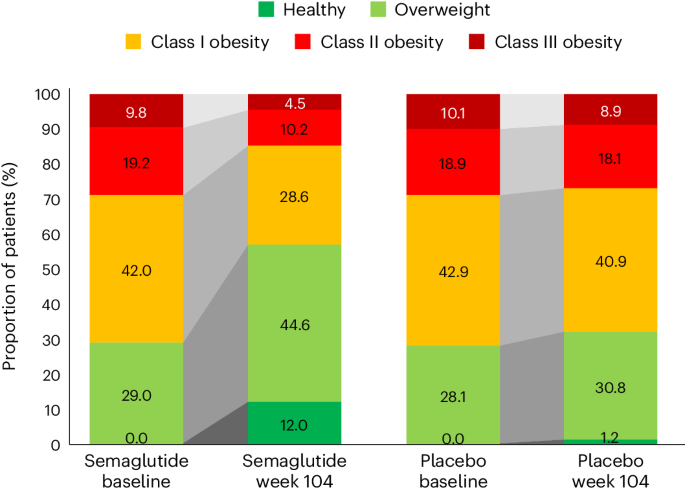
In the semaglutide group, 12.0% of patients achieved normal weight status at week 104 (from 0% at baseline), compared with 1.2% (from 0% at baseline) for placebo. BMI classes: healthy (BMI <25 kg m − 2 ), overweight (25 to <30 kg m − 2 ), class I obesity (30 to <35 kg m − 2 ), class II obesity (35 to <40 kg m − 2 ) and class III obesity (BMI ≥40 kg m − 2 ).
Weight and anthropometric outcomes by subgroups
The forest plot illustrated in Fig. 5 displays mean body weight percentage change from baseline to week 104 for semaglutide relative to placebo in prespecified subgroups. Similar relationships are depicted for WC changes in prespecified subgroups shown in Extended Data Fig. 1 . The effect of semaglutide (versus placebo) on mean percentage body weight loss as well as reduction in WC was found to be heterogeneous across several population subgroups. Women had a greater difference in mean weight loss with semaglutide versus placebo (−11.1% (95% CI −11.56 to −10.66) versus −7.5% in men (95% CI −7.78 to −7.23); P < 0.0001). There was a linear relationship between age category and degree of mean weight loss, with younger age being associated with progressively greater mean weight loss, but the actual mean difference by age group is small. Similarly, BMI category had small, although statistically significant, associations. Those with WHtR less than the median experienced slightly lower mean body weight change than those above the median, with estimated treatment differences −8.04% (95% CI −8.37 to −7.70) and −8.99% (95% CI −9.33 to −8.65), respectively ( P < 0.0001). Patients from Asia and of Asian race experienced slightly lower mean weight loss (estimated treatment difference with semaglutide for Asian race −7.27% (95% CI −8.09 to −6.46; P = 0.0147) and for Asia −7.30 (95% CI −7.97 to −6.62; P = 0.0016)). There was no difference in weight loss with semaglutide associated with ethnicity (estimated treatment difference for Hispanic −8.53% (95% CI −9.28 to −7.76) or non-Hispanic −8.52% (95% CI −8.77 to 8.26); P = 0.9769), glycemic status (estimated treatment difference for prediabetes −8.53% (95% CI −8.83 to −8.24) or normoglycemia −8.48% (95% CI −8.88 to −8.07; P = 0.8188) or renal function (estimated treatment difference for estimated glomerular filtration rate (eGFR) <60 or ≥60 ml min −1 1.73 m − 2 being −8.50% (95% CI −9.23 to −7.76) and −8.52% (95% CI −8.77 to −8.26), respectively ( P = 0.9519)).
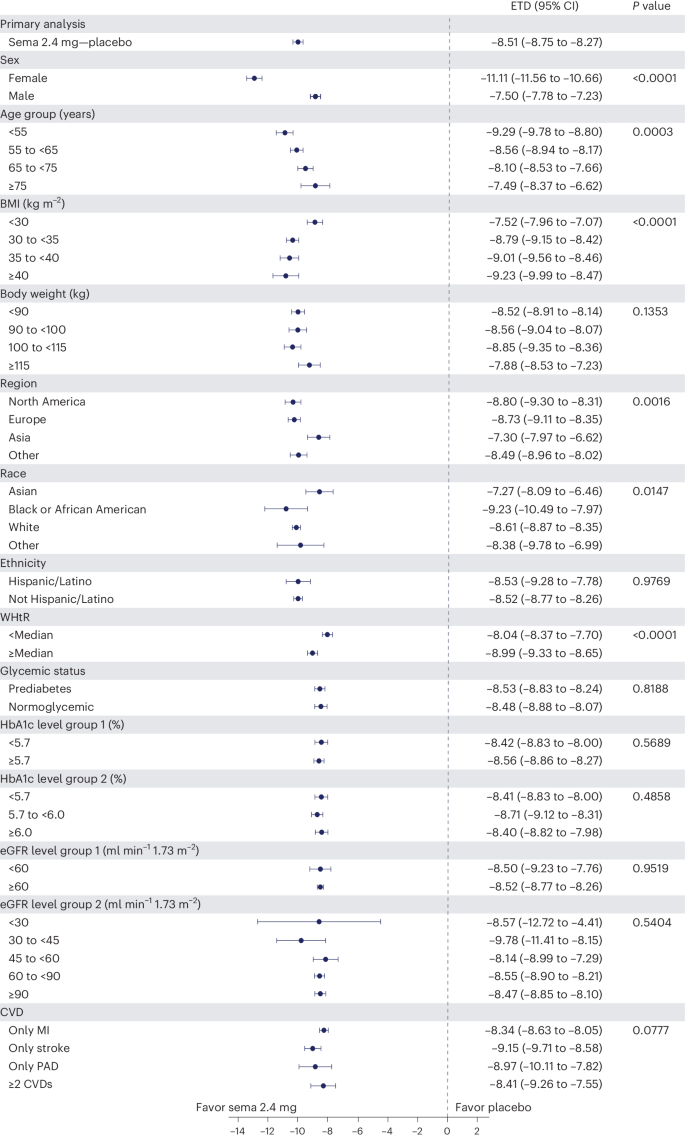
Data from the in-trial period. N = 17,604. P values represent test of no interaction effect. P values are two-sided and are not adjusted for multiplicity. The dots show estimated treatment differences, and the error bars show 95% CIs. Details of the statistical models are available in Methods . ETD, estimated treatment difference; HbA1c, glycated hemoglobin; MI, myocardial infarction; PAD, peripheral artery disease; sema, semaglutide.
Safety and tolerability according to baseline BMI category
We reported in the primary outcome of the SELECT trial that adverse events (AEs) leading to permanent discontinuation of the trial product occurred in 1,461 patients (16.6%) in the semaglutide group and 718 patients (8.2%) in the placebo group ( P < 0.001) 21 . For this analysis, we evaluated the cumulative incidence of AEs leading to trial product discontinuation by treatment assignment and by BMI category (Fig. 6 ). For this analysis, with death modeled as a competing risk, we tracked the proportion of in-trial patients for whom drug was withdrawn or interrupted for the first time (Fig. 6 , left) or cumulative discontinuations (Fig. 6 , right). Both panels of Fig. 6 depict a graded increase in the proportion discontinuing semaglutide, but not placebo. For lower BMI classes, discontinuation rates are higher in the semaglutide group but not the placebo group.
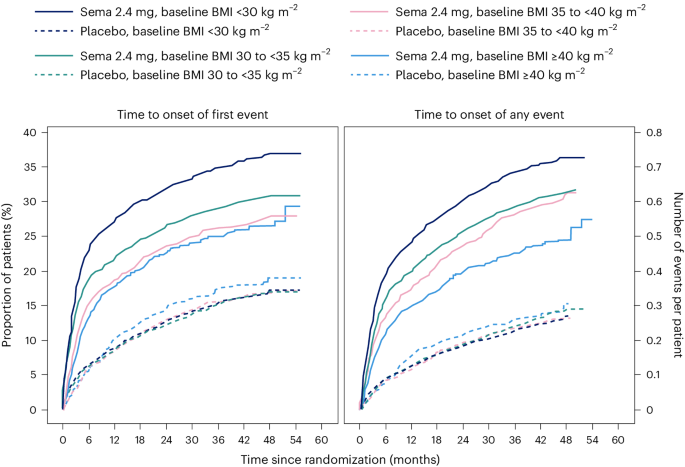
Data are in-trial from the full analysis set. sema, semaglutide.
We reported in the primary SELECT analysis that serious adverse events (SAEs) were reported by 2,941 patients (33.4%) in the semaglutide arm and by 3,204 patients (36.4%) in the placebo arm ( P < 0.001) 21 . For this study, we analyzed SAE rates by person-years of treatment exposure for BMI classes (<30 kg m − 2 , 30 to <35 kg m − 2 , 35 to <40 kg m − 2 , and ≥40 kg m − 2 ) and provide these data in Supplementary Table 2 . We also provide an analysis of the most common categories of SAEs. Semaglutide was associated with lower SAEs, primarily driven by CV event and infections. Within each obesity class (<30 kg m − 2 , 30 to <35 kg m − 2 , 35 to <40 kg m − 2 , and ≥40 kg m − 2 ), there were fewer SAEs in the group receiving semaglutide compared with placebo. Rates (events per 100 years of observation) of SAEs were 43.23, 43.54, 51.07 and 47.06 for semaglutide and 50.48, 49.66, 52.73 and 60.85 for placebo, with no evidence of heterogeneity. There was no detectable difference in hepatobiliary or gastrointestinal SAEs comparing semaglutide with placebo in any of the four BMI classes we evaluated.
The analyses of weight effects of the SELECT study presented here reveal that patients assigned to once-weekly subcutaneous semaglutide 2.4 mg lost significantly more weight than those receiving placebo. The weight-loss trajectory with semaglutide occurred over 65 weeks and was sustained up to 4 years. Likewise, there were similar improvements in the semaglutide group for anthropometrics (WC and WHtR). The weight loss was associated with a greater proportion of patients receiving semaglutide achieving improvement in BMI category, healthy BMI (<25 kg m − 2 ) and falling below the WC cutoff point above which increased cardiometabolic risk for the sex and race is greater 22 , 23 . Furthermore, both sexes, all races, all body sizes and those from all geographic regions were able to achieve clinically meaningful weight loss. There was no evidence of increased SAEs based on BMI categories, although lower BMI category was associated with increased rates of trial product discontinuation, probably reflecting exposure to a higher level of drug in lower BMI categories. These data, representing the longest clinical trial of the effects of semaglutide versus placebo on weight, establish the safety and durability of semaglutide effects on weight loss and maintenance in a geographically and racially diverse population of adult men and women with overweight and obesity but not diabetes. The implications of weight loss of this degree in such a diverse population suggests that it may be possible to impact the public health burden of the multiple morbidities associated with obesity. Although our trial focused on CV events, many chronic diseases would benefit from effective weight management 28 .
There were variations in the weight-loss response. Individual changes in body weight with semaglutide and placebo were striking; still, 67.8% achieved 5% or more weight loss and 44.2% achieved 10% weight loss with semaglutide at 2 years, compared with 21.3% and 6.9%, respectively, for those receiving placebo. Our first on-treatment analysis demonstrated that those on-drug lost more weight than those in-trial, confirming the effect of drug exposure. With semaglutide, lower BMI was associated with less percentage weight loss, and women lost more weight on average than men (−11.1% versus −7.5% treatment difference from placebo); however, in all cases, clinically meaningful mean weight loss was achieved. Although Asian patients lost less weight on average than patients of other races (−7.3% more than placebo), Asian patients were more likely to be in the lowest BMI category (<30 kg m − 2 ), which is known to be associated with less weight loss, as discussed below. Clinically meaningful weight loss was evident in the semaglutide group within a broad range of baseline categories for glycemia and body anthropometrics. Interestingly, at 2 years, a significant proportion of the semaglutide-treated group fell below the sex- and race-specific WC cutoff points, especially in those with BMI <35 kg m − 2 , and a notable proportion (12.0%) fell below the BMI cutoff point of 25 kg m − 2 , which is deemed a healthy BMI in those without unintentional weight loss. As more robust weight loss is possible with newer medications, achieving and maintaining these cutoff point targets may become important benchmarks for tracking responses.
The overall safety profile did not reveal any new signals from prior studies, and there were no BMI category-related associations with AE reporting. The analysis did reveal that tolerability may differ among specific BMI classes, since more discontinuations occurred with semaglutide among lower BMI classes. Potential contributors may include a possibility of higher drug exposure in lower BMI classes, although other explanations, including differences in motivation and cultural mores regarding body size, cannot be excluded.
Is the weight loss in SELECT less than expected based on prior studies with the drug? In STEP 1, a large phase 3 study of once-weekly subcutaneous semaglutide 2.4 mg in individuals without diabetes but with BMI >30 kg m − 2 or 27 kg m − 2 with at least one obesity-related comorbidity, the mean weight loss was −14.9% at week 68, compared with −2.4% with placebo 14 . Several reasons may explain the observation that the mean treatment difference was −12.5% in STEP 1 and −8.7% in SELECT. First, SELECT was designed as a CV outcomes trial and not a weight-loss trial, and weight loss was only a supportive secondary endpoint in the trial design. Patients in STEP 1 were desirous of weight loss as a reason for study participation and received structured lifestyle intervention (which included a −500 kcal per day diet with 150 min per week of physical activity). In the SELECT trial, patients did not enroll for the specific purpose of weight loss and received standard of care covering management of CV risk factors, including medical treatment and healthy lifestyle counseling, but without a specific focus on weight loss. Second, the respective study populations were quite different, with STEP 1 including a younger, healthier population with more women (73.1% of the semaglutide arm in STEP 1 versus 27.7% in SELECT) and higher mean BMI (37.8 kg m − 2 versus 33.3 kg m − 2 , respectively) 14 , 21 . Third, major differences existed between the respective trial protocols. Patients in the semaglutide treatment arm of STEP 1 were more likely to be exposed to the medication at the full dose of 2.4 mg than those in SELECT. In SELECT, investigators were allowed to slow, decrease or pause treatment. By 104 weeks, approximately 77% of SELECT patients on dose were receiving the target semaglutide 2.4 mg weekly dose, which is lower than the corresponding proportion of patients in STEP 1 (89.6% were receiving the target dose at week 68) 14 , 21 . Indeed, in our first on-treatment analysis at week 208, weight loss was greater (−11.7% for semaglutide) compared with the in-trial analysis (−10.2% for semaglutide). Taken together, all these issues make less weight loss an expected finding in SELECT, compared with STEP 1.
The SELECT study has some limitations. First, SELECT was not a primary prevention trial, and the data should not be extrapolated to all individuals with overweight and obesity to prevent major adverse CV events. Although the data set is rich in numbers and diversity, it does not have the numbers of individuals in racial subgroups that may have revealed potential differential effects. SELECT also did not include individuals who have excess abnormal body fat but a BMI <27 kg m − 2 . Not all individuals with increased CV risk have BMI ≥27 kg m − 2 . Thus, the study did not include Asian patients who qualify for treatment with obesity medications at lower BMI and WC cutoff points according to guidelines in their countries 29 . We observed that Asian patients were less likely to be in the higher BMI categories of SELECT and that the population of those with BMI <30 kg m − 2 had a higher percentage of Asian race. Asian individuals would probably benefit from weight loss and medication approaches undertaken at lower BMI levels in the secondary prevention of CVD. Future studies should evaluate CV risk reduction in Asian individuals with high CV risk and BMI <27 kg m − 2 . Another limitation is the lack of information on body composition, beyond the anthropometric measures we used. It would be meaningful to have quantitation of fat mass, lean mass and muscle mass, especially given the wide range of body size in the SELECT population.
An interesting observation from this SELECT weight loss data is that when BMI is ≤30 kg m − 2 , weight loss on a percentage basis is less than that observed across higher classes of BMI severity. Furthermore, as BMI exceeds 30 kg m − 2 , weight loss amounts are more similar for class I, II and III obesity. This was also observed in Look AHEAD, a lifestyle intervention study for weight loss 30 . The proportion (percentage) of weight loss seems to be less, on average, in the BMI <30 kg m − 2 category relative to higher BMI categories, despite their receiving of the same treatment and even potentially higher exposure to the drug for weight loss 30 . Weight loss cannot continue indefinitely. There is a plateau of weight that occurs after weight loss with all treatments for weight management. This plateau has been termed the ‘set point’ or ‘settling point’, a body weight that is in harmony with the genetic and environmental determinants of body weight and adiposity 31 . Perhaps persons with BMI <30 kg m − 2 are closer to their settling point and have less weight to lose to reach it. Furthermore, the cardiometabolic benefits of weight loss are driven by reduction in the abnormal ectopic and visceral depots of fat, not by reduction of subcutaneous fat stores in the hips and thighs. The phenotype of cardiometabolic disease but lower BMI (<30 kg m − 2 ) may be one where reduction of excess abnormal and dysfunctional body fat does not require as much body mass reduction to achieve health improvement. We suspect this may be the case and suggest further studies to explore this aspect of weight-loss physiology.
In conclusion, this analysis of the SELECT study supports the broad use of once-weekly subcutaneous semaglutide 2.4 mg as an aid to CV event reduction in individuals with overweight or obesity without diabetes but with preexisting CVD. Semaglutide 2.4 mg safely and effectively produced clinically significant weight loss in all subgroups based on age, sex, race, glycemia, renal function and anthropometric categories. Furthermore, the weight loss was sustained over 4 years during the trial.
Trial design and participants
The current work complies with all relevant ethical regulations and reports a prespecified analysis of the randomized, double-blind, placebo-controlled SELECT trial ( NCT03574597 ), details of which have been reported in papers describing study design and rationale 32 , baseline characteristics 24 and the primary outcome 21 . SELECT evaluated once-weekly subcutaneous semaglutide 2.4 mg versus placebo to reduce the risk of major adverse cardiac events (a composite endpoint comprising CV death, nonfatal myocardial infarction or nonfatal stroke) in individuals with established CVD and overweight or obesity, without diabetes. The protocol for SELECT was approved by national and institutional regulatory and ethical authorities in each participating country. All patients provided written informed consent before beginning any trial-specific activity. Eligible patients were aged ≥45 years, with a BMI of ≥27 kg m − 2 and established CVD defined as at least one of the following: prior myocardial infarction, prior ischemic or hemorrhagic stroke, or symptomatic peripheral artery disease. Additional inclusion and exclusion criteria can be found elsewhere 32 .
Human participants research
The trial protocol was designed by the trial sponsor, Novo Nordisk, and the academic Steering Committee. A global expert panel of physician leaders in participating countries advised on regional operational issues. National and institutional regulatory and ethical authorities approved the protocol, and all patients provided written informed consent.
Study intervention and patient management
Patients were randomly assigned in a double-blind manner and 1:1 ratio to receive once-weekly subcutaneous semaglutide 2.4 mg or placebo. The starting dose was 0.24 mg once weekly, with dose increases every 4 weeks (to doses of 0.5, 1.0, 1.7 and 2.4 mg per week) until the target dose of 2.4 mg was reached after 16 weeks. Patients who were unable to tolerate dose escalation due to AEs could be managed by extension of dose-escalation intervals, treatment pauses or maintenance at doses below the 2.4 mg per week target dose. Investigators were allowed to reduce the dose of study product if tolerability issues arose. Investigators were provided with guidelines for, and encouraged to follow, evidence-based recommendations for medical treatment and lifestyle counseling to optimize management of underlying CVD as part of the standard of care. The lifestyle counseling was not targeted at weight loss. Additional intervention descriptions are available 32 .
Sex, race, body weight, height and WC measurements
Sex and race were self-reported. Body weight was measured without shoes and only wearing light clothing; it was measured on a digital scale and recorded in kilograms or pounds (one decimal with a precision of 0.1 kg or lb), with preference for using the same scale throughout the trial. The scale was calibrated yearly as a minimum unless the manufacturer certified that calibration of the weight scales was valid for the lifetime of the scale. Height was measured without shoes in centimeters or inches (one decimal with a precision of 0.1 cm or inches). At screening, BMI was calculated by the electronic case report form. WC was defined as the abdominal circumference located midway between the lower rib margin and the iliac crest. Measures were obtained in a standing position with a nonstretchable measuring tape and to the nearest centimeter or inch. The patient was asked to breathe normally. The tape touched the skin but did not compress soft tissue, and twists in the tape were avoided.
The following endpoints relevant to this paper were assessed at randomization (week 0) to years 2, 3 and 4: change in body weight (%); proportion achieving weight loss ≥5%, ≥10%, ≥15% and ≥20%; change in WC (cm); and percentage change in WHtR (cm cm −1 ). Improvement in BMI category (defined as being in a lower BMI class) was assessed at week 104 compared with baseline according to BMI classes: healthy (BMI <25 kg m − 2 ), overweight (25 to <30 kg m − 2 ), class I obesity (30 to <35 kg m − 2 ), class II obesity (35 to <40 kg m − 2 ) and class III obesity (≥40 kg m − 2 ). The proportions of individuals with BMI <35 or ≥35 kg m − 2 who achieved sex- and race-specific cutoff points for WC (indicating increased metabolic risk) were evaluated at week 104. The WC cutoff points were as follows: Asian women <80 cm, non-Asian women <88 cm, Asian men <88 cm and non-Asian men <102 cm.
Overall, 97.1% of the semaglutide group and 96.8% of the placebo group completed the trial. During the study, 30.6% of those assigned to semaglutide did not complete drug treatment, compared with 27.0% for placebo.
Statistical analysis
The statistical analyses for the in-trial period were based on the intention-to-treat principle and included all randomized patients irrespective of adherence to semaglutide or placebo or changes to background medications. Continuous endpoints were analyzed using an analysis of covariance model with treatment as a fixed factor and baseline value of the endpoint as a covariate. Missing data at the landmark visit, for example, week 104, were imputed using a multiple imputation model and done separately for each treatment arm and included baseline value as a covariate and fit to patients having an observed data point (irrespective of adherence to randomized treatment) at week 104. The fit model is used to impute values for all patients with missing data at week 104 to create 500 complete data sets. Rubin’s rules were used to combine the results. Estimated means are provided with s.e.m., and estimated treatment differences are provided with 95% CI. Binary endpoints were analyzed using logistic regression with treatment and baseline value as a covariate, where missing data were imputed by first using multiple imputation as described above and then categorizing the imputed data according to the endpoint, for example, body weight percentage change at week 104 of <0%. Subgroup analyses for continuous and binary endpoints also included the subgroup and interaction between treatment and subgroup as fixed factors. Because some patients in both arms continued to be followed but were off treatment, we also analyzed weight loss by first on-treatment group (observation period until first time being off treatment for >35 days) to assess a more realistic picture of weight loss in those adhering to treatment. CIs were not adjusted for multiplicity and should therefore not be used to infer definitive treatment effects. All statistical analyses were performed with SAS software, version 9.4 TS1M5 (SAS Institute).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data will be shared with bona fide researchers who submit a research proposal approved by the independent review board. Individual patient data will be shared in data sets in a deidentified and anonymized format. Information about data access request proposals can be found at https://www.novonordisk-trials.com/ .
Obesity and overweight. World Health Organization https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (2021).
Cornier, M. A. et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation 124 , 1996–2019 (2011).
Article PubMed Google Scholar
Afshin, A. et al. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 377 , 13–27 (2017).
Jensen, M. D. et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J. Am. Coll. Cardiol. 63 , 2985–3023 (2014).
Poirier, P. et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 113 , 898–918 (2006).
Dai, H. et al. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: an analysis of the Global Burden of Disease Study. PLoS Med. 17 , e1003198 (2020).
Article PubMed PubMed Central Google Scholar
Ndumele, C. E. et al. Cardiovascular–kidney–metabolic health: a presidential advisory from the American Heart Association. Circulation 148 , 1606–1635 (2023).
Garvey, W. T. et al. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr. Pr. 22 , 1–203 (2016).
Article Google Scholar
Ryan, D. H. & Yockey, S. R. Weight loss and improvement in comorbidity: differences at 5%, 10%, 15%, and over. Curr. Obes. Rep. 6 , 187–194 (2017).
Wing, R. R. et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 34 , 1481–1486 (2011).
Article CAS PubMed PubMed Central Google Scholar
Wadden, T. A., Tronieri, J. S. & Butryn, M. L. Lifestyle modification approaches for the treatment of obesity in adults. Am. Psychol. 75 , 235–251 (2020).
Tchang, B. G. et al. Pharmacologic treatment of overweight and obesity in adults. in (eds. Feingold, K. R. et al.) Endotext https://www.ncbi.nlm.nih.gov/books/NBK279038/ (MDText.com, 2000).
Müller, T. D., Blüher, M., Tschöp, M. H. & DiMarchi, R. D. Anti-obesity drug discovery: advances and challenges. Nat. Rev. Drug Discov. 21 , 201–223 (2022).
Wilding, J. P. H. et al. Once-weekly semaglutide in adults with overweight or obesity. N. Engl. J. Med. 384 , 989–1002 (2021).
Article CAS PubMed Google Scholar
Wegovy (semaglutide) summary of product characteristics. European Medicines Agency https://www.ema.europa.eu/en/documents/product-information/wegovy-epar-product-information_en.pdf (2023).
WEGOVY (semaglutide) prescribing information. Food and Drug Administration https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/215256s007lbl.pdf (2023).
Sorli, C. et al. Efficacy and safety of once-weekly semaglutide monotherapy versus placebo in patients with type 2 diabetes (SUSTAIN 1): a double-blind, randomised, placebo-controlled, parallel-group, multinational, multicentre phase 3a trial. Lancet Diabetes Endocrinol. 5 , 251–260 (2017).
Ozempic (semaglutide) summary of product characteristics. European Medicines Agency https://www.ema.europa.eu/en/documents/product-information/ozempic-epar-product-information_en.pdf (2023).
OZEMPIC (semaglutide) prescribing information. Food and Drug Administration https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/209637lbl.pdf (2017).
Marso, S. P. et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 375 , 1834–1844 (2016).
Lincoff, A. M. et al. Semaglutide and cardiovascular outcomes in obesity without diabetes. N. Engl. J. Med. 389 , 2221–2232 (2023).
Ross, R. et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 16 , 177–189 (2020).
Snijder, M. B., van Dam, R. M., Visser, M. & Seidell, J. C. What aspects of body fat are particularly hazardous and how do we measure them? Int. J. Epidemiol. 35 , 83–92 (2006).
Lingvay, I. et al. Semaglutide for cardiovascular event reduction in people with overweight or obesity: SELECT study baseline characteristics. Obesity 31 , 111–122 (2023).
Basset, J. The Asia-Pacific perspective: redefining obesity and its treatment. International Diabetes Institute, World Health Organization Regional Office for the Western Pacific, International Association for the Study of Obesity & International Obesity Task Force https://www.vepachedu.org/TSJ/BMI-Guidelines.pdf (2000).
Hu, F. in Obesity Epidemiology (ed. Hu, F.) 53–83 (Oxford University Press, 2008).
Browning, L. M., Hsieh, S. D. & Ashwell, M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr. Res. Rev. 23 , 247–269 (2010).
Sattar, N. et al. Treating chronic diseases without tackling excess adiposity promotes multimorbidity. Lancet Diabetes Endocrinol. 11 , 58–62 (2023).
Obesity classification. World Obesity https://www.worldobesity.org/about/about-obesity/obesity-classification (2022).
Unick, J. L. et al. Effectiveness of lifestyle interventions for individuals with severe obesity and type 2 diabetes: results from the Look AHEAD trial. Diabetes Care 34 , 2152–2157 (2011).
Speakman, J. R. et al. Set points, settling points and some alternative models: theoretical options to understand how genes and environments combine to regulate body adiposity. Dis. Model. Mech. 4 , 733–745 (2011).
Ryan, D. H. et al. Semaglutide effects on cardiovascular outcomes in people with overweight or obesity (SELECT) rationale and design. Am. Heart J. 229 , 61–69 (2020).
Download references
Acknowledgements
Editorial support was provided by Richard Ogilvy-Stewart of Apollo, OPEN Health Communications, and funded by Novo Nordisk A/S, in accordance with Good Publication Practice guidelines ( www.ismpp.org/gpp-2022 ).
Author information
Authors and affiliations.
Pennington Biomedical Research Center, Baton Rouge, LA, USA
Donna H. Ryan
Department of Internal Medicine/Endocrinology and Peter O’ Donnell Jr. School of Public Health, University of Texas Southwestern Medical Center, Dallas, TX, USA
Ildiko Lingvay
Institute of Cardiovascular Science, University College London, London, UK
John Deanfield
VA Puget Sound Health Care System and University of Washington, Seattle, WA, USA
Steven E. Kahn
Novo Nordisk A/S, Søborg, Denmark
Eric Barros, G. Kees Hovingh, Ole Kleist Jeppesen & Tugce Kalayci Oral
Endocrinology and Metabolism Institute, Cleveland Clinic, Cleveland, OH, USA
Bartolome Burguera
Institute of Genetics and Cancer, University of Edinburgh, Edinburgh, UK
Helen M. Colhoun
Obesity Unit, Department of Endocrinology, Hospital das Clínicas, University of São Paulo, São Paulo, Brazil
Cintia Cercato
Internal Medicine Department D, Hasharon Hospital-Rabin Medical Center, Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
Dror Dicker
Center for Obesity Medicine and Metabolic Performance, Department of Surgery, University of Texas McGovern Medical School, Houston, TX, USA
Deborah B. Horn
First Department of Propaedeutic Internal Medicine, School of Medicine, National and Kapodistrian University of Athens, Athens, Greece
Alexander Kokkinos
Department of Cardiovascular Medicine, Cleveland Clinic, and Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, OH, USA
A. Michael Lincoff
Institute of Endocrinology & Diabetes, University of Lübeck, Lübeck, Germany
Sebastian M. Meyhöfer
Cardiovascular Division, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA
Jorge Plutzky
University of Groningen, University Medical Center Groningen, Department of Endocrinology, Groningen, the Netherlands
André P. van Beek
Department of Cardiovascular and Metabolic Medicine, University of Liverpool, Liverpool, UK
John P. H. Wilding
Northwestern University Feinberg School of Medicine, Chicago, IL, USA
Robert F. Kushner
You can also search for this author in PubMed Google Scholar
Contributions
D.H.R., I.L. and S.E.K. contributed to the study design. D.B.H., I.L., D.D., A.K., S.M.M., A.P.v.B., C.C. and J.P.H.W. were study investigators. D.B.H., I.L., D.D., A.K., S.M.M., A.P.v.B., C.C. and J.P.H.W. enrolled patients. D.H.R. was responsible for data analysis and manuscript preparation. All authors contributed to data interpretation, review, revisions and final approval of the manuscript.
Corresponding author
Correspondence to Donna H. Ryan .
Ethics declarations
Competing interests.
D.H.R. declares having received consulting honoraria from Altimmune, Amgen, Biohaven, Boehringer Ingelheim, Calibrate, Carmot Therapeutics, CinRx, Eli Lilly, Epitomee, Gila Therapeutics, IFA Celtics, Novo Nordisk, Pfizer, Rhythm, Scientific Intake, Wondr Health and Zealand Pharma; she declares she received stock options from Calibrate, Epitomee, Scientific Intake and Xeno Bioscience. I.L. declares having received research funding (paid to institution) from Novo Nordisk, Sanofi, Mylan and Boehringer Ingelheim. I.L. received advisory/consulting fees and/or other support from Altimmune, AstraZeneca, Bayer, Biomea, Boehringer Ingelheim, Carmot Therapeutics, Cytoki Pharma, Eli Lilly, Intercept, Janssen/Johnson & Johnson, Mannkind, Mediflix, Merck, Metsera, Novo Nordisk, Pharmaventures, Pfizer, Regeneron, Sanofi, Shionogi, Structure Therapeutics, Target RWE, Terns Pharmaceuticals, The Comm Group, Valeritas, WebMD and Zealand Pharma. J.D. declares having received consulting honoraria from Amgen, Boehringer Ingelheim, Merck, Pfizer, Aegerion, Novartis, Sanofi, Takeda, Novo Nordisk and Bayer, and research grants from British Heart Foundation, MRC (UK), NIHR, PHE, MSD, Pfizer, Aegerion, Colgate and Roche. S.E.K. declares having received consulting honoraria from ANI Pharmaceuticals, Boehringer Ingelheim, Eli Lilly, Merck, Novo Nordisk and Oramed, and stock options from AltPep. B.B. declares having received honoraria related to participation on this trial and has no financial conflicts related to this publication. H.M.C. declares being a stockholder and serving on an advisory panel for Bayer; receiving research grants from Chief Scientist Office, Diabetes UK, European Commission, IQVIA, Juvenile Diabetes Research Foundation and Medical Research Council; serving on an advisory board and speaker’s bureau for Novo Nordisk; and holding stock in Roche Pharmaceuticals. C.C. declares having received consulting honoraria from Novo Nordisk, Eli Lilly, Merck, Brace Pharma and Eurofarma. D.D. declares having received consulting honoraria from Novo Nordisk, Eli Lilly, Boehringer Ingelheim and AstraZeneca, and received research grants through his affiliation from Novo Nordisk, Eli Lilly, Boehringer Ingelheim and Rhythm. D.B.H. declares having received research grants through her academic affiliation from Novo Nordisk and Eli Lilly, and advisory/consulting honoraria from Novo Nordisk, Eli Lilly and Gelesis. A.K. declares having received research grants through his affiliation from Novo Nordisk and Pharmaserve Lilly, and consulting honoraria from Pharmaserve Lilly, Sanofi-Aventis, Novo Nordisk, MSD, AstraZeneca, ELPEN Pharma, Boehringer Ingelheim, Galenica Pharma, Epsilon Health and WinMedica. A.M.L. declares having received honoraria from Novo Nordisk, Eli Lilly, Akebia Therapeutics, Ardelyx, Becton Dickinson, Endologix, FibroGen, GSK, Medtronic, Neovasc, Provention Bio, ReCor, BrainStorm Cell Therapeutics, Alnylam and Intarcia for consulting activities, and research funding to his institution from AbbVie, Esperion, AstraZeneca, CSL Behring, Novartis and Eli Lilly. S.M.M. declares having received consulting honoraria from Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Daichii-Sankyo, esanum, Gilead, Ipsen, Eli Lilly, Novartis, Novo Nordisk, Sandoz and Sanofi; he declares he received research grants from AstraZeneca, Eli Lilly and Novo Nordisk. J.P. declares having received consulting honoraria from Altimmune, Amgen, Esperion, Merck, MJH Life Sciences, Novartis and Novo Nordisk; he has received a grant, paid to his institution, from Boehringer Ingelheim and holds the position of Director, Preventive Cardiology, at Brigham and Women’s Hospital. A.P.v.B. is contracted via the University of Groningen (no personal payment) to undertake consultancy for Novo Nordisk, Eli Lilly and Boehringer Ingelheim. J.P.H.W. is contracted via the University of Liverpool (no personal payment) to undertake consultancy for Altimmune, AstraZeneca, Boehringer Ingelheim, Cytoki, Eli Lilly, Napp, Novo Nordisk, Menarini, Pfizer, Rhythm Pharmaceuticals, Sanofi, Saniona, Tern Pharmaceuticals, Shionogi and Ysopia. J.P.H.W. also declares personal honoraria/lecture fees from AstraZeneca, Boehringer Ingelheim, Medscape, Napp, Menarini, Novo Nordisk and Rhythm. R.F.K. declares having received consulting honoraria from Novo Nordisk, Weight Watchers, Eli Lilly, Boehringer Ingelheim, Pfizer, Structure and Altimmune. E.B., G.K.H., O.K.J. and T.K.O. are employees of Novo Nordisk A/S.
Peer review
Peer review information.
Nature Medicine thanks Christiana Kartsonaki, Peter Rossing, Naveed Sattar and Vikas Sridhar for their contribution to the peer review of this work. Primary Handling Editor: Sonia Muliyil, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Extended data
Extended data fig. 1 effect of semaglutide treatment or placebo on waist circumference from baseline to week 104 by subgroups..
Data from the in-trial period. N = 17,604. P values represent test of no interaction effect. P values are two-sided and not adjusted for multiplicity. The dots show estimated treatment differences and the error bars show 95% confidence intervals. Details of the statistical models are available in Methods . BMI, body mass index; CI, confidence interval; CV, cardiovascular; CVD, cardiovascular disease; eGFR, estimated glomerular filtration rate; ETD, estimated treatment difference; HbA1c, glycated hemoglobin; MI, myocardial infarction; PAD, peripheral artery disease; sema, semaglutide.
Supplementary information
Reporting summary, supplementary tables 1 and 2.
Supplementary Table 1. Baseline characteristics by BMI class. Data are represented as number and percentage of patients. Renal function categories were based on the eGFR as per Chronic Kidney Disease Epidemiology Collaboration. Albuminuria categories were based on UACR. Smoking was defined as smoking at least one cigarette or equivalent daily. The category ‘Other’ for CV inclusion criteria includes patients where it is unknown if the patient fulfilled only one or several criteria and patients who were randomized in error and did not fulfill any criteria. Supplementary Table 2. SAEs according to baseline BMI category. P value: two-sided P value from Fisher’s exact test for test of no difference.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Ryan, D.H., Lingvay, I., Deanfield, J. et al. Long-term weight loss effects of semaglutide in obesity without diabetes in the SELECT trial. Nat Med (2024). https://doi.org/10.1038/s41591-024-02996-7
Download citation
Received : 01 March 2024
Accepted : 12 April 2024
Published : 13 May 2024
DOI : https://doi.org/10.1038/s41591-024-02996-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

Impact of Covid-19 on Bangladeshi university students mental health: ML and DL analysis
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Md Monir Ahammod Bin Atique
- For correspondence: [email protected]
- Info/History
- Preview PDF
The Covid-19 outbreak has adversely influenced university students across the world both physically and psychologically. The psychological struggle faced by students, is effected by various factors, including disruptions to daily routines and academic activities, increased reliance on smartphones and the internet, limited social interaction, and confinement to their homes. These impediments reflect a broader issue of imbalance in cognitive health status among them during the pandemic. In Bangladesh, despite having the necessary population to study, understanding the impact of Covid-19 on the mental health status of university students has been limited. Hence, it is imperative to diagnose mental health issues and deal with the underlying reasons in order to enhance students' psychological well-being, which leads to academic achievement. Nowadays, Artificial Intelligence (AI) based prediction models have the potential to play a crucial role in predicting mental state early. The purpose of the study is to explore the following effects of the pandemic on the mental health of Bangladeshi university students using Machine Learning (ML) and Deep Learning (DL) techniques. A reliable AI prediction system requires real-world data, that was collected by a survey through a Google form (online questionnaires) among 400 students of 16 universities, and the respondents were 253. In this paper, after data preprocessing, ten widely known ML and four DL models were developed to automatically and accurately predict mental well-being during or after the Covid-19 circumstance. According to our findings, the Random Forest (RF) algorithm and Siamese Neural Networks (SNNs) outperformed other models in terms of accuracy (86\% and 75\%). Additionally, Chi-Square test was conducted, which revealed the five most common and significant predictors (“Stable family income”, “Disruption of daily life”, “Own income”, “Sleep status”, and “Fear of getting infected with Covid-19”) of psychological health conditions. Overall, this work could assist university administrations, government agencies, and health specialists in taking appropriate measures to understand and maintain students' mental health. This research also suggests proper monitoring, government support, and social awareness during and after the worldwide epidemic to keep an excellent mental health state of university students.
Competing Interest Statement
The authors have declared no competing interest.
Funding Statement
This work was supported by Innovative Human Resource Development for Local 614 Intellectualization program through the Institute of Information & Communications 615 Technology Planning & Evaluation(IITP) grant funded by the Korea 616 government(MSIT)(IITP-2024-00156287, 50%). This work was partially supported 617 by the Korea Internet & Security Agency (KISA) - Information Security College Support 618 Project (50%)
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
The Ethics Committee of the University Research Ethics Board at University Grants Commission of Bangladesh waived ethical approval for this work. The data collection involved anonymous responses from university students via an online Google Form, where the identity of the participants was completely hidden. According to the ethical guidelines of our institution, research involving anonymous surveys where participants cannot be identified does not require ethical approval.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
Based on request data set will be shared.
View the discussion thread.
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
- Addiction Medicine (324)
- Allergy and Immunology (628)
- Anesthesia (165)
- Cardiovascular Medicine (2381)
- Dentistry and Oral Medicine (289)
- Dermatology (207)
- Emergency Medicine (380)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (838)
- Epidemiology (11777)
- Forensic Medicine (10)
- Gastroenterology (703)
- Genetic and Genomic Medicine (3751)
- Geriatric Medicine (350)
- Health Economics (635)
- Health Informatics (2401)
- Health Policy (933)
- Health Systems and Quality Improvement (899)
- Hematology (341)
- HIV/AIDS (782)
- Infectious Diseases (except HIV/AIDS) (13320)
- Intensive Care and Critical Care Medicine (768)
- Medical Education (366)
- Medical Ethics (105)
- Nephrology (398)
- Neurology (3510)
- Nursing (198)
- Nutrition (528)
- Obstetrics and Gynecology (675)
- Occupational and Environmental Health (665)
- Oncology (1825)
- Ophthalmology (538)
- Orthopedics (219)
- Otolaryngology (287)
- Pain Medicine (233)
- Palliative Medicine (66)
- Pathology (446)
- Pediatrics (1035)
- Pharmacology and Therapeutics (426)
- Primary Care Research (420)
- Psychiatry and Clinical Psychology (3180)
- Public and Global Health (6149)
- Radiology and Imaging (1280)
- Rehabilitation Medicine and Physical Therapy (749)
- Respiratory Medicine (828)
- Rheumatology (379)
- Sexual and Reproductive Health (372)
- Sports Medicine (323)
- Surgery (402)
- Toxicology (50)
- Transplantation (172)
- Urology (146)

Cultural Relativity and Acceptance of Embryonic Stem Cell Research
Article sidebar.
Main Article Content
There is a debate about the ethical implications of using human embryos in stem cell research, which can be influenced by cultural, moral, and social values. This paper argues for an adaptable framework to accommodate diverse cultural and religious perspectives. By using an adaptive ethics model, research protections can reflect various populations and foster growth in stem cell research possibilities.
INTRODUCTION
Stem cell research combines biology, medicine, and technology, promising to alter health care and the understanding of human development. Yet, ethical contention exists because of individuals’ perceptions of using human embryos based on their various cultural, moral, and social values. While these disagreements concerning policy, use, and general acceptance have prompted the development of an international ethics policy, such a uniform approach can overlook the nuanced ethical landscapes between cultures. With diverse viewpoints in public health, a single global policy, especially one reflecting Western ethics or the ethics prevalent in high-income countries, is impractical. This paper argues for a culturally sensitive, adaptable framework for the use of embryonic stem cells. Stem cell policy should accommodate varying ethical viewpoints and promote an effective global dialogue. With an extension of an ethics model that can adapt to various cultures, we recommend localized guidelines that reflect the moral views of the people those guidelines serve.
Stem cells, characterized by their unique ability to differentiate into various cell types, enable the repair or replacement of damaged tissues. Two primary types of stem cells are somatic stem cells (adult stem cells) and embryonic stem cells. Adult stem cells exist in developed tissues and maintain the body’s repair processes. [1] Embryonic stem cells (ESC) are remarkably pluripotent or versatile, making them valuable in research. [2] However, the use of ESCs has sparked ethics debates. Considering the potential of embryonic stem cells, research guidelines are essential. The International Society for Stem Cell Research (ISSCR) provides international stem cell research guidelines. They call for “public conversations touching on the scientific significance as well as the societal and ethical issues raised by ESC research.” [3] The ISSCR also publishes updates about culturing human embryos 14 days post fertilization, suggesting local policies and regulations should continue to evolve as ESC research develops. [4] Like the ISSCR, which calls for local law and policy to adapt to developing stem cell research given cultural acceptance, this paper highlights the importance of local social factors such as religion and culture.
I. Global Cultural Perspective of Embryonic Stem Cells
Views on ESCs vary throughout the world. Some countries readily embrace stem cell research and therapies, while others have stricter regulations due to ethical concerns surrounding embryonic stem cells and when an embryo becomes entitled to moral consideration. The philosophical issue of when the “someone” begins to be a human after fertilization, in the morally relevant sense, [5] impacts when an embryo becomes not just worthy of protection but morally entitled to it. The process of creating embryonic stem cell lines involves the destruction of the embryos for research. [6] Consequently, global engagement in ESC research depends on social-cultural acceptability.
a. US and Rights-Based Cultures
In the United States, attitudes toward stem cell therapies are diverse. The ethics and social approaches, which value individualism, [7] trigger debates regarding the destruction of human embryos, creating a complex regulatory environment. For example, the 1996 Dickey-Wicker Amendment prohibited federal funding for the creation of embryos for research and the destruction of embryos for “more than allowed for research on fetuses in utero.” [8] Following suit, in 2001, the Bush Administration heavily restricted stem cell lines for research. However, the Stem Cell Research Enhancement Act of 2005 was proposed to help develop ESC research but was ultimately vetoed. [9] Under the Obama administration, in 2009, an executive order lifted restrictions allowing for more development in this field. [10] The flux of research capacity and funding parallels the different cultural perceptions of human dignity of the embryo and how it is socially presented within the country’s research culture. [11]
b. Ubuntu and Collective Cultures
African bioethics differs from Western individualism because of the different traditions and values. African traditions, as described by individuals from South Africa and supported by some studies in other African countries, including Ghana and Kenya, follow the African moral philosophies of Ubuntu or Botho and Ukama , which “advocates for a form of wholeness that comes through one’s relationship and connectedness with other people in the society,” [12] making autonomy a socially collective concept. In this context, for the community to act autonomously, individuals would come together to decide what is best for the collective. Thus, stem cell research would require examining the value of the research to society as a whole and the use of the embryos as a collective societal resource. If society views the source as part of the collective whole, and opposes using stem cells, compromising the cultural values to pursue research may cause social detachment and stunt research growth. [13] Based on local culture and moral philosophy, the permissibility of stem cell research depends on how embryo, stem cell, and cell line therapies relate to the community as a whole . Ubuntu is the expression of humanness, with the person’s identity drawn from the “’I am because we are’” value. [14] The decision in a collectivistic culture becomes one born of cultural context, and individual decisions give deference to others in the society.
Consent differs in cultures where thought and moral philosophy are based on a collective paradigm. So, applying Western bioethical concepts is unrealistic. For one, Africa is a diverse continent with many countries with different belief systems, access to health care, and reliance on traditional or Western medicines. Where traditional medicine is the primary treatment, the “’restrictive focus on biomedically-related bioethics’” [is] problematic in African contexts because it neglects bioethical issues raised by traditional systems.” [15] No single approach applies in all areas or contexts. Rather than evaluating the permissibility of ESC research according to Western concepts such as the four principles approach, different ethics approaches should prevail.
Another consideration is the socio-economic standing of countries. In parts of South Africa, researchers have not focused heavily on contributing to the stem cell discourse, either because it is not considered health care or a health science priority or because resources are unavailable. [16] Each country’s priorities differ given different social, political, and economic factors. In South Africa, for instance, areas such as maternal mortality, non-communicable diseases, telemedicine, and the strength of health systems need improvement and require more focus. [17] Stem cell research could benefit the population, but it also could divert resources from basic medical care. Researchers in South Africa adhere to the National Health Act and Medicines Control Act in South Africa and international guidelines; however, the Act is not strictly enforced, and there is no clear legislation for research conduct or ethical guidelines. [18]
Some parts of Africa condemn stem cell research. For example, 98.2 percent of the Tunisian population is Muslim. [19] Tunisia does not permit stem cell research because of moral conflict with a Fatwa. Religion heavily saturates the regulation and direction of research. [20] Stem cell use became permissible for reproductive purposes only recently, with tight restrictions preventing cells from being used in any research other than procedures concerning ART/IVF. Their use is conditioned on consent, and available only to married couples. [21] The community's receptiveness to stem cell research depends on including communitarian African ethics.
c. Asia
Some Asian countries also have a collective model of ethics and decision making. [22] In China, the ethics model promotes a sincere respect for life or human dignity, [23] based on protective medicine. This model, influenced by Traditional Chinese Medicine (TCM), [24] recognizes Qi as the vital energy delivered via the meridians of the body; it connects illness to body systems, the body’s entire constitution, and the universe for a holistic bond of nature, health, and quality of life. [25] Following a protective ethics model, and traditional customs of wholeness, investment in stem cell research is heavily desired for its applications in regenerative therapies, disease modeling, and protective medicines. In a survey of medical students and healthcare practitioners, 30.8 percent considered stem cell research morally unacceptable while 63.5 percent accepted medical research using human embryonic stem cells. Of these individuals, 89.9 percent supported increased funding for stem cell research. [26] The scientific community might not reflect the overall population. From 1997 to 2019, China spent a total of $576 million (USD) on stem cell research at 8,050 stem cell programs, increased published presence from 0.6 percent to 14.01 percent of total global stem cell publications as of 2014, and made significant strides in cell-based therapies for various medical conditions. [27] However, while China has made substantial investments in stem cell research and achieved notable progress in clinical applications, concerns linger regarding ethical oversight and transparency. [28] For example, the China Biosecurity Law, promoted by the National Health Commission and China Hospital Association, attempted to mitigate risks by introducing an institutional review board (IRB) in the regulatory bodies. 5800 IRBs registered with the Chinese Clinical Trial Registry since 2021. [29] However, issues still need to be addressed in implementing effective IRB review and approval procedures.
The substantial government funding and focus on scientific advancement have sometimes overshadowed considerations of regional cultures, ethnic minorities, and individual perspectives, particularly evident during the one-child policy era. As government policy adapts to promote public stability, such as the change from the one-child to the two-child policy, [30] research ethics should also adapt to ensure respect for the values of its represented peoples.
Japan is also relatively supportive of stem cell research and therapies. Japan has a more transparent regulatory framework, allowing for faster approval of regenerative medicine products, which has led to several advanced clinical trials and therapies. [31] South Korea is also actively engaged in stem cell research and has a history of breakthroughs in cloning and embryonic stem cells. [32] However, the field is controversial, and there are issues of scientific integrity. For example, the Korean FDA fast-tracked products for approval, [33] and in another instance, the oocyte source was unclear and possibly violated ethical standards. [34] Trust is important in research, as it builds collaborative foundations between colleagues, trial participant comfort, open-mindedness for complicated and sensitive discussions, and supports regulatory procedures for stakeholders. There is a need to respect the culture’s interest, engagement, and for research and clinical trials to be transparent and have ethical oversight to promote global research discourse and trust.
d. Middle East
Countries in the Middle East have varying degrees of acceptance of or restrictions to policies related to using embryonic stem cells due to cultural and religious influences. Saudi Arabia has made significant contributions to stem cell research, and conducts research based on international guidelines for ethical conduct and under strict adherence to guidelines in accordance with Islamic principles. Specifically, the Saudi government and people require ESC research to adhere to Sharia law. In addition to umbilical and placental stem cells, [35] Saudi Arabia permits the use of embryonic stem cells as long as they come from miscarriages, therapeutic abortions permissible by Sharia law, or are left over from in vitro fertilization and donated to research. [36] Laws and ethical guidelines for stem cell research allow the development of research institutions such as the King Abdullah International Medical Research Center, which has a cord blood bank and a stem cell registry with nearly 10,000 donors. [37] Such volume and acceptance are due to the ethical ‘permissibility’ of the donor sources, which do not conflict with religious pillars. However, some researchers err on the side of caution, choosing not to use embryos or fetal tissue as they feel it is unethical to do so. [38]
Jordan has a positive research ethics culture. [39] However, there is a significant issue of lack of trust in researchers, with 45.23 percent (38.66 percent agreeing and 6.57 percent strongly agreeing) of Jordanians holding a low level of trust in researchers, compared to 81.34 percent of Jordanians agreeing that they feel safe to participate in a research trial. [40] Safety testifies to the feeling of confidence that adequate measures are in place to protect participants from harm, whereas trust in researchers could represent the confidence in researchers to act in the participants’ best interests, adhere to ethical guidelines, provide accurate information, and respect participants’ rights and dignity. One method to improve trust would be to address communication issues relevant to ESC. Legislation surrounding stem cell research has adopted specific language, especially concerning clarification “between ‘stem cells’ and ‘embryonic stem cells’” in translation. [41] Furthermore, legislation “mandates the creation of a national committee… laying out specific regulations for stem-cell banking in accordance with international standards.” [42] This broad regulation opens the door for future global engagement and maintains transparency. However, these regulations may also constrain the influence of research direction, pace, and accessibility of research outcomes.
e. Europe
In the European Union (EU), ethics is also principle-based, but the principles of autonomy, dignity, integrity, and vulnerability are interconnected. [43] As such, the opportunity for cohesion and concessions between individuals’ thoughts and ideals allows for a more adaptable ethics model due to the flexible principles that relate to the human experience The EU has put forth a framework in its Convention for the Protection of Human Rights and Dignity of the Human Being allowing member states to take different approaches. Each European state applies these principles to its specific conventions, leading to or reflecting different acceptance levels of stem cell research. [44]
For example, in Germany, Lebenzusammenhang , or the coherence of life, references integrity in the unity of human culture. Namely, the personal sphere “should not be subject to external intervention.” [45] Stem cell interventions could affect this concept of bodily completeness, leading to heavy restrictions. Under the Grundgesetz, human dignity and the right to life with physical integrity are paramount. [46] The Embryo Protection Act of 1991 made producing cell lines illegal. Cell lines can be imported if approved by the Central Ethics Commission for Stem Cell Research only if they were derived before May 2007. [47] Stem cell research respects the integrity of life for the embryo with heavy specifications and intense oversight. This is vastly different in Finland, where the regulatory bodies find research more permissible in IVF excess, but only up to 14 days after fertilization. [48] Spain’s approach differs still, with a comprehensive regulatory framework. [49] Thus, research regulation can be culture-specific due to variations in applied principles. Diverse cultures call for various approaches to ethical permissibility. [50] Only an adaptive-deliberative model can address the cultural constructions of self and achieve positive, culturally sensitive stem cell research practices. [51]
II. Religious Perspectives on ESC
Embryonic stem cell sources are the main consideration within religious contexts. While individuals may not regard their own religious texts as authoritative or factual, religion can shape their foundations or perspectives.
The Qur'an states:
“And indeed We created man from a quintessence of clay. Then We placed within him a small quantity of nutfa (sperm to fertilize) in a safe place. Then We have fashioned the nutfa into an ‘alaqa (clinging clot or cell cluster), then We developed the ‘alaqa into mudgha (a lump of flesh), and We made mudgha into bones, and clothed the bones with flesh, then We brought it into being as a new creation. So Blessed is Allah, the Best of Creators.” [52]
Many scholars of Islam estimate the time of soul installment, marked by the angel breathing in the soul to bring the individual into creation, as 120 days from conception. [53] Personhood begins at this point, and the value of life would prohibit research or experimentation that could harm the individual. If the fetus is more than 120 days old, the time ensoulment is interpreted to occur according to Islamic law, abortion is no longer permissible. [54] There are a few opposing opinions about early embryos in Islamic traditions. According to some Islamic theologians, there is no ensoulment of the early embryo, which is the source of stem cells for ESC research. [55]
In Buddhism, the stance on stem cell research is not settled. The main tenets, the prohibition against harming or destroying others (ahimsa) and the pursuit of knowledge (prajña) and compassion (karuna), leave Buddhist scholars and communities divided. [56] Some scholars argue stem cell research is in accordance with the Buddhist tenet of seeking knowledge and ending human suffering. Others feel it violates the principle of not harming others. Finding the balance between these two points relies on the karmic burden of Buddhist morality. In trying to prevent ahimsa towards the embryo, Buddhist scholars suggest that to comply with Buddhist tenets, research cannot be done as the embryo has personhood at the moment of conception and would reincarnate immediately, harming the individual's ability to build their karmic burden. [57] On the other hand, the Bodhisattvas, those considered to be on the path to enlightenment or Nirvana, have given organs and flesh to others to help alleviate grieving and to benefit all. [58] Acceptance varies on applied beliefs and interpretations.
Catholicism does not support embryonic stem cell research, as it entails creation or destruction of human embryos. This destruction conflicts with the belief in the sanctity of life. For example, in the Old Testament, Genesis describes humanity as being created in God’s image and multiplying on the Earth, referencing the sacred rights to human conception and the purpose of development and life. In the Ten Commandments, the tenet that one should not kill has numerous interpretations where killing could mean murder or shedding of the sanctity of life, demonstrating the high value of human personhood. In other books, the theological conception of when life begins is interpreted as in utero, [59] highlighting the inviolability of life and its formation in vivo to make a religious point for accepting such research as relatively limited, if at all. [60] The Vatican has released ethical directives to help apply a theological basis to modern-day conflicts. The Magisterium of the Church states that “unless there is a moral certainty of not causing harm,” experimentation on fetuses, fertilized cells, stem cells, or embryos constitutes a crime. [61] Such procedures would not respect the human person who exists at these stages, according to Catholicism. Damages to the embryo are considered gravely immoral and illicit. [62] Although the Catholic Church officially opposes abortion, surveys demonstrate that many Catholic people hold pro-choice views, whether due to the context of conception, stage of pregnancy, threat to the mother’s life, or for other reasons, demonstrating that practicing members can also accept some but not all tenets. [63]
Some major Jewish denominations, such as the Reform, Conservative, and Reconstructionist movements, are open to supporting ESC use or research as long as it is for saving a life. [64] Within Judaism, the Talmud, or study, gives personhood to the child at birth and emphasizes that life does not begin at conception: [65]
“If she is found pregnant, until the fortieth day it is mere fluid,” [66]
Whereas most religions prioritize the status of human embryos, the Halakah (Jewish religious law) states that to save one life, most other religious laws can be ignored because it is in pursuit of preservation. [67] Stem cell research is accepted due to application of these religious laws.
We recognize that all religions contain subsets and sects. The variety of environmental and cultural differences within religious groups requires further analysis to respect the flexibility of religious thoughts and practices. We make no presumptions that all cultures require notions of autonomy or morality as under the common morality theory , which asserts a set of universal moral norms that all individuals share provides moral reasoning and guides ethical decisions. [68] We only wish to show that the interaction with morality varies between cultures and countries.
III. A Flexible Ethical Approach
The plurality of different moral approaches described above demonstrates that there can be no universally acceptable uniform law for ESC on a global scale. Instead of developing one standard, flexible ethical applications must be continued. We recommend local guidelines that incorporate important cultural and ethical priorities.
While the Declaration of Helsinki is more relevant to people in clinical trials receiving ESC products, in keeping with the tradition of protections for research subjects, consent of the donor is an ethical requirement for ESC donation in many jurisdictions including the US, Canada, and Europe. [69] The Declaration of Helsinki provides a reference point for regulatory standards and could potentially be used as a universal baseline for obtaining consent prior to gamete or embryo donation.
For instance, in Columbia University’s egg donor program for stem cell research, donors followed standard screening protocols and “underwent counseling sessions that included information as to the purpose of oocyte donation for research, what the oocytes would be used for, the risks and benefits of donation, and process of oocyte stimulation” to ensure transparency for consent. [70] The program helped advance stem cell research and provided clear and safe research methods with paid participants. Though paid participation or covering costs of incidental expenses may not be socially acceptable in every culture or context, [71] and creating embryos for ESC research is illegal in many jurisdictions, Columbia’s program was effective because of the clear and honest communications with donors, IRBs, and related stakeholders. This example demonstrates that cultural acceptance of scientific research and of the idea that an egg or embryo does not have personhood is likely behind societal acceptance of donating eggs for ESC research. As noted, many countries do not permit the creation of embryos for research.
Proper communication and education regarding the process and purpose of stem cell research may bolster comprehension and garner more acceptance. “Given the sensitive subject material, a complete consent process can support voluntary participation through trust, understanding, and ethical norms from the cultures and morals participants value. This can be hard for researchers entering countries of different socioeconomic stability, with different languages and different societal values. [72]
An adequate moral foundation in medical ethics is derived from the cultural and religious basis that informs knowledge and actions. [73] Understanding local cultural and religious values and their impact on research could help researchers develop humility and promote inclusion.
IV. Concerns
Some may argue that if researchers all adhere to one ethics standard, protection will be satisfied across all borders, and the global public will trust researchers. However, defining what needs to be protected and how to define such research standards is very specific to the people to which standards are applied. We suggest that applying one uniform guide cannot accurately protect each individual because we all possess our own perceptions and interpretations of social values. [74] Therefore, the issue of not adjusting to the moral pluralism between peoples in applying one standard of ethics can be resolved by building out ethics models that can be adapted to different cultures and religions.
Other concerns include medical tourism, which may promote health inequities. [75] Some countries may develop and approve products derived from ESC research before others, compromising research ethics or drug approval processes. There are also concerns about the sale of unauthorized stem cell treatments, for example, those without FDA approval in the United States. Countries with robust research infrastructures may be tempted to attract medical tourists, and some customers will have false hopes based on aggressive publicity of unproven treatments. [76]
For example, in China, stem cell clinics can market to foreign clients who are not protected under the regulatory regimes. Companies employ a marketing strategy of “ethically friendly” therapies. Specifically, in the case of Beike, China’s leading stem cell tourism company and sprouting network, ethical oversight of administrators or health bureaus at one site has “the unintended consequence of shifting questionable activities to another node in Beike's diffuse network.” [77] In contrast, Jordan is aware of stem cell research’s potential abuse and its own status as a “health-care hub.” Jordan’s expanded regulations include preserving the interests of individuals in clinical trials and banning private companies from ESC research to preserve transparency and the integrity of research practices. [78]
The social priorities of the community are also a concern. The ISSCR explicitly states that guidelines “should be periodically revised to accommodate scientific advances, new challenges, and evolving social priorities.” [79] The adaptable ethics model extends this consideration further by addressing whether research is warranted given the varying degrees of socioeconomic conditions, political stability, and healthcare accessibilities and limitations. An ethical approach would require discussion about resource allocation and appropriate distribution of funds. [80]
While some religions emphasize the sanctity of life from conception, which may lead to public opposition to ESC research, others encourage ESC research due to its potential for healing and alleviating human pain. Many countries have special regulations that balance local views on embryonic personhood, the benefits of research as individual or societal goods, and the protection of human research subjects. To foster understanding and constructive dialogue, global policy frameworks should prioritize the protection of universal human rights, transparency, and informed consent. In addition to these foundational global policies, we recommend tailoring local guidelines to reflect the diverse cultural and religious perspectives of the populations they govern. Ethics models should be adapted to local populations to effectively establish research protections, growth, and possibilities of stem cell research.
For example, in countries with strong beliefs in the moral sanctity of embryos or heavy religious restrictions, an adaptive model can allow for discussion instead of immediate rejection. In countries with limited individual rights and voice in science policy, an adaptive model ensures cultural, moral, and religious views are taken into consideration, thereby building social inclusion. While this ethical consideration by the government may not give a complete voice to every individual, it will help balance policies and maintain the diverse perspectives of those it affects. Embracing an adaptive ethics model of ESC research promotes open-minded dialogue and respect for the importance of human belief and tradition. By actively engaging with cultural and religious values, researchers can better handle disagreements and promote ethical research practices that benefit each society.
This brief exploration of the religious and cultural differences that impact ESC research reveals the nuances of relative ethics and highlights a need for local policymakers to apply a more intense adaptive model.
[1] Poliwoda, S., Noor, N., Downs, E., Schaaf, A., Cantwell, A., Ganti, L., Kaye, A. D., Mosel, L. I., Carroll, C. B., Viswanath, O., & Urits, I. (2022). Stem cells: a comprehensive review of origins and emerging clinical roles in medical practice. Orthopedic reviews , 14 (3), 37498. https://doi.org/10.52965/001c.37498
[2] Poliwoda, S., Noor, N., Downs, E., Schaaf, A., Cantwell, A., Ganti, L., Kaye, A. D., Mosel, L. I., Carroll, C. B., Viswanath, O., & Urits, I. (2022). Stem cells: a comprehensive review of origins and emerging clinical roles in medical practice. Orthopedic reviews , 14 (3), 37498. https://doi.org/10.52965/001c.37498
[3] International Society for Stem Cell Research. (2023). Laboratory-based human embryonic stem cell research, embryo research, and related research activities . International Society for Stem Cell Research. https://www.isscr.org/guidelines/blog-post-title-one-ed2td-6fcdk ; Kimmelman, J., Hyun, I., Benvenisty, N. et al. Policy: Global standards for stem-cell research. Nature 533 , 311–313 (2016). https://doi.org/10.1038/533311a
[4] International Society for Stem Cell Research. (2023). Laboratory-based human embryonic stem cell research, embryo research, and related research activities . International Society for Stem Cell Research. https://www.isscr.org/guidelines/blog-post-title-one-ed2td-6fcdk
[5] Concerning the moral philosophies of stem cell research, our paper does not posit a personal moral stance nor delve into the “when” of human life begins. To read further about the philosophical debate, consider the following sources:
Sandel M. J. (2004). Embryo ethics--the moral logic of stem-cell research. The New England journal of medicine , 351 (3), 207–209. https://doi.org/10.1056/NEJMp048145 ; George, R. P., & Lee, P. (2020, September 26). Acorns and Embryos . The New Atlantis. https://www.thenewatlantis.com/publications/acorns-and-embryos ; Sagan, A., & Singer, P. (2007). The moral status of stem cells. Metaphilosophy , 38 (2/3), 264–284. http://www.jstor.org/stable/24439776 ; McHugh P. R. (2004). Zygote and "clonote"--the ethical use of embryonic stem cells. The New England journal of medicine , 351 (3), 209–211. https://doi.org/10.1056/NEJMp048147 ; Kurjak, A., & Tripalo, A. (2004). The facts and doubts about beginning of the human life and personality. Bosnian journal of basic medical sciences , 4 (1), 5–14. https://doi.org/10.17305/bjbms.2004.3453
[6] Vazin, T., & Freed, W. J. (2010). Human embryonic stem cells: derivation, culture, and differentiation: a review. Restorative neurology and neuroscience , 28 (4), 589–603. https://doi.org/10.3233/RNN-2010-0543
[7] Socially, at its core, the Western approach to ethics is widely principle-based, autonomy being one of the key factors to ensure a fundamental respect for persons within research. For information regarding autonomy in research, see: Department of Health, Education, and Welfare, & National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research (1978). The Belmont Report. Ethical principles and guidelines for the protection of human subjects of research.; For a more in-depth review of autonomy within the US, see: Beauchamp, T. L., & Childress, J. F. (1994). Principles of Biomedical Ethics . Oxford University Press.
[8] Sherley v. Sebelius , 644 F.3d 388 (D.C. Cir. 2011), citing 45 C.F.R. 46.204(b) and [42 U.S.C. § 289g(b)]. https://www.cadc.uscourts.gov/internet/opinions.nsf/6c690438a9b43dd685257a64004ebf99/$file/11-5241-1391178.pdf
[9] Stem Cell Research Enhancement Act of 2005, H. R. 810, 109 th Cong. (2001). https://www.govtrack.us/congress/bills/109/hr810/text ; Bush, G. W. (2006, July 19). Message to the House of Representatives . National Archives and Records Administration. https://georgewbush-whitehouse.archives.gov/news/releases/2006/07/20060719-5.html
[10] National Archives and Records Administration. (2009, March 9). Executive order 13505 -- removing barriers to responsible scientific research involving human stem cells . National Archives and Records Administration. https://obamawhitehouse.archives.gov/the-press-office/removing-barriers-responsible-scientific-research-involving-human-stem-cells
[11] Hurlbut, W. B. (2006). Science, Religion, and the Politics of Stem Cells. Social Research , 73 (3), 819–834. http://www.jstor.org/stable/40971854
[12] Akpa-Inyang, Francis & Chima, Sylvester. (2021). South African traditional values and beliefs regarding informed consent and limitations of the principle of respect for autonomy in African communities: a cross-cultural qualitative study. BMC Medical Ethics . 22. 10.1186/s12910-021-00678-4.
[13] Source for further reading: Tangwa G. B. (2007). Moral status of embryonic stem cells: perspective of an African villager. Bioethics , 21(8), 449–457. https://doi.org/10.1111/j.1467-8519.2007.00582.x , see also Mnisi, F. M. (2020). An African analysis based on ethics of Ubuntu - are human embryonic stem cell patents morally justifiable? African Insight , 49 (4).
[14] Jecker, N. S., & Atuire, C. (2021). Bioethics in Africa: A contextually enlightened analysis of three cases. Developing World Bioethics , 22 (2), 112–122. https://doi.org/10.1111/dewb.12324
[15] Jecker, N. S., & Atuire, C. (2021). Bioethics in Africa: A contextually enlightened analysis of three cases. Developing World Bioethics, 22(2), 112–122. https://doi.org/10.1111/dewb.12324
[16] Jackson, C.S., Pepper, M.S. Opportunities and barriers to establishing a cell therapy programme in South Africa. Stem Cell Res Ther 4 , 54 (2013). https://doi.org/10.1186/scrt204 ; Pew Research Center. (2014, May 1). Public health a major priority in African nations . Pew Research Center’s Global Attitudes Project. https://www.pewresearch.org/global/2014/05/01/public-health-a-major-priority-in-african-nations/
[17] Department of Health Republic of South Africa. (2021). Health Research Priorities (revised) for South Africa 2021-2024 . National Health Research Strategy. https://www.health.gov.za/wp-content/uploads/2022/05/National-Health-Research-Priorities-2021-2024.pdf
[18] Oosthuizen, H. (2013). Legal and Ethical Issues in Stem Cell Research in South Africa. In: Beran, R. (eds) Legal and Forensic Medicine. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-32338-6_80 , see also: Gaobotse G (2018) Stem Cell Research in Africa: Legislation and Challenges. J Regen Med 7:1. doi: 10.4172/2325-9620.1000142
[19] United States Bureau of Citizenship and Immigration Services. (1998). Tunisia: Information on the status of Christian conversions in Tunisia . UNHCR Web Archive. https://webarchive.archive.unhcr.org/20230522142618/https://www.refworld.org/docid/3df0be9a2.html
[20] Gaobotse, G. (2018) Stem Cell Research in Africa: Legislation and Challenges. J Regen Med 7:1. doi: 10.4172/2325-9620.1000142
[21] Kooli, C. Review of assisted reproduction techniques, laws, and regulations in Muslim countries. Middle East Fertil Soc J 24 , 8 (2020). https://doi.org/10.1186/s43043-019-0011-0 ; Gaobotse, G. (2018) Stem Cell Research in Africa: Legislation and Challenges. J Regen Med 7:1. doi: 10.4172/2325-9620.1000142
[22] Pang M. C. (1999). Protective truthfulness: the Chinese way of safeguarding patients in informed treatment decisions. Journal of medical ethics , 25(3), 247–253. https://doi.org/10.1136/jme.25.3.247
[23] Wang, L., Wang, F., & Zhang, W. (2021). Bioethics in China’s biosecurity law: Forms, effects, and unsettled issues. Journal of law and the biosciences , 8(1). https://doi.org/10.1093/jlb/lsab019 https://academic.oup.com/jlb/article/8/1/lsab019/6299199
[24] Wang, Y., Xue, Y., & Guo, H. D. (2022). Intervention effects of traditional Chinese medicine on stem cell therapy of myocardial infarction. Frontiers in pharmacology , 13 , 1013740. https://doi.org/10.3389/fphar.2022.1013740
[25] Li, X.-T., & Zhao, J. (2012). Chapter 4: An Approach to the Nature of Qi in TCM- Qi and Bioenergy. In Recent Advances in Theories and Practice of Chinese Medicine (p. 79). InTech.
[26] Luo, D., Xu, Z., Wang, Z., & Ran, W. (2021). China's Stem Cell Research and Knowledge Levels of Medical Practitioners and Students. Stem cells international , 2021 , 6667743. https://doi.org/10.1155/2021/6667743
[27] Luo, D., Xu, Z., Wang, Z., & Ran, W. (2021). China's Stem Cell Research and Knowledge Levels of Medical Practitioners and Students. Stem cells international , 2021 , 6667743. https://doi.org/10.1155/2021/6667743
[28] Zhang, J. Y. (2017). Lost in translation? accountability and governance of Clinical Stem Cell Research in China. Regenerative Medicine , 12 (6), 647–656. https://doi.org/10.2217/rme-2017-0035
[29] Wang, L., Wang, F., & Zhang, W. (2021). Bioethics in China’s biosecurity law: Forms, effects, and unsettled issues. Journal of law and the biosciences , 8(1). https://doi.org/10.1093/jlb/lsab019 https://academic.oup.com/jlb/article/8/1/lsab019/6299199
[30] Chen, H., Wei, T., Wang, H. et al. Association of China’s two-child policy with changes in number of births and birth defects rate, 2008–2017. BMC Public Health 22 , 434 (2022). https://doi.org/10.1186/s12889-022-12839-0
[31] Azuma, K. Regulatory Landscape of Regenerative Medicine in Japan. Curr Stem Cell Rep 1 , 118–128 (2015). https://doi.org/10.1007/s40778-015-0012-6
[32] Harris, R. (2005, May 19). Researchers Report Advance in Stem Cell Production . NPR. https://www.npr.org/2005/05/19/4658967/researchers-report-advance-in-stem-cell-production
[33] Park, S. (2012). South Korea steps up stem-cell work. Nature . https://doi.org/10.1038/nature.2012.10565
[34] Resnik, D. B., Shamoo, A. E., & Krimsky, S. (2006). Fraudulent human embryonic stem cell research in South Korea: lessons learned. Accountability in research , 13 (1), 101–109. https://doi.org/10.1080/08989620600634193 .
[35] Alahmad, G., Aljohani, S., & Najjar, M. F. (2020). Ethical challenges regarding the use of stem cells: interviews with researchers from Saudi Arabia. BMC medical ethics, 21(1), 35. https://doi.org/10.1186/s12910-020-00482-6
[36] Association for the Advancement of Blood and Biotherapies. https://www.aabb.org/regulatory-and-advocacy/regulatory-affairs/regulatory-for-cellular-therapies/international-competent-authorities/saudi-arabia
[37] Alahmad, G., Aljohani, S., & Najjar, M. F. (2020). Ethical challenges regarding the use of stem cells: Interviews with researchers from Saudi Arabia. BMC medical ethics , 21 (1), 35. https://doi.org/10.1186/s12910-020-00482-6
[38] Alahmad, G., Aljohani, S., & Najjar, M. F. (2020). Ethical challenges regarding the use of stem cells: Interviews with researchers from Saudi Arabia. BMC medical ethics , 21(1), 35. https://doi.org/10.1186/s12910-020-00482-6
Culturally, autonomy practices follow a relational autonomy approach based on a paternalistic deontological health care model. The adherence to strict international research policies and religious pillars within the regulatory environment is a great foundation for research ethics. However, there is a need to develop locally targeted ethics approaches for research (as called for in Alahmad, G., Aljohani, S., & Najjar, M. F. (2020). Ethical challenges regarding the use of stem cells: interviews with researchers from Saudi Arabia. BMC medical ethics, 21(1), 35. https://doi.org/10.1186/s12910-020-00482-6), this decision-making approach may help advise a research decision model. For more on the clinical cultural autonomy approaches, see: Alabdullah, Y. Y., Alzaid, E., Alsaad, S., Alamri, T., Alolayan, S. W., Bah, S., & Aljoudi, A. S. (2022). Autonomy and paternalism in Shared decision‐making in a Saudi Arabian tertiary hospital: A cross‐sectional study. Developing World Bioethics , 23 (3), 260–268. https://doi.org/10.1111/dewb.12355 ; Bukhari, A. A. (2017). Universal Principles of Bioethics and Patient Rights in Saudi Arabia (Doctoral dissertation, Duquesne University). https://dsc.duq.edu/etd/124; Ladha, S., Nakshawani, S. A., Alzaidy, A., & Tarab, B. (2023, October 26). Islam and Bioethics: What We All Need to Know . Columbia University School of Professional Studies. https://sps.columbia.edu/events/islam-and-bioethics-what-we-all-need-know
[39] Ababneh, M. A., Al-Azzam, S. I., Alzoubi, K., Rababa’h, A., & Al Demour, S. (2021). Understanding and attitudes of the Jordanian public about clinical research ethics. Research Ethics , 17 (2), 228-241. https://doi.org/10.1177/1747016120966779
[40] Ababneh, M. A., Al-Azzam, S. I., Alzoubi, K., Rababa’h, A., & Al Demour, S. (2021). Understanding and attitudes of the Jordanian public about clinical research ethics. Research Ethics , 17 (2), 228-241. https://doi.org/10.1177/1747016120966779
[41] Dajani, R. (2014). Jordan’s stem-cell law can guide the Middle East. Nature 510, 189. https://doi.org/10.1038/510189a
[42] Dajani, R. (2014). Jordan’s stem-cell law can guide the Middle East. Nature 510, 189. https://doi.org/10.1038/510189a
[43] The EU’s definition of autonomy relates to the capacity for creating ideas, moral insight, decisions, and actions without constraint, personal responsibility, and informed consent. However, the EU views autonomy as not completely able to protect individuals and depends on other principles, such as dignity, which “expresses the intrinsic worth and fundamental equality of all human beings.” Rendtorff, J.D., Kemp, P. (2019). Four Ethical Principles in European Bioethics and Biolaw: Autonomy, Dignity, Integrity and Vulnerability. In: Valdés, E., Lecaros, J. (eds) Biolaw and Policy in the Twenty-First Century. International Library of Ethics, Law, and the New Medicine, vol 78. Springer, Cham. https://doi.org/10.1007/978-3-030-05903-3_3
[44] Council of Europe. Convention for the protection of Human Rights and Dignity of the Human Being with regard to the Application of Biology and Medicine: Convention on Human Rights and Biomedicine (ETS No. 164) https://www.coe.int/en/web/conventions/full-list?module=treaty-detail&treatynum=164 (forbidding the creation of embryos for research purposes only, and suggests embryos in vitro have protections.); Also see Drabiak-Syed B. K. (2013). New President, New Human Embryonic Stem Cell Research Policy: Comparative International Perspectives and Embryonic Stem Cell Research Laws in France. Biotechnology Law Report , 32 (6), 349–356. https://doi.org/10.1089/blr.2013.9865
[45] Rendtorff, J.D., Kemp, P. (2019). Four Ethical Principles in European Bioethics and Biolaw: Autonomy, Dignity, Integrity and Vulnerability. In: Valdés, E., Lecaros, J. (eds) Biolaw and Policy in the Twenty-First Century. International Library of Ethics, Law, and the New Medicine, vol 78. Springer, Cham. https://doi.org/10.1007/978-3-030-05903-3_3
[46] Tomuschat, C., Currie, D. P., Kommers, D. P., & Kerr, R. (Trans.). (1949, May 23). Basic law for the Federal Republic of Germany. https://www.btg-bestellservice.de/pdf/80201000.pdf
[47] Regulation of Stem Cell Research in Germany . Eurostemcell. (2017, April 26). https://www.eurostemcell.org/regulation-stem-cell-research-germany
[48] Regulation of Stem Cell Research in Finland . Eurostemcell. (2017, April 26). https://www.eurostemcell.org/regulation-stem-cell-research-finland
[49] Regulation of Stem Cell Research in Spain . Eurostemcell. (2017, April 26). https://www.eurostemcell.org/regulation-stem-cell-research-spain
[50] Some sources to consider regarding ethics models or regulatory oversights of other cultures not covered:
Kara MA. Applicability of the principle of respect for autonomy: the perspective of Turkey. J Med Ethics. 2007 Nov;33(11):627-30. doi: 10.1136/jme.2006.017400. PMID: 17971462; PMCID: PMC2598110.
Ugarte, O. N., & Acioly, M. A. (2014). The principle of autonomy in Brazil: one needs to discuss it ... Revista do Colegio Brasileiro de Cirurgioes , 41 (5), 374–377. https://doi.org/10.1590/0100-69912014005013
Bharadwaj, A., & Glasner, P. E. (2012). Local cells, global science: The rise of embryonic stem cell research in India . Routledge.
For further research on specific European countries regarding ethical and regulatory framework, we recommend this database: Regulation of Stem Cell Research in Europe . Eurostemcell. (2017, April 26). https://www.eurostemcell.org/regulation-stem-cell-research-europe
[51] Klitzman, R. (2006). Complications of culture in obtaining informed consent. The American Journal of Bioethics, 6(1), 20–21. https://doi.org/10.1080/15265160500394671 see also: Ekmekci, P. E., & Arda, B. (2017). Interculturalism and Informed Consent: Respecting Cultural Differences without Breaching Human Rights. Cultura (Iasi, Romania) , 14 (2), 159–172.; For why trust is important in research, see also: Gray, B., Hilder, J., Macdonald, L., Tester, R., Dowell, A., & Stubbe, M. (2017). Are research ethics guidelines culturally competent? Research Ethics , 13 (1), 23-41. https://doi.org/10.1177/1747016116650235
[52] The Qur'an (M. Khattab, Trans.). (1965). Al-Mu’minun, 23: 12-14. https://quran.com/23
[53] Lenfest, Y. (2017, December 8). Islam and the beginning of human life . Bill of Health. https://blog.petrieflom.law.harvard.edu/2017/12/08/islam-and-the-beginning-of-human-life/
[54] Aksoy, S. (2005). Making regulations and drawing up legislation in Islamic countries under conditions of uncertainty, with special reference to embryonic stem cell research. Journal of Medical Ethics , 31: 399-403.; see also: Mahmoud, Azza. "Islamic Bioethics: National Regulations and Guidelines of Human Stem Cell Research in the Muslim World." Master's thesis, Chapman University, 2022. https://doi.org/10.36837/ chapman.000386
[55] Rashid, R. (2022). When does Ensoulment occur in the Human Foetus. Journal of the British Islamic Medical Association , 12 (4). ISSN 2634 8071. https://www.jbima.com/wp-content/uploads/2023/01/2-Ethics-3_-Ensoulment_Rafaqat.pdf.
[56] Sivaraman, M. & Noor, S. (2017). Ethics of embryonic stem cell research according to Buddhist, Hindu, Catholic, and Islamic religions: perspective from Malaysia. Asian Biomedicine,8(1) 43-52. https://doi.org/10.5372/1905-7415.0801.260
[57] Jafari, M., Elahi, F., Ozyurt, S. & Wrigley, T. (2007). 4. Religious Perspectives on Embryonic Stem Cell Research. In K. Monroe, R. Miller & J. Tobis (Ed.), Fundamentals of the Stem Cell Debate: The Scientific, Religious, Ethical, and Political Issues (pp. 79-94). Berkeley: University of California Press. https://escholarship.org/content/qt9rj0k7s3/qt9rj0k7s3_noSplash_f9aca2e02c3777c7fb76ea768ba458f0.pdf https://doi.org/10.1525/9780520940994-005
[58] Lecso, P. A. (1991). The Bodhisattva Ideal and Organ Transplantation. Journal of Religion and Health , 30 (1), 35–41. http://www.jstor.org/stable/27510629 ; Bodhisattva, S. (n.d.). The Key of Becoming a Bodhisattva . A Guide to the Bodhisattva Way of Life. http://www.buddhism.org/Sutras/2/BodhisattvaWay.htm
[59] There is no explicit religious reference to when life begins or how to conduct research that interacts with the concept of life. However, these are relevant verses pertaining to how the fetus is viewed. (( King James Bible . (1999). Oxford University Press. (original work published 1769))
Jerimiah 1: 5 “Before I formed thee in the belly I knew thee; and before thou camest forth out of the womb I sanctified thee…”
In prophet Jerimiah’s insight, God set him apart as a person known before childbirth, a theme carried within the Psalm of David.
Psalm 139: 13-14 “…Thou hast covered me in my mother's womb. I will praise thee; for I am fearfully and wonderfully made…”
These verses demonstrate David’s respect for God as an entity that would know of all man’s thoughts and doings even before birth.
[60] It should be noted that abortion is not supported as well.
[61] The Vatican. (1987, February 22). Instruction on Respect for Human Life in Its Origin and on the Dignity of Procreation Replies to Certain Questions of the Day . Congregation For the Doctrine of the Faith. https://www.vatican.va/roman_curia/congregations/cfaith/documents/rc_con_cfaith_doc_19870222_respect-for-human-life_en.html
[62] The Vatican. (2000, August 25). Declaration On the Production and the Scientific and Therapeutic Use of Human Embryonic Stem Cells . Pontifical Academy for Life. https://www.vatican.va/roman_curia/pontifical_academies/acdlife/documents/rc_pa_acdlife_doc_20000824_cellule-staminali_en.html ; Ohara, N. (2003). Ethical Consideration of Experimentation Using Living Human Embryos: The Catholic Church’s Position on Human Embryonic Stem Cell Research and Human Cloning. Department of Obstetrics and Gynecology . Retrieved from https://article.imrpress.com/journal/CEOG/30/2-3/pii/2003018/77-81.pdf.
[63] Smith, G. A. (2022, May 23). Like Americans overall, Catholics vary in their abortion views, with regular mass attenders most opposed . Pew Research Center. https://www.pewresearch.org/short-reads/2022/05/23/like-americans-overall-catholics-vary-in-their-abortion-views-with-regular-mass-attenders-most-opposed/
[64] Rosner, F., & Reichman, E. (2002). Embryonic stem cell research in Jewish law. Journal of halacha and contemporary society , (43), 49–68.; Jafari, M., Elahi, F., Ozyurt, S. & Wrigley, T. (2007). 4. Religious Perspectives on Embryonic Stem Cell Research. In K. Monroe, R. Miller & J. Tobis (Ed.), Fundamentals of the Stem Cell Debate: The Scientific, Religious, Ethical, and Political Issues (pp. 79-94). Berkeley: University of California Press. https://escholarship.org/content/qt9rj0k7s3/qt9rj0k7s3_noSplash_f9aca2e02c3777c7fb76ea768ba458f0.pdf https://doi.org/10.1525/9780520940994-005
[65] Schenker J. G. (2008). The beginning of human life: status of embryo. Perspectives in Halakha (Jewish Religious Law). Journal of assisted reproduction and genetics , 25 (6), 271–276. https://doi.org/10.1007/s10815-008-9221-6
[66] Ruttenberg, D. (2020, May 5). The Torah of Abortion Justice (annotated source sheet) . Sefaria. https://www.sefaria.org/sheets/234926.7?lang=bi&with=all&lang2=en
[67] Jafari, M., Elahi, F., Ozyurt, S. & Wrigley, T. (2007). 4. Religious Perspectives on Embryonic Stem Cell Research. In K. Monroe, R. Miller & J. Tobis (Ed.), Fundamentals of the Stem Cell Debate: The Scientific, Religious, Ethical, and Political Issues (pp. 79-94). Berkeley: University of California Press. https://escholarship.org/content/qt9rj0k7s3/qt9rj0k7s3_noSplash_f9aca2e02c3777c7fb76ea768ba458f0.pdf https://doi.org/10.1525/9780520940994-005
[68] Gert, B. (2007). Common morality: Deciding what to do . Oxford Univ. Press.
[69] World Medical Association (2013). World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA , 310(20), 2191–2194. https://doi.org/10.1001/jama.2013.281053 Declaration of Helsinki – WMA – The World Medical Association .; see also: National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. (1979). The Belmont report: Ethical principles and guidelines for the protection of human subjects of research . U.S. Department of Health and Human Services. https://www.hhs.gov/ohrp/regulations-and-policy/belmont-report/read-the-belmont-report/index.html
[70] Zakarin Safier, L., Gumer, A., Kline, M., Egli, D., & Sauer, M. V. (2018). Compensating human subjects providing oocytes for stem cell research: 9-year experience and outcomes. Journal of assisted reproduction and genetics , 35 (7), 1219–1225. https://doi.org/10.1007/s10815-018-1171-z https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6063839/ see also: Riordan, N. H., & Paz Rodríguez, J. (2021). Addressing concerns regarding associated costs, transparency, and integrity of research in recent stem cell trial. Stem Cells Translational Medicine , 10 (12), 1715–1716. https://doi.org/10.1002/sctm.21-0234
[71] Klitzman, R., & Sauer, M. V. (2009). Payment of egg donors in stem cell research in the USA. Reproductive biomedicine online , 18 (5), 603–608. https://doi.org/10.1016/s1472-6483(10)60002-8
[72] Krosin, M. T., Klitzman, R., Levin, B., Cheng, J., & Ranney, M. L. (2006). Problems in comprehension of informed consent in rural and peri-urban Mali, West Africa. Clinical trials (London, England) , 3 (3), 306–313. https://doi.org/10.1191/1740774506cn150oa
[73] Veatch, Robert M. Hippocratic, Religious, and Secular Medical Ethics: The Points of Conflict . Georgetown University Press, 2012.
[74] Msoroka, M. S., & Amundsen, D. (2018). One size fits not quite all: Universal research ethics with diversity. Research Ethics , 14 (3), 1-17. https://doi.org/10.1177/1747016117739939
[75] Pirzada, N. (2022). The Expansion of Turkey’s Medical Tourism Industry. Voices in Bioethics , 8 . https://doi.org/10.52214/vib.v8i.9894
[76] Stem Cell Tourism: False Hope for Real Money . Harvard Stem Cell Institute (HSCI). (2023). https://hsci.harvard.edu/stem-cell-tourism , See also: Bissassar, M. (2017). Transnational Stem Cell Tourism: An ethical analysis. Voices in Bioethics , 3 . https://doi.org/10.7916/vib.v3i.6027
[77] Song, P. (2011) The proliferation of stem cell therapies in post-Mao China: problematizing ethical regulation, New Genetics and Society , 30:2, 141-153, DOI: 10.1080/14636778.2011.574375
[78] Dajani, R. (2014). Jordan’s stem-cell law can guide the Middle East. Nature 510, 189. https://doi.org/10.1038/510189a
[79] International Society for Stem Cell Research. (2024). Standards in stem cell research . International Society for Stem Cell Research. https://www.isscr.org/guidelines/5-standards-in-stem-cell-research
[80] Benjamin, R. (2013). People’s science bodies and rights on the Stem Cell Frontier . Stanford University Press.
Mifrah Hayath
SM Candidate Harvard Medical School, MS Biotechnology Johns Hopkins University
Olivia Bowers
MS Bioethics Columbia University (Disclosure: affiliated with Voices in Bioethics)
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Med Internet Res
- PMC10612001

Examining the Persuasive Effects of Health Communication in Short Videos: Systematic Review
Zicheng zhu.
1 Department of Communications and New Media, Faculty of Arts & Social Sciences, National University of Singapore, Singapore, Singapore
2 Global Health Institute, Xi'an Jiaotong University, Xian, China
Renwen Zhang
Associated data.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist.
Search strategies for all searched databases.
Raw data set (4118 papers).
Removed duplicates (3810 papers).
Screened by title and abstract (36 papers).
Final data set (18 papers).
Full coding.
The ubiquity of short videos has demonstrated vast potential for health communication. An expansion of research has examined the persuasive effect of health communication in short videos, yet a synthesis of the research is lacking.
This paper aims to provide an overview of the literature by examining the persuasive effect of health communication in short videos, offering guidance for researchers and practitioners. In particular, it seeks to address 4 key research questions: What are the characteristics of short videos, samples, and research designs in short video–based health communication literature? What theories underpin the short video–based health communication literature? What are the persuasive effects of health communication in short videos? and What directions should future research in this area take?
Following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, an electronic search of 10 databases up to March 10, 2023, generated 4118 results. After the full-text screening, 18 articles met the eligibility criteria.
The current research lacks a uniform definition of short videos, demonstrates sample biases in location and education, and adopts limited methodologies. Most studies in this synthesis are theoretically grounded or use theoretical concepts, which are predominantly well examined in persuasion research. Moreover, relevant topics and suitable themes are effective in persuasive health communication outcomes, whereas the impact of diverse narrative techniques remains ambiguous.
Conclusions
We recommend that future research extends the definition of short videos beyond time constraints and explores non-Western and less-educated populations. In addition, researchers should consider diverse methods to provide a more comprehensive examination and investigate the impact of audience targeting and narrative techniques in short video health communication. Finally, investigating how the unique aspects of short videos interact with or challenge traditional persuasion theories is essential.
Introduction
Health communication scholars have used diverse modalities such as text, audio, and video to communicate health information to the public [ 1 ]. Many studies have demonstrated that compared with other modalities, video is more effective in disseminating health information owing to its engrossing nature [ 2 ], visual appeal, and ability to illustrate complex concepts [ 3 ]. According to the dual coding theory, people process information through 2 systems, 1 for visual information and another for verbal information [ 4 ]. The use of visual and verbal information in videos allows both systems to process and store information. Health messages disseminated through videos are more memorable because viewers can retrieve both imagery and verbal information.
In recent years, short videos have gained significant popularity and have become influential in people’s lives. TikTok, the most popular short video app, was downloaded globally more times than any other app in 2021 [ 5 ]. Instagram Reels, a short video feature on Instagram, has 2.35 billion monthly active users [ 6 ]. Similarly, YouTube Shorts has seen a remarkable 135% growth year over year, now boasting >1.5 billion monthly users [ 7 ]. Moreover, 85% of the marketers have identified short videos as the most effective format on social media [ 8 ]. The appeal of short videos is attributed to their ease of production, including easy editing of music, animation, and visual effects; convenient distribution; and their ability to cover a broad spectrum of topics, such as beauty, cooking, education, and technology [ 9 ].
Among various topics on short video platforms, health-related topics have grown extensively. During the COVID-19 pandemic, the World Health Organization used TikTok to share reliable information and counter misinformation regarding the virus [ 10 ]. As of July 12, 2020, videos with COVID-19–related hashtags on TikTok had received a total of 130.8 billion views [ 11 ]. The affordances of short video platforms, including live streaming, searching, metavoicing, and recommending, incentivize people to seek health information on the platforms [ 12 ]. Therefore, short videos have become a powerful tool for providing health advice and influencing people’s health beliefs and behaviors [ 13 ]. Consequently, understanding how to disseminate health information through short videos is crucial.
Thus far, a large body of work has examined the spread and impact of health-related information on short video platforms. For example, Basch et al [ 14 ] and Yalamanchili et al [ 15 ] examined COVID-19–related and vaccination-related content on TikTok and found that videos featuring humor, music, and dance were positively related to user engagement, as measured through views, comments, and likes. Understanding the factors that contribute to user engagement is essential. However, health communication researchers are also interested in the factors that influence the effects of short videos on users’ health attitudes and behaviors, which may inform the design of effective health campaigns. Therefore, an increasing number of studies have examined the persuasive effects of different designs of health-related short videos. Lipkus and Sanders [ 16 ], for instance, evaluated the effects of short videos with various themes of waterpipe tobacco smoking (WTS) on young adults’ risk beliefs and attitudes toward WTS.
Despite this, systematic efforts to analyze the persuasive effects of health communication through short videos remain scarce, leading to gaps in our understanding of this phenomenon. A recent systematic review by McCashin and Murphy [ 17 ] investigated the use of TikTok for public health and mental health purposes and concluded that the platform holds promise as a means of disseminating health information to young audiences. Nonetheless, most of the studies within the review by McCashin and Murphy [ 17 ] focused on the relationship between TikTok health video features and user engagement, neglecting to explore persuasive outcomes. Previous research has also examined the impact of video-based education on behavioral modification, revealing that effectiveness is contingent upon target behaviors and that gain-framed messages are more efficacious [ 18 ]. However, the average video length in these studies was 36 minutes, which exceeded the typical duration of short videos, rendering these findings inadequate for understanding the impact of health communication through short videos.
To address these knowledge gaps, this paper synthesizes the existing literature on the persuasive effects of health communication in short videos. Central to this review is a focus on studies that explore various design strategies of health-related short videos, rather than those comparing the persuasive efficacy of short videos with no videos or other media modalities, such as text or images. This focus of our study emerged from the ubiquity of short videos in today’s digital landscape, which shifts the main inquiry of stakeholders from whether to use short videos for health communication, to determine the best design strategies for maximum impact. Although studies contrasting short videos with no videos or other mediums offer insights into the overall viability of short videos for health communication, research into specific design elements directly addresses the main inquiry: discerning the most effective design strategies for health persuasion in short videos. Specifically, health communication in this paper is defined as the design and dissemination of health-related messages to influence individual and community decisions promoting health [ 19 ]. Given the lack of a consensus on short video duration, we refrained from imposing a specific time constraint. Instead, we focused on studies that self-identify as examining short videos. Our study addressed 4 research questions (RQ):
- RQ1: What are the characteristics of short videos, samples, and research designs in short video–based health communication literature?
- RQ2: What theories underpin the short video–based health communication literature?
- RQ3: What are the persuasive effects of health communication in short videos?
- RQ4: What directions should future research in this area take?
The insights provided by this review hold significant value for health researchers, practitioners, and policy makers as they offer guidance for designing effective health messages in short videos and inform future investigations into the role of short videos in disseminating health information.
Data Sources and Search Strategy
Following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) model [ 20 ], we executed a systematic search across 8 primary databases: ACM Digital Library, PsycINFO, Web of Science, Communication & Mass Media Complete, MEDLINE, Embase, CINAHL, and Scopus. Google Scholar was used as a supplementary source to augment the initial search. In addition, we incorporated the ProQuest Dissertations & Theses Global database to identify doctoral dissertations, as the inclusion of gray literature in systematic reviews is considered crucial for mitigating publication bias [ 21 ]. The PRISMA checklist can be found at Multimedia Appendix 1 .
As our review focuses on 3 main aspects, that is, short videos, health, and persuasive effects, we developed 3 sets of search strings ( Textbox 1 ). Specifically, for short videos, we used the term short video along with other prominent short video platforms [ 22 ]. For health and persuasive effects, we drew from the studies by Ehsan et al [ 23 ] and Walter et al [ 24 ] to generate the search strings. Consequently, the search strings were formulated as follows: (“short video” OR tiktok OR douyin OR “youtube shorts” OR “instagram reels” OR triller OR “snapchat spotlight” OR vine OR “facebook shorts”) AND (persua* OR impact OR effect OR outcome OR belief OR attitude OR behavior OR behaviour OR intention OR knowledge) AND (health OR medic* OR clinical OR disease OR disabilit* OR disorder OR ill* OR well-being OR wellbeing). We searched for these strings in the titles, abstracts, or keywords of articles within the databases. The search encompassed publications available up until the search date, March 10, 2023. The search strategies for all searched databases can be found in Multimedia Appendix 2 .
Search strings.
Short video
- short video
- youtube shorts
- instagram reels
- snapchat spotlight
- facebook shorts
Persuasive effects
Inclusion and Exclusion Criteria
Articles were included in our corpus if they (1) pertained to health; (2) investigated the content or characteristics of short videos; (3) related to persuasion, defined as a deliberate attempt to influence people’s attitudes, beliefs, intentions, or behaviors [ 25 ]; and (4) were empirical studies. We excluded articles that (1) were not health related, (2) did not explore the content or characteristics of short videos (eg, solely examined the impact of providing a short video vs no video on persuasive outcomes [ 26 ]), (3) were not pertinent to persuasion (eg, exclusively investigated user engagement with short videos [ 14 ]), (4) were not written in English, and (5) were not full articles. We did not exclude papers based on their methods or participants, as we aimed for inclusivity in our review.
Study Screening Method
Following the initial search, we identified 4118 articles. After duplicate removal, 3810 articles remained. Adhering to the inclusion and exclusion criteria, 2 authors of this study jointly screened 9.97% (380/3810) of articles, yielding satisfactory intercoder reliability with Krippendorff α=.82. The remaining articles (n=3430) were evenly allocated between the 2 coders for further scrutiny. The results were discussed among all authors to ensure compliance with the inclusion and exclusion criteria. Ultimately, the final data set comprised 18 articles. We consulted scholars in the field to verify that no relevant literature was missing from the data set. Figure 1 illustrates the PRISMA flow diagram representing the search and screening process. The lists of papers examined at each stage are presented in Multimedia Appendices 3 to 6 [ 16 , 27 - 43 ].

PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagram showing the flow of studies.
Data Extraction and Synthesis
The first author thoroughly reviewed the final articles and, in collaboration with the other authors, established a codebook. The coding decisions were informed by previous reviews on TikTok and health [ 17 ] and the RQs of this study. Specifically, we coded the study identification information, including authors, publication years, and study locations. In addition, we coded basic information related to the studies’ topics, such as the health domain and study objectives. To address RQ1, we coded the video length, sample size, age, race, sex, and education level of the sample; data collection method; and study duration. For RQ2, we coded the theories used in these studies. To answer RQ3, we coded the health message design, outcome variables, persuasive effects, moderators, mediators, and moderation and mediation effects. The first author coded all studies in the final data set and discussed the coding results with all authors to ensure accurate validation against the original papers. Table 1 presents an overview of the paper’s study characteristics, and Table 2 summarizes the persuasive effects. The complete coding is provided in Multimedia Appendix 7 .
Study characteristics of the papers.
a N/A: not applicable.
Persuasive effects and theories examined in the papers.
b WTS: waterpipe tobacco smoking.
Current research on health communication in short videos predominantly focuses on three themes: (1) the prevention of unhealthy behaviors, particularly among those susceptible to such actions (eg, WTS; 2/18, 11%); (2) diminishing health-related stigma (eg, albinism; 4/18, 22%); and (3) promoting the adoption or reduction of specific behaviors (eg, influenza vaccination; 12/18, 67%). In the following sections, we provide a more comprehensive account of the studies’ basic characteristics, the theories used, and the persuasive impact of health communication in short videos.
Study Characteristics
The research methodology used in the examined studies exhibits limited variation and potential issues with sample representation, which may subsequently affect the generalizability of the findings. Of the 18 studies, 16 (89%) used experimental designs, whereas 1 (5%) study used a survey approach [ 39 ] and 1 (5%) study implemented mixed methods, incorporating a focus group after the experiment [ 27 ]. In addition, the samples in the investigated studies displayed a bias concerning location and education. Most studies (12/18, 67%) were conducted in Western countries (ie, Europe, North America, and Oceania), with only 4 studies undertaken in Africa and Asia. Two studies did not report the study location, but their participants were predominantly White [ 16 , 34 ]. Notably, such a location bias may arise from the review’s inclusion criteria, which only considered studies written in English. Consequently, research conducted in non-Western countries and published in languages other than English might have been overlooked. Among the studies targeting adults and presenting participants’ education statistics, most of the participants (9/18, 50%) held at least some college degrees. The generalizability of the persuasive effects identified in existing studies to other countries and individuals with lower educational levels remains uncertain.
In addition, current research lacks a precise definition of short videos in terms of video length. Although most studies (14/18, 78%) feature short videos that do not exceed 10 minutes in duration—the maximum video length for TikTok as of February 2022 [ 44 ]—1 study included short videos of approximately 20 minutes [ 34 ]. Furthermore, among studies with videos shorter than 10 minutes, only 3 studies had videos ≤1 minute, a typical video length for short video platforms [ 45 ].
Most studies in this synthesis are either theoretically grounded (n=9) or used variables guided by theoretical concepts. However, the theories and theoretical concepts used in these studies are predominantly well examined, particularly in persuasion research. For instance, 6 studies used theories addressing factors influencing individuals’ behavioral intentions and behaviors—specifically, social cognitive theory, the theory of planned behavior, and the unified theory of acceptance and use of technology. The factors examined in these theories encompass the observation of others’ behaviors, norms and social influence, attitudes, behavioral control, and expectancy. These theories have been frequently applied to understand people’s acceptance of new technology and advocated behaviors [ 46 ].
In addition, 3 studies used theories concerning people’s beliefs and attitudes, namely inoculation theory, attribution theory, and a specific theoretical model addressing the treatment of disabilities in the workplace [ 29 , 30 , 34 ]. These theories aim to comprehend the impact of people’s thinking processes (ie, attribution process, the amount of information acquired, and pre-exposed counterargument) on their subsequent perceptions and reactions. Arguably, the application of these theories offers insights for designing health messages in short videos in the included studies. Nevertheless, few studies have investigated how the unique aspects of short videos extend or challenge these traditional theories and contribute to these theories.
Persuasive Effects of Health Communication in Short Videos
The studies included in this review examined diverse designs of health messages in short videos, reporting a variety of health-related outcomes such as attitudes and beliefs (14/18, 78%), behavioral intentions (10/18, 56%), and health-related knowledge (6/18, 33%). Remarkably, only 4 studies within the synthesis assessed individuals’ health behaviors. Despite the significance of attitudes and intentions as antecedents of behavior [ 47 ], the potential for attitude-behavior discrepancies cannot be dismissed [ 48 ]. Consequently, the extent to which alterations in individuals’ attitudes and intentions may elicit changes in their behavior remains unclear. In addition, 72% (13/18) of the studies assessed outcomes immediately following interventions, whereas the remaining 28% (5/18) were longitudinal studies, measuring outcomes from 1 week to 6 months after the intervention. Furthermore, 67% (12/18) of the studies gauged participants’ pre-exposure attitudes, beliefs, or behaviors concerning central health issues. In the following sections, we discuss the primary effects of health message design in short videos, accompanied by an analysis of examined moderators and mediators.
Main Persuasive Effects of the Design of Health Messages in Short Videos
The included studies investigated various aspects of health message design in short videos, including topic relevance, topic theme, and narrative and video appeal strategies.
Topic Relevance
Topic relevance, investigated in 10 studies, refers to the effectiveness of presenting health-related topics compared with unrelated topics for persuasion. For example, Davis et al [ 38 ] assessed the effectiveness of a glaucoma eye drop technique video against a general nutrition video in improving patients’ technique. Studies of this kind produced mixed results; some found relevant topics more persuasive [ 28 , 35 ], whereas others observed nonsignificant differences [ 41 , 43 ]. However, factors such as suboptimal sampling recruitment, high attrition rates, and low character-audience relatability may contribute to these observed insignificances [ 41 , 43 ].
Topic Theme
Overall, 9 studies examined topic themes. Demonstrating that distinct themes significantly influence persuasive outcomes, these studies underscore the importance of selecting suitable themes for health communication in short videos. For example, physical harm, harm to others, and myth-related themes were more effective than addiction themes in modifying WTS perceptions [ 16 ]. Educational content was more effective than contact content, featuring individuals living with a disease in increasing disease-specific knowledge and enhancing the assessments of affected individuals [ 27 , 30 ]. Generally, themes addressing affective stimuli processing and response efficacy were more persuasive than their counterparts [ 28 , 32 ]. There is 1 exception indicating that varying attribution styles of a health issue (ie, controllable vs uncontrollable) did not significantly influence weight bias [ 34 ]; this outcome may be attributable to the study’s sample comprising registered dietitians who had previously participated in weight bias reduction training programs, potentially limiting further improvement in their weight bias levels. This underscores the significance of selecting an appropriate sample, as participants with preexisting elevated baseline perceptions, attitudes, and intentions toward the focal issue may exhibit minor changes in persuasive outcomes.
Narrative and Video Appeal Techniques
The third dimension, narrative and video appeal techniques, investigated the persuasive impact of varying strategies and appeals while maintaining consistent themes across different short videos. Video appeal demonstrated promising effects, as engaging, appealing, and comprehensible short videos were more likely to inspire behavioral intentions [ 39 ]. Conversely, the persuasive impact of narrative techniques remains ambiguous, with studies reporting inconclusive and mixed outcomes [ 40 ]. This may correspond with previous findings suggesting smaller effect sizes for videos compared with other modalities such as video games and text [ 49 ], which may be attributed to the fact that reading necessitates ongoing mental simulation and video games are intrinsically richer in sensory input, whereas processing visual stimuli involves a more automatic process requiring minimal mental investment [ 50 ].
In addition, research examining narrative techniques indicated that narrative content was more effective than informational content in altering individuals’ perceptions of influenza threat but not their perceived efficacy, intentions, or behavior [ 33 ]. This discrepancy may be ascribed to the videos’ theme emphasizing the interconnected nature of influenza rather than the efficacy aspects of vaccination, once again highlighting the importance of short video themes. Furthermore, this implies a potential interaction effect between the theme and narrative technique in short videos, where the influence of narrative techniques may be undermined without an appropriate theme. Xiao and Yu [ 31 ] found that humorous short video messages increased message likability but reduced individuals’ risk perception, emphasizing the need for additional inquiries into the intricate balance between attention-grabbing narrative methods and achieving the intended persuasive results.
Moderators and Mediators
In light of the inconclusive findings regarding the primary persuasive effects of health messages in short videos, 10 studies investigated the conditions or mechanisms under which these persuasive effects occur. These studies provided evidence that the persuasive impact of health messages in short videos was moderated by individuals’ sociodemographic factors (eg, age, race, and therapeutic background [ 16 , 35 ]), health and media literacy [ 33 , 40 ], political ideology and beliefs [ 28 ], message dissemination phases [ 31 ], and congruence between exposed and evaluated cases [ 30 ]. Generally, narrative techniques were found to be particularly beneficial for individuals with low literacy because of their limited self-efficacy in understanding and processing information [ 33 , 40 ]. In addition, health messages in short videos were particularly effective for those initially skeptical about the topic, as others might have already been receptive to the issue [ 28 , 35 ].
A mere 3 studies within the synthesis explored the mediating effect, leaving the mechanism by which the design of health messages in short videos influences people’s attitudes and behaviors unclear. Ewing et al [ 36 ] found that avoidance parenting mediated the relationship between short videos instructing parents on assisting children in coping with fears and the children’s subsequent behaviors. González-Cabrera and Igartua [ 40 ] and Violeau et al [ 37 ] found that engagement with narratives and characters mediated the persuasive efficacy of short video health messages. These findings potentially suggest that, to bolster persuasive outcomes, relevant stakeholders might consider strategizing short video designs that enhance viewer engagement and consequently persuasive results. However, it is important to exercise caution concerning the context, as such engagement with narratives and characters might be associated with emotional arousal and could be less preferable than presenting factual matters, which aids individuals in coping with uncertainty during periods of heightened crisis severity [ 51 ].
Principal Findings
Given the increasing popularity of short video platforms, discerning how to capitalize on short videos for disseminating health information has emerged as a pressing concern for health researchers and practitioners [ 13 ]. Although previous systematic reviews have primarily concentrated on the impact of health communication in short videos on user engagement [ 17 ], this study presents a systematic review of existing research exploring the persuasive outcomes of health communication in short videos, which is crucial for guiding the effective design of health messages and campaigns.
A literature search yielded 18 papers, suggesting that this area remains relatively underexplored. This synthesis unveils that the design of health messages in short videos encompasses (1) topic relevance, (2) topic themes, and (3) narrative and video appeal techniques. The persuasive effects of the design of health messages were largely mixed, with evidence supporting and contradicting the effects within each category. In the following sections, we delve deeper into the insights obtained from this review and offer guidance for future research.
Addressing Methodological Limitations: Defining Short Videos and Expanding Sample Diversity and Research Design
This synthesis highlights the fact that extant studies lack a consistent definition of short videos. Remarkably, this issue is not solely present in the examined studies, but also in the broader research on short videos. For example, Cao et al [ 52 ] defined short videos as those lasting less than 1 minute, whereas Kaye et al [ 53 ] defined short videos as those shorter than 5 minutes. Owing to the vague definitions, the lengths of short videos in the analyzed studies vary, ranging from 25 seconds to 20 minutes. When the short video platform TikTok was launched in 2016, it had a time-limit restriction of 15 seconds [ 54 ]. Subsequently, TikTok extended its maximum video length to 1 minute, 3 minutes, and 10 minutes. In light of these continuous adjustments, it is debatable whether the video length alone is adequate for defining short videos. If videos up to 10 minutes are still considered short videos, how are they differentiated from general videos, such as those uploaded to YouTube? A potential solution involves considering other salient characteristics of short videos, such as low-cost production. For instance, short video platforms equip users with features such as music, animation, and visual effect editing, allowing them to effortlessly produce videos and blur the lines between producers and consumers [ 9 , 53 ]. Further discussion regarding alternative features beyond the time limit for defining short videos is warranted.
In addition, the samples in the examined studies display biases in terms of location and education. This could potentially be attributed to the review’s inclusion criteria, which only considered studies written in English, possibly overlooking research from diverse locations not written in English. Notwithstanding this limitation, most of the investigated studies in this review were conducted in Western countries, with only 4 studies undertaken in Africa and Asia. The Asia Pacific region, in fact, boasts a greater number of short video platform users than other regions [ 55 ]. Countries such as Indonesia, Brazil, and Mexico also exhibit a high number of users accessing short video platforms [ 56 ]. More importantly, previous research has shown that individuals from different countries exhibit diverse reactions to health information. For example, Koreans and Hong Kongers demonstrated higher trust in experience-based health information compared with Americans [ 57 ]. Hong Kongers and Americans also displayed distinct heuristic and cognitive mechanisms for processing persuasive health messages [ 58 ]. Consequently, the generalizability of the persuasive effects of health messages in short videos, as observed in the West, to other countries remains uncertain. Therefore, we advocate for future research to investigate health messages in short videos in non-Western contexts or to conduct cross-cultural studies comparing persuasive effects across different countries.
The education level of study participants is also disproportionately represented. The majority of participants in the analyzed studies possessed at least some college education. However, previous research indicates that individuals with lower educational levels face higher risks of problematic smartphone use [ 59 ] and are more prone to develop internet addiction [ 60 ]. Moreover, this group exhibits less trust in most health information sources, such as the internet, magazines, and newspapers [ 61 ], and is more susceptible to health misinformation [ 62 ]. This suggests that people with lower educational levels might be more inclined to overuse short video platforms and they may process health information differently than those with higher educational levels. Consequently, investigating the persuasive effect of health messages in short videos among individuals with lower educational levels could yield additional insights into the topic.
In addition, the literature examined in this review uses limited methods, with approximately all studies exclusively relying on web-based or laboratory experiments. This limitation in methods may hinder a comprehensive understanding of the persuasive effect of health communication in short videos. To enrich the understanding, future research can use various methods, incorporating interviews, surveys, experience sampling, and even mixed methods. In addition, only a few studies within the synthesis measured the actual behaviors. Although perceptions, beliefs, and attitudes are crucial antecedents of behaviors [ 47 ], inconsistencies between attitudes and behaviors may arise [ 49 ]. To address this gap, researchers should consider using field experiments that measure participants’ behaviors both before and after the study. For example, following the approach of Qiu and Kumar [ 63 ], investigators could create fictitious accounts on short video platforms and require participants in experimental and control groups to follow different accounts through which health messages with distinct designs are disseminated. In doing so, researchers can more accurately assess people’s behaviors and reactions to the design of health messages in short videos.
Navigating Design and Theory: Exploring Content, Narrative Techniques, and Theoretical Mechanisms
Overall, when comparing various topics, themes, and narrative techniques, researchers found that identifying relevant topics and appropriate themes was effective in persuasive outcomes for health communication in short videos. However, the persuasive effects of different narrative techniques remain uncertain, possibly because of the abbreviated length of the short videos and viewers’ limited exposure. In addition, the persuasive impact of the content is dependent on the sample. Consistent with previous research demonstrating that interventions promoting attitude change have the largest effect size among individuals with poorer baseline attitudes and no prior training on the focal issue [ 64 ], the examined studies suggest that participants’ baseline attitudes and prior training may potentially influence the persuasive effects of health communication in short videos. This underscores the fact that the content for health communication in short videos may be particularly beneficial for those with limited knowledge and unfavorable attitudes.
Furthermore, the effectiveness of narrative techniques for health communication in short videos remains ambiguous. Several studies found that the anticipated superior narrative style did not outperform alternative methods [ 65 , 66 ], aligning with the findings in the study by Tukachinsky [ 49 ] that narrative techniques used in videos had a smaller effect size than textual and video game stimuli, possibly because of reduced mental simulation requirements [ 50 ]. Consequently, there is an urgent need for further research to examine the overall effectiveness of narrative techniques for health communication in short videos and the boundary conditions of such narrative techniques, such as the context of the disease [ 31 ] and target audience [ 40 ].
However, it is encouraging to note that numerous studies in this review have explored moderators, which shed light on the intricate connection between the design of health-related short videos and their intended viewers. For instance, when designing health-related short videos, it is crucial for practitioners to focus on audiences who might initially be resistant to the health message, as others might have already accepted the messages. For example, when promoting vaccination, special attention could be directed toward individuals with a mistrust of governmental entities, as they may be less likely to heed governmental health advisories [ 28 ]. The chosen narrative techniques should be tailored to the audience. For audiences with limited media and health literacy, practitioners might opt for techniques that spark their emotional responses, such as firsthand testimonials or compelling storylines.
Although we have gleaned some understanding about moderators, the mechanisms underlying the persuasive effects of health messages in short videos have yielded mixed results and remain underexplored. Only a few studies in the synthesis have examined the mediation effect, leaving the mechanism in which the design of health messages in short videos influences people’s attitudes and behaviors unclear. Hence, we encourage future research to investigate the mechanisms underlying the observed effects, with a particular emphasis on two aspects: (1) individuals’ emotional reactions and (2) their cognitive processing. This is because Updegraff and Rothman [ 67 ] posited that persuasive health messages activate individuals’ emotional responses, such as fear, happiness, and sadness, which in turn guide their behaviors. In addition, the elaboration likelihood model suggests that message attributes influence the attention and consideration individuals devote to messages, subsequently affecting their susceptibility to persuasion [ 68 ]. In this context, individuals’ emotional reactions and cognitive processing of health messages in short videos may affect the persuasive effects of messages, highlighting the need for researchers to further examine these variables as mediators.
In addition, although most of the studies in the synthesis are theoretically grounded, the theories and concepts used have been widely examined, particularly in persuasion research. Few studies have explored how the unique aspects of short videos extend or challenge traditional persuasion theories. Given the distinct features of short videos, researchers can endeavor to expand existing theories or develop new ones to comprehend the persuasive effects of short videos. For example, owing to their brief duration, attention-grabbing features are vital for short video producers. However, attention-grabbing elements, such as humor, can act as a double-edged sword in persuasion, as they might compromise the credibility of health care messages [ 69 ] and diminish risk perception [ 31 ]. Thus, striking a delicate balance between garnering attention and persuading through short videos may present a challenge for health practitioners. Further theoretical discussion and insights are required.
Limitations
This review has several limitations. First, the initial keywords used for searching might have missed studies if they did not mention the search strings in their title, abstract, or keywords. For instance, while encompassing a broad array of short video platforms, this review may omit platforms that are not specified in the search string. To enhance comprehensiveness, future research should consider expanding the search strings to capture a wider range of short video platforms. Second, the purpose of this review is to provide a comprehensive overview of existing studies and offer guidance for researchers and practitioners, which led to the adoption of a fine-grained systematic review approach rather than a meta-analysis. The diverse research focuses among the included articles also impede the feasibility of conducting a meta-analysis. Nevertheless, as the number of studies in this area continues to grow, a more advanced meta-analysis may become necessary in the future. Finally, given the limited number of studies included in this review, our findings regarding persuasive impacts might be inconclusive. As more research surfaces in the future, a clear understanding of persuasion effects may be established.
Acknowledgments
This research was funded by National University of Singapore Start-up Grant.
Abbreviations
Multimedia appendix 1, multimedia appendix 2, multimedia appendix 3, multimedia appendix 4, multimedia appendix 5, multimedia appendix 6, multimedia appendix 7.
Conflicts of Interest: None declared.

- News Releases
Scientists discover blood proteins that may give cancer warning 7 years before diagnosis
Cancer Research UK
Two Cancer Research UK-funded studies from Oxford Population Health have discovered proteins in the blood that could warn people of cancer more than seven years before it is diagnosed.
Scientists identified 618 proteins linked to 19 different types of cancer, including 107 proteins in a group of people who blood was collected at least seven years before diagnosis.
The team have discovered that these proteins could be involved at the very earliest stages of cancer, where it could be prevented.
They believe that some of these proteins could be used to detect cancer much earlier than is currently possible. In the future, this could help treat the disease at a much earlier stage or prevent it altogether.
Cancer Research UK is funding researchers to look for the earliest signs of cancer as part of its long-term strategy to prevent cancer through research . In these studies, the team used a powerful technique called proteomics. Proteomics allows scientists to analyse a large set of proteins in tissue samples at a single point in time, to see how they interact with each other and find any important differences in proteins between different tissue samples.
In the first study, scientists analysed blood samples from UK Biobank which were taken from more than 44,000 people, including over 4,900 people who subsequently had a cancer diagnosis.
Using proteomics, the team analysed a set of 1,463 proteins from a single sample of blood from each person. They compared the proteins of people who did and did not go on to be diagnosed with cancer to look for important differences between them and find out which ones were linked to cancer risk. The scientists also identified 182 proteins that differed in the blood three years before a cancer diagnosis took place.
In the second study, the scientists looked at genetic data from over 300,000 cancer cases to do a deep dive into which blood proteins were involved in cancer development and could be targeted by new treatments.
The scientists found 40 proteins in the blood that influenced someone’s risk of getting 9 different types of cancer. While altering these proteins may increase or decrease the chances of someone developing cancer, the scientists also found that in some cases this may lead to unintended side-effects.
However, the team stress that they will need to do further research to find out the exact role these proteins play in cancer development, which of the proteins are the most reliable ones to test for, what tests could be developed to detect the proteins in the clinic and which drugs could target these proteins.
Dr Keren Papier, Senior Nutritional Epidemiologist at Oxford Population Health and joint first author of the first study, said:
"To save more lives from cancer, we need to better understand what happens at the earliest stages of the disease. Data from thousands of people with cancer has revealed really exciting insights into how the proteins in our blood can affect our risk of cancer. Now we need to study these proteins in depth to see which ones could be reliably used for prevention.”
Dr Joshua Atkins, Senior Genomic Epidemiologist at Oxford Population Health and joint first author of the first study, said:
“The genes we are born with, and the proteins made from them, are hugely influential in how cancer starts and grows. Thanks to the thousands of people who gave blood samples to UK BioBank, we are building a much more comprehensive picture of how genes influence cancer development over many years.
Dr Karl Smith-Byrne, Senior Molecular Epidemiologist at Oxford Population Health and a senior author of the first paper and first author of the second study, said:
“We’ve predicted how the body might respond to drugs that target specific proteins, including many potential side-effects. Before any clinical trials take place, we have some early indications of which proteins we might avoid targeting because of unintended side-effects.
“This research brings us closer to being able to prevent cancer with targeted drugs – once thought impossible but now much more attainable.”
Professor Ruth Travis, Senior Molecular Epidemiologist at Oxford Population Health and a senior author of both studies, said:
"To be able to prevent cancer, we need to understand the factors driving the earliest stages of its development. These studies are important because they provide many new clues about the causes and biology of multiple cancers, including insights into what’s happening years before a cancer is diagnosed.”
“We now have technology that can look at thousands of proteins across thousands of cancer cases, identifying which proteins have a role in the development of specific cancers, and which might have effects that are common to multiple cancer types.
Executive Director of Research and Innovation at Cancer Research UK, Dr Iain Foulkes, said:
“Preventing cancer means looking out for the earliest warning signs of the disease. That means intensive, painstaking research to find the molecular signals we should pay closest attention to.
“Discoveries from this research are the crucial first step towards offering preventative therapies which is the ultimate route for giving people longer, better lives, free from the fear of cancer.”
The papers, titled “Identifying proteomic risk factors for cancer using prospective and exome analyses of 1,463 circulating proteins and risk of 19 cancers in the UK Biobank” and “Identifying therapeutic targets for cancer among 2,074 circulating proteins and risk of nine cancers.” were published today (15 th May) and 29 th April respectively in Nature Communications* .
ENDS
For media enquiries to Cancer Research UK, contact Graeme Sneddon in the Cancer Research UK press office on 020 3469 5758 or, out of hours, on 020 3469 8301.
For media enquiries to Oxford Population Health, please contact [email protected] .
Notes to Editor
* The first paper will be available from https://www.nature.com/articles/s41467-024-48017-6 when the embargo lifts. The second paper is available from https://www.nature.com/articles/s41467-024-46834-3 .
About Cancer Research UK:
- Cancer Research UK is the world’s leading cancer charity dedicated to saving lives through research, influence and information.
- Cancer Research UK’s pioneering work into the prevention, diagnosis and treatment of cancer has helped save millions of lives.
- Cancer Research UK has been at the heart of the progress that has already seen survival in the UK double in the last 50 years.
- Today, 2 in 4 people survive their cancer for at least 10 years. Cancer Research UK wants to accelerate progress and see 3 in 4 people surviving their cancer by 2034.
- Cancer Research UK supports research into the prevention and treatment of cancer through the work of over 4,000 scientists, doctors and nurses.
- Together with its partners and supporters, Cancer Research UK is working towards a world where people can live longer, better lives, free from the fear of cancer.
For further information about Cancer Research UK's work or to find out how to support the charity, please call 0300 123 1022 or visit www.cancerresearchuk.org . Follow us on Twitter and Facebook
Nature Communications
Method of Research
Observational study
Subject of Research
Human tissue samples
Article Title
Identifying proteomic risk factors for cancer using prospective and exome analyses of 1,463 circulating proteins and risk of 19 cancers in the UK Biobank
Article Publication Date
15-May-2024
Disclaimer: AAAS and EurekAlert! are not responsible for the accuracy of news releases posted to EurekAlert! by contributing institutions or for the use of any information through the EurekAlert system.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Handwashing
- Hand Hygiene as a Family Activity
- Hand Hygiene FAQs
- Handwashing Facts
- Publications, Data, & Statistics
- Health Promotion Materials
- Global Handwashing Day
- Life is Better with Clean Hands Campaign
- Clinical Safety
- Healthcare Training
- Clean Hands Count Materials
About Handwashing
- Many diseases and conditions are spread by not washing hands with soap and clean, running water.
- Handwashing with soap is one of the best ways to stay healthy.
- If soap and water are not readily available, use a hand sanitizer with at least 60% alcohol to clean your hands.

Why it's important
Washing hands can keep you healthy and prevent the spread of respiratory and diarrheal infections. Germs can spread from person to person or from surfaces to people when you:
- Touch your eyes, nose, and mouth with unwashed hands
- Prepare or eat food and drinks with unwashed hands
- Touch surfaces or objects that have germs on them
- Blow your nose, cough, or sneeze into hands and then touch other people's hands or common objects
Key times to wash hands
You can help yourself and your loved ones stay healthy by washing your hands often, especially during these key times when you are likely to get and spread germs:
- Before, during, and after preparing food
- Before and after eating food
- Before and after caring for someone at home who is sick with vomiting or diarrhea
- Before and after treating a cut or wound
- After using the toilet
- After changing diapers or cleaning up a child who has used the toilet
- After blowing your nose, coughing, or sneezing
- After touching an animal, animal feed, or animal waste
- After handling pet food or pet treats
- After touching garbage
How it works
Washing your hands is easy, and it’s one of the most effective ways to prevent the spread of germs. Follow these five steps every time.
- Wet your hands with clean, running water (warm or cold), turn off the tap, and apply soap.
- Lather your hands by rubbing them together with the soap. Lather the backs of your hands, between your fingers, and under your nails.
- Scrub your hands for at least 20 seconds . Need a timer? Hum the “Happy Birthday” song from beginning to end twice.
- Rinse your hands well under clean, running water.
- Dry your hands using a clean towel or an air dryer.
Use hand sanitizer when you can't use soap and water
Washing hands with soap and water is the best way to get rid of germs in most situations. If soap and water are not readily available, you can use an alcohol-based hand sanitizer that contains at least 60% alcohol. You can tell if the sanitizer contains at least 60% alcohol by looking at the product label.
What you can do
CDC has health promotion materials to encourage kids and adults to make handwashing part of their everyday lives.
- Share social media graphics and messages.
- Print stickers and place clings on bathroom mirrors.
- Promote handwashing on or around Global Handwashing Day , celebrated each year on October 15.
- Distribute fact sheets to share information about hand hygiene for specific audiences.
- Frequent Questions About Hand Hygiene
- Hand Hygiene in Healthcare Settings
- The Life is Better with Clean Hands Campaign
Clean Hands
Having clean hands is one of the best ways to avoid getting sick and prevent the spread of germs to others.
For Everyone
Health care providers.

COMMENTS
Journal of Health Communication, Volume 29, Issue 4 (2024) See all volumes and issues. Volume 29, 2024 Vol 28, 2023 Vol 27, 2022 Vol 26, 2021 Vol 25, 2020 Vol 24, 2019 Vol 23, 2018 Vol 22, 2017 Vol 21, 2016 Vol 20, 2015 Vol 19, 2014 Vol 18, 2013 Vol 17, 2012 Vol 16, 2010-2011 Vol 15, 2010 Vol 14, 2009 Vol 13, 2008 Vol 12, 2007 Vol 11, 2006 Vol ...
Much of the recent research in this area has focused on whether empathic and positive communication are beneficial, 6,7 and whether empathic communication can be taught (it seems that it can). 8 A 2001 systematic review found that empathy and positive communication might also improve patient outcomes. 9 However, the evidence has moved on significantly, with numerous randomised trials having ...
The area of health communication research focuses primarily on the application of communication theory, concepts and strategies for enhancing public health services, and in fostering better understanding on how such processes work. The approaches are numerous and represent significant scholarship across biopsychosocial levels of analysis.
This essay is an excellent entry point for this research topic. Essays in this collection model different forms of critical analysis. For instance, Carter and Alexander's original research is an exemplar for connecting race, class, historical positioning, and health communication practices. Their interview-based original research highlights ...
This chapter starts from a holistic perspective on health in the society. It makes a. statement that, in order to become effective and sustainable, health communica-. tion needs to be studied, assessed, and practiced from a rights- or social justice-. P. Malikhao (*) Fecund Communication, Chiangmai, Thailand. e-mail: [email protected].
How to promote behavior change: lessons from health communication research. To reduce the risk of COVID-19 in the community, it is critical that we pay attention to optimal methods to ensure behavior change, both on the individual as well as on the community level. ... In the last few weeks, a number of papers and websites have been produced ...
Department of Communication Studies, The College of New Jersey, 2000. Pennington Road, Ewing, NJ 08628, USA. Abstract. There has been an increased interest in the use of. information technology ...
This paper examines the ways that qualitative inquiry can be especially useful ... Health communication research is an important, yet complex, area of applied inquiry designed to increase knowledge about the many communication challenges confronted in the
It is a significant research gap because older adults have unique communication needs, which, if not considered, their communication with healthcare providers could be ineffective . For example, older adults experience age-related changes in cognition, perception, and sensation, which can interfere with the communication process [ 14 ].
Introduction. Health communication is vital to the health ecosystem, especially in managing public health crises and promoting healthy living. 1-4 Health communication refers to using communication theory, evidence, techniques, and creativity to inform, educate and influence public views and perceptions and promote behaviours and practices that advance the health and wellbeing of individuals ...
Conference Paper. Full-text available. Jan 2019. Zülfiye Acar Şentürk. Mikail Batu. Onur Tos. PDF | On Sep 1, 2013, Thomas Hugh Feeley and others published An Introduction to Health ...
Methods: We systematically reviewed existing literature on health communication strategies in sub-Saharan Africa to answer formulated questions. A Google search was performed in October 2022 with ...
See our list of health communication research paper topics.Health communication is the study and application of the generation, creation, and dissemination of health-related information, health-related interactions among individual social actors and institutions, and their effects on different publics including individuals, community groups, and institutions.
These health communication strategies could play a very important role in developing and underdeveloped countries, where people are not much aware of the diseases and their preventive measure. In this paper the researchers have tried to make a systematic literature review of 20 different research outcomes of health communication.
Introduction. Health communication, i.e., interpersonal or mass communication activities focused on improving the health of individuals and populations [], has emerged as one of the most important public health issues in this century.The Healthy People 2010 project in the US suggests that health communication can contribute to all aspects of disease prevention and health promotion and that it ...
Built upon the literature on past technological interventions built for supporting job-seekers with autism, we define three major research challenges of (1) communication support, (2) employment stage-wise support, and (3) group work support. For each challenge, we review the current state-of-the-art practices and possible future solutions.
WC change from baseline to 104 weeks has been reported previously in the primary outcome paper ... OPEN Health Communications, ... A.K. declares having received research grants through his ...
Keywords: Health Communication, Behavioral Change Communication, HBM, Social Cognitive Theory. Categories and subcategories used in this review paper. Figures - uploaded by Rubal Kanozia
The Covid-19 outbreak has adversely influenced university students across the world both physically and psychologically. The psychological struggle faced by students, is effected by various factors, including disruptions to daily routines and academic activities, increased reliance on smartphones and the internet, limited social interaction, and confinement to their homes. These impediments ...
Voices in Bioethics is currently seeking submissions on philosophical and practical topics, both current and timeless. Papers addressing access to healthcare, the bioethical implications of recent Supreme Court rulings, environmental ethics, data privacy, cybersecurity, law and bioethics, economics and bioethics, reproductive ethics, research ethics, and pediatric bioethics are sought.
The research aims to analyse the evolving role of older adults in Cameroonian society and to examine the potential impact of this change on intergenerational relationships and the health of older adults. Introduction Africa is experiencing a gradual demographic shift due to rising life expectancy and increasing urbanisation. In sub-Saharan Africa, elderly individuals typically reside with ...
Specifically, health communication in this paper is defined as the design and dissemination of health-related messages to influence individual and community decisions promoting health . Given the lack of a consensus on short video duration, we refrained from imposing a specific time constraint. ... Current research on health communication in ...
Cancer Research UK-funded scientists at the University of Oxford have identified new links between blood proteins and different types of cancer. In two studies, published in Nature Communications ...
Health communication as a field of study ensures that such information get to the target audience. ... Utilising the qualitative research methodology, the paper scrutinised how The Standard ...
CDC has health promotion materials to encourage kids and adults to make handwashing part of their everyday lives. Share social media graphics and messages. Print stickers and place clings on bathroom mirrors. Promote handwashing on or around Global Handwashing Day, celebrated each year on October 15.