
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.

3.3 Assignment
Nursing team members working in inpatient or long-term care settings receive patient assignments at the start of their shift. Assignment refers to routine care, activities, and procedures that are within the legal scope of practice of registered nurses (RN), licensed practical/vocational nurses (LPN/VN), or assistive personnel (AP). [1] Scope of practice for RNs and LPNs is described in each state’s Nurse Practice Act. Care tasks for AP vary by state; regulations are typically listed on sites for the state’s Board of Nursing, Department of Health, Department of Aging, Department of Health Professions, Department of Commerce, or Office of Long-Term Care. [2]
See Table 3.3a for common tasks performed by members of the nursing team based on their scope of practice. These tasks are within the traditional role and training the team member has acquired through a basic educational program. They are also within the expectations of the health care agency during a shift of work. Agency policy can be more restrictive than federal or state regulations, but it cannot be less restrictive.
Patient assignments are typically made by the charge nurse (or nurse supervisor) from the previous shift. A charge nurse is an RN who provides leadership on a patient-care unit within a health care facility during their shift. Charge nurses perform many of the tasks that general nurses do, but also have some supervisory duties such as making assignments, delegating tasks, preparing schedules, monitoring admissions and discharges, and serving as a staff member resource. [3]
Table 3.3a Nursing Team Members’ Scope of Practice and Common Tasks [4]
|
| ||
|---|---|---|
| RN |
| |
| LPN/VN | Tasks That Potentially Can Be Delegated According to the Five Rights of Delegation: | |
| AP |
|
An example of a patient assignment is when an RN assigns an LPN/VN to care for a client with stable heart failure. The LPN/VN collects assessment data, monitors intake/output throughout the shift, and administers routine oral medication. The LPN/VN documents this information and reports information back to the RN. This is considered the LPN/VN’s “assignment” because the skills are taught within an LPN educational program and are consistent with the state’s Nurse Practice Act for LPN/VN scope of practice. They are also included in the unit’s job description for an LPN/VN. The RN may also assign some care for this client to AP. These tasks may include assistance with personal hygiene, toileting, and ambulation. The AP documents these tasks as they are completed and reports information back to the RN or LPN/VN. These tasks are considered the AP’s assignment because they are taught within a nursing aide’s educational program, are consistent with the AP’s scope of practice for that state, and are included in the job description for the nursing aide’s role in this unit. The RN continues to be accountable for the care provided to this client despite the assignments made to other nursing team members.
Special consideration is required for AP with additional training. With increased staffing needs, skills such as administering medications, inserting Foley catheters, or performing injections are included in specialized training programs for AP. Due to the impact these skills can have on the outcome and safety of the client, the National Council of State Board of Nursing (NCSBN) recommends these activities be considered delegated tasks by the RN or nurse leader. By delegating these advanced skills when appropriate, the nurse validates competency, provides supervision, and maintains accountability for client outcomes. Read more about delegation in the “ Delegation ” section of this chapter.
When making assignments to other nursing team members, it is essential for the RN to keep in mind specific tasks that cannot be delegated to other nursing team members based on federal and/or state regulations. These tasks include, but are not limited to, those tasks described in Table 3.3b.
Table 3.3b Examples of Tasks Outside the Scope of Practice of Nursing Assistive Personnel
|
| |
|---|---|
| LPN/VN | refers to adjusting the dosage of medication until the desired effects are achieved.) |
| Assistive Personnel (AP) |
As always, refer to each state’s Nurse Practice Act and other state regulations for specific details about nursing team members’ scope of practice when providing care in that state.
Find and review Nurse Practice Acts by state at https://www.ncsbn.org/policy/npa.page .
Read more about the Wisconsin’s Nurse Practice Act and the standards and scope of practice for RNs and LPNs Wisconsin’s Legislative Code Chapter N6.
Read more about scope of practice, skills, and practices of nurse aides in Wisconsin at DHS 129.07 Standards for Nurse Aide Training Programs.
- American Nurses Association and NCSBN. (2019). National guidelines for nursing delegation . https://www.ncsbn.org/public-files/NGND-PosPaper_06.pdf ↵
- McMullen, T. L., Resnick, B., Chin-Hansen, J., Geiger-Brown, J. M., Miller, N., & Rubenstein, R. (2015). Certified nurse aide scope of practice: State-by-state differences in allowable delegated activities. Journal of the American Medical Directors Association, 16 (1), 20–24. https://doi.org/10.1016/j.jamda.2014.07.003 ↵
- RegisteredNursing.org. (2021, April 13). What is a charge nurse? https://www.registerednursing.org/specialty/charge-nurse/ ↵
- RegisteredNursing.org. (2021, January 27). Assignment, delegation and supervision: NCLEX-RN. https://www.registerednursing.org/nclex/assignment-delegation-supervision/ ↵
- State of Wisconsin Department of Health Services. (2018). Medication administration by unlicensed assistive personnel (UAP): Guidelines for registered nurses delegating medication administration to unlicensed assistive personnel. https://www.dhs.wisconsin.gov/publications/p01908.pdf ↵
Routine care, activities, and procedures that are within the authorized scope of practice of the RN, LPN/VN, or routine functions of the assistive personnel.
Making adjustments to medication dosage per an established protocol to obtain a desired therapeutic outcome.
Nursing Management and Professional Concepts Copyright © by Chippewa Valley Technical College is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book
Delegating vs. assigning: What you need to know
Registered nurses (RNs) often delegate to other RNs, licensed practical nurses/vocational nurses (LPN/LVNs), and assistive personnel (AP). (In some states or jurisdictions, LPN/LVNs may be allowed to delegate, so “licensed nurses” will be used in this article.) Delegating appropriately protects patients and reduces the risk of legal liability, yet the parameters of delegation often are not fully understood.
One common area of misunderstanding is delegation vs. assignment. Knowing the differences between the two is essential to ensure you delegate appropriately. The primary difference relates to scope of practice and where the clinician learned the activities to be carried out.
According to national guidelines for nursing delegation from the National Council of State Boards of Nursing (NCSBN) and American Nurses Association (ANA), an assignment refers to the “routine care, activities, and procedures that are within the authorized scope of practice of the RN or LPN/VN or part of the routine functions of the AP.” This definition covers fundamental skills that the assignee would have learned in a basic education program. A licensed nurse is still responsible for ensuring the assignment is carried out correctly.
According to the NCSBN/ANA guideline, delegation applies when the delegatee is performing a “specific nursing activity, skill, or procedure that is beyond the delegatee’s traditional role and not routinely performed.” As opposed to work that is part of an assignment, the work associated with delegation was not learned in a basic education program. Therefore, the delegatee must have obtained additional education and have verified competence in the delegated area for which they will be responsible. The licensed nurse maintains overall accountability for the patient, but the delegatee is responsible for the delegated activity, skill, or procedure.
Licensed nurses can’t delegate activities that involve clinical reasoning, nursing judgment, or critical decision making, and the delegated responsibility has to be within the delegator’s scope of practice under the state’s or jurisdiction’s nurse practice act (NPA).
Responsibilities
Organizational administrators, the delegator, and the delegatee each have responsibilities when an activity, skill, or procedure is delegated.
Professionals who work at the administrative or managerial level of the organization set the cultural tone for the nursing work environment and are responsible for managing the delegation processes. Those at the administrative level within an organization define what nursing responsibilities may be delegated, to whom, and under what set(s) of circumstances. They are also responsible for developing and maintaining policies and procedures associated with delegation, periodically evaluating the efficacy and safety of delegation processes, and training and educating staff.
The delegator is responsible for determining the needs of the patient, when delegation is appropriate, and if the delegatee is competent to complete the delegated task. Delegators must follow delegation guidelines in the NPA and relevant organizational policies and procedures. Clear communication is key, and the delegator must be available as a resource to the delegatee. Delegators also need to evaluate outcomes as they maintain overall accountability for the patient. Delegators must be prepared to step in at any point if it appears the delegatee is not handling the assignment appropriately. Any problems should be reported to nursing leadership.
The delegatee is responsible for only accepting activities that fall within their competence and that they feel comfortable completing safely. Delegatees must communicate with the delegator, particularly if the patient’s condition changes, and complete the activity correctly, including fulfilling any documentation requirements. Delegatees maintain accountability for the delegated activity and need to notify the delegator immediately if they have difficulty completing the task.
One special case
NCSBN notes that in some cases, APs are taught how to perform skills that were previously thought to be exclusively RN and LPN/LVN responsibilities, such as certified medical assistants administering injections. In these cases, it’s best to consider such tasks as being delegated and, therefore, validate competency.
Keeping patients safe
Knowing the differences between assigning and delegating helps protect patients and avoid legal action should an error occur. Assignments involve routine tasks learned in basic education and that fall under designated scope of practice, while delegation involves tasks that were learned through additional education and for which competency has been determined.
Good communication and an understanding of the responsibilities of delegators and delegatees is essential to avoid misunderstanding. Remember, the licensed nurse remains accountable for the patient, but the delegatee is responsible for the delegated task.
Five rights of delegation
The ncsbn outlines five rights of delegation. in the case of a lawsuit, a key component would be whether you adhered to these rights:.
- Right task . The task needs to fall within the delegatee’s job description or is part of organizational policies and procedures.
- Right circumstance . The patient must be stable.
- Right person . The delegatee must have the appropriate skills and knowledge to perform the task.
- Right directions and communication . Clear directions need to be given, with the delegator verifying understanding by the delegatee. Communication must be two-way, with the delegatee asking questions as needed.
- Right supervision and evaluation . The delegator needs to monitor the delegated activity, including evaluating patient outcomes.
Article by: Cynthia Saver, MS, RN, President of CLS Development, Inc., in Columbia, Md and Georgia Reiner, MS, CPHRM, Risk Analyst, NSO
National Council of State Boards of Nursing. National guidelines for nursing delegation. J Nurs Reg. 2016;7(1):5-12.
NCSBN, ANA. National guidelines for nursing delegation. 2019.
#Delegating #RN
Share this article:
Frequently Asked Questions
You have questions. We have answers. (It's why we're here.)
What kinds of activities might trigger a disciplinary action by a licensing board or regulatory agency?
The fact is anyone can file a complaint against you with the state board for any reason—even your own employer—and it doesn’t have to be solely connected to your professional duties. All complaints need to be taken seriously, no matter how trivial or unfounded they may appear.
How does a shared limit policy work?
The business, and all eligible employees and sub-contractors you regularly employ, will be considered when determining your practice’s premium calculation and share the same coverage limits you select for the business.
We have a shared limit policy. Are employees covered if they practice outside our office?
If your employees are moonlighting, either for pay or as a volunteer, they should carry an individual professional liability insurance policy to cover those services. Otherwise, they might not be covered for claims that arise out of these activities.
There are plenty more where those came from.
See more FAQs
More learning right here
Check out these related articles.
Nurse Case Study: Failure to monitor and inadequate documentation in home health setting
RN working in home health setting fails to monitor and properly document ulcer wounds in post-surgical Alzheimer’s patient.
Nurse Case Study: Failure to monitor high fall risk ICU patient; failure to educate family on fall prevention
This medical malpractice case study, presented by NSO and CNA, involves a registered nurse working in a critical care setting.
opens in a new window
- South Dakota Nurse November 2018 issue is now available.

8 Steps for Making Effective Nurse-Patient Assignments
This article appears on page 14 of
South Dakota Nurse November 2018
Reprinted from American Nurse Today
Successful assignments require attention to the needs of both nurses and patients.
YOUR MANAGER wants you to learn how to make nurse patient assignments. What? Already? When did you became a senior nurse on your floor? But you’re up to the challenge and ready to learn the process.
Nurse-patient assignments help coordinate daily unit activities, matching nurses with patients to meet unit and patient needs for a specific length of time. If you are new to this challenge, try these eight tips as a guide for making nurse-patient assignments.
1. Find a mentor
Most nurses learn to make nurse-patient assignments from a colleague. Consider asking if you can observe your charge nurse make assignments. Ask questions to learn what factors are taken into consideration for each assignment. Nurses who make assignments are aware of their importance and are serious in their efforts to consider every piece of information when making them. By asking questions, you’ll better understand how priorities are set and the thought that’s given to each assignment. Making nurse-patient assignments is challenging, but with your mentor’s help, you’ll move from novice to competent in no time.
2. Gather your supplies (knowledge)
Before completing any nursing task, you need to gather your supplies. In this case, that means knowledge. You’ll need information about the unit, the nurses, and the patients. (See What you need to know.) Some of this information you already know, and some you’ll need to gather. But make sure you have everything you need before you begin making assignments. Missing and unknown information is dangerous and may jeopardize patient and staff safety. The unit and its environment will set the foundation for your assignments. The environment (unit physical layout, average patient length of stay [LOS]) defines your process and assignment configuration (nurse-to-patient ratios). You’re probably familiar with your unit’s layout and patient flow, but do you know the average LOS or nurse-to-patient ratios? Do you know what time of day most admissions and discharges occur or the timing of certain daily activities? And do other nursing duties need to be covered (rapid response, on call to another unit)? Review your unit’s policy and procedures manual for unit staffing and assignment guidelines. The American Nurses Association’s ANA ‘s Principles for Nurse Staffing 2nd edition also is an excellent resource.
Review the assignment sheet or whiteboard used on your unit. It has clues to the information you need. It provides the framework for the assignment-making process, including staff constraints, additional duties that must be covered, and patient factors most important on your unit. Use the electronic health record (EHR) to generate various useful pieces of patient information. You also can use the census sheet, patient acuity list, or other documents of nursing activity, such as a generic hospital patient summary or a unit-specific patient report that includes important patient factors.
Depending on your unit, the shift, and the patient population, you’ll need to consider different factors when making assignments. Ask yourself these questions: What patient information is important for my unit? Does my unit generate a patient acuity or workload factor? What are the time-consuming tasks on my unit (medications, dressing changes, psychosocial support, total care, isolation)? Which patients require higher surveillance or monitoring? Finally, always talk to the clinical nurses caring for the patients. Patient conditions change faster than they can be documented in the EHR, so rely on the clinical nurses to confirm each patient’s acuity and individual nurses’ workloads. Nurses want to be asked for input about their patients’ condition, and they’re your best resource.
Now ask yourself: How well do I know the other nurses on my unit? This knowledge is the last piece of information you need before you can make assignments. The names of the nurses assigned to the shift can be found on the unit schedule or a staffing list from a centralized staffing office. If you know the nurses and have worked with them, you’ll be able to determine who has the most and least experience, who’s been on the floor the longest, and who has specialty certifications. You’ll also want to keep in mind who the newest nurses are and who’s still on orientation.
3. Decide on the process
Now that you’ve gathered the information you need, you’re ready to develop your plan for assigning nurses. This step usually combines the unit layout with your patient flow. Nurses typically use one of three processes–area, direct, or group–to make assignments. (See Choose your process.)
4. Set priorities for the shift
The purpose of nurse-patient assignments is to provide the best and safest care to patients, but other goals will compete for consideration and priority. This is where making assignments gets difficult. You’ll need to consider continuity of care, new nurse orientation, patient requests and satisfaction, staff well-being, fairness, equal distribution of the workload, nurse development, and workload completion.
5. Make the assignments
Grab your writing instrument and pencil in that first nurse’s name. This first match should satisfy your highest priority. For example, if nurse and any other returning nurses are reassigned to the patients they had on their previous shift. If, however, you have a complex patient with a higher-than-average acuity, you just assigned your best nurse to this patient. After you’ve satisfied your highest priority, move to your next highest priority and match nurses with unassigned patients and areas.
Sounds easy, right? Frequently, though, you’ll be faced with competing priorities that aren’t easy to rate, and completing the assignments may take a few tries. You want to satisfy as many of your priorities as you can while also delivering safe, quality nursing care to patients. You’ll shuffle, move, and change assignments many times before you’re satisfied that you’ve maximized your priorities and the potential for positive outcomes. Congratulate yourself–the nurse-patient assignments are finally made.
6. Adjust the assignments
You just made the assignments, so why do you need to adjust them? The nurse-patient assignment list is a living, breathing document. It involves people who are constantly changing–their conditions improve and deteriorate, they’re admitted and discharged, and their nursing needs can change in an instant. The assignment process requires constant evaluation and reevaluation of information and priorities. And that’s why the assignments are usually written in pencil on paper or in marker on a dry-erase board. As the charge nurse, you must communicate with patients and staff throughout the shift and react to changing needs by updating assignments. Your goal is to ensure patients receive the best care possible; how that’s accomplished can change from minute to minute.
7. Evaluate success
What’s the best way to evaluate the success of your nurse-patient assignments? Think back to your priorities and goals. Did all the patients receive safe, quality care? Did you maintain continuity of care? Did the new nurse get the best orientation experience? Were the assignments fair? Measure success based on patient and nurse outcomes.
Check in with the nurses and patients to get their feedback. Ask how the assignment went. Did everyone get his or her work done? Were all the patients’ needs met? What could have been done better? Get specifics. Transparency is key here. Explain your rationale for each assignment (including your focus on patient safety) and keep in mind that you have more information than the nurses. You’re directing activity across the entire unit, so you see the big picture. Your colleagues will be much more understanding when you share your perspective. When you speak with patients, ask about their experiences and if all their needs were met.
8. Keep practicing
Nurse-patient assignments never lose their complexity, but you’ll get better at recognizing potential pitfalls and maximizing patient and nurse outcomes. Keep practicing and remember that good assignments contribute to nurses’ overall job satisfaction.
What you need to know
Before you make decisions about nurse-patient assignments, you need as much information as possible about your unit, nurses, and patients.
Common patient decision factors Demographics • Age • Cultural background • Gender • Language
Acuity • Chief complaint • Code status • Cognitive status • Comorbidities • Condition • Diagnosis • History • Lab work • Procedures • Type of surgery • Vital signs • Weight
Workload • Nursing interventions • Admissions, discharges, transfers • Blood products • Chemotherapy • Drains • Dressing changes • End-of-life care • I.V. therapy • Lines • Medications • Phototherapy • Treatments • Activities of daily living • Bowel incontinence • Feedings • Total care
Safety measures • Airway • Contact precautions • Dermatologic precautions • Fall precautions • Restraints • Surveillance
Psychosocial support • Emotional needs • Familial support • Intellectual needs
Care coordination • Consultations • Diagnostic tests • Orders • Physician visit
Common nurse decision factors Demographics • Culture/race • Gender • Generation/age • Personality
Preference • Request to be assigned/not assigned to a patient
Competence • Certification • Education • Efficiency • Experience • Knowledge/knowledge deficit • Licensure • Orienting • Skills • Speed • Status (float, travel)
Choose your process
Your nurse-patient assignment process may be dictated by unit layout, patient census, or nurse-to-patient ratio. Most nurses use one of three assignment processes.
Area assignment This process involves assigning nurses and patients to areas. If you work in the emergency department (ED) or postanesthesia care unit (PACU), you likely make nurse-patient assignments this way. A nurse is assigned to an area, such as triage in the ED or Beds 1 and 2 in the PACU, and then patients are assigned to each area throughout the shift.
Direct assignment The second option is to assign each nurse directly to a patient. This process works best on units with a lower patient census and nurse-to-patient ratio. For example, on a higher-acuity unit, such as an intensive care unit, the nurse is matched with one or two patients, so a direct assignment is made.
Group assignment With the third option, you assign patients to groups and then assign the nurse to a group. Bigger units have higher censuses and nurse-to-patient ratios (1:5 or 1:6). They also can have unique physical features or layouts that direct how assignments are made. A unit might be separated by hallways, divided into pods, or just too large for one nurse to safely provide care to patients in rooms at opposite ends of the unit. So, grouping patients together based on unit geography and other acuity/workload factors may be the safest and most effective way to make assignments.
You also can combine processes. For example, in a labor and delivery unit, you can assign one nurse to the triage area (area process) while another nurse is assigned to one or two specific patients (direct process). Unit characteristics direct your process for making assignments. Your process will remain the same unless your unit’s geography or patient characteristics (length of stay, nurse-patient ratio) change.
Stephanie B. Allen is an assistant professor at Pace University in Pleasantville, New York.
Selected references Allen SB. The nurse-patient assignment process: What clinical nurses and patients think. MEDSURG Nurs. 2018;27(2):77-82. Allen SB. The nurse-patient assignment: Purposes and decision factors. J Nurs Adm. 2015;45(12):628-35. Allen SB. Assignments matter: Results of a nurse-patient assignment survey. MEDSURG Nurs [in press]. American Nurses Association (ANA). ANA‘s Principles for Nurse Staffing. 2nd ed. Silver Spring, MD: ANA; 2012.
The Importance of Nursing Assignments: A Comprehensive Guide
Stella Jones
In the world of healthcare, nursing assignments play a crucial role in ensuring patient care, safety, and the smooth functioning of medical facilities. These assignments are not just routine tasks but are pivotal in maintaining the well-being of patients and the overall healthcare system. In this comprehensive guide, we will delve into the significance of nursing assignments, their impact on patient outcomes, and how nurses can excel in this vital aspect of their profession.
Introduction
Nursing assignments are the backbone of patient care. They encompass a wide range of tasks that nurses perform daily, contributing significantly to the recovery and well-being of patients. In this article, we will explore the multifaceted importance of nursing assignments and their far-reaching impact on healthcare.
2. Understanding Nursing Assignments
The role of nurses.
Nurses are the primary caregivers in healthcare settings. Their responsibilities go beyond administering medication and conducting medical procedures. Nurses are responsible for providing holistic care, which includes emotional support, patient education, and continuous monitoring.
Types of Nursing Assignments
Nursing assignments can be categorized into various types, such as direct patient care, administrative tasks, and critical care assignments. Each type requires specific skills and knowledge to ensure optimal patient outcomes.
3. The Importance of Clear Communication
Interdisciplinary collaboration.
Effective communication is vital in nursing assignments. Nurses must collaborate with physicians, therapists, and other healthcare professionals to provide comprehensive care. Clear and timely communication ensures that every member of the healthcare team is on the same page, leading to better patient outcomes.
Patient-Cantered Care
Patients rely on nurses to advocate for them and communicate their needs to the medical team. Nursing assignments often involve explaining complex medical procedures and treatment plans in a way that patients can understand. This patient-centered approach fosters trust and enhances the overall quality of care.
Ensuring Patient Safety
Medication administration.
One of the critical aspects of nursing assignments is medication administration. Nurses must accurately administer medications, monitor patients for adverse reactions, and educate them about their medications. Mistakes in this area can have severe consequences, emphasizing the need for precision.
Monitoring Vital Signs
Regular monitoring of vital signs, such as blood pressure, heart rate, and temperature, is an integral part of nursing assignments. Timely detection of changes in a patient’s condition can be lifesaving.
Infection Control
Nurses play a pivotal role in preventing healthcare-associated infections. Proper hygiene, sterilization, and adherence to infection control protocols are essential components of nursing assignments.
Time Management in Nursing Assignments
Nursing assignments often involve juggling multiple tasks and patients. Effective time management is crucial to ensure that all responsibilities are met without compromising patient care.
Documentation and Record Keeping
Accurate documentation of patient information, care plans, and interventions is essential for continuity of care and legal purposes. Nursing assignments include maintaining detailed records to facilitate communication among healthcare providers.
Critical Thinking and Problem Solving
Nursing assignments frequently require quick thinking and problem-solving skills. Nurses must assess situations, identify potential issues, and take appropriate actions to address them promptly.
Emotional Intelligence in Nursing
Empathy and emotional intelligence are invaluable in nursing assignments. Patients often experience fear, anxiety, and pain, and nurses need to provide emotional support while delivering care.
Quality Assurance and Nursing Assignments
Quality assurance measures are integral to nursing assignments. Regular audits and assessments ensure that nursing care meets established standards, enhancing the quality of healthcare delivery.
Continuing Education and Training
The field of healthcare is ever-evolving, and nurses must stay updated with the latest medical advancements. Continuous education and training are essential components of nursing assignments to ensure that nurses provide the best possible care.
The Future of Nursing Assignments
As technology advances and healthcare systems evolve, nursing assignments may undergo significant changes. Nurses must adapt to new technologies and practices to maintain the highest standards of patient care.
Challenges in Nursing Assignments
Nursing assignments come with their set of challenges, including high workload, emotional stress, and demanding schedules. Addressing these challenges is crucial to ensuring the well-being of nurses and, in turn, patient care.
In conclusion, nursing assignment help are the foundation of quality patient care. They encompass a wide array of tasks, from administering medication to providing emotional support. Nurses play a pivotal role in ensuring patient safety, communication, and overall well-being. As the healthcare landscape continues to evolve, nursing assignments will remain a cornerstone of healthcare delivery.
Q1: What are nursing assignments?
Nursing assignments are tasks and responsibilities that nurses perform in healthcare settings to ensure patient care and safety.
Q2: How important is communication in nursing assignments?
Communication is crucial in nursing assignments as it facilitates collaboration among healthcare professionals and ensures patient-centered care.
Q3: What challenges do nurses face in nursing assignments?
Nurses may face challenges such as high workload, emotional stress, and the need for continuous learning in their nursing assignments.
Q4: How do nursing assignments contribute to patient safety?
Nursing assignments, including medication administration and vital sign monitoring, are essential for detecting and addressing changes in a patient’s condition, thereby enhancing patient safety.
Q5: What is the future of nursing assignments in healthcare?
The future of nursing assignments may involve adapting to new technologies and practices as healthcare systems evolve to meet the changing needs of patients.

Written by Stella Jones
Text to speech

Nursing School Assignments and Tips to Ace All of Them

If you are about to start nursing school or considering enrolling in a nursing program, you would want to know what to expect. You will write many papers in nursing school and do many other assignments. This is true whether you pursue ADN, BSN, MSN, DNP, or PhD in Nursing.
Before we delve into the types of assignments and papers to expect in nursing school, let us begin by dispelling the myth that nursing school is hell; it is NOT. Instead, it is a beautiful and exciting journey into a noble profession. It entails a commitment to life-long continuous learning for you to grow.
Nursing school writing assignments are an excellent way for students to understand concepts taught in the classroom. You might wonder what kinds of assignments nursing students do. These assignments come in various forms and help students build critical thinking, creativity, research, clinical reasoning, and problem-solving skills that are critical in clinical settings.
This blog post looks at the diverse assignments you should expect or will cover in nursing school, including some tips to help you ace them and get better grades.
Common Nursing School Writing Assignments
Classwork forms the core of most nursing programs. You must have high-quality assignment submissions to attain better grades in nursing school. As soon as you decide to become a nursing student, you sign up for a marathon of writing different types of papers.
Whether you love or hate it, you will write papers before graduating from nursing school; that is the norm. Although not so many, you will encounter a few homework and assignments where you must submit a well-researched, formatted, and organized nursing paper.
The typical nursing school assignments include essays, research papers, term papers, and case studies. Others are article critiques/reviews, critical appraisal, evidence synthesis tables (synthesis matrix), PowerPoint Presentations, posters, discussion posts/ responses, and policy analysis papers. Other advanced papers include nursing care plans, SBAR template papers, evidence-based papers, capstone projects, theses, dissertations, proposals, etc.
These assignments are submitted either individually or as a group. Let us expound on this so you have a clear picture.
Essays for nursing classes come in various forms, including admission essays , scholarship essays, descriptive essays, persuasive essays, speech essays, expository essays, and narrative essays.
Notably, nursing essays focus on a single perspective, argument, or idea, which constantly forms the thesis of the paper.
Nursing essays focus on various topics relating to nursing practice and the broader healthcare field. You can write an essay examining a nursing theory or non-nursing theory or discuss a nursing issue .
Some essays, such as reflective nursing essays, use reflective models to reflect, analyze, and understand personal and professional encounters during clinical practice.
Each nursing essay should demonstrate your understanding of the topic, critical analysis, and organization skills. Besides, you should use evidence from peer-reviewed scholarly sources to support your arguments and ideas.
Discussion Board Posts
If you pursue a hybrid or exclusively online nursing program, you will be assigned to write weekly discussion forum posts and responses. Discussion board posts are short essay-like assignments posted in a threaded format so students can discuss nursing and healthcare topics.
You will write an original discussion post, between 200 and 300 words long, and post it on the forum. You are also expected to write a peer-response post in response to or to comment on an original post done by your peers.
Discussion boards help nursing students advance theoretical concepts, learn from one another, share ideas, and get feedback that can help them advance their knowledge in clinical reasoning and practice.
Research Papers
Nursing practice is evidence-driven, translating evidence into practice to ensure quality, accessible, and affordable healthcare. As such, nursing research takes precedence during studies and when practicing.
Nursing professors assign nursing students to write research papers on various evidence-based practice topics. The students must prove their worth by researching, analyzing, and organizing facts.
Related Writing Guides:
- How to write a nursing school research paper.
- Systematic Reviews vs Literature Review
Research papers help student nurses to review literature, conduct research, implement solutions, and draw evidence-based conclusions.
Research papers are critical in developing research and writing skills, maintaining good communication, and fostering creativity and clinical reasoning.
Potential nursing research paper topics can be quality improvement, healthcare/nursing informatics , healthcare policies, practice privileges, nursing ethics, ethical dilemmas , pathophysiology, and epidemiology .
Term Papers
In nursing school, a term paper is a type of assignment completed and submitted toward the end of the semester.
Usually, a professor can assign you a specific term paper topic, or they can let you choose a topic and consult with them for approval.
Term papers can be done individually or as a group project. A term paper has an impact on your final grade.
You should use credible scholarly sources published within the last five years for recent information.
Besides, also ensure that you plan your time well, do everything as per the instructions, and submit the nursing term paper before the deadline.
A term paper can also be a nursing process change report that is expected to address an area that needs change.
Case Studies
Nursing school case study assignments are an essential learning tool.
Most professors assign hypothetical clinical case studies or case scenarios (snippets) to test your clinical reasoning skills.
As a nursing educational tool, nursing case studies help you to develop practical, theoretical knowledge by simulating real-world experiences.
When analyzing a case study, you must use concepts and knowledge from class and class text to assess a patient, plan and implement care, and evaluate the outcomes.
Sometimes, you encounter simulated or digital clinical experience case studies such as iHuman and Shadow Health .
You should be very keen when analyzing a case study and when writing the analysis report.
Case studies help you get beyond books and use your creativity, clinical reasoning, problem-solving, and analytical skills to apply theoretical knowledge to real-world problems.
Your professor can give you a case study of a patient presenting with a given condition and expect you to take them through the care planning process, including admission and discharge, as you would in a real healthcare setting.
Other times, you can be asked to develop a hypothetical case study of a patient presenting with a chronic disease or a disorder and then use the case study guidelines, including head-to-toe assessment , diagnosis , nursing care planning , and discharge planning.
Related Guides:
- How to write a great nursing case study.
- How to complete a case conceptualization report (for psychiatric nursing students)
Nursing Care Plans and SOAP Notes
A nursing care plan can be part of a case study or a stand-alone assignment. Nursing care plans are essential in nursing education as they help students develop effective nursing care planning. Formulating a nursing care plan for a patient scenario or case helps treat them as you define the guidelines and roles of nurses in caring for the patient.
You also develop solid action plans for focused and patient-centred care by documenting the patient's needs. When they are part of an assignment, you can tabulate the nursing care plan using columns so that you explore every aspect independently.
Remember to use evidence from peer-reviewed scholarly sources when giving rationale.
The SOAP notes are a clinical tool healthcare professionals use to organize patient information to minimize confusion and assess, diagnose, and treat patients. Check our comprehensive guide on developing good SOAP Notes in nursing school .
Concept Maps
Another common nursing school assignment is concept maps. Concept mapping helps you visually organize, compartmentalize, and categorize information about nursing care planning, medical diagnosis, pathophysiology, SBAR, nursing responsibilities, etc.
A nursing concept map assignment equips you with strong critical thinking, analytical, and problem-solving skills. You also hone your clinical reasoning skills in the process.
Whether it is part of an assignment or a stand-alone, learn how to write great concept maps to score the best grades.
Concept Analysis Papers
If you are taking BSN, MSN, or DNP, you will likely be assigned to write a concept analysis paper. Make sure to distinguish this from a concept paper that is a proposal. A concept analysis paper examines the structure and function of a nursing concept.
The process entails a review of the literature and creativity in coming up with borderline, related, contrast, inverted, and illegitimate cases.
You also explore the antecedents and consequences of the concept before finalizing with empirical referents.
If you need to learn about the structure of a good concept analysis paper, check out our nursing concept analysis guide . We have listed concepts you can analyze depending on your speciality, instructions, and passion.
Capstone Projects
At an advanced stage in nursing school, students are expected to submit longer research papers; capstone project papers. A nursing capstone project is a final project that allows students to demonstrate the skills, knowledge, and concepts gained throughout the nursing program.
In nursing education, the capstone project typically covers an evidence-based practice issue or problem. You can write a nursing change paper, look into a clinical process, problem, or issue, and then develop recommendations based on a study.
Most of the MSN and DNP capstone projects focus on clinical change or quality improvement. You will be expected to develop a PICOT question and formulate a research study to examine the issue, implement a change process using evidence-based models, and make recommendations.
Nursing capstone projects are individual research projects based on nursing topics either of your professional or personal interest. You have to demonstrate competency and commitment to improve health outcomes.
Apart from capstone projects, you will also write a nursing thesis and dissertation papers, which depend on the program requirements and your professor's preferences.
Check out these specific writing guides for advanced papers:
- How to write a nursing dissertation or thesis
- Tips for choosing the best nursing dissertation topic
- How to write an excellent capstone project paper
- List of capstone project topics for nursing school
- How to formulate a PICOT question
- PICOT question examples to inspire nursing students
Group Assignments
In nursing school and practice, collaboration and teamwork are highly recommended. You will encounter collaborative group assignments such as presentations (PowerPoint slides, Prezi, or other platforms), simulation assignments, writing nursing reports, and group research projects.
Group projects allow you to research, learn, and organize ideas together so that you can understand concepts better. It is essential to avoid social loafing in a group to gain more. Besides, plan your time well and avoid excuses.
You can also be assigned to work on simulation exercises as a group of nursing students. The aim of such exercises is to build a collaborative, teamwork, and decision-making spirit among the team.
When in such groups, expect to work with your peers to assess the hypothetical patient, communicate with your peers, formulate a care plan, and manage any arising issues as you would in clinical settings. Do not take such activities for granted; they contribute significantly to your grade.
Presentations
Your professor can assign you to design a PowerPoint Slide accompanied by speaker notes and send it for grading or present it online or in class. Under presentations, you will also be requested to design flyers, posters, and other visual documents to disseminate information.
It could be about a disease, health promotion, or nursing research. You must also make PowerPoint slides when presenting a thesis, dissertation, or capstone for assessments. Remember, this is the chance to bring out your creativity.
Expect other assignments such as dosage calculations, HESI test exams, skills checkoffs, electronic medical record documentation, nursing student portfolio, online quizzes, drug write-ups, process recordings, group drug presentations, etc.
In most cases, you will be given a template to use wisely and make it as appealing as possible.
Tips to Help You Ace Nursing Assignments
A lot goes into getting the best grades in nursing school. One of the main determinants of your nursing school grades is the assignments, which you are required to do and complete within set deadlines.
Even though many nursing students perform better on clinical, that needs to reflect in written assignments. Most students fear research and writing or do not take writing assignments seriously. Regardless of the assignment, here are some practical and effective tips to help you ace your nursing school writing assignments and surprise everyone, including yourself.
1. Plan your Time
The number one challenge for nursing students that inhibits them from completing assignments is the need for more time management.
Most students are juggling studies and work to make ends meet. It worsens when you have a massive workload from more than one class and a family to look after.
The simple trick to beat this is to manage your time well. You can schedule your assignments for periods when you are free and when you can concentrate and cover more. Assignments have deadlines ranging from hours to days or a few weeks.
To succeed, keep track of your assignments and other academic activities, such as mid-term and final examinations, so that you can plan your study periods. You can use online time management tools and apps to allocate your nursing school homework time.
With proper planning, you should be reassured about the last-minute rush to complete your assignment, which is responsible for the colossal failure we are experiencing in nursing schools.
2. Follow the Course Guidelines to the T
Guidelines, prompts, and reading materials accompany each writing assignment and homework. Sometimes a professor can be generous enough also to give you access to the Rubric, which breaks down how they will assess assignments. Ensure you read everything and note what is required before working on any paper.
Pay attention to these, read, and familiarize yourself with the course guidelines. Understand the formatting requirements preferred by your school, such as Vancouver, APA, or Harvard. Most nursing schools will specify this in the course documents. Also, check the databases and journal articles you can use when writing your nursing assignments.
Preparing in advance by reading the course materials to identify the recommended study materials. You will have a deeper understanding, knowledge, and skills to handle every nursing assignment correctly.
3. Have an Active Study Buddy
A nursing study buddy can be one of your classmates whom you study with. Study buddies offer mutual support, which comes in handy when completing assignments.
Select a bright and committed person with something to offer so you are not only giving. Set the study hours and have accountability follow-ups to ensure you cover much of the syllabus and concepts in time.
A study buddy can help you understand nursing concepts, theories, models, and frameworks. They can also help you review your written papers and give valuable feedback when editing and proofreading your nursing papers.
A knowledgeable, accountable, committed study partner can help you revamp your grades by submitting high-quality assignments.
4. Join a Study Group
A study group is a tried and tested means of completing nursing assignments. Apart from building your teamwork and collaborative skills, you can brainstorm ideas, critique one another, and learn more about the class assignments. With diversity in thoughts, you can get valuable insights and inputs for personal-level work.
Besides, you are also guaranteed to ace the nursing group assignments with ease. When doing group work, try to rotate into new groups so that you can appreciate the diversity of thoughts and reasoning. You can also identify individuals from your groups, those that are active, as your study buddies.
When you have accountability partners within the group, you commit to given tasks and make necessary follow-ups. If you are a part-time student, consider having students whose free time is similar to yours to benefit everyone.
5. Get Writing Assignment Help
As with other subjects in college and university, nursing students face challenges such as time management, complexity of assignments, too many assignments, and writer's block. When you feel overwhelmed with completing your nursing class assignments, you can always pay someone to handle the class for you or at least do your coursework or assignments.
One sure way to get assistance without drawing too much attention is by trusting assignment help websites like NurseMyGrade.com with your papers. Many students do not have time to complete assignments or find them challenging. Consequently, many hire nursing assignment helpers from nursing paper writing platforms.
If you feel like hiring the right professionals, use NurseMyGrade. We offer customized writing solutions to nursing students at different academic levels. Our nursing experts can complete short and lengthy assignments. You will have a well-researched and formatted paper written in Vancouver, APA, MLA, ASA, AMA, Harvard, or any citation style you choose.
You can use the tips and insights above to master nursing school assignments. We wish you all the best as you strive towards excellence. Don't worry about the many assignments. Instead, be grateful that they will equip you with knowledge, skills, and experience to make you the best nurse.
How Many Papers to Write in Nursing School
We have so far covered the general aspects of the types of assignments to expect in nursing school. Under the assignments, you may ask yourself if you must write many papers in nursing school.
While the answer depends on your professor, institutional curriculum requirements, and nursing level, you will undoubtedly write a couple of academic papers before graduating from nursing school. You will write research papers, essays, proposals, white papers, policy analysis papers, capstone project papers, case studies, scholarship essays, personal statements, quality improvement reports, etc.
Suppose you are pursuing a Licensed Practical Nurse (LPN) program. In that case, you will likely write between 13 and 15 papers during the LPN program, including short and long essays, reflective journals, essays, patient-based case studies, and others as your professor pleases.
If you are in a 2-year ADN program, expect to complete about 20 to 30 papers, including care plans, SBAR reports, essays, case studies analyses, research papers, reports, and other assignments.
For a 4-year Bachelor of Science in Nursing (BSN) program, you will write between 35 and 50 papers. If you are taking the online class program options, like the WGU BSN program, you might write more papers because they form the basis for your assessment.
BSN-level papers are demanding because you must strictly adhere to the formatting styles and be critical and organized in your presentation.
If you are taking a Master of Science in Nursing (MSN) program, an advanced-level study for registered nurses (RNs), you will do about 20-50 papers, given that it offers the foundation for nursing research. Again, at an advanced level, the MSN writing assignments are complex.
You need to plan well, research widely, and analyze facts thoroughly before drawing conclusions. During this level, expect to write papers such as MSN essays, discussion posts and responses, specialized case studies, research papers, clinical reports, advanced SOAP notes, nursing care plans, policy papers, position papers (white papers), dissertations, theses, capstone papers, project papers, and change project papers.
You are expected to show exquisite research skills for the Doctor of Nursing Practice (DNP) program, considered the highest level or terminal degree in nursing practice. At this level, you have specialized, advanced your knowledge, and have adequate experience.
Mostly, DNP papers are a little longer. You will write between 20-30 papers; depending on your nursing school curriculum and supervisor's preference, it could be less or more.
If you opt for the research route, you will write many research papers, technical papers, policy analysis papers, white papers, reflection papers, nursing dissertations, PICOT-based change project papers (DNP change project papers), and other assignments.
Finally, for the Doctor of Philosophy (PhD) in nursing programs, you should expect to write between 10 and 15 papers covering research-oriented topics.
Attaining this degree makes you the epitome of success in the field. You can advance into a nursing researcher, educator, leader, or manager.
We have writers that can help you handle all these types of papers regardless of the academic level. Our Online Nursing Writing pros are available for hire anytime and any day.
Having worked successfully with many nursing clients/students, we are confident to help you achieve your dreams.
Before you go …
There are many assignments and papers to complete in nursing school, including written assignments, quizzes, exams (oral and written), reflective journals, journal entries, e-Portfolio, integrative reviews, teaching plans, presentations, etc. Whether taking an LPN program or advancing your career by pursuing a Ph.D. in Nursing, you will do many nursing school assignments.
Do not take assignments as a punishment. Instead, consider them as tools to equip and shape you into a desirable nurse practitioner.
If you feel overwhelmed, stressed, and anxious about completing the assignments, you can hire our nursing writers to help you. We can help you ace nursing assignments online and ensure that you get 100% well-researched, organized, and proofread papers.
Our papers are 100% original and non-plagiarized. The writers understand how to structure nursing papers, formulate great paragraphs using the MEAN, PEEL, or TEEL formats, and write desirable papers consistently, scoring the best grades. You can call us your nursing assignment slayers or acers because, in a few hours, we will help you get it all behind you. We can help you ace online nursing classes and tests/quizzes .
Click on the Order button and fill out the form to get our writers started in making you a nursing paper that gives the best grade. No topic is challenging for us, and we allow you direct communication with the writer in the process of getting help.
Struggling with
Related Articles

Hardest Nursing Classes and How to Pass Them Well

Nursing Student's Ultimate Guide to Writing a Nursing Care Plan

Tips and Steps for Writing a Great Community Health Assessment Paper
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
The Nursing Process: A Comprehensive Guide
In 1958, Ida Jean Orlando began developing the nursing process still evident in nursing care today. According to Orlando’s theory, the patient’s behavior sets the nursing process in motion. Through the nurse ‘s knowledge to analyze and diagnose the behavior to determine the patient’s needs.
Application of the fundamental principles of critical thinking , client-centered approaches to treatment, goal-oriented tasks, evidence-based practice (EBP) recommendations, and nursing intuition, the nursing process functions as a systematic guide to client-centered care with five subsequent steps. These are assessment , diagnosis, planning, implementation, and evaluation ( ADPIE ).
Table of Contents
What is the nursing process.
- What is the purpose of the nursing process?
Characteristics of the nursing process
Nursing process steps, collecting data, objective data or signs, subjective data or symptoms, verbal data, nonverbal data, primary source, secondary source, tertiary source, health interview, physical examination, observation, validating data, documenting data.
- 2. Diagnosis: “What is the problem?”
Initial Planning
Ongoing planning, discharge planning, developing a nursing care plan, behavioral nursing interventions, community nursing interventions, family nursing interventions, health system nursing interventions, physiological nursing interventions, safety nursing interventions, skills used in implementing nursing care, 1. reassessing the client, 2. determining the nurse’s need for assistance, nursing intervention categories, independent nursing interventions, dependent nursing interventions, interdependent nursing interventions, 4. supervising the delegated care, 5. documenting nursing activities, 1. collecting data, 2. comparing data with desired outcomes, 3. analyzing client’s response relating to nursing activities, 4. identifying factors contributing to success or failure, 5. continuing, modifying, or terminating the nursing care plan, 6. discharge planning.
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse’s critical thinking to provide the best care possible to the client.
What is the purpose of the nursing process?
The following are the purposes of the nursing process:
- To identify the client’s health status and actual or potential health care problems or needs (through assessment).
- To establish plans to meet the identified needs.
- To deliver specific nursing interventions to meet those needs.
- To apply the best available caregiving evidence and promote human functions and responses to health and illness (ANA, 2010).
- To protect nurses against legal problems related to nursing care when the standards of the nursing process are followed correctly.
- To help the nurse perform in a systematically organized way their practice.
- To establish a database about the client’s health status, health concerns, response to illness, and the ability to manage health care needs.
The following are the unique characteristics of the nursing process:
- Patient-centered . The unique approach of the nursing process requires care respectful of and responsive to the individual patient’s needs, preferences, and values. The nurse functions as a patient advocate by keeping the patient’s right to practice informed decision-making and maintaining patient-centered engagement in the health care setting.
- Interpersonal . The nursing process provides the basis for the therapeutic process in which the nurse and patient respect each other as individuals, both of them learning and growing due to the interaction. It involves the interaction between the nurse and the patient with a common goal.
- Collaborative . The nursing process functions effectively in nursing and inter-professional teams, promoting open communication, mutual respect, and shared decision-making to achieve quality patient care .
- Dynamic and cyclical .The nursing process is a dynamic, cyclical process in which each phase interacts with and is influenced by the other phases.
- Requires critical thinking . The use of the nursing process requires critical thinking which is a vital skill required for nurses in identifying client problems and implementing interventions to promote effective care outcomes.
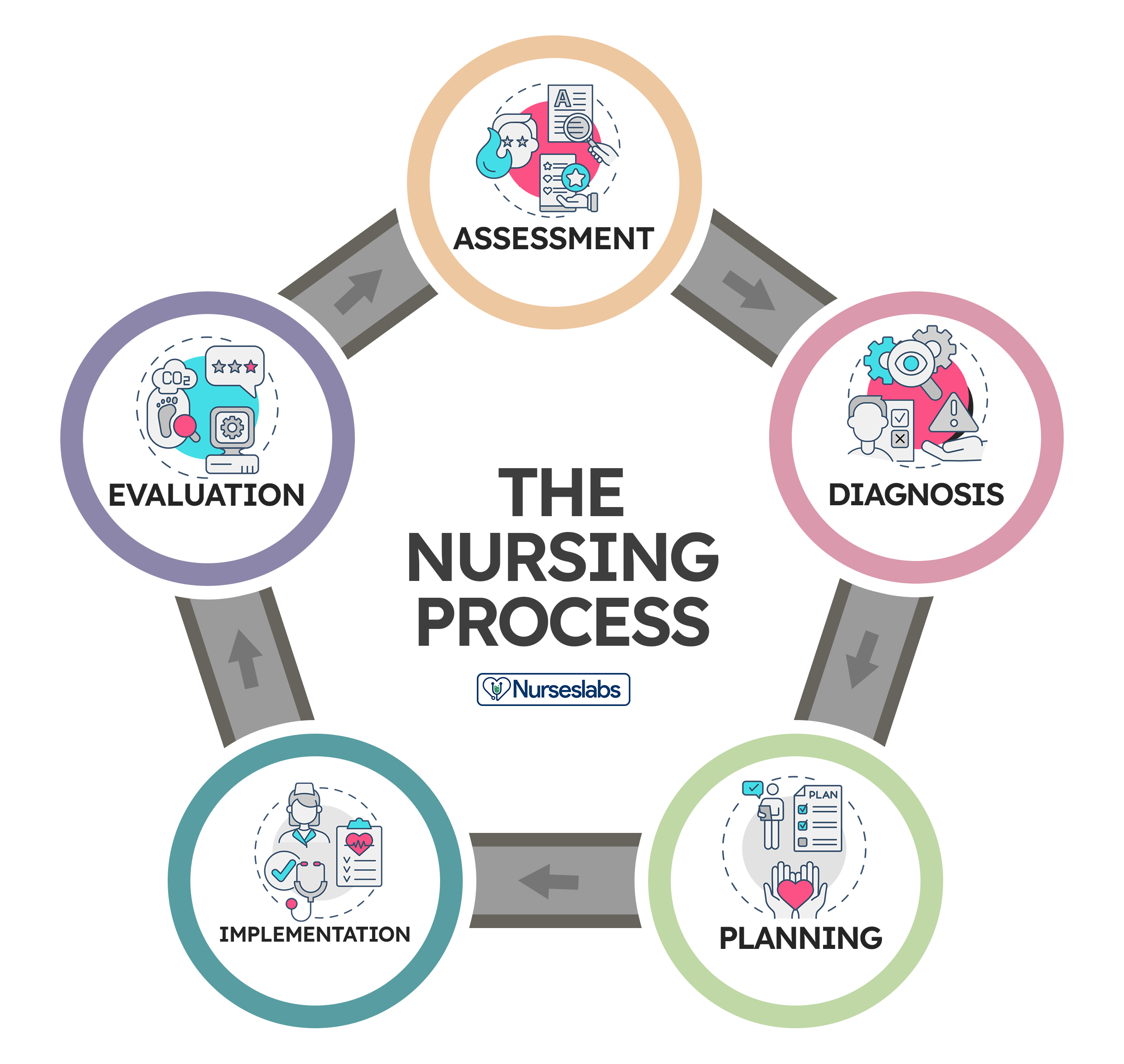
The nursing process consists of five steps: assessment, diagnosis, planning, implementation, and evaluation . The acronym ADPIE is an easy way to remember the components of the nursing process. Nurses need to learn how to apply the process step-by-step. However, as critical thinking develops through experience, they learn how to move back and forth among the steps of the nursing process.
The steps of the nursing process are not separate entities but overlapping, continuing subprocesses. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps of the nursing process are detailed below:
1. Assessment: “What data is collected?”
The first phase of the nursing process is assessment . It involves collecting, organizing, validating, and documenting the clients’ health status. This data can be obtained in a variety of ways. Usually, when the nurse first encounters a patient, the nurse is expected to assess to identify the patient’s health problems as well as the physiological, psychological, and emotional state and to establish a database about the client’s response to health concerns or illness and the ability to manage health care needs. Critical thinking skills are essential to the assessment, thus requiring concept-based curriculum changes.
Data collection is the process of gathering information regarding a client’s health status. The process must be systematic and continuous in collecting data to prevent the omission of important information concerning the client.
The best way to collect data is through head-to-toe assessment. Learn more about it at our guide: Head to Toe Assessment: Complete Physical Assessment Guide
Types of Data
Data collected about a client generally falls into objective or subjective categories, but data can also be verbal and nonverbal.
Objective data are overt, measurable, tangible data collected via the senses, such as sight, touch , smell , or hearing , and compared to an accepted standard, such as vital signs, intake and output , height and weight, body temperature, pulse, and respiratory rates, blood pressure , vomiting , distended abdomen, presence of edema , lung sounds, crying, skin color, and presence of diaphoresis.
Subjective data involve covert information, such as feelings, perceptions, thoughts, sensations, or concerns that are shared by the patient and can be verified only by the patient, such as nausea , pain , numbness, pruritus, attitudes, beliefs, values, and perceptions of the health concern and life events.
Verbal data are spoken or written data such as statements made by the client or by a secondary source. Verbal data requires the listening skills of the nurse to assess difficulties such as slurring, tone of voice, assertiveness, anxiety , difficulty in finding the desired word, and flight of ideas.
Nonverbal data are observable behavior transmitting a message without words, such as the patient’s body language, general appearance , facial expressions, gestures, eye contact, proxemics (distance), body language, touch, posture, clothing. Nonverbal data obtained can sometimes be more powerful than verbal data, as the client’s body language may not be congruent with what they really think or feel. Obtaining and analyzing nonverbal data can help reinforce other forms of data and understand what the patient really feels.
Sources of Data
Sources of data can be primary, secondary, and tertiary . The client is the primary source of data, while family members , support persons, records and reports, other health professionals, laboratory and diagnostics fall under secondary sources.
The client is the only primary source of data and the only one who can provide subjective data. Anything the client says or reports to the members of the healthcare team is considered primary.
A source is considered secondary data if it is provided from someone else other than the client but within the client’s frame of reference. Information provided by the client’s family or significant others are considered secondary sources of data if the client cannot speak for themselves, is lacking facts and understanding, or is a child. Additionally, the client’s records and assessment data from other nurses or other members of the healthcare team are considered secondary sources of data.
Sources from outside the client’s frame of reference are considered tertiary sources of data . Examples of tertiary data include information from textbooks, medical and nursing journals, drug handbooks, surveys, and policy and procedural manuals.
Methods of Data Collection
The main methods used to collect data are health interviews, physical examination, and observation.
The most common approach to gathering important information is through an interview. An interview is an intended communication or a conversation with a purpose, for example, to obtain or provide information, identify problems of mutual concern, evaluate change, teach, provide support, or provide counseling or therapy. One example of the interview is the nursing health history , which is a part of the nursing admission assessment. Patient interaction is generally the heaviest during the assessment phase of the nursing process so rapport must be established during this step.
Aside from conducting interviews, nurses will perform physical examinations, referencing a patient’s health history, obtaining a patient’s family history, and general observation can also be used to gather assessment data. Establishing a good physical assessment would, later on, provide a more accurate diagnosis, planning, and better interventions and evaluation .
Observation is an assessment tool that depends on the use of the five senses (sight, touch, hearing, smell, and taste ) to learn information about the client. This information relates to characteristics of the client’s appearance, functioning, primary relationships, and environment. Although nurses observe mainly through sight, most of the senses are engaged during careful observations such as smelling foul odors, hearing or auscultating lung and heart sounds and feeling the pulse rate and other palpable skin deformations.
Validation is the process of verifying the data to ensure that it is accurate and factual. One way to validate observations is through “double-checking,” and it allows the nurse to complete the following tasks:
- Ensures that assessment information is double-checked, verified, and complete. For example, during routine assessment, the nurse obtains a reading of 210/96 mm Hg of a client with no history of hypertension . To validate the data, the nurse should retake the blood pressure and if necessary, use another equipment to confirm the measurement or ask someone else to perform the assessment.
- Ensure that objective and related subjective data are valid and accurate. For example, the client’s perceptions of “feeling hot” need to be compared with the measurement of the body temperature.
- Ensure that the nurse does not come to a conclusion without adequate data to support the conclusion. A nurse assumes tiny purple or bluish-black swollen areas under the tongue of an older adult client to be abnormal until reading about physical changes of aging.
- Ensure that any ambiguous or vague statements are clarified. For example, a 86-year-old female client who is not a native English speaker says that “I am in pain on and off for 4 weeks,” would require verification for clarity from the nurse by asking “Can you describe what your pain is like? What do you mean by on and off?”
- Acquire additional details that may have been overlooked. For example, the nurse is asking a 32-year-old client if he is allergic to any prescription or non-prescription medications. And what would happen if he takes these medications.
- Distinguish between cues and inferences. Cues are subjective or objective data that can be directly observed by the nurse; that is, what the client says or what the nurse can see, hear, feel, smell, or measure. On the other hand, inferences are the nurse’s interpretation or conclusions made based on the cues. For example, the nurse observes the cues that the incision is red, hot, and swollen and makes an inference that the incision is infected.
Once all the information has been collected, data can be recorded and sorted. Excellent record-keeping is fundamental so that all the data gathered is documented and explained in a way that is accessible to the whole health care team and can be referenced during evaluation.
2. Diagnosis: “What is the problem?”
The second step of the nursing process is the nursing diagnosis . The nurse will analyze all the gathered information and diagnose the client’s condition and needs. Diagnosing involves analyzing data, identifying health problems, risks, and strengths, and formulating diagnostic statements about a patient’s potential or actual health problem. More than one diagnosis is sometimes made for a single patient. Formulating a nursing diagnosis by employing clinical judgment assists in the planning and implementation of patient care .
The types, components, processes, examples, and writing nursing diagnosis are discussed more in detail here “ Nursing Diagnosis Guide: All You Need To Know To Master Diagnosing ”
3. Planning: “How to manage the problem?”
Planning is the third step of the nursing process. It provides direction for nursing interventions . When the nurse, any supervising medical staff, and the patient agree on the diagnosis, the nurse will plan a course of treatment that takes into account short and long-term goals. Each problem is committed to a clear, measurable goal for the expected beneficial outcome.
The planning phase is where goals and outcomes are formulated that directly impact patient care based on evidence-based practice (EBP) guidelines. These patient-specific goals and the attainment of such assist in ensuring a positive outcome. Nursing care plans are essential in this phase of goal setting. Care plans provide a course of direction for personalized care tailored to an individual’s unique needs. Overall condition and comorbid conditions play a role in the construction of a care plan. Care plans enhance communication, documentation, reimbursement , and continuity of care across the healthcare continuum.
Types of Planning
Planning starts with the first client contact and resumes until the nurse-client relationship ends, preferably when the client is discharged from the health care facility.
Initial planning is done by the nurse who conducts the admission assessment. Usually, the same nurse would be the one to create the initial comprehensive plan of care.
Ongoing planning is done by all the nurses who work with the client. As a nurse obtain new information and evaluate the client’s responses to care, they can individualize the initial care plan further. An ongoing care plan also occurs at the beginning of a shift. Ongoing planning allows the nurse to:
- determine if the client’s health status has changed
- set priorities for the client during the shift
- decide which problem to focus on during the shift
- coordinate with nurses to ensure that more than one problem can be addressed at each client contact
Discharge planning is the process of anticipating and planning for needs after discharge. To provide continuity of care, nurses need to accomplish the following:
- Start discharge planning for all clients when they are admitted to any health care setting.
- Involve the client and the client’s family or support persons in the planning process.
- Collaborate with other health care professionals as needed to ensure that biopsychosocial, cultural, and spiritual needs are met.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes potential needs or risks. Care plans provide communication among nurses, their patients, and other healthcare providers to achieve health care outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
The planning step of the nursing process is discussed in detail in Nursing Care Plans (NCP): Ultimate Guide and Database .
4. Implementation: “Putting the plan into action!”
The implementation phase of the nursing process is when the nurse puts the treatment plan into effect. It involves action or doing and the actual carrying out of nursing interventions outlined in the plan of care. This typically begins with the medical staff conducting any needed medical interventions.
Interventions should be specific to each patient and focus on achievable outcomes. Actions associated with a nursing care plan include monitoring the patient for signs of change or improvement, directly caring for the patient or conducting important medical tasks such as medication administration, educating and guiding the patient about further health management, and referring or contacting the patient for a follow-up.
A taxonomy of nursing interventions referred to as the Nursing Interventions Classification (NIC) taxonomy, was developed by the Iowa Intervention Project. The nurse can look up a client’s nursing diagnosis to see which nursing interventions are recommended.
Nursing Interventions Classification (NIC) System
There are more than 550 nursing intervention labels that nurses can use to provide the proper care to their patients. These interventions are categorized into seven fields or classes of interventions according to the Nursing Interventions Classification system.
These are interventions designed to help a patient change their behavior. With behavioral interventions, in contrast, patient behavior is the key and the goal is to modify it. The following measures are examples of behavioral nursing interventions:
- Encouraging stress and relaxation techniques
- Providing support to quit smoking
- Engaging the patient in some form of physical activity , like walking , to reduce the patient’s anxiety , anger, and hostility
These are interventions that refer to the community-wide approach to health behavior change. Instead of focusing mainly on the individual as a change agent, community interventionists recognize a host of other factors that contribute to an individual’s capacity to achieve optimal health, such as:
- Implementing an education program for first-time mothers
- Promoting diet and physical activities
- Initiating HIV awareness and violence-prevention programs
- Organizing a fun run to raise money for breast cancer research
These are interventions that influence a patient’s entire family.
- Implementing a family-centered approach in reducing the threat of illness spreading when one family member is diagnosed with a communicable disease
- Providing a nursing woman support in breastfeeding her new baby
- Educating family members about caring for the patient
These are interventions that designed to maintain a safe medical facility for all patients and staff, such as:
- Following procedures to reduce the risk of infection for patients during hospital stays.
- Ensuring that the patient’s environment is safe and comfortable, such as repositioning them to avoid pressure ulcers in bed
These are interventions related to a patient’s physical health to make sure that any physical needs are being met and that the patient is in a healthy condition. These nursing interventions are classified into two types: basic and complex.
- Basic. Basic interventions regarding the patient’s physical health include hands-on procedures ranging from feeding to hygiene assistance.
- Complex. Some physiological nursing interventions are more complex, such as the insertion of an IV line to administer fluids to a dehydrated patient.
These are interventions that maintain a patient’s safety and prevent injuries, such as:
- Educating a patient about how to call for assistance if they are not able to safely move around on their own
- Providing instructions for using assistive devices such as walkers or canes, or how to take a shower safely.
When implementing care, nurses need cognitive, interpersonal, and technical skills to perform the care plan successfully.
- Cognitive Skills are also known as Intellectual Skills are skills involve learning and understanding fundamental knowledge including basic sciences, nursing procedures, and their underlying rationale before caring for clients. Cognitive skills also include problem-solving, decision-making, critical thinking, clinical reasoning, and creativity.
- Interpersonal Skills are skills that involve believing, behaving, and relating to others. The effectiveness of a nursing action usually leans mainly on the nurse’s ability to communicate with the patient and the members of the health care team.
- Technical Skills are purposeful “hands-on” skills such as changing a sterile dressing , administering an injection, manipulating equipment, bandaging, moving , lifting, and repositioning clients. All of these activities require safe and competent performance.
Process of Implementing
The process of implementing typically includes the following:
Prior to implementing an intervention, the nurse must reassess the client to make sure the intervention is still needed. Even if an order is written on the care plan, the client’s condition may have changed.
Other nursing tasks or activities may also be performed by non- RN members of the healthcare team. Members of this team may include unlicensed assistive personnel (UAP) and caregivers , as well as other licensed healthcare workers, such as licensed practical nurses/licensed vocational nurses (LPNs/LVNs). The nurse may need assistance when implementing some nursing intervention, such as ambulating an unsteady obese client, repositioning a client, or when a nurse is not familiar with a particular model of traction equipment needs assistance the first time it is applied.
3. Implementing the nursing interventions
Nurses must not only have a substantial knowledge base of the sciences, nursing theory, nursing practice , and legal parameters of nursing interventions but also must have the psychomotor skills to implement procedures safely. It is necessary for nurses to describe, explain, and clarify to the client what interventions will be done, what sensations to anticipate, what the client is expected to do, and what the expected outcome is. When implementing care, nurses perform activities that may be independent, dependent, or interdependent.
Nursing interventions are grouped into three categories according to the role of the healthcare professional involved in the patient’s care:
A registered nurse can perform independent interventions on their own without the help or assistance from other medical personnel, such as:
- routine nursing tasks such as checking vital signs
- educating a patient on the importance of their medication so they can administer it as prescribed
A nurse cannot initiate dependent interventions alone. Some actions require guidance or supervision from a physician or other medical professional, such as:
- prescribing new medication
- inserting and removing a urinary catheter
- providing diet
- Implementing wound or bladder irrigations
A nurse performs as part of collaborative or interdependent interventions that involve team members across disciplines.
- In some cases, such as post- surgery , the patient’s recovery plan may require prescription medication from a physician, feeding assistance from a nurse, and treatment by a physical therapist or occupational therapist.
- The physician may prescribe a specific diet to a patient. The nurse includes diet counseling in the patient care plan. To aid the patient, even more, the nurse enlists the help of the dietician that is available in the facility.
Delegate specific nursing interventions to other members of the nursing team as appropriate. Consider the capabilities and limitations of the members of the nursing team and supervise the performance of the nursing interventions. Deciding whether delegation is indicated is another activity that arises during the nursing process.
The American Nurses Association and the National Council of State Boards of Nursing (2006) define delegation as “the process for a nurse to direct another person to perform nursing tasks and activities.” It generally concerns the appointment of the performance of activities or tasks associated with patient care to unlicensed assistive personnel while retaining accountability for the outcome.
Nevertheless, registered nurses cannot delegate responsibilities related to making nursing judgments. Examples of nursing activities that cannot be delegated to unlicensed assistive personnel include assessment and evaluation of the impact of interventions on care provided to the patient.
Record what has been done as well as the patient’s responses to nursing interventions precisely and concisely.
5. Evaluation: “Did the plan work?”
Evaluating is the fifth step of the nursing process. This final phase of the nursing process is vital to a positive patient outcome. Once all nursing intervention actions have taken place, the team now learns what works and what doesn’t by evaluating what was done beforehand. Whenever a healthcare provider intervenes or implements care, they must reassess or evaluate to ensure the desired outcome has been met. The possible patient outcomes are generally explained under three terms: the patient’s condition improved, the patient’s condition stabilized, and the patient’s condition worsened.
Steps in Evaluation
Nursing evaluation includes (1) collecting data, (2) comparing collected data with desired outcomes, (3) analyzing client’s response relating to nursing activities, (4) identifying factors that contributed to the success or failure of the care plan, (5) continuing, modifying, or terminating the nursing care plan , and (6) planning for future nursing care.
The nurse recollects data so that conclusions can be drawn about whether goals have been fulfilled. It is usually vital to collect both objective and subjective data. Data must be documented concisely and accurately to facilitate the next part of the evaluating process.
The documented goals and objectives of the nursing care plan become the standards or criteria by which to measure the client’s progress whether the desired outcome has been met, partially met, or not met.
- The goal was met , when the client response is the same as the desired outcome.
- The goal was partially met , when either a short-term outcome was achieved but the long-term goal was not, or the desired goal was incompletely attained.
- The goal was not met.
It is also very important to determine whether the nursing activities had any relation to the outcomes whether it was successfully accomplished or not.
It is required to collect more data to confirm if the plan was successful or a failure. Different factors may contribute to the achievement of goals. For example, the client’s family may or may not be supportive, or the client may be uncooperative to perform such activities.
The nursing process is dynamic and cyclical. If goals were not sufficed, the nursing process begins again from the first step. Reassessment and modification may continually be needed to keep them current and relevant depending upon general patient condition. The plan of care may be adjusted based on new assessment data. Problems may arise or change accordingly. As clients complete their goals, new goals are set. If goals remain unmet, nurses must evaluate the reasons these goals are not being achieved and recommend revisions to the nursing care plan .
Discharge planning is the process of transitioning a patient from one level of care to the next. Discharge plans are individualized instructions provided as the client is prepared for continued care outside the healthcare facility or for independent living at home. The main purpose of a discharge plan is to improve the client’s quality of life by ensuring continuity of care together with the client’s family or other healthcare workers providing continuing care.
The following are the key elements of IDEAL discharge planning according to the Agency for Healthcare Research and Quality:
- I nclude the patient and family as full partners in the discharge planning process.
- Describe what life at home will be like
- Review medications
- Highlight warning signs and problems
- Explain test results
- Schedule follow-up appointments
- E ducate the patient and family in plain language about the patient’s condition, the discharge process, and next steps throughout the hospital stay.
- A ssess how well doctors and nurses explain the diagnosis, condition, and next steps in the patient’s care to the patient and family and use teach back.
- L isten to and honor the patient’s and family’s goals, preferences, observations, and concerns.
A discharge plan includes specific components of client teaching with documentation such as:
- Equipment needed at home. Coordinate home-based care and special equipment needed.
- Dietary needs or special diet . Discuss what the patient can or cannot eat at home.
- Medications to be taken at home. List the patient’s medications and discuss the purpose of each medicine, how much to take, how to take it, and potential side effects.
- Resources such as contact numbers and addresses of important people. Write down the name and contact information of someone to call if there is a problem.
- Emergency response: Danger signs. Identify and educate patients and families about warning signs or potential problems.
- Home care activities. Educate patient on what activities to do or avoid at home.
- Summary. Discuss with the patient and family about the patient’s condition, the discharge process, and follow-up checkups.
39 thoughts on “The Nursing Process: A Comprehensive Guide”
This article is helpful
So helpful And easy to understand A very good guide for nurses
I’m a clinical instructor teaching Fundamentals this semester. The article will be very helpful to give an in-depth explanation of “The Nursing Process” to students. Thank you.
Very detailed and easy to understand. Thx
Am a student I find it very educative
This is so helpful
Excellent information that is clearly outlined and user friendly.
This is so wonderful thank you
So helpful thank you
this is very helpful thank you
Helpful. So grateful
Is the nursing process the same as “critical thinking”?
Great information! Thanks!
This is very helpful. Thank you
Great explanation, in the understanding of Nursing process
Very Helpful to students, thank you for sharing
Excellent job. A great help to all nursing students. Thank you for sharing. God bless you.
Hi Joycelyn, Thank you so much for your kind words! It’s really rewarding to hear that it’s helping nursing students out there. We’re all about sharing knowledge and making things a bit easier. 😊 If there’s anything else you’d like to see or know, just let me know. And blessings right back at you!
Thank you so much…It’s a very comprehensive reference.
You’re very welcome, A.C! I’m glad you found the nursing process reference comprehensive and useful. Just out of curiosity, is there a particular step in the nursing process you’d like to explore more deeply, or do you have any specific areas where you’d like more detailed information?
I am a nursing student and I see this as a helpful tool, very detailed and easy to understand thanks for sharing
Hi Mawuli, I’m delighted to know that you’re finding our resources helpful! If you have any specific questions or if there’s a particular topic you’d like more information on, please feel free to ask. I’m here to assist you with any nursing-related inquiries you may have. Keep up the great work in your studies! 🩺📚🌟
Keep updating me about Nursing pdfs. You guys are really good at your work!!
Hey Mokete, Thank you so much for the kind words! We’re thrilled to hear that you’re finding our nursing resources helpful. We’ll do our best to keep you updated with more valuable nursing PDFs and information. If there’s anything specific you’d like to see or if you have any questions, feel free to let us know. Keep up the great work in your nursing journey! 👩⚕️📚🌟
Thanks it really helps alot
Glad to be of help! Thank you!
This guideline very useful for Nurses building their competency and practice quality of care of Nursing to use as reference please allow to download free especially to Nurses who live in developing countries since it is not affordable to buy it
You can download the articles by printing them as PDF :) You can use a service called printfriendly (google it) to make PDFs of our webpages.
Excellent work done I’m very happy to see this stuffs
Thank you so much…It’s a very comprehensive reference. God bless you
Hello Theophilus, You’re very welcome, and thank you for the blessings! 😊 I’m glad you found the reference on the nursing process comprehensive. Just out of curiosity, is there a particular part of the nursing process you’re most interested in, or any aspect you’d like to explore more deeply?
God bless you too, and if you have any more questions, feel free to ask!
Very helpful information. Thank you.
Thank you so much, Alisa. If you need more information or help regarding this, let us know.
You’re doing a great job here. Please can you do it in such a way for us to download it as a pdf?
Hi Millicent, Thank you so much for the kind words! 😊 I’m really glad you’re finding the site useful.
Regarding your request to download content as a PDF, a neat trick you can use is the “print” function in your web browser. Here’s how you can do it:
Open the page you want to save as a PDF. -Go to the “File” menu in your browser and select “Print,” or simply press Ctrl+P (Cmd+P on Mac). -In the print window, look for a destination option and select “Save as PDF” or something similar. -Adjust any settings as needed, then click “Save” or “Print,” and choose where you want to save the file on your computer.
This way, you can turn any page into a PDF for your personal use. If you have any more questions or need further assistance, feel free to ask. Always here to help!
Very helpful Thank you
Leave a Comment Cancel reply

Level loading nurse assignments based on the work intensity
- Nursing assignments frequently are based on ratios and geography rather than work intensity associated with a specific patient assignment.
- Nurse satisfaction and perceptions of assignment fairness are highly correlated with workload.
- A quantifiable work intensity tool was developed and used to create fair, equitable, level-loaded assignments, and increasing nurse satisfaction.
J ennifer*, a nurse on a 45-bed acute care unit in a busy hospital, wants to quit her job again. She starts today like every other day this week—feeling overwhelmed. Jennifer has five patients: Maria is anxiously waiting for a test to determine if she has cancer. The prep for the test has her going to the bathroom every 10 minutes for several hours. Angelica, who’s 22 years old, has sickle cell disease. She is using a patient-controlled analgesia (PCA) pump but remains in significant pain and requires constant respiratory mon itoring and hourly medications as needed. Roberto is a postoperative patient with continuous bladder irrigation who also needs hand irrigation in addition to vital signs every hour times four and then every 4 hours. Henry, a 91-year-old man whose hemoglobin is 6.2 g/dL after a GI bleed, needs 2 units of blood. He’s forgetful, and this is his first hospitalization, so he’s frightened. Hazel is an 81-year-old grandmother with pneumonia who rarely sees Jennifer, who is busy caring for the more acutely ill patients. *Names are fictitious.
A nurse’s workload has a significant effect on patient out comes, yet too often assignments don’t take into account all the factors contributing to that workload. For example, nursing assignments based on ratios or patients’ geographic location on the unit, without considering the intensity of work required to care for individual patients, can lead to unequal workloads, frustration, and reduced satisfaction. Patients may feel that nurses are rushed or don’t have time for them, and nurses may feel guilty about not spending enough time with their patients.
Our hospital system (Cone Health in Greensboro, North Carolina) successfully used Lean methodology to address the issue of ensuring equitable workload when making staff assignments. An interdisciplinary team made up of content experts, stakeholders, and “fresh eyes” (people not directly involved in the assignment process) assembled to complete a weeklong nursing assignment rapid improvement event (RIE), which included describing the current situation, analyzing gaps, and brainstorming and implementing solutions. Our objective during the RIE was to create a dynamic staffing model that allows for assignment level loading and equitable resource allocation.
Where we started
When we started this project, staffing was based on standard ratios, geography, and patient volume; the complexity of the patient wasn’t always taken into account. Nurses felt overburdened with the intensity of work in their individual assignments and that the workload wasn’t fairly distributed. A staff survey demonstrated that nurses felt inefficient, stressed, and short-staffed. In addition, nursing supervisors had difficulty appropriately allocating resources without an accurate nursing workload evaluation.
Several existing tools measure patient acuity, but effectiveness often varies by specialty and level of care. The Cone Health Work Intensity Tool (CHWIT) uses objective and subjective criteria to assign a score (from 1 [lowest intensity] to 20 [highest intensity]) to each patient, making this tool more widely applicable.
For example, a patient with heart failure who needs medications every 4 hours and frequent assistance to the bathroom would be a level 2. However, a complex patient in the intensive care unit who requires continuous renal replacement therapy and a nursing ratio of 1:1 would be a level 10.
With this example in mind, a nurse caring for five level 2 patients and a nurse caring for one-level 10 patient would have equitable assignments based on work intensity. Geography and continuity of care aren’t calculated in the work intensity level, but they’re taken into consideration when making assignments.
What we discovered
Our initial analysis revealed that staffing assignments weren’t made based on work intensity. Instead, each charge nurse used his or her judgment, geography, and budgeted ratios to allocate nursing resources. Without a measured process, charge nurses had no way to accurately gauge which patients required more resources. And even if a charge nurse felt that a group of patients needed more, he or she couldn’t define the work intensity to make adjustments accordingly.
Nursing supervisors frequently are required to make complex decisions related to staff distribution across multiple work units, but they didn’t have a way to make rational and fair decisions about where scarce resources should be allocated. They relied on budgeted matrices. Patient complexity and total departmental workload weren’t considered.
Failure to question existing practice, unclear expectations, and ineffective resource utilization were a few of the root causes identified in the gap analysis. Other challenging components included census disparity, patient churn, and compression complexity (what nurses experience when they’re expected to assume additional, unplanned responsibilities while also performing their regular duties in a condensed time frame).
Finding a solution
The work intensity for each patient had to be quantified to create fair and equitable assignments and to facilitate staff allocation. A process for measuring work intensity and patient level loading was developed by providers, nurses, and clinical experts and rolled out throughout the hospital. An interdisciplinary team developed standard work for the new process, and then department champions and RIE team members provided education to nurses on each department. Key points (such as who was responsible for assigning numbers to the patients and the process for dividing assignments based on work intensity) were developed for the charge nurse, staff nurse, and leadership to follow daily, and champions (RIE team members and department directors and assistant directors) for each department assisted staff with the new pro cess. Follow-up meetings with the champions, pro cess owner, and RIE team leader were scheduled to address any issues. Process control boards, which displayed the department’s progress, opportunities for improvement, and ongoing direct-care problem solving, were posted on each department for use in daily huddles.
We also developed the Cone Health Work Intensity Tool (CHWIT), which is used to assign a score to each patient based on objective and subjective criteria. (See Measuring intensity .) Individual patient scores are added to calculate a cumulative score for the department, which is then divided by the number of nurses working to come up with the department’s work intensity score. This final score allows nursing supervisors to view the total points for each department and reallocate staff accurately to the higher-scoring departments. CHWIT serves as a guide to standardize work intensity across all departments, so that all nurses and nursing departments speak a common language. The result is equitable assignment distribution (level loading) among the nursing staff. (See Leveling assignments .)
To track tool use and equal workload distribution, the scores were entered into a database and the assignment variance scores were calculated to show how far each nurse’s score was from the average. In other words, if the total work intensity score for the department was 40 and four nurses were working, the average was 10 points per nurse. Target state was +1 to -1 from the average. In this example, an acceptable range would be a score of 9 to 11 per nurse. The assignment variance score was tabulated per department and for the hospital every 2 weeks. The pre-intervention work intensity variance was -2.5 to +2.6 from the average. The variance 60 days after implementing CHWIT was -.83 to +.86. The large pre-intervention variance showed that assignments weren’t level loaded—some nurses’ scores were 2.6 higher (heavier load) than other nurses’, and some were 2.5 lower (lighter load). With time, the variance score decreased, indicating that assignments were more even.
The RIE team administered a pre-intervention nursing satisfaction survey to all inpatient departments and post intervention surveys at 30, 60, and 90 days. At each interval, respondents were asked, “How often do you feel assignments are fairly distributed?” At 90 days, results yielded 97.7% favorable results compared to 63% pre-intervention. Nurses reported that they had more input in each shift assignment and that the assignments were more evenly distributed. Initially, geography issues were posted at the process control boards as barriers, but they declined significantly when the effects of more even assignments were realized.
Making a difference
Today is a new day for Jennifer. Her department now uses CHWIT and nursing assignments are level loaded by work intensity for the oncoming shift. Jennifer still has five patients, but because the entire department is evaluated as a whole with each patient having his or her own work intensity score, assignments are more equitable. Jennifer is still busy with Angelica’s PCA pump, and she will make sure that Henry receives another unit of blood. However, her two new patients are stable with scheduled meds and procedures, giving Jennifer adequate time to spend with Hazel. Jennifer can leave work knowing that she had time to spend with her patients and that she made a difference.
The authors work at Cone Health in Greensboro, North Carolina. Tara Dark is an RN4. Waqiah M. Ellis is executive director of nursing and patient services.
References:
Al-Balushi S, Sohal AS, Singh PJ, Al Hajri A, Al Farsi YM, Al Abri R. Readiness factors for lean implementation in healthcare settings—A literature review. J Health Organ Manag. 2014;28(2):135-53.
Drotz E, Poksinska B. Lean in healthcare from employees’ perspectives. J Health Organ Manag. 2014;28(2):177-95.
Firestone-Howard B, Zedreck Gonzalez JF, Dudjak LA, Ren D, Rader S. The effects of implementing a patient acuity tool on nurse satisfaction in a pulmonary medicine unit. Nurs Adm Q . 2017;41(4):E5-14.
Kidd M, Grove K, Kaiser M, Swoboda B, Taylor A. A new patient-acuity tool promotes equitable nurse-patient assignments. Am Nurse Today . 2014;9(3). myamericannurse.com/a-new-patient-acuity-tool-promotes-equitable-nurse-patient-assignments/
2 Comments .
only 5 patients? try 8-9 patients, 7 on a good day
Is there any way I can get hold of the author to request for permission to access and utilize this tool? Thank you.
Comments are closed.

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.

Examining Public Perception of Nurses

From the Midwest to the Middle East

Increasing diversity in nursing with support from Nurses on Boards Coalition

Adventures in lifelong learning

The power of language

Making peace with imperfection

When laws and nursing ethics collide

Taking on health disparities

Oncology nursing: Clinical assistant onboarding

Medication safety and pediatric health

Confidence is in

Tailored falls prevention plans

Men in nursing

FAQs: AI and prompt engineering

Caring for adults with autism spectrum disorder
Function definition grammar is wrong
The reference page on compound statements contains pseudo-grammar of the function definition syntax:
According to this grammar, the statement
should be a valid function declaration.
This disagrees with the full grammar specification and actual interpreter behaviour: it throws
More explanation needed. You see claiming that * should be a valid parameter list and hence a valid defparameter , parameter , and identifier . What do you think i am missing?
Perhaps, I see problem.
The parameter_list is ORed expression, one alternative of which is parameter_list_no_posonly . That one - also ORed expression with alternative:
With the first variant of the parameter_list_starargs syntax - all could be optional, except the * .
Related Topics
| Topic | Replies | Views | Activity | |
|---|---|---|---|---|
| Documentation | 10 | 602 | February 26, 2024 | |
| Documentation | 3 | 663 | September 20, 2023 | |
| Documentation | 3 | 426 | September 20, 2023 | |
| Python Help | 9 | 2381 | January 22, 2019 | |
| Ideas | 55 | 10306 | April 28, 2019 |
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Five rights of nursing delegation.
Jennifer M. Barrow ; Sandeep Sharma .
Affiliations
Last Update: July 24, 2023 .
- Introduction
Many definitions for delegation exist in professional literature. One of the most commonly cited definitions of the word was jointly established by the American Nurses Association and the National Council of State Boards of Nursing. These groups describe delegation as the process for a nurse to direct another person to perform nursing tasks and activities. Delegation involves at least two individuals: the delegator, and the delegatee. The delegator is a registered nurse who distributes a portion of patient care to the delegatee.
Essential Components of Delegation
Responsibility
Based on individual states’ nurse practice acts, registered nurses have a professional duty to perform patient care tasks dependably and reliably.
Authority refers to an individual’s ability to complete duties within a specific role. This authority derives from nurse practice acts and organizational policies and job descriptions.
Accountability
Accountability within the nursing context refers to nursing professionals’ legal liability for their actions related to patient care. During delegation, delegators transfer responsibility and authority for completing a task to the delegatee; however, the delegator always maintains accountability for the task's completion. The registered nurse is always accountable for the overall outcome of delegated tasks based on each state's nurse practice act provisions.
Possible legal and ethical constraints arise regarding delegation in nursing. Therefore, the American Nurses Association developed the five rights of delegation to assist nurses in making safe decisions.
Five Rights of Delegation
- Right circumstance
Right person
- Right supervision
- Right direction and communication [1]
- Issues of Concern
Five Rights of Delegation Case Study Approach
Mark is a new graduate registered nurse who has recently completed nursing orientation. He is now on his second week of non-precepted practice on a busy medical-surgical unit. During the middle of his busy night shift, Mark has several tasks that need to be completed quickly. These tasks include a linen change for a patient who just vomited, an assessment of a possibly infiltrated intravenous line, and the administration of intravenous pain medication for a patient who rates her pain 10 out of 10. Mark also needs to make hourly rounds within the next few minutes, and he is very behind on his charting. He knows he must delegate some of the tasks to his coworkers. However, Mark is unsure what he can delegate and to whom. He decides to use the five rights of delegation to help with his delegation decisions.
Right tasks
First, Mark needs to determine which tasks are right to delegate. Some questions he may ask at this time would include (1) which tasks are legally appropriate to delegate and (2) can I delegate these tasks based on this organization’s policies and procedures? Correctly answering these questions will require familiarity with institutional and nurse practice act guidance. Generally, registered nurses are responsible for assessment, planning, and evaluation within the nursing process. These actions should not be delegated to someone who is not a registered nurse. [2]
Right circumstances
After determining the right tasks for delegation, Mark considers the right circumstances of delegation. In so doing, Mark may ask the following questions: (1) are appropriate equipment and resources available to perform the task, (2) does the delegatee have the right supervision to accomplish the task, and (3) is the environment favorable for delegation in this situation? To appropriately answer these questions, it is imperative that Mark completes an assessment on each client. Patients who are or may become unstable and cases with unpredictable outcomes are not good candidates for delegation. For example, it may be appropriate for unlicensed assistive personnel to feed patients requiring assistance with the activities of daily living. However, if a patient has a high risk for aspiration and a complicated specialty diet, delegation of feeding to unlicensed assistive personnel may not be safe.
If a task and circumstance are right for delegation, the next “right” of delegation is the right person. Mark needs to consider if the potential delegatees have the requisite knowledge and experience to complete delegated tasks safely, especially concerning the assessed patient acuity. Before delegating a task, the registered nurse must know the delegatee’s job description and previous training. Mark may be unsure about his potential delegatee’s qualifications. Therefore, he might ask the following questions before delegating a task: (1) have you received training to perform this task, (2) have you ever performed this task with a patient, (3) have you ever completed this task without supervision, and (4) what problems have you encountered in performing this task in the past?
Right supervision
The right supervision must be available in all delegation situations. Nurse practice acts require the registered nurse to provide appropriate supervision for all delegated tasks. In the case study, Mark must be sure that the delegatee will provide feedback after the task is complete. Following task completion, Mark is responsible for evaluating the outcome of the task with the patient. Registered nurses are accountable for evaluation and the overall patient outcomes.
Right direction and communication
Finally, the delegator must give the right direction and communication to the delegatee. All delegators must communicate performance expectations precisely and directly. [3] Mark should not assume that his delegatee knows what to do and how to do it, even for routine tasks. Mark must consider whether the delegatee understood the assigned task, directions, patient limitations, and expected outcomes before the delegatee assumes responsibility for it. The delegatee also must comprehend what, how, and when to report back after the delegated task is complete. Delegatees also need a deadline for task completion for time-sensitive tasks. [4]
Using the five rights of delegation, Mark appropriately took care of his patients’ needs. Mark delegated the linen change to trained unlicensed assistive personnel, and he entrusted his hourly rounds to his shift charge nurse. Mark opted to assess the patient with a possibly infiltrated intravenous site first. Upon finding the site infiltrated, he assessed his patient, removed the intravenous line, and placed a warm compress on the patient’s elevated extremity. He then administered another patient’s requested pain medications after delegating new intravenous catheter placement to an intravenous-certified coworker for the patient with the infiltration. Mark was able to complete all his documentation requirements by the end of his shift.
- Clinical Significance
Reasons Delegation is Necessary for the Modern Health Care Environment
If delegation decisions are so challenging and legally charged, why should nurses delegate? Fiscal constraints, nursing shortages, and increases in patient care complexity have cultivated an environment in which delegation is necessary. If appropriately used, delegation can significantly improve patient care outcomes.
Improper Delegation
Improper delegation can negatively impact patient care while also potentially exposing the delegator to legal action. [5] All members of the health care team have valuable contributions to make toward safe, effective patient care.
Essentials of Communication
While employing the five rights of delegation in nursing practice, it is important to remember that the way the delegator asks the delegatee to perform a task can make a big difference. The delegator must use direct, honest, open, closed-loop communication to encourage teamwork and safe task performance. [6] Of the five rights of delegation, the right communication and direction are arguably the most important in ensuring good quality and safety outcomes. [7] Common delegation deficiencies for registered nurses occur when delegating tasks to unlicensed assistive personnel. These include unclear delegation directions from the registered nurse, a lack of retained accountability and follow-through, and the failure of the registered nurse to obtain the agreement of the unlicensed assistive personnel. [8]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Jennifer Barrow declares no relevant financial relationships with ineligible companies.
Disclosure: Sandeep Sharma declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Barrow JM, Sharma S. Five Rights of Nursing Delegation. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- Review Delegation of medication administration from registered nurses to non-registered support workers in community care settings: A systematic review with critical interpretive synthesis. [Int J Nurs Stud. 2022] Review Delegation of medication administration from registered nurses to non-registered support workers in community care settings: A systematic review with critical interpretive synthesis. Shore CB, Maben J, Mold F, Winkley K, Cook A, Stenner K. Int J Nurs Stud. 2022 Feb; 126:104121. Epub 2021 Oct 29.
- The effectiveness of delegation interventions by the registered nurse to the unlicensed assistive personnel and their impact on quality of care, patient satisfaction, and RN staff satisfaction: a systematic review. [JBI Libr Syst Rev. 2012] The effectiveness of delegation interventions by the registered nurse to the unlicensed assistive personnel and their impact on quality of care, patient satisfaction, and RN staff satisfaction: a systematic review. Hopkins U, Itty AS, Nazario H, Pinon M, Slyer J, Singleton J. JBI Libr Syst Rev. 2012; 10(15):895-934.
- Review The Authority for Certain Clinical Tasks Performed by Unlicensed Patient Care Technicians and LPNs/LVNs in the Hemodialysis Setting: An Update and Invitation to Take Action. [Nephrol Nurs J. 2021] Review The Authority for Certain Clinical Tasks Performed by Unlicensed Patient Care Technicians and LPNs/LVNs in the Hemodialysis Setting: An Update and Invitation to Take Action. Cahill ML, Painter DR, Branch JL. Nephrol Nurs J. 2021 Mar-Apr; 48(2):119-129.
- Factors impacting nursing assistants to accept a delegation in the acute care settings: A mixed method study. [J Clin Nurs. 2024] Factors impacting nursing assistants to accept a delegation in the acute care settings: A mixed method study. Crevacore C, Coventry L, Duffield C, Jacob E. J Clin Nurs. 2024 Jun; 33(6):2153-2164. Epub 2024 Mar 31.
- From a regulatory lens: a perspective on the delegation of nursing activities to unlicensed assistive personnel. [Semin Nurse Manag. 1995] From a regulatory lens: a perspective on the delegation of nursing activities to unlicensed assistive personnel. Roberts F. Semin Nurse Manag. 1995 Dec; 3(4):198-200.
Recent Activity
- Five Rights of Nursing Delegation - StatPearls Five Rights of Nursing Delegation - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

COMMENTS
It has clues to the information you need. It provides the framework for the assignment-making process, including staff constraints, additional duties that must be covered, and patient factors most impor-tant on your unit. Use the electronic health record (EHR) to generate various useful pieces of patient in-formation.
3.3 Assignment. Nursing team members working in inpatient or long-term care settings receive patient assignments at the start of their shift. Assignment refers to routine care, activities, and procedures that are within the legal scope of practice of registered nurses (RN), licensed practical/vocational nurses (LPN/VN), or assistive personnel ...
The Ultimate Guide to Nursing Assignments: 7 Tips and Strategies. Nursing assignments are a critical component of every nursing student's academic journey. They serve as opportunities to test your knowledge, apply theoretical concepts to real-world scenarios, and develop essential skills necessary for your future nursing career.
Delegation. According to the NCSBN/ANA guideline, delegation applies when the delegatee is performing a "specific nursing activity, skill, or procedure that is beyond the delegatee's traditional role and not routinely performed.". As opposed to work that is part of an assignment, the work associated with delegation was not learned in a ...
Making nurse-patient assignments is challenging, but with your mentor's help, you'll move from novice to competent in no time. 2. Gather your supplies (knowledge) Before completing any nursing task, you need to gather your supplies. In this case, that means knowledge. You'll need information about the unit, the nurses, and the patients.
Delivering safe, quality client care often requires registered nurses (RN) to manage care provided by the nursing team. Making assignments, delegating tasks, and supervising nursing team members are essential managerial components of an entry-level staff RN role. As previously discussed, nursing team members include RNs, licensed practical/vocational nurses (LPN/VN), and assistive personnel ...
Introduction. Nursing assignments are the backbone of patient care. They encompass a wide range of tasks that nurses perform daily, contributing significantly to the recovery and well-being of ...
Effective nursing management is crucial for ensuring high-quality patient care and maintaining a harmonious work environment. This involves several key concepts, including organizing, delegation, motivation, supervision, coordination, and conflict management. Organizing is a crucial management function that ensures tasks are logically ...
Nurse-patient assignments are created based on knowledge and understanding of nursing unit environment, nurse qualities, and patient characteristics. Clinical nurses are vital resources for critical changes in patient status. Nurse-patient assignments should be frequently reassessed and changed as needed to ensure continuous, safe, quality ...
Using their relative importance as input for the nursing planning process, we improved the nursing assignment process performance from 0.09 to 1.05, with an increase in the sigma level from −0. ...
nursing assignment: the method(s) by which the patient care load is distributed among the nursing personnel available to provide care.
A nursing care plan can be part of a case study or a stand-alone assignment. Nursing care plans are essential in nursing education as they help students develop effective nursing care planning. Formulating a nursing care plan for a patient scenario or case helps treat them as you define the guidelines and roles of nurses in caring for the patient.
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse's critical thinking to provide the best care possible to the client.. What is the purpose of the nursing process? The following are the purposes of the nursing ...
11 unique nursing units in the hospital. Results are reported by the nursing unit to show similarities and diversity among nursing units in regard to purposes and factors of the assignment process. For exam-ple, it was more meaningful to report that every unit Table 1. Participant Characteristics (n = 14) Range Mean Age, y 25-63 39
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills. Images sourced from Getty Images. Critical thinking in nursing is essential to providing high-quality patient care.
The goal was to develop national guidelines based on current research and literature to facilitate and standardize the nursing delegation process. These guidelines provide direction for employers, nurse leaders, staff nurses, and delegatees. Keywords: Delegation, evidence-based, guidelines, nursing assignment, regulation, research.
7 Leadership Styles in Nursing. Nursing leadership styles can impact job satisfaction, nurse retention rates, quality of care, and patient outcomes. The nurse's educational background, personality, and work environment may influence their nursing leadership style. Each type of nurse leader role can be valuable when utilized in the right setting.
Nurses do this activity every shift. They know how to find pertinent information and use the nursing process as a critical thinking model to guide patient care. The nursing process becomes a road map for the actions and interventions that nurses implement to optimize their patients' well-being and health. This chapter will explain how to use the nursing process as standards of professional ...
The initial nursing assessment, the first step in the five steps of the nursing process, involves the systematic and continuous collection of data; sorting, analyzing, and organizing that data; and the documentation and communication of the data collected. Critical thinking skills applied during the nursing process provide a decision-making framework to develop and guide a plan of care for the ...
The pre-intervention work intensity variance was -2.5 to +2.6 from the average. The variance 60 days after implementing CHWIT was -.83 to +.86. The large pre-intervention variance showed that assignments weren't level loaded—some nurses' scores were 2.6 higher (heavier load) than other nurses', and some were 2.5 lower (lighter load).
As health care technology continues to advance, clients require increasingly complex nursing care, and as staffing becomes more challenging, health care agencies respond with an evolving variety of nursing and assistive personnel roles and responsibilities to meet these demands. As an RN, you are on the frontlines caring for ill or injured clients and their families, advocating for clients ...
Page 2 of 10 Definitions Accountability: "To be answerable to oneself and others for one's own choices, decisions and actions as measured against a standard…" (American Nurses Association, 2015, p. 41). Delegated Responsibility: A nursing activity, skill or procedure that is transferred from a licensed nurse to adelegatee.
You see claiming that * should be a valid parameter list and hence a valid defparameter, parameter, and identifier.What do you think i am missing? Perhaps, I see ...
Many definitions for delegation exist in professional literature. One of the most commonly cited definitions of the word was jointly established by the American Nurses Association and the National Council of State Boards of Nursing. These groups describe delegation as the process for a nurse to direct another person to perform nursing tasks and activities. Delegation involves at least two ...