An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Subst Abuse
- PMC10176789

The Impact of Recreational Cannabis Legalization on Cannabis Use and Associated Outcomes: A Systematic Review
Kyra n farrelly.
1 Department of Psychology, York University, Toronto, ON, Canada
2 Peter Boris Centre for Addictions Research, St. Joseph’s Healthcare Hamilton, McMaster University, Hamilton, ON, Canada
Jeffrey D Wardell
3 Institute for Mental Health Policy Research, Centre for Addiction and Mental Health, Toronto, ON, Canada
4 Department of Psychiatry, University of Toronto, Toronto, ON, Canada
Emma Marsden
Molly l scarfe, peter najdzionek, jasmine turna.
5 Michael G. DeGroote Centre for Medicinal Cannabis Research, McMaster University & St. Joseph’s Healthcare Hamilton, Hamilton, ON, Canada
James MacKillop
6 Homewood Research Institute, Guelph, ON, Canada
Background:
Recreational cannabis legalization has become more prevalent over the past decade, increasing the need to understand its impact on downstream health-related outcomes. Although prior reviews have broadly summarized research on cannabis liberalization policies (including decriminalization and medical legalization), directed efforts are needed to synthesize the more recent research that focuses on recreational cannabis legalization specifically. Thus, the current review summarizes existing studies using longitudinal designs to evaluate impacts of recreational cannabis legalization on cannabis use and related outcomes.
A comprehensive bibliographic search strategy revealed 61 studies published from 2016 to 2022 that met criteria for inclusion. The studies were predominantly from the United States (66.2%) and primarily utilized self-report data (for cannabis use and attitudes) or administrative data (for health-related, driving, and crime outcomes).
Five main categories of outcomes were identified through the review: cannabis and other substance use, attitudes toward cannabis, health-care utilization, driving-related outcomes, and crime-related outcomes. The extant literature revealed mixed findings, including some evidence of negative consequences of legalization (such as increased young adult use, cannabis-related healthcare visits, and impaired driving) and some evidence for minimal impacts (such as little change in adolescent cannabis use rates, substance use rates, and mixed evidence for changes in cannabis-related attitudes).
Conclusions:
Overall, the existing literature reveals a number of negative consequences of legalization, although the findings are mixed and generally do not suggest large magnitude short-term impacts. The review highlights the need for more systematic investigation, particularly across a greater diversity of geographic regions.
Introduction
Cannabis is one of the most widely used substances globally, with nearly 2.5% of the world population reporting past year cannabis use. 1 Cannabis use rates are particularly high in North America. In the U.S., 45% of individuals reported ever using cannabis and 18% reported using at least once annually in 2019. 2 , 3 In Canada, approximately 21% of people reported cannabis use in the past year use in 2019. 4 In terms of cannabis use disorder (CUD), a psychiatric disorder defined by clinically significant impairment in daily life due to cannabis use, 5 ~5.1% of the U.S. population ages 12+ years met criteria in 2020, with ~13.5% of individuals ages 18 to 25 years meeting criteria. 6
Overall, rates of cannabis use have shown long-term increasing trends among several age groups in North America. 7 - 9 Moreover, research has revealed recent cannabis use increases in at risk populations, such as individuals with depression and pregnant women. 10 , 11 Parallel to increased cannabis use over time, rates of cannabis-related consequences have also increased across Canada and the U.S., including cannabis dependence and CUD, 8 , 12 crime rates (eg, increased possession charges), 8 and cannabis-impaired driving (and, lower perception of impairment and risk from cannabis use). 11 , 13 , 14 Further, cannabis use poses a risk for early-onset or use during adolescence as there is evidence that cannabis use in adolescence is linked with poorer cognitive performance, psychotic disorders, and increased risk of mood and addictive disorders. 15 With the rates of negative consequences from cannabis use increasing, particularly in North America where cannabis has become legal in many parts of the US and all of Canada, understanding the role of cannabis legalization in these changes is crucial to inform ongoing changes in cannabis policies worldwide.
The legal status of cannabis varies widely across countries and regions. Although cannabis is largely illegal at the global level, policies surrounding cannabis use are becoming steadily liberalized. Decriminalization (reduced penalties for self-use but not distribution) is more widespread worldwide, including in the Netherlands, Portugal, and parts of Australia. Medical legalization is also seen in Peru, Germany, New Zealand, the Netherlands and across many U.S. states. To date, Canada, Uruguay, and Malta are the only 3 countries to legalize recreational cannabis use at the national level. Further, individual U.S. states began legalizing recreational cannabis in 2012, with nearly half of U.S. states having legalized recreational cannabis by 2023. As national and subnational recreational legalization continues to gain support and take effect, understanding the consequences of such major regulatory changes is crucial to informing ongoing policy changes.
There are arguments both for and against recreational cannabis legalization (RCL). Common pro-legalization arguments involve increasing regulatory control over product distribution, weakening organized crime, reducing burden and inequality in the criminal justice system, and generating economic benefits such as tax revenues and commercial activity. 16 Furthermore, as cannabis obtained from illicit markets is of varying and unknown potency, 17 cannabis legalization may help better regulate the potency and quality of cannabis products. 18 On the other hand, there are anti-legalization arguments such as the possibility of legalization leading to increased use among youth and increased cannabis-impaired driving. 16 A nationally representative survey in the U.S. found that pro-legalization arguments were perceived to be more persuasive than public health anti-legalization arguments in a U.S. nationally representative survey, 19 suggesting policymaker concerns regarding RCL do not seem to hold as much weight in the general public. However, while research may be increasing surrounding the impacts of RCL, the general consensus of if RCL leads to more positive or negative consequences is unclear.
With RCL becoming more prevalent globally, the impacts it may have on a variety of health-related outcomes are of critical importance. Prevalence of cannabis use is of course a relevant issue, with many concerned that RCL will cause significant spikes in rates of cannabis use for a variety of groups, including youth. However, current studies have revealed mixed evidence in the U.S., 20 , 21 thus there is a need to synthesize the extant literature to better understand the balance of evidence and potential impacts of RCL across different samples and more diverse geographic areas. Another common question about RCL is whether it will result in changes in attitudes toward cannabis. These changes are of interest as they might forecast changes in consumption or adverse consequences. Similarly, there are concerns surrounding RCL and potential spill-over effects that may influence rates of alcohol and other substance use. 22 Thus, there remains a need to examine any changes in use of other substance use when studying effects of RCL.
Beyond changes in cannabis and other substance use and attitudes, health-related impacts of RCL are important to consider as there are links between cannabis use and adverse physical and mental health consequences (eg, respiratory and cardiovascular diseases, psychosis). 23 Additionally, emergency service utilization associated with cannabis consumption is a frequent concern associated with RCL, particularly due to the spikes in admissions following RCL in Colorado. 24 However, the rates of cannabis-related emergency service admissions more globally (eg, in legal countries like Canada and Uruguay) have not been fully integrated into summaries of the current literature. Finally, another health-related consequence of RCL is potential impacts on opioid use. While opioid-related outcomes can fall into substance use, they are considered health-related for this review as much of the discussion surrounding RCL and opioids involve cannabis substituting opioid use for medicinal reasons or using cannabis as an alternate to prescription opioids in the healthcare system. The current opioid crisis is a global public health problem with serious consequences. While there is evidence that medicinal cannabis may reduce prescription opioid use 25 and that cannabis may be a substitute for opioid use, 26 the role of recreational cannabis legalization should also be examined as the 2 forms of cannabis use are not interchangable 27 and have shown unique associations with prescription drug use. 28 Thus, there is a need to better understand how and if RCL has protective or negative consequences on opioid-related outcomes.
Due to the impairing effects of cannabis on driving abilities and the relationship with motor vehicle accidents, 29 another important question surrounding RCL is how these policy changes could result in adverse driving-related outcomes. An understanding of how RCL could influence impaired driving prevalence is needed to give insight into how much emphasis jurisdictions should put on impaired driving rates when considering RCL implementation. A final consequence of RCL that is often debated but requires a deeper understanding is how it impacts cannabis-related arrest rates. Cannabis-related arrests currently pose a significant burden on the U.S. and Canadian justice system. 30 , 31 Theoretically, RCL may ease the strain seen on the justice system and have positive trickle-down effects on criminal-related infrastructure. However, the overall implications of RCL on arrest rates is not well understood and requires a systematic evaluation. With the large number of RCL associated outcomes there remains a need to synthesize the current evidence surrounding how RCL can impact cannabis use and other relevant outcomes
Present review
Currently, no reviews have systematically evaluated how RCL is associated with cannabis-use changes across a variety of age groups as well as implications on other person- or health-related outcomes. The present review aims to fill an important gap in the literature by summarizing the burgeoning research examining a broad range of consequences of RCL across the various jurisdictions that have implemented RCL to date. Although previous reviews have considered the implications of RCL, 32 , 33 there has recently been a dramatic increase in studies in response to more recent changes in recreational cannabis use policies, requiring additional efforts to synthesize the latest research. Further, many reviews focus on specific outcomes (eg, parenting, 34 adolescent use 35 ). There remains a need to systematically summarize how RCL has impacted a variety of health-related outcomes to develop a more comprehensive understanding of the more negative and positive outcomes of RCL. While a few reviews have examined a broad range of outcomes such as cannabis use, related problems, and public health implications, 32 , 33 some reviews have been limited to studies from a single country or published in a narrow time window. 32 Thus, a broader review is necessary to examine multiple types of outcomes from studies in various geographic regions. Additionally, a substantial amount of the current literature examining the impact of RCL relies on cross-sectional designs (eg, comparing across jurisdictions with vs without recreational legalization) which severely limit any conclusions about causal associations. Thus, given its breadth, the current systematic review is more methodologically selective by including only studies with more rigorous designs (such as longitudinal cohort studies), which provide stronger evidence regarding the effects of RCL. In sum, the aim of the current review was to characterize the health-related impacts of RCL, including changes in these outcomes in either a positive or negative direction.
The review is compliant with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 36 ). Full-text extraction was initiated immediately following article search, therefore the protocol was not registered with PROSPERO. Relevant articles on cannabis legalization were principally identified using the Boolean search terms (“cannabis” OR “marijuana” OR “THC” OR “marihuana”) AND “legalization” AND (“recreational” OR “non-medical” OR “nonmedical”) AND (“longitudinal” OR “pre-post” OR “prospective” OR “timeseries” OR “cohort”). The search was conducted using PubMed/MEDLINE, EMBASE, and PsycINFO through November 2022. Relevant studies identified through secondary means (eg, prior knowledge of a relevant publication, articles brought to the authors’ attention) were also included for screening. Titles and abstracts resulting from the initial search were screened in Covidence (Veritas Health Innovation Inc) by 2 reviewers for suitability for full-text review and final inclusion. Conflicts were discussed by both reviewers and a final decision was made by consensus. Following screening, reviewers read and extracted relevant data. To be included, an article was required to meet the following criteria: (i) an original empirical research article published in a peer-reviewed journal; (ii) written in (or available in) English; (iii) RCL serves as an independent variable; (iv) quantitative study design that clearly permitted the evaluation of the role of RCL with a more rigorous non-cross-sectional study design (eg, pre- vs post-legalization, longitudinal, cohort, interrupted time series, etc.); and (v) reports on health-related outcomes (ie, changes in consumption or attitudes, as opposed to changes in price or potency).
RCL related outcomes that were considered were those specifically involving the behavior, perceptions, and health of individuals. Population-level outcomes (eg, health-care utilization or impaired driving) were considered eligible for inclusion as they involve the impacts that legalization has on individual behavior. Thus, economic- or product-level outcomes that do not involve individual behavior (eg, cannabis prices over time, changes in cannabis strain potency) were considered out of scope. The outcome groups were not decided ahead of time and instead 5 main themes in outcomes emerged from our search and were organized into categories for ease of presentation due to the large number of studies included.
Studies that examined medicinal cannabis legalization or decriminalization without recreational legalization, and studies using exclusively a cross-sectional design were excluded as they were outside the scope of the current review. The study also excluded articles that classified RCL as the passing of legal sales rather than implementation of RCL itself as RCL is often distinct from introduction of legal sales, or commercialization. Thus, we excluded studies examining commercialization as they were outside the scope of the current review.
Characteristics of the literature
The search revealed 65 relevant articles examining RCL and related outcomes (see Figure 1 ). There were 5 main themes established: cannabis use and other substance use behaviors ( k = 28), attitudes toward cannabis ( k = 9), health-related outcomes ( k = 33), driving related impacts ( k = 6), and crime-related outcomes ( k = 3). Studies with overlapping themes were included in all appropriate sections. Most studies (66.2%) involved a U.S. sample, 32.3% examined outcomes in Canada, and 1.5% came from Uruguay. Regarding study design, the majority (46.2%) utilized archival administrative data (ie, hospital/health information across multiple time points in one jurisdiction) followed by cohort studies (18.5%). The use of administrative data was primarily used in studies examining health-related outcomes, such as emergency department utilization. Studies examining cannabis use or attitudes over time predominantly used survey data. Finally, both driving and crime related outcome studies primarily reported findings with administrative data.

Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) study flow diagram.
Changes in cannabis and other substance use
Cannabis and other substance use changes represented the second largest number of studies, with 28 articles identified. Studies examining changes in cannabis use behaviors were divided by subpopulation (ie, adolescents, young adults, general population adults, clinical populations, and maternal use; see Table 1 ). Finally, we separately summarized studies reporting changes in concurrent use of other substances, and routes of cannabis administration.
Studies investigating the role of recreational cannabis legalization on cannabis and other substance consumption.
Author, author of article; Year, publication year of article; Location, jurisdiction article data was collected in; Date of Legalization, year legalization was enacted in jurisdiction; Sample, total N of article sample; RCL, Recreational Cannabis Legalization.
Cannabis use changes in adolescents (~12-17)
Ten studies examined changes in cannabis use among adolescents and found that changes in the rates of use were inconsistent following RCL. Gunadi et al 37 found an association between RCL and more pronounced transition from non-use to cannabis use when compared to states with no legalization and those with medical cannabis legalization ( P ⩽ .001) combined, but not when compared to states with medical cannabis legalization only. Another study found that in states with RCL adolescents who never used cannabis but used e-cigarettes were more likely to use cannabis at follow-up than those living in states without RCL (aOR = 18.39, 95% CI: 4.25-79.68vs aOR = 5.09, 95% CI: 2.86-9.07, respectively) suggesting a risk of cannabis initiation among legal states. 38 Among adolescents reporting recent alcohol and cannabis co-use, one study found a significant increase in the frequency of past 30-day cannabis use following RCL ( b = 0.36, SE = 0.07, P ⩽ .001). 39 In a Canadian study using a repeated cross-sectional design as well as a longitudinal design to examine changes in cannabis use, results revealed that adolescents had increased odds of ever using cannabis in the year following RCL in the cross-sectional data ( P = .009). 40 However, the longitudinal sample revealed no significant differences in the odds of ever use, current use, and regular use of cannabis post-legalization. There is also evidence of RCL impacts on adolescent cannabis use consequences, as a Washington study found a significant indirect effect of RCL on cannabis consequences through perceived risk as a mediator ( B = 0.37, P ⩽ .001). 41
On top of the above evidence, there were multiple studies examining cannabis use changes over time among adolescents in Washington and Oregon that found higher rates of cannabis use associated with cohorts examined during RCL compared to non-legal cohorts, 42 - 44 although the differences across legal cohorts were not significant in all cases. 42 Furthermore, in another study, RCL did not impact initiation of use, but for current users the RCL group had significantly greater increased rates of cannabis use compared to the pre-RCL group (RR = 1.26, 95% CI = 1.10, 1.45). 43 For the final study, cannabis use increased in the post-RCL group but patterns of use (frequency; daily vs weekly use) were similar across groups. 44 Overall, the preceding 8 studies reveal some evidence that RCL was associated with increasing rates of cannabis use in adolescent. However, 5 studies point to some inconsistent associations of RCL and cannabis use and suggest that overall relationship of RCL and adolescent cannabis as mixed.
Three studies add to these inconsistent findings and point to lack of an association between RCL and changes in cannabis use among adolescents. Two studies found no significant increase in the frequency of or prevalence of cannabis use following RCL. 41 , 45 Finally, a study examining trends of adolescent cannabis use and associations with period effects (ie, external world events that could influence use) suggests laws and regulations associated with RCL were not associated with cannabis use changes. 46 The current research reveals conflicting evidence about the role of RCL on adolescent cannabis use.
Cannabis use changes in young adults (~18-25)
Young adulthood, typically defined as ages 18 to 25 and also known as emerging adulthood, is commonly associated with decreased parental supervision, increased availability of substances, and greater substance experimentation making it a key developmental period for the onset of cannabis use. 47 Four studies examined the impact of RCL on cannabis use among young adults, 2 of which found significant associations between RCL and increased cannabis use in college students. 47 , 48 Barker and Moreno 48 found the rate of students ever using cannabis did not change. However, in those who had used cannabis prior to RCL, the proportion of students using in the past 28-days increased faster following RCL in Washington (legal-state) when compared with the rate of increase in Wisconsin (non-legal state; P ⩽ .001). 48 Further, in college students from Oregon, rates of cannabis use increased significantly from before to after RCL ( P = .0002). 47 Another study looked at changes in cannabis use in a sample of young adults from the U.S. who had never vaped cannabis at the time of recruitment. 49 Results revealed that cannabis use in the past year did not differ in states with or without RCL, although, those living in states with RCL did show a larger increase in rates of cannabis vaping across time, compared to those in non-RCL states. Finally, in a sample of youth from Oregon and Washington, RCL predicted a higher likelihood of past-year cannabis use ( P = .001). 50 In contrast to the adolescent literature, studies examining cannabis use in young adult samples fairly consistently point to an association between RCL and increasing rates of cannabis use.
Cannabis use changes in general population adults
Five studies examined changes in cannabis use in adults (without further age subclassification) associated with RCL. Four of these studies suggested higher rates of cannabis use in adults for RCL jurisdictions compared to non-legal states post-RCL, or increased use following RCL. 37 , 45 , 51 , 52 Past 30-day cannabis use increased significantly 1-month post-RCL and remained elevated 6-months post-RCL (ps = 0.01) in a sample of adults from California. 51 Another study found an association between RCL and transition from non-users to cannabis users and non-users to weekly users when compared to states with no medical legalization or RCL ( P ⩽ .001) and states with no legalization combined with those with medical cannabis legalization ( P ⩽ .001). 37 Meanwhile, in Canada, a significant increase in prevalence of cannabis use was observed following RCL. 45 Additionally, in those reporting no cannabis use prior to RCL in Canada, there were significant increases in cannabis use frequency, quantity of cannabis used, and severity of cannabis misuse following RCL. 52 The opposite pattern was seen for those reporting cannabis use prior to RCL, with significant decreases in frequency of use, quantity, and misuse. 52 However, not all studies found RCL was associated with increased cannabis use. For instance, a repeated cross-sectional study of adult in the U.S. found no association between RCL and frequency of cannabis use. 53
A benefit of the extant literature examining general population cannabis use is that it covers a variety of jurisdictions and study designs, albeit with some heterogeneity and mixed findings. On balance, the evidence within the current literature, generally suggests an increase in cannabis use for adults in the general population following RCL with 80% of the reviewed studies supporting this conclusion.
Maternal use
Three studies examined whether rates of cannabis use during pregnancy have increased following RCL. Two studies suggested increased cannabis use during pregnancy associated with RCL. In one study urine screen-detected cannabis use during pregnancy increased from 6% to 11% following RCL in California ( P = .05). 54 Another study in a sample of women participating in an intensive case management program for heavy alcohol and/or drug use during pregnancy, examined cannabis use among those exiting from the program before versus after RCL. Findings revealed women exiting after RCL were more likely to report using cannabis in the 30 days prior to exit compared to those pre-RCL (OR = 2.1, P ⩽ .0001). 55 One study revealed no significant difference in cannabis or alcohol use associated with RCL in women living with HIV during pregnancy or the postpartum period. 56 Overall, the evidence from these three studies suggests there may be increases in perinatal cannabis use following RCL, but the small number of studies and unique features of the samples suggests a need for more research.
Clinical populations use
Six studies examined cannabis use in clinical populations. One study investigated use and trauma admissions for adults and pediatric patients in California. 57 Results showed an increase in adult trauma patients with THC+ urine tests from pre- to post-RCL (9.4% to 11.0%; P = .001), but no difference for pediatric trauma patients. A study based in Colorado and Washington, found that cannabis use rates in inflammatory bowel disease patients significantly increased from 107 users to 413 ( P ⩽ .001) pre to post-RCL. 58 A Canada-based study of women with moderate-to-severe pelvic pain found an increase in the prevalence of current cannabis use following RCL (13.3% to 21.5%; P ⩽ .001). 59 Another Canadian study showed an increase in the prevalence of current cannabis use after RCL among cancer patients (23.1% to 29.1%; P ⩽ .01). 60 Finally, two studies examined changes in cannabis use among individuals receiving treatment for a substance use disorder. In a sample of Canadian youth in an outpatient addictions treatment program, there was no change in the rate of cannabis use following RCL. 61 Further, in a sample of individuals receiving treatment for opioid use disorder, cannabis use was compared for those recruited 6 months before or after RCL with no significant changes in the prevalence or frequency of self-reported ( P = .348 and P = .896, respectively) or urine screen-detected ( P = .087 and P = .638, respectively) cannabis use following RCL. 62 Although these studies only represent a small number of observations, their findings do reveal associations between RCL and increasing cannabis use within some clinical samples.
Changes in polysubstance and other substance use
One study examined simultaneous cannabis and alcohol use among 7th, 9th, and 11th grade students in the U.S. 39 This study found that RCL was associated with a 6% increase in the odds of past 30-day alcohol and cannabis co-use. The association was even stronger in students with past 30-day alcohol use and heavy drinking. However, among past 30-day cannabis users, RCL was associated with a 24% reduction in co-use. This study suggests at least a modest association between RCL and concurrent cannabis and alcohol use among adolescents.
Numerous studies examined changes of alcohol and other substance use pre to post RCL. With regard to alcohol, one study from Colorado and Washington found a decrease in alcohol consumption among adolescents following RCL, 42 whereas another Washington study found RCL predicted a higher likelihood of alcohol use among youth. 50 A Canadian study also found no significant effect of RCL on rates of alcohol or illicit drug use among youth. 61 Finally, in a sample of trauma patients in California the findings around changes in substance use were mixed. 57 In adult patients, the rates of positive screens for alcohol, opiates, methamphetamine, benzodiazepine/barbiturate, and MDMA did not change following RCL, but there was an increase in positive screens for cocaine. In pediatric patients, increases were seen in positive screens for benzodiazepine/barbiturate, but positive screens for alcohol, opiates, methamphetamine, and cocaine did not change. 57 The current evidence is divided on whether RCL is associated with increased alcohol and other substance use, with 40% of studies finding an association and 60% not observing one or finding mixed results.
In the case of cigarettes, Mason et al 42 did find significant cohort effects, where the post-RCL cohort was less likely to consume cigarettes compared to the pre-RCL one (Coefficient: − 2.16, P ⩽ .01). However, these findings were not echoed in more recent studies. Lack of an effect for cigarette use is supported by an Oregon study that found RCL was not associated with college student’s cigarette use. 47 Similarly, RCL was not significantly associated with past-year cigarette use in a sample of young adults from Oregon and Washington. 50 On balance, there is little evidence that RCL is linked with changes in cigarette smoking.
Route of administration
The increase in smoke-free alternative routes of cannabis administration (eg, vaping and oral ingestion of edibles) 63 , 64 make method of cannabis consumption an important topic to understand in the context of RCL. Two studies examined differences in route of cannabis consumption as a function of cannabis policy. One study examined changes in the number of different modes of cannabis use reported by high school students in Canada. 65 Results showed that from pre-to-post RCL 31.3% of students maintained a single mode of use, 14.3% continued to use cannabis in multiple forms, while 42.3% expanded from a single mode to multiple modes of administration and 12.1% reduced the number of modes they used. Another study found that smoking, vaping, and edibles (in that order) were the most frequent modes of cannabis use pre- and post-RCL in California, suggesting minimal impact of RCL on mode of cannabis use. 51 However, the least common mode of cannabis use was blunts, which did decline following RCL (13.5%-4.3%). 51 Overall, the evidence suggests RCL may be associated with changes in modes of cannabis consumption, but as the evidence is only from two studies there still remains a need for more studies examining RCL and cannabis route of administration.
Nine studies examined RCL and cannabis attitudes (see Table 2 ). Regarding cannabis use intentions, one U.S. study found that for both a non-RCL state and a state that underwent RCL, intention to use in young adults significantly increased post-RCL, suggesting a lack of RCL specific effect, 48 and that aside from the very first time point, there were no significant differences between the states in intention to use. Further, attitudes and willingness to use cannabis, between the RCL and non-RCL state remained similar overtime ( P s ⩾ .05), although both states reported significantly more positive attitudes toward cannabis following RCL ( P ⩽ .001). 48 However, another study U.S. from found differences in adolescent use intentions across RCL, whereby those in the RCL cohort in jurisdictions that allowed sales were less likely to increase intent to use cannabis ( P = .04), but the RCL cohort without sales were more likely to increase intent to use ( P = .02). 43 The pre-RCL cohort in communities that opted out of sales were also less likely to increase willingness to use compared to the cohort with legal sales ( P = .02). 43 Both studies reveal contrasting findings surrounding RCL’s relationship with cannabis use intentions and willingness to use.
Studies examining recreational cannabis legalization and attitudes surrounding cannabis.
Looking at cannabis use motives, one study found a non-significant increase in recreational motives for cannabis use post-RCL. 60 Similarly following RCL in Canada, 24% of individuals previously reporting cannabis use exclusively for medical purposes declared using for both medical and non-medical purposes following RCL, and 24% declared use for non-medical purposes only, 66 suggesting RCL can influence recreational/nonmedicinal motivations for cannabis use among those who previously only used for medical reasons.
In studies examining perceived risk and perceptions of cannabis use, one U.S. study found an indirect effect between RCL and increased consequences of use in adolescents through higher perceived risk ( P ⩽ .001), but no association with frequency of use. 41 Another U.S. study revealed mixed results and found that RCL was not associated with perceived harm of use in youth. 50 Further, youth in one study did not report differences in perceptions of safety of cannabis, ease of accessing cannabis use or on concealing their use from authority, 61 which contrasts with another study finding increased reports of problems accessing cannabis post-RCL ( P ⩽ .01). 60 Regarding health perceptions, a California study found that cannabis use was perceived as more beneficial for mental health, physical health, and wellbeing in adults at 6 months post-RCL compared to pre-RCL and 1-month post-RCL ( P = .02). 51 Mental health perceptions of cannabis use increased from being perceived as “slightly harmful” pre-RCL to perceived as “slightly beneficial” at 6 months post-RCL. 51 However, in a sample of treatment seeking individuals with an opioid use disorder, the vast majority of participants reported beliefs that RCL would not impact their cannabis use, with no difference in beliefs pre- to post-RCL (85.9% reported belief it would have no impact pre-RCL and 85.7%, post-RCL). 62 The combined results of the studies suggest potential associations of RCL with risk and benefit perceptions of cannabis use, however as 55% of studies suggest a lack of or inconsistent association with RCL, on balance the literature on RCL’s impact on cannabis attitudes is mixed.
Health-related outcomes
We identified 33 articles that examined various health-related outcomes associated with RCL (see Table 3 ). The largest number involved hospital utilization (ie, seeking emergency services for cannabis-related problems such as unintentional exposure, CUD, and other harms). Other health-care outcomes included opioid-related harms, mental health variables, and adverse birth outcomes.
Studies investigating the relationship of recreational cannabis legalization and health-related outcomes.
Author, Author of article; Year, Publication year of article; Location, Jurisdiction article data was collected in; Date of Legalization, Year legalization was enacted in jurisdiction; Sample, Total N of article sample; CDC, Center for Disease Prevention; WONDER, Wide-Ranging Online Data for Epidemiologic Research; RCL, Recreational Cannabis Legalization.
Emergency service utilization
Seventeen studies examined the association between RCL and use of emergency services related to cannabis (eg, hospital visits, calls to regional poison centers). Regarding emergency service rates in youth, a Colorado study found the rate of pediatric cannabis-related emergency visits increased pre- to post-RCL ( P ⩽ .0001). 67 Similarly, cannabis-related visits requiring further evaluation in youth also increased. 67 This increasing need for emergency service related to cannabis exposure in youth following RCL was supported in 4 other U.S. studies. 68 - 71 A Canadian study supported the U.S. studies, finding a 2.6 increase in children admissions for cannabis poisonings post-RCL. 72 In contrast, overall pediatric emergency department visits did not change from pre- to post-RCL in Alberta, Canada, 73 but there was a non-significant increase of the rate and proportion of children under 12 presenting to the emergency department. However, unintentional cannabis ingestion did increase post-RCL for children under 12 (95% CI: 1.05-1.47) and older adolescents (1.48, 95% CI: 1.21-1.81). 74 Taken together, these studies do suggest a risk for increasing cannabis-related emergency visits in youth following RCL, with 75% of studies finding an association between RCL and increasing emergency service rates in youth.
There is also evidence of increased hospital utilization in adults following RCL. Five studies found evidence of increased emergency service utilization or poison control calls from cannabis exposure associated with RCL in the U.S. and Canada. 24 , 69 , 74 - 76 Finally, a Colorado study saw an increase in cannabis involved pregnancy-related hospital admissions from 2011 to 2018, with notable spikes after 2012 and 2014, timeframes associated with state RCL. 77
However, some evidence points to a lack of association between RCL and emergency service utilization. A chart review in Ontario, Canada found no difference in number of overall cannabis emergency room visits pre- versus post-RCL ( P = .27). 78 When broken down by age group, visits only increased for those 18 to 29 ( P = .03). This study also found increases in patients only needing observation ( P = .002) and fewer needing bloodwork or imaging services (both P s ⩽.05). 78 Further in a California study that found overall cannabis exposure rates were increasing, when breaking these rates down by age there was no significant change in calls for those aged 13 and up, only for those 12 and under. 69 An additional Canadian study found that rates of cannabis related visits were already increasing pre-RCL. 79 Following RCL, although there was a non-significant immediate increase in in cannabis-related emergency visits post-RCL this was followed a significant drop off in the increasing monthly rates seen prior to RCL. 79 Another Canadian study that examined cannabis hyperemesis syndrome emergency visits found that rates of admissions were increasing prior to RCL and the enactment of RCL was not associated with any changes in rates of emergency admissions. 80 As this attenuation occurred in Canada prior to commercialization where strict purchasing policy was in place, it may suggest that having proper regulations in place can prevent the uptick in cannabis-related emergency visits seen in U.S. studies.
Other hospital-related outcomes examined included admissions for cannabis misuse and other substance use exposure. One study found decreasing CUD admission rates over time (95% CI: −4.84, −1.91), with an accelerated, but not significant, decrease in Washington and Colorado (following RCL) compared to the rest of the U.S. 81 In contrast, another study found increased rates of healthcare utilization related to cannabis misuse in Colorado compared to New York and Oklahoma ( P s ⩽.0005). 82 With respect to other substance use, findings revealed post-RCL increases in healthcare utilization in Colorado for alcohol use disorder and overdose injuries but a decrease in chronic pain admissions compared to both controls ( P ⩽ .05). 82 However, two Canadian studies found the rate of emergency department visits with co-ingestant exposure of alcohol, opioid, cocaine, and unclassified substances in older adolescents and adults decreased post-RCL. 73 , 77 Another Canadian study found no change in cannabis-induced psychosis admissions nor in alcohol- or amphetamine-induced admissions. 83
Finally, three studies examined miscellaneous hospital-related outcomes. A study examining hospital records in Colorado to investigate facial fractures (of significance as substance impairment can increase the risk of accidents) showed a modest but not significant influence of RCL. 84 The only significant increases of facial trauma cases were maxillary and skull base fracture cases ( P s ⩽ .001) suggesting a partial influence of RCL on select trauma fractures. The second study found increased trauma activation (need for additional clinical care in hospital) post-RCL in California ( P = .01). 57 Moreover, both adult and pediatric trauma patients had increased mortality after RCL ( P = .03; P = .02, respectively). 57 The final study examining inflammatory bowel disease (IBD) outcomes in the U.S. found more cannabis users on total parenteral nutrition post-RCL (95% CI: 0.02, 0.89) and lower total hospital costs in users post-RCL (95% CI: −15 717, −1119). 58 No other IBD outcomes differed pre- to post-RCL (eg, mortality, length of stay, need for surgery, abscess incision and drainage).
Overall, these studies point to increased cannabis-related health-care utilization following RCL for youth and pediatrics (75% finding an increase). However, the impact of legalization on adult rates of cannabis-related emergency visits is mixed (44% finding lack of an association with RCL). As findings also varied across different countries (ie, Canada vs the U.S.), it suggests the importance of continually monitoring the role of RCL across different jurisdictions which may have different cannabis regulations in place. These studies also suggest there may be other health consequences associated with RCL. Further research should be done to examine trends of other emergency service use that could be influenced by RCL.
Two studies reported a weak or non-existent effect of RCL on opioid related outcomes. 85 , 86 First, a U.S. administrative study found no association of RCL and opioid prescriptions from orthopedic surgeons. 85 The second study found that, of U.S. states that passed RCL, those that passed policies before 2015 had fewer Schedule III opioid prescriptions ( P = .003) and fewer total doses prescribed ( P = .027), 86 but when compared to states with medicinal cannabis legislation, there were no significant differences. However, 3 studies suggested a potential protective effect of RCL, with one study finding a significant decrease for monthly opioid-related deaths following RCL (95% CI: –1.34, –0.03), compared to medical cannabis legalization and prohibition. 87 A Canadian study examining opioid prescription claims also found an accelerated decline in claims for public payers post-RCL compared to declines seen pre-RCL ( P ⩽ .05). 88 Next a study examining women with pelvic pain found that post-RCL patients were less likely to report daily opioid use, including use for pain ( P = .026). 59 These studies indicate some inconsistencies in relationships between RCL, opioid prescriptions and use indicators in the current literature, while the literature on balance points to a potential relationship with RCL (60%), the overall evidence is still mixed as 40% of studies support a weak association with RCL.
Adverse birth outcomes
Changes in adverse birth outcomes including small for gestational age (SGA) births, low birth weight, and congenital anomalies were examined in two studies. The first study, which examined birth outcomes in both Colorado and Washington, found that RCL was associated with an increase in congenital anomaly births for both states ( P ⩽ .001, P = .01 respectively). 89 Preterm births also significantly increased post-RCL, but only in Colorado ( P ⩽ .001). Regarding SGA outcomes, there was no association with RCL for either state. 89 Similarly, the second study did find an increase in the prevalence of low birth weight and SGA over time, but RCL was not directly associated with these changes. 90 Although the current literature is small and limited to studies in Washington and Colorado, the evidence suggests minimal changes in adverse birth outcomes following RCL.
Mental health outcomes
Six studies examined mental health related outcomes. A Canadian study examining psychiatric patients did not see a difference in rates of psychotic disorders pre- to post-RCL. 45 Similarly, another Canadian study did not see a difference in hospital admissions with schizophrenia or related codes post-RCL. 83 However, the prevalence of personality disorders and “other” diagnoses was higher post-RCL ( P = .038). 45 In contrast, another Canadian study found that rates of pediatric cannabis-related emergency visits with co-occurring personality and mood-related co-diagnoses decreased post-RCL among older adolescents. 73 A U.S. study examining the relationship between cannabis use and anxious mood fluctuations in adolescents found RCL had no impact on the association. 91 Similarly, another Canadian study found no difference in mental health symptomology pre- to post-RCL. 61 In contrast, anxiety scores in women with pelvic pain were higher post-RCL compared to pre-RCL ( P = .036). 59 The small number and mixed findings of these studies, 66.7% finding no association or mixed findings and 33.3% finding an association but in opposite directions, identify a need for further examination of mental health outcomes post-RCL.
Miscellaneous health outcomes
Three studies examined additional health-related outcomes. First, a California study examined changes in medical cannabis status across RCL. Post-RCL, 47.5% of medical cannabis patients remained medical cannabis patients, while 73.8% of non-patients remained so. 92 The transition into medical cannabis patient status post-RCL represented the smallest group (10%). Cannabis legalization was the most reported reason for transition out of medical cannabis patient status (36.2%). 92 Next, a study examining pelvic pain in women found that post-RCL patients reported greater pain catastrophizing ( P ⩽ .001), less anti-inflammatory ( P ⩽ .001) and nerve medication use ( P = .027), but more herbal pain medication use ( P = .010). 59 Finally, a Canadian study that examined cannabinoids in post-mortem blood samples reported that post-RCL deaths had higher odds of positive cannabis post-mortem screens compared to pre-RCL (95% CI: 1.09-1.73). 93 However, the majority of growth for positive cannabinoid screens took place in the two years prior to RCL implementation. In sub-group analyses, only 25- to 44-year-olds had a significant increase in positive cannabinoid screens (95% CI: 0.05-0.19). Additional post-mortem drug screens found an increase in positive screens for amphetamines ( P ⩽ .001) and cocaine ( P = .042) post-RCL. These additional health outcomes demonstrate the wide-ranging health impacts that may be associated with RCL and indicate a continued need to examine the role of RCL on a variety of outcomes.
Driving-related outcomes
Six studies examined rates of motor vehicle accidents and fatalities (see Table 4 ). Two U.S. studies found no statistical difference in fatal motor vehicle collisions associated with RCL. 94 , 95 Further, a California-based study examining THC toxicology screens in motor vehicle accident patients, did find a significant increase in positive screens, but this increase was not associated with implementation of RCL. 96 However, three studies suggest a negative impact of RCL, as one U.S. study found both RCL states and their neighboring states had an increase in motor vehicle fatalities immediately following RCL. 97 Additionally, a Canadian study did find a significant increase in moderately injured drivers with cannabis positive blood screens post-RCL. 98 Finally, a study in Uruguay found RCL was associated with increased immediate fatal crashes for cars, but not motorcycles; further investigation suggested this effect was noticeable in urban areas, but not rural areas. 99 While the overall evidence was inconsistent, current evidence does suggest a modest increase, seen in two studies, in motor vehicle accidents associated with RCL. Further longitudinal research in more jurisdictions is needed to understand the long-term consequences of RCL on motor vehicle accidents.
Studies looking at recreational cannabis legalization and driving related outcomes.
Crime-related outcomes
Three studies explored crime-related outcomes associated with RCL (see Table 5 ). A Washington study examining cannabis-related arrest rates in adults did find significant drops in cannabis-related arrests post-RCL for both 21+ year olds (87% drop; P ⩽ .001) and 18 to 20-year-olds (46% drop; P ⩽ .001). 100 However, in another study examining Oregon youth this post-RCL decline for arrests was not seen; cannabis-related allegations in youth actually increased following RCL (28%; 95% CI = 1.14, 1.44). 101 Further, declines in youth allegations prior to RCL ceased after RCL was implemented. In contrast, a Canadian study did find significant decreases in cannabis-related offenses in youth post RCL ( P ⩽ .001), but rates of property and violent crime did not change across RCL. 102 These studies highlight the diverse effects of RCL across different age groups. However, there remains a need for a more comprehensive evaluation on the role of RCL on cannabis-related arrests.
Studies investigating recreational cannabis legalization and crime related outcomes.
Author, Author of article; Year, Publication year of article; Location, Jurisdiction article data was collected in; Date of Legalization, Year legalization was enacted in jurisdiction; Sample, Total N of article sample; RCL, Recreational Cannabis Legalization.
Notably, two studies also examined race disparities in cannabis-related arrests. For individuals 21+ relative arrest disparities between Black and White individuals grew post-RCL. 100 When looking at 18 to 20-year-olds, cannabis-related arrest rates for Black individuals did slightly decrease, albeit non-significantly, but there was no change in racial disparities. 100 In youth ages 10 to 17, Indigenous and Alaska Native youth were more likely than White youth to receive a cannabis allegation before RCL (95% CI: 2.31, 3.01), with no change in disparity following RCL (95% CI: 2.10, 2.81). 101 On the other hand, Black youth were more likely to receive a cannabis allegation than White youth prior to RCL (95% CI: 1.66, 2.13), but the disparity decreased following RCL (95% CI: 1.06, 1.43). 101 These studies suggest improvements in racial disparities for cannabis-related arrests following RCL, although there ware only two studies and they are limited to the U.S.
The aim of this systematic review was to examine the existing literature on the impacts of RCL on a broad range of behavioral and health-related outcomes. The focus on more rigorous study designs permits greater confidence in the conclusions that can be drawn. The literature revealed five main outcomes that have been examined: cannabis use behaviors, cannabis attitudes, health-related outcomes, driving-related outcomes, and crime-related outcomes. The overall synthesizing of the literature revealed heterogenous and complex effects associated with RCL implementation. The varied findings across behavioral and health related outcomes does not give a clear or categorical answer as to whether RCL is a negative or positive policy change overall. Rather, the review reveals that while a great deal of research is accumulating, there remains a need for more definitive findings on the causal role of RCL on a large variety of substance use, health, attitude-related, driving, and crime-related outcomes.
Overall, studies examining cannabis use behavior revealed evidence for cannabis use increases following RCL, particularly for young adults (100%), peri-natal users (66%), and certain clinical populations (66%). 47 , 54 , 59 While general adult samples had some mixed findings, the majority of studies (80%) suggested increasing rates of use associated with RCL. 51 Of note, the increasing cannabis use rates found in peri-natal and clinical populations are particularly concerning as they do suggest increasing rates in more vulnerable samples where potential adverse consequences of cannabis use are more pressing. 103 However, for both groups the overall literature revealed only a few studies and thus requires further examination. Further, a reason to caution current conclusions surround RCL impacts on substance use, is that there is research suggesting cannabis use rates were increasing prior to RCL in Canada. 104 Thus, there still remains a need to better disentangle causal consequences of RCL on cannabis use rates.
In contrast to studies of adults, studies of adolescents pointed to inconsistent evidence of RCL’s influence on cannabis use rates, 38 , 45 with 60% of studies finding no change or inconsistent evidence surrounding adolescent use following RCL. Thus, a key conclusion of the cannabis use literature is that there is not overwhelming evidence that RCL is associated with increasing rates of cannabis among adolescents, which is notable as potential increases in adolescent use is a concern often voiced by critics of RCL. 16 This might suggest that current RCL policies that limit access to minors may be effective. However, a methodological explanation for the discrepancy between findings for adolescents and adults is that adults may be more willing to report their use of cannabis following RCL as it is now legal for them to use. However, for adolescents’ cannabis use remained illicit, which may lead to biased reporting from adolescents. Thus, additional research using methods to overcome limitations of self-reports may be required.
With regard to other substance use, primarily alcohol and cigarettes, there is little evidence that RCL is associated with increased use rates and may even be associated with decreased rates of cigarette use. 42 , 61 The lack of a relationship with RCL and increasing alcohol and other substance use, seen in 60% of studies, is relevant due to concerns of RCL causing “spill-over” effects to substances other than cannabis. However, the decreasing rates on cigarette use associated with RCL seen in 33% of studies may also suggest a substitution effect of cannabis. 105 It is possible that RCL encourages a substitution effect where cannabis is used to replace use other substances such as cigarettes, but 66% of studies found no association of RCL and cigarette use so further research examining a potential substitution effect is needed. In sum, the literature points to a heterogenous impact of RCL on cannabis and other substance use rates, suggesting complex effects of RCL on use rates that may vary across age and population. However, the review also highlights that there are still limited studies examining RCL and other substance use, particularly a lack of multiple studies examining the same age group.
The current evidence for the impact of RCL on attitudes surrounding cannabis revealed mixed or limited results, with 44% studies finding some sort of relationship with attitudes and RCL and 55% studies suggest a lack of or inconsistent relationship. Studies examining cannabis use attitudes or willingness to use revealed conflicting evidence whereas some studies pointed to increased willingness to use associated with RCL, 43 and others found no change or that changes were not specific to regions that implemented RCL. 48 For attitude-related studies that did reveal consistent findings (eg, use motivation changes, perceptions of lower risk and greater benefits of use), the literature was limited in the number of studies or involved heterogenous samples, making it difficult to make conclusive statements surrounding the effect of RCL. As cannabis-related attitudes (eg, perceived risk, intentions to use) can have implications for cannabis use and consequences 106 , 107 it is interesting that current literature does not reveal clear associations of cannabis-related attitudes and RCL. Rather, this review reveals a need for more research examining changes in cannabis-attitudes over time and potential impacts of RCL.
In terms of health outcomes, the empirical literature suggests RCL is associated with increased cannabis-related emergency visits 24 , 67 , 70 , 76 and other health consequences (eg, trauma-related cases 57 ). The literature also suggests there may be other potential negative health consequences associated with RCL, such as increasing adverse birth outcomes and post-mortem cannabis screens. 45 , 89 Synthesizing of the literature points to a well-established relationship of RCL and increasing cannabis-related emergency visits. While some extant literature was mixed, on balance most studies included in the review (70.6%) found consistent evidence of increased emergency service use (eg, emergency department admissions and poison control calls) for both adolescents and adults with only 31% of studies finding mixed or no association with RCL. This points to a need for stricter RCL policies to prevent unintentional consumption or hyperemesis such as promoting safe or lower risk use of cannabis (eg, using lower THC products, avoiding deep inhales while smoking), clearer packaging for cannabis products, and safe storage procedures.
However, the literature on health outcomes outside of emergency service utilization is limited and requires more in-depth evaluations to be fully understood. Additionally, not all health-outcomes indicated negative consequences associated with RCL. There is emerging evidence of the potential of RCL to help decrease CUD and multiple substance hospital admissions 74 , 82 Furthermore, while some findings were mixed and the number of studies limited, 60% of studies found potential for RCL to have protective effects for opioid-related negative consequences. 87 , 88 However, opioid-related findings should be considered in the context of population-level changes in opioid prescriptions and shifting opioid policy influence. 108 Thus, findings may be a result of changes driven by the response to the opioid epidemic rather than RCL, and there remains a need to better disentangle RCL impacts on opioid-related consequences. It is also worth noting that some opioid and cannabis studies are underwritten by the cannabis industry, so the findings should be interpreted with caution due to potential for conflicts of interest. 88 In sum, the overall literature suggests that RCL is associated with both negative and positive health-related consequences and reveals a need to examine the role of RCL across a wide range of health outcomes.
The findings from the driving-related literature do suggest RCL is associated with increased motor vehicle accidents (50% of studies) although the literature was quite evenly split as higher accident rates were not seen across all studies (50% studies). These results point to potential negative consequence associated with RCL and may indicate a need for better measures to prevent driving while under the influence of cannabis in legalized jurisdictions. However, as the evidence was split and predominately in the U.S. additional studies spanning diverse geographical jurisdictions are still needed.
On the other hand, the findings from crime-related outcomes showed some inconsistencies. While one study did suggest minimal decreases for substance-use related arrests in adults, the findings were not consistent across the two studies examining arrest-rates in youth. 100 - 102 These potential decreases in arrest rates for adults can have important implications as cannabis-related crime rates make up a large amount of overall crime statistics and drug-specific arrests. 30 , 31 This discrepancy in youth findings between a U.S. and Canadian study are notable as Canadian RCL policies do include stipulations to allow small scale regulations in youth. Thus, it suggests RCL policies that maintain prohibition of use among underage youth do not address issues related to arrests and crime among youth. In fact, the current literature suggests that cannabis-related charges are still being enforced for youth under the legal age of consumption in the U.S. Another important outcome revealed is racial disparities in cannabis-related arrests. Previous evidence has shown there are racial disparities, particularly between Black, Indigenous, and Hispanic individuals compared to White counterparts, in cannabis-related charges and arrests. 109 , 110 Regarding racial disparities and RCL, there was very little evidence of decreases in disparities for cannabis-related arrests following RCL. 100 , 101 This racialized arresting is significant as it can be associated with additional public health concerns such as physical and mental health outcomes, harm to families involved, and to communities. 111 This finding is particularly concerning as it suggests racialized arrests for cannabis are still occurring despite the intentions of liberalization of cannabis policies to help reduce racial disparities in the criminal justice system. However, it is important to note that there were only 2 studies of racial disparities in cannabis-related arrests and both were conducted in the U.S. Thus, additional research is required before drawing any firm conclusions about the ability of RCL to address systemic issues in the justice system.
Limitations
The findings should be considered within context of the following limitations. The research was predominately from North America (U.S. and Canada). While both countries have either federal or state RCL, findings only from two countries that are geographically connected may not reflect the influence of RCL across different cultures and countries globally. The majority of studies also relied on self-report data for cannabis-related outcomes. Thus, there is a risk that any increases in use or other cannabis-related outcomes may be due to an increased comfort in disclosing cannabis use due to RCL.
Given the large number of studies on multiple outcomes, we chose to focus on implementation of RCL exclusively, rather than related policy changes such as commercialization (ie, the advent of legal sales), to allow for clearer conclusions about the specific impacts on RCL. However, a limitation is that the review does not address the impact of commercialization or changes in product availability. While outside the scope of the current review, it does limit the conclusions that can be drawn about RCL overall as some jurisdictions implemented features of commercialization separately from legalization. For example, in Ontario, Canada, storefronts and edible products became legal a year after initial RCL (when online purchase was the exclusive modality), which may have had an additional impact on behavioral and health-related outcomes. Additionally, the scope of the review was limited to recreational legalization and did not consider other forms of policy changes such as medicinal legalization or decriminalization, as these have been summarized more comprehensively in prior reviews. 112 - 114 Further, this review focused on behavioral and health outcomes; other important outcomes to examine in the future include economic aspects such as cannabis pricing and purchasing behaviors, and product features such as potency. Finally, as this review considered a broad range of outcomes, we did not conduct a meta-analysis which limits conclusions that can be drawn regarding the magnitude of the associations.
Conclusions
The topic of RCL is a contentious and timely issue. With nationwide legalization in multiple countries and liberalizing policies across the U.S., empirical research on the impacts of RCL has dramatically expanded in recent years. This systematic review comprehensively evaluated a variety of outcomes associated with RCL, focusing on longitudinal study designs and revealing a wide variety of findings in terms of substance use, health, cannabis attitudes, crime, and driving outcomes examined thus far. However, the current review highlights that the findings regarding the effects of RCL are highly heterogenous, often inconsistent, and disproportionately focused on certain jurisdictions. With polarizing views surrounding whether RCL is a positive or negative policy change, it is noteworthy that the extant literature does not point to one clear answer at the current time. In general, the collective results do not suggest dramatic changes or negative consequences, but instead suggest that meaningful tectonic shifts are happening for several outcomes that may or may not presage substantive changes in personal and public health risk. Furthermore, it is clear that a more in-depth examinations of negative (eg, frequent use, CUD prevalence, ‘gateway’ relationships with other substance use), or positive consequences (eg, therapeutic benefits for mental health and/or medical conditions, use of safer products and routes of administration), are needed using both quantitative and qualitative approaches.
Acknowledgments
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding support from the Peter Boris Chair in Addictions Research and a Canada Research Chair in Translational Addiction Research (JM). Funders had no role in the design or execution of the review.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: James MacKillop discloses he is a principal and senior scientist in Beam Diagnostics, Inc, and a consultant to ClairvoyantRx. No other authors have disclosures.
Author Contributions: The author’s contribution is as follows: study conceptualization and design: KF, JW, JT, JM; data collection and interpretation: KF, EM, MS; manuscript writing and preparation: KF, EM, MS, PN; manuscript reviewing and editing: JW, JT, JM. All authors have reviewed and approved the final manuscript.
- Research article
- Open access
- Published: 04 February 2020
Marijuana legalization and historical trends in marijuana use among US residents aged 12–25: results from the 1979–2016 National Survey on drug use and health
- Xinguang Chen 1 ,
- Xiangfan Chen 2 &
- Hong Yan 2
BMC Public Health volume 20 , Article number: 156 ( 2020 ) Cite this article
106k Accesses
69 Citations
83 Altmetric
Metrics details
Marijuana is the most commonly used illicit drug in the United States. More and more states legalized medical and recreational marijuana use. Adolescents and emerging adults are at high risk for marijuana use. This ecological study aims to examine historical trends in marijuana use among youth along with marijuana legalization.
Data ( n = 749,152) were from the 31-wave National Survey on Drug Use and Health (NSDUH), 1979–2016. Current marijuana use, if use marijuana in the past 30 days, was used as outcome variable. Age was measured as the chronological age self-reported by the participants, period was the year when the survey was conducted, and cohort was estimated as period subtracted age. Rate of current marijuana use was decomposed into independent age, period and cohort effects using the hierarchical age-period-cohort (HAPC) model.
After controlling for age, cohort and other covariates, the estimated period effect indicated declines in marijuana use in 1979–1992 and 2001–2006, and increases in 1992–2001 and 2006–2016. The period effect was positively and significantly associated with the proportion of people covered by Medical Marijuana Laws (MML) (correlation coefficients: 0.89 for total sample, 0.81 for males and 0.93 for females, all three p values < 0.01), but was not significantly associated with the Recreational Marijuana Laws (RML). The estimated cohort effect showed a historical decline in marijuana use in those who were born in 1954–1972, a sudden increase in 1972–1984, followed by a decline in 1984–2003.
The model derived trends in marijuana use were coincident with the laws and regulations on marijuana and other drugs in the United States since the 1950s. With more states legalizing marijuana use in the United States, emphasizing responsible use would be essential to protect youth from using marijuana.
Peer Review reports
Introduction
Marijuana use and laws in the united states.
Marijuana is one of the most commonly used drugs in the United States (US) [ 1 ]. In 2015, 8.3% of the US population aged 12 years and older used marijuana in the past month; 16.4% of adolescents aged 12–17 years used in lifetime and 7.0% used in the past month [ 2 ]. The effects of marijuana on a person’s health are mixed. Despite potential benefits (e.g., relieve pain) [ 3 ], using marijuana is associated with a number of adverse effects, particularly among adolescents. Typical adverse effects include impaired short-term memory, cognitive impairment, diminished life satisfaction, and increased risk of using other substances [ 4 ].
Since 1937 when the Marijuana Tax Act was issued, a series of federal laws have been subsequently enacted to regulate marijuana use, including the Boggs Act (1952), Narcotics Control Act (1956), Controlled Substance Act (1970), and Anti-Drug Abuse Act (1986) [ 5 , 6 ]. These laws regulated the sale, possession, use, and cultivation of marijuana [ 6 ]. For example, the Boggs Act increased the punishment of marijuana possession, and the Controlled Substance Act categorized the marijuana into the Schedule I Drugs which have a high potential for abuse, no medical use, and not safe to use without medical supervision [ 5 , 6 ]. These federal laws may have contributed to changes in the historical trend of marijuana use among youth.
Movements to decriminalize and legalize marijuana use
Starting in the late 1960s, marijuana decriminalization became a movement, advocating reformation of federal laws regulating marijuana [ 7 ]. As a result, 11 US states had taken measures to decriminalize marijuana use by reducing the penalty of possession of small amount of marijuana [ 7 ].
The legalization of marijuana started in 1993 when Surgeon General Elder proposed to study marijuana legalization [ 8 ]. California was the first state that passed Medical Marijuana Laws (MML) in 1996 [ 9 ]. After California, more and more states established laws permitting marijuana use for medical and/or recreational purposes. To date, 33 states and the District of Columbia have established MML, including 11 states with recreational marijuana laws (RML) [ 9 ]. Compared with the legalization of marijuana use in the European countries which were more divided that many of them have medical marijuana registered as a treatment option with few having legalized recreational use [ 10 , 11 , 12 , 13 ], the legalization of marijuana in the US were more mixed with 11 states legalized medical and recreational use consecutively, such as California, Nevada, Washington, etc. These state laws may alter people’s attitudes and behaviors, finally may lead to the increased risk of marijuana use, particularly among young people [ 13 ]. Reported studies indicate that state marijuana laws were associated with increases in acceptance of and accessibility to marijuana, declines in perceived harm, and formation of new norms supporting marijuana use [ 14 ].
Marijuana harm to adolescents and young adults
Adolescents and young adults constitute a large proportion of the US population. Data from the US Census Bureau indicate that approximately 60 million of the US population are in the 12–25 years age range [ 15 ]. These people are vulnerable to drugs, including marijuana [ 16 ]. Marijuana is more prevalent among people in this age range than in other ages [ 17 ]. One well-known factor for explaining the marijuana use among people in this age range is the theory of imbalanced cognitive and physical development [ 4 ]. The delayed brain development of youth reduces their capability to cognitively process social, emotional and incentive events against risk behaviors, such as marijuana use [ 18 ]. Understanding the impact of marijuana laws on marijuana use among this population with a historical perspective is of great legal, social and public health significance.
Inconsistent results regarding the impact of marijuana laws on marijuana use
A number of studies have examined the impact of marijuana laws on marijuana use across the world, but reported inconsistent results [ 13 ]. Some studies reported no association between marijuana laws and marijuana use [ 14 , 19 , 20 , 21 , 22 , 23 , 24 , 25 ], some reported a protective effect of the laws against marijuana use [ 24 , 26 ], some reported mixed effects [ 27 , 28 ], while some others reported a risk effect that marijuana laws increased marijuana use [ 29 , 30 ]. Despite much information, our review of these reported studies revealed several limitations. First of all, these studies often targeted a short time span, ignoring the long period trend before marijuana legalization. Despite the fact that marijuana laws enact in a specific year, the process of legalization often lasts for several years. Individuals may have already changed their attitudes and behaviors before the year when the law is enacted. Therefore, it may not be valid when comparing marijuana use before and after the year at a single time point when the law is enacted and ignoring the secular historical trend [ 19 , 30 , 31 ]. Second, many studies adapted the difference-in-difference analytical approach designated for analyzing randomized controlled trials. No US state is randomized to legalize the marijuana laws, and no state can be established as controls. Thus, the impact of laws cannot be efficiently detected using this approach. Third, since marijuana legalization is a public process, and the information of marijuana legalization in one state can be easily spread to states without the marijuana laws. The information diffusion cannot be ruled out, reducing the validity of the non-marijuana law states as the controls to compare the between-state differences [ 31 ].
Alternatively, evidence derived based on a historical perspective may provide new information regarding the impact of laws and regulations on marijuana use, including state marijuana laws in the past two decades. Marijuana users may stop using to comply with the laws/regulations, while non-marijuana users may start to use if marijuana is legal. Data from several studies with national data since 1996 demonstrate that attitudes, beliefs, perceptions, and use of marijuana among people in the US were associated with state marijuana laws [ 29 , 32 ].
Age-period-cohort modeling: looking into the past with recent data
To investigate historical trends over a long period, including the time period with no data, we can use the classic age-period-cohort modeling (APC) approach. The APC model can successfully discompose the rate or prevalence of marijuana use into independent age, period and cohort effects [ 33 , 34 ]. Age effect refers to the risk associated with the aging process, including the biological and social accumulation process. Period effect is risk associated with the external environmental events in specific years that exert effect on all age groups, representing the unbiased historical trend of marijuana use which controlling for the influences from age and birth cohort. Cohort effect refers to the risk associated with the specific year of birth. A typical example is that people born in 2011 in Fukushima, Japan may have greater risk of cancer due to the nuclear disaster [ 35 ], so a person aged 80 in 2091 contains the information of cancer risk in 2011 when he/she was born. Similarly, a participant aged 25 in 1979 contains information on the risk of marijuana use 25 years ago in 1954 when that person was born. With this method, we can describe historical trends of marijuana use using information stored by participants in older ages [ 33 ]. The estimated period and cohort effects can be used to present the unbiased historical trend of specific topics, including marijuana use [ 34 , 36 , 37 , 38 ]. Furthermore, the newly established hierarchical APC (HAPC) modeling is capable of analyzing individual-level data to provide more precise measures of historical trends [ 33 ]. The HAPC model has been used in various fields, including social and behavioral science, and public health [ 39 , 40 ].
Several studies have investigated marijuana use with APC modeling method [ 17 , 41 , 42 ]. However, these studies covered only a small portion of the decades with state marijuana legalization [ 17 , 42 ]. For example, the study conducted by Miech and colleagues only covered periods from 1985 to 2009 [ 17 ]. Among these studies, one focused on a longer state marijuana legalization period, but did not provide detailed information regarding the impact of marijuana laws because the survey was every 5 years and researchers used a large 5-year age group which leads to a wide 10-year birth cohort. The averaging of the cohort effects in 10 years could reduce the capability of detecting sensitive changes of marijuana use corresponding to the historical events [ 41 ].
Purpose of the study
In this study, we examined the historical trends in marijuana use among youth using HAPC modeling to obtain the period and cohort effects. These two effects provide unbiased and independent information to characterize historical trends in marijuana use after controlling for age and other covariates. We conceptually linked the model-derived time trends to both federal and state laws/regulations regarding marijuana and other drug use in 1954–2016. The ultimate goal is to provide evidence informing federal and state legislation and public health decision-making to promote responsible marijuana use and to protect young people from marijuana use-related adverse consequences.
Materials and methods
Data sources and study population.
Data were derived from 31 waves of National Survey on Drug Use and Health (NSDUH), 1979–2016. NSDUH is a multi-year cross-sectional survey program sponsored by the Substance Abuse and Mental Health Services Administration. The survey was conducted every 3 years before 1990, and annually thereafter. The aim is to provide data on the use of tobacco, alcohol, illicit drug and mental health among the US population.
Survey participants were noninstitutionalized US civilians 12 years of age and older. Participants were recruited by NSDUH using a multi-stage clustered random sampling method. Several changes were made to the NSDUH after its establishment [ 43 ]. First, the name of the survey was changed from the National Household Survey on Drug Abuse (NHSDA) to NSDUH in 2002. Second, starting in 2002, adolescent participants receive $30 as incentives to improve the response rate. Third, survey mode was changed from personal interviews with self-enumerated answer sheets (before 1999) to the computer-assisted person interviews (CAPI) and audio computer-assisted self-interviews (ACASI) (since 1999). These changes may confound the historical trends [ 43 ], thus we used two dummy variables as covariates, one for the survey mode change in 1999 and another for the survey method change in 2002 to control for potential confounding effect.
Data acquisition
Data were downloaded from the designated website ( https://nsduhweb.rti.org/respweb/homepage.cfm ). A database was used to store and merge the data by year for analysis. Among all participants, data for those aged 12–25 years ( n = 749,152) were included. We excluded participants aged 26 and older because the public data did not provide information on single or two-year age that was needed for HAPC modeling (details see statistical analysis section). We obtained approval from the Institutional Review Board at the University of Florida to conduct this study.
Variables and measurements
Current marijuana use: the dependent variable. Participants were defined as current marijuana users if they reported marijuana use within the past 30 days. We used the variable harmonization method to create a comparable measure across 31-wave NSDUH data [ 44 ]. Slightly different questions were used in NSDUH. In 1979–1993, participants were asked: “When was the most recent time that you used marijuana or hash?” Starting in 1994, the question was changed to “How long has it been since you last used marijuana or hashish?” To harmonize the marijuana use variable, participants were coded as current marijuana users if their response to the question indicated the last time to use marijuana was within past 30 days.
Chronological age, time period and birth cohort were the predictors. (1) Chronological age in years was measured with participants’ age at the survey. APC modeling requires the same age measure for all participants [ 33 ]. Since no data by single-year age were available for participants older than 21, we grouped all participants into two-year age groups. A total of 7 age groups, 12–13, ..., 24–25 were used. (2) Time period was measured with the year when the survey was conducted, including 1979, 1982, 1985, 1988, 1990, 1991... 2016. (3). Birth cohort was the year of birth, and it was measured by subtracting age from the survey year.
The proportion of people covered by MML: This variable was created by dividing the population in all states with MML over the total US population. The proportion was computed by year from 1996 when California first passed the MML to 2016 when a total of 29 states legalized medical marijuana use. The estimated proportion ranged from 12% in 1996 to 61% in 2016. The proportion of people covered by RML: This variable was derived by dividing the population in all states with RML with the total US population. The estimated proportion ranged from 4% in 2012 to 21% in 2016. These two variables were used to quantitatively assess the relationships between marijuana laws and changes in the risk of marijuana use.
Covariates: Demographic variables gender (male/female) and race/ethnicity (White, Black, Hispanic and others) were used to describe the study sample.
Statistical analysis
We estimated the prevalence of current marijuana use by year using the survey estimation method, considering the complex multi-stage cluster random sampling design and unequal probability. A prevalence rate is not a simple indicator, but consisting of the impact of chronological age, time period and birth cohort, named as age, period and cohort effects, respectively. Thus, it is biased if a prevalence rate is directly used to depict the historical trend. HAPC modeling is an epidemiological method capable of decomposing prevalence rate into mutually independent age, period and cohort effects with individual-level data, while the estimated period and cohort effects provide an unbiased measure of historical trend controlling for the effects of age and other covariates. In this study, we analyzed the data using the two-level HAPC cross-classified random-effects model (CCREM) [ 36 ]:
Where M ijk represents the rate of marijuana use for participants in age group i (12–13, 14,15...), period j (1979, 1982,...) and birth cohort k (1954–55, 1956–57...); parameter α i (age effect) was modeled as the fixed effect; and parameters β j (period effect) and γ k (cohort effect) were modeled as random effects; and β m was used to control m covariates, including the two dummy variables assessing changes made to the NSDUH in 1999 and 2002, respectively.
The HAPC modeling analysis was executed using the PROC GLIMMIX. Sample weights were included to obtain results representing the total US population aged 12–25. A ridge-stabilized Newton-Raphson algorithm was used for parameter estimation. Modeling analysis was conducted for the overall sample, stratified by gender. The estimated age effect α i , period β j and cohort γ k (i.e., the log-linear regression coefficients) were directly plotted to visualize the pattern of change.
To gain insight into the relationship between legal events and regulations at the national level, we listed these events/regulations along with the estimated time trends in the risk of marijuana from HAPC modeling. To provide a quantitative measure, we associated the estimated period effect with the proportions of US population living with MML and RML using Pearson correlation. All statistical analyses for this study were conducted using the software SAS, version 9.4 (SAS Institute Inc., Cary, NC).
Sample characteristics
Data for a total of 749,152 participants (12–25 years old) from all 31-wave NSDUH covering a 38-year period were analyzed. Among the total sample (Table 1 ), 48.96% were male and 58.78% were White, 14.84% Black, and 18.40% Hispanic.
Prevalence rate of current marijuana use
As shown in Fig. 1 , the estimated prevalence rates of current marijuana use from 1979 to 2016 show a “V” shaped pattern. The rate was 27.57% in 1979, it declined to 8.02% in 1992, followed by a gradual increase to 14.70% by 2016. The pattern was the same for both male and female with males more likely to use than females during the whole period.
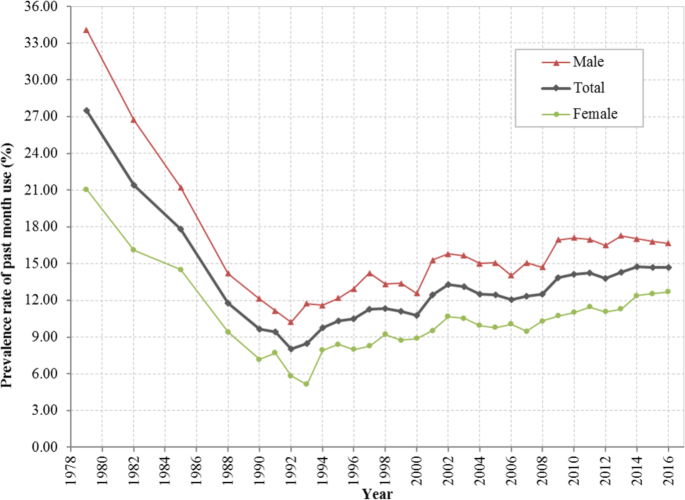
Prevalence rate (%) of current marijuana use among US residents 12 to 25 years of age during 1979–2016, overall and stratified by gender. Derived from data from the 1979–2016 National Survey on Drug Use and Health (NSDUH)
HAPC modeling and results
Estimated age effects α i from the CCREM [ 1 ] for current marijuana use are presented in Fig. 2 . The risk by age shows a 2-phase pattern –a rapid increase phase from ages 12 to 19, followed by a gradually declining phase. The pattern was persistent for the overall sample and for both male and female subsamples.
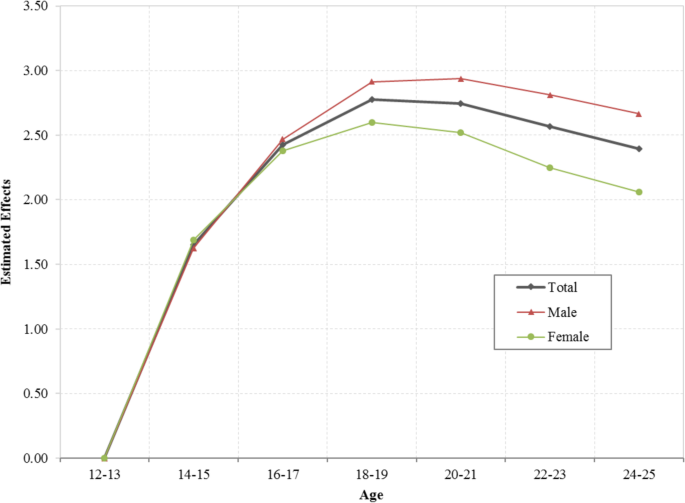
Age effect for the risk of current marijuana use, overall and stratified by male and female, estimated with hierarchical age-period-cohort modeling method with 31 waves of NSDUH data during 1979–2016. Age effect α i were log-linear regression coefficients estimated using CCREM (1), see text for more details
The estimated period effects β j from the CCREM [ 1 ] are presented in Fig. 3 . The period effect reflects the risk of current marijuana use due to significant events occurring over the period, particularly federal and state laws and regulations. After controlling for the impacts of age, cohort and other covariates, the estimated period effect indicates that the risk of current marijuana use had two declining trends (1979–1992 and 2001–2006), and two increasing trends (1992–2001 and 2006–2016). Epidemiologically, the time trends characterized by the estimated period effects in Fig. 3 are more valid than the prevalence rates presented in Fig. 1 because the former was adjusted for confounders while the later was not.
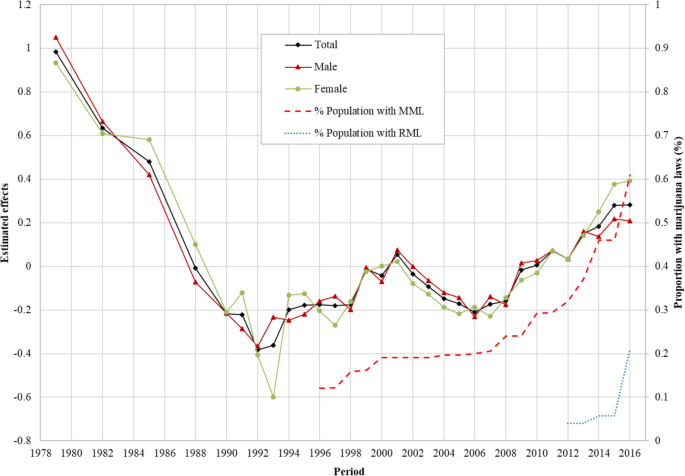
Period effect for the risk of marijuana use for US adolescents and young adults, overall and by male/female estimated with hierarchical age-period-cohort modeling method and its correlation with the proportion of US population covered by Medical Marijuana Laws and Recreational Marijuana Laws. Period effect β j were log-linear regression coefficients estimated using CCREM (1), see text for more details
Correlation of the period effect with proportions of the population covered by marijuana laws: The Pearson correlation coefficient of the period effect with the proportions of US population covered by MML during 1996–2016 was 0.89 for the total sample, 0.81 for male and 0.93 for female, respectively ( p < 0.01 for all). The correlation between period effect and proportion of US population covered by RML was 0.64 for the total sample, 0.59 for male and 0.49 for female ( p > 0.05 for all).
Likewise, the estimated cohort effects γ k from the CCREM [ 1 ] are presented in Fig. 4 . The cohort effect reflects changes in the risk of current marijuana use over the period indicated by the year of birth of the survey participants after the impacts of age, period and other covariates are adjusted. Results in the figure show three distinctive cohorts with different risk patterns of current marijuana use during 1954–2003: (1) the Historical Declining Cohort (HDC): those born in 1954–1972, and characterized by a gradual and linear declining trend with some fluctuations; (2) the Sudden Increase Cohort (SIC): those born from 1972 to 1984, characterized with a rapid almost linear increasing trend; and (3) the Contemporary Declining Cohort (CDC): those born during 1984 and 2003, and characterized with a progressive declining over time. The detailed results of HAPC modeling analysis were also shown in Additional file 1 : Table S1.

Cohort effect for the risk of marijuana use among US adolescents and young adults born during 1954–2003, overall and by male/female, estimated with hierarchical age-period-cohort modeling method. Cohort effect γ k were log-linear regression coefficients estimated using CCREM (1), see text for more details
This study provides new data regarding the risk of marijuana use in youth in the US during 1954–2016. This is a period in the US history with substantial increases and declines in drug use, including marijuana; accompanied with many ups and downs in legal actions against drug use since the 1970s and progressive marijuana legalization at the state level from the later 1990s till today (see Additional file 1 : Table S2). Findings of the study indicate four-phase period effect and three-phase cohort effect, corresponding to various historical events of marijuana laws, regulations and social movements.
Coincident relationship between the period effect and legal drug control
The period effect derived from the HAPC model provides a net effect of the impact of time on marijuana use after the impact of age and birth cohort were adjusted. Findings in this study indicate that there was a progressive decline in the period effect during 1979 and 1992. This trend was corresponding to a period with the strongest legal actions at the national level, the War on Drugs by President Nixon (1969–1974) President Reagan (1981–1989) [ 45 ], and President Bush (1989) [ 45 ],and the Anti-Drug Abuse Act (1986) [ 5 ].
The estimated period effect shows an increasing trend in 1992–2001. During this period, President Clinton advocated for the use of treatment to replace incarceration (1992) [ 45 ], Surgeon General Elders proposed to study marijuana legalization (1993–1994) [ 8 ], President Clinton’s position of the need to re-examine the entire policy against people who use drugs, and decriminalization of marijuana (2000) [ 45 ] and the passage of MML in eight US states.
The estimated period effect shows a declining trend in 2001–2006. Important laws/regulations include the Student Drug Testing Program promoted by President Bush, and the broadened the public schools’ authority to test illegal drugs among students given by the US Supreme Court (2002) [ 46 ].
The estimated period effect increases in 2006–2016. This is the period when the proportion of the population covered by MML progressively increased. This relation was further proved by a positive correlation between the estimated period effect and the proportion of the population covered by MML. In addition, several other events occurred. For example, over 500 economists wrote an open letter to President Bush, Congress and Governors of the US and called for marijuana legalization (2005) [ 47 ], and President Obama ended the federal interference with the state MML, treated marijuana as public health issues, and avoided using the term of “War on Drugs” [ 45 ]. The study also indicates that the proportion of population covered by RML was positively associated with the period effect although not significant which may be due to the limited number of data points of RML. Future studies may follow up to investigate the relationship between RML and rate of marijuana use.
Coincident relationship between the cohort effect and legal drug control
Cohort effect is the risk of marijuana use associated with the specific year of birth. People born in different years are exposed to different laws, regulations in the past, therefore, the risk of marijuana use for people may differ when they enter adolescence and adulthood. Findings in this study indicate three distinctive cohorts: HDC (1954–1972), SIC (1972–1984) and CDC (1984–2003). During HDC, the overall level of marijuana use was declining. Various laws/regulations of drug use in general and marijuana in particular may explain the declining trend. First, multiple laws passed to regulate the marijuana and other substance use before and during this period remained in effect, for example, the Marijuana Tax Act (1937), the Boggs Act (1952), the Narcotics Control Act (1956) and the Controlled Substance Act (1970). Secondly, the formation of government departments focusing on drug use prevention and control may contribute to the cohort effect, such as the Bureau of Narcotics and Dangerous Drugs (1968) [ 48 ]. People born during this period may be exposed to the macro environment with laws and regulations against marijuana, thus, they may be less likely to use marijuana.
Compared to people born before 1972, the cohort effect for participants born during 1972 and 1984 was in coincidence with the increased risk of using marijuana shown as SIC. This trend was accompanied by the state and federal movements for marijuana use, which may alter the social environment and public attitudes and beliefs from prohibitive to acceptive. For example, seven states passed laws to decriminalize the marijuana use and reduced the penalty for personal possession of small amount of marijuana in 1976 [ 7 ]. Four more states joined the movement in two subsequent years [ 7 ]. People born during this period may have experienced tolerated environment of marijuana, and they may become more acceptable of marijuana use, increasing their likelihood of using marijuana.
A declining cohort CDC appeared immediately after 1984 and extended to 2003. This declining cohort effect was corresponding to a number of laws, regulations and movements prohibiting drug use. Typical examples included the War on Drugs initiated by President Nixon (1980s), the expansion of the drug war by President Reagan (1980s), the highly-publicized anti-drug campaign “Just Say No” by First Lady Nancy Reagan (early 1980s) [ 45 ], and the Zero Tolerance Policies in mid-to-late 1980s [ 45 ], the Anti-Drug Abuse Act (1986) [ 5 ], the nationally televised speech of War on Drugs declared by President Bush in 1989 and the escalated War on Drugs by President Clinton (1993–2001) [ 45 ]. Meanwhile many activities of the federal government and social groups may also influence the social environment of using marijuana. For example, the Federal government opposed to legalize the cultivation of industrial hemp, and Federal agents shut down marijuana sales club in San Francisco in 1998 [ 48 ]. Individuals born in these years grew up in an environment against marijuana use which may decrease their likelihood of using marijuana when they enter adolescence and young adulthood.
This study applied the age-period-cohort model to investigate the independent age, period and cohort effects, and indicated that the model derived trends in marijuana use among adolescents and young adults were coincident with the laws and regulations on marijuana use in the United States since the 1950s. With more states legalizing marijuana use in the United States, emphasizing responsible use would be essential to protect youth from using marijuana.
Limitations
This study has limitations. First, study data were collected through a household survey, which is subject to underreporting. Second, no causal relationship can be warranted using cross-sectional data, and further studies are needed to verify the association between the specific laws/regulation and the risk of marijuana use. Third, data were available to measure single-year age up to age 21 and two-year age group up to 25, preventing researchers from examining the risk of marijuana use for participants in other ages. Lastly, data derived from NSDUH were nation-wide, and future studies are needed to analyze state-level data and investigate the between-state differences. Although a systematic review of all laws and regulations related to marijuana and other drugs is beyond the scope of this study, findings from our study provide new data from a historical perspective much needed for the current trend in marijuana legalization across the nation to get the benefit from marijuana while to protect vulnerable children and youth in the US. It provides an opportunity for stack-holders to make public decisions by reviewing the findings of this analysis together with the laws and regulations at the federal and state levels over a long period since the 1950s.
Availability of data and materials
The data of the study are available from the designated repository ( https://nsduhweb.rti.org/respweb/homepage.cfm ).
Abbreviations
Audio computer-assisted self-interviews
Age-period-cohort modeling
Computer-assisted person interviews
Cross-classified random-effects model
Contemporary Declining Cohort
Hierarchical age-period-cohort
Historical Declining Cohort
Medical Marijuana Laws
National Household Survey on Drug Abuse
National Survey on Drug Use and Health
Recreational Marijuana Laws
Sudden Increase Cohort
The United States
CDC. Marijuana and Public Health. 2017. Available from: https://www.cdc.gov/marijuana/index.htm . Accessed 13 June 2018.
SAMHSA. Results from the 2015 National Survey on Drug Use and Health: Detailed Tables. 2016 [cited 2018 Jan 31]. Available from: https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.htm
Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda, Board on Population Health and Public Health Practice, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. Washington, D.C.: National Academies Press; 2017.
Collins C. Adverse health effects of marijuana use. N Engl J Med. 2014;371(9):879.
PubMed Google Scholar
Belenko SR. Drugs and drug policy in America: a documentary history. Westport: Greenwood Press; 2000.
Google Scholar
Gerber RJ. Legalizing marijuana: Drug policy reform and prohibition politics. Westport: Praeger; 2004.
Single EW. The impact of marijuana decriminalization: an update. J Public Health Policy. 1989:456–66.
Article CAS Google Scholar
SFChronicle. Ex-surgeon general backed legalizing marijuana before it was cool [Internet]. 2016 [cited 2018 Oct 7]. Available from: https://www.sfchronicle.com/business/article/Ex-surgeon-general-backed-legalizing-marijuana-6799348.php
PROCON. 31 Legal Medical Marijuana States and DC. 2018 [cited 2018 Oct 4]. Available from: https://medicalmarijuana.procon.org/view.resource.php?resourceID=000881
Bifulco M, Pisanti S. Medicinal use of cannabis in Europe: the fact that more countries legalize the medicinal use of cannabis should not become an argument for unfettered and uncontrolled use. EMBO Rep. 2015;16(2):130–2.
European Monitoring Centre for Drugs and Drug Addiction. Models for the legal supply of cannabis: recent developments (Perspectives on drugs). 2016. Available from: http://www.emcdda.europa.eu/publications/pods/legal-supply-of-cannabis . Accessed 10 Jan 2020.
European Monitoring Centre for Drugs and Drug Addiction. Cannabis policy: status and recent developments. 2017. Available from: http://www.emcdda.europa.eu/topics/cannabis-policy_en#section2 . Accessed 10 Jan 2020.
Hughes B, Matias J, Griffiths P. Inconsistencies in the assumptions linking punitive sanctions and use of cannabis and new psychoactive substances in Europe. Addiction. 2018;113(12):2155–7.
Article Google Scholar
Anderson DM, Hansen B, Rees DI. Medical marijuana laws and teen marijuana use. Am Law Econ Rev. 2015;17(2):495-28.
United States Census Bureau. Annual Estimates of the Resident Population by Single Year of Age and Sex for the United States, States, and Puerto Rico Commonwealth: April 1, 2010 to July 1, 2016 2016 Population Estimates. 2017 [cited 2018 Mar 14]. Available from: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk
Chen X, Yu B, Lasopa S, Cottler LB. Current patterns of marijuana use initiation by age among US adolescents and emerging adults: implications for intervention. Am J Drug Alcohol Abuse. 2017;43(3):261–70.
Miech R, Koester S. Trends in U.S., past-year marijuana use from 1985 to 2009: an age-period-cohort analysis. Drug Alcohol Depend. 2012;124(3):259–67.
Steinberg L. The influence of neuroscience on US supreme court decisions about adolescents’ criminal culpability. Nat Rev Neurosci. 2013;14(7):513–8.
Sarvet AL, Wall MM, Fink DS, Greene E, Le A, Boustead AE, et al. Medical marijuana laws and adolescent marijuana use in the United States: a systematic review and meta-analysis. Addiction. 2018;113(6):1003–16.
Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O’Malley PM, et al. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry. 2015;2(7):601–8.
Pacula RL, Chriqui JF, King J. Marijuana decriminalization: what does it mean in the United States? National Bureau of Economic Research; 2003.
Donnelly N, Hall W, Christie P. The effects of the Cannabis expiation notice system on the prevalence of cannabis use in South Australia: evidence from the National Drug Strategy Household Surveys 1985-95. Drug Alcohol Rev. 2000;19(3):265–9.
Gorman DM, Huber JC. Do medical cannabis laws encourage cannabis use? Int J Drug Policy. 2007;18(3):160–7.
Lynne-Landsman SD, Livingston MD, Wagenaar AC. Effects of state medical marijuana laws on adolescent marijuana use. Am J Public Health. 2013 Aug;103(8):1500–6.
Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical marijuana laws on marijuana and alcohol use: the devil is in the details. National Bureau of Economic Research; 2013.
Harper S, Strumpf EC, Kaufman JS. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann Epidemiol. 2012;22(3):207–12.
Stolzenberg L, D’Alessio SJ, Dariano D. The effect of medical cannabis laws on juvenile cannabis use. Int J Drug Policy. 2016;27:82–8.
Wang GS, Roosevelt G, Heard K. Pediatric marijuana exposures in a medical marijuana state. JAMA Pediatr. 2013;167(7):630–3.
Wall MM, Poh E, Cerdá M, Keyes KM, Galea S, Hasin DS. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21(9):714–6.
Chen X, Yu B, Stanton B, Cook RL, Chen D-GD, Okafor C. Medical marijuana laws and marijuana use among U.S. adolescents: evidence from michigan youth risk behavior surveillance data. J Drug Educ. 2018;47237918803361.
Chen X. Information diffusion in the evaluation of medical marijuana laws’ impact on risk perception and use. Am J Public Health. 2016;106(12):e8.
Chen X, Yu B, Stanton B, Cook RL, Chen DG, Okafor C. Medical marijuana laws and marijuana use among US adolescents: Evidence from Michigan youth risk behavior surveillance data. J Drug Educ. 2018;48(1-2):18-35.
Yang Y, Land K. Age-Period-Cohort Analysis: New Models, Methods, and Empirical Applications. Boca Raton: Chapman and Hall/CRC; 2013.
Yu B, Chen X. Age and birth cohort-adjusted rates of suicide mortality among US male and female youths aged 10 to 19 years from 1999 to 2017. JAMA Netw Open. 2019;2(9):e1911383.
Akiba S. Epidemiological studies of Fukushima residents exposed to ionising radiation from the Fukushima Daiichi nuclear power plant prefecture--a preliminary review of current plans. J Radiol Prot. 2012;32(1):1–10.
Yang Y, Land KC. Age-period-cohort analysis of repeated cross-section surveys: fixed or random effects? Sociol Methods Res. 2008;36(3):297–326.
O’Brien R. Age-period-cohort models: approaches and analyses with aggregate data. Boca Raton: Chapman and Hall/CRC; 2014.
Book Google Scholar
Chen X, Sun Y, Li Z, Yu B, Gao G, Wang P. Historical trends in suicide risk for the residents of mainland China: APC modeling of the archived national suicide mortality rates during 1987-2012. Soc Psychiatry Psychiatr Epidemiol. 2018;54(1):99–110.
Yang Y. Social inequalities in happiness in the United States, 1972 to 2004: an age-period-cohort analysis. Am Sociol Rev. 2008;73(2):204–26.
Reither EN, Hauser RM, Yang Y. Do birth cohorts matter? Age-period-cohort analyses of the obesity epidemic in the United States. Soc Sci Med. 2009;69(10):1439–48.
Kerr WC, Lui C, Ye Y. Trends and age, period and cohort effects for marijuana use prevalence in the 1984-2015 US National Alcohol Surveys. Addiction. 2018;113(3):473–81.
Johnson RA, Gerstein DR. Age, period, and cohort effects in marijuana and alcohol incidence: United States females and males, 1961-1990. Substance Use Misuse. 2000;35(6–8):925–48.
Substance Abuse and Mental Health Services Administration. Results from the 2013 NSDUH: Summary of National Findings, SAMHSA, CBHSQ. 2014 [cited 2018 Sep 23]. Available from: https://www.samhsa.gov/data/sites/default/files/NSDUHresultsPDFWHTML2013/Web/NSDUHresults2013.htm
Bauer DJ, Hussong AM. Psychometric approaches for developing commensurate measures across independent studies: traditional and new models. Psychol Methods. 2009;14(2):101–25.
Drug Policy Alliance. A Brief History of the Drug War. 2018 [cited 2018 Sep 27]. Available from: http://www.drugpolicy.org/issues/brief-history-drug-war
NIDA. Drug testing in schools. 2017 [cited 2018 Sep 27]. Available from: https://www.drugabuse.gov/related-topics/drug-testing/faq-drug-testing-in-schools
Wikipedia contributors. Legal history of cannabis in the United States. 2015. Available from: https://en.wikipedia.org/w/index.php?title=Legal_history_of_cannabis_in_the_United_States&oldid=674767854 . Accessed 24 Oct 2017.
NORML. Marijuana law reform timeline. 2015. Available from: http://norml.org/shop/item/marijuana-law-reform-timeline . Accessed 24 Oct 2017.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Department of Epidemiology, University of Florida, Gainesville, FL, 32608, USA
Bin Yu & Xinguang Chen
Department of Epidemiology and Health Statistics School of Health Sciences, Wuhan University, Wuhan, 430071, China
Xiangfan Chen & Hong Yan
You can also search for this author in PubMed Google Scholar
Contributions
BY designed the study, collected the data, conducted the data analysis, drafted and reviewed the manuscript; XGC designed the study and reviewed the manuscript. XFC and HY reviewed the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Hong Yan .
Ethics declarations
Ethics approval and consent to participate.
The study was reviewed and approved by the Institutional Review Board at the University of Florida. Data in the study were public available.
Consent for publication
All authors consented for the publication.
Competing interests
The authors declare that they have no competing interests.

Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: table s1..
Estimated Age, Period, Cohort Effects for the Trend of Marijuana Use in Past Month among Adolescents and Emerging Adults Aged 12 to 25 Years, NSDUH, 1979-2016. Table S2. Laws at the federal and state levels related to marijuana use.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Yu, B., Chen, X., Chen, X. et al. Marijuana legalization and historical trends in marijuana use among US residents aged 12–25: results from the 1979–2016 National Survey on drug use and health. BMC Public Health 20 , 156 (2020). https://doi.org/10.1186/s12889-020-8253-4
Download citation
Received : 15 June 2019
Accepted : 21 January 2020
Published : 04 February 2020
DOI : https://doi.org/10.1186/s12889-020-8253-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescents and young adults
- United States
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Estimating the effects of legalizing recreational cannabis on newly incident cannabis use
Roles Conceptualization, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Epidemiology and Biostatistics, College of Human Medicine, Michigan State University, East Lansing, MI, United States of America
Roles Formal analysis, Methodology, Validation, Writing – review & editing
Affiliation Department of Economics, College of Social Science, Michigan State University, East Lansing, MI, United States of America
Roles Methodology, Project administration, Supervision, Writing – review & editing
Roles Conceptualization, Supervision, Writing – review & editing
- Barrett Wallace Montgomery,
- Meaghan H. Roberts,
- Claire E. Margerison,
- James C. Anthony

- Published: July 21, 2022
- https://doi.org/10.1371/journal.pone.0271720
- Peer Review
- Reader Comments
Liberalized state-level recreational cannabis policies in the United States (US) fostered important policy evaluations with a focus on epidemiological parameters such as proportions [e.g., active cannabis use prevalence; cannabis use disorder (CUD) prevalence]. This cannabis policy evaluation project adds novel evidence on a neglected parameter–namely, estimated occurrence of newly incident cannabis use for underage (<21 years) versus older adults. The project’s study populations were specified to yield nationally representative estimates for all 51 major US jurisdictions, with probability sample totals of 819,543 non-institutionalized US civilian residents between 2008 and 2019. Standardized items to measure cannabis onsets are from audio computer-assisted self-interviews. Policy effect estimates are from event study difference-in-difference (DiD) models that allow for causal inference when policy implementation is staggered. The evidence indicates no policy-associated changes in the occurrence of newly incident cannabis onsets for underage persons, but an increased occurrence of newly onset cannabis use among older adults (i.e., >21 years). We offer a tentative conclusion of public health importance: Legalized cannabis retail sales might be followed by the increased occurrence of cannabis onsets for older adults, but not for underage persons who cannot buy cannabis products in a retail outlet. Cannabis policy research does not yet qualify as a mature science. We argue that modeling newly incident cannabis use might be more informative than the modeling of prevalences when evaluating policy effects and provide evidence of the advantages of the event study model over regression methods that seek to adjust for confounding factors.
Citation: Montgomery BW, Roberts MH, Margerison CE, Anthony JC (2022) Estimating the effects of legalizing recreational cannabis on newly incident cannabis use. PLoS ONE 17(7): e0271720. https://doi.org/10.1371/journal.pone.0271720
Editor: Giuseppe Carrà, Universita degli Studi di Milano-Bicocca, ITALY
Received: March 2, 2022; Accepted: July 6, 2022; Published: July 21, 2022
Copyright: © 2022 Montgomery et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The data relevant to this study is available from Github at https://github.com/Predict-This/Recreational-Cannabis-Leagalization .
Funding: There was no research support from the cannabis or other non-federal or non-university sources. BWM, MHR, CEM, and JCA wish to acknowledge support from the Michigan State University Vice President for Graduate Studies and Research (university funds) as well as federal research grant support from the National Institutes of Health (5R25DA051249). BWM and MHR also wish to acknowledge the Michigan State University Graduate School for funding from the Graduate Enrichment Fellowship and the University Distinguished Fellowship, respectively. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. There was no additional external funding received for this study.
Competing interests: The authors have declared that no competing interests exist.
Introduction
In drug dependence epidemiology, the estimated prevalences of active drug use are population health statistics that hide important patterns of (a) incidence (occurrence of first onsets) and (b) duration (e.g., duration and frequency of use after it starts). Lapouse [ 1 ], building upon prior work [ 2 ], argued that incidence estimates tell us about causes. In contrast, prevalence estimates tell us about caseloads and health services burdens. In a more recent review of the substance use epidemiology literature, Wu and colleagues echo these sentiments and note an abundance of research on prevalence, but a lack of literature on incidence [ 3 ].
Cheng and colleagues exploited this incidence-prevalence differentiation to show that a large sub-population of young adults in the United States (US) deliberately delayed their first drink until after the legal minimum drinking age [ 4 , 5 ]. Prevalence hid this pattern. Members of our research group hypothesized that age-specific cannabis use incidence would show a similar pattern developing in jurisdictions that legalized cannabis: Once the legal minimum age for recreational cannabis use was set at 21 in some states, many young adults will wait until cannabis use is legal for them to try it [ 6 ].
These initial observations motivated this research to estimate whether legalizing recreational cannabis might affect the occurrence of newly incident cannabis use (i.e., incidence). Cannabis use incidence in the US has traditionally peaked between ages 15 and 17 with steady declines as each cohort gets older [ 6 ]. Since all states that legalized recreational cannabis set 21 as the legal minimum age to purchase recreational cannabis, we analyze incidence before and after the age 21 milestone is reached. We sought to understand how legalizing recreational cannabis may be affecting incidence for these two age strata and how the estimates can inform the US population experiences after cannabis policy liberalization.
We can see no prior research on cannabis use incidence post recreational cannabis legalization (RCL). The published literature to this point has evaluated prevalence of recent use, prevalence of cannabis use disorder (CUD), and frequency of use. Concerning associations between cannabis liberalization and cannabis use prevalence among youth, most published evidence indicates that prevalence did not change after legalization, and perhaps may have dropped in some sub-[ 7 , 8 , 9 , 10 , 11 , 12 ]. Yet, a minority of studies provide firm evidence of appreciable cannabis use prevalence increases among adolescents [ 13 , 14 , 15 , 16 ]. As for CUD prevalence, the published evidence indicates that the 12-17-year-old participants in the National Surveys on Drug Use and Health (NSDUH) in states with legalized recreational cannabis might have been more likely to be CUD cases, but causal attribution to cannabis policy change remains uncertain [ 17 ]. As for the frequency of cannabis use among adolescents, the published estimates show no changes post RCL [ 17 , 18 , 19 , 20 ].
Among adults of legal age to purchase cannabis in these states, the evidence looks quite different. Apart from a few early findings [ 15 , 21 , 22 ], the published estimates consistently show that the prevalence of cannabis use among adults may increase after legalization [ 9 , 10 , 17 ]. Increased odds of CUD were found among NSDUH respondents 26 and older [ 17 ] and poly use of cannabis with other drugs, including alcohol, was also found to have increased in adults over the age of 26 [ 23 ]. Nevertheless, other studies find no evidence of change and deem the evidence to be inconclusive [ 10 , 20 ]. One study described an increase in frequent use in the 26 and older age group, but in no other sub-groups [ 17 ]. Another study found no increase in frequent or daily use in any sub-group [ 10 ].
To add novelty to cannabis policy evaluation research, we turned to the event study framework, an extension of the classic differences-in-differences (DiD) model. The DiD model is popular when the research goal is to estimate causal policy effects in the context of policy interventions in which the exposure and control groups are likely to differ on many dimensions. Its popularity might be traced to its constraints on unobserved confounding variables with the framework of relatively loose assumptions that the contrasted observed trends are parallel [ 24 ]. The event study model extension defines periods before and after legalization as intervention leads and lags. These lead and lag indicators allow for dynamic modeling of estimated changes in cannabis use incidence before and after the intervention.
We sought to estimate the causal effect of US state cannabis policy liberalization on the occurrence of newly incident cannabis use with respect to the legal minimum age. We produced age-stratified estimates for underage population members who were prohibited from purchasing cannabis, and for adults who were allowed to purchase retail cannabis, in several time periods relative to the dates of legalization.
Study population and sample
For this study, the population was specified to include non-institutionalized US civilian residents, sampled and assessed for successive NSDUH survey waves, 2008 through 2019. These NSDUH cross‐sectional surveys were conducted with multistage area probability sampling to draw state-level representative samples and to over-sample 12-to-17‐year‐olds. The total sample size for surveys conducted in this period includes 819,543 respondents. The average weighted screening participation level for the sample was 82% with an average interview participation level of 71% [ 25 ]. As this research used publicly available and anonymized data, the research was determined as not human subjects research by the Michigan State University Institutional Review Board on 8/26/2021 (MSU Study ID: STUDY00006620).
Standardized audio computer-assisted self-interview modules assessed each newly incident user’s month and year of first cannabis use, from which incidence estimates were derived from the NSDUH Restricted Data Access portal (R-DAS). R-DAS estimates are analysis-weighted with Taylor series derived variances and 95% confidence intervals (CI). The R-DAS portal also allows for state-specific analysis of data but can only be downloaded in pairs of years and not individual years (e.g., 2018–2019 vs. 2018, 2019). Thus, we produce estimates from six year-pairs in these analyses, not from 12 individual years.
We categorized states into different analysis groups according to each state’s year of legalization through 2018. Because the 2018–2019 year-pair is the most recent available data in R-DAS at the time of analysis, states that legalized cannabis in 2019 or later were categorized into the control group in which retail cannabis remained illegal. Washington and Colorado were included in the 2012 group. Oregon, Alaska, and Washington D.C. were in the 2014 group. California, Maine, Massachusetts, and Nevada were included in the 2016 group. Vermont and Michigan were included in the 2018 group. All other states were categorized into the control group for this analysis.
Primary outcome
Study design and statistical analysis
Recent explorations and analyses by econometricians revealed that estimating an average treatment effect is a bit of an over-simplification, especially when policy adoption is staggered [ 26 , 27 , 28 , 29 ]. With a policy intervention described as a ‘treatment’, the average treatment effect on the treated (ATT) is a weighted average of all the possible two-period estimators. This estimate can be problematic if it averages out important treatment effect heterogeneity that can take place over time. If treatment effects vary over time, then the ATT estimate is biased [ 26 ].
We found some evidence that drug policy intervention effects might change over time due to these lagged policy effects, thus we believe the event study model is better suited to this context [ 30 , 31 ]. Our study design contrasts estimates of cannabis incidence in the RCL states relative to non-RCL states before and after the legalization of cannabis at the state level. The DiD event study modelling yields estimates in each period relative to the year prior to legalization while controlling for fixed differences across states and national trends over time.
As described earlier, our datasets are constructed at the state category ( s ) by year ( t ) level. In our primary analyses, Y st denotes the cannabis incidence estimate for each state grouping in each year-pair. In the equation, β s denotes state fixed effects and β t denotes the fixed effects of time in calendar years. As a result, general time trends in cannabis incidence for each group of states are accommodated.
If occurrences of newly incident cannabis use trend similarly in all groups before legalization, we would expect that the estimated coefficients for the lead indicators will be small and indifferent from the null value in a test of the parallel trends assumption built into our model. When estimated coefficients for the lag indicators are positive departures from the null, this provides supporting evidence to reject the null hypothesis (e.g., an increase in the occurrence of newly incident cannabis use in RCL states).
In addition to the event study estimates of change at each time interval, we also present a simple 2x2 DiD estimate of the ATT as a summary of the estimated effect on those aged 21 and older across all post-legalization years through 2019 and an average treatment effect with the same method for the 12-to-20-year-olds. This estimate is derived from the same equation with the event study dummy variables replaced with a single indicator for post-policy change states.
Dates of legalization vs. dates of implementation.
We note that the mean number of days between the date of legalization and actual retail sales in the states in our sample (except for Washington D.C. where sales have never been legal) is approximately 500 days [ 32 ]. We set the T0 interval for this study to be a close approximation of this interval of elapsed time between policy enactment and actual implementation (i.e., start of retail sales).
Alternative specifications and robustness checks.
To ensure the robustness of our analyses, we examined two alternate specifications. The first alternate specification uses the same method to estimate the effect of RCL on cannabis prevalence. The estimate for prevalence has been studied extensively in the literature and we compare our results to prior estimates as a check of face validity for our model. The second robustness check uses a time placebo as a check of robustness. In this model, a random year within the data was selected as the year that states legalized cannabis. The model is then run with the same specifications. If any of this model’s coefficients are large enough to reject the null hypothesis, the evidence suggests a potentially spurious relationship.
All beta coefficients from the models are multiplied by 100 for interpretation as percent changes in the one-year cumulative incidence proportions. All analyses were performed in SAS version 9.04 with NSDUH analysis weights and Taylor series variances.
Descriptive statistics
In aggregate, the population sample under study included 819,543 respondents from the NSDUH surveys conducted between the years 2008 and 2019. The unweighted sample distributions indicate 48% female, 60% White, 13% Black, 18% Hispanic, 2% Native American, 4% Asian, and 4% of more than one race or another race or ethnicity ( Table 1 ). Within the sample, 11% used cannabis recently (past month). Table 1 provides the total unweighted sample characteristics with the NSDUH Public Data Analysis System (P-DAS) used to derive these values.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0271720.t001
S1 – S5 Figs show cannabis use incidence estimates for those aged 21 and older over time in different combinations of the state legal categories. Upon visual inspection, the parallel lines assumption and assumption of no anticipation look to have been met in every group by group comparison. For the sake of context and comparison, the average proportion of newly incident cannabis use between 2008 and 2019 in states that never legalized cannabis is 6.2% for 12-to-20-year-olds and 0.5% for those aged 21 and older. The average proportion of newly incident cannabis use in the two years prior to legalization for states that did legalize cannabis is 7.8% for 12-to-20-year-olds and 0.9% for those aged 21 and older.
Event study findings
Figs 1 and 2 show the primary findings for individuals aged 21 and older ( Fig 1 ) and those between the ages of 12 and 20 ( Fig 2 ). For those who were legally able to purchase cannabis (21 and older), the legalization of cannabis is estimated to have had no effect on newly incident cannabis use in the years of legalization. However, between two and four years after legalization, RCLs are estimated to have increased incidence by 0.6% [95% Confidence Interval (CI) = 0.1, 1.0]. The corresponding estimate for the interval four to seven years after passage of the RCL is 1.3% [0.8, 1.8] ( Fig 1 ). For the 12-to-20-year-olds, the estimated cannabis incidence does not vary appreciably in any period ( Fig 2 ).
https://doi.org/10.1371/journal.pone.0271720.g001
https://doi.org/10.1371/journal.pone.0271720.g002
DiD findings
When including the total time post-legalization, the simple ATT estimate derived from the 2x2 DiD indicates no substantial differences in cannabis incidence before and after the laws were passed (p = 0.12). However, since we expected no effect before cannabis sales became effective, we estimated a separate ATT for two years of legalization and later in the 21+ age group as 0.7% (p = 0.003, [0.3, 1.1]). The estimated average treatment effects for those aged 12 to 20 years indicated no differences after the legalization date (p = 0.27) or the effective date (p = .53).
Alternative specifications and robustness checks
In our first alternate specification, we estimate that the effect of cannabis legalization increased the prevalence of cannabis use in the past month among those aged 21 and older by 3.2% between two and four years after legalization (p = 0.0005, [1.6, 4.7]). The corresponding estimate for the interval four to seven years after legalization is 4.3% (p = 0.0002, [2.3, 6.2]) ( S6 Fig ). In the 12-to-20-year-old age group, no appreciable variation in estimated cannabis use prevalence is seen across these study intervals (P = 0.39 and 0.33, respectively) ( S7 Fig ).
In the time placebo analysis based upon a randomized legalization date, the date of placebo legalization was set to the year 2011 for all the states that legalized cannabis through 2018. S8 Fig shows an estimated coefficient that does increase slightly over time, yet the estimated effect of this ’placebo’ policy change is null. Note especially that for the adolescents (<21 years), the coefficients are distributed more or less at random in relation to the zero value, with no appreciable differences or patterns ( S9 Fig ).
These results show consistent evidence of an increase in the occurrence of newly incident cannabis use for adults aged 21 years and older after the removal of prohibitions against cannabis retail sales. For those aged 12-20-years-old, the study estimates support the hypothesis that RCLs did not affect the occurrence of newly incident cannabis use for underage persons. In the simple 2x2 DiD models, we estimate an average increase in cannabis use incidence of 0.7 percentage points after recreational cannabis began being legally sold through the year 2019, nearly double the difference between these state groups pre-legalization.
The innovations of this policy analysis relative to prior efforts can be seen in several areas. First, we focus on occurrence of newly incident cannabis use, separating out the population of sustained cannabis users. Prior studies on the associations between RCLs and cannabis use epidemiology focused on past-month cannabis use prevalence [ 7 , 8 , 9 , 10 , 13 , 16 , 19 , 21 , 22 ], the prevalence of daily or frequent users [ 19 , 11 , 19 ], and prevalence of CUD [ 10 , 17 ]. As such, the importance of understanding changes in cannabis use incidence in response to legalizing recreational cannabis cannot be overstated. Prevalence of use and dependence syndromes and frequency of use are of great public health importance, yet they tell us nothing about whether new users are entering into the population of cannabis users. This study provides an important initial thread of evidence about how liberalized cannabis policies might affect the number of cannabis users who otherwise might never have tried the drug.
Second, our research approach allows for the possibility raised by Cheng and colleagues [ 4 , 5 ] with respect to alcohol and by Montgomery, Vsevolozhskaya, & Anthony with respect to cannabis [ 6 ]. That is, there might exist a large pool of law-abiding individuals who would never have used cannabis if retail sales had not been allowed, but who try cannabis once it becomes legal for them to do so.
Third, this is the first study of which we are aware that has examined the heterogeneity of treatment effects in the years post RCL. The event study design allows for the estimation of effects by years relative to the passage of the recreational cannabis legislation and the effective dates of implementation. This has resulted in three important pieces of evidence: 1) Estimated effects of cannabis legalization on incidence of use seems to increase over time (albeit with possible diminishing returns); 2) Estimated effect sizes vary across age strata defined by the legal minimum retail sales age; and 3) Estimated effect size might be zero for the population to whom cannabis remains illegal. This last piece of evidence might provide some reassurance to policy makers who worry about increased incidence among adolescent populations of the jurisdictions that permit cannabis purchases by adults.
Fourth, the use of a quasi-experimental DiD design provides some allowance for a causal interpretation of estimated intervention effects. With some noteworthy exceptions [ 11 , 13 ], the evidence published on cannabis policy effects has relied mostly on controlling for observed variables between the populations. Considerable differences exist between populations in states with and without legalized recreational cannabis. It seems reasonable to ask whether controlling for pre-contemplated and measured variables is sufficient to produce valid estimates. The DiD framework constrains unobserved variables within a limited framework of model-based assumptions. Our research included evaluation of some of these often-untested assumptions (e.g., no anticipation; parallel trends).
Lastly, due to our focus on cannabis incidence, this study’s estimates cannot be compared directly with findings of prior cannabis policy evaluations. Nonetheless, a limited comparison is possible and can be seen in the results from our application of the DiD approach to estimates of the prevalence of cannabis use. As in the estimates published by Cerdá and colleagues [ 13 ] and by Coley and colleagues [ 11 ], our DiD approach disclosed no appreciable policy influence on cannabis prevalence estimates for people under the age of 21. Our estimates of prevalence are similar to the estimates seen in Cerdá et al., Martins et al., and Reed’s more recent findings ([ 17 , 10 , 9 ]. We also note that our findings may help the field to understand seemingly conflicting earlier null findings in this age [ 15 , 21 , 22 ]. Synthesizing the above findings, we suggest that the increases in the use of cannabis in the adult age group may have only began increasing after a few years when recreational cannabis shops began sales.
Limitations and strengths
Before describing some directions for future cannabis policy research, we must describe several limitations of our empirical study. First, it’s difficult to conceptualize cannabis policy evaluation studies that do not rely upon self-reports from general population samples. In other domains, we might look to retail sales records, but before cannabis policy shifts to permit retail sales there are no pre-policy measurements. We also might look to employer records on drug-testing of employees, but these databases are selective and non-representative of the larger population experience, without coverage of the important age strata we have studied. It seems unlikely that cannabis policy evaluation research will overcome the self-report as a limitation for the time being. As an extension of this concern about self-report, we must acknowledge the possibility of differential response biases. Might population members be more likely to disclose cannabis use when they can use cannabis without concern about legal consequences? This question has yet to be answered. The assessments were conducted using confidential standardized audio computer-assisted self-interview modules which have been shown to reduce biases of this type.
Some other limitations of this work include the sensitivity of the findings to different definitions of the study period and an inability to control for sub-state level recreational cannabis legality. The limitation regarding the definition of the study period is important, specifically to our estimate of the ATT. When including the two-year period immediately after legalization (before sales began) in the treatment period, we detected no differences. However, using a study design that allows for dynamic treatment effects and having estimates that are robust to alternate specifications allow us to show where and when the difference in trends occur. This supports the argument that the effect of cannabis legalization is driven by the opening of outlets where recreational cannabis is sold.
Another limitation of this work at the state level is that many counties and municipalities within states that have legalized recreational cannabis have chosen to ban the sale or cultivation of cannabis within that sub-state area. For example, in Washington State, 15% of counties and 55% of municipalities have prohibited the sale of cannabis [ 33 ] while in California, 69% of counties and 70% of cities prohibit the sale [ 34 ]. Like the null finding between the date of legalization and effective dates of cannabis sales, we expect that estimates of the effects of legalizing recreational cannabis at the state level are diminished by incorporating incidence for many individuals who reside in areas where recreational cannabis is effectively in this pre-implementation state. This sub-group heterogeneity is averaged out in our state-level estimates. While a sub-state analysis is beyond the scope of this study, future research should seek to replicate this analysis at the municipality or county level.
The strengths of this work are the robustness of the estimates, the novelty of the design in this space, and the interpretations that it allows for. Our estimates of the effects of recreational cannabis liberalization on cannabis use incidence by age group were robust to both the check of face validity using the same method to estimate past-month prevalence and the alternate specification using a time-placebo analysis. The use of the DiD event study design moves this field forward by allowing for a dynamic estimate of the causal effect of RCL on the outcome of choice.
As we have demonstrated, it is not reasonable to assume that the effect of cannabis legalization is homogenous over time, especially not if the period includes the time before cannabis sales began. Therefore, future research on the effects of RCL should allow for time-specific effect heterogeneity. Although this is only one study, from which conclusions should not be drawn, this design allows for a visualization of the policy lag effect, about which much has been written [ 30 , 31 ]. We see that the effect is not linear and is perhaps rather sigmoidal in shape with the increases in incidence and prevalence beginning to plateau, although more data is needed to confirm the trend.
Conclusions
This study contributes novel estimates of how liberalized cannabis policies within US jurisdictions might have influenced occurrence of newly incident cannabis use in the underage (<21 years) and in the adult populations, now allowed to purchase cannabis products in retail outlets. Cannabis policy liberalization continues to be a contentious issue in the national political landscape with different risks and benefits described for all of the potential paths forward. Policy-makers and the voters who elect these policy-makers cannot make the best judgments in the absence of evidence, unless their decisions are to be based on potentially erroneous prejudices or beliefs. The evidence from this study is not perfect, but the estimates provide an evidence base that can be judged in relation to an important question–namely, should we worry about underage cannabis use when adults are allowed to buy cannabis products in retail shops? And might the occurrence of adult-onset newly incident cannabis use increase if this policy change is made? The answer to the first question at this point seems to be that there has been no policy influence on cannabis incidence in the underage adolescent population after adults have been allowed to buy cannabis in retail shops. The answer to the second question at this point indicates a tangible uptick in the occurrence of newly incident cannabis use among adults who otherwise might never have tried cannabis. We are hopeful that voters, policymakers, and public health officials can use this evidence as they forecast what might change if cannabis policies are liberalized to permit adult purchases from retail cannabis shops in their jurisdictions.
Supporting information
S1 fig. cannabis incidence in 21 and older age group, first wave legalizing states vs untreated states..
https://doi.org/10.1371/journal.pone.0271720.s001
S2 Fig. Cannabis incidence in 21 and older age group, second wave legalizing states vs untreated states.
https://doi.org/10.1371/journal.pone.0271720.s002
S3 Fig. Cannabis incidence in 21 and older age group, third wave legalizing states vs untreated states.
https://doi.org/10.1371/journal.pone.0271720.s003
S4 Fig. Cannabis incidence in 21 and older age group, first wave legalizing states vs third wave legalizing states.
https://doi.org/10.1371/journal.pone.0271720.s004
S5 Fig. Cannabis incidence in 21 and older age group, second wave legalizing states vs third wave legalizing states.
https://doi.org/10.1371/journal.pone.0271720.s005
S6 Fig. Effect of time since cannabis legalization on past month cannabis prevalence in the 21 and older age group.
https://doi.org/10.1371/journal.pone.0271720.s006
S7 Fig. Effect of time since legalization on past-month cannabis prevalence in the 12-to-20-age-group.
https://doi.org/10.1371/journal.pone.0271720.s007
S8 Fig. Placebo effect of time since cannabis legalization on cannabis incidence in the 21 and older age group.
https://doi.org/10.1371/journal.pone.0271720.s008
S9 Fig. Placebo effect of time since cannabis legalization on cannabis incidence in the 12-to-20-age-group.
https://doi.org/10.1371/journal.pone.0271720.s009
- View Article
- PubMed/NCBI
- Google Scholar
- 21. Marijuana legalization in Colorado: Early findings [Internet]. State.co.us. 2016 [cited 2022 Mar 1]. Available from: https://cdpsdocs.state.co.us/ors/docs/reports/2016-SB13-283-Rpt.pdf
- 24. Angrist JD, Pischke JS. Mostly harmless econometrics. Princeton university press; 2008 Dec 15. Princeton university press.
- 32. Legal recreational marijuana states and DC [Internet]. Recreational Marijuana. 2022 [cited 2022 Mar 1]. Available from: https://marijuana.procon.org/legal-recreational-marijuana-states-and-dc/
- 33. MRSC—Marijuana Regulation in Washington State [Internet]. Mrsc.org. [cited 2022 Mar 1]. Available from: http://mrsc.org/Home/Explore-Topics/Legal/Regulation/Marijuana-Regulation-in-Washington-State.aspx
The Impact of Recreational Cannabis Legalization on Cannabis Use and Associated Outcomes: A Systematic Review
Affiliations.
- 1 Department of Psychology, York University, Toronto, ON, Canada.
- 2 Peter Boris Centre for Addictions Research, St. Joseph's Healthcare Hamilton, McMaster University, Hamilton, ON, Canada.
- 3 Institute for Mental Health Policy Research, Centre for Addiction and Mental Health, Toronto, ON, Canada.
- 4 Department of Psychiatry, University of Toronto, Toronto, ON, Canada.
- 5 Michael G. DeGroote Centre for Medicinal Cannabis Research, McMaster University & St. Joseph's Healthcare Hamilton, Hamilton, ON, Canada.
- 6 Homewood Research Institute, Guelph, ON, Canada.
- PMID: 37187466
- PMCID: PMC10176789
- DOI: 10.1177/11782218231172054
Background: Recreational cannabis legalization has become more prevalent over the past decade, increasing the need to understand its impact on downstream health-related outcomes. Although prior reviews have broadly summarized research on cannabis liberalization policies (including decriminalization and medical legalization), directed efforts are needed to synthesize the more recent research that focuses on recreational cannabis legalization specifically. Thus, the current review summarizes existing studies using longitudinal designs to evaluate impacts of recreational cannabis legalization on cannabis use and related outcomes.
Method: A comprehensive bibliographic search strategy revealed 61 studies published from 2016 to 2022 that met criteria for inclusion. The studies were predominantly from the United States (66.2%) and primarily utilized self-report data (for cannabis use and attitudes) or administrative data (for health-related, driving, and crime outcomes).
Results: Five main categories of outcomes were identified through the review: cannabis and other substance use, attitudes toward cannabis, health-care utilization, driving-related outcomes, and crime-related outcomes. The extant literature revealed mixed findings, including some evidence of negative consequences of legalization (such as increased young adult use, cannabis-related healthcare visits, and impaired driving) and some evidence for minimal impacts (such as little change in adolescent cannabis use rates, substance use rates, and mixed evidence for changes in cannabis-related attitudes).
Conclusions: Overall, the existing literature reveals a number of negative consequences of legalization, although the findings are mixed and generally do not suggest large magnitude short-term impacts. The review highlights the need for more systematic investigation, particularly across a greater diversity of geographic regions.
Keywords: Cannabis; attitudes; crime; driving; health; legalization; marijuana.
© The Author(s) 2023.
Publication types
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
The Evidence—and Lack Thereof—About Cannabis
Research is still needed on cannabis’s risks and benefits.
Lindsay Smith Rogers
Although the use and possession of cannabis is illegal under federal law, medicinal and recreational cannabis use has become increasingly widespread.
Thirty-eight states and Washington, D.C., have legalized medical cannabis, while 23 states and D.C. have legalized recreational use. Cannabis legalization has benefits, such as removing the product from the illegal market so it can be taxed and regulated, but science is still trying to catch up as social norms evolve and different products become available.
In this Q&A, adapted from the August 25 episode of Public Health On Call , Lindsay Smith Rogers talks with Johannes Thrul, PhD, MS , associate professor of Mental Health , about cannabis as medicine, potential risks involved with its use, and what research is showing about its safety and efficacy.
Do you think medicinal cannabis paved the way for legalization of recreational use?
The momentum has been clear for a few years now. California was the first to legalize it for medical reasons [in 1996]. Washington and Colorado were the first states to legalize recreational use back in 2012. You see one state after another changing their laws, and over time, you see a change in social norms. It's clear from the national surveys that people are becoming more and more in favor of cannabis legalization. That started with medical use, and has now continued into recreational use.
But there is a murky differentiation between medical and recreational cannabis. I think a lot of people are using cannabis to self-medicate. It's not like a medication you get prescribed for a very narrow symptom or a specific disease. Anyone with a medical cannabis prescription, or who meets the age limit for recreational cannabis, can purchase it. Then what they use it for is really all over the place—maybe because it makes them feel good, or because it helps them deal with certain symptoms, diseases, and disorders.
Does cannabis have viable medicinal uses?
The evidence is mixed at this point. There hasn’t been a lot of funding going into testing cannabis in a rigorous way. There is more evidence for certain indications than for others, like CBD for seizures—one of the first indications that cannabis was approved for. And THC has been used effectively for things like nausea and appetite for people with cancer.
There are other indications where the evidence is a lot more mixed. For example, pain—one of the main reasons that people report for using cannabis. When we talk to patients, they say cannabis improved their quality of life. In the big studies that have been done so far, there are some indications from animal models that cannabis might help [with pain]. When we look at human studies, it's very much a mixed bag.
And, when we say cannabis, in a way it's a misnomer because cannabis is so many things. We have different cannabinoids and different concentrations of different cannabinoids. The main cannabinoids that are being studied are THC and CBD, but there are dozens of other minor cannabinoids and terpenes in cannabis products, all of varying concentrations. And then you also have a lot of different routes of administration available. You can smoke, vape, take edibles, use tinctures and topicals. When you think about the explosion of all of the different combinations of different products and different routes of administration, it tells you how complicated it gets to study this in a rigorous way. You almost need a randomized trial for every single one of those and then for every single indication.
What do we know about the risks of marijuana use?
Cannabis use disorder is a legitimate disorder in the DSM. There are, unfortunately, a lot of people who develop a problematic use of cannabis. We know there are risks for mental health consequences. The evidence is probably the strongest that if you have a family history of psychosis or schizophrenia, using cannabis early in adolescence is not the best idea. We know cannabis can trigger psychotic symptoms and potentially longer lasting problems with psychosis and schizophrenia.
It is hard to study, because you also don't know if people are medicating early negative symptoms of schizophrenia. They wouldn't necessarily have a diagnosis yet, but maybe cannabis helps them to deal with negative symptoms, and then they develop psychosis. There is also some evidence that there could be something going on with the impact of cannabis on the developing brain that could prime you to be at greater risk of using other substances later down the road, or finding the use of other substances more reinforcing.
What benefits do you see to legalization?
When we look at the public health landscape and the effect of legislation, in this case legalization, one of the big benefits is taking cannabis out of the underground illegal market. Taking cannabis out of that particular space is a great idea. You're taking it out of the illegal market and giving it to legitimate businesses where there is going to be oversight and testing of products, so you know what you're getting. And these products undergo quality control and are labeled. Those labels so far are a bit variable, but at least we're getting there. If you're picking up cannabis at the street corner, you have no idea what's in it.
And we know that drug laws in general have been used to criminalize communities of color and minorities. Legalizing cannabis [can help] reduce the overpolicing of these populations.
What big questions about cannabis would you most like to see answered?
We know there are certain, most-often-mentioned conditions that people are already using medical cannabis for: pain, insomnia, anxiety, and PTSD. We really need to improve the evidence base for those. I think clinical trials for different cannabis products for those conditions are warranted.
Another question is, now that the states are getting more tax revenue from cannabis sales, what are they doing with that money? If you look at tobacco legislation, for example, certain states have required that those funds get used for research on those particular issues. To me, that would be a very good use of the tax revenue that is now coming in. We know, for example, that there’s a lot more tax revenue now that Maryland has legalized recreational use. Maryland could really step up here and help provide some of that evidence.
Are there studies looking into the risks you mentioned?
Large national studies are done every year or every other year to collect data, so we already have a pretty good sense of the prevalence of cannabis use disorder. Obviously, we'll keep tracking that to see if those numbers increase, for example, in states that are legalizing. But, you wouldn't necessarily expect to see an uptick in cannabis use disorder a month after legalization. The evidence from states that have legalized it has not demonstrated that we might all of a sudden see an increase in psychosis or in cannabis use disorder. This happens slowly over time with a change in social norms and availability, and potentially also with a change in marketing. And, with increasing use of an addictive substance, you will see over time a potential increase in problematic use and then also an increase in use disorder.
If you're interested in seeing if cannabis is right for you, is this something you can talk to your doctor about?
I think your mileage may vary there with how much your doctor is comfortable and knows about it. It's still relatively fringe. That will very much depend on who you talk to. But I think as providers and professionals, everybody needs to learn more about this, because patients are going to ask no matter what.
Lindsay Smith Rogers, MA, is the producer of the Public Health On Call podcast , an editor for Expert Insights , and the director of content strategy for the Johns Hopkins Bloomberg School of Public Health.
Could Medical Marijuana Help Address the Opioid Epidemic?
Policy Is Public Health
Medical Marijuana Laws Linked to Health and Labor Supply Benefits in Older Adults
Related Content

How Dangerous is Dengue?

Research Identifies Characteristics of Cities That Would Support Young People’s Mental Health

Alumni Spotlight: Junrui Di, PhD '19

Child Diarrhea Has a Cheap and Easy Fix—Why Isn’t It Reaching Patients?

How Abortion Trigger Laws Impact Mental Health
This website uses cookies.
By clicking the "Accept" button or continuing to browse our site, you agree to first-party and session-only cookies being stored on your device to enhance site navigation and analyze site performance and traffic. For more information on our use of cookies, please see our Privacy Policy .
- Journal of Economic Literature
The Public Health Effects of Legalizing Marijuana
- D. Mark Anderson
- Daniel I. Rees
- Article Information
Additional Materials
- Author Disclosure Statement(s) (158.63 KB)
JEL Classification
- R41 Transportation: Demand, Supply, and Congestion; Travel Time; Safety and Accidents; Transportation Noise
- Introduction
- Conclusions
- Article Information
Age and sex standardized rate of hospitalizations due to cannabis per 100 000 individuals and per 1000 all-cause hospital admissions between January 2015 and March 2021. Shaded regions indicate 95% CIs.
Age and sex standardized rate of hospitalizations due to cannabis per 100 000 individuals and per 1000 all-cause hospital admissions between January 2015 and March 2021 for each province. Shaded regions indicate 95% CIs.
eTable 1. Timeline of legalization of cannabis in Canada
eTable 2. Sensitivity analysis using different starting dates for commercialization for immediate and gradual changes in rates of monthly hospitalizations due to cannabis in four largest provinces in Canada
eTable 3. Changes in cannabis sales in first and last year of study
eFigure 1. Sensitivity analysis using January 2020 as start of commercialization period of age and sex standardized rates of hospitalizations due to cannabis per 100,000 individuals and per 1,000 all-cause hospitalizations due to cannabis in the four largest provinces in Canada
eFigure 2. Changes over time in monthly per capita spending on cannabis ($CAD per individual aged 15+years) in Canada, Ontario, Alberta, Quebec and British Columbia
eReferences.
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Myran DT , Gaudreault A , Konikoff L , Talarico R , Liccardo Pacula R. Changes in Cannabis-Attributable Hospitalizations Following Nonmedical Cannabis Legalization in Canada. JAMA Netw Open. 2023;6(10):e2336113. doi:10.1001/jamanetworkopen.2023.36113
Manage citations:
© 2024
- Permissions
Changes in Cannabis-Attributable Hospitalizations Following Nonmedical Cannabis Legalization in Canada
- 1 Bruyère Research Institute, Ottawa, Ontario, Canada
- 2 Clinical Epidemiology Program, Ottawa Hospital Research Institute, Ottawa, Ontario, Canada
- 3 Department of Family Medicine, University of Ottawa, Ottawa, Ontario, Canada
- 4 ICES uOttawa, Ottawa Hospital Research Institute, Ottawa, Ontario, Canada
- 5 Suzanne Dworak-Peck School of Social Work, University of Southern California, Los Angeles
- 6 Institute for Addiction Science, University of Southern California, Los Angeles
Question How have rates of hospitalizations due to cannabis changed, nationally and between provinces, since nonmedical cannabis was legalized in Canada?
Findings In this cross-sectional study of 26.9 million individuals in 4 Canadian provinces, rates of cannabis-related hospitalizations declined immediately after legalization during a period of legal market immaturity and later increased during a period of legal market expansion and the COVID-19 pandemic.
Meaning The findings in this study caution that greater levels of legal cannabis market access may be associated with an increase in a variety of cannabis-attributable harms.
Importance The impact of adult-use cannabis legalization and subsequent commercialization (ie, increasing store and product access) on hospitalizations in Canada is unclear.
Objectives To examine changes in overall and subtypes of hospitalizations due to cannabis and associated factors following legalization in Canada and to compare changes between provinces.
Design, Setting, and Participants This repeated cross-sectional analysis included all acute hospitalizations for individuals aged 15 to 105 years in Canada’s 4 most populous provinces (Ontario, Quebec, Alberta and British Columbia, population 26.9 million individuals in 2018). Data were obtained from routinely collected health administrative databases. Immediate and gradual changes in the age- and sex-standardized rates of hospitalizations due to cannabis were compared using an interrupted time series design over 3 time periods: prelegalization (January 2015 to September 2018), legalization with product and store restrictions (October 2018 to February 2020), and commercialization, which overlapped with the COVID-19 pandemic (March 2020 to March 2021).
Main Outcomes and Measures Rates of hospitalizations due to cannabis per 100 000 individuals and per 1000 all-cause hospital admissions.
Results There were 105 203 hospitalizations due to cannabis over the 7-year study period, 69 192 of which (65.8%) were among male individuals, and 34 678 (33%) of which were among individuals aged 15 to 24 years. Overall, the age- and sex-standardized rate of hospitalizations increased 1.62 times between January 2015 (3.99 per 100 000 individuals) and March 2021 (6.46 per 100 000 individuals). The largest relative increase in hospitalizations was for cannabis-induced psychosis (rate ratio, 1.40; 95% CI, 1.34 to 1.47 during the commercialization period relative to the prelegalization period). Nationally, legalization with restrictions was associated with a gradual monthly decrease of −0.06 (95% CI −0.08 to −0.03) in hospitalizations due to cannabis per 100 000 individuals. Commercialization and the COVID-19 pandemic were associated with an immediate increase of 0.83 (95% CI, 0.30 to 1.30) hospitalizations due to cannabis per 100 000 individuals. There was provincial variation in changes, with provinces with less mature legal markets experiencing the greatest declines immediately following legalization.
Conclusions and Relevance This cross-sectional study found that legalization with restrictions was not associated with an increase in hospitalizations due to cannabis but commercialization was. The findings suggest that commercialization of cannabis may be associated with increases in cannabis-related health harms, including cannabis-induced psychosis.
Canada legalized nonmedical cannabis for adult use in October 2018. 1 There is increasing recognition that regular and heavy cannabis use is associated with various adverse health concerns, including psychosis, increased anxiety, depression, altered brain functioning, and cannabis dependence and addiction. 2 - 5 Cannabis use results in a large number of health system encounters, including emergency department (ED) visits and hospitalizations, and is the leading cause of hospitalizations for substance use in Canadian youth. 6 ED visits due to cannabis have also been increasing rapidly over time in the US and Europe. 7 , 8 However, the impact of nonmedical cannabis legalization on health care visits due to cannabis remains unclear. Several studies have investigated changes over time in ED visits due to cannabis in two provinces (Alberta or Ontario) in Canada following legalization. 9 - 14 Two brief reports have also examined changes in hospitalizations due to cannabis—a potentially more severe and specific indicator of cannabis-related health harms—in Ontario and Quebec. 15 , 16 Studies to date have used differing lengths of follow-up and not compared changes following legalization in health service use due to cannabis between provinces or at the national level. This is an important gap, as prior work has established substantial variation in key cannabis policies, including product types and store access. 1 , 17 , 18 Consequently, limited information is available about how cannabis retail policies may be associated with changes in cannabis harms postlegalization. In addition, to date, studies on changes in health service use due to cannabis following legalization have not directly compared changes across different types of presentations (eg, changes in visits for psychosis vs visit for intoxication), which limits knowledge about the kinds of cannabis harms that may have increased the most following legalization.
Although all provinces in Canada were legally required to allow the sale of cannabis in October 2018, each province and territory were allowed to set their own regulations regarding how cannabis would be sold and the types of products that could be introduced. 1 Initially, all provinces in Canada were only allowed to sell dried cannabis flower. In October 2019, cannabis producers were allowed to apply to begin selling new high-potency cannabis products, including edibles, vape pens, and concentrates. Most provinces allowed these products to come to market starting in early 2020. Notably, Quebec did not permit these products over concern of their potential appeal to children and youth. 19 Provinces also took differing approaches to cannabis retail store access. Alberta had a rapid expansion of stores and legal sales immediately following legalization. In contrast, Ontario and British Columbia initially had very low cannabis sales and store access, followed by rapid growth beginning in early 2020. Quebec had the lowest per capita stores and sales throughout the study. See eTable 1 in Supplement 1 for further details on cannabis policy in Canada.
These different approaches to legalization provide an opportunity to explore how different regulatory approaches to cannabis markets may impact the overall burden on public health. This study had 3 objectives: to examine changes at the national level in hospitalizations due to cannabis following legalization using data from Canada’s 4 most populous provinces (Ontario, Quebec, Alberta, and British Columbia, which together comprise 86% of the population of Canada); to compare changes in hospitalizations across the 4 provinces and contextualize changes by variation in cannabis retail policy; and to compare changes in hospitalizations according to different causes of cannabis-related harms (eg, acute intoxication, abuse, dependence, withdrawal, poisoning, and psychosis) to determine whether there have been any changes in these conditions over the 3 distinct policy periods in Canada since legalization.
This repeated cross-sectional study was approved by the research ethics board of the Ottawa Hospital Research Institute. Because this study used deidentified aggregate health information, no informed consent was required. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We conducted a repeated cross-sectional population-based study using health administrative databases from Ontario, Quebec, Alberta, and British Columbia (population of 26.9 million individuals aged 15 to 105 years in 2018). 20 We included hospitalizations from all individuals aged 15 to 105 years who were eligible for the province’s single-payer universal health insurance between January 2015 and March 2021. We calculated crude rates and age- and sex-standardized rates using direct standardization from the 2016 Canadian Census. We used an interrupted time series design to examine immediate and gradual changes in hospitalizations over 3 distinct policy periods: prelegalization (January 2015 to September 2018), legalization with strict controls (October 2018 to February 2020), and commercialization, including increasing store access and product type (March 2020 to March 2021), which overlapped with the COVID-19 pandemic. We began our study in 2015, as this was the start of hospitalization data being available in all 4 provinces. We categorized the transition between legalization with restrictions to commercialization as occurring in March 2020. This transition is consistent with prior work and reflects when expanded products became widely available (ie, mid-January 2020) and when store growth began to accelerate in Ontario (April 2020) in addition to the declaration of states of emergency across Canada (March 2020) along with large changes in health service use in response to the COVID-19 pandemic. 9 - 11 , 21 As a sensitivity analysis, we defined the commercialization period as beginning in January 2020.
Hospitalization data were obtained from the Canadian Institute of Health Informatics using the Discharge Abstract Database and the Hospital Morbidity Database between January 1, 2015, and September 30, 2021. These databases capture all acute care hospitalizations in Canada from each province’s universal health care insurance. An estimated 97% of Canadians are eligible for and covered by their province’s universal health coverage. 22
The primary outcome was the rate of hospitalizations due to cannabis per capita 100 000 per capita and per 1000 all-cause hospital admissions. We examined hospitalizations due to cannabis per 1000 all-cause hospitalizations to contextualize changes during the commercialization period with overall changes in health care visits. Hospitalizations due to cannabis were identified when 1 of the following International Classification of Diseases , 10th Revision ( ICD-10 ) codes was listed as the main or contributing reason for hospitalization: T40.7 (poisoning by cannabis, including derivatives) and F12.X (mental and behavioral disorders due to use of cannabinoids). We examined the monthly count of overall hospitalizations and subgroups, including sex and age (15 to 24 years and ≥25 years). We examined specific diagnostic types classified as acute intoxication (F12.0), harmful cannabis use (formerly cannabis abuse, F12.1), cannabis dependence (F12.2), cannabis withdrawal (F12.3), cannabis-induced psychosis (F12.5, F12.7), poisoning from cannabis and derivates (T40.7), and other or unspecified mental and behavioral disorders from cannabis (F12.6, F12.8, F12.9).
We present descriptive statistics to characterize and compare the absolute numbers and rate per person-years of hospitalizations due to cannabis across the 3 policy periods and the whole study period. We computed crude rate ratios with Wald 95% CIs.
We then calculated the monthly age- and sex-standardized rate of our primary outcomes per 100 000 individuals and per 1000 all-cause admissions over the 3 periods (prelegalization, legalization with restrictions, and commercialization/COVID-19). Rates were standardized using direct standardization with the 2016 Canadian Census as the reference population. We then used an interrupted time series approach with segmented linear regression analysis to assess the immediate and gradual changes in rates over the 3 policy periods. We included indicators representing the 4 seasons to account for seasonal variation, and all analyses included first-order autoregressive covariance structures. When examining rates per 100 000 individuals, we included 2 binary indicator variables, 1 for March 2020 and 1 for April 2020, to account for large decreases in overall health service use at onset of the pandemic, consistent with prior work. Models were estimated using restricted maximum likelihood. 23 When visualizing monthly trends, we presented deseasonalized rates with the season fixed in winter. We expressed the immediate and gradual changes postlegalization as absolute mean rate changes with 95% CIs and interpreted statistical significance when the 95% CIs did not cross 1. All analyses were completed using SAS version 9.4 (SAS institute).
During the 7-year study period, there were 105 203 hospitalizations due to cannabis (63.36 per 100 000 person years), with 69 192 (65.8%) hospitalizations among male individuals and 34 678 (33.0%) among individuals aged 15 to 24 years. Table 1 lists the characteristics of hospitalizations due to cannabis for the whole study period, the prelegalization period, the legalization period, and the commercialization/COVID-19 pandemic period. The most common reason for admission was harmful cannabis use (51 631 of 105 203 [46.2%]), followed by cannabis dependence (22 266 of 105 203 [19.9%]), other (18 756 of 105 203 [16.8%]), and cannabis-induced psychosis (3387 of 105 203 [9.7%]). The largest relative inhcrease in hospitalization rates was for cannabis-induced psychosis (rate ratio, 1.40; 95% CI, 1.34 to 1.47 in the commercialization/COVID-19 period relative to prelegalization) and for cannabis withdrawal (rate ratio, 1.37; 95% CI, 1.20 to 1.56 in the legalization period relative to prelegalization). The largest absolute increase in hospitalization rates was for harmful cannabis use (35.16 during commercialization vs 29.15 prelegalization per 100 000 person years). Increases in hospitalizations due to cannabis over time were similar for men and women and greater for individuals 25 years and older compared to those aged 15 to 24 years.
Figure 1 displays the national (4 combined provinces) age- and sex-standardized monthly rate of hospitalizations between January 2015 and March 2021 per 100 000 individuals and per 1000 hospitalizations due to cannabis. Between the first and last month of the study, the age- and sex-standardized rate of hospitalizations due to cannabis per 100 000 individuals increased 1.62 times from 3.99 per 100 000 individuals in January 2015 to 6.46 per 100 000 individuals in March 2021. Over the same period, the rate of hospitalizations due to cannabis per 1000 all-cause hospitalizations increased 1.71 times from 5.31 per 1000 hospitalizations in January 2015 to 9.10 per 1000 hospitalizations in March 2021.
Table 2 reports the segmented regression model coefficients for the absolute change in rates of monthly hospitalizations per capita nationally and for each of the 4 provinces. Nationally, the prelegalization age- and sex-standardized rates were increasing by 0.04 (95% CI, 0.03 to 0.04) hospitalizations per 100 000 individuals each month. The restricted legalization period was associated with an insignificant immediate level decrease of 0.19 (95% CI, −0.46 to 0.10) hospitalizations per 100 000 individuals per month and a significant monthly slope decrease of −0.06 (95% CI, −0.08 to −0.03) hospitalizations per 100 000 individuals. Cannabis commercialization and the overlapping COVID-19 period were associated with a significant immediate level change of 0.83 (95% CI, 0.36 to 1.30) hospitalizations per 100 000 individuals per month and an insignificant monthly slope increase of 0.02 (95% CI, −0.04 to 0.07) hospitalizations per 100 000 individuals. Similar patterns were observed for changes in visits per 1000 total hospital admissions, but the attenuation of the prelegalization trend during the restricted legalization period was no longer significant (see Table 2 for model coefficients for changes per 1000 admissions). Our sensitivity analysis starting the commercialization period during January 2020 showed a smaller immediate level change of 0.44 (95% CI, 0.03 to 0.84) monthly hospitalizations per 100 000 individuals and a greater monthly slope increase or 0.07 (95% CI, 0.02 to 0.12) hospitalizations per 100 000 individuals (see eFigure 1 and eTable 2 in Supplement 1 for changes over time and model coefficients).
Figure 2 displays monthly age- and sex-standardized rates of hospitalizations between January 2015 and March 2021 per 100 000 and 1000 admissions separately for each of the four provinces. Quebec had the largest increase in hospitalizations, from 5.71 per 100 000 individuals in January 2015 to 11.84 per 100 000 individuals in March 2021. Alberta had the second largest increase, from 5.40 in January 2015 to 8.21 in March 2021, followed by Ontario (1.51 per 100 000 individuals in January 2015 to 2.01 per 100 000 individuals in Mach 2021), and British Columbia experienced the smallest increase in hospitalizations from 6.92 per 100 000 individuals in January 2015 to 8.21 per 100 000 individuals in March 2021. Prelegalization visits were increasing 10 times faster in Quebec than Ontario. The restricted legalization phase was associated with a significant attenuation in the prelegalization slope for all provinces except Alberta. Commercialization/COVID-19 were associated with a significant level increase in all provinces except Quebec but no significant slope change was observed in any province.
Over our 7-year study period, there was a 1.62-fold increase in the age- and sex-standardized rates of monthly hospitalizations due to cannabis in Canada. The first 1.5 years following legalization, when stores and products were restricted, was associated with a modest decrease in hospitalizations. In contrast, the period when cannabis became broadly commercialized in Canada, which overlapped with the COVID-19 pandemic, was associated with increased hospitalizations due to cannabis. Men had almost double the rates of hospitalizations due to cannabis throughout the study period, but this disparity was constant over time. Increases in cannabis-related hospitalizations were greater in individuals 25 years and older compared to those aged 15 to 24 years. There was variation in changes postlegalization in the type of hospitalization due to cannabis, with the largest relative increases for cannabis-induced psychosis. Broadly, these findings caution that greater levels of market commercialization and product proliferation may increase a variety of cannabis-attributable harms. However, the current study cannot isolate the impacts of the COVID-19 pandemic.
Changes in hospitalizations due to cannabis during our study period varied by regulatory period. Hospitalizations were increasing rapidly leading up to legalization, consistent with increasing cannabis use over time. 24 Several factors may have contributed to this trend, including changing social norms related to cannabis use and increasing access from illicit nonmedical and legal medical sources. 25 , 26 Hospitalizations decreased immediately following legalization, which may have been the result of decreased cannabis availability in the early phases of legalization due to national shortages of legal cannabis product and contraction in the illegal market (eg, increased enforcement activities and voluntary closures of illicit dispensaries while trying to open a legal store). 27 , 28 Hospitalizations began increasing again in early 2020, coinciding with a major expansion of retail access, an increasing variety of highly potent legal cannabis products, and the COVID-19 pandemic. 29 - 31 Disentangling COVID-19 from commercialization is challenging, but several factors support the theory that commercialization contributed to the observed increases. First, increases hospitalizations due to cannabis were far greater than all-cause hospitalizations and substance-use specific hospitalizations, suggesting that a factor other than pandemic influences on general substance use or health service use contributed. 32 Second, our sensitivity analysis using a commercialization starting point prepandemic (January 2020) showed similar results, suggesting that hospitalizations due to cannabis began increasing before the onset of the pandemic. Third, higher-potency cannabis products, which are associated with increased risk of harm, increased during the commercialization period following the introduction of new high-potency products starting in January 2020 (eg, vape pens and concentrates), along with a general trend of increasing tetrahydrocannabinol content in legal dried flower products since legalization. 33 , 34 The findings are also consistent with increases in ED visits and hospitalizations due to cannabis from US states that legalized nonmedical cannabis before the pandemic. 35 - 37
We observed substantial variation in changes over time in hospitalizations due to cannabis by province in Canada. Hospitalizations increased in all provinces over time in the lead-up to legalization. During the restricted legalization period, hospitalizations began decreasing over time in Ontario and British Columbia, which is consistent with legal sales data showing Ontario ($1.48 CAD) and British Columbia ($ 0.95 CAD) had the lowest per capita legal cannabis sales (average monthly sales in $CAD per individual 15 years and older) during the first year after legalization. Visits declined to a lesser extent in Quebec and did not change over time in Alberta, consistent with these provinces having 2 to 4 times higher legal sales over the first year (Alberta, $4.61 CAD and Quebec $2.27 CAD). 38 The greatest increases in hospitalizations due to cannabis during the commercialization/COVID-19 period were in Ontario and British Columbia, which had much larger legal cannabis sales growth between the final and first year of the study than Alberta and Quebec (see eFigure 2 in Supplement 1 for monthly cannabis sales over time). Our findings are also consistent with the prevalence of self-reported past 3-month cannabis use, which have not changed postlegalization in Quebec but have increased in Alberta, Ontario, and British Columbia. 39 Ongoing monitoring postpandemic and as the market continues to expand is needed.
To date, most studies examining changes in ED visits or hospitalizations due to cannabis postlegalization in Canada have either examined a single type of cannabis health care visit (eg, cannabis-induced psychosis) or aggregated visit types together. 9 - 13 , 40 Consequently, there is no data on direct comparisons on changes in different types of cannabis harms over time. We observed that cannabis-induced psychosis had the largest relative increase in rates of hospitalizations. Prior evidence suggests that one-third of individuals with first-presentation cannabis-induced psychosis will subsequently develop schizophrenia, raising concerns about potential important long-term impacts of legalization. 41 The largest absolute increase in rates of hospitalization was for harmful cannabis use. These increases in cannabis-induced psychosis and harmful cannabis use (eg, cannabis use disorders) are consistent with reported increases in daily cannabis after legalization use in Canada following legalization along with the availability of higher-potency cannabis products both of which increase the risk of adverse events. 33 , 34 , 42
Our findings have important policy implications within Canada and other countries considering legalizing cannabis. They suggest that cannabis legalization with strict controls may not cause any immediate change in rates of hospitalizations and may even have a modest public health benefit, as legalization in this study was associated with a decrease in cannabis-related health service use visits. However, our findings also caution that commercialization and rapid expansion of the cannabis retail market may reverse these benefits with consistent increases in hospitalizations due to cannabis across the different provincial regulatory approaches in Canada. 43
This study has limitations. First, as previously discussed, the close timing of the COVID-19 pandemic and the cannabis retail market commercialization prevent causal attribution of either event to the observed changes. 32 Second, because of coding changes (migration from ICD-9 to ICD-10 in April 2019) we excluded hospitalizations in specialized mental health hospitals from Ontario, the most populous province in Canada. Consequently, our study underestimates the population-level rate of hospitalizations due to cannabis in Ontario and when aggregated at the national level. Third, greater physician awareness and willingness of patients to disclose cannabis use after legalization could contribute to observed increases. However, this bias is unlikely to be responsible for changes observed in the study (eg, initial decline followed by an increase). Fourth, while the codes used to identify hospitalizations due to cannabis are part of an established indicator, further research is needed to understand their ability to differentiate specific presentations. 6 Fifth, there were large differences in rates of hospitalizations due to cannabis between provinces which likely reflect both health system differences (eg, bed capacity) and differences in documentation of cannabis harms. While this variation does not challenge within-province comparisons, it does limit comparability between provinces. Sixth, use of aggregate health administrative data limited our ability to investigate important clinical questions (eg, whether increases were related to new cannabis use disorders or exacerbation of existing ones), and further research using alternative designs is indicated.
In this cross-sectional study, hospitalizations due to cannabis were increasing prelegalization and may have increased further following the legalization of nonmedical cannabis use by adults in Canada. The findings suggest that the initial period of time following legalization in Canada with tightly controlled products and limited store access was not associated with increases in hospitalizations due to cannabis. In contrast, there is some evidence to support that the period in which stores and products expanded was associated with increases in cannabis hospitalizations, particularly for cannabis-induced psychosis. Importantly, the overlap of store and product expansion and the COVID-19 pandemic challenge attribution of increases. Ongoing surveillance efforts are needed, but restrictions on product type and store access may be reasonably precautionary measures for jurisdictions consideration legalization.
Accepted for Publication: August 23, 2023.
Published: October 5, 2023. doi:10.1001/jamanetworkopen.2023.36113
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Myran DT et al. JAMA Network Open .
Corresponding Author: Daniel T. Myran, MD, MPH, Clinical Epidemiology Program, Ottawa Hospital Research Institute, 1053 Carling Ave, Box 693, Ottawa, ON K1Y 4E9, Canada ( [email protected] ).
Author Contributions: Dr Myran and Mr Talarico had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design : All authors.
Acquisition, analysis, or interpretation of data : Myran, Konikoff, Talarico, Pacula.
Drafting of the manuscript : Myran, Gaudreault, Konikoff.
Critical review of the manuscript for important intellectual content : Myran, Konikoff, Talarico, Pacula.
Statistical analysis : Myran, Talarico.
Obtained funding : Myran.
Administrative, technical, or material support : Gaudreault, Konikoff, Talarico.
Supervision : Myran.
Conflict of Interest Disclosures: Dr Myran reported grants from Canadian Institutes of Health Research during the conduct of the study. No other disclosures were reported.
Funding/Support: This study was supported by a grant from the Canadian Centre on Substance Use and Addiction and fellowships from the Canadian Institutes of Health Research and the University of Ottawa Department of Family Medicine (Dr Myran).
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information. The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Marijuana and Cannabinoids: Health, Research and Regulatory Considerations (Position Paper)
Executive summary.
Marijuana and related substance misuse are complex issues impacting family medicine, patient health, and public health. The American Academy of Family Physicians (AAFP) believes family physicians are essential in addressing all forms of inappropriate substance use. The AAFP urges its members to be involved in the diagnosis, treatment, and prevention of substance use, as well as secondary diseases impacted or caused by use. The World Health Organization (WHO) reports approximately 2.5% of the global population uses cannabis annually, making it the most commonly used drug worldwide. 1 Simultaneously, the AAFP acknowledges preliminary evidence indicates marijuana and cannabinoids may have potential therapeutic benefits, while also recognizing subsequent negative public health and health outcomes associated with cannabis use. 2
During the 20 th century, law enforcement and public policy activities have undermined opportunities for scientific exploration. Barriers to facilitating both clinical and public health research regarding marijuana is detrimental to treating patients and the health of the public. The lack of regulation poses a danger to public health and impedes meaningful, patient-centered research to exploring both therapeutic and negative impacts of marijuana and cannabinoids.
Relevant AAFP Policy
Marijuana Possession for Personal Use The American Academy of Family Physicians (AAFP) opposes the recreational use of marijuana. However, the AAFP supports decriminalization of possession of marijuana for personal use. The AAFP recognizes the benefits of intervention and treatment for the recreational use of marijuana, in lieu of incarceration, for all individuals, including youth. 3
The AAFP also recognizes that several states have passed laws approving limited recreational use and/or possession of marijuana. Therefore, the AAFP advocates for further research into the overall safety and health effects of recreational use, as well as the effects of those laws on patient and societal health. 4
It should be noted that cannabis and marijuana are not interchangeable terms. In this position paper, cannabis is an overarching term used to refer to the plant Cannabis sativa . Substances derived from the cannabis plant include marijuana, hemp, and cannabinoids.
Call to Action Family physicians have a vested interest in policies that advance and protect the health of their patients and the public. The regulatory environment surrounding cannabis, medical and recreational marijuana, and cannabidiol (CBD) is rapidly changing, along with the retail environment. This shift has not been accompanied by robust scientific research regarding the health effects of cannabis, both therapeutic or detrimental. The AAFP recognizes the need for substantial clinical, public health, and policy evidence and research regarding cannabis, marijuana, cannabinoids, and CBD to inform evidence-based practice and the impact on public health.
- The AAFP promotes a society which is free of substance misuse, including alcohol and drugs. 3
- The AAFP recognizes there is support for the medical use of marijuana and cannabinoids, but advocates that usage be based on high-quality, evidence-based public health, policy, and patient-centered research, including the impact on vulnerable populations. 3
- The AAFP advocates for further studies into the use of medical marijuana and related compounds. This process should also ensure appropriate funding allocated for this research.
- The AAFP calls for decreased regulatory barriers to facilitate clinical and public health cannabis research, including reclassifying cannabis from a Schedule I controlled substance. 3
- The AAFP advocates for further research into the overall safety and health effects of recreational use, as well as the impact of legal recreational marijuana use laws on patient and societal health. 4
- The AAFP advocates for robust regulation regarding labeling and child-proof packaging of all marijuana and cannabinoid products.
- The AAFP opposes the recreational use and legalization of marijuana, but supports decriminalization of marijuana for personal use. The AAFP recognizes the benefits associated with intervention and treatment, in lieu of incarceration. 4
- The AAFP advocates for regulation regarding marketing claims, labeling, and advertising of all marijuana and cannabinoid products.
- The AAFP supports requirements testing current marijuana and cannabinoid products for safety, dosing, and product consistency.
In the Exam Room
- The AAFP urges its members to be involved in the diagnosis, treatment, and prevention of substance use, as well as the secondary diseases impacted by use.
- The AAFP calls for family physicians to discuss the health consequences of marijuana and cannabis use, as well as prevention strategies to prevent use and unintended consequences of marijuana exposure in at-risk populations.
Cannabis use, both medically and recreationally, is prevalent throughout history. Extensive evidence indicates cannabis was used by ancient civilizations, dating back more than 5,000 years ago. 1 In the U.S. in the 19th and early 20th centuries, cannabis was frequently used for medicinal purposes, often prescribed by clinicians. 1,5 Cannabis was first listed in the United States Pharmacopoeia in 1851, indicating use as an analgesic, hypnotic, and anticonvulsant agent. 5 After the 1937 Marihuana Tax Act , in 1942, cannabis was removed from the United States Pharmacopoeia . 5
Attitudes and perceived risk of marijuana use have changed with the varying levels of legalization in the U.S. Surveying marijuana use is essential to gauge public health implications of increased access to marijuana, cannabinoid, and cannabis products. According to the 2018 National Institute on Drug Abuse (NIDA) Monitoring the Future Survey (MTF), daily, past month, past year, and lifetime marijuana use among 8 th graders has declined, and remained unchanged in 10 th and 12 th graders, when compared to the 2013 MTF survey. 6 Despite the changing landscape of marijuana regulations nationwide, past year use of marijuana reached and maintained its lowest levels in more than two decades in 2016 among 8 th and 10 th graders. 6 However, marijuana vaping did significantly increase between 2017 and 2018, mirroring trends in youth tobacco use. 6 The NIDA 2017 National Survey on Drug Use and Health indicates nearly 53% of adults between the ages of 18-25 have tried marijuana at some point in their lifetime, 35% have used marijuana within the past year, and 22% within the past month. 7 While the lifetime use remains relatively stable for this cohort, from 2015-2017, past year and past month use increased 2.7% and 2.3%, respectively. 7 Nearly half of adults 26 or older reported using marijuana at some point in their lifetime. 7 Although adults ages 26 and up report the highest percentage of lifetime use, this age group has a significantly lower past year use (12%) and past month use (8%). 7
Forms and Use of Cannabis The cannabis plant, Cannabis sativa , is comprised of both non-psychoactive and psychoactive chemicals called cannabinoids. 5 The cannabinoid commonly known for its psychoactive properties is delta-9-tetrahydrocannabinol (THC). 5 CBD is the most abundant cannabinoid in cannabis, and is considered to be largely non-psychoactive. 5 The biological system responsible for the synthesis and degradation of cannabinoids in mammals is referred to as the endocannabinoid system, which is largely comprised of two g-coupled protein receptors (GPCRs). 8 The GPCRs—CB1 and CB2—are found throughout many bodily tissues. However, CB1 is most concentrated in the neural tissues. 5,8 CB2 receptors are found in the brain, but are mostly found in immune cells, like macrophages, microglia, osteoclasts, and osteoblasts. 5,8
There are many forms of, and products derived from, the Cannabis sativa plant, including hemp, CBD, and marijuana. Cannabis sativa with less than 0.3% THC is considered industrial hemp, and can be used for industrial agriculture cultivation. 9,10 Industrial hemp can be harvested and used for many things, including fibers for textiles, food products, and building materials. 11,12 CBD, the non-psychoactive cannabinoid, is extracted from the flower of industrial hemp. 13 Marijuana and hemp, technically speaking, are the same plant. 13 However, the hemp variety of cannabis contains no more than 0.3% THC, while the marijuana variety contains 5-20% THC. 13
Marijuana and CBD are most commonly used via inhalation, ingestion, and topical absorption. 5 Inhalation can be through combustible mechanisms using dried flowers, including the use of a pipe, rolled joints, blunts, and water pipes (also called bongs). 14 Vaping marijuana and CBD concentrates are an increasingly popular inhalation method. 5,6 Concentrates, the concentrated form of marijuana and CBD, come in various forms, including oil, butter, or a dark sticky substance often referred to as shatter. 15 Concentrates can be both smoked or vaporized, and may also be used as additives or cooking agents for ingestion. 5,15 There are many different ways to ingest cannabinoids. Food products—called edibles—like brownies, gummies, cookies, and candies are common forms of cannabis ingestion, as well as liquid forms like juices, soda, and tea. 5,16 Tinctures are liquid, ultra-concentrated alcohol-based cannabis extracts commonly applied in and absorbed through the mouth. 17 Topical cannabis is applied to, and absorbed through, the skin in a cream or salve form. 18
Routes or methods of administration affect cannabis delivery. When cannabis is smoked or vaporized, onset of effect is within 5-10 minutes with a duration of 2-4 hours. 19 When ingested, effect is within 60-180 minutes with a duration of 6-8 hours. 19 The oromucosal route has an onset of 15-45 minutes and a duration of 6-8 hours. 19 Topical administration of cannabis or cannabinoids has variable onset and duration. 19 The smoked or vaporized method offers the more rapid activity for acute symptoms with the topical preparations offering less systemic effects. 19
Health Effects of Cannabis
Although there is preliminary evidence indicating cannabinoids may have some therapeutic benefit, a large portion of the evidence is very limited for many reasons. These include small sample sizes, lack of control groups, poor study design, and the use of unregulated cannabis products. There are also clear negative health and public health consequences that must be considered, as well as the need for a significant increase in evidence. More research is needed to create a robust evidence base to weigh the potential therapeutic benefits against potential negative impacts on health and public health. Currently, there are three medical formulations of cannabis approved for use in the U.S.; dronabinol, nabilone, and epidiolex. 20 Nabiximols is approved for use in the United Kingdom. 21 Dronabinol is delta-9 THC and ingested as either an oral solution or an oral capsule. 22 Nabilone is an oral capsule containing synthetic THC. 23 Epidiolex is a CBD oral solution. 24 Nabiximols is an oral mucosa spray containing the cannabinoids THC and CBD. 25
In 2015, Whiting, et al, performed a meta-analysis and systematic review of research on the medical use of cannabis. 25 This systematic review served as the basis for many recommendations in 2017 by the National Academy of Science, Engineering, and Health Report on medical marijuana. 5 Dronabinol, nabilone, and nabiximols were included in the studies. However, other cannabis formulations were found in research trials, including CBD, marijuana, and other cannabinoids. 26 Evidence is most substantial for nausea and vomiting associated with chemotherapy, chronic pain treatment, multiple sclerosis spasticity, and intractable seizures associated with Dravet syndrome and Lennox-Gastaut syndrome. 27 There is moderate evidence for the use of cannabinoids for sleep and limited evidence for use in psychiatric conditions, such as post-traumatic stress disorder, depression, anxiety, and psychosis; appetite stimulation and weight gain; and no evidence for cancer treatment. 5
Dronabinol and nabilone were both approved in 1985 for use in treating refractory chemotherapy-induced nausea and vomiting. 5,23 Dronabinol is approved by the Food and Drug Administration (FDA) for appetite stimulation and weight gain, despite limited and often inconclusive evidence that it or other cannabinoids are effective. 22 This drug has traditionally been used in human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) patients to mitigate weight loss and to treat anorexia-cachexia syndrome associated with cancer and anorexia nervosa. 5,22
Cannabinoids have been assessed for chronic pain management. Many forms of chronic pain management were studied, including cancer and chemotherapy-induced pain, fibromyalgia, neuropathic pain, rheumatoid arthritis, non-cancer pain, and musculoskeletal pain. Several studies indicate smoked THC and nabiximols were both associated with pain reduction. 5,25,26 There is limited, mixed evidence regarding the viability of cannabinoids for some forms of chronic pain management. 5 However, limitations exist with these studies, including the variable doses of THC and CBD; unregulated, non-FDA approved products; and conflicting evidence. Studies assessing cannabinoids in treating the spasticity due to multiple sclerosis or paraplegia have mixed results. The cannabinoids nabiximols, dronabinol, and TCH/CBD have all been associated with decreased spasticity. Nabilone and nabiximols were the only drugs with statically-significant decreases. 2,25
In 2018, the FDA approved a cannabidiol oral solution called epidiolex for the treatment of refractory seizures associated with Dravet syndrome and Lennox-Gastaut syndrome. 28 Epidiolex was associated with significant seizure reduction when compared to placebo. 29–31 Dravet syndrome and Lennox-Gastaut syndrome are disorders associated with severe seizures, impaired cognitive skills and development, and uncontrollable muscle contractions. 29–31
Moderate evidence exists for the use of cannabis for sleep. Nabilone and nabiximols have been associated with improvement in sleep from a baseline and sleep restfulness. 2,5,25 Improved sleep was also considered a secondary outcome when evaluating other conditions (chronic pain, multiple sclerosis) with various cannabinoids. 2,5,25
There is limited evidence for the use of cannabis or cannabinoids for the treatment of post-traumatic stress disorder (PTSD), anxiety, depression, or psychosis. Of the limited evidence, nabilone was associated with a decrease in PTSD related nightmares. 5,25 One small study indicated CBD improved public speaking anxiety. 5 There are no studies directly evaluating the effectiveness of cannabis in the treatment of depression. However, some studies measured depression as a secondary outcome, but indicated no difference in depression when compared to placebo. 25 Limited evidence (two studies) have shown no difference in treating psychosis with CBD, amisulpride, or placebo. 25 Evidence indicates individuals who use marijuana are more likely to experience temporary psychosis and chronic mental illness, including schizophrenia. 5,32
There was no evidence or insufficient evidence for the use of cannabis or cannabinoids in the treatment of cancer; neurodegenerative disorders like Huntington’s chorea, Parkinson’s disease, or amyotrophic lateral sclerosis; irritable bowel syndrome; or addiction. 5
Cannabis overdose is rare in adults and adolescents. 33 Children who experience acute intoxication from cannabis generally ingest marijuana or other cannabinoids through experimentation. 33 When compared to adults and adolescents, children are more likely to experience life-threatening symptoms of acute cannabis intoxication, which may include depressed respiration rates, hyperkinesis, or coma. 33 Management consists of supportive care dependent on the manifestation of symptoms. 33 Adults and adolescents may experience increased blood pressure and respiratory rates, red eyes, dry mouth, increased appetite, and slurred speech. 33
Negative health effects are also associated with marijuana and cannabinoid use. Frequent marijuana use has been associated with disorientation. In teens, it has been linked with depression, anxiety, and suicide. 5,32 However, this is not a proven causal relationship. Lung health can also be negatively impacted depending on the delivery mechanism. 34 Smoking marijuana can cause lung tissue scarring and damage blood vessels, further leading to an increased risk of bronchitis, cough, and phlegm production. 34 This generally decreases when users quit. 34
Secondhand smoke is a serious issue associated with marijuana use. However, there is limited evidence on how it impacts heart and lung health. 34 Detectable THC has been found in children who live in the home or have a caretaker who use marijuana, subjecting children to developmental risks of THC exposure. 35 Fetal, youth, and adolescent exposure to THC is associated with negative health effects, including impacting brain development. 34 There is inconsistent, insufficient evidence to determine the long-term effects of marijuana and cannabinoid use while breastfeeding. 36 However, THC has been detected in breast milk for up to six days post-cannabinoid use, and exposure to cannabinoids is known to impact development in children. 37 Evidence also suggests cannabis use during pregnancy may be linked with preterm birth. 38 Cardiovascular health may be impacted by smoked marijuana use. However, the negative health effects are associated with the harmful chemicals in smoke similar to tobacco smoke. 34
Approximately 9% of all individuals who use marijuana develop an addiction, which is variable by age of first use and frequency of use. 34 That number for addiction jumps to 17% for individuals who begin using marijuana as teenagers and 25-50% of those who smoke marijuana daily. 34 Marijuana use does not typically lead to harder drug use, like cocaine and heroin, in most individuals. 39 Further research is needed to evaluate any potential gateway effect. 39
Mental health outcomes associated with marijuana use include an increased risk of anxiety and depression. Marijuana has been linked to schizophrenia, psychoses, and advancing the trajectory of the disease, particularly in individuals with pre-existing genetic indicators. 5,34 Global research also suggests daily use of high-potency marijuana increases risk for psychotic episodes among individuals with no underlying mental health condition. 40 While it is widely accepted that marijuana acutely impairs cognitive function, studies suggest differential outcomes regarding short- versus long-term cognitive impairment. 34
Research Considerations
The regulatory environment surrounding cannabis, marijuana, and cannabinoid research creates barriers detrimental to facilitating meaningful medical, public health, policy, and public safety research. Approval for research expands beyond institutional review boards. Due to the Schedule I classification by the Drug Enforcement Agency (DEA), researchers seeking to investigate health effects associated with cannabis must follow a regimented application process. 41 Applicants must submit an Investigational New Drug (IND) application to the FDA, which will then be reviewed to determine scientific validity and research subjects’ rights and safety. 42 Researchers must also follow the NIDA regulatory procedures for obtaining cannabis for research purposes. 41 Researchers may only use cannabis supplied by the University of Mississippi, the single NIDA-approved source for cannabis research. 41 Requiring research to rely on one source of cannabis limits availability and the variety of products. While the University of Mississippi cultivates different strains of cannabis, it is unable to supply the vast array of strains of cannabis found in the evolving retail environment with varying levels of THC, CBD, and cannabinoid content. 5 Substantial funding and capacity is required for researchers to obtain all regulatory approval and remain in compliance while conducting cannabis-related research. The required processes and procedures present a serious burden, dissuading researchers from pursuing cannabis-related projects. This has led to a lack of empirical evidence regarding a myriad of health-related issues, including potential therapeutic benefits of cannabis, public health impact, health economics, and the short- and long-term health effects from cannabis use.
In order to address the research gaps associated with both beneficial and harmful effects of cannabinoids used in both medical and recreational capacities, the AAFP calls for a comprehensive review of processes and procedures required to obtain approval for cannabis research.
The AAFP encourages the appropriate regulatory bodies, such as the DEA, NIDA, FDA, Department of Health and Human Services (DHHS), National Institutes of Health (NIH), and the Centers for Disease Control and Prevention (CDC), to collaborate with non-governmental stakeholders to determine procedures to decrease the burden of cannabis-related research while maintaining appropriate regulatory safety guards. This should include a reclassification of marijuana from Schedule I to facilitate clinical research. The AAFP calls for increased funding from both public and private sectors to support rigorous scientific research to address gaps in evidence regarding cannabis to protect the health of the public and inform evidence-based practices. 3 Future research should address the impact of cannabis use on vulnerable and at-risk populations.
Regulatory Considerations
While cannabis was federally regulated in 1906 for consumer and safety standards and labeling requirements, the Marihuana Tax Act of 1937 was the first federal regulation to impose a fine or imprisonment for non-medical use and distribution of cannabis. 5 The tax act also regulated production, distribution, and use of cannabis, further requiring anyone dealing with cannabis to register with the federal government. 5 In 1970, the DEA classified marijuana as a Schedule I drug, which is defined as a drug with no current acceptable medical use and a high potential for abuse. 43 Other Schedule 1 drugs include heroin, lysergic acid diethylamide (LSD), 3,4-methylenedioxymethamphetamine (ecstasy), methaqualone, and peyote. 43 Since this class of substances is determined as having no medical usage, they cannot be legally prescribed and thus, there is no medical coverage for them.
Marijuana is illegal under federal law. Penalties cover possession, sale, cultivation, and paraphernalia. However, the Agriculture Improvement Act of 2018 included a U.S. Department of Agriculture (USDA) Hemp Production Program, removing hemp from the Controlled Substances Act. 10,44 As a result, CBD sourced from hemp plants containing no more than 0.3% THC is legal to produce. 10,44 The FDA has approved three medications containing cannabinoids: epidiolex (CBD), dronabinol, and nabilone (synthetic cannabinoids). 5 No other forms of cannabis are currently regulated by the FDA. The AAFP calls upon the FDA to take swift action to regulate CBD and cannabinoid products now legal in order to protect the health of the public.
States have separate marijuana, cannabinoid, and cannabis laws, some of which mirror federal laws, while others may be more harsh, or have decriminalized and even legalized marijuana and cannabis. 45 In 1996, California was the first state to legalize the medical use of marijuana. 46 States have subsequently decriminalized and/or legalized cannabinoids, medical marijuana, and recreational marijuana. 46 As of August 2019, 30 states, along with the District of Columbia, Guam, and Puerto Rico have legalized marijuana in varying forms. 46 Decriminalization laws may include reduction of fines for possession of small amounts of marijuana, reclassification of criminal to civil infractions, excluding the infraction from criminal records and expunging prior offenses and convictions related to marijuana. 47 Thirty-three states, along with the District of Columbia, Guam, Puerto Rico, and the U.S. Virgin Islands have a comprehensive, publicly-available medical marijuana/cannabis program, and 13 of these states have also removed jail time for possessing small amounts of non-medical marijuana. 47 Adult recreational marijuana use is legal in 13 states and the District of Columbia. 47 Vermont and the District of Columbia, however, do not allow the sale of marijuana for recreational purposes. This means it is not a crime to use and possess marijuana recreationally, but commercial sales are not allowed. 47 States have also authorized the sale of products that have low levels of THC, but high levels of CBD. These products are widely available in retail locations, but are highly unregulated. 47 The benefits of CBD touted by the public and retailers are largely anecdotal. The vast majority of these claims are not substantiated by valid research.
Decriminalizing and legalizing marijuana can decrease the number of individuals arrested and subsequently prosecuted for possession and/or use. 48 However, evidence suggests that these practices are not applied equitably. People of color are more likely to be arrested and prosecuted for marijuana possession despite overall decreased arrest rates. 48 Incarceration impacts health. People who are incarcerated have significantly higher rates of disease than those who are not, and are less likely to have access to adequate medical care. 49
The AAFP “opposes the recreational use of marijuana. However, the AAFP supports decriminalization of possession of marijuana for personal use. The AAFP recognizes the benefits of intervention and treatment for the recreational use of marijuana, in lieu of incarceration, for all individuals, including youth.” 4 The AAFP calls for family physicians to advocate to prevent unnecessary incarceration by diverting eligible people from the justice system to substance abuse and/or mental health treatment. 49
There are many public health considerations when regulating cannabis products. Serious public health concerns include impaired driving, youth exposure to advertisements, and accidental poisoning in children. Second to alcohol, marijuana is the most common illicit drug associated with impaired driving and accidents. 34 Marijuana slows reaction time and decision making, substantially increasing risk for traffic accidents. 50 Some states have a zero-tolerance policy, where there is no allowable detectable level of THC while driving, while other states have set five nanograms per milliliter or higher limits of THC, or minimally-detectable amounts of THC. 51
Evidence indicates adolescents who are exposed to medical marijuana advertising are more likely to have positive views of and subsequently use marijuana. 52 Those exposed to medical marijuana advertising were more likely to report past use and expectant future use. 52 These adolescents also reported agreeing with statements like, marijuana helps people relax and get away from their problems. 52 Adolescent exposure to medical marijuana advertising was also associated with self-reporting negative consequences associated with marijuana use, including missing school and concentration issues. 52 The AAFP calls for immediate regulation of advertising of all marijuana and cannabinoid products to decrease youth exposure to aid in preventing initiation and subsequent use of marijuana.
Children are most susceptible to severe effects associated with marijuana poisoning, including decreased coordination, lethargy, sedation, difficulty concentrating, and slurred speech. 53 Exposure may also include serious, potentially life-threatening symptoms like respiratory distress and coma. 33 Unintentional exposures to marijuana in children have increased each year since 2012, likely due to legalization policies across the U.S. and popularity of edibles. 53 Edibles often look exactly like their non-THC counterparts, and come in brightly colored packaging appealing to children, often mimicking candy products. 53 Effective legislation requiring childproof packaging for edible products can help mitigate and prevent unintentional exposure in children. 54 Family physicians should discuss safe storage of all cannabis products with their patients who live with children. 54 Under the Child Abuse Prevention and Treatment Act (CAPTA), physicians are mandated reporters of suspected child abuse and neglect. 55 The 2010 law requires states to enact laws for reporting substance use-exposed infants to child protective services. 55
Family physicians play a key role in addressing marijuana, cannabinoid, and cannabis product use; reducing barriers to research; and advocating for appropriate policy to protect the health of patients and the public.
Family physicians can address the inappropriate use of marijuana, cannabinoid, and cannabis products. Family physicians should discuss safe storage of all cannabis products with patients who live with or serve as primary caregivers for children to prevent unintended exposure. 56 It is important to discuss the developmental and negative impacts of marijuana and cannabis products with individuals who are or can become pregnant, children, and adolescents. Family physicians should also emphasize the serious consequences of impaired driving and marijuana intoxication.
It is essential to decrease barriers to research all forms of marijuana, cannabis, and cannabinoids, including a reclassification of cannabis as a Schedule I drug. High-quality research regarding the impact on patients, public health, society, and health policy are essential to providing patient-centered care and promoting evidence-based public health practices. Immediate regulations for marijuana and cannabinoid products, including CBD, like product safety and consistency safeguards, child-proof packaging, labeling, marketing claims and advertising, and impairment standards are vital for consumer safety and injury prevention. Regulatory measures focused on preventing youth initiation of marijuana and cannabinoid product use must be prioritized to prevent a public health epidemic.
The health benefits associated with intervention and treatment of recreational marijuana and cannabinoid use, in lieu of incarceration, is an important policy consideration.
Utilizing an interdisciplinary, evidence-based approach to addressing both medical and recreational marijuana and cannabis use is essential to promote public health, inform policy, and provide patient-centered care. Family physicians, in partnership with public health and policy professionals, can play an imperative role in addressing the changing landscape of marijuana and cannabis products.
- Bridgeman MB, Abazia DT. Medicinal cannabis: history, pharmacology, and implications for the acute care setting. P T . 2017;42(3):180-188. Accessed August 20, 2019.
- Abrams DI. The therapeutic effects of cannabis and cannabinoids: An update from the National Academies of Sciences, Engineering and Medicine report. Eur J Intern Med . 2018;49:7-11.
- American Academy of Family Physicians. Substance abuse and addiction . Accessed August 20, 2019.
- American Academy of Family Physicians. Marijuana possession for personal use . Accessed August 20, 2019.
- The National Academies of Science, Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids . Washington, D.C.: National Academies Press; 2017.
- National Institute on Drug Abuse. DrugFacts: Monitoring the Future Survey: high school and youth trends. www.drugabuse.gov/publications/drugfacts/monitoring-future-survey-high-school-youth-trends. Accessed August 20, 2019.
- National Institute on Drug Abuse. National Survey of Drug Use and Health . Accessed August 20, 2019.
- Mackie K. Cannabinoid receptors: where they are and what they do. J Neuroendocrinol . 2008;20(s1):10-14.
- Hilderbrand RL. Hemp & cannabidiol: what is a medicine? Mo Med . 2018;115(4):306-309. Accessed August 20, 2019.
- U.S. Department of Agriculture. Hemp production program . Accessed August 20, 2019.
- Heidi H. Oregon State University launches largest, most comprehensive hemp research center in the nation. Oregon State University. www.today.oregonstate.edu/news/oregon-state-university-launches-largest-most-comprehensive-hemp-research-center-nation. Accessed August 20, 2019.
- Lee MJ. The legalization of hemp. Accessed August 20, 2019.
- Shipman M. Is hemp the same thing as marijuana? NC State University. Accessed August 20, 2019.
- National Institute on Drug Abuse. What is marijuana? Accessed August 20, 2019.
- Drug Policy Alliance. Marijuana concentrates. Accessed August 20, 2019.
- MacCoun RJ, Mello MM. Half-baked — the retail promotion of marijuana edibles. N Engl J Med . 2015;372(11):989-991.
- Peschel W, Peschel, Wieland. Quality control of traditional cannabis tinctures: pattern, markers, and stability. Sci Pharm . 2016;84(3):567-584.
- Rosenblatt S, Tucker J, DeAngelo S. Methods and compositions of cannabis extracts. Accessed August 20, 2019.
- MacCallum CA, Russo EB. Practical considerations in medical cannabis administration and dosing. Eur J Intern Med . 2018;49:12-19.
- U.S. Food and Drug Administration. FDA regulation of cannabis and cannabis-derived products: questions and answers . Accessed August 20, 2019.
- National Cancer Institute. NCI Drug Dictionary. Nabiximols. Accessed August 20, 2019.
- U.S. Food and Drug Administration. Syndros (dronabinol) oral solution . Accessed August 20, 2019.
- U.S. Food and Drug Administration. CESAMETTM (nabilone) capsules. Accessed August 20, 2019.
- Greenwich Biosciences. Epidiolex® (cannabidiol). www.epidiolex.com/. Accessed August 20, 2019.
- Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use. A systematic review and meta-analysis. JAMA . 2015;313(24):2456-2473.
- Abuhasira R, Shbiro L, Landschaft Y. Medical use of cannabis and cannabinoids containing products – Regulations in Europe and North America. Eur J Intern Med . 2018;49:2-6.
- Devinsky O, Cilio MR, Cross H, et al. Cannabidiol: pharmacology and potential therapeutic role in epilepsy and other neuropsychiatric disorders. Epilepsia . 2014;55(6):791-802.
- U.S. Food and Drug Administration. FDA approves first drug comprised of an active ingredient derived from marijuana to treat rare, severe forms of epilepsy. Accessed August 20, 2019.
- Devinsky O, Patel AD, Cross JH, et al. Effect of cannabidiol on drop seizures in the Lennox–Gastaut syndrome. N Engl J Med . 2018;378(20):1888-1897.
- Devinsky O, Cross JH, Laux L, et al. Trial of cannabidiol for drug-resistant seizures in the Dravet syndrome. N Engl J Med . 2017;376(21):2011-2020.
- Perucca E. Cannabinoids in the treatment of epilepsy: hard evidence at last? J Epilepsy Res . 2017;7(2):61-76.
- Volkow ND, Swanson JM, Evins AE, et al. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: a review. JAMA Psychiatry . 2016;73(3):292-297.
- Wang GS. Cannabis (marijuana): acute intoxication. UpToDate. Accessed August 20, 2019.
- Volkow ND, Baler RD, Compton WM, Weiss SRB. Adverse health effects of marijuana use. N Engl J Med . 2014;370(23):2219-2227.
- Wilson KM, Torok MR, Wei B, et al. Detecting biomarkers of secondhand marijuana smoke in young children. Pediatr Res . 2017;81(4):589-592.
- Reece-Stremtan S, Marinelli KA. ABM Clinical Protocol #21: Guidelines for Breastfeeding and Substance Use or Substance Use Disorder, Revised 2015. Breastfeed Med . 2015;10(3):135-141.
- Bertrand KA, Hanan NJ, Honerkamp-Smith G, Best BM, Chambers CD. Marijuana use by breastfeeding mothers and cannabinoid concentrations in breast milk. Pediatrics . 2018;142(3):e20181076.
- Corsi DJ, Walsh L, Weiss D, et al. Association between self-reported prenatal cannabis use and maternal, perinatal, and neonatal outcomes. JAMA . 2019;322(2):145-152.
- Centers for Disease Control and Prevention. Does marijuana use lead to other drug use? Accessed August 20, 2019.
- Di Forti M, Quattrone D, Freeman TP, et al. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. The Lancet Psychiatry . 2019;6(5):427-436.
- U.S. Food and Drug Administration. Marijuana research with human subjects . Accessed August 20, 2019.
- National Institute on Drug Abuse (NIDA). NIDA’s role in providing marijuana for research. www.drugabuse.gov/drugs-abuse/marijuana/nidas-role-in-providing-marijuana-research. Accessed August 20, 2019.
- U.S. Drug Enforcement Administration. Drug scheduling . Accessed August 20, 2019.
- U.S. Food and Drug Administration. Statement from FDA Commissioner Scott Gottlieb, M.D., on signing of the Agriculture Improvement Act and the agency's regulation of products containing cannabis and cannabis-derived compounds. Accessed August 20, 2019.
- American Bar Assocation. Conflicting state and federal marijuana laws create ethical complications for lawyers. Accessed August 20, 2019.
- National Conference of State Legislatures. Marijuana laws. www.ncsl.org/bookstore/state-legislatures-magazine/marijuana-deep-dive.aspx. Accessed August 20, 2019.
- National Conference of State Legislatures. Marijuana laws. Accessed August 20, 2019.
- Drug Policy Alliance. From prohibition to progress: a status report on marijuana legalization. Accessed August 20, 2019.
- American Academy of Family Physicians. Incarceration and health: a family medicine perspective (position paper) . Accessed August 20, 2019.
- Centers for Disease Control and Prevention. What you need to know about marijuana use and driving . Accessed August 20, 2019.
- National Conference of State Legislatures. Drugged driving | Marijuana-impaired driving . Accessed August 20, 2019.
- RAND Corporation. Adolescents who view more medical marijuana advertising are more likely to use marijuana, have positive views about the drug . Accessed August 20, 2019.
- Center on Addiction. Childhood poisoning: safeguarding young children from addictive substances. Accessed August 20, 2019.
- Center on Addiction. Toddlers and THC: the number of young children exposed to marijuana is on the rise. Accessed August 20, 2019.
- Child Welfare Information Gateway. Mandatory reporters of child abuse and neglect. Accessed August 20, 2019.
- Children’s Hospital Colorado. Marijuana safety in the home . Accessed August 20, 2019.
(July 2019 BOD)
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
24-17-An Ongoing Debate: Should Marijuana be Legal in the United States?

STUDENTS: Anna Ferraris and Cassie Dierolf
DESCRIPTION: Marijuana is widely used in the United States, with federal laws on its use being confusing and contradictory. This legal ambiguity creates uncertainty among Americans. Many argue for its legalization due to its medicinal benefits, potential to address social and racial disparities, and economic opportunities.
FACULTY ADVISOR: Littleton
COURSE: HHD 200N
No comments yet.
Leave a reply click here to cancel reply..
You must be logged in to post a comment.
Topics › Drug Policy
Marijuana legalization is not associated with increases in youth suicide rates
Youth suicide rates actually tend to drop following legal access to recreational and medical marijuana..

The Journal of the American Academy of Child & Adolescent Psychiatry (JAACAP) just published a paper that found that new marijuana legalization laws correlated with increases in suicide among youth. Although the authors likely did their math correctly, they may have chosen a modeling strategy that produced inaccurate results. The results also don’t explain how marijuana laws are connected to these suicide rate increases among youth when youth marijuana use did not increase after marijuana markets were established at the state level.
In the new publication, “ Association Between Marijuana Laws and Suicide Among 12- to 25-Year-Olds in the United States From 2000 to 2019 ”, Christopher J. Hammond, J. Madison Hyer, Anne E. Boustead, Mary A. Fristad, Danielle L. Steelesmith, Guy N. Brock, Deborah S. Hasin, and Cynthia A. Fontanella compared suicide mortality data to state-level marijuana legalization efforts, such as permitting regulated medical and recreational markets. The authors found that recreational marijuana laws were associated with a 9% increase in suicide rates among all youth ages 14 to 16. They also found that medical and recreational laws were associated with 10% and 16% increases in suicide rates among female youth ages 12 to 25, respectively.
My preprint study with Robert Capodilupo, Michael Schemenaur, and Jeffrey A. Singer found the opposite results among similar age groups—marijuana laws were associated with a decline in suicide rates. So why the difference?
The difference is due to technical concerns of statistical analysis. Concisely, the authors chose an inappropriate model given the data distribution. The methods in the Hammond study exaggerate the effect of marijuana laws on suicide rates in states with relatively few suicides. States that had not yet or never did legalize marijuana were more likely to have near-zero suicide rates, because suicide rates have increased across all states over time. Because of the model the authors selected, the JAACAP study shows that states with regulated marijuana markets have higher suicide rates, regardless of whether suicides have risen at faster rates in those states after their marijuana laws went into effect.
The new JAACAP study employed a negative binomial regression , which assumes that the plurality of states had zero suicides to begin with and then examines changes in the number of suicides in each state. In reality, suicides occur in every state, and the average state-level suicide rate is approximately 14 deaths per 100,000 population. Therefore, state-level suicide rates don’t follow a negative binomial distribution.
For example, consider the distributions of state-level suicide rates among males ages 15 to 19 in Figure 1 below, which we analyzed in our study. The raw data (on the left) almost follow a normal distribution in which observations are closely grouped around a median value. A negative binomial distribution, however, assumes the modal observation is a zero value. Many statistical models exist to help researchers match their approach to the data and, in theory, the distribution curve associated with any model should closely fit the shape of the data. In Figure 1, we superimpose the data shape implied by the two models over the data as a red line. In our preferred model (on the right), we have taken a natural log of the data and then treated it as a normal distribution. The data fits the normal distribution shape implied by the red line much better than the model used by the Hammond team. This means that a basic linear regression on log-transformed data is more appropriate for this type of analysis, lending greater credibility to our analysis and conclusions.
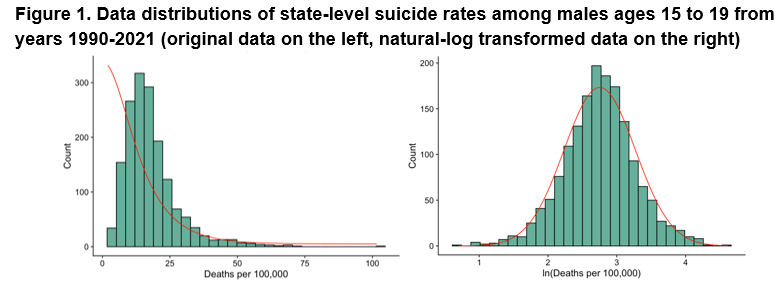
After transforming the data and controlling for various sociodemographic factors, such as personal income and unemployment, we found that suicide rates on average generally drop among female and male youth after states allow both medical and recreational marijuana access, although these results weren’t statistically significant for all of our robustness checks. Therefore, suicide rates tend to drop with greater marijuana access, but we can’t conclude that the policies themselves were the cause of the drop. However, suicide rates do predictively drop about 5.4% for males ages 30 to 39 following medical marijuana access, which drove reductions in the total male suicide rate ( table of our full results). To be clear, our results are all associations and should not necessarily be interpreted as causal, but the data show that suicide rates don’t increase after state laws allow for greater marijuana access.
Actual marijuana use by teens hasn’t changed with legalization, another strike against the Hammond study’s conclusion. If marijuana legalization led to changes in suicide rates among youth, you’d expect it to be because youth are using marijuana more often. However, our analysis also shows that rates of marijuana use among youth remained stable after states adopted recreational marijuana markets (Figure 2).
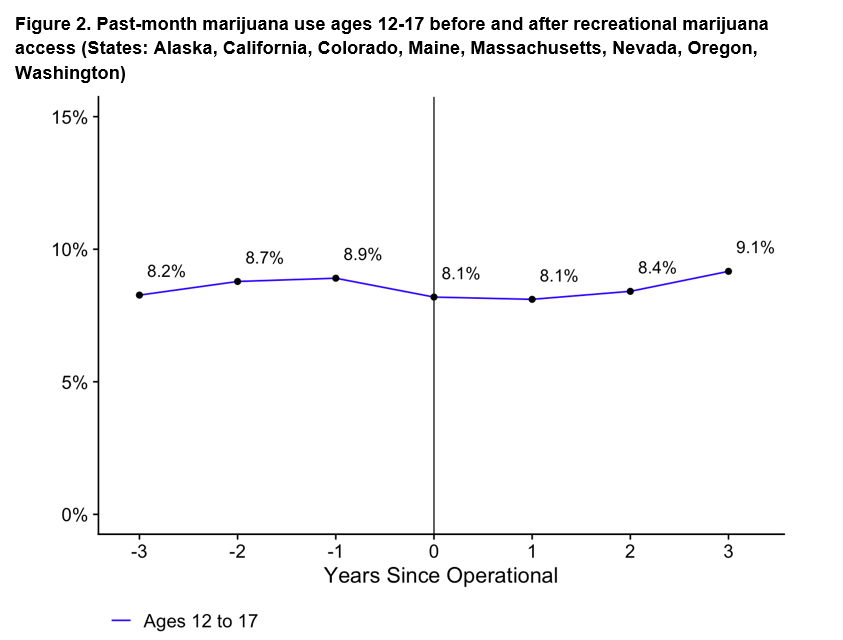
Inappropriate model selection is why conflicting results appear throughout the public health literature. In the case of suicide rates, our study rigorously shows that they tend to drop among youth following both recreational and medical marijuana access, which supports the original findings by Anderson et al. (2014) in the American Journal of Public Health .

IMAGES
VIDEO
COMMENTS
Introduction. Cannabis is one of the most widely used substances globally, with nearly 2.5% of the world population reporting past year cannabis use. 1 Cannabis use rates are particularly high in North America. In the U.S., 45% of individuals reported ever using cannabis and 18% reported using at least once annually in 2019. 2,3 In Canada, approximately 21% of people reported cannabis use in ...
Rebecca L. Haffajee. Amanda Mauri. Evidence regarding the effects of recreational cannabis legalization on public health is inconsistent. Future research should assess heterogeneous policy design ...
for Medicinal Cannabis Research, McMaster University & St. Joseph's Healthcare Hamilton, Hamilton, ON, Canada. 6Homewood Research Institute, Guelph, ON, Canada. ABSTRACT BACkgROUnd: Recreational cannabis legalization has become more prevalent over the past decade, increasing the need to understand its impact on downstream health-related outcomes.
Background Marijuana is the most commonly used illicit drug in the United States. More and more states legalized medical and recreational marijuana use. Adolescents and emerging adults are at high risk for marijuana use. This ecological study aims to examine historical trends in marijuana use among youth along with marijuana legalization. Method Data (n = 749,152) were from the 31-wave ...
INTRODUCTION. Before 2014, cannabis could not be legally sold or purchased for recreational purposes anywhere in the United States. By early 2022, more than 141 million Americans lived in a state with recreationally legal cannabis [].These rapid state-by-state changes in policy resulted in vastly different cannabis environments between states.
The Public Health Effects of Legalizing Marijuana D. Mark Anderson and Daniel I. Rees NBER Working Paper No. 28647 April 2021 JEL No. I1,I12,I18,K42 ABSTRACT Thirty-six states have legalized medical marijuana and 14 states have legalized the use of marijuana for recreational purposes.
Liberalized state-level recreational cannabis policies in the United States (US) fostered important policy evaluations with a focus on epidemiological parameters such as proportions [e.g., active cannabis use prevalence; cannabis use disorder (CUD) prevalence]. This cannabis policy evaluation project adds novel evidence on a neglected parameter-namely, estimated occurrence of newly incident ...
Key Points. Question Is recreational cannabis legalization (RCL) associated with a reduction in cannabis possession arrest rates in US states that have already decriminalized cannabis; if so, does this change differ by age and race?. Findings In this cross-sectional study using difference-in-differences analysis for data from 31 states, RCL was associated with a 40% reduction in cannabis ...
Background: Recreational cannabis legalization has become more prevalent over the past decade, increasing the need to understand its impact on downstream health-related outcomes. Although prior reviews have broadly summarized research on cannabis liberalization policies (including decriminalization and medical legalization), directed efforts are needed to synthesize the more recent research ...
Cannabis legalization has benefits, such as removing the product from the illegal market so it can be taxed and regulated, but science is still trying to catch up as social norms evolve and different products become available. In this Q&A, adapted from the August 25 episode of Public Health On Call, Lindsay Smith Rogers talks with Johannes ...
Overall, rates of cannabis use have shown long-term increasing trends among several age groups in North America. 7-9 Moreover, research has revealed recent cannabis use increases in at risk populations, such as individuals with depression and pregnant women. 10,11 Parallel to increased cannabis use over time, rates of cannabis-related consequences have also increased across Canada and the U.S ...
(March 2023) - Thirty-six states have legalized medical marijuana and 18 states have legalized the use of marijuana for recreational purposes. In this paper, we review the literature on the public health consequences of legalizing marijuana, focusing on studies that have appeared in economics journals as well as leading public policy, public ...
4 The average disease burden from drugs use is shown as follows for 2000 and 2016. DALYs 2000 (drug disorders) DALYs 2016 (drug disorders) however, Australia managed to reduce the disease burden ...
This paper summarizes the research on the impacts of cannabis decriminalization and legalization on the criminal justice system, specifically focusing on six impacts: 1) cannabis and other drug possession arrests, 2) racial disparities in cannabis-related arrests, 3) broader crime
As of 2018 there have been eight states in the United States legalize the recreational use. of Marijuana: Colorado, Washington, Nevada, California, Oregon, Alaska, Maine and. Massachusetts. This research paper is going to discuss the history of marijuana and why it was. originally made illegal throughout the United States.
Hospitalizations were increasing rapidly leading up to legalization, consistent with increasing cannabis use over time. 24 Several factors may have contributed to this trend, including changing social norms related to cannabis use and increasing access from illicit nonmedical and legal medical sources. 25,26 Hospitalizations decreased ...
The legalization of cannabis has both social and political implications. On the one hand, it has led to a decriminalization of cannabis use and reduced the burden on the criminal justice system. On the other hand, there are still concerns about the impact of cannabis use on health and the potential increase in drug use overall.
In this position paper, cannabis is an overarching term ... to facilitate clinical and public health cannabis research, ... a status report on marijuana legalization. Accessed August 20, 2019. ...
Pew Research Center
STUDENTS: Anna Ferraris and Cassie Dierolf DESCRIPTION: Marijuana is widely used in the United States, with federal laws on its use being confusing and contradictory. This legal ambiguity creates uncertainty among Americans. Many argue for its legalization due to its medicinal benefits, potential to address social and racial disparities, and economic opportunities.
The Journal of the American Academy of Child & Adolescent Psychiatry (JAACAP) just published a paper that found that new marijuana legalization laws correlated with increases in suicide among youth.Although the authors likely did their math correctly, they may have chosen a modeling strategy that produced inaccurate results. The results also don't explain how marijuana laws are connected to ...