- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Medicare Assignment: Everything You Need to Know
Medicare assignment.
- Providers Accepting Assignment
- Providers Who Do Not
- Billing Options
- Assignment of Benefits
- How to Choose
Frequently Asked Questions
Medicare assignment is an agreement between Medicare and medical providers (doctors, hospitals, medical equipment suppliers, etc.) in which the provider agrees to accept Medicare’s fee schedule as payment in full when Medicare patients are treated.
This article will explain how Medicare assignment works, and what you need to know in order to ensure that you won’t receive unexpected bills.
fizkes / Getty Images
There are 35 million Americans who have Original Medicare. Medicare is a federal program and most medical providers throughout the country accept assignment with Medicare. As a result, these enrollees have a lot more options for medical providers than most of the rest of the population.
They can see any provider who accepts assignment, anywhere in the country. They can be assured that they will only have to pay their expected Medicare cost-sharing (deductible and coinsurance, some or all of which may be paid by a Medigap plan , Medicaid, or supplemental coverage provided by an employer or former employer).
It’s important to note here that the rules are different for the 29 million Americans who have Medicare Advantage plans. These beneficiaries cannot simply use any medical provider who accepts Medicare assignment.
Instead, each Medicare Advantage plan has its own network of providers —much like the health insurance plans that many Americans are accustomed to obtaining from employers or purchasing in the exchange/marketplace .
A provider who accepts assignment with Medicare may or may not be in-network with some or all of the Medicare Advantage plans that offer coverage in a given area. Some Medicare Advantage plans— health maintenance organizations (HMOs) , in particular—will only cover an enrollee’s claims if they use providers who are in the plan's network.
Other Medicare Advantage plans— preferred provider organizations (PPOs) , in particular—will cover out-of-network care but the enrollee will pay more than they would have paid had they seen an in-network provider.
Original Medicare
The bottom line is that Medicare assignment only determines provider accessibility and costs for people who have Original Medicare. People with Medicare Advantage need to understand their own plan’s provider network and coverage rules.
When discussing Medicare assignment and access to providers in this article, keep in mind that it is referring to people who have Original Medicare.
How to Make Sure Your Provider Accepts Assignment
Most doctors, hospitals, and other medical providers in the United States do accept Medicare assignment.
Provider Participation Stats
According to the Centers for Medicare and Medicaid Services, 98% of providers participate in Medicare, which means they accept assignment.
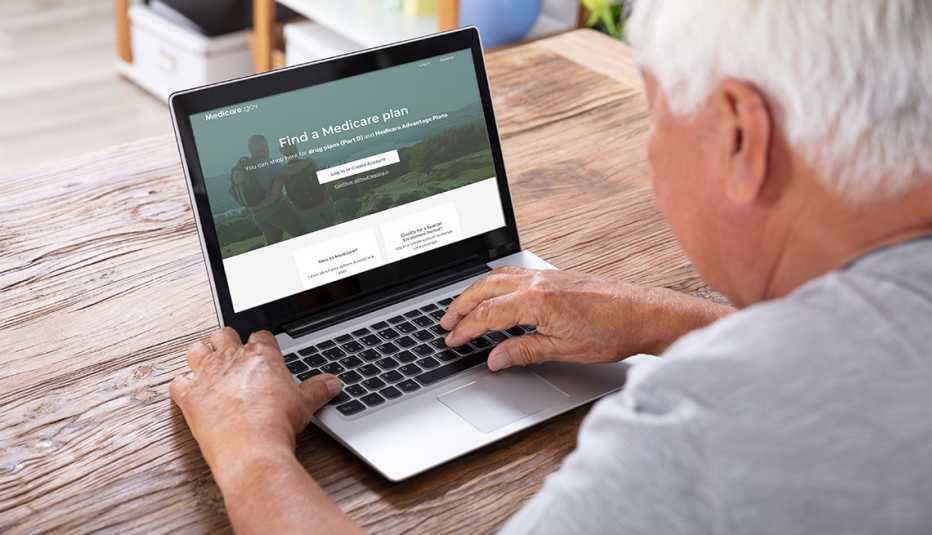
You can ask the provider directly about their participation with Medicare. But Medicare also has a tool that you can use to find participating doctors, hospitals, home health care services, and other providers.
There’s a filter on that tool labeled “Medicare-approved payment.” If you turn on that filter, you will only see providers who accept Medicare assignment. Under each provider’s information, it will say “Charges the Medicare-approved amount (so you pay less out-of-pocket).”
What If Your Provider Doesn’t Accept Assignment?
If your medical provider or equipment supplier doesn’t accept assignment, it means they haven’t agreed to accept Medicare’s approved amounts as payment in full for all of the services.
These providers can still choose to accept assignment on a case-by-case basis. But because they haven’t agreed to accept Medicare assignment for all services, they are considered nonparticipating providers.
Note that "nonparticipating" does not mean that a provider has opted out of Medicare altogether. Medicare will still pay claims for services received from a nonparticipating provider (i.e., one who does not accept Medicare assignment), whereas Medicare does not cover any of the cost of services obtained from a provider who has officially opted out of Medicare.
If a Medicare beneficiary uses a provider who has opted out of Medicare, that person will pay the provider directly and Medicare will not be involved in any way.
Physicians Who Have Opted Out
Only about 1% of all non-pediatric physicians have opted out of Medicare.
For providers who have not opted out of Medicare but who also don’t accept assignment, Medicare will still pay nearly as much as it would have paid if you had used a provider who accepts assignment. Here’s how it works:
- Medicare will pay the provider 95% of the amount they would pay if the provider accepted assignment.
- The provider can charge the person receiving care more than the Medicare-approved amount, but only up to 15% more (some states limit this further). This extra amount, which the patient has to pay out-of-pocket, is known as the limiting charge . But the 15% cap does not apply to medical equipment suppliers; if they do not accept assignment with Medicare, there is no limit on how much they can charge the person receiving care. This is why it’s particularly important to make sure that the supplier accepts Medicare assignment if you need medical equipment.
- The nonparticipating provider may require the person receiving care to pay the entire bill up front and seek reimbursement from Medicare (using Form CMS 1490-S ). Alternatively, they may submit a claim to Medicare on behalf of the person receiving care (using Form CMS-1500 ).
- A nonparticipating provider can choose to accept assignment on a case-by-case basis. They can indicate this on Form CMS-1500 in box 27. The vast majority of nonparticipating providers who bill Medicare choose to accept assignment for the claim being billed.
- Nonparticipating providers do not have to bill your Medigap plan on your behalf.
Billing Options for Providers Who Accept Medicare
When a medical provider accepts assignment with Medicare, part of the agreement is that they will submit bills to Medicare on behalf of the person receiving care. So if you only see providers who accept assignment, you will never need to submit your own bills to Medicare for reimbursement.
If you have a Medigap plan that supplements your Original Medicare coverage, you should present the Medigap coverage information to the provider at the time of service. Medicare will forward the claim information to your Medigap insurer, reducing administrative work on your part.
Depending on the Medigap plan you have, the services that you receive, and the amount you’ve already spent in out-of-pocket costs, the Medigap plan may pay some or all of the out-of-pocket costs that you would otherwise have after Medicare pays its share.
(Note that if you have a type of Medigap plan called Medicare SELECT, you will have to stay within the plan’s network of providers in order to receive benefits. But this is not the case with other Medigap plans.)
After the claim is processed, you’ll be able to see details in your MyMedicare.gov account . Medicare will also send you a Medicare Summary Notice. This is Medicare’s version of an explanation of benefits (EOB) , which is sent out every three months.
If you have a Medigap plan, it should also send you an EOB or something similar, explaining the claim and whether the policy paid any part of it.
What Is Medicare Assignment of Benefits?
For Medicare beneficiaries, assignment of benefits means that the person receiving care agrees to allow a nonparticipating provider to bill Medicare directly (as opposed to having the person receiving care pay the bill up front and seek reimbursement from Medicare). Assignment of benefits is authorized by the person receiving care in Box 13 of Form CMS-1500 .
If the person receiving care refuses to assign benefits, Medicare can only reimburse the person receiving care instead of paying the nonparticipating provider directly.
Things to Consider Before Choosing a Provider
If you’re enrolled in Original Medicare, you have a wide range of options in terms of the providers you can use—far more than most other Americans. In most cases, your preferred doctor and other medical providers will accept assignment with Medicare, keeping your out-of-pocket costs lower than they would otherwise be, and reducing administrative hassle.
There may be circumstances, however, when the best option is a nonparticipating provider or even a provider who has opted out of Medicare altogether. If you choose one of these options, be sure you discuss the details with the provider before proceeding with the treatment.
You’ll want to understand how much is going to be billed and whether the provider will bill Medicare on your behalf if you agree to assign benefits (note that this is not possible if the provider has opted out of Medicare).
If you have supplemental coverage, you’ll also want to check with that plan to see whether it will still pick up some of the cost and, if so, how much you should expect to pay out of your own pocket.
A medical provider who accepts Medicare assignment is considered a participating provider. These providers have agreed to accept Medicare’s fee schedule as payment in full for services they provide to Medicare beneficiaries. Most doctors, hospitals, and other medical providers do accept Medicare assignment.
Nonparticipating providers are those who have not signed an agreement with Medicare to accept Medicare’s rates as payment in full. However, they can agree to accept assignment on a case-by-case basis, as long as they haven’t opted out of Medicare altogether. If they do not accept assignment, they can bill the patient up to 15% more than the Medicare-approved rate.
Providers who opt out of Medicare cannot bill Medicare and Medicare will not pay them or reimburse beneficiaries for their services. But there is no limit on how much they can bill for their services.
A Word From Verywell
It’s in your best interest to choose a provider who accepts Medicare assignment. This will keep your costs as low as possible, streamline the billing and claims process, and ensure that your Medigap plan picks up its share of the costs.
If you feel like you need help navigating the provider options or seeking care from a provider who doesn’t accept assignment, the Medicare State Health Insurance Assistance Program (SHIP) in your state may be able to help.
A doctor who does not accept Medicare assignment has not agreed to accept Medicare’s fee schedule as payment in full for their services. These doctors are considered nonparticipating with Medicare and can bill Medicare beneficiaries up to 15% more than the Medicare-approved amount.
They also have the option to accept assignment (i.e., accept Medicare’s rate as payment in full) on a case-by-case basis.
There are certain circumstances in which a provider is required by law to accept assignment. This includes situations in which the person receiving care has both Medicare and Medicaid. And it also applies to certain medical services, including lab tests, ambulance services, and drugs that are covered under Medicare Part B (as opposed to Part D).
In 2021, 98% of American physicians had participation agreements with Medicare, leaving only about 2% who did not accept assignment (either as a nonparticipating provider, or a provider who had opted out of Medicare altogether).
Accepting assignment is something that the medical provider does, whereas assignment of benefits is something that the patient (the Medicare beneficiary) does. To accept assignment means that the medical provider has agreed to accept Medicare’s approved fee as payment in full for services they provide.
Assignment of benefits means that the person receiving care agrees to allow a medical provider to bill Medicare directly, as opposed to having the person receiving care pay the provider and then seek reimbursement from Medicare.
Centers for Medicare and Medicaid Services. Medicare monthly enrollment .
Centers for Medicare and Medicaid Services. Annual Medicare participation announcement .
Centers for Medicare and Medicaid Services. Lower costs with assignment .
Centers for Medicare and Medicaid Services. Find providers who have opted out of Medicare .
Kaiser Family Foundation. How many physicians have opted-out of the Medicare program ?
Center for Medicare Advocacy. Durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) updates .
Centers for Medicare and Medicaid Services. Check the status of a claim .
Centers for Medicare and Medicaid Services. Medicare claims processing manual. Chapter 26 - completing and processing form CMS-1500 data set .
Centers for Medicare and Medicaid Services. Ambulance fee schedule .
Centers for Medicare and Medicaid Services. Prescription drugs (outpatient) .
By Louise Norris Norris is a licensed health insurance agent, book author, and freelance writer. She graduated magna cum laude from Colorado State University.
Use our RMD calculator to estimate your required withdrawals from tax-deferred retirement plans.
Popular Searches
AARP daily Crossword Puzzle
Hotels with AARP discounts
Life Insurance
AARP Dental Insurance Plans
Suggested Links
AARP MEMBERSHIP — $12 FOR YOUR FIRST YEAR WHEN YOU SIGN UP FOR AUTOMATIC RENEWAL
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
- right_container
Work & Jobs
Social Security
AARP en Español
- Membership & Benefits
AARP Rewards
- AARP Rewards %{points}%
Conditions & Treatments
Drugs & Supplements
Health Care & Coverage
Health Benefits

Staying Fit
Your Personalized Guide to Fitness

AARP Hearing Center
Ways To Improve Your Hearing

Brain Health Resources
Tools and Explainers on Brain Health
How to Save Your Own Life
Scams & Fraud
Personal Finance
Money Benefits

View and Report Scams in Your Area

AARP Foundation Tax-Aide
Free Tax Preparation Assistance

AARP Money Map
Get Your Finances Back on Track

Budget & Savings
Make Your Appliances Last Longer
Small Business
Age Discrimination

Flexible Work
Freelance Jobs You Can Do From Home

AARP Skills Builder
Online Courses to Boost Your Career

31 Great Ways to Boost Your Career

ON-DEMAND WEBINARS
Tips to Enhance Your Job Search

Get More out of Your Benefits

When to Start Taking Social Security

10 Top Social Security FAQs

Social Security Benefits Calculator

Medicare Made Easy
Original vs. Medicare Advantage

Enrollment Guide
Step-by-Step Tool for First-Timers

Prescription Drugs
9 Biggest Changes Under New Rx Law

Medicare FAQs
Quick Answers to Your Top Questions
Care at Home
Financial & Legal
Life Balance

LONG-TERM CARE
Understanding Basics of LTC Insurance

State Guides
Assistance and Services in Your Area

Prepare to Care Guides
How to Develop a Caregiving Plan

End of Life
How to Cope With Grief, Loss
Recently Played
Word & Trivia
Atari® & Retro
Members Only
Staying Sharp
Mobile Apps
More About Games

Right Again! Trivia

Right Again! Trivia – Sports

Atari® Video Games

Throwback Thursday Crossword
Travel Tips
Vacation Ideas
Destinations
Travel Benefits

Beach vacation ideas
Vacations for Sun and Fun

Plan Ahead for Tourist Taxes

AARP City Guide
Discover Seattle

How to Pick the Right Cruise for You
Entertainment & Style
Family & Relationships
Personal Tech
Home & Living
Celebrities
Beauty & Style

TV for Grownups
Best Reality TV Shows for Grownups

Robert De Niro Reflects on His Life
Free Online Novel
Read 'Chase'

Sex & Dating
Spice Up Your Love Life

Navigate All Kinds of Connections

How to Create a Home Gym

Store Medical Records on Your Phone?

Maximize the Life of Your Phone Battery

Virtual Community Center
Join Free Tech Help Events

Create a Hygge Haven

Soups to Comfort Your Soul

AARP Smart Guide
Spring Clean All of Your Spaces
Driver Safety
Maintenance & Safety
Trends & Technology

How to Keep Your Car Running

We Need To Talk
Assess Your Loved One's Driving Skills

AARP Smart Driver Course

Building Resilience in Difficult Times

Tips for Finding Your Calm

Weight Loss After 50 Challenge

Cautionary Tales of Today's Biggest Scams

7 Top Podcasts for Armchair Travelers

Jean Chatzky: ‘Closing the Savings Gap’

Quick Digest of Today's Top News

AARP Top Tips for Navigating Life

Get Moving With Our Workout Series
You are now leaving AARP.org and going to a website that is not operated by AARP. A different privacy policy and terms of service will apply.
Go to Series Main Page
What is Medicare assignment and how does it work?
Kimberly Lankford,
Because Medicare decides how much to pay providers for covered services, if the provider agrees to the Medicare-approved amount, even if it is less than they usually charge, they’re accepting assignment.
A doctor who accepts assignment agrees to charge you no more than the amount Medicare has approved for that service. By comparison, a doctor who participates in Medicare but doesn’t accept assignment can potentially charge you up to 15 percent more than the Medicare-approved amount.
That’s why it’s important to ask if a provider accepts assignment before you receive care, even if they accept Medicare patients. If a doctor doesn’t accept assignment, you will pay more for that physician’s services compared with one who does.

AARP Membership — $12 for your first year when you sign up for Automatic Renewal
How much do I pay if my doctor accepts assignment?
If your doctor accepts assignment, you will usually pay 20 percent of the Medicare-approved amount for the service, called coinsurance, after you’ve paid the annual deductible. Because Medicare Part B covers doctor and outpatient services, your $240 deductible for Part B in 2024 applies before most coverage begins.
All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent. You can get some preventive services and screenings, such as mammograms and colonoscopies , without paying a deductible or coinsurance if the provider accepts assignment.
What if my doctor doesn’t accept assignment?
A doctor who takes Medicare but doesn’t accept assignment can still treat Medicare patients but won’t always accept the Medicare-approved amount as payment in full.
This means they can charge you up to a maximum of 15 percent more than Medicare pays for the service you receive, called “balance billing.” In this case, you’re responsible for the additional charge, plus the regular 20 percent coinsurance, as your share of the cost.
How to cover the extra cost? If you have a Medicare supplement policy , better known as Medigap, it may cover the extra 15 percent, called Medicare Part B excess charges.
All Medigap policies cover Part B’s 20 percent coinsurance in full or in part. The F and G policies cover the 15 percent excess charges from doctors who don’t accept assignment, but Plan F is no longer available to new enrollees, only those eligible for Medicare before Jan. 1, 2020, even if they haven’t enrolled in Medicare yet. However, anyone who is enrolled in original Medicare can apply for Plan G.
Remember that Medigap policies only cover excess charges for doctors who accept Medicare but don’t accept assignment, and they won’t cover costs for doctors who opt out of Medicare entirely.
Good to know. A few states limit the amount of excess fees a doctor can charge Medicare patients. For example, Massachusetts and Ohio prohibit balance billing, requiring doctors who accept Medicare to take the Medicare-approved amount. New York limits excess charges to 5 percent over the Medicare-approved amount for most services, rather than 15 percent.

AARP NEWSLETTERS

%{ newsLetterPromoText }%
%{ description }%
Privacy Policy
ARTICLE CONTINUES AFTER ADVERTISEMENT
How do I find doctors who accept assignment?
Before you start working with a new doctor, ask whether he or she accepts assignment. About 98 percent of providers billing Medicare are participating providers, which means they accept assignment on all Medicare claims, according to KFF.
You can get help finding doctors and other providers in your area who accept assignment by zip code using Medicare’s Physician Compare tool .
Those who accept assignment have this note under the name: “Charges the Medicare-approved amount (so you pay less out of pocket).” However, not all doctors who accept assignment are accepting new Medicare patients.
AARP® Vision Plans from VSP™
Exclusive vision insurance plans designed for members and their families
What does it mean if a doctor opts out of Medicare?
Doctors who opt out of Medicare can’t bill Medicare for services you receive. They also aren’t bound by Medicare’s limitations on charges.
In this case, you enter into a private contract with the provider and agree to pay the full bill. Be aware that neither Medicare nor your Medigap plan will reimburse you for these charges.
In 2023, only 1 percent of physicians who aren’t pediatricians opted out of the Medicare program, according to KFF. The percentage is larger for some specialties — 7.7 percent of psychiatrists and 4.2 percent of plastic and reconstructive surgeons have opted out of Medicare.
Keep in mind
These rules apply to original Medicare. Other factors determine costs if you choose to get coverage through a private Medicare Advantage plan . Most Medicare Advantage plans have provider networks, and they may charge more or not cover services from out-of-network providers.
Before choosing a Medicare Advantage plan, find out whether your chosen doctor or provider is covered and identify how much you’ll pay. You can use the Medicare Plan Finder to compare the Medicare Advantage plans and their out-of-pocket costs in your area.
Return to Medicare Q&A main page
Kimberly Lankford is a contributing writer who covers Medicare and personal finance. She wrote about insurance, Medicare, retirement and taxes for more than 20 years at Kiplinger’s Personal Finance and has written for The Washington Post and Boston Globe . She received the personal finance Best in Business award from the Society of American Business Editors and Writers and the New York State Society of CPAs’ excellence in financial journalism award for her guide to Medicare.
Discover AARP Members Only Access
Already a Member? Login

More on Medicare

How Do I Create a Personal Online Medicare Account?
You can do a lot when you decide to look electronically

I Got a Medicare Summary Notice in the Mail. What Is It?
This statement shows what was billed, paid in past 3 months
Understanding Medicare’s Options: Parts A, B, C and D
Making sense of the alphabet soup of health care choices
Recommended for You
AARP Value & Member Benefits

Learn, earn and redeem points for rewards with our free loyalty program

AARP® Dental Insurance Plan administered by Delta Dental Insurance Company
Dental insurance plans for members and their families

The National Hearing Test
Members can take a free hearing test by phone

AARP® Staying Sharp®
Activities, recipes, challenges and more with full access to AARP Staying Sharp®
SAVE MONEY WITH THESE LIMITED-TIME OFFERS
Medicare Interactive Medicare answers at your fingertips -->
Participating, non-participating, and opt-out providers, outpatient provider services.
You must be logged in to bookmark pages.
Email Address * Required
Password * Required
Lost your password?
If you have Original Medicare , your Part B costs once you have met your deductible can vary depending on the type of provider you see. For cost purposes, there are three types of provider, meaning three different relationships a provider can have with Medicare . A provider’s type determines how much you will pay for Part B -covered services.
- These providers are required to submit a bill (file a claim ) to Medicare for care you receive. Medicare will process the bill and pay your provider directly for your care. If your provider does not file a claim for your care, there are troubleshooting steps to help resolve the problem .
- If you see a participating provider , you are responsible for paying a 20% coinsurance for Medicare-covered services.
- Certain providers, such as clinical social workers and physician assistants, must always take assignment if they accept Medicare.
- Non-participating providers can charge up to 15% more than Medicare’s approved amount for the cost of services you receive (known as the limiting charge ). This means you are responsible for up to 35% (20% coinsurance + 15% limiting charge) of Medicare’s approved amount for covered services.
- Some states may restrict the limiting charge when you see non-participating providers. For example, New York State’s limiting charge is set at 5%, instead of 15%, for most services. For more information, contact your State Health Insurance Assistance Program (SHIP) .
- If you pay the full cost of your care up front, your provider should still submit a bill to Medicare. Afterward, you should receive from Medicare a Medicare Summary Notice (MSN) and reimbursement for 80% of the Medicare-approved amount .
- The limiting charge rules do not apply to durable medical equipment (DME) suppliers . Be sure to learn about the different rules that apply when receiving services from a DME supplier .
- Medicare will not pay for care you receive from an opt-out provider (except in emergencies). You are responsible for the entire cost of your care.
- The provider must give you a private contract describing their charges and confirming that you understand you are responsible for the full cost of your care and that Medicare will not reimburse you.
- Opt-out providers do not bill Medicare for services you receive.
- Many psychiatrists opt out of Medicare.
Providers who take assignment should submit a bill to a Medicare Administrative Contractor (MAC) within one calendar year of the date you received care. If your provider misses the filing deadline, they cannot bill Medicare for the care they provided to you. However, they can still charge you a 20% coinsurance and any applicable deductible amount.
Be sure to ask your provider if they are participating, non-participating, or opt-out. You can also check by using Medicare’s Physician Compare tool .
Update your browser to view this website correctly. Update my browser now

What Does It Mean for a Doctor to Accept Medicare Assignment?
Written by: Malini Ghoshal, RPh, MS
Reviewed by: Malinda Cannon, Licensed Insurance Agent
Key Takeaways
Doctors who accept Medicare assignment are paid agreed-upon rates for services.
It’s important to verify that your doctor accepts assignment before receiving services to avoid high out-of-pocket costs.
A doctor or clinician may be “non-participating” but can still agree to accept Medicare assignment for some services.
If you visit a doctor or clinician who has opted out (doesn’t accept Medicare), you may have to pay for your entire visit cost unless it’s a medical emergency.
Medigap Supplemental insurance (Medigap) plans won’t pay for service costs from doctors who don’t accept assignment.
One of the things that Original Medicare beneficiaries often enjoy about their coverage is that they can use it anywhere in the country. Unlike plans with provider networks, they can visit doctors either at home or on the road; both are covered the same.
But do all doctors accept Medicare patients?
Truth is, this wide-ranging coverage area only applies to doctors who accept Medicare assignment. Fortunately, most do. If you’re eligible for Medicare, it’s important to visit doctors and clinicians who accept Medicare assignment. This will help keep your out-of-pocket costs within your control. Doctors who agree to accept Medicare assignment sign an agreement that they’re willing to accept payment from Medicare for their services.
If you’re a current beneficiary or nearing enrollment, you may have other questions. Do all doctors accept Medicare Advantage plans? What about Medicare Supplement insurance (Medigap)? Read on to learn how to find doctors that accept Medicare assignment and how this keeps your healthcare costs down.
My Medicare coverage doesn’t address all of my needs.
What Is Medicare Assignment of Benefits?
When you’re eligible for Medicare, you have the option to visit doctors and clinicians who accept assignment. This means they are Medicare-approved providers who agree to receive Medicare reimbursement rates for covered services. This helps save you money.
If you have Original Medicare (Part A and B), your doctor visits are covered by your Part B plan. Inpatient services such as hospital stays and some skilled nursing care are covered by Part A .
In order for a participating doctor (or facility) to bill Medicare and be reimbursed, you must authorize Medicare to reimburse your doctor directly for your covered services. This is called the Medicare assignment of benefits. You transfer your right to receive Medicare payment for a covered service to your doctor or other provider.
Note: If you have a Medicare Supplement insurance ( Medigap ) plan to pay for out-of-pocket costs, you may also need to sign a separate assignment of benefits form for Medigap reimbursement. More on Medigap below.
How Can I Find Doctors Near Me That Accept Medicare?
There are several ways to find doctors and other clinicians who accept Medicare assignment close to you.
First, let’s take a look at the different types of Medicare providers.
They include:
Participating providers: Medicare-participating doctors and providers sign a participation agreement stating they will accept Medicare reimbursement rates for their services.
Non-participating providers: Doctors or providers who are non-participating providers are eligible to accept Medicare assignment but haven’t signed a Medicare agreement. They may choose to accept assignment on a case-by-case basis. If you visit a non-participating provider, make sure to ask if they accept assignment for your particular service. Also get a copy of their fees. They will need to select “yes” on Centers for Medicare & Medicaid Services CMS Form 1500 to accept assignment for the service.
Opt-out providers: Some doctors and other providers choose not to accept Medicare. If they choose to opt out, the period is two years (based on Medicare guidelines). The opt-out automatically renews if the provider doesn’t request a change in their status. You would be responsible for paying all costs for services received from an opt-out provider. You cannot bill Medicare for reimbursement unless the service was an urgent or emergency medical need. According to a report from KFF , roughly 1% of non-pediatric physicians opted out of Medicare in 2023.
Visiting a doctor who doesn’t accept assignment may cost you more. These providers can charge you up to 15% more than the Medicare-approved rate for a given service. This 15% charge is called the limiting charge. Some states limit this extra charge to a certain percent. This may also be called the Part B excess charge.
Here are some tips for finding doctors and providers who accept Medicare assignment:
- The easiest way to find a doctor who accepts Medicare assignment is to contact their office and ask them directly.
- If you’re looking for a new doctor, you can use the Medicare search tool to find clinicians and doctors that accept Medicare assignment.
- You can also ask a state health insurance assistance program (SHIP) representative for help in locating a doctor that accepts Medicare assignment.
- Don’t assume that having a longstanding relationship with your doctor means nothing will ever change. Check in with them to make sure they still accept Medicare assignment and whether they’re planning to opt out.
Note: Your doctor can choose to become a non-participating provider or opt out of participating in Medicare. It’s important to verify they accept Medicare assignment before receiving any services.
What Medicare coverage is right for my specific situation?
Do Doctors Who Accept Medicare Have to Accept Supplement Plans?
If your doctor accepts Medicare assignment and you have Original Medicare (Medicare Part A and Part B) with a Medicare Supplement (Medigap) plan, they will accept the supplemental insurance. Depending on your Medigap plan coverage , it may pay all or part of your out-of-pocket costs such as deductibles, copayments and coinsurance.
However, if you have a Medicare Advantage plan (Part C), you may have a network of covered doctors under the plan. If you visit an out-of-network doctor, you may need to pay all or part of the cost for your services.
Keep in mind that you can’t have a Medigap supplemental plan if you have a Medicare Advantage plan.
If you have questions or want to learn more about different Medicare plans like Original Medicare with Medigap versus Medicare Advantage, GoHealth has licensed insurance agents ready to help. They can shop your different options and offer impartial guidance where you need it.
Do Most Doctors Accept Medicare Advantage Plans?
Many doctors accept Medicare Advantage (Part C) plans, but these plans often use provider networks. These networks are groups of doctors and providers in an area that have agreed to treat an insurance company’s customers. If you have a Part C plan, you may be required to see in-network doctors with few exceptions. However, these types of plans are popular options for all-in-one coverage for your health needs. Plans must offer Part A and B coverage, plus a majority also include Part D , or prescription drug coverage. But whether a doctor accepts a Medicare Advantage plan may depend on where you live and the type of Medicare Advantage plan you have.
There are several types of Medicare Advantage plans including:
- Health Maintenance Organization (HMO): These plans have a network of covered providers, as well as a primary care physician to manage your care. If you visit a doctor outside your plan network, you may have to pay the full cost of your visit.
- Preferred Provider Organization (PPO): You’ll probably still have a primary care physician, but these are more flexible plans that allow you to go out of network in some cases. But you may have to pay more.
- Private Fee for Service (PFFS): You may be able to visit any doctor or provider with these plans, but your costs may be higher.
- Special Needs Plan (SNP): This type of plan is only for certain qualified individuals who either have a specific health condition ( C-SNP ) or who qualify for both Medicaid and Medicare insurance ( D-SNP ).
Still have questions? GoHealth has the answers you need.
What Are Medicare Assignment Codes?
Medicare assignment codes help Medicare pay for covered services. If your doctor or other provider accepts assignment and is a participating provider, they will file for reimbursement for services with a CMS-1500 form and the code will be “assigned.”
But non-participating providers can select “not assigned.” This means they are not accepting Medicare-assigned rates for a given service. They can charge up to 15% over the full Medicare rate for the service.
If you go to a doctor or provider who accepts assignment, you don’t need to file your own claim. Your doctor’s office will directly file with Medicare. Always check to make sure your doctor accepts assignment to avoid excess charges from your visit.
Health Insurance Claim Form . CMS.gov.
Lower costs with assignment . Medicare.gov.
How Many Physicians Have Opted-Out of the Medicare Program? KFF.org.
Joining a plan . Medicare.gov.
This website is operated by GoHealth, LLC., a licensed health insurance company. The website and its contents are for informational and educational purposes; helping people understand Medicare in a simple way. The purpose of this website is the solicitation of insurance. Contact will be made by a licensed insurance agent/producer or insurance company. Medicare Supplement insurance plans are not connected with or endorsed by the U.S. government or the federal Medicare program. Our mission is to help every American get better health insurance and save money. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
Let's see if you're missing out on Medicare savings.
We just need a few details.
Related Articles

What Is Medicare IRMAA?
What Is an IRMAA in Medicare?

How to Report Medicare Fraud
Medicare Fraud Examples & How to Report Abuse

How to Change Your Address with Medicare
Reporting a Change of Address to Medicare

Can I Get Medicare if I’ve Never Worked?
Can You Get Medicare if You've Never Worked?

Why Are Some Medicare Advantage Plans Free?
Why Are Some Medicare Advantage Plans Free? $0 Premium Plans Explained

What Is Medicare Assignment?

Am I Enrolled in Medicare?

When and How Do I Enroll?
When and How Do I Enroll in Medicare?

Medicare Frequently Asked Questions
Let’s see if you qualify for Medicare savings today!
- Individuals myGov is a simple and secure way to access online government services.
- PRODA Log in to access HPOS, Business Hub, Aged Care Provider Portal and a range of other government online services.
- Centrelink Business Online
- Child Support Business Online
Assignment of benefit
Signature requirements when a patient assigns their Medicare benefit to the servicing provider as full payment for health services.
on this page
Responsible person, patient unable to sign - sensitive issue, patient unable to sign - deceased, email agreement.
If a patient is unable to sign an assignment of benefit form , you can get a signature from any of the following:
- the patient’s parent
- the patient’s guardian
- another responsible person.
In the absence of a parent, guardian or responsible person, leave the ‘patient signature’ section blank.
Where the signature space is either left blank or another person signs on the patient’s behalf, the assignment of benefit form must include the following:
- the notation ‘Patient unable to sign’
- in the ‘Practitioner’s Use’ section, the reason why the patient was unable to sign. For example, use ‘unconscious’, ‘injured hand’ or ‘verbal consent obtained’.
For Medicare Easyclaim , consent from the patient, the patient’s parent, guardian or other responsible person is acceptable. Press the OK or YES button on the EFTPOS terminal.
‘Responsible person’ refers to an adult person accompanying the patient or in whose care the patient has been placed.
A responsible person can include someone who is any of the following:
- the parent or guardian
- holds power of attorney
- holds a guardianship order
- the next of kin.
This does not include the:
- health professional who rendered the service
- health professional’s staff
- hospital proprietor or staff
- aged care home proprietor or staff.
If you assess the reason a patient is unable to sign is of a highly sensitive nature, write in the ‘Practitioner’s Use’ section either:
- ‘due to medical condition’
- ‘due to sensitive condition’.
Only do this if revealing the reason would:
- mean an unacceptable breach of patient confidentiality
- unduly embarrass or distress the recipient of the patient’s copy of the assignment of benefit form.
This should not be routine practice. You can’t use ‘extenuating circumstances’ as a reason for no patient signature.
You and the patient must have entered into a bulk bill agreement at the time of service. This must include having the patient sign the assignment of benefit form.
If the patient has not signed the form, a signature from a responsible person is acceptable.
A responsible person can be either:
- the executor of the will
- an appointed administrator.
You must not write ‘patient deceased’ as a reason for not getting a signature on the assignment of benefit form.
Follow the steps in the table below when a patient assigns their right to a Medicare benefit to you by email.
For privacy reasons, don’t include the Medicare card number and provider number in the email.
This process complies with section 10 of the Electronic Transactions Act 1999 . This act outlines the steps to be taken for an electronic signature to be recognised.
It also meets the legal requirement of needing a patient signature to assign a Medicare benefit.
Example email
Dear Mr Jones (patient)
Details of the telehealth consultation to be claimed with Medicare:
Item number: 91822
Benefit amount: $78.05
Date and time of consultation: 01.07.2022 10:30 am
Patient name: Peter Jones
Health professional name: Jane Smith
If you (the patient) agree to the assignment of the Medicare benefit directly to the health professional (bulk bill), reply to this email including the following wording:
- ‘Yes, I agree to the assignment of the Medicare benefit directly to the health professional.’
- your (the patient’s) name or the name of parent or guardian (where a child is the patient and unable to sign).
Regards Dr Jane Smith
Privacy note: Your personal information is protected by law, including the Privacy Act 1988, and is collected by Services Australia for the assessment and administration of payments and services. This information is required to process your application or claim. Your information may be used by the agency, or given to other parties where you have agreed to that, or where it is required or authorised by law (including for the purpose of research or conducting investigations). You can get more information about the way in which the agency will manage your personal information, including our privacy policy .
Read more about Assignment of benefit and signature requirements for telehealth services .
This information was printed 10 April 2024 from https://www.servicesaustralia.gov.au/assignment-benefit-signature-requirements-and-exemptions . It may not include all of the relevant information on this topic. Please consider any relevant site notices at https://www.servicesaustralia.gov.au/site-notices when using this material.
Printed link references
- For Therapists
- Medical Billing Services
PECOS for dummies Part I: Reassigning Benefits
- by Rocky Fenton
Are you a confused or burnt-out provider? Well just be burnt-out, because we are about to give you a step-by-step guide to reassigning your benefits through PECOS! Reassigning benefits means you can start seeing Medicare patients under a new organization, and in return be reimbursed something less dismal than most of your commercial payors fee schedules. And if you are still confused – feel free to reach out to our team and we will be more than happy to assist you!
Note: you can find all this information on the Noridian website and on YouTube. I provided both links below.
Enrollment: PECOS Reassignment of Benefits through Individual Provider
Source: https://med.noridianmedicare.com/
Source Video: https://www.youtube.com/watch?v=GmwKposslao
- Log in to PECOS
- Select “My Associates”
- On the “My associates” page select “View Enrollments”
- Scroll to the “Existing Enrollments” section – Select “View/Manage Reassignments” – “Manage Reassignments”
- Select “Add a new reassignment”
- Answer if entity or individual receiving benefits is enrolled in Medicare (Yes typically)
- “Additional Changes” dialogue box should show – select “no” unless changing other information
- Select “Start Application”
- Navigate to “Reassignment” topic – Click “Begin Submission”
- “Filter Reassignment of Benefits” dialogue box should show – Select “Add Information”
- Select whether benefits will be reassigned to “Individual” or “Organization” – Select “Next Page”
- Effective Date of Information – ** cannot be more than 60 days in future from when application is received, or application will be returned
- Legal business name – should match exactly as it appears on IRS documentation
- Fill out remaining TIN and NPI information – Select “Next Page”
- Enter Medicare ID number, including all preceding numbers and letters. If it is a new organization, enter “Pending” and select next page
- “Reassignment Practice Location Choice” dialogue box should appear. Select what the primary (and secondary if necessary) practice location you intend the provider to practice. Enter the location address and continue
- Verify the information and select “Next Topic”. Or if adding multiple reassignments to multiple TINs – Select “Add information” at the top and repeat the previous steps
- “Contact Person” dialogue box should appear. Review and add any contacts. Select “Review Complete”
- Check the “Error/Warning” tab and review anything that needs attention. Click “Begin Submission” when complete
- Signature method – If provider is completing the application select “Electronic”. If someone is working on behalf of the provider – select “E-Sign” and instructions will be sent to the provider’s email that you enter on the following prompt. Select “Next Page”
- The following page will require documentation uploaded. “Authorization Statements” will be E-Signed by the provider. Once this has been completed – select Complete Submission
- Application status can be monitored from the My Enrollments Page
- If the application is returned for correction
- 30 days are allotted for the corrections to be made
- All signatures must be submitted for processing to begin on the application
- Upload the required documents as a PDF or TIFF
Enrollment: PECOS Reassignment of Provider through Organizations Enrollment
Source Video: https://www.youtube.com/watch?v=x-rIn0NQRWc
- Select “View Enrollments”
- Select “View/Manage” Reassignments at the bottom of the dialogue box
- Select “Manage Reassignments”
- Select “Add reassignment of benefits where someone is reassigning benefits to the group or organization”
- “Additional Changes” dialogue box should show – select “No, I only need to make Reassignment Updates” if you do not wish to make any other changes
- Select “Start Application” and navigate to the “Reassignment” topic
- “Filter Reassignment of Benefits dialogue box will show – select “Add Information”
- “Accept Reassignment” dialogue box should show – fill out the requested information for who will be accepting reassignment
- “Medicare Identification Numbers” dialogue box should show – enter Medicare Identification Number. If the organization has more than one ID – select “Add More” and fill out the remaining IDs
- “Practice Location Address…” dialogue box should show – select the Primary location where services are rendered. This section can also be left blank
- *Note – Multiple Reassignment additions can be made on one 855B enrollment, however it is recommended to limit this to 25 reassignments to be added or deleted to decrease processing time
- “Contact Person” dialogue box should show – select “add information” and complete the main contact’s information and click “Save”
- “Enrollment Submission” dialogue box should show – Review any warning / error checks if needed. Select “Begin Submission” on the “Error/Warning Check” tab
- A Signature method prompt will appear – If the provider is signing off, select “Electronic” and select “Next Page”
- If you are the provider and are E-Signing, review the terms and conditions at the bottom and check the “Yes” box. If you are not the provider, you can enter the providers email address and instructions will be sent to them for an E-signature.
- Select the “Complete Submission” button.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
HHS Finalizes Policies to Make Marketplace Coverage More Accessible and Expand Essential Health Benefits
Today, the Biden-Harris Administration, through the U.S. Department of Health and Human Services (HHS)’s Centers for Medicare & Medicaid Services (CMS), announced policies for the Affordable Care Act Marketplaces that make it easier for low-income people to enroll in coverage, provides states the ability to increase access to routine adult dental services, and sets network adequacy standards for the time and distance people travel for appointments with in-network providers. Finally, the rule will standardize certain operations across the Marketplaces to increase reliability and consistency for consumers. The 2025 Notice of Benefit and Payment Parameters final rule builds on the Administration’s previous work expanding access to quality, affordable health care and raising standards for Marketplace plans nationwide.
“More than 21 million Americans signed up for high-quality, affordable health care coverage through the ACA Marketplaces in 2024. We want to build on this success to make Marketplace plans even better,” said HHS Secretary Xavier Becerra. “This rule will allow coverage of routine dental benefits for the first time, expand requirements to ensure reliable access to health care providers, and ensure consumers with lower incomes can sign up for coverage when they need it.”
“Access to affordable, quality health care options remain a concern across the country and a top priority for CMS,” said CMS Administrator Chiquita Brooks-LaSure. “This rule includes groundbreaking ways to access health care services - such as addressing barriers for routine adult dental coverage for the first time and including considerations for how far people travel to see a health care provider. At CMS, we continue to explore ways to help Americans access high-quality coverage through the ACA Marketplaces.”
Increasing Access to Health Care Services Adult Dental Services
CMS has expanded access to dental benefits by finalizing measures to allow states the option to add routine adult dental services as an essential health benefit (EHB). For the first time, and starting on January 1, 2027, every state will be able to update their EHB-benchmark plans to include routine non-pediatric dental services, such as cleanings, diagnostic X-rays, and restorative services like fillings and root canals, through the EHB-benchmark application process beginning in 2025.
Network Adequacy
The final rule creates more consistent, nationwide standards on how far and how long a consumer must travel to see various types of providers in State Marketplaces and State-based Marketplaces on the Federal Platform (SBM-FPs). State Marketplaces and State-based Marketplaces must review a plan’s network information prior to certifying any plan as a qualified health plan (QHP), consistent with the reviews conducted by the Federally-facilitated Marketplaces (FFMs).
Making It Easier to Enroll in Coverage Special Enrollment Periods
The rule extends the special enrollment period (SEP) for consumers with household incomes at or below 150% of the FPL (for the 2025 plan year, $38,730 for a family of three) to enroll in coverage in any month rather than only during Open Enrollment. Previously, this SEP was only available when enhanced subsidies under the IRA were available.
The rule also aligns the dates of Open Enrollment periods across almost all Marketplaces to generally begin on November 1 and end no earlier than January 15, with the option to extend the Open Enrollment period beyond January 15.
Additionally, the rule aims to prevent coverage gaps for those transitioning between different Marketplaces or from other insurance coverage by allowing those selecting coverage during certain SEPs to receive coverage beginning the first day of the month after the QHP is selected, as opposed to coverage beginning at a later date if the consumer enrolls between the 15th and the end of the month.
Streamlining the Enrollment Process This rule includes multiple policies to standardize operations among the Federally-facilitated and State-based Marketplaces to ensure a more streamlined consumer experience, such as requiring Marketplaces to have live call center representatives available during call center hours of operation to assist consumers with QHP application submission and enrollment, generally holding Open Enrollment from November 1-January 15 (with the option for Marketplaces to extend Open Enrollment to a later date), and automatically re-enrolling people who are enrolled in a catastrophic plan for the next year, in order to prevent gaps in coverage.
For more information on the final rule, see the fact sheet at https://www.cms.gov/newsroom/fact-sheets/hhs-notice-benefit-and-payment-parameters-2025-final-rule
Click here to view the final rule: https://www.cms.gov/files/document/cms-9895-f-patient-protection-final.pdf
Sign Up for Email Updates
Receive the latest updates from the Secretary, Blogs, and News Releases
Subscribe to RSS
Receive latest updates

Related News Releases
Biden-harris administration finalizes rule expanding access to care and increasing protections for people with medicare advantage and medicare part d, hhs releases white paper focused on preventing drug shortages, cms finalizes payment updates for 2025 medicare advantage and medicare part d programs, media inquiries.
For general media inquiries, please contact [email protected] .

An official website of the United States government
Here’s how you know
The .gov means it’s official.
Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure.
The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Fact Sheets Contract Year 2025 Medicare Advantage and Part D Final Rule (CMS-4205-F)
- Medicare Part D
On April 4, 2024, the Centers for Medicare & Medicaid Services (CMS) issued a final rule that revises the Medicare Advantage Program, Medicare Prescription Drug Benefit Program (Medicare Part D), Medicare Cost Plan Program, Programs of All-Inclusive Care for the Elderly (PACE), and Health Information Technology Standards and Implementation Specifications. Additionally, this final rule addresses several key provisions that remain from the CY 2024 Medicare Advantage and Part D proposed rule, CMS-4201-P, published on December 14, 2022. Together, the changes in this final rule build on existing Biden-Harris Administration policies to strengthen protections and guardrails, promote healthy competition, and ensure Medicare Advantage and Part D plans best meet the needs of enrollees. In addition, these policies promote access to behavioral health care providers, promote equity in coverage, and improve supplemental benefits.
This fact sheet discusses the major provisions of the 2025 final rule which can be downloaded here: https://www.federalregister.gov/public-inspection/2024-07105/medicare-program-medicare-advantage-and-the-medicare-prescription-drug-benefit-program-for-contract
Enhancements to Medicare Advantage and Medicare Part D
New Guardrails for Plan Compensation to Agents and Brokers to Stop Anti-Competitive Steering
Many individuals with Medicare rely on agents and brokers to help navigate complex Medicare choices as they comparison shop for coverage options. The Medicare statute requires that CMS must establish guidelines to ensure that the use of compensation creates incentives for agents and brokers to enroll individuals in the Medicare Advantage or Part D plan intended to best meet the prospective enrollee’s health care needs. However, excessive compensation, and other bonus arrangements, offered by plans to agents and brokers can result in individuals being steered to some Medicare Advantage and Part D plans over others based on the agent or broker’s financial interests, rather than the prospective enrollee’s health care needs.
CMS is cracking down on that. Specifically, CMS is finalizing requirements that redefine “compensation” to set a clear, fixed amount that agents and brokers can be paid regardless of the plan the individual enrolls in, addressing loopholes that result in commissions above this amount that create anti-competitive and anti-consumer steering incentives. The provisions of this final rule, which are applicable beginning with the upcoming Annual Enrollment Period, ensure that agent and broker compensation reflect only the legitimate activities required of agents and brokers, by broadening the scope of the regulatory definition of “compensation,” so that it is inclusive of all activities associated with the sales to/enrollment of an individual into a Medicare Advantage or Part D plan. In response to feedback from stakeholders, CMS is increasing the final national agent/broker fixed compensation amount for initial enrollments into a Medicare Advantage or Part D plan by $100, which is an amount higher than what was proposed ($31). CMS believes this increase will provide agents and brokers with sufficient funds to serve individuals with Medicare. This increase will eliminate variability in payments and improve the predictability of compensation for agents and brokers. This increase will be added to agent and broker compensation payments for the Annual Election Period in Fall 2024 and applied to all enrollments effective in CY2025 and future contract years.
Additionally, the final rule generally prohibits contract terms between Medicare Advantage organizations/Part D sponsors and middleman Third Party Marketing Organizations (TPMOs), such as field marketing organizations, which may directly or indirectly create an incentive to inhibit an agent or broker’s ability to objectively assess and recommend the plan that is best suited to a potential enrollee’s needs. In the final rule, CMS provides several examples of contract terms that will be impermissible under this prohibition, including provisions offering volume-based bonuses for enrollment into certain plans.
These final policies advance the goals of President Biden’s historic Competition Council and Executive Order signed in July 2021 , by helping to ensure a robust and competitive Medicare Advantage marketplace.
Limiting the Distribution of Personal Beneficiary Data by Third-Party Marketing Organizations
Some TPMOs have been selling and reselling personal beneficiary data, which can undermine existing rules that prohibit cold calling people with Medicare and result in other aggressive marketing tactics for Medicare Advantage and Part D plans. Individuals may be unaware that by placing a call or clicking on a generic-looking web link, they are unwittingly agreeing and providing consent for their personal beneficiary data to be collected and sold to other entities for future marketing activities. To curtail this practice, in this final rule, CMS is codifying the requirement that personal beneficiary data collected by a TPMO for marketing or enrolling the individual into a Medicare Advantage or Part D plan may only be shared with another TPMO when prior express written consent is given by the individual. Further, the TPMO must obtain this written consent through a transparent, and prominently placed, disclosure from the individual to share the information and be contacted for marketing or enrollment purposes, separately for each TPMO that receives the data; i.e., one-to-one consent, which is generally consistent with Federal Trade Commission (FTC) and Federal Communications Commission (FCC) regulations.
Improving Access to Behavioral Health Care Providers
CMS is taking steps to improve access to behavioral health care services for Medicare Advantage plan enrollees by finalizing important updates to network adequacy standards, helping to achieve the goals outlined in the CMS Behavioral Health Strategy . The Consolidated Appropriations Act, 2023 established a new statutory Medicare benefit category for services furnished by marriage and family therapists (MFTs) and mental health counselors (MHCs). Through separate rulemaking in the Calendar Year 2024 Physician Fee Schedule final rule, CMS implemented these new statutory requirements for MHCs so that they can enroll in Medicare. Many MFTs and MHCs practice within outpatient behavioral health facilities, such as mental health centers, substance use treatment centers, and hospitals. To help ensure that people with a Medicare Advantage plan have access to behavioral health providers, including these newly enrolled providers, CMS is adding network adequacy evaluation standards for a new facility-specialty provider category, called “Outpatient Behavioral Health,” that will include a range of behavioral health providers under one category. Specialists in this new facility-specialty category include MFTs and MHCs, Opioid Treatment Program providers, Community Mental Health Centers, addiction medicine physicians, and other providers, like nurse practitioners (NPs), physician assistants (PAs), and Clinical Nurse Specialists (CNSs), who regularly furnish addiction medicine and behavioral health counseling or therapy services covered by Medicare. To address concerns from commenters that some NPs, PAs, and CNSs might lack the necessary skills, training, or expertise to effectively address the behavioral health needs of enrollees, we added specific criteria that MA organizations must use to determine when an NP, PA or CNS can be included in the Outpatient Behavioral Health category to meet the new network adequacy standards for Outpatient Behavioral Health. Specifically, Medicare Advantage plans must independently verify that the provider they are adding to their network has furnished or will furnish such services to at least 20 patients within a12-month period, using reliable information about services furnished by the provider, such as the Medicare Advantage plan’s claims data, prescription drug claims data, electronic health records or similar data in order to make this determination.
In addition, while evaluating an MA organization’s network, CMS is adding this Outpatient Behavioral Health facility specialty to the list of the specialty types that will receive a 10% credit toward meeting required time and distance standards. The Medicare Advantage organization’s contracted network of providers must include one or more telehealth providers of that specialty type who provide additional telehealth benefits for covered services.
Mid-Year Enrollee Notification of Available Supplemental Benefits
An increasing share of Medicare dollars is going toward Medicare Advantage plan rebates, roughly $337 billion over the last 10 years, and the 2023 Trustees Report estimated $67 billion in 2024 alone. Medicare Advantage plans can use these rebate dollars to advertise a wide array of supplemental benefits, including special supplemental benefits for chronically ill enrollees. In 2022, over 99% of Medicare Advantage plans offered at least one supplemental benefit. The median was 23 supplemental benefits, and the most frequently offered benefits were vision, hearing, fitness, and dental. Some of these benefits address unmet social determinants of health needs, such as food insecurity or inadequate access to transportation. However, at the same time, some plans have indicated that enrollee utilization of many supplemental benefits is low. To ensure the large federal investment of taxpayer dollars in supplemental benefits is actually making its way to enrollees and is not primarily used to market benefits that individuals rarely use, the final rule requires Medicare Advantage plans to engage in outreach efforts so that enrollees are aware of the supplemental benefits available to them. CMS is requiring Medicare Advantage plans to issue a “Mid-Year Enrollee Notification of Unused Supplemental Benefits” annually, between June 30 and July 31 of the plan year, that is personalized to each enrollee, and that includes a list of any supplemental benefits not accessed by the individual during the first six months of the year. In addition, the notification will include the scope of the benefit, cost-sharing, instructions on how to access the benefit, any network application information for each available benefit, and a customer service number to call if additional help is needed. These policies advance the goals of President Biden’s historic Competition Council and Executive Order signed in July 2021 by helping make consumers aware of their plan benefits, facilitating better decision-making and consumer choice in the Medicare Advantage marketplace.
New Standards for Supplemental Benefits for the Chronically Ill
The Bipartisan Budget Act of 2018 authorized Medicare Advantage plans to cover new special supplemental benefits for the chronically ill (SSBCI), which are benefits provided only to eligible chronically ill enrollees and that must have a reasonable expectation of improving or maintaining health or overall function of the enrollee. CMS is finalizing new requirements for Medicare Advantage plans to demonstrate, with support from research by the time they submit bids, that SSBCI items and services meet the legal threshold of having a reasonable expectation of improving the health or overall function of chronically ill enrollees. Medicare Advantage plans must establish and maintain bibliographies of relevant research studies or other data to demonstrate that an SSBCI meets these requirements. Additionally, CMS updated SSBCI marketing and communications requirements to prevent misleading marketing and communications related to these benefits that may make it appear that the benefits are available to everyone. These policies advance the goals of President Biden’s historic Competition Council and Executive Order signed in July 2021 by helping to ensure a robust and competitive Medicare Advantage marketplace made up of plan options with meaningful benefits.
Annual Health Equity Analysis of Utilization Management Policies and Procedures
Prior authorization policies and procedures may have a disproportionate impact on underserved populations and may delay or deny access to certain services. The final rule ensures that Medicare Advantage organizations analyze their utilization management (UM) policies and procedures from a health equity perspective. CMS is updating the composition of, and responsibilities for, the UM committee to require: 1) at least one member of the UM committee has expertise in health equity, 2) the UM committee conducts plan-level annual health equity analysis of prior authorization policies and procedures used by the Medicare Advantage plan, and 3) the results of the analysis be made publicly available on the plan’s website. The goal of the health equity analysis is to create additional transparency and identify disproportionate impacts of UM policies and procedures on enrollees who receive the Part D low-income subsidy, who are dually eligible, or who have a disability.
Enhance Enrollees’ Rights to Appeal a Medicare Advantage Plan’s Decision to Terminate Coverage for Non-Hospital Provider Services
Currently, enrollees in a Medicare Advantage plan do not have the same access to Quality Improvement Organization (QIO) review of a fast-track appeal as individuals in Traditional Medicare. CMS is revising regulations to (1) require the QIO, instead of the Medicare Advantage plan, to review untimely fast-track appeals of a Medicare Advantage plan’s decision to terminate services in a skilled nursing facility, comprehensive outpatient rehabilitation facility or by a home health agency; and (2) fully eliminate the provision requiring forfeiture of an enrollee’s right to appeal a termination of services from these providers when they leave the facility. These changes will bring Medicare Advantage plan regulations in line with the parallel reviews available to individuals Traditional Medicare and expand the rights of Medicare Advantage plan enrollees to access the fast-track appeals process.
Increasing the Percentage of Dually Eligible Managed Care Enrollees Who Receive Medicare and Medicaid Services From the Same Organization
Dually eligible individuals face a complex assortment of enrollment options. The rule will improve experiences and outcomes for dually eligible individuals by increasing the percentage of dually eligible Medicare Advantage enrollees who are in affiliated Medicaid managed care plans, as opposed to Medicare Advantage plans that differ from the enrollee’s Medicaid plan. To achieve this, the rule (a) revises the current Part D quarterly special enrollment period (SEP) for dually eligible, and other Part D low-income subsidy (LIS) enrolled individuals, to a once-per-month SEP to enroll in a standalone prescription drug plan and (b) creates a new integrated care SEP to allow dually eligible individuals to elect an integrated dual eligible special needs plan (D-SNP) when the individual also receives Medicaid services through an affiliated managed care plan. Further, this rule (c) limits enrollment in certain D–SNPs to those individuals who are also enrolled in an affiliated Medicaid managed care organization (MCO), and (d) limits the number of D–SNP plan benefit packages an MA organization, its parent organization, or entity that shares a parent organization with the MA organization, can offer in the same service area as an affiliated Medicaid MCO.
Increasing the percentage of dually eligible Medicare Advantage enrollees who are in plans that also cover Medicaid will expand access to integrated materials, unified appeal processes across Medicare and Medicaid, and continued Medicare services during an appeal for those individuals. By reducing the number of plans that can enroll dually eligible individuals outside of the annual election period, the rule will also reduce aggressive, confusing marketing tactics toward dually eligible individuals throughout the year. These policies advance the goals of President Biden’s historic Competition Council and Executive Order signed in July 2021 by promoting choice and facilitating improved access to an array of Medicare coverage options for individuals with low incomes.
For D-SNP PPOs, Limit Out-of-Network Cost Sharing
The rule limits out-of-network cost sharing for Medicare Advantage D-SNP preferred provider organizations (PPOs) for specific services beginning in 2026. The rule will reduce cost-shifting to Medicaid, increase payments to safety net providers, expand dually eligible enrollees’ access to providers, and protect dually eligible enrollees from unaffordable costs.
Contracting Standards for Dual Eligible Special Needs Plan Look-Alikes
The rule will lower the Medicare Advantage D-SNP look-alike threshold from 80% to 70% in 2025 and to 60% in 2026. This policy will help to address the continued proliferation of Medicare Advantage plans that are serving high percentages of dually eligible individuals without meeting the requirements to be a D-SNP and promoting full implementation of requirements for D-SNPs, including minimum integration standards as required under section 1859(f)(8)(D)(i) of the Act, as added by the Bipartisan Budget Act of 2018.
Standardize the Medicare Advantage Risk Adjustment Data Validation (RADV) Appeals Process
The final rule addresses operational constraints in existing Risk Adjustment Data Validation (RADV) appeal regulations. CMS is finalizing revisions to the appeals process whereby Medicare Advantage organizations will not request both a medical record review determination appeal and a payment error calculation appeal at the same time. Medicare Advantage organizations that request a medical record review determination appeal may only request a payment error calculation appeal after the completion of the medical record review determination administrative RADV appeal process. Additionally, the final rule clarifies that a revised audit report containing a recalculated payment error calculation will not be issued by the Secretary at each level of appeal, but instead will be issued when a medical record review determination appeal or a payment error calculation appeal is final, as applicable. Finally, the final rule includes a requirement that if the CMS Administrator does not decline to review or does not elect to review within 90 days of receipt of either the Medicare Advantage organization’s or CMS’ timely request for review (whichever is later), the hearing officer’s decision becomes final.
More Flexibility to More Quickly Substitute Lower Cost Biosimilar Biological Products for Their Reference Products
CMS is finalizing two changes to provide Part D sponsors with more flexibility to make midyear substitutions of biosimilars for their reference products on their formularies:
- All biosimilars may be substituted as formulary maintenance changes: Part D sponsors may treat formulary substitutions of all biosimilars for their reference products as “maintenance changes” that would not require explicit prior approval by CMS. This option has previously been available only for interchangeable biological products. Part D sponsors previously had to obtain explicit approval prior to substituting biosimilars other than interchangeable biological products, and these substitutions applied only to enrollees who began therapy after the effective date of the change — delaying enrollees’ access to cheaper options. Treating all biosimilar substitutions as maintenance changes means that midyear formulary substitutions of biosimilars for their reference products would apply to all enrollees (including those already taking the reference product prior to the effective date of the change) following a 30-day advance notice to affected enrollees.
- New interchangeable biological products may be immediately substituted: We are finalizing additional flexibility for interchangeable biological products not on the market at the time that Part D sponsors submit their initial formulary for CMS approval. Part D sponsors meeting certain requirements have the additional option to immediately substitute a new interchangeable biological product for a reference product and provide notice of the change to affected enrollees after making such change.
These changes provide Part D sponsors with mechanisms to give enrollees access to equally effective — but potentially more affordable — options sooner than under the current policy. Consistent with the work of the President’s Competition Council, these regulations continue the Biden-Harris Administration's commitment to promoting enhanced access to affordable biosimilar and generic products.
Medicare Part D Medication Therapy Management (MTM) Program
CMS is finalizing improved targeting criteria for the Medicare Part D MTM program that will help ensure more consistent, equitable, and expanded access to MTM services. Specifically, we are finalizing changes to the MTM eligibility criteria to: (1) add HIV/AIDS to the list of core chronic diseases, requiring plan sponsors to include all ten core chronic diseases identified by CMS in their targeting criteria; (2) require plan sponsors to include all Part D maintenance drugs and expressly state that Part D sponsors retain the flexibility to include all Part D drugs in their targeting criteria; and (3) revise the methodology for calculating the MTM cost threshold to be commensurate with the average annual cost of eight generic drugs (set at $1,623 for CY 2025). CMS is not finalizing the proposal to reduce the maximum number of drugs a plan sponsor may require for targeting enrollees taking multiple Part D drugs and is retaining the maximum number of drugs as eight drugs.
- Previous Newsroom article
- Next Newsroom article
CMS News and Media Group Catherine Howden, Director Media Inquiries Form 202-690-6145
The Federal Register
The daily journal of the united states government, request access.
Due to aggressive automated scraping of FederalRegister.gov and eCFR.gov, programmatic access to these sites is limited to access to our extensive developer APIs.
If you are human user receiving this message, we can add your IP address to a set of IPs that can access FederalRegister.gov & eCFR.gov; complete the CAPTCHA (bot test) below and click "Request Access". This process will be necessary for each IP address you wish to access the site from, requests are valid for approximately one quarter (three months) after which the process may need to be repeated.
An official website of the United States government.
If you want to request a wider IP range, first request access for your current IP, and then use the "Site Feedback" button found in the lower left-hand side to make the request.

IMAGES
VIDEO
COMMENTS
For Medicare beneficiaries, assignment of benefits means that the person receiving care agrees to allow a nonparticipating provider to bill Medicare directly (as opposed to having the person receiving care pay the bill up front and seek reimbursement from Medicare). Assignment of benefits is authorized by the person receiving care in Box 13 of ...
The Medicare assignment code is what shows proof that Medicare has agreed to represent you and cover your medical bills. This method allows for easy communication between health providers and Medicare when caring for your medical needs. Participating healthcare providers file for service reimbursement with a Medicare assignment of benefits form.
All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent. You can get some preventive services and screenings, such as mammograms and colonoscopies, without paying a deductible or coinsurance if the provider accepts assignment.
If your doctor, provider, or supplier doesn't accept assignment: You might have to pay the full amount at the time of service. They should submit a claim to Medicare for any Medicare-covered services they give you, and they can't charge you for submitting a claim. If they refuse to submit a Medicare claim, you can submit your own claim to ...
Nonassignment of Benefits. The second reimbursement method a physician/supplier has is choosing to not accept assignment of benefits. Under this method, a non-participating provider is the only provider that can file a claim as non-assigned. When the provider does not accept assignment, the Medicare payment will be made directly to the beneficiary.
Summary: Medicare Assignment is an agreement between healthcare providers and Medicare, where providers accept the Medicare-approved amount as full payment, preventing them from charging beneficiaries extra. This benefits Medicare beneficiaries by controlling their costs and ensuring they only pay deductibles and copayments.
The information in "Your Medicare Benefits" describes the Medicare Program at the time it was printed. Changes may occur after printing. Visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) to get the most current information. TTY users can call 1-877-486-2048. "Your Medicare Benefits" isn't a legal document.
1. Participating providers, or those who accept Medicare assignment. These providers have an agreement with Medicare to accept the Medicare-approved amount as full payment for their services. You don't have to pay anything other than a copay or coinsurance (depending on your plan) at the time of your visit.
Medicare assignment simply means that your provider has agreed to stick to a Medicare fee schedule when it comes to what they charge for tests and services. Medicare regularly updates fee schedules, setting specific limits for what it will cover for things like office visits and lab testing. ... Benefits may vary by carrier and location ...
Medicare assignment, or Medicare assignment of benefits, is the process in which a Medicare beneficiary authorizes Medicare to directly reimburse health care providers for services. To ensure all services are charged at Medicare-determined rates, recipients should verify whether their primary physicians fall under the accept assignment ...
Participating providers accept Medicare and always take assignment. Taking assignment means that the provider accepts Medicare's approved amount for health care services as full payment. These providers are required to submit a bill (file a claim) to Medicare for care you receive. Medicare will process the bill and pay your provider directly ...
Medicare assignment codes help Medicare pay for covered services. If your doctor or other provider accepts assignment and is a participating provider, they will file for reimbursement for services with a CMS-1500 form and the code will be "assigned.". But non-participating providers can select "not assigned.".
Non-assignment of Benefits. Non-assigned is the method of reimbursement a physician/supplier has when choosing to not accept assignment of benefits. Under this method, a non-participating provider is the only provider that can file a claim as non-assigned. When the provider does not accept assignment, the Medicare payment will be made directly ...
Section 6: Certification Statements and Signatures. The signatures in this section authorize the reassignment of benefits to an eligible individual or entity or the termination of a reassignment of benefits. Signature dates cannot be more than 120 days prior to the receipt date.
Medicare assignment of benefits is a way to identify providers who accept Medicare benefits and those who do not. These providers can be individual physicians, whole hospitals or various suppliers such as physical therapists who work independently.
Coordination of benefits (COB) allows plans that provide health and/or prescription coverage for a person with Medicare to determine their respective payment responsibilities (i.e., determine which insurance plan has the primary payment responsibility and the extent to which the other plans will contribute when an individual is covered by more than one plan).
terminate a reassignment of Medicare benefits after enrollment in the Medicare program or make a change in their reassignment of Medicare benefit information using either: • The Internet-based Provider Enrollment, Chain and Ownership System (PECOS), or • The paper CMS-855R application. Be sure you are using the most current version.
Participating physicians/practitioners and suppliers sign an agreement with Medicare to accept assignment of Medicare benefits for all Medicare patients. A claim for which a beneficiary elects to assign his/her benefits under a Medigap policy to a participating physician/practitioner and supplier is called a "mandated Medigap transfer."
This form is to be signed by the patient or other authorized person. MEDICARE ASSIGNMENT OF BENEFITS FROM (PDF) Other documentation required for prescribing CGM to Medicare patients: Certificate of Medical Necessity (serves as the prescription) Images of insurance card (s) (front/back) Chart notes reflecting coverage criteria. When prescribing ...
You must not write 'patient deceased' as a reason for not getting a signature on the assignment of benefit form. Email agreement. Follow the steps in the table below when a patient assigns their right to a Medicare benefit to you by email. For privacy reasons, don't include the Medicare card number and provider number in the email.
Reassigning benefits means you can start seeing Medicare patients under a new organization, and in return be reimbursed something less dismal than most of your commercial payors fee schedules. And if you are still confused - feel free to reach out to our team and we will be more than happy to assist you!
form title expedited review notice-notice of medicare provider non-coverage revision date 2008-02-29 ... (assignment) of appeal rights revision date 2018-03-01 ... form title application for hospital insurance benefits for individuals with end stage renal disease revision date 2023-02-28
The Centers for Medicare & Medicaid Services April 2 released its final rule for qualified health plans offered through the health insurance marketplaces for 2025. Beginning in plan year 2025, CMS will require plans participating in state-based marketplaces to comply with time and distance network adequacy standards that are at least as stringent as those for the federally facilitated marketplace.
In addition, the beneficiary does not need to assign benefits in any circumstance where assignment is mandatory. Thus, in most cases, a signed assignment of benefits is not needed. Resource. CMS Internet Only Manual, Publication 100-04, Medicare Claims Processing Manual, Chapter 1, Section 50.1.6
Today, the Biden-Harris Administration, through the U.S. Department of Health and Human Services (HHS)'s Centers for Medicare & Medicaid Services (CMS), announced policies for the Affordable Care Act Marketplaces that make it easier for low-income people to enroll in coverage, provides states the ability to increase access to routine adult dental services, and sets network adequacy standards ...
Mid-Year Enrollee Notification of Available Supplemental Benefits. An increasing share of Medicare dollars is going toward Medicare Advantage plan rebates, roughly $337 billion over the last 10 years, and the 2023 Trustees Report estimated $67 billion in 2024 alone. Medicare Advantage plans can use these rebate dollars to advertise a wide array ...
The contract labor allocation proportion for wages and salaries is equal to the Wages and Salaries cost weight as a percent of the sum of the Wages and Salaries cost weight and the Employee Benefits cost weight. Using the 2022 Medicare cost report data, this percentage is 85 percent (1 percentage point higher than the percentage in the 2018 ...