5 free worksheets for people struggling with OCD, developed by experts
By Elle Warren
• Clinically reviewed by April Kilduff, MA, LCPC
Dec 1, 2023 • 6 min read minute read
Reviewed by April Kilduff, MA, LCPC
There are a multitude of barriers to accessing mental healthcare. Whether it’s financial, insurance-related, time, or motivation, you may find yourself unable to immediately access treatment for OCD.
If you are experiencing those barriers, or if you just want a supplement to your treatment with some extra “homework,” we have resources for you. Putting your thoughts and experiences down on paper can be valuable for any mental health struggle—especially for highly behavioral conditions like OCD—so we’ve compiled 5 OCD worksheets developed with the help of leading experts in OCD treatment.
These worksheets focus on support systems, mental compulsions, taboo thoughts, relationship OCD: cognitive distortions & compulsions, and identifying your core fear(s).
Each worksheet also has a linked video that will explain and guide you through it. We recommend watching those before you begin, and following along in the worksheet.

Worksheet #1: Support Systems
This worksheet focuses on the importance of having support systems in OCD recovery, as well as the different forms support can take. Dr. Nicholas Farrell , Regional Clinical Director at NOCD, says support systems can be “very important to the recovery journey.”
When you’re facing the challenging but rewarding work of OCD recovery, it’s beneficial to have people in your life to encourage you and hold you accountable. This is true for most challenges in life, and mental health is no exception.
Moreover, it’s important for the people closest to you to understand your condition and treatment. If they don’t have an understanding of how your OCD shows up, and how you can get better, they may be more likely to engage in enabling behaviors that help keep you stuck.
This worksheet will ask you to reflect on the ways you receive emotional, tangible, informational, and social support. If you are lacking support in any of those areas, you can brainstorm ways to seek or ask for support.
There is also a section for you to reflect on the ways your loved ones have provided reassurance to you when you compulsively ask for it. It prompts you to instead reflect on how your loved ones could provide validation without the reassurance.
Follow along with the video guide for our Support Systems worksheet here.
Worksheet #2: Mental Compulsions
This worksheet offers education around mental compulsions, which are any internal actions done to relieve the distress of your intrusive thoughts & triggers.
Dr. Farrell says it’s important for people to know about mental compulsions because, naturally, “they tend to be hidden.” Outside of describing your experience to a mental health professional, you’re really the only one who can identify or notice them.
You will learn about three primary categories of mental compulsions:
- Mental review/rumination
- Thought neutralizing, blocking, or distracting
- Self-reassurance
You will reflect on what mental compulsions you engage in, which thoughts, feelings, and uncertainties you’re trying to avoid by doing them, and how you can prioritize long-term recovery over short-term relief (which is all that compulsions can provide).
Follow along with the video guide for our Mental Compulsions worksheet here.
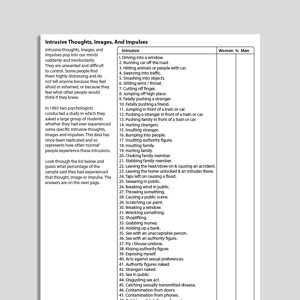
Worksheet #3: Taboo Thoughts
This worksheet talks about a very common thread among OCD themes and intrusive thoughts: they can be taboo, inappropriate, or deeply uncomfortable in nature.
Some of the more taboo themes include harm OCD , pedophilia OCD , and sexual orientation OCD . While these can feel deeply shameful, Dr. Farrell stresses the “universal nature” of intrusive thoughts.
You might feel like you’re the only one who has ever had these thoughts, but in fact, there are decades of research that point to the contrary. Dr. Farrell likes to show clients this research about the prevalence of all sorts of intrusive thought themes, among those with and without OCD.
You will learn that intrusive thoughts are ego-dystonic, meaning they don’t align with the sufferer’s values, beliefs, or morals. You will then be asked to reflect on how you judge yourself and your intrusive thoughts—how do you label them in your head?
You will be guided in speaking to yourself as you would a friend. Would you tell your friend with these uncontrollable thoughts that they are shameful, disgusting, or bad? It’s highly unlikely that you would. This worksheet will help you practice not speaking to yourself that way, either.
Follow along with the video guide on Taboo Intrusive Thoughts here.
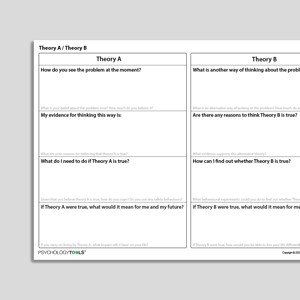
Worksheet #4: Relationship OCD: Cognitive distortions & compulsions
This worksheet focuses first on cognitive distortions that people often engage in when they’re struggling with relationship OCD, though the information can equally be applied to other themes, too.
Cognitive distortions are tricks that OCD plays on us. Dr. Farrell describes them as “thinking errors.” They include:
- All-or-nothing thinking ( My relationship has to be perfect otherwise we should break up )
- Catastrophizing ( If I can’t be 100% certain about our relationship right now, I’m going to ruin my life in the future )
- Selective abstraction ( My partner always gets stains on their clothes—can I live with that forever? )
- Mind reading ( Other people probably think we’re bad for each other )
- Hyper-responsibility ( If we don’t work out, I could be holding them back from meeting the right person, and it’ll all be my fault )
You’ll reflect on how cognitive distortions show up for you, then learn about common compulsions that people with relationship OCD engage in, such as constant “checking” of your feelings and attraction , “confessing” your intrusive thoughts because you feel so guilty, or seeking reassurance about your relationship (“we’re not going to break up, right?”).
You will then think how you can challenge both your cognitive distortions and compulsions to accept uncertainty and discomfort.
Follow along with the video guide on Cognitive Distortions in Relationship OCD here.
Worksheet #5: Core fears
The goal of this worksheet is to understand any “core fears” that are involved in your obsessions. As such, you will begin by learning more about obsessions—those repetitive, intrusive thoughts that often show up as “what ifs” and threaten our perception of safety.
After you get specific about your obsessions, you will learn more about the many faces of compulsions. Compulsions can show up in a million ways, and be mental (internal) or physical (external), but you will review a list of examples.
Finally, you will walk through the “downward arrow” exercise. You will start with your surface-level obsession ( what if I run over someone with my car? ) and then answer the question of, “If that came true, then…” until you get to the fundamental fear that causes you such distress. Perhaps the root is that you could be an evil person. Maybe it’s that you don’t have control over your impact on others.
Regardless, identifying your core fear allows you to get more specific about how you can face your fears—and at the end of the worksheet, you’ll brainstorm ways to do just that.
Follow along with the video guide on Core Fears here.
Use the OCD recovery tools at your disposal
Self-reflection and awareness is crucial to OCD recovery, but it can also be draining. Be patient and compassionate with yourself. You don’t have to do these all at once. If it feels overwhelming, you can do just one per day or even one per week, and really sit with each concept. Hopefully, you learn something new about OCD and about your unique experience of it.
If you want to give yourself the best chance at conquering OCD, please know that specialized, evidence-based therapy is available to you. The effectiveness of exposure and response prevention (ERP) therapy has been proven by decades of rigorous research, and it’s more accessible today than ever before.
Here at NOCD, every therapist receives intensive training in ERP, and we accept most major insurance plans to help you get started. If you’re ready to regain control of your life for OCD, I strongly encourage you to learn more about NOCD’s specialized approach to OCD treatment.
We specialize in treating OCD
Reach out to us. We're here to help.
Use insurance to access world-class treatment with an OCD specialist
Obsessive Compulsive Disorder (OCD) including Body Dysmorphic Disorder (BDD)

Resource type
Therapy tool.

"Should" Statements
Information handouts
Am I Experiencing Obsessive Compulsive Disorder (OCD)?

Approval-/Admiration-Seeking
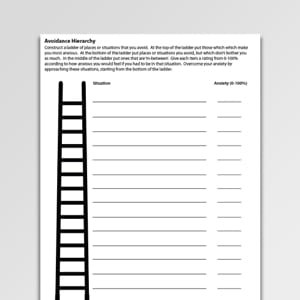
Avoidance Hierarchy (Archived)
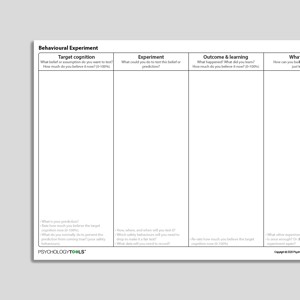
Behavioral Experiment

Behavioral Experiment (Portrait Format)

Catastrophizing

Checking Certainty And Doubt
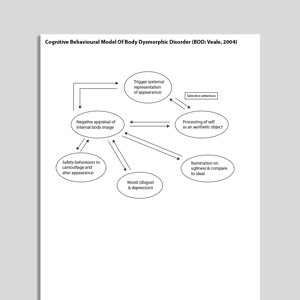
Cognitive Behavioral Model Of Body Dysmorphic Disorder (BDD: Veale, 2004)

Cognitive Behavioral Model Of Intolerance Of Uncertainty And Generalized Anxiety Disorder Symptoms (Hebert, Dugas, 2019)

Cognitive Behavioral Treatment Of Childhood OCD: It's Only A False Alarm: Therapist Guide
Treatments That Work™

Cognitive Behavioral Treatment of Childhood OCD: It's Only a False Alarm: Workbook

Cognitive Distortions – Unhelpful Thinking Styles (Common)

Cognitive Distortions – Unhelpful Thinking Styles (Extended)

Defectiveness

Dependence/Incompetence

Disqualifying The Positive

Embracing Uncertainty

Emotional Inhibition

Emotional Reasoning

Exposure And Response (Ritual) Prevention For Obsessive Compulsive Disorder (Second Edition): Therapist Guide

Exposure And Response Prevention

Exposure Practice Form

Exposure Session Record

Facing Your Fears And Phobias

Fear Ladder

Habituation

Intolerance Of Uncertainty

Intrusion Record

Intrusive Memory Record
Intrusive Thoughts Images And Impulses

Jumping To Conclusions

Maximizing The Effectiveness Of Exposure Therapy

Obsessive Compulsive Disorder (OCD) Formulation

OCD Hierarchy

Personalizing

Recognizing Obsessive Compulsive Disorder (OCD)

Self-Monitoring Record (Universal)
Theory A / Theory B

Theory A / Theory B (Archived)

Therapy Blueprint (Universal)

Therapy Blueprint For OCD

Thought Suppression And Intrusive Thoughts

Thought-Action Fusion

Treating Your OCD With Exposure And Response (Ritual) Prevention (Second Edition): Workbook

Uncertainty Beliefs – Experiment Record

Understanding Body Dysmorphic Disorder

Understanding Obsessive Compulsive Disorder (OCD)

Unhelpful Thinking Styles (Archived)

Urges – Self-Monitoring Record

What Is Body Dysmorphic Disorder (BDD)?

What Is Exposure Therapy?

What Keeps Body Dysmorphic Disorder (BDD) Going?


What Keeps Obsessive Compulsive Disorder (OCD) Going?

Your Stone Age Brain
Links to external resources.
Psychology Tools makes every effort to check external links and review their content. However, we are not responsible for the quality or content of external links and cannot guarantee that these links will work all of the time.
- Scale Download Primary Link Archived Link
- Obsessive Compulsive Cognition Working Group. (2001). Development and initial validation of the Obsessive Beliefs Questionnaire and the Interpretation of Intrusions Inventory. Behaviour Research and Therapy, 39, 987–1006.
- Obsessive Compulsive Inventory (OCI) scoring grid Download Primary Link
- Relationship Obsessive Compulsive Inventory (ROCI) Download Primary Link Archived Link
- Partner Related Obsessive Compulsive Symptom Inventory Download Primary Link Archived Link
- OCD Trauma Timeline Interview (OTTI) | Wadsworth, Van Kirk,August, MacLaren Kelly, Jackson, Nelson & Luehrs | 2023 Download Primary Link Archived Link
- Vancouver Obsessional Compulsive Inventory (VOCI) Download Primary Link Archived Link
Guides and workbooks
- What you need to know about OCD | International OCD Foundation (IOCDF) Download Primary Link
- Managing obsessive compulsive disorder | Simon Enright Download Primary Link Archived Link
- Obsessive compulsive disorder: patient treatment manual | Clinical Research Unit for Anxiety and Depression (CRUfAD) Download Primary Link Archived Link
- OCD: An OCD-UK Information Guides For People Affected By Obsessive Compulsive Disorder | OCD-UK Download Archived Link
- Self-Help: Managing Your OCD At Home | Anxiety Canada Download Primary Link Archived Link
Information Handouts
- "Just Right" OCD Symptoms | IOCDF | 2009 Download Primary Link
- What are postpartum and perinatal OCD? | IOCDF Download Primary Link
Information (Professional)
- Scrupulosity and OCD: information packet for faith leaders | IOCDF, ADAA Download Primary Link Archived Link
Presentations
- Cognitive behavioral therapy for OCD | Sabine Wilhelm Download Primary Link Archived Link
- New directions in implementing exposure and response prevention: an inhibitory learning perspective | Jonathan Abramowitz | 2018 Download Primary Link Archived Link
- Cognitive Therapy for Contamination-Related OCD: ERP and Beyond | Adam Radomsky | 2011 Download Archived Link
- Interoceptive exposure: an underused weapon in the arsenal against obsessions and compulsions | Jonathan Abramowitz | 2018 Download Primary Link Archived Link
- Family affair: involving a partner or spouse in exposure and response prevention for OCD | Jonathan Abramowitz | 2018 Download Primary Link Archived Link
- A couple-based approach to CBT for BDD | Lillian Reuman, Jonathan Abramowitz | 2016 Download Primary Link Archived Link
- Body dysmorphic disorder | David Veale | 2017 Download Primary Link Archived Link
Treatment Guide
- NICE Guidelines For OCD and BDD | NICE | 2005 Download Primary Link
- Treatment of patients with OCD | American Psychiatric Association (APA) | 2007 Download Primary Link
- Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders (2014) | Katzman et al | 2014 Download Primary Link Archived Link
- A psychological perspective on hoarding – DCP good practice guidelines | Holmes, S., Whomsley, S., Kellet S. | 2015 Download Archived Link
- Treatment Manual For OCD | Clinical Research Unit for Anxiety Disorders (CRUFAD) | 2010 Download Primary Link Archived Link
Recommended Reading
- Veale, D. (2004). Advances in a cognitive behavioural model of body dysmorphic disorder. Body Image ,1, 113-125 Download Primary Link Archived Link
- Gillihan, S., Williams, M. T., Malcoun, E., Yadin, E., Foa, E. B. (2012) Common pitfalls in exposure and response prevention (EX/RP) for OCD. Journal of Obsessive-Compulsive and Related Disorders, 1, 251-257 Download Primary Link
- Rachman, S. (1997). A cognitive theory of obsessions. Behaviour Research and Therapy, 35(9), 793-802 Download Archived Link
- Mataix-Cols, D., et al (2010). Hoarding disorder: A new diagnosis for DSM-V? Depression and Anxiety, 27, 556-572. Download Archived Link
- Salkovskis, P. (1999). Psychological treatment of obsessive–compulsive disorder. Behaviour Research and Therapy, 37, S37-S52 Download Primary Link Archived Link
- Salkovskis, P. M. (2007). Psychological treatment of obsessive–compulsive disorder.Psychiatry,6(6), 229-233 Download Primary Link Archived Link
- Veale, D. (2007). Cognitive behavioural therapy for obsessive compulsive disorder. Advances in Psychiatric Treatment. 13, 438-446 Download Primary Link Archived Link
- Veale, D., Freeston, M., Krebs, G., Heyman, I., & Salkovskis, P. (2009). Risk assessment and management in obsessive–compulsive disorder. Advances in psychiatric treatment, 15(5), 332-343. Download Primary Link Archived Link
- Danesh, M., Beroukhim, K., Nguyen, C., Levin, E., & Koo, J. (2015). Body dysmorphic disorder screening tools for the dermatologist: A systematic review.Pract Dermatol,2, 44-49. Download Primary Link Archived Link
- Krebs, G., de la Cruz, L. F., & Mataix-Cols, D. (2017). Recent advances in understanding and managing body dysmorphic disorder. Evidence-Based Mental Health, 20(3), 71-75. Download Primary Link Archived Link
- Doron, G., & Derby, D. (2015). Assessment and treatment of relationship-related OCD symptoms (ROCD): a modular approach. Handbook of Obsessive-Compulsive Disorder across the Lifespan. Hoboken, NJ: Wiley (Forthcoming). Download Primary Link Archived Link
- Veale, D. (2001). Cognitive-behavioural therapy for body dysmorphic disorder. Advances in Psychiatric Treatment, 7, 125-132 Download Primary Link Archived Link
- Assessment and treatment of relationship-related OCD symptoms | Guy Doron, Danny Derby | 2017 Download Primary Link Archived Link
- Clark, D. A., & Rhyno, S. (2005). Unwanted intrusive thoughts in nonclinical individuals. Intrusive thoughts in clinical disorders: Theory, research, and treatment, 1-29 Download Primary Link Archived Link
What Is Obsessive Compulsive Disorder?
Signs and symptoms of ocd.
People with OCD experience obsessional thoughts, images, urges, and doubts. They often feel compelled to act or think in certain ways.
Obsessions are intrusive thoughts—thoughts that are unwanted and unacceptable, and which pop into our minds unbidden. Obsessions can be thoughts in the form of words, but also of images (pictures in our minds), urges or impulses, or feelings of doubt. Obsessive thoughts are experienced as unacceptable, disgusting, or senseless, and people with OCD find it hard not to pay attention to them. Examples of obsessions include:
- thoughts such as ‘My hands have been contaminated with germs’ or ‘Perhaps I am a pedophile’
- images of my family being murdered
- doubts such as ‘Have I left the stove on?’
- urges such as wanting to shout profanities
Compulsions follow from the way in which the individual interprets the intrusive thoughts. Compulsions are the reactions or mental actions that a person does in order to neutralize or ‘make safe’ following an obsession. People with OCD typically carry out compulsions in order to prevent a harm from happening for which they might be responsible, and/or to reduce any strong emotion which they feel. Exactly what someone with OCD may feel compelled to do will depend upon the meaning their intrusions have for them. Examples of compulsions might include:
- carefully washing food after having an intrusive thought about germs;
- calling family members to check they are OK after having an intrusive image about their deaths;
- going back to the house to check after doubting whether the stove was turned off;
- avoiding a public place after having an urge to shout profanities.
Prevalence of OCD
The lifetime prevalence rate of OCD in the United States is estimated to be 2.3% in adults (Kessler et al., 2005), and 1% to 2.3% in children and adolescents (Zohar, 1999).
Psychological Models and Theory of OCD
The cognitive behavioral theory of OCD proposes that when someone experiences an intrusive thought it is the appraisal—what they make of having the thought—that is most important (Salkovskis, Forrester, & Richards, 1998). Intrusive thoughts, even very unpleasant ones, are common and entirely normal . What seems to happen in OCD is that the fact of having intrusive thoughts is interpreted as being especially significant and, as a result, is especially anxiety-provoking. People with OCD are more likely to feel especially responsible for any potential harms and may feel especially strong emotion should they have intrusive thoughts about harm occurring. Compulsions are understood to be an active attempt to reduce harm. According to the cognitive model of OCD targets for intervention include:
- understanding and addressing the meaning of the intrusions;
- targeting compulsions and safety-seeking behaviors;
- modifying attentional biases.
Evidence-Based Psychological Approaches for Working with OCD
Cognitive behavioral therapy (CBT) is an evidence-based psychological treatment for OCD. Historically, CBT for OCD has involved the behavioral approach of exposure with response prevention (ERP). More cognitive approaches within CBT attempt to understand the patient’s appraisal of their intrusions and to find ways of exploring the validity and consequences of these appraisals.
Resources for Working with OCD
Psychology Tools resources available for working therapeutically with OCD may include:
- psychological models of obsessive-compulsive disorder (OCD)
- information handouts for obsessive-compulsive disorder (OCD)
- exercises for obsessive-compulsive disorder (OCD)
- CBT worksheets for obsessive-compulsive disorder (OCD)
- self-help programs for obsessive-compulsive disorder (OCD)
- Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry , 62 (6), 593–602.
- Salkovskis, P. M., Forrester, E., & Richards, C. (1998). Cognitive–behavioral approach to understanding obsessional thinking. The British Journal of Psychiatry , 173 (S35), 53–63.
- Zohar, A. H. (1999). The epidemiology of obsessive-compulsive disorder in children and adolescents. Child and Adolescent Psychiatric Clinics of North America , 8 (3), 445–460.
- For clinicians
- For students
- Resources at your fingertips
- Designed for effectiveness
- Resources by problem
- Translation Project
- Help center
- Try us for free
- Terms & conditions
- Privacy Policy
- Cookies Policy

Assessments & Worksheets
The following are a list of various assessments and worksheets that you may find helpful in your practice., assessments.
- Obsessional Beliefs Questionnaire (OBQ-44) and the Obsessional Beliefs Questionnaire Score Key
- Identifying Treatment-Interfering Behaviors (TIBS)
- ASI-IV and the ASI-IV Score Key
- Obsessive Concerns Checklist
- Compulsive Activities Checklist
- Child Saving Inventory - Parent Version
- BTTI Worry Management Worksheet
- BTTI Utility Analysis
- PISA Worksheet
- ERP Motivator IA - What Have I Lost To OCD?
- Response Prevention Plan
- Information-seekers vs reassurance-seekers
In This Section
More resources.
- Fact Sheets & Brochures
- Books About OCD
- From the Experts
- Educational Resources
Search iocdf.org
Your gift has the power to change the life of someone living with ocd..
- Patient Care & Health Information
- Diseases & Conditions
- Obsessive-compulsive disorder (OCD)
Steps to help diagnose obsessive-compulsive disorder may include:
- Psychological evaluation. This includes talking about your thoughts, feelings, symptoms and behavior patterns to find out if you have obsessions or compulsive behaviors that get in the way of your quality of life. With your permission, this may include talking to your family or friends.
- Physical exam. This may be done to rule out other issues that could cause your symptoms and check for any related complications.
Diagnostic challenges
It's sometimes hard to diagnose OCD because symptoms can be like those of obsessive-compulsive personality disorder, anxiety disorders, depression, schizophrenia or other mental health disorders. And it's possible to have OCD and another mental health disorder. Work with your doctor so that you can get the right diagnosis and treatment.
- Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your Obsessive-compulsive disorder (OCD)-related health concerns Start Here
Obsessive-compulsive disorder treatment may not result in a cure. But it can help bring symptoms under control so that they don't rule your daily life. Depending on how serious your OCD is, you may need long-term, ongoing or more-intensive treatment.
The two main treatments for OCD are psychotherapy and medicines. Psychotherapy also is known as talk therapy. Often, a mix of both treatments is most effective.
- Psychotherapy
Cognitive behavioral therapy (CBT), a type of psychotherapy, is effective for many people with OCD . Exposure and response prevention (ERP), a part of CBT therapy, involves exposing you over time to a feared object or obsession, such as dirt. Then you learn ways not to do your compulsive rituals. ERP takes effort and practice, but you may enjoy a better quality of life once you learn to manage your obsessions and compulsions.
Certain psychiatric medicines can help control the obsessions and compulsions of OCD . Most commonly, antidepressants are tried first.
Antidepressants approved by the Food and Drug Administration (FDA) to treat OCD include:
- Fluoxetine (Prozac) for adults and children 7 years and older.
- Fluvoxamine (Luvox) for adults and children 8 years and older.
- Paroxetine (Paxil) for adults only.
- Sertraline (Zoloft) for adults and children 6 years and older.
- Clomipramine (Anafranil) for adults and children 10 years and older.
However, your doctor may prescribe other antidepressants and psychiatric medicines.
Medicines: What to consider
When talking with your doctor about medicines for OCD , consider:
- Medicine selection. In general, the goal is to effectively control symptoms at the lowest possible dose. OCD may sometimes require higher doses of medicines to be the most effective in controlling your symptoms. It's not unusual to try several drugs before finding one that works well. Your doctor might recommend more than one medicine to effectively manage your symptoms. It can take weeks to months to get better after starting a medicine for your symptoms.
- Side effects. All psychiatric medicines may have side effects. Talk to your doctor about possible side effects and about any health monitoring needed while taking psychiatric drugs. And let your doctor know if you have troubling side effects.
- Suicide risk. Most antidepressants are generally safe, but the FDA requires that all antidepressants carry black box warnings. These are the strictest warnings for prescriptions. In some cases, children, teenagers and young adults under 25 may have an increase in suicidal thoughts or behavior when taking antidepressants. This is especially true in the first few weeks after starting or when the dose is changed. If suicidal thoughts occur, contact your doctor or get emergency help at once. Keep in mind that antidepressants are more likely to lower suicide risk in the long run by making your mood better.
- Interactions with other substances. When taking an antidepressant, tell your doctor about any other prescription medicines available without a prescription, herbs or other supplements you take. Some antidepressants can make some other medicines less effective and cause dangerous reactions when combined with certain medicines or herbal supplements.
- Stopping antidepressants. Antidepressants aren't thought to be addictive, but sometimes physical dependence can occur. Stopping treatment suddenly or missing several doses can cause withdrawal-like symptoms. This is sometimes called discontinuation syndrome. Don't stop taking your medicine without talking to your doctor, even if you're feeling better. You may have a relapse of OCD symptoms. Work with your doctor to lower your dose safely over time.
Talk to your doctor about the risks and benefits of using specific medicines.
Other treatment
Sometimes, psychotherapy and medicines can't control OCD symptoms. In cases that don't respond to treatment, other options may be offered:
- Intensive outpatient and residential treatment programs. Full treatment programs that stress ERP therapy principles may help people with OCD who struggle with being able to function because of how serious their symptoms are. These programs usually last several weeks.
- Deep brain stimulation (DBS). The FDA has approved DBS to treat OCD in adults ages 18 years and older who don't respond to traditional treatment. DBS involves implanting electrodes within certain areas of your brain. These electrodes produce electrical impulses that may help control impulses that aren't typical. DBS isn't widely available, and it is rarely used.
- Transcranial magnetic stimulation (TMS). The FDA has approved three TMS devices — BrainsWay, MagVenture and NeuroStar — to treat OCD in adults. These devices are used when traditional treatment hasn't been effective. TMS doesn't require surgery. It uses magnetic fields to stimulate nerve cells in the brain to make symptoms of OCD better. During a TMS session, an electromagnetic coil is placed against your scalp near your forehead. The coil delivers a magnetic pulse that stimulates nerve cells in your brain.
If you're thinking about DBS or TMS , talk with your doctor to make sure you understand all the pros and cons and possible health risks.
More Information
Obsessive-compulsive disorder (OCD) care at Mayo Clinic
- Cognitive behavioral therapy
- Deep brain stimulation
- Electroconvulsive therapy (ECT)
- Transcranial magnetic stimulation
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Lifestyle and home remedies
Obsessive-compulsive disorder is a chronic condition, which means that it may always be part of your life. While a professional should treat OCD , you can do some things to build on your treatment plan:
- Practice what you learn. Work with your mental health professional to pinpoint methods to help manage symptoms. Practice these methods regularly.
- Take your medicines as directed. Even if you're feeling well, don't skip your medicines. If you stop, OCD symptoms are likely to return.
- Pay attention to warning signs. You and your doctor may have pinpointed issues that can cause your OCD symptoms. Make a plan so that you know what to do if symptoms return. Contact your doctor or therapist if you notice any changes in symptoms or how you feel.
- Check first before taking other medicines. Contact the doctor who's treating you for OCD before you take medicines prescribed by another doctor or before taking any medicines available without a prescription, vitamins, herbal remedies or other supplements. This will help reduce possible interactions.
Coping and support
Coping with obsessive-compulsive disorder can be challenging. Medicines can have unwanted side effects, and you may feel embarrassed or angry about having a condition that requires long-term treatment.
Here are some ways to help cope with OCD :
- Learn about OCD . Learning about your condition can help you stick to your treatment plan.
- Stay focused on your goals. Keep your recovery goals in mind, and remember that recovery from OCD is an ongoing process.
- Join a support group. Reaching out to others facing similar challenges can provide you with support and help you cope with challenges.
- Find healthy outlets. Explore healthy ways to channel your energy, such as hobbies and recreational activities. Exercise regularly, eat a healthy diet and get adequate sleep.
- Learn relaxation and stress management. In addition to professional treatment, stress management methods such as meditation, visualization, muscle relaxation, massage, deep breathing, yoga or tai chi may ease stress and anxiety.
- Stick with your regular activities. Try not to avoid meaningful activities. Go to work or school as you usually would. Spend time with family and friends. Don't let OCD get in the way of your life.
Preparing for your appointment
You may start by seeing your primary care team. Because obsessive-compulsive disorder often requires specialized care, you may need to see a mental health professional, such as a psychiatrist or psychologist.
What you can do
To prepare for your appointment, think about your needs and goals for treatment. Make a list of:
- Any symptoms you've noticed, including the types of obsessions and compulsions you've had and things that you may be staying away from or no longer doing because of your distress.
- Key personal information, including any major stresses, recent life changes and family members with similar symptoms.
- All medicines, vitamins, herbal remedies or other supplements, as well as the doses.
- Questions to ask your doctor or therapist.
Questions to ask might include:
- Do you think I have OCD ?
- How do you treat OCD ?
- How can treatment help me?
- Are there medicines that might help?
- Will exposure and response prevention therapy help?
- How long will treatment take?
- What can I do to help myself?
- Are there any brochures or other printed material that I can have?
- Can you recommend any websites?
Don't hesitate to ask any other questions during your appointment.
What to expect from your doctor
Your doctor is likely to ask you some questions, such as:
- Do certain thoughts go through your mind over and over despite trying to ignore them?
- Do you have to have things arranged in a certain way?
- Do you have to wash your hands, count things, or check things over and over?
- When did your symptoms start?
- Have symptoms been continuous or once in a while?
- What, if anything, seems to improve the symptoms?
- What, if anything, appears to make the symptoms worse?
- How do the symptoms affect your daily life? Do you stay away from anything because of your symptoms?
- In a typical day, how much time do you spend on obsessive thoughts and compulsive behaviors?
- Have any of your relatives had a mental health disorder?
- Have you had any trauma or major stress?
Your doctor or mental health professional will ask more questions based on your responses, symptoms and needs. Preparing for questions like these will help you make the most of your appointment time.
- Kara PJ, et al. Deep brain stimulation for obsessive compulsive disorder: Evolution of surgical stimulation target parallels changing model of dysfunctional brain circuits. Frontiers in Neuroscience. 2019; doi:10.3389/fnins.2018.00998.
- Allscripts EPSi. Mayo Clinic. 2019.
- Obsessive-compulsive and related disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5-TR. 5th ed. American Psychiatric Association; 2022. https://dsm.psychiatryonline.org. Accessed May 17, 2023.
- Blair Simpson H. Pharmacotherapy for obsessive-compulsive disorder in adults. https://www.uptodate.com/search. Accessed May 17, 2023.
- Blair Simpson H. Obsessive-compulsive disorder in adults: Epidemiology, pathogenesis, clinical manifestations, course, and diagnosis. https://www.uptodate.com/search. Accessed May 17, 2023.
- Abromowitz J. Psychotherapy for obsessive-compulsive disorder in adults. https://www.uptodate.com/search. Accessed May 17, 2023.
- Obsessive-compulsive disorder. National Alliance on Mental Illness. https://www.nami.org/Learn-More/Mental-Health-Conditions/Obsessive-compulsive-Disorder/Overview. Accessed May 17, 2023.
- Obsessive-compulsive disorder in children and adolescents. American Academy of Child & Adolescent Psychiatry. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Obsessive-Compulsive-Disorder-In-Children-And-Adolescents-060.aspx. Accessed May 17, 2023.
- Obsessive-compulsive disorder: When unwanted thoughts or repetitive behaviors take over. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd. Accessed May 17, 2023.
- Mental health medications. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/mental-health-medications. Accessed May 17, 2023.
- AskMayoExpert. Obsessive-compulsive disorder (OCD). Mayo Clinic; 2023.
- Depression. National Institute of Mental Health. https://www.nimh.nih.gov/health/publications/depression. Accessed May 17, 2023.
- Obsessive-compulsive disorder (OCD). Merck Manual Professional Version. https://www.merckmanuals.com/professional/psychiatric-disorders/obsessive-compulsive-and-related-disorders/obsessive-compulsive-disorder-ocd. Accessed May 17, 2023.
- Woody EZ, et al. Obsessive compulsive disorder (OCD): Current treatments and a framework for neurotherapeutic research. Advances in Pharmacology. 2019; doi:10.1016/bs.apha.2019.04.003.
- Cervin M. Obsessive-compulsive disorder: Diagnosis, clinical features, nosology and epidemiology. Psychiatric Clinics of North America. https://www.clinicalkey.com. Accessed May 17, 2023.
- Sawchuk CN (expert opinion). Mayo Clinic. June 23, 2023.
Associated Procedures
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

ERP for OCD: A Brief Primer
Ocd is a debilitating disorder, but treatment is available..
Posted January 19, 2019 | Reviewed by Jessica Schrader
- What Is Obsessive-Compulsive Disorder?
- Find a therapist to treat OCD
Obsessive-compulsive disorder (OCD) is an oft-debilitating disorder that affects 1-3% of the U.S. population. The main symptoms of OCD are, as the name suggests, obsessions and compulsions. Obsessions are intrusive unwanted thoughts, images, or impulses that cause much distress and anxiety . Compulsions are behaviors or rituals that are performed repeatedly in order to reduce the anxiety. Obsessions tend to cluster around common themes: Contamination worries, doubting/harm fears, symmetry/completeness urges, and unacceptable thoughts (blasphemous, violent, sexual ). Compulsions, too, tend to fall into fairly clear categories: Cleaning/washing, checking, arranging/ordering, and counting/mental rituals.
The causes of OCD are not known. Biology is certainly involved, as obsessions and compulsions run in families , and appear in various medical conditions, including Huntington’s chorea, Parkinson’s disease, Tourette disorder, schizophrenia, and certain epilepsies, brain injuries, and tumors. The disorder may appear in childhood or later; it is often chronic, exacerbated by stress , and co-morbid with other anxiety and mood difficulties.
People with OCD characteristically find themselves preoccupied with distressing unwelcome thoughts. For example, they may believe they are responsible for some harm that may come to themselves or others, and assume that any influence they have over an outcome equals total responsibility for it (“I will fail to do something and it will lead to myself/others being hurt”). They often seek perfection and are distressed by its unattainability (“my hands are not perfectly clean; not clean enough”). People with OCD often experience what is known as, ‘thought-action fusion,’ equating a thought with an action. When distressing thoughts come to occupy and overwhelm them, they will often attempt to suppress the thoughts directly, a futile effort sometimes known as the ‘white bear problem’ (if we try not to think of a white bear, we end up thinking about it). Preoccupations with dangers, flaws, or mistakes are common. People with OCD often spend much energy and time ‘looking for trouble’ so to speak, acutely attuned to the cloud in the silver lining.
To deal with the distress caused by fearful thoughts and images, people with OCD turn to increasingly elaborate rituals and safety behaviors. These rituals of cleaning, checking, ordering, or counting are a means of anxiety avoidance. Like many other avoidance strategies, they work well in the short term. Alas in the long term they become a problem themselves. People with OCD end up working for their rituals long after the rituals have ceased working for them. In this, the underlying dynamics of OCD resemble drug addiction , in which the substance that was used for stress relief over time becomes a destructive stressor itself.
Obsessions and compulsions may be thought of as extreme, grotesque permutations of common and benign thoughts and behaviors. Many of us have occasional repetitive, intrusive, or strange thoughts. You imagine punching your boss in the face. You ruminate over lost love. Many of us perform stereotyped or superstitious behaviors. You wear your lucky tie to the job interview. You press the elevator button several times in a row. These behaviors may resemble OCD, but what sets them apart from the disorder is that they do not overwhelm you or cause significant distress and disruption in your life. In this case, to paraphrase Marks, quantity often creates quality. Washing your hands routinely after you go to the bathroom is not OCD. Washing your hands 100 times until they are red and raw is.
By the available empirical evidence , the best behavioral treatment for OCD is Exposure and Response Prevention (ERP). ERP is designed to break the two maladaptive associations that reside at the core of OCD: The association between sensations of distress and the objects, situations, or thoughts that produce the distress, and the association between performing ritualistic behaviors and decreasing the distress.
With regard to obsessions, the goal of ERP is to have the client learn that they can have intrusive thoughts and experience distress without losing control of their behavior and without having to suppress their feelings or escape (or avoid) fearful situations. Exposure is the key therapeutic component to that end. Exposure is a procedure in which the client purposely confronts objects, images, thoughts, or situations that elicit distress and anxiety (but pose no real danger). The client then stays in those situations long enough for the anxiety to decrease.
Such a decrease in anxiety is achieved via several concurrent processes. First is physiological habituation , a process whereby nervous system arousal (which is necessary for the experience of anxiety) is reduced upon prolonged exposure to the same stimulus. Second is inhibitory learning , a process whereby new associations inhibit (rather than extinguish) old ones. Third is psychological empowerment, whereby the client learns from experience that they can manage distress, thus developing greater self-efficacy regarding coping. Fourth is skill acquisition whereby practice makes competence and competence reduces the need for fear . Finally, change during exposure happens through what is known in the literature as expectancy violations , as predicted disastrous consequences fail to materialize.
With regard to compulsions, the goal of ERP is for the client to learn, through experience, that they don’t need rituals to manage anxiety well. Response prevention is the key component here. It involves, as the name indicates, preventing the client from performing the ritual behaviors they engage in to reduce anxiety. As mentioned above, compulsive rituals are a form of anxiety avoidance. As such they prevent the clients from ever experiencing the benefits of true exposure. Response prevention, in contrast, facilitates the client’s heightened anxious arousal during exposure, and therefore helps the exposure exert its therapeutic effects.

Generally, ERP treatment will proceed in an orderly sequence of stages. Treatment will usually begin with a thorough assessment of symptoms. The therapist will work with the client to 1. Identify the client’s obsessions, their intrusive thoughts, images, or urges. 2. Identify the client’s rituals, what they do to decrease their anxiety, get rid of the thoughts, images, or urges, or minimize the likelihood of a feared consequence. 3. Identify the feared consequences (“if you had thought X and couldn't perform ritual Y what are you worried would happen?”) 4. Identify avoidances, situations that the client avoids so as not to feel anxious or have intrusive thoughts, images, or urges.
The second step is a process known as psycho- education in which, as the name implies, the client will receive accurate information about OCD, including prevalence statistics, common symptoms, available treatments and their effectiveness. The ERP approach is usually introduced during the process of psycho-education, and the client learns about the treatment rationale, goals , structure, and components.
Then, the therapist and client will usually develop an ‘exposure hierarchy,’ (AKA ‘anxiety ladder’) consisting of feared and avoided things, places, and situations. To gauge the client’s distress, the therapist will often use a Subjective Units of Distress Scale (SUDS). Each item in the hierarchy will receive a SUDS rating (0-100), ranking items in order from least distressing to most distressing.
Once the hierarchy is set, ERP sessions will tackle each item on it, working gradually up the levels of distress. As the client faces distressful items, they are concurrently prevented from engaging in corresponding rituals or distracting ‘safety behaviors.’ ERP can be conducted in session—in the therapy room, with a therapist; or In Vivo—in real-life situations with a therapist. It can also be carried out as homework without a therapist, and the therapist may also use ‘imaginal exposure’—having clients use their imagination to picture an exposure situation.
ERP works best when the exercises are specific and well designed, when the client’s anxious arousal is intense, and when the ‘dose’ of exposure is substantial and systematic. Sessions are often longer than usual (90-120 minutes), and twice or thrice weekly sessions are common. ERP is a sort of psychological workout. As in any workout, you tend to get out of it what you’ve put in. ERP is also aversive by design. It works through pain, not away from or around it. Thus, many people with OCD ask for constant reassurance during therapy. While reassurance is often useful in therapy, it undermines the effectiveness of ERP, interfering with full exposure. Reassurance seeking is in essence an OCD symptom (a ritual). Both client and therapist need to be aware of this. The therapist must remain accepting and non-punitive yet firm in emphasizing the importance of full exposure head on, sans distractions or detours . The client needs to summon their courage and perseverance, and accept the fact that short-term pain is the price of acquiring long-term health and wellbeing. The short-term pain of ERP is a better deal than living with the long-term punishment of untreated OCD.
If you are curious about your own OCD symptoms, here is a link to a solid screening instrument.
To find a therapist, please visit the Psychology Today Therapy Directory .

Noam Shpancer, Ph.D., is a professor of psychology at Otterbein University and a practicing clinical psychologist in Columbus, Ohio.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
18 Anxiety Worksheets for Adults, Teens & More

And yet, it can also be energizing, focusing our attention and preparing us for action — an evolutionary response to the unexpected, difficult, or downright dangerous (Workman & Reader, 2015).
It is not so much what happens but how we respond that matters the most (Joseph, 2013).
Therapists, counselors, and coaches can help by working with clients to change how they react to anxiety-inducing situations.
In this article, we introduce a collection of free worksheets for use by mental health professionals with their clients or as self-help activities.
Before you continue, we thought you might like to download our three Stress & Burnout Prevention Exercises (PDF) for free . These science-based exercises will equip you and your clients with tools to better manage stress and find a healthier balance in your life.
This Article Contains
5 best anxiety worksheets, 4 anxiety worksheets for teens, 3 social anxiety worksheets, 3 anxiety activities for adults, cbt worksheets for anxiety, positivepsychology.com resources, a take-home message.
We can learn to break free from anxiety. With the right approaches, the same situations can have different outcomes (Forsyth & Eifert, 2016).
The following five worksheets encourage clients to recognize that they are not alone in their experiences and can, indeed, learn how to cope with anxiety.
The activities work on their own or can be combined. They support clients by helping them identify situations that cause anxiety, using mindfulness and meditation to restore a balanced perspective, and recognizing that someone should not be defined by the extreme emotions they are experiencing (Forsyth & Eifert, 2016; Southwick & Charney, 2018):
1. Anxiety Hierarchy
Intense fears, phobias, and stressful situations can be highly anxiety provoking. It is helpful to establish a list of challenging situations that result in extreme upset or negative emotions for clients (American Psychological Association, 2016).
Use the Anxiety Hierarchy exercise to list situations that lead to anxiety and rate them on a scale from 1 (mild discomfort) to 10 (extreme emotions such as panic).
Once these anxiety-inducing situations are listed and sorted in order, the practitioner can use graded exposure practices as part of systematic desensitization.
2. Breath Awareness While Waiting
Waiting for an event can leave us excited, concerned, nervous, or anxious. We may notice changes to our physiology (increased heart rate, sweating, and faster breathing), cognition (erratic thinking, poor decision-making, and a failing memory), and emotions (fear, upset, and panic ; Peterson, 2018).
Work with the client to identify times they are waiting during the week — for example, waiting for the bus, at the school gates, at an appointment — and how they expect to feel.
Then use this breath awareness practice for mindful breathing: slowly breathing in through the nose, holding, and slowly breathing out through the mouth. As unhelpful thoughts enter the mind, direct attention back to breathing.
3. Creating a Mindfulness Anxiety Plan
Our behavior often follows patterns, and so does our anxiety. It is possible to anticipate when anxiety might show up, especially when we become more in tune with our bodies and the events around us (Peterson, 2018).
By creating a mindfulness anxiety plan , we can be ready with a list of actions to perform when we begin to recognize our anxiety taking shape and in advance of situations that can be difficult. These actions should aim to improve our wellbeing and leave us less anxious throughout the day
For example, “If my anxiety is getting away from me, I will call my best friend.” Or “Every day, I will go outside for a walk at lunchtime and try to be more mindful.”
4. Who Am I Beyond My Anxiety?
We are not our emotions, but when fearful or anxious, we spend a great deal of time and energy focusing on what is wrong with us, forgetting our strengths (Forsyth & Eifert, 2016).
In this exercise , the client mindful reflects on the following prompts (among others):
I am someone who … I really like … My most important relationship is … I feel my best when …
Reading through the answers helps remind us that anxiety does not define who we are.
5. Funeral Meditation
Often, we stop ourselves from taking on or embracing a challenge for fear of failure or experiencing anxiety.
Despite its foreboding name, the Funeral Meditation is used within Acceptance and Commitment Therapy to help free ourselves from the grip of anxiety (Forsyth & Eifert, 2016).
This powerful meditation helps us reflect on what matters to us, recognizing that, at any time, we can start living in line with how we want to be remembered.
After several calming breaths, we imagine what our funeral would be like, including:
How do people look? Who would be there? What would they say? What would we like people to say about us?
Recognizing our values can help us eliminate anxiety and begin living the way we want.

The following worksheets can also be adapted for adult populations, and mental health practitioners will find them valuable when working with adolescents coping with anxiety.
1. Best and Worst
Children and teens can benefit from stepping back from anxiety-inducing situations to reflect upon how, despite being scary, they can also be exciting.
For example, joining a new class, school, or social group can bring with it feelings of anxiety. When also recognized as exciting, it can be energizing, leading to positive emotions such as hope, curiosity, and gratitude.
Work with your teen client to:
- Identify and capture a situation that makes them feel nervous or scared.
- Use the diagram to capture what is exciting in the left-hand circle and what is scary about the situation in the right-hand circle.
- Write down aspects of the situation that are both scary and exciting in the intersection between the two circles.
Identifying how something fills us with fear while providing energy can help us have a more balanced view regarding how to approach what is ahead.
2. FLARE for Anxiety and Fear
This helpful worksheet helps teach acceptance of difficult feelings (rather than hiding from or rejecting them) through self-acceptance and self-compassion (Khazan, 2019).
The FLARE acronym directs the client to:
- Feel each sensation. Become aware of their heart rate, breath, and body temperature.
- Label the sensations. Do they feel worried, fearful, or anxious?
- Allow the experience to remain as it is. They can say to themselves, “It is OK to feel this way.”
- Respond by refocusing on breathing, taking each breath slowly and making the out-breath longer than the in-breath.
- Expand awareness of their environment and reflect on what they are grateful for that day.
By focusing on positive emotions, the approach builds toward a spiral of positive feelings (Fredrickson, 2010).
3. Radio Doom and Gloom
Teenagers are vulnerable to focusing on the worst events, situations, and outcomes. As a result, it can almost seem like an endless radio program playing in the background, broadcasting negative stories and songs all day long.
While it’s not easy to turn down the volume on the radio (or turn it off completely), we can attend to it less. By learning to treat such negative thinking as background noise and focusing more on current activities, its impact and ability to heighten anxiety are reduced.
4. When I’m Scared
Children and adolescents (and even adults) feel scared sometimes. And that’s OK. It’s a perfectly normal fight-or-flight response to a perceived — or actual — uncomfortable or dangerous situation.
Talking to an adult can help.
When I’m Scared can be used with individual youths or in a group setting.
They are asked to write down what makes them frightened, how it affects their thinking, how it feels physically, and one thing might be that makes them feel better.
Download 3 Free Stress & Burnout Prevention Exercises (PDF)
These detailed, science-based exercises will equip you or your clients with tools to manage stress better and find a healthier balance in their life.
Download 3 Stress & Burnout Prevention Exercises Pack (PDF)
By filling out your name and email address below.
- Email Address *
- Your Expertise * Your expertise Therapy Coaching Education Counseling Business Healthcare Other
- Email This field is for validation purposes and should be left unchanged.
Social anxiety leads to persistent fear and the avoidance of social situations because of concerns about being evaluated by others (Schneier & Goldmark, 2015).
Therapy and the use of interventions enable clients to increase their social engagement and form deep, meaningful relationships (Schneier & Goldmark, 2015).
The following worksheets are valuable for mental health professionals helping clients identify what triggers their anxious thinking and manage them through visualization and mindfulness.
1. A Mountain of Worries
Our worries can mount up. Stresses, concerns, upsets, and things going wrong may seem never-ending, with even the most minor problems blown out of proportion, leaving our anxiety out of control.
This exercise captures situations that bother us and is particularly helpful for social anxiety, where we can begin to identify and reflect on unhelpful thought patterns and learn to expect and plan for how to handle them.
2. Event visualization worksheet
Visualization can feel as real to the mind as experiencing a situation first-hand — especially a social one — and offers a safe and controlled environment to explore and experiment with existing and future challenges (Clough & Strycharczyk, 2015).
Visualizing an event, especially one we are worrying about, can be a powerful and helpful way of reducing concern and anxiety and gaining confidence without the risk of failure or being overwhelmed.
Use the worksheet to:
- Identify an event likely to cause anxiety.
- Visualize the event in as much detail as possible using all the senses.
- Imagine the people and the situation.
- Reflect on how being successful might feel.
Clients can repeat the visualization exercise several times until they feel comfortable and less anxious.
3. The Documentary of You
Anxiety can arise from any environment and is particularly common in social situations (Schneier & Goldmark, 2015).
Mindfulness can help us think about ourselves and our situations with more compassion and forgiveness and less judgment (Forsyth & Eifert, 2016).
In this exercise , the client imagines their life playing out as a movie on a screen. They capture on paper, nonjudgmentally, situations that leave them feeling anxious.
Following a series of grounding breaths, the client considers each one mindfully without becoming too involved.
Finally, they reflect on how reading the story now makes them feel. What is their degree of anxiety?

Changing your relationship with it can help us take charge of our lives (Forsyth & Eifert, 2016).
Try the following three activities to create coping strategies, identify what we can control while learning to accept everything else, and become more comfortable with discomfort.
1. Anxiety Strategy Cards
Preparation is a crucial part of managing anxiety. This sheet contains a list of cards to help clients develop strategies for events and situations where they feel out of control and stressed, with their anxiety building.
Each card offers a valuable reminder of a powerful technique that will help them restore their physical, cognitive, emotional, and behavioral balance.
For example:
When I feel anxious, I could try … controlled breathing. When I feel anxious, I could try … visualization. When I feel anxious, I could try … a grounding technique.
Use them with psychoeducation and technique training to build confidence in the client’s ability to handle and overcome tough times.
2. Control–Influence–Accept Model
We can’t control every situation, so it’s helpful to recognize those that can be influenced by our behavior and those that cannot.
The Control–Influence–Accept Model can stop individuals from feeling overwhelmed and experiencing feelings of hopelessness, frustration, and anxiety when they experience a loss of control or indecision (Thompson & Thompson, 2018).
The client is encouraged to perform each of the following:
- Identify a potentially tricky situation.
- Capture what can be controlled or influenced.
- What cannot be controlled or influenced must be accepted.
- List what needs to be accepted.
Having performed each step, the client reflects on how they now feel about the situation and whether they are left wishing to control or influence anything they have accepted.
3. Interoceptive Exposure
Anxiety has a strong physical element that we can use to increase awareness of panic-related physiological symptoms .
Interoceptive exposure is built on the premise that exposure to such sensations can increase our familiarity with them and our preparedness for future anxiety-inducing situations.
The worksheet uses activities that induce physical, cognitive, and emotional discomfort to replicate the sensations of panic and anxiety.
Note: These should only be used under the guidance of a physician or health professional in a suitably safe environment.
Cognitive-Behavioral Therapy (CBT) treats anxiety by restructuring the client’s thinking, with the therapist exploring maladaptive expectations and worries related to upcoming events (Dobson & Dozois, 2021).
1. Anxiety Record
Reflecting on and sharing what makes us anxious can leave us feeling vulnerable, but it is essential. Understanding what leaves us feeling this way allows us to prepare for situations and learn appropriate coping skills.
One of the most powerful techniques is recognizing and, if possible, replacing unhelpful thinking.
Use the simple form in the worksheet to capture the following:
What does the anxiety feel like? When does it happen? What thoughts do you experience? How realistic are these thoughts? What thoughts could you replace them with? Are they more realistic?
Capturing our anxieties is an essential part of reducing them and bringing them under control.
2. Dealing with anxiety: Reverse the Rabbit Hole
The two words “what if?” can be anxiety- inducing, sending our thoughts racing down a rabbit hole of all that could go wrong.
What if I forget the words when I’m on stage? What if my date doesn’t like me?
Reframing an experience helps us experience it differently. We can turn a negative into a positive — reverse the rabbit hole.
In this exercise , we write negative outcomes in the left-hand column and then a corresponding reversed, positive outcome on the right.
What if I nail the speech? What if my date goes really well?
3. Tackling Anxious Thoughts
Anxiety can bias our thinking by making us buy into the likelihood of something terrible happening. As a result, it can be helpful to consider the following three points:
What is the worst potential consequence of this scenario? What is the best possible consequence of this scenario? What do you feel is the most likely consequence of this scenario?
Following these questions, the client thinks about how it would feel in a year’s time if the worst actually happened.
After all, even if the worst outcome becomes a reality, it may be less catastrophic than we imagine.
17 Exercises To Reduce Stress & Burnout
Help your clients prevent burnout, handle stressors, and achieve a healthy, sustainable work-life balance with these 17 Stress & Burnout Prevention Exercises [PDF].
Created by Experts. 100% Science-based.
We have many resources available for therapists to support clients experiencing anxiety.
More extensive versions of the following tools are available with a subscription to the Positive Psychology Toolkit© , but they are described briefly below:
- Replacing Unhelpful Thoughts with Helpful Alternatives CBT is based on the premise that emotions and behaviors result from a person’s interpretation of a situation.
This exercise invites clients to examine the “helpfulness” of a thought they are having about a current challenging situation before formulating a more helpful alternative thought:
- Step one – Describe a challenging situation.
- Step two – Identify the automatic unhelpful thought.
- Step three – Rate the helpfulness of this thought.
- Step four – Come up with a more helpful alternative thought.
- Step five – Rate the helpfulness of this alternative thought.
- Step one – Visualize yourself in a relaxing environment.
- Step two – Add detail to the visualization by exploring all your senses.
- Step three – Enjoy the scene you have created and allow yourself to spend some time taking it all in.
- Step four – Close your eyes and continue taking slow, deep breaths as you visualize the stress leaving your body in waves with each exhale.
This exercise is valuable for stress reduction by connecting the sensations of relaxation with peaceful visual imagery during times of stress.
If you’re looking for more science-based ways to help others manage stress without spending hours on research and session prep, check out this collection of 17 validated stress management tools for practitioners. Use them to help others identify signs of burnout and create more balance in their lives.
Anxiety is a normal reaction to life events and can be beneficial in many situations, alerting us to dangers and increasing our attention and readiness for action.
It is often less about our environment or the challenges we face, but how we interpret them.
As a result, anxiety can dramatically impair our ability to function and perform in education, work, and social environments (American Psychological Association, 2016).
Its effects are widespread, impacting 30% of adults at some point in their lives and preventing them from living normally (American Psychiatric Association, 2021). They can find themselves avoiding opportunities and shying away from challenges due to intrusive thoughts or concerns.
Anxiety disorders are treatable. Therapists and counselors can help clients manage anxiety-inducing situations by changing how they view them and learning to cope with stressful conditions.
The anxiety worksheets in this article can be used independently or together as interventions for better managing anxiety. When combined with ongoing therapeutic assessment, it is possible to see how clients bring their feelings under control and return to the lives they wish to lead.
We hope you enjoyed reading this article. Don’t forget to download our three Stress & Burnout Prevention Exercises (PDF) for free .
Ed: Updated March 2023
- American Psychiatric Association. (2021). What are anxiety disorders? Retrieved March 17, 2023, from https://www.psychiatry.org/patients-families/anxiety-disorders/what-are-anxiety-disorders
- American Psychological Association. (2016). Beyond worry: How psychologists help with anxiety disorders . Retrieved March 13, 2023, from https://www.apa.org/topics/anxiety/disorders
- Clough, P., & Strycharczyk, D. (2015). Developing mental toughness: Coaching strategies to improve performance, resilience and wellbeing . Kogan Page.
- Dobson, K. S., & Dozois, D. J. (2021). Handbook of cognitive-behavioral therapies . Guilford Press.
- Forsyth, J. P., & Eifert, G. H. (2016). The mindfulness & acceptance workbook for anxiety: A guide to breaking free from anxiety, phobias & worry using acceptance & commitment therapy (2nd ed.). New Harbinger Publications.
- Fredrickson, B. (2010). Positivity: Groundbreaking research reveals how to release your inner optimist and thrive . Oneworld.
- Joseph, S. (2013). What doesn’t kill us: A guide to overcoming adversity and moving forward . Piatkus.
- Khazan, I. Z. (2019). Biofeedback and mindfulness in everyday life: Practical solutions for improving your health and performance . W.W. Norton & Company.
- Khesht-Masjedi, M. F., Shokrgozar, S., Abdollahi, E., Habibi, B., Asghari, T., Ofoghi, R. S., & Pazhooman, S. (2019). The relationship between gender, age, anxiety, depression, and academic achievement among teenagers. Journal of Family Medicine and Primary Care , 8 (3), 799–804.
- Peterson, T. J. (2018). The mindfulness workbook for anxiety: The 8-week solution to help you manage anxiety, worry & stress . Althea Press.
- Schneier, F., & Goldmark, J. (2015). Social anxiety disorder. In D. J. Stein & B. Vythilingum (Eds.), Anxiety disorders and gender (pp. 49–67). Springer.
- Southwick, S. M., & Charney, D. S. (2018). Resilience: The science of mastering life’s greatest challenges . Cambridge University Press.
- Thompson, S., & Thompson, N. (2018). The critically reflective practitioner . Macmillan International Higher Education.
- Workman, L., & Reader, W. (2015). Evolutionary psychology: An introduction . Cambridge University Press.
Share this article:
Article feedback
What our readers think.
Thank you. This helps so much I would definitely recommend this article especially for anxious people like me. Very generous of you guys.
I am a mental health professional Mental Health Skill Building and some of this information is very good for my clients. Thank you.
Thank you. So many resources and ideas in one place. We are in New Zealand. It is hard to access quality support here and too many don’t.
I am DYING for the ‘What if’ download. I do this all the time.
Awesome site – thank you!!
what an amazing website, jam packed with FREE and very useful information, thank you so much!!! I am currently working with a teenager and the ‘what-if’ worksheet alone is pure gold and just the thing I was looking for right now.
How do I get the What If worksheet?
Let us know your thoughts Cancel reply
Your email address will not be published.
Save my name, email, and website in this browser for the next time I comment.
Related articles

Overcome Languishing & Flourish: A Positive Psychology Guide
Amidst the turmoil of the recent pandemic, one positive psychology construct has captured more attention than any other. As societies worldwide had to endure lockdowns [...]

7 Trauma Response Types & How to Recognize Them
Over-sharing. Over-explaining. Trauma dumping. Hyperindependence. Hypersexualization. People pleasing. Do these sound like common traits your clients have? These may not be character traits but, instead, [...]

6 Best Diaphragmatic Breathing Exercises to Reduce Anxiety
Our brain controls our breathing largely without conscious awareness. We shower, watch football, listen to music, and sleep while our respiratory system functions in the [...]
Read other articles by their category
- Body & Brain (49)
- Coaching & Application (58)
- Compassion (25)
- Counseling (51)
- Emotional Intelligence (23)
- Gratitude (18)
- Grief & Bereavement (21)
- Happiness & SWB (40)
- Meaning & Values (26)
- Meditation (20)
- Mindfulness (44)
- Motivation & Goals (45)
- Optimism & Mindset (34)
- Positive CBT (30)
- Positive Communication (20)
- Positive Education (47)
- Positive Emotions (32)
- Positive Leadership (19)
- Positive Parenting (15)
- Positive Psychology (34)
- Positive Workplace (37)
- Productivity (17)
- Relationships (43)
- Resilience & Coping (37)
- Self Awareness (21)
- Self Esteem (38)
- Strengths & Virtues (32)
- Stress & Burnout Prevention (34)
- Theory & Books (46)
- Therapy Exercises (37)
- Types of Therapy (64)
- Phone This field is for validation purposes and should be left unchanged.
3 Stress Exercises Pack

IMAGES
VIDEO
COMMENTS
Overcoming Your OCD A Therapy Assignment Workbook ... used as therapeu]c homework. Overcoming Your OCD is one of a series of workbooks designed ... Obsessive-compulsive disorder impacts people of all ages and walks of life. It is defined by obsessive, uncontrollable, recurring thoughts, images, and impulses that are intrusive and ...
This OCD worksheet packet includes a blank exposure hierarchy template, and an exposure therapy homework form. The homework form provides a professional way for you to record your client's weekly exposure homework, and it gives your clients a nice place to keep track of their progress. To learn more about implementing these tools, check out our ...
Whether it's financial, insurance-related, time, or motivation, you may find yourself unable to immediately access treatment for OCD. If you are experiencing those barriers, or if you just want a supplement to your treatment with some extra "homework," we have resources for you. Putting your thoughts and experiences down on paper can be ...
1. Recurrent and persistent thoughts, urges, or impulses, that are experienced at some time during the disturbance as intrusive and unwanted, and often cause anxiety. 2. The individual attempts to ignore or suppress these thoughts, urges, or images, or to neutralize them with another thought or action. Compulsions.
Obsessive-compulsive disorder (OCD) is characterized by intrusive thoughts, images, urges, or impulses that are interpreted as threating (obsessions). These lead to active and counterproductive attempts to reduce the thoughts and/or discharge the perceived responsibility associated with them (compulsions). Cognitive and behavioral approaches ...
treatments for OCD CBT that relies primarily on behavioral techniques such as exposure and response prevention (ERP) is recommended because it has the best evidentiary support *American Psychiatric Association. Practice guideline for the treatment of patients with obsessive-compulsive disorder. Am J Psychiatry 2007; 164(suppl):1-56.
Cognitive behavioral therapy (CBT) encompasses a range of therapy techniques that are highly beneficial in treating obsessive compulsive disorder (OCD), including exposure and response prevention and cognitive restructuring. Most people who receive CBT treatment for OCD start noticing improvements within weeks. CBT generally consists of weekly, one-hour therapy sessions lasting approximately ...
Homework assignments pertaining to the treatment of obsessive-compulsive disorder typically differ depending on the stage of the therapy. In the early stages of therapy, practitioners assigning homework will often invite clients to self-monitor their experience of compulsions, rituals, or responses (Franklin, Huppert, & Roth Ledley, 2005).
5. Engage in self-care. Finding ways to manage your anxiety on a daily basis can also be extremely helpful. By taking the time to explore your own interests and focusing on your own well-being ...
Exposure Hierarchy. Create a list of anxiety-producing situations, beginning with the most distressing, and ending with the least distressing. Rank how distressing each item is on a scale of 1 to 10. Anxiety, Obsession, or Compulsion Trigger. Distress Level (1 - 10)
13. Don't wait for the "perfect moment" to start your therapy homework assignments. Procrastination is a feature of many people's OCD, so start your therapy homework assignments the day you get them. The perfect moment is whenever you begin doing them. 14. Don't be side-tracked by perfectionism. Perfectionism can be another feature of ...
Treatments for OCD. Cognitive-behavioral therapy is a treatment for OCD that uses two scientifically based techniques to change a person's behavior and thoughts: exposure and response prevention (ERP) and cognitive therapy. CBT is conducted by a cognitive-behavioral therapist who has special training in treating OCD.
International OCD Foundation PO Box 961029, Boston, MA 02196 (617) 973-5801 | EIN: 22-2894564
Diagnostic challenges. It's sometimes hard to diagnose OCD because symptoms can be like those of obsessive-compulsive personality disorder, anxiety disorders, depression, schizophrenia or other mental health disorders. And it's possible to have OCD and another mental health disorder. Work with your doctor so that you can get the right diagnosis and treatment.
Cognitive-Behavioral Therapy Worksheets (PDFs) To Print and Use. If you're a therapist looking for ways to guide your client through treatment or a hands-on person who loves to learn by doing, there are many cognitive-behavioral therapy worksheets that can help. 1. Coping styles worksheet.
Homework compliance is associated with short-term and long-term improvement of many disorders and unhealthy behaviors, including anxiety, depression, pathological behaviors, smoking, and drug dependence (Tang & Kreindler, 2017). Greater homework adherence increases the likelihood of beneficial therapy outcomes (Mausbach et al., 2010).
xii THE COMPLETE ANXIETY TREATMENT AND HOMEWORK PLANNER Neurologically Impaired 91 Michele J. Rusin and Arthur E. Jongsma, Jr. Conjoint Treatment of Anxiety 99 K. Daniel O'Leary, Richard E. Heyman, and Arthur E. Jongsma, Jr. Group Treatment of Anxiety 107 Kim Paleg and Arthur E. Jongsma, Jr. ...
3 Steps for Coping With Relationship OCD. Generally, ERP treatment will proceed in an orderly sequence of stages. Treatment will usually begin with a thorough assessment of symptoms. The therapist ...
Behavior therapy for OCD involves exposure and response prevention (E/RP). ... Homework is necessary because the situations or objects that trigger OCD are unique to the individual's environment and often cannot be reproduced in the therapist's office. In intensive CBT, the therapist may come to the patient's home or workplace to conduct ...
Cognitive behavioral therapy (CBT) is known to be a highly effective approach to mental health treatment. One factor underlying its success is the homework component of treatment. It's certainly ...
Treatment and managing. Medication, therapy, and self-management may reduce OCD symptoms. Antidepressant treatment with cognitive behavioral therapy and a type of therapy called exposure and ...
Topics include relaxation, anxiety education, the cycle of anxiety, fight-or-flight, and more. Navigation. Open sidebar. Menu. Worksheets Interactives Videos Articles. Client Education Professional Guides ... These tools are intended to supplement treatment, and are not a replacement for counseling, therapy, or other treatment by appropriately ...
Use this quiz to help determine if you might need to consult a mental health professional for diagnosis and treatment of Obsessive-Compulsive Disorder. Updated Jan 21, 2022.
CBT Worksheets for Anxiety. Cognitive-Behavioral Therapy (CBT) treats anxiety by restructuring the client's thinking, with the therapist exploring maladaptive expectations and worries related to upcoming events (Dobson & Dozois, 2021).. 1. Anxiety Record. Reflecting on and sharing what makes us anxious can leave us feeling vulnerable, but it is essential.
Free worksheets, treatment guides, and videos for mental health professionals. Topics include CBT, anger management, self-esteem, relaxation, and more. Navigation. Open sidebar. Menu. ... Coping Skills: Anxiety. Become a professional member of Therapist Aid. Customizable Worksheets. Interactive Therapy Tools. No More Ads.