Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List

Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Mental health and the pandemic: What U.S. surveys have found
The coronavirus pandemic has been associated with worsening mental health among people in the United States and around the world . In the U.S, the COVID-19 outbreak in early 2020 caused widespread lockdowns and disruptions in daily life while triggering a short but severe economic recession that resulted in widespread unemployment. Three years later, Americans have largely returned to normal activities, but challenges with mental health remain.
Here’s a look at what surveys by Pew Research Center and other organizations have found about Americans’ mental health during the pandemic. These findings reflect a snapshot in time, and it’s possible that attitudes and experiences may have changed since these surveys were fielded. It’s also important to note that concerns about mental health were common in the U.S. long before the arrival of COVID-19 .
Three years into the COVID-19 outbreak in the United States , Pew Research Center published this collection of survey findings about Americans’ challenges with mental health during the pandemic. All findings are previously published. Methodological information about each survey cited here, including the sample sizes and field dates, can be found by following the links in the text.
The research behind the first item in this analysis, examining Americans’ experiences with psychological distress, benefited from the advice and counsel of the COVID-19 and mental health measurement group at Johns Hopkins Bloomberg School of Public Health.
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022.
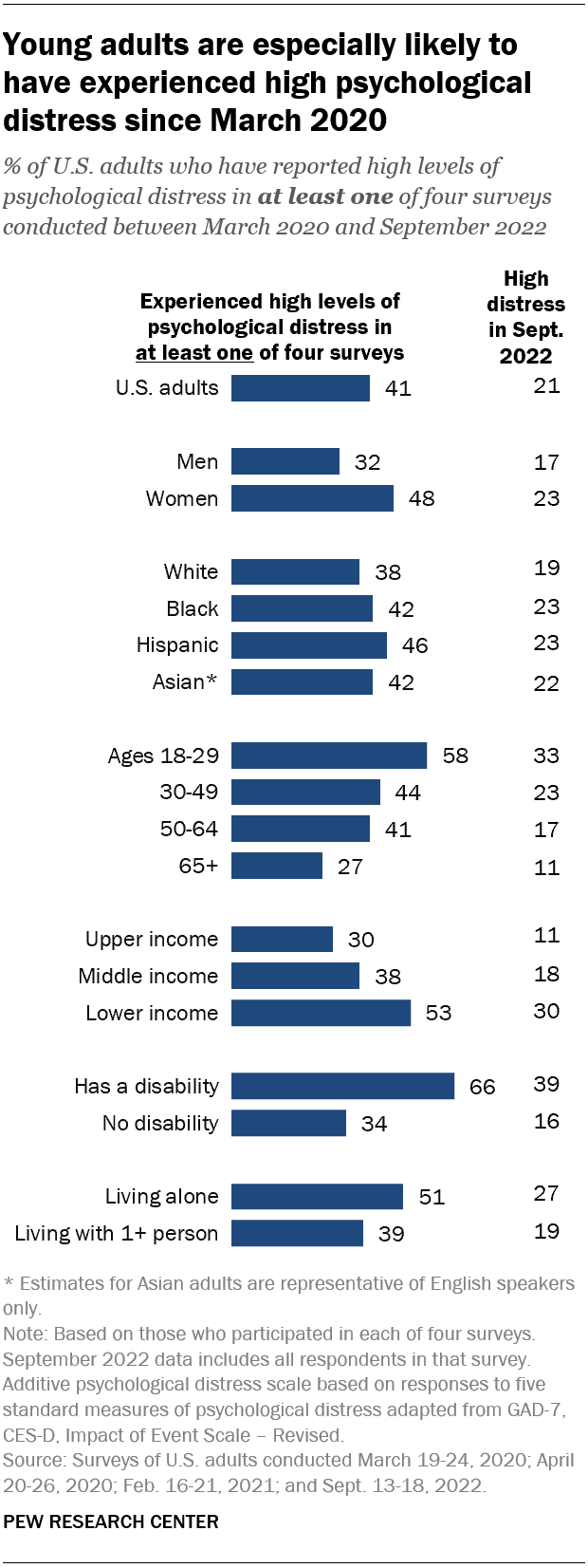
Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began: 58% of Americans ages 18 to 29 fall into this category, based on their answers in at least one of these four surveys.
Women are much more likely than men to have experienced high psychological distress (48% vs. 32%), as are people in lower-income households (53%) when compared with those in middle-income (38%) or upper-income (30%) households.
In addition, roughly two-thirds (66%) of adults who have a disability or health condition that prevents them from participating fully in work, school, housework or other activities have experienced a high level of distress during the pandemic.
The Center measured Americans’ psychological distress by asking them a series of five questions on subjects including loneliness, anxiety and trouble sleeping in the past week. The questions are not a clinical measure, nor a diagnostic tool. Instead, they describe people’s emotional experiences during the week before being surveyed.
While these questions did not ask specifically about the pandemic, a sixth question did, inquiring whether respondents had “had physical reactions, such as sweating, trouble breathing, nausea, or a pounding heart” when thinking about their experience with the coronavirus outbreak. In September 2022, the most recent time this question was asked, 14% of Americans said they’d experienced this at least some or a little of the time in the past seven days.
More than a third of high school students have reported mental health challenges during the pandemic. In a survey conducted by the Centers for Disease Control and Prevention from January to June 2021, 37% of students at public and private high schools said their mental health was not good most or all of the time during the pandemic. That included roughly half of girls (49%) and about a quarter of boys (24%).
In the same survey, an even larger share of high school students (44%) said that at some point during the previous 12 months, they had felt sad or hopeless almost every day for two or more weeks in a row – to the point where they had stopped doing some usual activities. Roughly six-in-ten high school girls (57%) said this, as did 31% of boys.
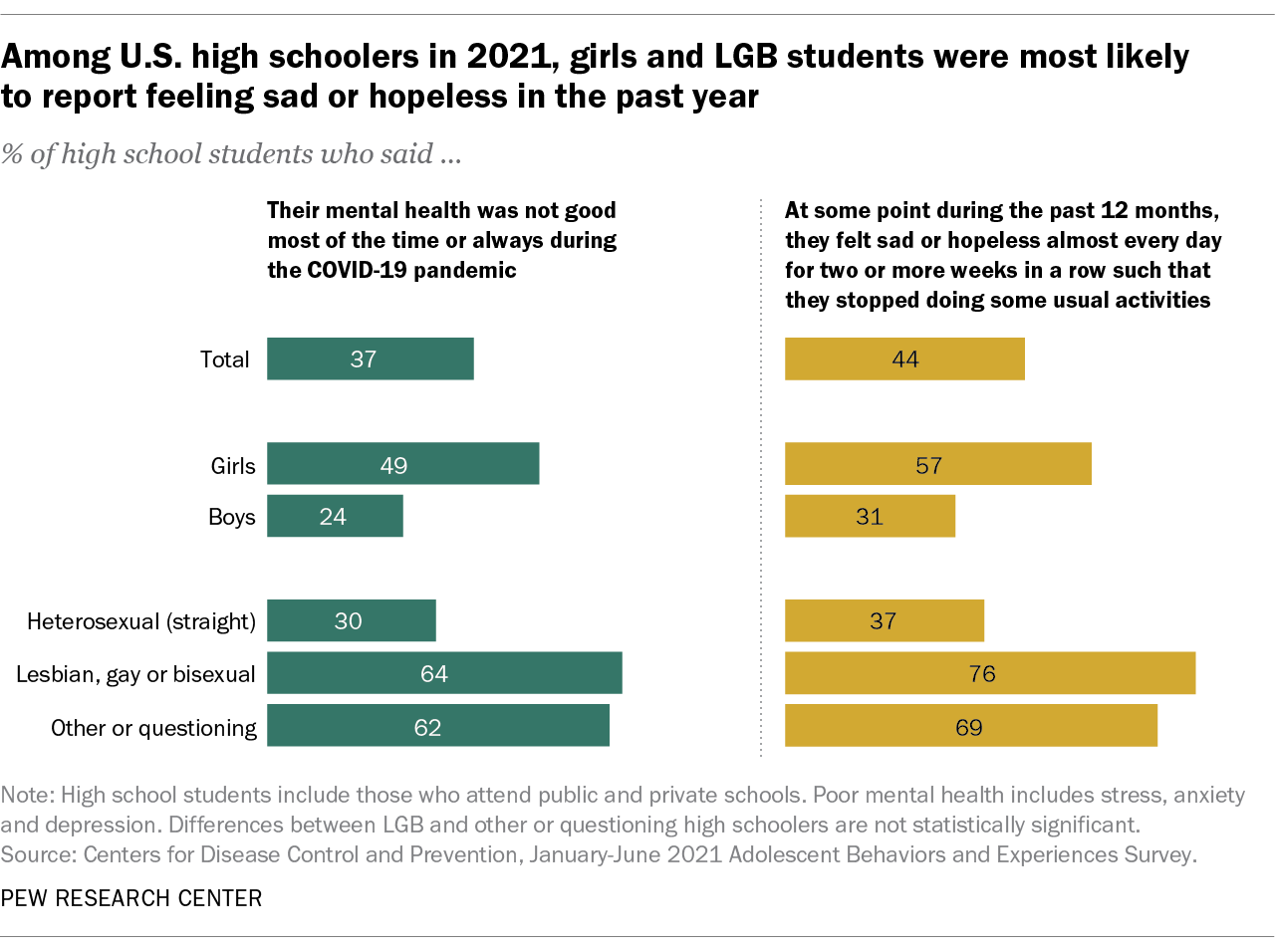
On both questions, high school students who identify as lesbian, gay, bisexual, other or questioning were far more likely than heterosexual students to report negative experiences related to their mental health.
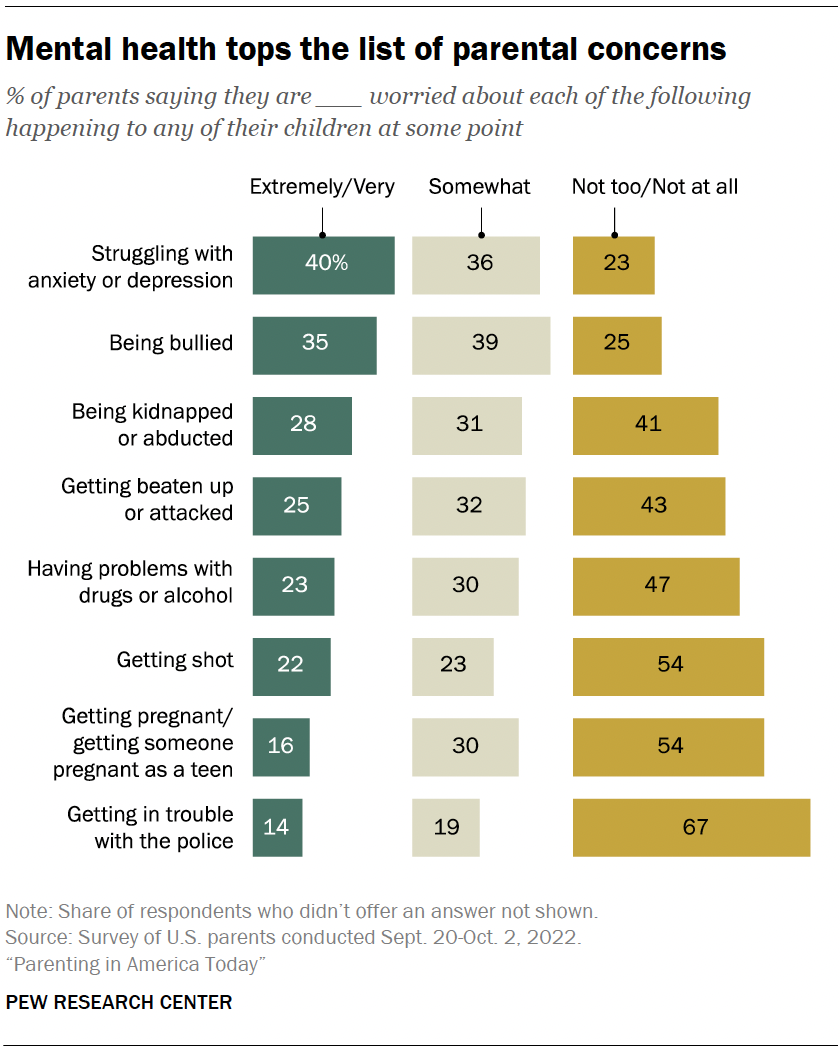
Mental health tops the list of worries that U.S. parents express about their kids’ well-being, according to a fall 2022 Pew Research Center survey of parents with children younger than 18. In that survey, four-in-ten U.S. parents said they’re extremely or very worried about their children struggling with anxiety or depression. That was greater than the share of parents who expressed high levels of concern over seven other dangers asked about.
While the fall 2022 survey was fielded amid the coronavirus outbreak, it did not ask about parental worries in the specific context of the pandemic. It’s also important to note that parental concerns about their kids struggling with anxiety and depression were common long before the pandemic, too . (Due to changes in question wording, the results from the fall 2022 survey of parents are not directly comparable with those from an earlier Center survey of parents, conducted in 2015.)
Among parents of teenagers, roughly three-in-ten (28%) are extremely or very worried that their teen’s use of social media could lead to problems with anxiety or depression, according to a spring 2022 survey of parents with children ages 13 to 17 . Parents of teen girls were more likely than parents of teen boys to be extremely or very worried on this front (32% vs. 24%). And Hispanic parents (37%) were more likely than those who are Black or White (26% each) to express a great deal of concern about this. (There were not enough Asian American parents in the sample to analyze separately. This survey also did not ask about parental concerns specifically in the context of the pandemic.)
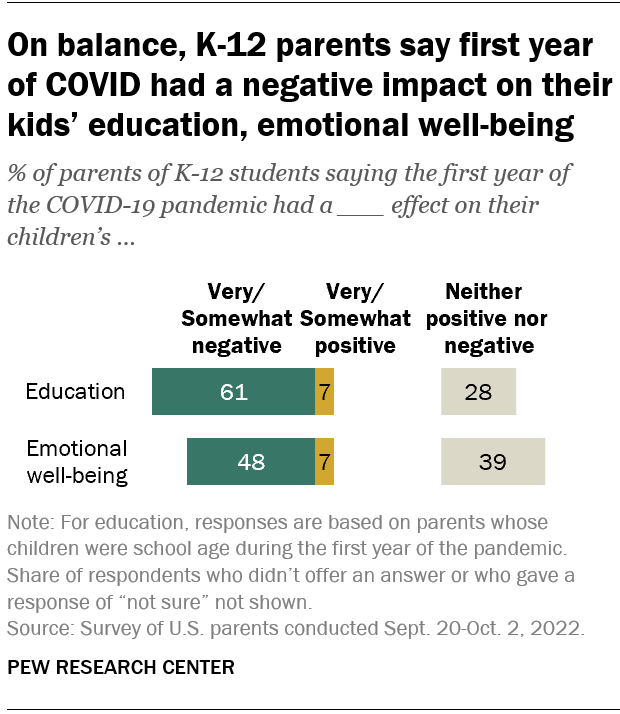
Looking back, many K-12 parents say the first year of the coronavirus pandemic had a negative effect on their children’s emotional health. In a fall 2022 survey of parents with K-12 children , 48% said the first year of the pandemic had a very or somewhat negative impact on their children’s emotional well-being, while 39% said it had neither a positive nor negative effect. A small share of parents (7%) said the first year of the pandemic had a very or somewhat positive effect in this regard.
White parents and those from upper-income households were especially likely to say the first year of the pandemic had a negative emotional impact on their K-12 children.
While around half of K-12 parents said the first year of the pandemic had a negative emotional impact on their kids, a larger share (61%) said it had a negative effect on their children’s education.
- Coronavirus (COVID-19)
- Happiness & Life Satisfaction
- Medicine & Health
- Teens & Youth

John Gramlich is an associate director at Pew Research Center .
How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Online religious services appeal to many americans, but going in person remains more popular, about a third of u.s. workers who can work from home now do so all the time, how the pandemic has affected attendance at u.s. religious services, economy remains the public’s top policy priority; covid-19 concerns decline again, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy

Latest Issue
Psychiatry’s new frontiers
Hope amid crisis
Recent Issues
- AI explodes Taking the pulse of artificial intelligence in medicine
- Health on a planet in crisis
- Real-world health How social factors make or break us
- Molecules of life Understanding the world within us
- The most mysterious organ Unlocking the secrets of the brain
- All Articles
- The spice sellers’ secret
- ‘And yet, you try’
- Making sense of smell
- Before I go
- My favorite molecule
- View all Editors’ Picks
- Diversity, Equity & Inclusion
- Infectious Diseases
- View All Articles
Reasons for hope
Solutions for the mental health crisis emerge through innovative research, diagnostics and treatments
By Nina Bai
Illustration by Jules Julien
Photography by Leslie Williamson

It’s the spring of hope for mental health, astir with novel discoveries, life-changing therapies and more openness than ever before — yet, for many, it feels like the winter of despair. The pandemic years, that crucible of stress, isolation and uncertainty, fueled and exposed mental health problems. In 2022, nearly 1 in 4 American adults (about 59 million people) said they experienced a mental illness in the previous year, but only half of those afflicted reported receiving any mental health treatment.
Among children and adolescents, the prevalence of mental illness, which had been steadily creeping upward, jumped during the pandemic, according to the U.S. Substance Abuse and Mental Health Services Administration. In 2019, 15.7% of American adolescents aged 12-17 reported experiencing a major depressive episode in the past year. In 2022, that number was 19.5%. That same year, 13.4% of adolescents — just over 1 in 8 — seriously thought about killing themselves.
And even as the pandemic has stoked demand for mental health care, it also has worn down the mental health workforce, already short-handed, with early retirements and widespread burnout. Access to affordable, effective interventions remains a daunting barrier. People face long waiting lists and lack of insurance coverage. Many treatable conditions remain undiagnosed because people lack a way to obtain assessments.
Yet, below this perfect storm of mental health crisis, there is a strong undercurrent of hope that begins in the lab. Research is leading the way toward treatments that are more effective, more personalized and more accessible.
“The manner in which we know the brain now, compared with what we knew in previous decades, is incredibly different,” said Victor Carrión , MD, the John A. Turner, MD, Endowed Professor for Child and Adolescent Psychiatry and vice chair of the department of psychiatry and behavioral sciences.

Direct impact on patients
New imaging technologies allow researchers to see the neural circuitry that goes awry in neuropsychiatric disorders, lab-grown clumps of brain tissue — known as organoids — can simulate the impact of genetics in autism, and artificial intelligence can surmise signals that predict the onset of depression and anxiety.
Moreover, these discoveries, rather than moving slowly through specialist silos, can now rapidly inform new treatments. “Collaboration is vital for translation, and our departmental awards and programs promote and emphasize synergy between research and clinical practice,” said Laura Roberts , MD, the Katharine Dexter McCormick and Stanley McCormick Memorial Professor and chair of the department of psychiatry and behavioral sciences.
“Our bench scientists doing tremendous research also work alongside our clinicians to make sure that new knowledge translates to the clinical setting and has a direct impact on patient care,” she said.
Researchers developing transcranial magnetic stimulation, for example, work with clinicians who treat patients with severe depression to design clinical trials, and their techniques are informed by teams inventing new ways to measure the flow of brain signals and those building virtual reality models of the brain.
A clearer understanding of the biology of mental health disorders not only leads to breakthrough treatments — but just as powerfully, helps dissipate stigma.
“There’s been a large shift in stigma in the past 25 years,” said Heather Gotham , PhD, clinical professor of psychiatry and behavioral sciences, who leads the coordination of a nationwide network of centers dedicated to implementing evidence-based mental health care.
The Mental Health Technology Transfer Center Network, funded by the Substance Abuse and Mental Health Services Administration, offers training in preventing school violence, substance use in the workplace, adolescent depression and more, and it offers support for mental health providers seeing refugees and asylum seekers.
“Collaboration is vital for translation, and our departmental awards and programs promote and emphasize synergy between research and clinical practice.” Laura Roberts, the Katharine Dexter McCormick and Stanley McCormick Memorial Professor and chair of the department of psychiatry and behavioral sciences
“One thing that’s made a difference is the greater understanding that mental health disorders and substance use disorders are chronic, relapsing disorders of the body, just like diabetes and heart disease,” Gotham said.
With this new awareness, more people want to be mental health literate. In the past few years, Gotham has seen a surge of interest, from a broader community, in the network’s online courses — from teachers, for example, who want to be more responsive to the needs of students and reduce stigma in the classroom.
Less stigma also means more money for research and mental health services. Funding for mental health has become a rare bipartisan issue. In 2022, Congress passed the Bipartisan Safer Communities Act, which has provided $245 million to fund mental health services like training for school personnel, first responders and law enforcement and expanding the 988 suicide and crisis lifeline.
Stanford Medicine researchers know that to make the most impact with their discoveries they must reach those who need help the most — through online symptom screenings, virtual therapy, group therapy, inclusive clinical trials and community interventions.
They are training mental health professionals locally and globally in new evidence-based techniques. Providers in more than 38 countries, for example, have been trained in cue-centered therapy, a 15-week treatment program developed at Stanford Medicine to help children and teens recover from chronic trauma. Recently, pro bono training in cue-centered therapy was provided to clinicians in Ukraine.
What gives Roberts hope is that a more open conversation on mental health is drawing together experts from different fields with a shared purpose. “It used to be that clinicians would stay in their clinical practice and refer to journals for new research, and researchers would stay in the lab and never see a patient — and we don’t have that now,” she said. “I see more openness and more flexibility from the current generation of researchers and clinicians.”
Read on in this issue of Stanford Medicine to learn about some of the ways Stanford Medicine researchers and clinicians are advancing the understanding of mental health and sharing that knowledge.
Nina Bai is a science writer in the Stanford Medicine Office of Communications.
Email the author
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 07 August 2023
Youth mental health crisis management
Nature Mental Health volume 1 , pages 525–526 ( 2023 ) Cite this article
2069 Accesses
10 Altmetric
Metrics details
Adolescence and young adulthood are decisive times for neurobiological, cognitive and emotional development, all of which converge on mental health. Research into the identification of risks for developing mental health disorders and early intervention in young people are crucial for curtailing the youth mental health crisis.
Adolescence and young adulthood make up a singular time in an individual’s life, in terms of both the amount of change that occurs and the personal evolution prompted by learning about oneself and our relationships with others and the world around us. It can also be amorphous. There is no definite age boundary on adolescence, although it is anchored to the onset of puberty. But by most definitions, including that of the World Health Organization, the boundaries are between ages 10 and 19. The period after, or ‘young adulthood’, generally covers ages 19–25.

Modern conceptualizations of adolescence and young adulthood go beyond age ranges and include well-developed theories that describe the numerous changes that individuals undergo during this period, including physical and neurobiological maturation, psychological and cognitive development, and heightened emotional lability. Perhaps not as simple as the picturesque “sturm und drang” (storm and stress) model put forth by G. Stanley Hall, the twentieth century American psychologist who is credited with establishing the study of the adolescent developmental period, but remnants of this description persist.
Across many fields that study mental health in adolescence and young adulthood, there is an acknowledgment that this time in an individual’s life is marked by the complex interplay between new experiences and environments and one’s emotional and cognitive responses. The experience and expression of emotions that arise for young people can be overwhelming, especially in light of newly developing regulatory mechanisms. And although heightened emotionality can be part of normative or typical development, adolescence, in particular, is often the time when mental health difficulties emerge. In addition to depression and anxiety, other psychiatric illnesses commonly present during adolescence, including obsessive-compulsive disorder, schizophrenia, eating disorders and substance-use disorders.
At the same time that an awareness has grown among healthcare providers, parents, educators and young people themselves, plus decades of adolescent and young adult psychopathology research, there is an alarming global trend of increasingly adverse youth mental health. Recent estimates 1 indicate that 25% of people under age 18 have experienced increased symptoms of depression, which is double the proportion from before the COVID-19 pandemic. Suicidality, including ideation and attempts, has risen in recent years, and suicide is the second leading cause of death among people aged 15–19 globally.
The rapid rise in negative mental health outcomes in young people has prompted health and government policymakers to refer to the present situation as a youth mental health “crisis”. In 2021, the US surgeon general added youth mental health to one of its current priorities and released the ‘ Protecting youth mental health ’ report 2 , detailing a multisectoral advisement on mitigating harms from the pandemic, social media and stigma. This year, the European Commission published its public health plan ‘ A comprehensive approach to mental health ’ 3 , which underscores more consideration of social determinants of health that affect young people, such as nutrition and access to alcohol and tobacco, as part of its focus on prevention of mental health disorders. Even with considerable focus on the potential role of the pandemic as a magnifier of mental health inequities and disruption and isolation for young people, there is concern that many negative changes have been in play for at least a decade, according to US Centers for Disease Control and Prevention data from 2011–2021 showing that young female, LGBT+ and people of color have experienced increased rates of violence, suicidality and substance use over time 4 . The pandemic has forced a reckoning on a global scale that youth mental health is in jeopardy, but recognizing the warning signs can be complex and challenging. Given the impact of youth mental health on influencing the trajectory of mental health and wellbeing across the lifespan, it is essential that we improve how mental health problems are identified for prevention, as well as how to implement interventions earlier.
In this month’s issue of Nature Mental Health , we include an assortment of original primary research and commentary that highlight important findings and provide advances in understanding the course of youth mental health disorders, from detection to intervention.
In the ‘front half’ of the journal, senior editor Ana Donnelly has a Q&A with Christian Kieling, an associate professor of child and adolescent psychiatry in Brazil, about his work on the Identifying Depression Early in Adolescence (IDEA) project, using a range of methods, including psychoneuroimmunology, imaging and qualitative research, to stratify risk for developing depression in adolescence. In a Perspective piece, Anne Duffy introduces us to children of parents with severe mental illness, who are themselves at increased risk of developing a mental illness, but who may benefit from developmentally sensitive interventions. Associate Editor Natalia Gass reports in a Research Highlight on new work from Yun-Jun Sun, Barbara Sahakian et al., finding that reading for pleasure in childhood was associated with greater academic achievement and cognitive performance and negatively correlated with psychopathology scores and mental health problems, concluding that reading for pleasure could be a useful mental health intervention owing to its scalability and relatively low cost.
Also in this issue, we publish original research on the patterns of violence and mental health outcomes in young adults both before and during the COVID-19 pandemic. In an Article , Wisteria Deng and coauthors sample more than 200,000 college students in the USA, and found greater levels of depressive and anxiety symptoms and increased numbers of sexual violence and assaults experienced by people from gender and sexual minorities during the pandemic. These data reinforce the disproportionate and heightened mental health and sexual violence risks for young people from gender and sexual minorities and the need to increase on-campus safety and crisis intervention. Two other papers out this month use different techniques to investigate psychiatric biomarkers. Margaret Westwater and colleagues report findings that show that the genetic risk for disordered eating was associated with distinct brain structure differences and symptom profiles in a sample of more than 4,900 adolescents. Using plasma-based proteomics, Katja Kanninen and coauthors present some of the first work in identifying protein alteration biomarkers associated with the risk of developing a mental health disorder.
Much of the work published now may not be immediately actionable in a real-world setting, yet it provides clear directive for where a more solid evidence base is needed — for example, with more representative participants or country settings. It also can be extremely valuable in determining where the thresholds for clinical utility of biomarkers should be placed, such as during routine screening programs or potentially at younger ages. In the face of the youth mental health crisis, concurrently pursuing several lines of inquiry is essential. From neurobiological markers, school-based interventions and social determinants of health to reducing stigma, changing the course of the youth mental health crisis will require all of the tools that we have available.
Racine, N. et al. JAMA Pediatr. 175 , 1142–1150 (2021).
Article PubMed Google Scholar
The US Surgeon General’s Advisory. https://go.nature.com/3OrweUh (2021).
European Commission. https://go.nature.com/43HTMsv (2023).
CDC. https://go.nature.com/43D1Xq0 (2021).
Download references
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Youth mental health crisis management. Nat. Mental Health 1 , 525–526 (2023). https://doi.org/10.1038/s44220-023-00112-1
Download citation
Published : 07 August 2023
Issue Date : August 2023
DOI : https://doi.org/10.1038/s44220-023-00112-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Share full article
Advertisement
The Morning
A fresh approach to a crisis.
A group of researchers posited another explanation for the youth mental health crisis: too much discussion.

By Ellen Barry
She covers mental illness.
For years now, policymakers have sought an explanation for the mental health crisis among young people. Suicide attempts and psychiatric hospitalizations were rising even before the pandemic. Then the rates of anxiety and depression doubled worldwide.
Why is this happening? The social psychologist Jonathan Haidt points to smartphones, and the algorithms that draw kids away from healthy play and into dangerous, addictive thought loops. No, his critics say. The real problem is a grim social landscape of school shootings, poverty and global warming. Or academic pressure. Or insufficient health care.
A group of researchers in Britain now propose another, at least partial, explanation: We talk about mental disorders so much. I cover this notion in a story The Times published today .
This hypothesis is called “prevalence inflation.” It holds that our society has become so saturated with discussion of mental health that young people may interpret mild, transient suffering as symptoms of a medical disorder.
This is a problem, they say, because identifying with a psychiatric diagnosis may not be helpful. Students who self-label as anxious or depressed are more likely than similar students who don’t self-label to view themselves as powerless over the disorder, recent studies have shown. They may respond by avoiding stressful situations like parties or public speaking, which could make their problems worse.
One of the psychologists behind the prevalence inflation theory, Lucy Foulkes of the University of Oxford, traces her skepticism back to 2018, when she began teaching undergraduates. They were “bombarded” with messages warning that they might be in crisis, she said. “It seemed like the more we were trying to raise awareness about it, it wasn’t getting better, and in fact, it only seemed to be getting worse.”
She grew critical of curricula that teach children to recognize and manage their emotions, sometimes referred to as social emotional learning. Schools have introduced an array of programs, teaching children the basics of techniques like mindfulness and cognitive behavioral therapy, which have proved beneficial in adults.
Several recent studies have found lackluster or negative effects for students who received trainings, especially those who started out with more severe symptoms. That evidence has done little to dampen their popularity, Foulkes said.
An urgent need
Many experts in the field of adolescent mental health defend awareness campaigns and school-based trainings. “Especially with teens, we need more universal interventions, not less,” said Zachary Blumkin, a child psychologist at Columbia University Irving Medical Center.
The main reason, they say, is that traditional, one-on-one therapy and psychiatric care is not easily available. Teenagers in crisis can wait months to see a clinician. They often land in emergency rooms as a last resort.
For that reason, the field has gravitated toward preventive models. These teach all students — not just the troubled ones — to manage distressing emotions. A 2023 meta-analysis of 252 such programs concluded that, generally, children benefit from them. There is also promise in a more tailored approach , one that lets schools focus on kids with the most acute needs.
Some experts also disagree that over-diagnosis is a problem.
Andrew Gerber, a child psychiatrist, says we should think of mental illness as a spectrum: Disorders like anxiety or depression occur in a bell curve distribution, so they’re more like hypertension than appendicitis. And like hypertension, he said, they’re worth treating early in their progression, with medication and therapy. “Anyone who tries to define a sharp line between ‘real’ illness and what is not real, no matter where they put the line, is doomed to get it wrong and do damage in the process,” said Gerber, the president and medical director at Silver Hill Hospital in New Canaan, Conn.
Foulkes disagrees. Even when we have good treatments, we’re bad at identifying whose disorder is likely to deteriorate, she said. And some children struggle because something is wrong at home, like domestic abuse or poverty or bullying. Mindfulness trainings are unlikely to help these kids.
“A lot of the time, what’s causing the problem is not something that’s going to improve with medication or therapy,” she said. “You’re running the risk of just telling people they have a problem without helping alleviate it.”
A generation is growing up fluent in the language of mental health, something that will benefit teens who badly need treatment. But others may apply medical diagnoses to the painful, normal adversity of growing up.
The “prevalence inflation” hypothesis asks us to keep an eye on those excesses. People hurt after breakups and struggle to adjust to new schools; negative feelings aren’t always a sign of mental illness. They can even teach us resilience.
Rates of mental health disorders are rising among American adolescents. Read one 13-year-old’s story .
There aren’t always enough resources to support teenagers’ mental health. As schools search for solutions, some student-led clubs step in .
Are smartphones driving teenagers to depression? It’s complicated , writes David Wallace-Wells in Times Opinion.
THE LATEST NEWS
Israel-hamas war.
The Israeli military said it was asking tens of thousands of Gazans sheltering in eastern Rafah to temporarily evacuate to what it described as a humanitarian zone.
Hamas claimed responsibility for a rocket attack that Israeli officials said killed three soldiers and left three more critically wounded.
Israel moved to shut down local operations of Al Jazeera , a Qatar-based news outlet.
Cease-fire talks between Israel and Hamas are at an impasse. The main obstacle is the duration of a pause.
Four children from Gaza arrived in the U.S. to receive urgent medical treatment . They were greeted at Kennedy Airport with toys and balloons.
Campus Protests
U.C.L.A. said that it would resume in-person classes today and that it had created a new campus security office .
New York Magazine and the Columbia student newspaper surveyed the campus about the protests . More than 60 percent of respondents said they had views on the conflict they avoided saying publicly.
More college professors — many of whom came of age during the era of Vietnam War protests — are joining student demonstrations , The Wall Street Journal reports.
More International News
Around Shanghai, women gather in bars and bookstores to debate their place in a country ruled by men.
Panamanians elected José Raúl Mulino, a former public security minister, as their next president .
Paris committed to making the Olympics more accessible for people with disabilities. Advocacy groups are concerned that the city remains unprepared .
In the 19th century, Belgian troops decapitated a Congolese leader and took his skull as a trophy. The leader’s descendants are struggling to have his remains returned .
Kim Godwin, the first Black woman to run a broadcast news division, said she would step down as president of ABC News after a tumultuous tenure.
Sony and the private equity firm Apollo are in talks to acquire Paramount .
Other Big Stories
New York City’s congestion pricing program aims to generate $15 billion for the mass transit system, but lawsuits threaten that windfall .
In Florida, Chinese residents expressed frustration with a new law that prohibits many Chinese citizens from buying homes in the state because of national security concerns.
We should welcome the emergence of this year’s cicadas with wonder, Margaret Renkl writes.
Ross Douthat suggests books and essays that could improve the intellectual diversity of university curricula.
Gail Collins and Bret Stephens discuss campus protests and Donald Trump .
Here are columns by Maureen Dowd on the three faces of Trump and Thomas Friedman on Israel and Saudi Arabia .
MORNING READS
Community: For generations of immigrants, Sunday soccer in a park in Queens is more than a game .
Health: Ultraprocessed foods are linked to poor health. But what are they exactly?
Loneliness: Social connection experts offer advice on cultivating a sense of belonging .
Ask Vanessa: “How do I know if my untucked shirt is too long?”
Kocktails: As nonalcoholic cocktails become a staple on American menus, some children have begun to partake .
Metropolitan Diary: A necklace rescue in Midtown .
Lives Lived: Bernard Hill was a British actor who incarnated humble masculine leadership as Capt. Edward J. Smith in “Titanic” and as Théoden, the king of Rohan, in two “Lord of the Rings” films. He died at 79 .
Formula One: McLaren’s Lando Norris secured his first victory at the Miami Grand Prix .
No punches pulled: At a live Netflix comedy roast, former Patriots players and Kevin Hart among others roasted Tom Brady about his divorce and Deflategate.
N.H.L.: The Dallas Stars eliminated the defending Stanley Cup champion Las Vegas Golden Knights in a thrilling 2-1 Game 7 win .
N.B.A.: Donovan Mitchell’s 24 second-half points led the Cleveland Cavaliers to a comeback win in their own Game 7 against the Orlando Magic.
ARTS AND IDEAS
The artist Frank Stella, who helped usher in the Minimalist movement of the 1960s, died on Saturday at 87. His career began during the Eisenhower era, when artistic tendencies — much like ideas about gender and sexuality — fell into fixed categories: one was either a figurative artist or an abstract one. Things changed, the critic Deborah Solomon writes, but Stella did not. “He never stopped insisting on the inherent superiority of abstract painting,” she adds. Read her full appraisal of Stella .
More on culture
Madonna ended her retrospective Celebration Tour with a free show in Rio de Janeiro, which was attended by an estimated 1.6 million people .
Trying to find your own song of the summer? Vulture has published a bracket to sort through this year’s pop deluge.
The HBO series “The Sympathizer” is a rebuttal to a Hollywood staple. It is its own Vietnam War movie and a detailed work of film criticism , James Poniewozik writes.
Over the weekend, “The Fall Guy,” starring Ryan Gosling, earned only $28.5 million . It is Hollywood’s lowest start to the summer box office season since 1995.
THE MORNING RECOMMENDS …
Make Dolester Miles’s famous coconut pecan cake .
Watch the Met Gala red carpet tonight.
Stargaze with a telescope for beginners .
Clear your phone’s camera roll .
Take our news quiz .
Here is today’s Spelling Bee . Yesterday’s pangram was maypole .
And here are today’s Mini Crossword , Wordle , Sudoku , Connections and Strands .
Thanks for spending part of your morning with The Times. See you tomorrow.
Correction: Yesterday’s newsletter named two different Kentucky Derby winners. The winner was Mystik Dan, not Sierra Leone.
Sign up here to get this newsletter in your inbox . Reach our team at [email protected] .
Ellen Barry is a reporter covering mental health for The Times. More about Ellen Barry
55 research questions about mental health
Last updated
11 March 2024
Reviewed by
Brittany Ferri, PhD, OTR/L
Research in the mental health space helps fill knowledge gaps and create a fuller picture for patients, healthcare professionals, and policymakers. Over time, these efforts result in better quality care and more accessible treatment options for those who need them.
Use this list of mental health research questions to kickstart your next project or assignment and give yourself the best chance of producing successful and fulfilling research.
- Why does mental health research matter?
Mental health research is an essential area of study. It includes any research that focuses on topics related to people’s mental and emotional well-being.
As a complex health topic that, despite the prevalence of mental health conditions, still has an unending number of unanswered questions, the need for thorough research into causes, triggers, and treatment options is clear.
Research into this heavily stigmatized and often misunderstood topic is needed to find better ways to support people struggling with mental health conditions. Understanding what causes them is another crucial area of study, as it enables individuals, companies, and policymakers to make well-informed choices that can help prevent illnesses like anxiety and depression.
- How to choose a strong mental health research topic
As one of the most important parts of beginning a new research project, picking a topic that is intriguing, unique, and in demand is a great way to get the best results from your efforts.
Mental health is a blanket term with many niches and specific areas to explore. But, no matter which direction you choose, follow the tips below to ensure you pick the right topic.
Prioritize your interests and skills
While a big part of research is exploring a new and exciting topic, this exploration is best done within a topic or niche in which you are interested and experienced.
Research is tough, even at the best of times. To combat fatigue and increase your chances of pushing through to the finish line, we recommend choosing a topic that aligns with your personal interests, training, or skill set.
Consider emerging trends
Topical and current research questions are hot commodities because they offer solutions and insights into culturally and socially relevant problems.
Depending on the scope and level of freedom you have with your upcoming research project, choosing a topic that’s trending in your area of study is one way to get support and funding (if you need it).
Not every study can be based on a cutting-edge topic, but this can be a great way to explore a new space and create baseline research data for future studies.

Assess your resources and timeline
Before choosing a super ambitious and exciting research topic, consider your project restrictions.
You’ll need to think about things like your research timeline, access to resources and funding, and expected project scope when deciding how broad your research topic will be. In most cases, it’s better to start small and focus on a specific area of study.
Broad research projects are expensive and labor and resource-intensive. They can take years or even decades to complete. Before biting off more than you can chew, consider your scope and find a research question that fits within it.
Read up on the latest research
Finally, once you have narrowed in on a specific topic, you need to read up on the latest studies and published research. A thorough research assessment is a great way to gain some background context on your chosen topic and stops you from repeating a study design. Using the existing work as your guide, you can explore more specific and niche questions to provide highly beneficial answers and insights.
- Trending research questions for post-secondary students
As a post-secondary student, finding interesting research questions that fit within the scope of your classes or resources can be challenging. But, with a little bit of effort and pre-planning, you can find unique mental health research topics that will meet your class or project requirements.
Examples of research topics for post-secondary students include the following:
How does school-related stress impact a person’s mental health?
To what extent does burnout impact mental health in medical students?
How does chronic school stress impact a student’s physical health?
How does exam season affect the severity of mental health symptoms?
Is mental health counseling effective for students in an acute mental crisis?
- Research questions about anxiety and depression
Anxiety and depression are two of the most commonly spoken about mental health conditions. You might assume that research about these conditions has already been exhausted or that it’s no longer in demand. That’s not the case at all.
According to a 2022 survey by Centers for Disease Control and Prevention (CDC), 12.5% of American adults struggle with regular feelings of worry, nervousness, and anxiety, and 5% struggle with regular feelings of depression. These percentages amount to millions of lives affected, meaning new research into these conditions is essential.
If either of these topics interests you, here are a few trending research questions you could consider:
Does gender play a role in the early diagnosis of anxiety?
How does untreated anxiety impact quality of life?
What are the most common symptoms of anxiety in working professionals aged 20–29?
To what extent do treatment delays impact quality of life in patients with undiagnosed anxiety?
To what extent does stigma affect the quality of care received by people with anxiety?
Here are some examples of research questions about depression:
Does diet play a role in the severity of depression symptoms?
Can people have a genetic predisposition to developing depression?
How common is depression in work-from-home employees?
Does mood journaling help manage depression symptoms?
What role does exercise play in the management of depression symptoms?
- Research questions about personality disorders
Personality disorders are complex mental health conditions tied to a person’s behaviors, sense of self, and how they interact with the world around them. Without a diagnosis and treatment, people with personality disorders are more likely to develop negative coping strategies during periods of stress and adversity, which can impact their quality of life and relationships.
There’s no shortage of specific research questions in this category. Here are some examples of research questions about personality disorders that you could explore:
What environments are more likely to trigger the development of a personality disorder?
What barriers impact access to care for people with personality disorders?
To what extent does undiagnosed borderline personality disorder impact a person’s ability to build relationships?
How does group therapy impact symptom severity in people with schizotypal personality disorder?
What is the treatment compliance rate of people with paranoid personality disorder?
- Research questions about substance use disorders
“Substance use disorders” is a blanket term for treatable behaviors and patterns within a person’s brain that lead them to become dependent on illicit drugs, alcohol, or prescription medications. It’s one of the most stigmatized mental health categories.
The severity of a person’s symptoms and how they impact their ability to participate in their regular daily life can vary significantly from person to person. But, even in less severe cases, people with a substance use disorder display some level of loss of control due to their need to use the substance they are dependent on.
This is an ever-evolving topic where research is in hot demand. Here are some example research questions:
To what extent do meditation practices help with craving management?
How effective are detox centers in treating acute substance use disorder?
Are there genetic factors that increase a person’s chances of developing a substance use disorder?
How prevalent are substance use disorders in immigrant populations?
To what extent do prescription medications play a role in developing substance use disorders?
- Research questions about mental health treatments
Treatments for mental health, pharmaceutical therapies in particular, are a common topic for research and exploration in this space.
Besides the clinical trials required for a drug to receive FDA approval, studies into the efficacy, risks, and patient experiences are essential to better understand mental health therapies.
These types of studies can easily become large in scope, but it’s possible to conduct small cohort research on mental health therapies that can provide helpful insights into the actual experiences of the people receiving these treatments.
Here are some questions you might consider:
What are the long-term effects of electroconvulsive therapy (ECT) for patients with severe depression?
How common is insomnia as a side effect of oral mental health medications?
What are the most common causes of non-compliance for mental health treatments?
How long does it take for patients to report noticeable changes in symptom severity after starting injectable mental health medications?
What issues are most common when weaning a patient off of an anxiety medication?
- Controversial mental health research questions
If you’re interested in exploring more cutting-edge research topics, you might consider one that’s “controversial.”
Depending on your own personal values, you might not think many of these topics are controversial. In the context of the research environment, this depends on the perspectives of your project lead and the desires of your sponsors. These topics may not align with the preferred subject matter.
That being said, that doesn’t make them any less worth exploring. In many cases, it makes them more worthwhile, as they encourage people to ask questions and think critically.
Here are just a few examples of “controversial” mental health research questions:
To what extent do financial crises impact mental health in young adults?
How have climate concerns impacted anxiety levels in young adults?
To what extent do psychotropic drugs help patients struggling with anxiety and depression?
To what extent does political reform impact the mental health of LGBTQ+ people?
What mental health supports should be available for the families of people who opt for medically assisted dying?
- Research questions about socioeconomic factors & mental health
Socioeconomic factors—like where a person grew up, their annual income, the communities they are exposed to, and the amount, type, and quality of mental health resources they have access to—significantly impact overall health.
This is a complex and multifaceted issue. Choosing a research question that addresses these topics can help researchers, experts, and policymakers provide more equitable and accessible care over time.
Examples of questions that tackle socioeconomic factors and mental health include the following:
How does sliding scale pricing for therapy increase retention rates?
What is the average cost to access acute mental health crisis care in [a specific region]?
To what extent does a person’s environment impact their risk of developing a mental health condition?
How does mental health stigma impact early detection of mental health conditions?
To what extent does discrimination affect the mental health of LGBTQ+ people?
- Research questions about the benefits of therapy
Therapy, whether that’s in groups or one-to-one sessions, is one of the most commonly utilized resources for managing mental health conditions. It can help support long-term healing and the development of coping mechanisms.
Yet, despite its popularity, more research is needed to properly understand its benefits and limitations.
Here are some therapy-based questions you could consider to inspire your own research:
In what instances does group therapy benefit people more than solo sessions?
How effective is cognitive behavioral therapy for patients with severe anxiety?
After how many therapy sessions do people report feeling a better sense of self?
Does including meditation reminders during therapy improve patient outcomes?
To what extent has virtual therapy improved access to mental health resources in rural areas?
- Research questions about mental health trends in teens
Adolescents are a particularly interesting group for mental health research due to the prevalence of early-onset mental health symptoms in this age group.
As a time of self-discovery and change, puberty brings plenty of stress, anxiety, and hardships, all of which can contribute to worsening mental health symptoms.
If you’re looking to learn more about how to support this age group with mental health, here are some examples of questions you could explore:
Does parenting style impact anxiety rates in teens?
How early should teenagers receive mental health treatment?
To what extent does cyberbullying impact adolescent mental health?
What are the most common harmful coping mechanisms explored by teens?
How have smartphones affected teenagers’ self-worth and sense of self?
- Research questions about social media and mental health
Social media platforms like TikTok, Instagram, YouTube, Facebook, and X (formerly Twitter) have significantly impacted day-to-day communication. However, despite their numerous benefits and uses, they have also become a significant source of stress, anxiety, and self-worth issues for those who use them.
These platforms have been around for a while now, but research on their impact is still in its infancy. Are you interested in building knowledge about this ever-changing topic? Here are some examples of social media research questions you could consider:
To what extent does TikTok’s mental health content impact people’s perception of their health?
How much non-professional mental health content is created on social media platforms?
How has social media content increased the likelihood of a teen self-identifying themselves with ADHD or autism?
To what extent do social media photoshopped images impact body image and self-worth?
Has social media access increased feelings of anxiety and dread in young adults?
- Mental health research is incredibly important
As you have seen, there are so many unique mental health research questions worth exploring. Which options are piquing your interest?
Whether you are a university student considering your next paper topic or a professional looking to explore a new area of study, mental health is an exciting and ever-changing area of research to get involved with.
Your research will be valuable, no matter how big or small. As a niche area of healthcare still shrouded in stigma, any insights you gain into new ways to support, treat, or identify mental health triggers and trends are a net positive for millions of people worldwide.
Editor’s picks
Last updated: 11 January 2024
Last updated: 15 January 2024
Last updated: 25 November 2023
Last updated: 12 May 2023
Last updated: 30 April 2024
Last updated: 18 May 2023
Last updated: 10 April 2023
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next.

Users report unexpectedly high data usage, especially during streaming sessions.

Users find it hard to navigate from the home page to relevant playlists in the app.

It would be great to have a sleep timer feature, especially for bedtime listening.

I need better filters to find the songs or artists I’m looking for.
Log in or sign up
Get started for free
A mental health crisis has been brewing in the regions for years — and 'it's costing some people everything'
WARNING: This article contains references to mental health and suicide.
Despite living with major depression, experiencing regular panic attacks and having a history of suicide attempts, it still took Sam Webb 10 months to see a psychiatrist in a major regional town.
It was 2020 and Mr Webb had just moved from Sydney back to his home town of Bathurst, a three-hour drive from the New South Wales state capital.
The 58-year-old was shocked to find how long it took to see any sort of mental health professional.
It was six weeks to see a new GP, a crucial first step to be referred to other services.
A psychologist appointment was a three-month wait, while a psychiatrist was nine months.
Mr Webb felt left on his own.
"At the absolute worst, I was preparing for suicide and then a fully-fledged suicide attempt," he said.
Equally alarming was his history of dissociative episodes, when he could go for hours without remembering what he had done.
In one episode, Mr Webb said he regained full awareness about half an hour after missing his usual train station.
"I remember getting up in the morning, but I don't remember leaving home. I don't remember walking to the train," he said.
In another episode, he was giving a presentation to the board of the investment bank where he worked, when he unexpectedly walked out halfway through.
He had no idea what had happened until a colleague asked him about it.
"You function quite well, apparently. But it's like breathing. It's like blinking. You're on automatic pilot and you're not aware of it," he said.
None of this made a difference to the speed at which Mr Webb was seen by a mental health professional.
He said the difference in services from Sydney to Bathurst was stark.
"It is night and day … You have choices in Sydney," he said.
With the fatal stabbings in Bondi Junction sparking debate about gaps in the mental health system, Mr Webb said he was worried more people were being left behind.
"It's bloody dangerous," he said.
"It's costing the community and it's costing individuals. And it's costing some individuals everything."
Why aren't mental health professionals moving to the country?
Seven million Australians live outside the major cities, but regional parts of the country have long struggled to attract qualified health workers.
The mental health field has been particularly difficult to staff.
Data released in 2020 by the Australian Institute of Health and Welfare showed the number of Medicare-subsidised mental health services decreased dramatically as the distance from capital cities increased.
The rate of suicide, though, was the opposite.
The most remote parts of Australia had a disproportionately high rate, while major cities had the lowest.
The high suicide rate outside the capital cities (60 per cent higher than metropolitan areas) can be partly attributed to the declining availability of mental health services in the regions.
Rates of risky drinking, fewer employment opportunities and greater exposure to natural disasters are also considered factors, according to the National Rural Health Alliance.
The Australian Association of Psychologists has described the disparity between metropolitan and regional areas as "beyond comprehension".
The Association is calling for an urgent increase in the Medicare rebate for generalist psychologists to $150 per session.
"Most psychologists would be able to bulk bill and that would make it so much more affordable and accessible for the Australian population," president Sahra O'Doherty said.
The town where you can’t give away a psychology practice
On the mid-north coast of NSW, the town of Kempsey lies sandwiched between major holiday destinations.
Yet Kempsey is one of the poorest regions of the state, and the local health service says the rates of attention-deficit/hyperactivity disorder (ADHD) are more than two and a half times the national average.
The rates of psychosis are almost triple.
Allan Anderson has been working as a private psychologist in Kempsey for 15 years.
He just turned 80 and has been trying to give away his thriving practice for free so he can retire, but no one has been interested.
"It's very difficult for me to walk away because there's a great need here and not many people to fill that need," he said.
"It's very unsafe for the community generally to have people here who need help, who want help, and it's just not available."
Part of the lack of appeal is the money a psychologist can earn in a poorer area.
Mr Anderson said the Medicare rebate he could access for a session was $95 per hour.
"That's not enough for anyone to get by on. My running costs here are about $150 an hour.
"You can't expect people to be attracted to this town and live, and make a living as a psychologist, especially if they bulk bill."
Mr Anderson said many people in Kempsey could "absolutely not" afford to pay a gap fee to make up the difference.
Some of his patients were recently paroled prisoners who needed to see a psychologist as part of their release but couldn't pay him anything in addition to the Medicare rebate.
Mr Anderson estimated he bulk billed about a third of his clients who needed it the most, but that required him to find income elsewhere in his practice to make up for taking a loss.
"The Medicare rebate hasn't changed in 15 years and so all the costs have gone up, rents have gone up for psychologists and other expenses, staffing costs have gone up and so it's worse.
"There are more people requiring mental health to be bulk billed."
What's the fix?
More money is needed, but that won't make the difference alone, according to those in the sector.
Australian Psychological Society president Catriona Davis-McCabe said the cost of professional help was prohibitive for too many people.
"People are having to use a credit card instead of a Medicare card to pay to support their mental health, and it's just not acceptable," she said.
Dr Davis-McCabe called for specific rural Medicare loadings for psychologists working in rural areas, much like GPs can access, as well as incentives to move out of the cities, much like doctors can access.
But even if more funding was made available, she said there were not enough psychologists in Australia, and the federal government urgently needed to create more training spaces for them.
"We could really turn this around very quickly if we got more psychologists on the ground and … into the places where people need them."
Ms O'Doherty said the government should return the number of Medicare-funded psychology sessions per year to 20, as it was increased to during the early COVID era.
In a statement, Health Minister Mark Butler acknowledged there were "structural challenges" impacting the supply and distribution of the mental health workforce outside big cities.
He said new Medicare subsidies for telehealth psychiatry appointments and $109 million to fund postgraduate psychology places were among the actions the government was taking.
Mr Butler said doubling the number of Medicare-subsidised psychologist appointments meant tens of thousands of Australians had missed out on spots due to the increased demand.
The statement did not answer questions on whether he would increase the Medicare subsidy for psychologists or offer regional loadings.
"Mental health reform will not happen overnight," he said.
Sam Webb said he was able to get through his lowest points with what he calls "rolling therapy", riding his motorbike around the rolling countryside that surrounds Bathurst.
After going through a period "as a hermit", he was also able to find some support from friends he had in the area.
He said sometimes he was amazed he was still alive, given the state of his mental health when he was unable to find help.
"It came down to nothing more than good luck."
- X (formerly Twitter)
Related Stories
Chantelle stopped psychologist visits due to cost. she says they've become something only the wealthy can afford.
Training medical students in regional Australia makes them more likely to return, new study finds
Annette recruited two doctors to her rural GP clinics, but then they pulled out overnight
- Mental Health
- Regional Communities
Why am I lonely? Lack of social connections hurts Americans' mental health.
Tens of millions of people don’t have relationships that provide meaning in daily life. no amount of federal money − no number of mental health workers or programs − will solve that problem..
We need a new way to think about mental health − one that recognizes every person’s role in tackling the crisis that surrounds us.
We all know this crisis exists. After the COVID-19 pandemic, record numbers of people have reported mental health challenges. About 20% of U.S. adults − nearly 60 million Americans − have a diagnosable mental illness. Nearly 40% of high school students − and half of high school girls − say their mental health has struggled in recent years. Anxiety, depression and suicide have soared. So has addiction , which about 1 in 5 Americans now struggle with.
Amid this crisis, government at all levels is desperately trying to make a difference, mainly through new programs and funding streams. President Joe Biden’s proposed 2024 budget, for instance, envisions a 44% increase in federal spending on the Substance Abuse and Mental Health Services Administration. In the State of the Union address, he called for funding “ more mental health workers .”
We need more than increased spending to help with the mental health problem
And states like Florida and Virginia are now spending record amounts on mental health services.
Yet more money and more workers aren’t silver bullets. It’s true that America has just one mental health professional for every 350 people who need help , but there’s no credible path to close that gap. Even if we could, more than half of people with mental health challenges still avoid care because of social stigma.
That helps explain why big federal funding increases before the pandemic didn’t make much of a difference − mental health challenges continued to rise.
Clearly, some root cause is going unaddressed.
Hence the need for a new approach. The mental health advocates and substance abuse experts whom my organization has worked with over the past decade show the way. They prove that the mental health crisis isn’t just a clinical crisis. It’s really a crisis of community.
To be sure, clinical settings and clinical tools are essential for many people with mental health disorders. But it’s also true that mental health is ultimately about psychological well-being. Everyone is looking for a life of meaning, and finding that life requires a supportive community.
Americans increasingly feel isolated and lonely
The famous psychologist Abraham Maslow said it better than I can. Based on his experience treating tens of thousands of patients, he realized that mental health challenges ultimately arise when people’s deeper needs aren’t met. Most notably, when people lack relationships, belonging and love, they get lonely, leading to anxiety and depression. Left unchecked, loneliness can ruin someone’s life.
What’s happening in America supports Maslow’s theory. Last year, the U.S. surgeon general called loneliness an “epidemic,” and an American Psychiatric Association poll conducted this January found that a third of of adults say they have experienced feelings of loneliness at least once a week over the past year.
About 30% of millennials have zero best friends , while Generation Z has been called “the loneliest generation.” The situation is so bad that some in Gen Z have posted “friendship applications” on social media .
My generation's isolation is real: Gen Z doesn't care about sports. That's part of a bigger problem.
No wonder mental health is plummeting. Tens of millions of people don’t have the relationships that provide meaning in daily life. No amount of federal money − no number of mental health workers or programs − will solve that problem. The real solution is communities coming together and people reaching out to one another, in a spirit of mutual support.
I’ve seen this truth play out nationwide.
The Phoenix , which promotes sobriety and fights social isolation, is helping thousands of people beat substance abuse through a supportive community that’s often focused on physical fitness.
The Confess Project is training barbers and beauty industry professionals to be sort of paraprofessional mental health counselors, forging stronger bonds with millions of people through their everyday work, particularly among communities of color that have stigmas related to mental health.
Then there’s Give an Hour , in which mental health professionals help train people to be informal “peer supporters.”
Relationships, mental health support make a difference
It turns out that the combination of relationships and mental health support makes a remarkable difference.
These efforts are promising − but not nearly enough. Loneliness continues to soar, and with rising political polarization and social-media-driven isolation, this crisis looks set to continue getting worse.
Help fight depression and anxiety: Parents need help regulating their children's social media
As it does, more and more Americans will experience mental health challenges. While many will certainly need clinical help, let’s realize that the worst thing we can do is to expect others to solve this crisis.
The best thing we can do is to come alongside them ourselves.
Evan Feinberg is chair of the Stand Together Foundation and senior vice president of Stand Together .

- Newsletters
BREAKING NEWS
Roanoke Police investigating motorcycle crash on Bullitt Avenue SE
Virginia tech students take initiative to address mental health crisis, research continues to show mental health is a crisis on campuses across the country.
Abbie Coleman , Multimedia Journalist
BLACKSBURG, Va. – A crisis on college campuses around the country.
A new Wiley research study published this year shows more than 80% of college students say they’re struggling emotionally.
When Jilly Riccio was in high school, she lost her close friend Jamison Novello in a way she never imagined.
Have the morning's biggest stories arrive in your inbox every day at noon
“One of my friends died by suicide. That’s why it struck a chord and stuck with me, and that’s why I’ve been so passionate about it.”
During that time, Riccio was a part of her school’s SAFE Club — a way to talk openly about suicide, and mental health. But when she got to Virginia Tech, she quickly realized there was nothing close to that on campus.
Spring of last year, she decided to take matter’s into her own hands, creating the SAFE Club at Virginia Tech.
“It’s been really successful, and almost like therapy for me,” Riccio said.
10 News sat down with students at Virginia Tech to see how the mental health crisis impacts them.
Junior Jackie Mitchell said she wasn’t aware of the extent of her mental health problems until college.
“My mom was just like, ‘Oh you just have the jitters,’ but I came to Virginia Tech and was like, ‘I’m going to try therapy since it’s a free option,’ and they said, ‘You have anxiety,’” Mitchell said.
As Jackie told 10 News, anxiety for her wasn’t just ‘the jitters.’
“My body would physically shut down,” she said.
Abby Conner is the Communications Chair for the Clear Minds Project at Virginia Tech.
She said she hears students say time and time again, they feel alone.
“Some people are like, ‘Oh my issue isn’t that big,’ but to you, it is. It’s the biggest thing going on in your life,” Conner said.
Conner, her friend Aiden Williams, along with other students on campus created the Clear Minds Project this semester to bring awareness to resources for mental health, as well as help students navigate them.
“Mental health stuff especially, the insurance is terrible in Virginia, so it’s really complicated. Any information we can provide about that, we’re trying to do,” Williams said.
The Clear Minds Project, along with the SAFE Club, are just some of the resources for struggling students.
They appreciate and support the counseling efforts from Virginia Tech, but tell us they recognize how important community with other students is for healing.
“When you hear a student that has gone through something similar as you or can relate to you, because then you really do feel less alone. When you realize there’s a club, there’s a whole community where you can go to and you don’t even really have to say anything, you just have them there, I think that’s so important,” Riccio said.
Copyright 2024 by WSLS 10 - All rights reserved.
About the Author
Abbie coleman.
Abbie Coleman officially joined the WSLS 10 News team in January 2023.
Click here to take a moment and familiarize yourself with our Community Guidelines.
Recommended Videos
Financial stress is making us mentally and physically ill. Here’s how to cope

Years ago, I received a surprise in the mail: a $500 bill for a recent X-ray. I was earning an entry-level media salary at the time (for the uninitiated, that’s equivalent to peanuts), and the shock of having to figure out how to cover an unexpected expense sent my pulse racing with anxiety and my head pounding with stress.
I was in good company. Research shows again and again that our finances can take a toll on our minds . Money has consistently topped Americans’ list of stressors since the American Psychological Association began running its annual Stress in America Survey in 2007; it contributed to what the APA deemed the country’s “ mental health crisis ” risk in 2020. At the time, Americans were grappling with the coronavirus recession. They’ve since added the price of food , record-high credit card debt , and little student debt relief to their worries.
The Chicago-based nonprofit Financial Health Network began investigating the link between our finances and our health last year in the wake of the pandemic, examining literature and running a mass survey. Its latest research installment, released in April , employed a focus group. Participants revealed that money worries weren’t just causing their mental well-being to decline, but their physical health, reporting back pain and stomach aches so painful they couldn’t work. (So that explains my medical bill-induced headache).
“There’s a clear relationship between mental health and stress and how we feel in our bodies,” Angela Fontes, vice president of policy and research at Financial Health Network, tells Fortune .
We can partly thank the gut-brain connection for that. Stress and anxiety can manifest physically as nausea, shortness of breath, or stomach pain, to name a few symptoms.
What’s more: The health-money relationship is a vicious cycle. Poor mental well-being can also negatively impact our finances. Fontes explains that this manifests in various ways—compulsive spending as a coping mechanism; difficulty paying bills while carrying a heavy mental load; and missing work or not performing well, which she says can impact wages and long-term job success.
Consider that depression can result in neglecting even the most basic hygiene like brushing your teeth, says Khara Croswaite Brindle , a licensed financial therapist in Colorado. “We know that money isn’t basic, it requires a bit of mental energy to manage, so being in depression could mean our money is neglected in addition to our physical and mental health needs,” she explains.
Whether the chicken or the egg comes first, here’s how to make sure your physical, mental, and financial well-being are all on the same page.
Take a break to reset your mind
People fall into one of three categories, says Fontes: financially healthy; financially coping—getting by day to day but not preparing for long-term goals; and financially vulnerable—struggling with nearly every aspect of their financial lives. This last cohort comprises two sub groups: Those who experienced a financial shock (and typically overcome it) and those who have been chronically struggling financially, which increases the potential of long-term mental health challenges.
This can be the result of financial trauma , generational debt or intergenerational poverty, lack of financial literacy, or even a few poor money choices. But the root of any of these money challenges is emotion, says Croswaite Brindle: “Whether it’s anxiety, depression, dread, or avoidance, money is inherently emotional.”
She says seeing a financial therapist to discuss things like money beliefs and spending patterns can help you navigate your emotions so they don’t take a toll on your mental and physical health. “People can change their thoughts, feelings, and behaviors with money, putting them on the path to a better financial situation,” she says. Of course, some of the most financially vulnerable may not be able to afford therapy. Fontes says that many participants in the study coped by taking time to do one thing, like exercise or meditation , to get their mind in a different space that would make tackling their financial challenges feel more doable. And that’s a good place to start.
“A lot of this is about control,” she says, explaining that big triggers for this cycle are unexpected expenses like debt accumulation. “Getting and doing something that sort of helps restore that sense of control really seems to be a critical first step.”
Take baby steps toward saving
Even if your finances aren’t in poor shape, you should still take preventative measures so they don’t nosedive if your mental health tanks.
That might look like sitting down and reviewing your money once a week or examining your savings and investment accounts to see if you can tuck away another $10 a month, Fontes says.
A savings cushion can help protect against unexpected expenses. It can also help during low points—like having the house cleaned so you can feel better in your environment or ordering food when you don’t have the energy to cook, Croswaite Brindle says. It gives you permission and the means to access what you need or take time off without your household taking a financial hit, she adds.
“Savings isn’t always about the long game anymore, but about how do we live a comfortable life now while thinking about the future?” Croswaite Brindle says. “Not an either-or but a both-and way of thinking.”
More on stress and your health:
- Work-related stress is fueling America’s mental health crisis. Here are solutions to make it better
- Stress is making your biological age older than it actually is. Recovering could make you younger again
- These are the top 10 most stressed states in America
- 6 proven ways to cope with financial stress
Most Popular


IMAGES
COMMENTS
At least four-in-ten U.S. adults (41%) have experienced high levels of psychological distress at some point during the pandemic, according to four Pew Research Center surveys conducted between March 2020 and September 2022. Young adults are especially likely to have faced high levels of psychological distress since the COVID-19 outbreak began ...
Gen Z adults ages 18-23 are the most likely age group to report experiencing common symptoms of depression, with 75% noting that in the prior 2 weeks they felt so tired that they sat around and did nothing. 51% of Gen Z teens ages 13-17 say the pandemic has made planning for their future feel impossible. Despite these numerous stressors, 71 ...
The voices of adolescents and their parents, while shielded by anonymity, deepen an understanding of this mental health crisis. Matt Richtel is a best-selling author and Pulitzer Prize-winning ...
Illustration by Sébastien Thibault. There is a mental-health crisis in science — at all career stages and across the world. Graduate students are being harassed and discriminated against, paid ...
The H1N1 crisis: a case study of the integration of mental and behavioral health in public health crises. Disaster Med Public Health Prep 2012;6:67-71. Crossref
Mental health. Mental health is a state of mental well-being that enables people to cope with the stresses of life, realize their abilities, learn well and work well, and contribute to their community. It has intrinsic and instrumental value and is integral to our well-being. At any one time, a diverse set of individual, family, community and ...
Medical groups, schools, and advocacy organizations have been raising the alarm about the ongoing crisis in youth mental health, which was only exacerbated by the COVID-19 pandemic. New research shows that emergency department (ED) visits for suicidal ideation have been on the rise since before the pandemic, and suicide among youth may be ...
The World Health Organization today released its largest review of world mental health since the turn of the century. The detailed work provides a blueprint for governments, academics, health professionals, civil society and others with an ambition to support the world in transforming mental health. In 2019, nearly a billion people - including 14% of the world's adolescents - were living ...
The Covid-19 pandemic era ushered in a new set of challenges for youth in the United States, leading to a mental health crisis as declared by the United States surgeon general just over a year ago.But U.S. children and teens have been suffering for far longer. In the 10 years leading up to the pandemic, feelings of persistent sadness and hopelessness—as well as suicidal thoughts and ...
A spotlight from our 2021 State of Mental Health in America report. This report explores the data from the over 1.5 million people who took a screen through the MHA Online Screening Program from January to September 2020, to understand the impact of the COVID-19 pandemic on mental health.
Background. Mental health-related crises (MHC) in the community are increasing. This can partly be attributed to increased transitions from institutions to community treatment, 1 while the COVID-19 pandemic also had an impact, with the National Health Service in the UK, reporting a significant increase in urgent and emergency referrals of people in crisis. 2 Police and paramedics are often the ...
The White House Report on Mental Health Research Priorities is the first of its kind to outline an Administration-wide set of critical and timely needs and opportunities in mental health research ...
Experiencing a mental health crisis. More than half of the service user participants reported a previous experience of having a MH crisis (n = 34), although a number of people were unsure whether this was their first crisis or not ().There was a higher percentage of people in site C (36%) reporting it as their first crisis, reflecting recruitment mainly via the VS, than in the other sites ...
In 2022, Congress passed the Bipartisan Safer Communities Act, which has provided $245 million to fund mental health services like training for school personnel, first responders and law enforcement and expanding the 988 suicide and crisis lifeline. Stanford Medicine researchers know that to make the most impact with their discoveries they must ...
Mental health is a focus of NIH research during the COVID-19 pandemic. Researchers at NIH and supported by NIH are creating and studying tools and strategies to understand, diagnose, and prevent mental illnesses or disorders and improve mental health care for those in need. ... Call or text the 988 Suicide & Crisis Lifeline at 988 (para ayuda ...
America's Mental Health Crisis In this Issue. Young people are contending with anxiety, jails have become de facto mental health centers, and deaths are rising from drug overdoes—but we know the way forward, if we have the will. Our nation is facing a new public health threat. Accelerated but not solely caused by the COVID-19 pandemic ...
Scope of Mental Health Promotion and Prevention in the Current Situation. Literature provides considerable evidence on the effectiveness of various preventive mental health interventions targeting risk and protective factors for various mental illnesses (18, 36-42).There is also modest evidence of the effectiveness of programs focusing on early identification and intervention for severe ...
Research into the identification of risks for developing mental health disorders and early intervention in young people are crucial for curtailing the youth mental health crisis.
Our nation is facing a mental health crisis among people of all ages, and the COVID-19 ... mental health research experts and mental health service providers from across the U.S.
By nearly every metric, student mental health is worsening. During the 2020-2021 school year, more than 60% of college students met the criteria for at least one mental health problem, according to the Healthy Minds Study, which collects data from 373 campuses nationwide (Lipson, S. K., et al., Journal of Affective Disorders, Vol. 306, 2022).In another national survey, almost three quarters ...
A group of researchers posited another explanation for the youth mental health crisis: too much discussion. By Ellen Barry She covers mental illness. For years now, policymakers have sought an ...
Mental health and related conditions are a hot-button healthcare topic in 2024. With an estimated one in five Americans living with a mental health condition, ongoing research into the causes, treatment options, and possible triggers has never been more necessary.. Research in the mental health space helps fill knowledge gaps and create a fuller picture for patients, healthcare professionals ...
President Joe Biden reflected in his State of the Union in March on the COVID-19 pandemic and how it had wreaked havoc on people's day-to-day lives, spurring "a mental health crisis of isolation and loneliness." Data supports this: As the pandemic unfolded, one 2021 study found that about 4 in 10 adults reported symptoms of anxiety or depression, four times pre-pandemic levels.
WARNING: This article contains references to mental health and suicide. Despite living with major depression, experiencing regular panic attacks and having a history of suicide attempts, it still ...
The goal is to stimulate a broader discussion about the necessary measures to address the mental health crisis among young people, to inform policy and healthcare strategies, and ultimately, to improve the mental health outcomes for this vulnerable population in the post-pandemic world. ... International Journal of Environmental Research and ...
But new research is showing that mental illness is a crisis of young people. Indeed, 50% of all mental health problems appear by age 14 and 75% by age 24. It's a pattern that experts are quickly ...
The mental health advocates and substance abuse experts whom my organization has worked with over the past decade show the way. They prove that the mental health crisis isn't just a clinical ...
Research continues to show mental health is a crisis on campuses across the country. ... 10 News sat down with students at Virginia Tech to see how the mental health crisis impacts them.
The latest research on the connection between money and the mind finds our finances even take a toll on our physical health. ... it contributed to what the APA deemed the country's "mental ...