An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Galen Med J


Use of Hospital Information System to Improve the Quality of Health Care from Clinical Staff Perspective
Ali mohammadpour.
1 School of Para Medicine, Hamadan University of Medical Sciences, Hamadan, Iran
Mohammad Mehdi Ghaemi
2 School of Management and Information Science, Kerman University of Medical Sciences, Kerman, Iran
Reza Darrudi
3 Department of Health Information Technology, Neyshabur University of Medical Sciences, Neyshabur, Iran
Hassan Ebrahimpour Sadagheyani
Background:.
The development of hospital information systems (HISs) has a significant effect on care processes. In this regard, the clinical staff’s perspective is very important in evaluating the success of these systems. The present study aimed to evaluate the clinical staff’s perspective at hospitals affiliated to Neyshabur University of Medical Sciences on the effectiveness of the HIS in improving their performance and strategies for increasing the system effectiveness.
Materials and Methods:
In the present cross-sectional study, 120 clinical staff who actively worked with the HIS were included. A two-part questionnaire was used for data gathering.
From the perspective of the research population, the effective score of HIS was %64.42 in improving their performance, and %81.85 in the case of developed HIS according to the suggested strategies. According to the research scale, the effectiveness of the system could be improved from good to excellent in the case of implementation of strategies, so that there was a statistically significant difference between the pre- and post-effectiveness (P<0.001).
Conclusion:
Positive population perspective on the effectiveness of HIS in-performance improvement of the clinical staff indicated that there was a good context for the development and utilization of information technology in the hospitals. The clinical staff’s opinions and work needs as the primary group of patient care should be taken into consideration in order to increase the effectiveness of the HIS.
Introduction
Information technology (IT) has changed various aspects of human life and brought about fundamental changes in it [ 1 , 2 , 3 ]. The health sector is an area that is affected by IT[ 1 , 3 , 4 , 5 ]. The process of collecting and accessing health information is the most influential dimension in health [ 6 ]. Since providing health care for society is very complex and closely linked to information, it is impossible to ignore information and communication technology in medical and health care, especially hospital information systems (HIS) [ 7 ]. The HIS is a system that provides the process of collecting, storing, processing, retrieving, and displaying information needed for hospital education, management, and research [ 8 ]. The main purpose of this system is to support hospital activities at the practical, tactical, and strategic levels to provide better service for patients [ 9 ]. In general, some studies have indicated the impact of using these systems in the health care system [ 10 , 11 ]. For instance, studies have indicated that health service-providing systems utilize significant benefits such as reduction of patient waiting time [ 12 ], reduction of mortality [ 13 , 14 ], drug side effects management [ 15 , 16 ], health care professionals’ prompt and timely access to up-to-date patient information [ 12 , 17 , 18 ], reduction of medical errors [ 12 , 19 ], optimal service management [ 20 , 21 ], and improvement of care processes up to 60% [ 22 ]. Although some studies have positively evaluated the impact of the HIS, it is important to note that achieving the aforementioned benefits requires considering different infrastructures, including major users’ views in the system. In other words, the system needs to be accepted by the main users [ 11 ] because the system rejection ultimately leads to the effectiveness and performance of the HIS. The performance of any information system refers to a degree of organizational effectiveness that is achieved through the information system; hence, improving the HIS performance implies that the information system performance is tailored to internal and external changes and users’ different demands [ 3 ]. Cilliers and Flowerday (2013) found that 72% of HIS users believed that telemedicine helped improve the quality of their work. In this regard, users in rural areas used the information system and were more satisfied than users who worked in urban care centers, reflecting the appropriateness of the system’s performance to work environment processes and users’ demands in the information system [ 23 ]. All hospitals in Iran have HISs, but these software are manufactured by different companies [ 24 ]. The HIS of Neyshabur University of Medical Sciences (Version 8) was obtained from Tirageh-Computer Co. in Tehran in 2009 and was first implemented at Hakim Hospital and is currently being used in both Hakim and 22-e-Bahman hospitals. HISs of Neyshabur University of Medical Sciences have subsystems including electronic patient record management, hospital financial management procedures, evidence-based decision support systems, patient scheduling, paraclinical subsystems, and ward management [ 6 , 23 ]. Given that the hope for the system's effetiveness in improving care for hospital clinical staff indicated the belief that the use of the system helped them achieve their career goals and made them successful in providing quality care. There was no study on HIS in hospitals affiliated to Neyshabur University of Medical Sciences. Hence, the present study aimed to investigate the impact of the HIS on the improvement of clinical staff performance and strategies to increase its effectiveness from the perspective of clinical staff.
Materials and Methods
The present cross-sectional study was conducted in Neyshabur in 2019. The research population consisted of 120 clinical staff at Hakim and 22-e-Bahman hospitals of Neyshabur University of Medical Sciences (physicians, nurses, staff of laboratory sciences, midwifery, radiology, anesthesia, operating room, and health IT) who used the HIS. The census method was used in the present study; hence, all clinical and care staff who were bachelor and higher than bachelor degree used the HIS at least two days a week and were directly involved in patient care were included. Three nurses and two physicians were excluded due to lack of willingness to continue cooperation in the study. Neyshabur University of Medical Sciences has two teaching-clinical hospitals. It has used the manufactured HIS by Tirageh Computer Co. of Tehran since 2009. The data collection tool was a researcher-made questionnaire based on valid scientific literature [ 2 , 13 ,][ 25 ], medical informatics expert’s opinion, health IT, and available indices in a model by Ahitof and Newman [ 26 ]. The present questionnaire consisted of two parts; first, about demographic information of the research population (age, sex, education degree, field of study, work experience, and status of users’ training courses). Second, with 43 two-part questions; first, for examining the research population’s view about the impact of the HIS on improving the clinical staff performance (therapeutic, educational, research, and management processes in the hospital domain); and the second part about the importance of that item as an effective feature in enhancing the effectiveness of the HIS in the further improvement of performance. The reliability of the questionnaire was measured by the Cronbach’s alpha coefficient (α=97%) and its validity by the content validity. The questionnaire items included the 5-point scale (Very Low, Low, Medium, High, and Very high) with scores of 1 to 5, respectively (Figure-1). The effective score of HIS as the evaluation criterion on the improvement in clinical staff performance was calculated by the following formula: Effectiveness Index = {Σ (WtA × A + WtB × B +…WtN * N)}/ (N × 5) Where: A, B… N are the mean effectiveness ratings to survey questions on the main factors. WtA…N are relative importance weights given by clinicians to each of the main factors. N is the number of main factors. Number 5 is the highest score of any item. The following scale was used for to further interpretation of effective score of each factor on the performance improvement and also as a solution to improve the effectiveness of the HIS. The normality of the explanatory variables was checked by using the Shapiro-Wilk test. This study was approved by the Research Ethics Committee Neyshabur University of Medical Sciences under Opinion number IR.NUMS.REC.1398.004. Questionnaires were completed in person at the workplace of the research population. The results were reported according to descriptive statistics indices including mean and standard deviation; and the Paired T-Test, ANOVA, and the Pearson correlation coefficient by SPSS Version 25 (SPSS Inc. Chicago, Illinois, USA) were used to compare groups at a significant level of 0.05.
Based on research findings, most (80%)HIS users were women. The mean age of participants was 33.85±8.2 years, and most of them were in the age group of 20-39, and 33 (27.5%) had less than five years of work experience. Ninety-five (79.17%) had bachelor's degrees, and 48 (40%) were nurses. Among them, 15 (12%) physicians used the system less than the rest. Also, 45 (37.5%) were users of computer training courses or HIS ( Table-1 ). According to the research findings, there was a statistically significant difference between mean current effectiveness score (3.22) and the score of HIS effectiveness after developing factors as strategies for increasing the effectiveness of the HIS (4.09). In addition, with the development of the factors considered as strategies to increase the efficiency of HIS, the performance of clinical staff will improve (P<0.001, r=0.7). Also, based on the results of the current and developed effect difference column of the HIS, the HIS was far from ideal in terms of information integration (diff [BA]=1.18) and establishing telemedicine (diff [BA]=1.12, Table-2 ). According to the research population view, the highest effect of the HIS on improving their performance (improving therapeutic, educational, research, and management processes) belonged to accelerating paraclinical processes (mean=3.62), access to information (mean=3.43), and medical research (mean=3.65). The effectiveness score of the HIS on staff performance improvement was calculated to be 64.42% ( Figure-2 ) that was good based on the research scale ( Table-2 ). From the perspective of the research population, formulating specific rules for the acceptance of computer documentation in judicial authorities (mean=4.53), cooperation between IT experts, other staff, especially physicians and nurses (mean=4.33), facilitating education and research, simplifying paraclinical processes (mean=4.28), and the system, and defining user needs and priorities (mean=4.23), and computer literacy, and holding related HIS courses (mean=4.16) were the important factors in increasing the effectiveness of the HIS in improving their performance. The effectiveness score of the HIS on the staff performance was calculated to be 81.85% ( Figure-3 ) by developing factors. The HIS effectiveness was high based on the research scale ( Table-2 ). According to the relationship between the research population’s view on the effectiveness of the HIS in improving staff performance, there were significant relationships between research population jobs and medical research facilitation factors (P<0.001), formulating specific rules on the acceptance of computerized documentation in judicial authorities (P=0.001), integrating hospital systems (P=0.002), patient safety (P=0.004), identifying and defining user preferences and needs (P<0.001), identifying problems, obstacles and application of IT (P=0.028), and appropriate foresight (P=0.001), private sector partnerships, maintaining the data confidentiality and security(P<0.001), the collaboration of IT experts with other staff, especially physicians and nurses (P<0.001), and the ability to learn and training continues to improve care (P=0.001). In the examination of the relationship between the research population’s view on the effectiveness of HIS in improving the staff performance, a significant relationship was only found between gender and telecommunications facilities (P<0.001). In terms of each factor as a way to increase effectiveness, everyone had the same views except for cooperation of the private sector (P=0.001), and the collaboration between IT experts and other staff, especially physicians and nurses (P<0.001); there was no significant difference ( Table-3 ). According to the investigation the relationship between the research population’s view on the effectiveness of the HIS in improving the clinical staff performance and the health care system and having computer-related training courses and the HIS, there was a significant relationship only in influencing the medical research (P<0.001), enhancing patient safety (P<0.003) and identifying problems, barriers and application of IT, and proper foresight (P<0.042). The clinical staff had no similar view on the extent of effectiveness of specific laws in the adoption of computerized documentation in judicial authorities (P=0.047) and the private sector participation in the development of the HIS to increase the effectiveness of HIS (P<0.001), integration of health information (P=0.031), and the collaboration between IT experts and other staff, especially physicians and nurses (P<0.001). There was no significant difference in terms of the effectiveness of other factors ( Table-3 ). Regarding Table-4 , physicians had a more positive view on the current effect of HIS on the improvement of performance and health care system than other staff; and they reported the importance of factors. Paramedics and nurses evaluated the impact of the HIS on the performance improvement and quality of care. Furthermore, nurses had a more emphasis on improving their performance by improving the examined factors. Also, Table-4 indicated a significant difference between the research population's views on the effectiveness of the HIS in improving the staff performance and the health care system (therapeutic, educational, research, and managerial processes) and the importance of the effectiveness of factors in enhancing the clinical staff performance and the health care system through the HIS (P<0.001); and the correlation coefficient between the effect of factors and their importance was r=0.78 in the nursing group, r=0.69 in paramedics and IT staff, and r=0.26 in physicians ( Table-4 ).

The formula of Current Effectiveness Index calculation

Formula for calculating the effectiveness index after applying changes
Despite great effort to develop and utilize HISs and improve their effectiveness in improving patient care, the present study indicated an index of 64.42 out of 100 and reflected that there was still a gap to complete effectiveness. In a study by Itumalla (2012) in Indian hospitals, the customer satisfaction with the effectiveness of the HIS in improving the quality of care was 75.87 [ 2 ], reflecting the fact that we were weak in the use of information systems. However, the effectiveness could reach the index of 81.85 out of 100 by utilizing the solutions provided by HISs users. Many studies have emphasized the positive impact of HISs on cardiac care, intensive care, medication administration, and nursing care [ 27 , 28 , 29 ]. The present study examined and analyzed the factors and indicated the most remarkable effectiveness of the HIS in improving the clinical staff performance occurred by accelerating paraclinical activities, the process of diagnosis and treatment, access to quality information, and medical research. The results of some other studies also confirmed the findings of the present study [ 11 , 30 , 31 ]. According to findings of the present study, the possibility of using the telemedicine and providing facilities in the HIS to increase the patient safety such as the possibility of using simulators to train students and the ability to measure patients’ vital symptoms through wireless sensors were important factors that played insignificant roles in improving patient care, indicating the fact that the HIS surveys needed upgrading telemedicine and providing facilities for patient safety. In this regard, Cilliers and Flowerday stated that only 34% of health centers in South Africa used telemedicine. They stated that the staff’s lack of knowledge and awareness of telemedicine was the most important obstacle to the implementation and effective implementation use of telemedicine [ 23 ]. What is important is the influence of research factors on increasing the effectiveness of HIS and improving the clinical staff performance. Based on our findings, two factors, namely the formulation of specific laws for accepting computerized documentation in judicial authorities and the IT expert collaboration with other staff, especially physicians and nurses, to optimize the HIS, could significantly impact the clinical staff performance. In the field of computerized document acceptance, the acceptance of these documents by judicial authorities could prevent many processes from being reworked and thus save time for staff to do care. Therefore, the Ministry of Health needs to adopt laws and mechanisms to resolve the problem. According to our results, physicians had more positive views on the effectiveness of the HIS in improving their performance than other staff and reported the greater effectiveness of the HIS in medical research. Sadoughi et al.(2017) found that according to physicians, the greatest effectiveness of the HIS in improving care was due to its use in medical research, and it was consistent with findings of the present study [ 32 ]. Karami also stated that smart systems could be considered as a tool for accessing the latest medical findings to make the best decisions for treating patients. Furthermore, the access to all patient information avoided many reworks and accelerated the process of treatment and diagnosis [ 28 ]. The willingness to consult and receive self-care training in disease management [ 33 ][ 34 ] is the motivation for telemedicine and teleconsultation, which are major applications of health IT [ 35 ] and play important roles in accelerating service delivery, reducing costs [ 36 ], and subsequently increasing productivity. On the other hand, concepts of expediting service delivery, reducing costs, and increasing productivity are somehow related. Increased productivity can be due to lower costs due to the use of IT [ 37 ]. The use of telemedicine and teleconsultation can play important roles in expediting service delivery that inevitably result in lower service costs [ 23 ]. In the present study, the findings also confirmed the effectiveness of the HIS on the above cases. According to findings of the present study, According to findings of the present study, from the perspective of the research population, the integration of HIS, as an important factor in increasing the effectiveness of the HIS to improve the clinical staff’s performance, was far from ideal; hence, the IT professionals should pay more attention to this issue as the information sharing, and electronification of health services needed a secure-integrated environment [ 38 ]. In examining the relationship between the research population’s view on the effectiveness of the HIS on the staff performance improvement, it was found that nurses significantly considered a higher gap between the current and optimal status; and it was consistent with results of a study by Jebraeily et al. [ 39 ]. Since nurses are the main clinical users of the HIS, they play important roles in documenting and performing patient care; hence, adopting IT and meeting their business needs in HIS processes can have a significant impact on the development of these technologies and pave the way for better utilization of these systems.The familiarity and use of a small number of physicians as care managers with the HIS and participation of HIS users involved in patient care were the most important weak and power points of the present study, respectively.
The positive viewpoint of the research population on the effectiveness of the HIS in improving the clinical staff’s performance and the belief in improvement of the system by developing the proposed factors indicated that there was a good context for the development and exploitation of ITs in the hospitals, and projects such as hopeful health electronic records could be planned for its development and utilization. The effectiveness of HIS can increases in improving the performance of clinical staff and the health care system by creating an appropriate organizational culture and providing adequate training for therapists as key users of these systems, and paying attention to their work needs in the HIS. Since the implementation, implementation, and support of such systems are very costly, it is important to pay attention to the importance of budgeting in this field and take necessary measures to ensure the full acceptance of the documents derived from these systems in the legal assemblies.
Acknowledgment
Hereby, the authors sincerely thank and appreciate all of those who collaborated with the authors during this research and all the authorities of Neyshabur University of Medical Sciences, Iran. This study was funded by the Neyshabur University of Medical Sciences, Iran (grant number: 97282).
Conflict of Interest
The authors declare that there is no conflict of interest.

Levels of measurement and scaling
HAMS: An Integrated Hospital Management System to Improve Information Exchange
- Conference paper
- First Online: 11 June 2020
- Cite this conference paper

- Francesco Lubrano 17 ,
- Federico Stirano 17 ,
- Giuseppe Varavallo 17 ,
- Fabrizio Bertone 17 &
- Olivier Terzo 17
Part of the book series: Advances in Intelligent Systems and Computing ((AISC,volume 1194))
Included in the following conference series:
- Conference on Complex, Intelligent, and Software Intensive Systems
8828 Accesses
1 Citations
Effective management of hospitals and health care facilities is based on the knowledge of the available resources (e.g. staff, beds, services). Furthermore, during emergencies, a reliable exchange information system is a crucial factor in providing a timely response. This paper describes the Hospital Availability Management System (HAMS), a software developed in the framework of the EU-funded SAFECARE project. The main goal of HAMS is to provide the current status of a hospital (or health-care facility) to the internal staff, but also to first responders (paramedics, firefighters, civil protection, etc.) in order to manage the flow of patients correctly. Beyond the data coming from the normal operations of a hospital, the HAMS is able to integrate inputs from incident detection systems deployed in the hospital, to automatically update availability data after cyber and/or physical incidents, also taking into account the propagation of impacts among interconnected assets. Finally, HAMS implements the OASIS EDXL-HAVE standard, to allow the exchange of information in a open and interoperable format.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Information Systems in Support of the Decision-Making Tools
Framework for Enabling Technical and Organizational Interoperability in the Management of Environmental Crises and Disasters

Intelligent Systems for Monitoring and Prevention in Healthcare Information Systems
1 introduction.
During a situation of emergency, it is important for hospitals to be able to communicate with each other and with emergency care providers about their shortage or availability of resources in terms of bed and staff capacity. With this information, first responders are able to manage at their best the flow of patients and this improves the response time and the health service resilience during emergencies.
For example, the emergency related to the spread of the COVID-19 virus in Italy required the activation of the Remote Control Center for Health Rescue (CROSS - Centrale Remota Operazioni Soccorso Sanitario) by the Italian Department of Civil Protection. This remote control centre acts in cooperation with the regional contact points to monitor and manage the available resources for hospitals and healthcare facilities on the whole national territory. Its goal is to give support to the areas where the emergency occurred and, if needed, to get access to resources of nearby areas. The mechanism is based on requests of resources (beds, personnel, etc.) that the CROSS platform aims to satisfy, identifying which other areas can provide the needed resources.
As a consequence, effective management of emergencies and crisis depends on the knowledge of each healthcare facility of the status of its own resources and on timely information availability, reliability and intelligibility. Therefore, having a fast communication of incidents and a subsequent processing of availability is a key point in order to provide relevant information as soon as possible, giving to emergency managers the possibility to take more accurate decisions. Furthermore, it’s mandatory to identify a common protocol/language to exchange data about availability among the different Stakeholders to facilitate the overall management.
The Hospital Availability Management System (HAMS), developed in the framework of the EU-funded SAFECARE project Footnote 1 , has been designed and developed to support hospitals in both aspects. Thus, the role of the HAMS is to manage the availability of hospital assets and provide hospital status and asset availability information in case of emergency. From one side, HAMS is able to provide operators with the current availability of hospital resources through a graphic interface. Thanks to the integration with incident detection systems and impact propagation models, HAMS considers not only health emergency but also incidents (physical or cyber) that can hinder the normal operations of the structure. On the other side, HAMS is able to export data in a format compliant with the EDXL-HAVE standard [ 1 ].
This paper provides a description of the HAMS system, its context and the innovation it brings, also compared to similar existing systems. Section 2 describes which are the current approaches in the definition of system for emergency management in hospitals. Section 3 provides an overall description of a more complex system in which the HAMS is one of the building blocks. Finally, Sect. 4 describes the HAMS system, its architecture and its integration with the other modules developed within the SAFECARE project.
2 Related Works
One of the essential parts of a hospital management system is the management of information about resources availability. A system that handles the hospital status and its resources availability is in charge of tracking the occupancy rates, calculating the number of required employees and estimating the number of available employees and other resources such as departments, bed availability, services, medical equipment, drugs, etc. Such information is of primary importance in emergency situation and different software that handles it should exchange this information through a common language. For this purpose several standards have been developed and this section provide a description of software that implemented the EDXL-HAVE standard.
Analyzing this standard, one of the first software based on it was the SAHANA Disaster Management System (DMS) [ 2 , 3 ]. Sahana DMS system was used in 2010 during the earthquake emergency in Haiti and in particular in the city of Port-au-Prince. This system helped to handle the flow of victims in Haiti, sharing data about hospital availability with emergency managers.
Liapis et al. [ 4 ] described how, within the IMPRESS project, they implemented management system of Hospital Availability, through which hospitals or other health care institutions can exchange information about facilities and resources. The data about the hospital availability are entered by the hospital operators that report the bed, staff and service availability to the crisis center and first responders. In this case, operators usually receive a request from another hospital or emergency call center and answer the request reporting the availability of the hospital.
Health Resources Availability Mapping System (HeRAMS) [ 5 , 6 ] developed by the WHO and Global Health Cluster, is another relevant example. Its purpose is to evaluate the availability of services and resources in the hospitals located in territories in crisis or health emergency. The system is based on surveys carried out in hospitals to collect information about the availability of health resources and services such as staff, beds, medical equipment, drugs. The results of the surveys are reported in an interactive dashboard to visualize the status of hospital resources. Based on the results, the WHO in collaboration with the local health ministries, develops analytical reports to plan future measures to improve the situation. This solution is therefore useful to help governments managing health services during emergency.
The analysis of the main projects in the management of hospital availability shows that the use of a standard in crisis or emergency is essential to exchange information quickly and reliably between different hospital systems.
3 SAFECARE Cyber-Physical Integrated Security System
SAFECARE project is developing an integrated solution for the cyber and physical security of the healthcare sector in general [ 9 ]. As so, the HAMS service is a component plugged in more complex infrastructure, consisting of cyber and physical incident detection systems and a centralised system capable to combine and store incoming data and evaluate potential impacts when security incidents occur (Fig. 1 ).
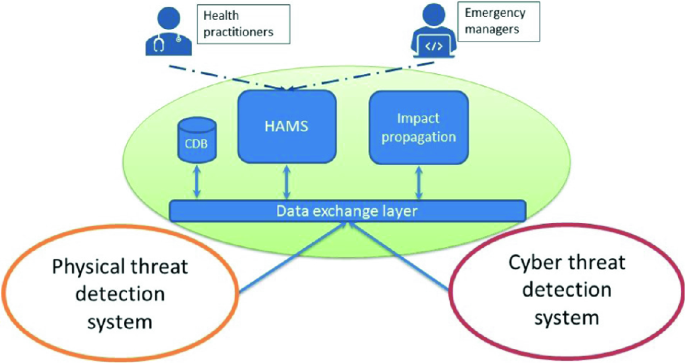
SAFECARE global architecture
Data about hospital assets are statically stored in a database, that in SAFECARE terminology is called Central Database (CDB). Such data includes departments, medical devices, facilities, personnel, etc. Moreover, dynamic information and messages such as fire alarms, physical access control alarms, malware detection and so on, are automatically generated by various sensors and systems and generally directed to human operators, that can validate or reject them. Once incidents are validated by human operators, potential impacts corresponding to that incident are evaluated and simulated. Impacts are a list of assets that may have been involved in the incident and for each asset a corresponding likelihood and severity is estimated. With the information contained in incidents and impacts, the HAMS can evaluate and update the availability and status of each resource. Indeed, the key is to optimize the way the availability of an asset in the system is updated when it changes.
4 Hospital Availability Management System
4.1 relevant data.
When an incident occurs in a healthcare facility, such as hospital, the internal staff must have updated information on the availability status of several elements in order to adequately respond to the incident and safely continue the hospital activities for patients and staff. The required information can be grouped into three main categories: hospital assets (including services), bed capacity and staff availability.
Hospital assets include all the medical devices inside the hospital. Knowing which assets are available allows the hospital staff to understand which kind of patients can be accepted or if they have to be transported in another structure. Beyond medical devices, hospital assets include all the services required for the proper work and management of the hospital. These services are crucial to provide an effective assistance to patients and users and to guarantee their security and safety, even if at first sight, some of them may seem not essential. For example, the IT system is not specifically related to the treatment of a patient. However, it is crucial for the management and recording of its personal data and for protecting them from unauthorized access.
Finally, two essential elements that a hospital management system must handle are the number of available beds and available staff. The number of total and available beds should not be expressed by a total amount for the entire healthcare facility, but for each medical ward in order to provide a clear picture of how many patients, and which of them, can be admitted in the structure. Strictly related to the bed capacity is the assessment of available staff (doctors, nurses, paramedics, etc.) as they are a crucial elements to assist patients. Thus bed and staff availability are related and the availability of a ward or a hospital strictly depends on these two elements. According to this principle, in some open standards like the EDXL-HAVE, they are considered together, and the bed capacity parameter reflects fully staffed and equipped beds.
4.2 HAMS Data Model
As described above, the HAMS deeply relies on the EDXL-HAVE standard to represent data internally and to share them with other systems. This section provides a description of the main data types effectively used by the HAMS, through a detailed description of the standard. EDXL [ 7 ] is a set of standards approved by OASIS to manage the entire emergency life cycle. It was developed to exchange and share information easily between different emergency systems. EDXL-HAVE (HAVE) [ 8 ] is an XML messaging standard developed by OASIS in the context of emergency management. A HAVE schema consists of a root element that uniquely identifies the organization that is responsible for the reporting facilities. Figure 2 shows the HAMS data model based on EDXL-HAVE main data types. Each facility is described through several attributes and a list of sub-elements that allow a complete description of hospital departments, services, and resources.
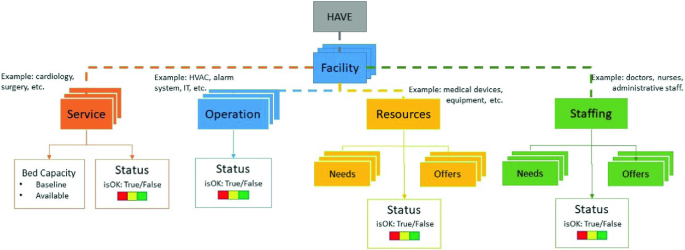
HAMS internal data model
HAVE is the top-level container element for Hospital Availability Exchange (HAVE) message. It has the following attributes:
organizationInformation; it provides basic information about the name and location of the organization for which the status and availability is being reported;
reportingPeriod; it provides information about the period to which the report refers to. If this element is left blank, the assumption is that the file refers to the last 24 h.
HAVE element has also a list of facilities. Each Facility contains the following main attributes:
name of the facility;
kind of facility (e.g. hospital, long term care, senior residence, temporary Clinic);
geoLocation field that provides geo-spatial information about facility location;
status of the facility from the perspective of the person responsible for it;
Facilities can have several sub-elements, such as services, operations and resources. Each Service is represented by a set of attributes:
name of the service;
code that uniquely defines and represents the service;
status of the service;
bedCapacity, an element that reports bed capacity of a service, represented by two attributes:
baselineCount: contains the total amount of beds.
availableCount: contains the number of vacant/available beds;
Systems that are not considered medical assets but that are fundamental for the proper operation of the healthcare facility are represented as Operation elements. Operations are characterized by a name, a kind and a status.
Finally, medical devices and staff are represented by the resource element and staffing element. Through these elements it is possible to represent the status of the resources (medical devices and staff) in terms of offers or needs too.
4.3 HAMS Internal Architecture
The HAMS has been designed as a web application, following the client-server paradigm.
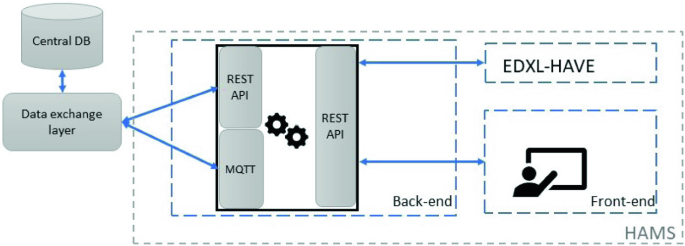
HAMS internal architecture
The Fig. 3 describes the internal architecture of the HAMS and the interconnections with other systems. Describing the HAMS architecture, two different parts can be identified:
The back-end part of the HAMS is a python web server that hosts all the logic to manage hospital status and resources availability, and also to elaborate incidents and impacts (defined in the SAFECARE terminology), and interacts with the rest of the SAFECARE systems, through the MQTT client and leveraging on REST APIs. Indeed, HAMS exchanges data communicating through the MQTT protocol, implemented in the Data Exchange Layer in the SAFECARE architecture. The MQTT protocol is based on a star logical topology: a broker is the center and manages all the connections with the clients. The transmitted messages are associated with a topic, and a client is able to receive messages associated with the topics it previously subscribed to. The messages are structured using the JSON format, and specific JSON schema has been defined for each message type. Data Exchange Layer also exposes several REST APIs to allow different modules to retrieve or store data from the Central database. Besides the communication with the Central database, the HAMS itself provides REST APIs to the front-end part and to other applications compliant with the EDXL-HAVE standard. In particular, one REST API is devoted to provide hospital data in EDXL-HAVE format. In this case, the individual facility can provide up-to-date reports via a web service, and an aggregator could poll the data regarding that facility to collect information and provide new insights based on the analysis of aggregated data.
The HAMS front-end is a web interface developed with the JavaScript framework Vue.js. The front-end represents the graphical user interface of the HAMS and it is in charge of providing an easy-to-use interface for hospital administrators and staff that manage the asset availability. Through this interface, it is possible to control the general availability of departments in each hospital as well as the availability of medical devices belonging to each department. Indeed, this interface is composed of three different views: i) a home page, that provide some general information, the overall status and the position in a map of the selected facility. It is useful to have information about position visualised in a map because hospitals may be composed of different buildings, distributed over a region; ii) a dashboard that provides a list of departments, showing for each of them the current status, the availability of beds and staff compared to the total amount (baseline), and the current status of the medical devices that belongs to that department; iii) a reporting page through which users can set manually the actual status of departments or medical devices and store updated values into the central database.
4.4 Integration with SAFECARE System
Taking into account the provisioning of availability data and the possibility of manually reporting information into the platform, the HAMS can be considered as stand-alone software to manage the availability of an hospital, but its operation is fully merged with the SAFECARE system and in particular, is an important phase of the incident lifecycle.
At boot time, HAMS populates its internal data structure with all the relevant information regarding the hospital obtaining the static data from the central database. In SAFECARE project, the Central Database, through the Data Exchange Layer, exports some REST APIs, that can be used by the HAMS module to get information about the various assets of the hospital and the corresponding baseline availability data. Following a similar approach of the HAVE standard, asset availability status is mapped using a two level approach: a Boolean value (yes or no), indicating if the asset is available or not, and a colour code (green, yellow, red) to better detail the availability. If an asset is marked with a “green” status, it is working in normal condition, thus it is fully available; if it is marked with a “yellow” status, the asset is still available, but it has been involved in an incident thus a specific attention must be put in order to avoid that the status will deteriorate; finally, if it is marked with a “red” status, there is a severe/extreme deviation from normal operation, making the asset not available. Furthermore, if an asset is a department or a facility, the static data provided by the central database module include the total number of beds as well as the number of staff people.
When fully operational, the HAMS receives messages from the incident detection modules, through the data exchange layer. This information provides data on the assets involved in an incident, associated with a severity level. Incidents are evaluated and validated by specialized human operators, so they are considered reliable. Based on the asset involved and on the severity of the incident, the internal logic of the HAMS applies several policies in order to automatically decide whether there is the need to update the status of involved assets. For example, if a physical incident reports a loitering and suspicious behaviour of two people in a hall, the incident will be managed but the HAMS will not update any availability. Instead, if a cyber incident reports an attack with high severity to a medical device or an IT system, the HAMS will update the status of these assets.
The updated status and availability are shown to the final user through the graphic interface. At the same time, the HAMS module updates a specific table of the Central Database in order to keep track of the history of availability changes.
After an incident is validated by a human operator, it is forwarded to the HAMS, and the other decision modules present into SAFECARE system. One of these module is the Impact propagation module [ 10 ]. This software, triggered by incident messages, evaluates the incident taking into account the directly involved assets and the severity, and it provides a list of assets that could potentially be impacted, simulating potential cascading effects of that incident. Thus, the output of the impact propagation module is a list of assets with a corresponding likelihood that indicates how likely it is for an asset to be affected or impacted by the incident. Once this process ends, the list of potentially involved assets is also forwarded to the HAMS. Upon these values, the HAMS will compute the final hospital availability after the incident, updating medical devices status as well as bed and staff availability if necessary. Updates of status and resource availability are stored into the Central Database and showed by the HAMS web interface, so that users can visualise updated information. These features, combined with the standardized data model and the possibility to get the hospital status through a specific REST API too, make the HAMS an innovative tool in its application field.
5 Conclusions
This paper describes the Hospital Availability Management Systems, developed as a sub-module of a more complex system that manages cyber and physical security in hospitals, considered critical infrastructures. The need to have updated information about the status and the availability of medical devices, available beds, and medical staff is crucial during emergencies. HAMS can manage this information, allowing authorized users to get data through a web interface or through a REST API that exports data according to the EDXL-HAVE format. It provides such information to other software and management systems, which are able to gather data from different infrastructures and to provide indications to first responders. This can improve the health service resilience and it is useful to reroute the flow of patients in case of incident. Through the integration with the SAFECARE system, HAMS aims to automatically update data about the availability of hospital assets, speeding up this process. Thus, HAMS can be considered as a step forward towards a fully automatic system able to update single asset availability based on incidents.
https://www.safecare-project.eu/ .
O’Donnell, D., Wilkins, B., Brooks, R., Robertson, S.M. (eds.): Emergency Data Exchange Language (EDXL) Hospital AVailability Exchange (HAVE) Version 2.0., 18 March 2019. OASIS Committee Specification 02. HL7 Informative Document: https://docs.oasis-open.org/emergency/edxl-have/v2.0/cs02/edxl-have-v2.0-cs02.html . Latest version: https://docs.oasis-open.org/emergency/edxl-have/v2.0/edxl-have-v2.0.html
Careem, M., De Silva, C., De Silva, R., Raschid, L., Weerawarana, S.: Sahana: overview of a disaster management system. In: 2006 International Conference on Information and Automation, pp. 361–366. IEEE, December 2006
Google Scholar
Currion, P., Silva, C.D., Van de Walle, B.: Open source software for disaster management. Commun. ACM 50 (3), 61–65 (2007)
Article Google Scholar
Liapis, A., et al.: A position paper on improving preparedness and response of health services in major crises. In: Bellamine Ben Saoud, N., Adam, C., Hanachi, C. (eds.) Information Systems for Crisis Response and Management in Mediterranean Countries, ISCRAM-med 2015. Lecture Notes in Business Information Processing, vol. 233. Springer, Cham (2015)
World Health Organization. Health Resources Availability Mapping System (HeRAMS) (2016)
Elamein, M., Woods, P., Elshaiekh, N.: Assessment of (HeRAMS) Knowledge Management System of Humanitarian Emergency in Sudan (2014)
Waters, J.: Emergency Data Exchange Language (EDXL) Distribution Element Version 2.0. (2013)
Waters, J., Dwarkanath, S.: The Hospital AVailability Exchange (EDXL HAVE) Standard (2010)
Bertone, F., Lubrano, F., Gavelli, M., Terzo, O., Biasin, E., Kamenjasevic, E., Suciu, G.: Integrated cyber-physical security approach for healthcare sector. In: Soldatos, J., Philpot, J., Giunta, G. (eds.) Cyber-Physical Threat Intelligence for Critical Infrastructures Security: A Guide to Integrated Cyber-Physical Protection of Modern Critical Infrastructures. Now Publishers (2020)
Atigui, F., Hamdi, F., Lammari, N., Si-said Cherfi, S.: Vulnerability and incident propagation in cyber-physical systems. In: Soldatos, J., Philpot, J., Giunta, G. (eds.) Cyber-Physical Threat Intelligence for Critical Infrastructures Security: A Guide to Integrated Cyber-Physical Protection of Modern Critical Infrastructures. Now Publishers (2020)
Download references
Acknowledgements
This research received funding from the European Union’s H2020 Research and Innovation Action “Secure societies – Protecting freedom and security of Europe and its citizens” challenge, under grant agreement 787002 (project SAFECARE).
Author information
Authors and affiliations.
LINKS Foundation, via Boggio 61, Turin, Italy
Francesco Lubrano, Federico Stirano, Giuseppe Varavallo, Fabrizio Bertone & Olivier Terzo
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Francesco Lubrano .
Editor information
Editors and affiliations.
Department of Information and Communication Engineering, Faculty of Information Engineering, Fukuoka Institute of Technology, Fukuoka, Japan
Leonard Barolli
Institute of Information Technology, Lodz University of Technology, Łódź, Poland
Aneta Poniszewska-Maranda
Faculty of Business Administration, Rissho University, Tokyo, Japan
Tomoya Enokido

Rights and permissions
Reprints and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this paper
Cite this paper.
Lubrano, F., Stirano, F., Varavallo, G., Bertone, F., Terzo, O. (2021). HAMS: An Integrated Hospital Management System to Improve Information Exchange. In: Barolli, L., Poniszewska-Maranda, A., Enokido, T. (eds) Complex, Intelligent and Software Intensive Systems. CISIS 2020. Advances in Intelligent Systems and Computing, vol 1194. Springer, Cham. https://doi.org/10.1007/978-3-030-50454-0_32
Download citation
DOI : https://doi.org/10.1007/978-3-030-50454-0_32
Published : 11 June 2020
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-50453-3
Online ISBN : 978-3-030-50454-0
eBook Packages : Intelligent Technologies and Robotics Intelligent Technologies and Robotics (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
This paper is in the following e-collection/theme issue:
Published on 8.4.2024 in Vol 26 (2024)
Longitudinal Monitoring of Clinician-Patient Video Visits During the Peak of the COVID-19 Pandemic: Adoption and Sustained Challenges in an Integrated Health Care Delivery System
Authors of this article:

Original Paper
- Jessica A Palakshappa 1, 2 , MD, MS ;
- Erica R Hale 1, 2 , MS ;
- Joshua D Brown 1 , PhD ;
- Carol A Kittel 2 , MA ;
- Emily Dressler 2 , PhD ;
- Gary E Rosenthal 1, 2 , MD ;
- Sarah L Cutrona 3, 4 , MD, MPH ;
- Kristie L Foley 2 , MS, PhD ;
- Emily R Haines 2 , PhD ;
- Thomas K Houston II 1, 2 , MD, MPH
1 Atrium Health Wake Forest Baptist, Winston Salem, NC, United States
2 Wake Forest University School of Medicine, Winston Salem, NC, United States
3 Department of Population and Quantitative Health Sciences, University of Massachusetts Chan Medical School, Worcester, MA, United States
4 Center for Healthcare Organization and Implementation Research, Veterans Affairs Bedford Healthcare System, Bedford, MA, United States
Corresponding Author:
Jessica A Palakshappa, MD, MS
Wake Forest University School of Medicine
1 Medical Center Blvd
Winston Salem, NC, 27157
United States
Phone: 1 336 716 8465
Email: [email protected]
Background: Numerous prior opinion papers, administrative electronic health record data studies, and cross-sectional surveys of telehealth during the pandemic have been published, but none have combined assessments of video visit success monitoring with longitudinal assessments of perceived challenges to the rapid adoption of video visits during the pandemic.
Objective: This study aims to quantify (1) the use of video visits (compared with in-person and telephone visits) over time during the pandemic, (2) video visit successful connection rates, and (3) changes in perceived video visit challenges.
Methods: A web-based survey was developed for the dual purpose of monitoring and improving video visit implementation in our health care system during the COVID-19 pandemic. The survey included questions regarding rates of in-person, telephone, and video visits for clinician-patient encounters; the rate of successful connection for video visits; and perceived challenges to video visits (eg, software, hardware, bandwidth, and technology literacy). The survey was distributed via email to physicians, advanced practice professionals, and clinicians in May 2020. The survey was repeated in March 2021. Differences between the 2020 and 2021 responses were adjusted for within-respondent correlation across surveys and tested using generalized estimating equations.
Results: A total of 1126 surveys were completed (511 surveys in 2020 and 615 surveys in 2021). In 2020, only 21.7% (73/336) of clinicians reported no difficulty connecting with patients during video visits and 28.6% (93/325) of clinicians reported no difficulty in 2021. The distribution of the percentage of successfully connected video visits (“Over the past two weeks of scheduled visits, what percentage did you successfully connect with patients by video?”) was not significantly different between 2020 and 2021 ( P =.74). Challenges in conducting video visits persisted over time. Poor connectivity was the most common challenge reported by clinicians. This response increased over time, with 30.5% (156/511) selecting it as a challenge in 2020 and 37.1% (228/615) in 2021 ( P =.01). Patients not having access to their electronic health record portals was also a commonly reported challenge (109/511, 21.3% in 2020 and 137/615, 22.3% in 2021, P =.73).
Conclusions: During the pandemic, our health care delivery system rapidly adopted synchronous patient-clinician communication using video visits. As experience with video visits increased, the reported failure rate did not significantly decline, and clinicians continued to report challenges related to general network connectivity and patient access to technology.
Introduction
Interest in telehealth from policy makers, health care providers, patients, and families continues to grow [ 1 ], including newer modalities such as video visits [ 2 ]. Video visits refer to clinician-patient communication that includes real time video and audio assessment of the patient when the clinician is in a different location. Video visits have the potential to improve efficiency for clinicians and to improve access for patients, particularly those who reside in rural areas or with transportation barriers [ 3 ]. The technology to support video visits has existed for decades; however, only a small minority of clinicians used this form of telehealth in their practices [ 4 ] prior to the COVID-19 pandemic. There are multiple reasons why telehealth adoption was slow despite its potential benefits including changing cost and reimbursement policies, federal and state licensing laws, incompatible electronic health records, and gaps in internet access in certain areas.
The COVID-19 pandemic and subsequent public health emergency led to fundamental shifts in how health care was delivered in the United States, including the rapid adoption of telehealth services. Before the public health emergency, approximately 13,000 fee-for-service Medicare beneficiaries received telehealth services in a week and that number increased to nearly 1.7 million beneficiaries by the last week of April 2020 [ 5 ]. While the need to avoid in-person contact fueled the initial rapid rise, regulations and restrictions were temporarily lifted during this time facilitating its use. Clinicians were also paid for telehealth services at the same rate as in-person medical services. Several studies have reported on the rapid uptake of telehealth, including video visits, in this context [ 6 - 8 ]. However, few reports have explored rates of success and failure of video visits over time. The challenges clinicians face in conducting video visits have also not been explored. Understanding these challenges will be important for improving and expanding the reach of telehealth services after the pandemic has ended.
In the context of the rapidly increasing use of telehealth to conduct video visits, and consistent with the sociotechnical model’s [ 9 ] emphasis on monitoring the implementation of health information technology in complex adaptive health care systems, our health care delivery system initiated a series of brief assessments of video visit adoption. The research objective of this report is to summarize the findings of the video visit monitoring including (1) the use of video visits (compared with in-person and telephone visits) over time during the pandemic, (2) video visit successful connection rates, and (3) changes in perceived video visit challenges. With patient and clinician skills and experience with video visits increasing over time, our primary hypothesis was that clinicians’ perceived challenges to completing video visits (eg, software, hardware, bandwidth, and technology literacy) would decline over time.
Study Design
The design was a longitudinal series of 2 cross-sectional assessments (2020 and 2021). In summary, for the dual purpose of monitoring and improving telehealth implementation in our health care delivery system, institutional leaders developed a brief web-based survey regarding the use of video visits and challenges. The survey was initially distributed in 2020. Given the ongoing public health emergency and the need to re-evaluate telehealth use, the survey was repeated in 2021. Institutional leaders encouraged clinicians to complete the survey, communicating encouragement via emails and announcements at in-person faculty and departmental meetings.
Ethical Considerations
As the brief assessments were distributed by the clinical system as part of ongoing quality improvement, the project was approved as an research protocol as exempt from human participants approval by the Wake Forest University School of Medicine Institutional Review Board (IRB00077473). The survey did not collect identifying information from the participants.
Survey Development
Published in 2010 by Sittig and Singh [ 9 ], the sociotechnical model of health information technology was the first to fully emphasize the importance of system monitoring in implementation frameworks. Key aspects of monitoring, including measuring how the technology is being used by clinicians and whether implementation outcomes are being achieved, were considered when developing the survey. The survey was developed with a literature search, expert review, and iterative pilot-testing (see Multimedia Appendix 1 ). The final survey included 12 questions related to rates of in-person, telephone, and video for clinician-patient encounters; the rate of successful connection for video visits; and perceived challenges to video visits (eg, software, hardware, bandwidth, and technology literacy).
Study Population
The study population included all outpatient clinicians practicing across the health care delivery system; we excluded clinicians without direct patient care responsibilities. The system includes 5 hospitals and over 350 primary care and specialty clinics that provide care to over 2 million persons annually. The brief assessment was distributed to clinicians in 2020 and 2021 (1937 clinicians and 2843 clinicians, respectively).
Survey Distribution and Data Collection
As we are an integrated health care delivery system, we had access to the contact details of all providers. Our group practice clinical operations executive committee facilitated the survey distribution by requesting that each department chair and clinical service line director send an email to their team of providers to notify them of the survey and encourage completion. Surveys were collected and managed using REDCap (Research Electronic Data Capture), a secure, web-based app designed to support data capture [ 10 , 11 ]. A unique survey link was distributed via email to each clinician in May 2020 and March 2021. The system sent up to 2 reminder emails if the recipient had not yet completed the survey.
Statistical Analysis
To take full advantage of the data collected, we first analyzed the results as 2 cross-sectional surveys. In this primary analysis, we included all respondents in each year. We recognize that a subset of clinicians also responded in both years. Thus, as a secondary analysis, we analyzed the data limited to the longitudinal cohort who participated in both years. First, summary statistics are presented as count (frequency) for categorical variables and mean (SD) or median (IQR) for continuous variables as appropriate. Generalized estimating equations were then used to model frequency distributions of in-person, telephone, and video visits, and patient and clinician challenges. These logit models were adjusted for within-respondent correlation across surveys via an exchangeable correlation structure. P values of .05 were considered statistically significant. P values for multiple comparisons in frequency distributions of in-person, telephone, and video visits between physicians, advanced practice professionals (APPs), and other clinicians were adjusted via the Tukey-Kramer method to control for type I errors with a corrected P value <.05 deemed statistically significant [ 12 ]. All statistical analyses were performed with R (version 4.2.1; R Core Team) [ 13 ].
We recognize that a subset of clinicians responded in both years. Thus, as a secondary analysis, we analyzed the data limited to the longitudinal cohort who participated in both surveys. For the secondary analysis, matched pairs analyses were performed as were performed in the entire sample with only those responses from clinicians that completed both surveys.
Surveillance Participation and Participant Characteristics
In 2020, 1937 surveys were sent and 511 responses were received (response rate 26.4%). In 2021, 2843 surveys were sent and 615 responses were received (response rate 21.6%). In both years, over 55% of the respondents were physicians from a wide range of clinical specialties. About half of the clinicians who completed the survey in 2020 also completed it in 2021 ( Table 1 ).
a n=511 responses in 2020 and n=615 responses in 2021.
b n=300 responses in 2020 and n=353 responses in 2021.
Health Care Delivery by In-Person and Telephone
To place the volume of telehealth in context, we first asked about the number of in-person encounters completed over the past 2 weeks ( Table 2 ). The distribution of responses differed between 2020 and 2021 ( P <.001). Modeled probabilities show fewer respondents reported zero (22.2% vs 4.9%) or 1 to 10 (33.5% vs 11.5%) in-person visits in 2021 as compared with 2020. The volume of in-person visits increased over time ( Table 2 ). Further, the majority of respondents (399/509, 78.4%) reported at least 1 telephone visit in 2020 and 65.7% (369/562) in 2021 although the distribution of responses differed from 2020 to 2021 ( P <.001).
a Differences in frequency distributions between 2020 and 2021 tested via generalized estimating equation modeling; P value adjusted using Tukey-Kramer method to control for type I errors.
Health Care Delivery by Video Visits
Many health care providers were engaged in virtual care, with 65.9% (336/510) health care providers reporting video visit encounters in 2020 and 57.6% (325/564) health care providers reporting video visit encounters in 2021 ( Table 2 ) although the distribution of responses again changed from 2020 to 2021 ( P <.001). Compared with 2020, fewer 2021 respondents reported 11-25 (18.6% vs 6.7%), 26-50 (5.9% vs 2.8%), or over 50 (2.4% vs 2%) visits.
Secondary analyses were robust to missing data and showed that the results (distributions of in-person, phone, and video visits) did not change when limiting the data to only respondents who participated in both surveys.
Comparing Health Care Delivery by Physicians, APPs, and Others
We also compared health care delivery modality by type of clinician (physicians, APPs, or others). Patterns of health care delivery reported in the overall sample were similar in the physician, APP, and other subgroups. There were no significant differences between physicians and APPs in the number of patient encounters that were completed as in-person, telephone visits, or video visits in 2020 or 2021.
Perceived Challenges to Patient-Clinician Connection Using Video Visits
The use of video visits came with challenges. In 2020, only 21.7% (73/336) of clinicians reported no difficulty connecting with patients during video visits and 28.6% (93/325) of clinicians reported no difficulty in 2021 ( Figure 1 ). The distribution of the percentage of successfully connected video visits (“Over the past two weeks of scheduled visits, what percentage did you successfully connect with patients by video?”) was not significantly different between 2020 and 2021 ( P =.74, Figure 1 ). There was also no significant difference between physicians and APPs in the rate of successful video connection with patients in either year.

Clinicians were asked about the challenges in successfully completing video visits (see Table 3 ). The most commonly reported challenge was poor connectivity. This response increased over time with 30.5% (156/511) selecting it as a challenge in 2020 and 37.1% (228/615) selecting it as a challenge in 2021 ( P =.01). Patients not having access to their electronic health record portals was also a commonly reported challenge (109/511, 21.3% in 2020 and 137/615, 22.3% in 2021; P =.73).
a P value adjusted using the Tukey-Kramer method to control for type I errors.
b For some clinical video visits, a prerequisite was that patients needed to have registered with the patient portal.
Principal Findings
Although telehealth technology was available in our health care delivery system prior to the COVID-19 pandemic, it saw only limited use for providing synchronous care to patients prior to the pandemic. Inconsistent reimbursement for services, restrictions on the physical location of patients and clinicians during telehealth, and rules about types of visits that were acceptable for telehealth services all contributed to its limited use [ 14 , 15 ]. With the pandemic, and consistent with other reports, our health care delivery system rapidly expanded the provision of clinical care by way of video visits. Later in the pandemic, in-person visits did increase, but the use of video visits remained well above prepandemic levels.
Overall, there has been a shift toward a more positive sentiment about telehealth and telemedicine since the start of the pandemic. A scoping review by Doraiswamy et al [ 16 ] reported 543 telehealth-related papers (mostly opinions, commentaries, and perspectives; 61%) published across 331 different journals from January to June 2020. Most of these new reports had a “celebratory” or favorable sentiment about the use of telehealth. The scope of the increase in telehealth during the public health emergency likely contributed to this sentiment though concerns about patient and clinician connection, the lack of physical examinations, and cost-effectiveness were still noted by some. Although our providers reported benefits for clinical video telehealth beyond audio-only calls for patient-provider visits, failure to connect using clinical video visits was common.
While reports have documented challenges with clinical video telehealth [ 17 ], few have monitored these challenges over time. During the pandemic, as our health care delivery system’s experience with video visits grew, clinicians did not report a meaningful reduction in connection failure rate. The most frequently reported challenges were general network connectivity and those related to the digital divide (eg, patient lack of internet access, needed software, or internet-connected cameras). Gaps in access to technology and the internet for telehealth may impact some patient groups more than others. For example, older age, rural residence, dual Medicare and Medicaid enrollment, and non-Hispanic Black or Hispanic race or ethnicity have been shown to be associated with a lower probability of technology ownership, access to the internet, and use of the internet for communication in cancer survivors [ 18 ]. Further, over 10% of clinicians also reported that they experienced software or hardware challenges (eg, limited availability of internet cameras at a clinical location). Expanding telehealth will require ongoing investments in technology for clinicians. New workflows to support successful connection during video visits and follow-up processes may also be needed.
Our video visit monitoring results were shared with clinical operations leadership. In response to the sustained challenges noted, we initiated a new video visit program to provide patient support prior to scheduled video visits. Our technology navigators are a specially trained, centralized team and are directed to reach out to vulnerable patients and families to facilitate video visit access. A new electronic health record dashboard identified patients with (1) a scheduled video visit and (2) 1 or more risk factors (eg, lack of a prior successful video visit and lack of patient portal access). We further prioritized patients older than 65 years and those living in rural areas. Technology navigators reached out by telephone to contact these at-risk patients to assess their technology access (eg, internet, software, webcam, or smartphone), technology literacy and perceived competence, and availability of at-home support from family and friends. The technology navigators then troubleshoot any challenges noted by the patients and offer to conduct a “practice” video visit. Evaluation of this program is ongoing. In 2022-2023, the navigators contacted 1266 patients at high risk for video visit failure. Among those contacted, 515 requested and were provided assistance. With previsit support from the navigators, the patient-provider scheduled video visit completion rate was 84% as compared with a 60% completion rate among those patients who did not receive support.
Limitations of our video visit surveillance analysis include that the data were collected across 1 health care delivery system with an integrated electronic health care record system. The perceptions and challenges may be different in a smaller health care system and in those with different health care record systems. The survey measured only clinician-reported telehealth use and success rates which may be limited by recall. As with all surveys, our results may be biased as only about one-quarter of the sample responded. It is possible that respondents experienced more challenges conducting video visits than those who did not respond. Further, not all clinicians longitudinally completed both the 2020 and 2021 surveys—due both to response rates and providers leaving and entering the health care system. Thus, changes over time may represent differences in the underlying sample. For example, new clinicians may have been more or less familiar with conducting video visits.
Conclusions
Recent reviews have noted the need for more evidence related to telehealth’s implementation, effectiveness, and health equity in telehealth access [ 16 , 19 , 20 ]. Although internet and smartphone access has increased over the last decade (with older adults being one of the fastest-growing subgroups of new adoption), our longitudinal video visit surveillance reveals that the digital divide is still a significant barrier to video visit access.
Although Healthy People 2030 (a set of national objectives to improve health and well-being) includes developmental and research objectives related to patient portals and increasing the use of telehealth to improve access to health services [ 21 ], some social determinants of health taxonomies do not include technology access. If telehealth is increasingly an important component of health care access, then technology access (eg, internet, smartphone, patient portal, and connected hardware, such as internet-connected video) should be considered a social determinant of health [ 22 ]. A comprehensive solution to overcoming the digital divide has not yet been achieved. However, some partial solutions include directly providing technology to patients, providing detailed instructions, and support services (eg, our technology navigator program), and engaging trusted caregivers (family and friends) who may be able to assist patients [ 23 - 27 ].
Acknowledgments
The project was supported through the National Cancer Institute Cancer Moonshot initiative—iDAPT: Implementation and Informatics–Developing Adaptable Processes and Technologies for Cancer Control (P50 CA244693); the Wake Forest Clinical and Translational Science Award (5UL1TR001420); and also a career development award to JAP (1K23AG073529).
Conflicts of Interest
None declared.
Brief Provider Telehealth Assessment.
- World Health Organization. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth 2009. Geneva, Switzerland. World Health Organization; 2010.
- Moulaei K, Shanbehzadeh M, Bahaadinbeigy K, Kazemi-Arpanahi H. Survey of the patients' perspectives and preferences in adopting telepharmacy versus in-person visits to the pharmacy: a feasibility study during the COVID-19 pandemic. BMC Med Inform Decis Mak. 2022;22(1):99. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nesbitt TS. The evolution of telehealth: where have we been and where are we going? In: Lustig TA, editor. The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary. Washington, DC. National Academies Press; 2012;11-16.
- Kane CK, Gillis K. The use of telemedicine by physicians: still the exception rather than the rule. Health Aff (Millwood). 2018;37(12):1923-1930. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kane CK, Gillis K. The use of telemedicine by physicians: still the exception rather than the rule. Health Aff (Millwood). Dec 2018;37(12):1923-1930. [ CrossRef ] [ Medline ]
- Weiner JP, Bandeian S, Hatef E, Lans D, Liu A, Lemke KW. In-person and telehealth ambulatory contacts and costs in a large US insured cohort before and during the COVID-19 pandemic. JAMA Netw Open. 2021;4(3):e212618. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gilson SF, Umscheid CA, Laiteerapong N, Ossey G, Nunes KJ, Shah SD. Growth of ambulatory virtual visits and differential use by patient sociodemographics at one urban academic medical center during the COVID-19 pandemic: retrospective analysis. JMIR Med Inform. 2020;8(12):e24544. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hatef E, Wilson RF, Hannum SM, Zhang A, Kharrazi H, Weiner JP, et al. Use of Telehealth During the COVID-19 Era. Rockville, MD. Agency for Healthcare Research and Quality; 2023.
- Sittig DF, Singh H. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care. 2010;19(Suppl 3):i68-i74. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Midway S, Robertson M, Flinn S, Kaller M. Comparing multiple comparisons: practical guidance for choosing the best multiple comparisons test. PeerJ. 2020;8:e10387. [ FREE Full text ] [ CrossRef ] [ Medline ]
- R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria. R Foundation for Statistical Computing; 2023.
- Shaver J. The state of telehealth before and after the COVID-19 pandemic. Prim Care. 2022;49(4):517-530. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hyder MA, Razzak J. Telemedicine in the United States: an introduction for students and residents. J Med Internet Res. 2020;22(11):e20839. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Doraiswamy S, Abraham A, Mamtani R, Cheema S. Use of telehealth during the COVID-19 pandemic: scoping review. J Med Internet Res. 2020;22(12):e24087. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Garfan S, Alamoodi AH, Zaidan BB, Al-Zobbi M, Hamid RA, Alwan JK, et al. Telehealth utilization during the Covid-19 pandemic: a systematic review. Comput Biol Med. 2021;138:104878. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lama Y, Davidoff AJ, Vanderpool RC, Jensen RE. Telehealth availability and use of related technologies among medicare-enrolled cancer survivors: cross-sectional findings from the onset of the COVID-19 pandemic. J Med Internet Res. 2022;24(1):e34616. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Moulaei K, Moulaei R, Bahaadinbeigy K. Barriers and facilitators of using health information technologies by women: a scoping review. BMC Med Inform Decis Mak. 2023;23(1):176. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Rodriguez JA, Shachar C, Bates DW. Digital inclusion as health care: supporting health care equity with digital-infrastructure initiatives. N Engl J Med. 2022;386(12):1101-1103. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Healthy people 2030: health IT. U.S. Department of Health and Human Services. URL: https://health.gov/healthypeople/objectives-and-data/browse-objectives/health-it [accessed 2024-03-14]
- Benda NC, Veinot TC, Sieck CJ, Ancker JS. Broadband internet access is a social determinant of health!. Am J Public Health. 2020;110(8):1123-1125. [ CrossRef ] [ Medline ]
- Francis J, Kadylak T, Makki TW, Rikard RV, Cotten SR. Catalyst to connection: when technical difficulties lead to social support for older adults. Am Behav Sci. 2018;62(9):1167-1185. [ CrossRef ]
- Cotten SR, Yost EA, Berkowsky RW, Winstead V, Anderson WA. Designing Technology Training for Older Adults in Continuing Care Retirement Communities, 1st Edition. Boca Raton, FL. CRC Press; 2016.
- Sadasivam RS, Kinney RL, Lemon SC, Shimada SL, Allison JJ, Houston TK. Internet health information seeking is a team sport: analysis of the Pew internet survey. Int J Med Inform. 2013;82(3):193-200. [ CrossRef ] [ Medline ]
- Luger TM, Hogan TP, Richardson LM, Cioffari-Bailiff L, Harvey K, Houston TK. Older veteran digital disparities: examining the potential for solutions within social networks. J Med Internet Res. 2016;18(11):e296. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Houston TK, Richardson LM, Cotten SR. Patient-directed digital health technologies: is implementation outpacing evidence? Med Care. 2019;57(2):95-97. [ CrossRef ] [ Medline ]
Abbreviations
Edited by G Eysenbach, T Leung; submitted 26.10.23; peer-reviewed by K Moulaei; comments to author 19.12.23; revised version received 24.01.24; accepted 09.03.24; published 08.04.24.
©Jessica A Palakshappa, Erica R Hale, Joshua D Brown, Carol A Kittel, Emily Dressler, Gary E Rosenthal, Sarah L Cutrona, Kristie L Foley, Emily R Haines, Thomas K Houston II. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 08.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.

IMAGES
VIDEO
COMMENTS
Introduction. Information technology (IT) has changed various aspects of human life and brought about fundamental changes in it [1,2,3].The health sector is an area that is affected by IT[1,3,4,5].The process of collecting and accessing health information is the most influential dimension in health [].Since providing health care for society is very complex and closely linked to information, it ...
Abstract: The literature on the topic of health information systems (HISs) is reviewed in this paper. Specifically, the paper. reviews the literature on (i) the theoretical concept o f HISs (The ...
Hospital Information Systems ... The response of healthcare professionals to the use of hospital information systems is an important research topic that can explain the success or failure of any HIS development and implementation project4. ... Paper forms were also used to enhance the response of the participants who needed to be reminded with ...
It is commonly defined as a comprehensive information system used to collect, store, process, retrieve, and. communicate patient care and administrative information for all hospital-affiliated ...
Health information system deployment has been driven by the transformation and digitalization currently confronting healthcare. The need and potential of these systems within healthcare have been tremendously driven by the global instability that has affected several interrelated sectors. Accordingly, many research studies have reported on the inadequacies of these systems within the ...
Although prior studies reported nationwide surveys on the adoption of EHR systems, they mainly focus on the usability of EHR 9 or emphasize the hospital-level usages and adoptions. 11 This study instead employs a qualitative research approach, as the primary objective was to explore clinicians' in-depth assessment of factors relevant to a ...
The paper presents a contextual approach to analyse studies on the evaluation of health information systems (HISs) by applying a content, context and process (CCP) framework. • The study shows the role of context has been largely neglected in HISs evaluations. • The lack of a proper method in stakeholder identification was identified. •
There have been several studies centred on health information systems with many insights provided to enhance health care applications globally. These studies have provided theoretical schemes for fortifying the enactment and utilisation of the Health Information System (HIS). In addition, these research studies contribute greatly to the development of HIS in alignment with major stakeholders ...
Healthcare-IS papers accentuate the unique contribution IS researchers can make to better understand, manage, and design for the healthcare context, by analyzing empirical data and explore contextual influences by applying and elaborating IS theories ( Chiasson & Davidson 2004 ). As shown in. Table 1.
This research review paper aims to provide a comprehensive overview of the current state of intelligent information systems in the healthcare sector, focusing on the main areas of application, the challenges faced, and the prospects of these technologies. Intelligent information systems (IIS) have become a crucial component in modern healthcare ...
1.Introduction and m otivation. In a review of health care information systems research (often referred to as health information technology or HIT research) published in Information Systems (IS) journals, Chiasson and Davidson (2004) challenged the IS field to expand its "contextual envelope" by embracing the health care sector as a socially important and theoretically interesting context ...
Abstract: Health information system deployment has been driven by the transformation and digital-. ization currently confronting healthcare. The need and potential of these systems within ...
Wellbeing can be ensured in society through quality healthcare, a minimum of medical errors, and the improved performance of healthcare professionals. To this end, health information systems have been implemented in hospitals, with this implementation representing progress in medicine and information technologies. As a result, life expectancy has significantly increased, standards in ...
Level 3: Centralised electronic health systems with both paper-based and electronic features: In this instance, the use of a paper-based system would occur when a healthcare worker records a patient's health information and medical record in a patient's file. To maintain consistency, standardised forms are used to record patient's ...
The purpose of our study aimed to identify attributes capable of improving physicians' satisfaction levels with the use of a hospital information system (HIS). A model inclusive of system quality, information quality, and service quality related to an HIS is used to form antecedents of user satisfaction. Survey methodology was used to collect an attributive set representing the system ...
The Hospital Availability Management System (HAMS), developed in the framework of the EU-funded SAFECARE project 1, has been designed and developed to support hospitals in both aspects. Thus, the role of the HAMS is to manage the availability of hospital assets and provide hospital status and asset availability information in case of emergency.
This paper aims to examine the role of hospital information systems in improving health care quality in hospital. Primary data was collected through distributing questionnaire to patient. A total ...
Background: Numerous prior opinion papers, administrative electronic health record data studies, and cross-sectional surveys of telehealth during the pandemic have been published, but none have combined assessments of video visit success monitoring with longitudinal assessments of perceived challenges to the rapid adoption of video visits during the pandemic.
A hospital is a place that needs more effective and efficient management of information, people, and assets. This paper demonstrates the design and implementation of an autonomous system with mern ...
1.2 Abstract. Hospital Management System provides the benefits of stream lined operations, enhanced. administration, control, superior patient care, strict cost control and improved ...