An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager

Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Twenty years of research on attention-deficit/hyperactivity disorder (ADHD): looking back, looking forward
Affiliations.
- 1 Academic Unit of Psychology, Center for Innovation in Mental Health, University of Southampton, Southampton, UK.
- 2 Clinical and Experimental Sciences (CNS and Psychiatry), Faculty of Medicine, University of Southampton, Southampton, UK.
- 3 Solent NHS Trust, Southampton, UK.
- 4 New York University Child Study Center, New York City, New York, USA.
- 5 Division of Psychiatry and Applied Psychology, School of Medicine, University of Nottingham, Nottingham, UK.
- 6 Departments of Paediatrics and Psychiatry, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Melbourne, Victoria, Australia.
- 7 Murdoch Children's Research Institute, Melbourne, Victoria, Australia.
- 8 Royal Children's Hospital, Melbourne, Victoria, Australia.
- PMID: 30301823
- PMCID: PMC10270437
- DOI: 10.1136/ebmental-2018-300050
In this clinical review we summarise what in our view have been some the most important advances in the past two decades, in terms of diagnostic definition, epidemiology, genetics and environmental causes, neuroimaging/cognition and treatment of attention-deficit/hyperactivity disorder (ADHD), including: (1) the most recent changes to the diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders and International Classification of Diseases; (2) meta-analytic evidence showing that, after accounting for diagnostic methods, the rates of ADHD are fairly consistent across Western countries; (3) the recent finding of the first genome-wide significant risk loci for ADHD; (4) the paradigm shift in the pathophysiological conceptualisation of ADHD from alterations in individual brain regions to a complex dysfunction in brain networks; (5) evidence supporting the short-term efficacy of ADHD pharmacological treatments, with a different profile of efficacy and tolerability in children/adolescents versus adults; (6) a series of meta-analyses showing that, while non-pharmacological treatment may not be effective to target ADHD core symptoms, some of them effectively address ADHD-related impairments (such as oppositional behaviours for parent training and working memory deficits for cognitive training). We also discuss key priorities for future research in each of these areas of investigation. Overall, while many research questions have been answered, many others need to be addressed. Strengthening multidisciplinary collaborations, relying on large data sets in the spirit of Open Science and supporting research in less advantaged countries will be key to face the challenges ahead.
© Author(s) (or their employer(s)) 2018. No commercial re-use. See rights and permissions. Published by BMJ.
PubMed Disclaimer
Conflict of interest statement
Competing interests: SC declares reimbursement for travel and accommodation expenses from the Association for Child and Adolescent Central Health (ACAMH) in relation to lectures delivered for ACAMH, and from Healthcare Convention for educational activity on ADHD. DC declares grants and personal fees from Shire and Servier; personal fees from Eli Lilly, Novartis and Oxford University Press; and grants from Vifor.
- Attention-deficit/hyperactive disorder: missing the bull's eye. Leon C, Sharma R, Kaur S. Leon C, et al. Evid Based Ment Health. 2019 Feb;22(1):e1. doi: 10.1136/ebmental-2018-300079. Epub 2019 Jan 21. Evid Based Ment Health. 2019. PMID: 30665988 Free PMC article. No abstract available.
Similar articles
- Guidance for identification and treatment of individuals with attention deficit/hyperactivity disorder and autism spectrum disorder based upon expert consensus. Young S, Hollingdale J, Absoud M, Bolton P, Branney P, Colley W, Craze E, Dave M, Deeley Q, Farrag E, Gudjonsson G, Hill P, Liang HL, Murphy C, Mackintosh P, Murin M, O'Regan F, Ougrin D, Rios P, Stover N, Taylor E, Woodhouse E. Young S, et al. BMC Med. 2020 May 25;18(1):146. doi: 10.1186/s12916-020-01585-y. BMC Med. 2020. PMID: 32448170 Free PMC article.
- Attention-deficit hyperactivity disorder. Posner J, Polanczyk GV, Sonuga-Barke E. Posner J, et al. Lancet. 2020 Feb 8;395(10222):450-462. doi: 10.1016/S0140-6736(19)33004-1. Epub 2020 Jan 23. Lancet. 2020. PMID: 31982036 Free PMC article. Review.
- Attention-deficit hyperactivity disorder (ADHD): an updated review of the essential facts. Tarver J, Daley D, Sayal K. Tarver J, et al. Child Care Health Dev. 2014 Nov;40(6):762-74. doi: 10.1111/cch.12139. Epub 2014 Apr 14. Child Care Health Dev. 2014. PMID: 24725022 Review.
- [Is emotional dysregulation a component of attention-deficit/hyperactivity disorder (ADHD)?]. Villemonteix T, Purper-Ouakil D, Romo L. Villemonteix T, et al. Encephale. 2015 Apr;41(2):108-14. doi: 10.1016/j.encep.2013.12.004. Epub 2014 Apr 1. Encephale. 2015. PMID: 24703785 French.
- Attention deficit/hyperactivity disorder: a focused overview for children's environmental health researchers. Aguiar A, Eubig PA, Schantz SL. Aguiar A, et al. Environ Health Perspect. 2010 Dec;118(12):1646-53. doi: 10.1289/ehp.1002326. Epub 2010 Sep 8. Environ Health Perspect. 2010. PMID: 20829148 Free PMC article. Review.
- The meaning of boredom : Properly managing childhood boredom could lead to more fulfilling lives. Uehara I, Ikegaya Y. Uehara I, et al. EMBO Rep. 2024 Jun;25(6):2515-2519. doi: 10.1038/s44319-024-00155-0. Epub 2024 May 13. EMBO Rep. 2024. PMID: 38741007 Free PMC article.
- Stimulant medications in children with ADHD normalize the structure of brain regions associated with attention and reward. Wu F, Zhang W, Ji W, Zhang Y, Jiang F, Li G, Hu Y, Wei X, Wang H, Wang SA, Manza P, Tomasi D, Volkow ND, Gao X, Wang GJ, Zhang Y. Wu F, et al. Neuropsychopharmacology. 2024 Jul;49(8):1330-1340. doi: 10.1038/s41386-024-01831-4. Epub 2024 Feb 26. Neuropsychopharmacology. 2024. PMID: 38409281
- Management Strategies for Borderline Personality Disorder and Bipolar Disorder Comorbidities in Adults with ADHD: A Narrative Review. MacDonald L, Sadek J. MacDonald L, et al. Brain Sci. 2023 Oct 26;13(11):1517. doi: 10.3390/brainsci13111517. Brain Sci. 2023. PMID: 38002478 Free PMC article. Review.
- Inflammation, Dopaminergic Brain and Bilirubin. Jayanti S, Dalla Verde C, Tiribelli C, Gazzin S. Jayanti S, et al. Int J Mol Sci. 2023 Jul 14;24(14):11478. doi: 10.3390/ijms241411478. Int J Mol Sci. 2023. PMID: 37511235 Free PMC article. Review.
- Attention deficit hyperactivity disorder is associated with (a)symmetric tonic neck primitive reflexes: a systematic review and meta-analysis. Wang M, Yu J, Kim HD, Cruz AB. Wang M, et al. Front Psychiatry. 2023 Jul 7;14:1175974. doi: 10.3389/fpsyt.2023.1175974. eCollection 2023. Front Psychiatry. 2023. PMID: 37484683 Free PMC article. Review.
- Polanczyk G, de Lima MS, Horta BL, et al. . The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 2007;164:942–8. 10.1176/ajp.2007.164.6.942 - DOI - PubMed
- Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med 2006;36:159–65. 10.1017/S003329170500471X - DOI - PubMed
- Sibley MH, Mitchell JT, Becker SP. Method of adult diagnosis influences estimated persistence of childhood ADHD: a systematic review of longitudinal studies. Lancet Psychiatry 2016;3:1157–65. 10.1016/S2215-0366(16)30190-0 - DOI - PubMed
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, DSM-5. Fifth edn. American Psychiatric Publishing, 2013.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fourth edn: American Psychiatric Publishing, 2000.
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Europe PubMed Central
- Ovid Technologies, Inc.
- PubMed Central
- Genetic Alliance
- MedlinePlus Health Information
Miscellaneous
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Search Menu
- Sign in through your institution
- Advance articles
- Virtual Issues
- Author Guidelines
- Open Access
- Self-Archiving Policy
- Why publish with this journal?
- About Journal of Pediatric Psychology
- About the Society of Pediatric Psychology
- Editorial Board
- Student Resources
- Advertising and Corporate Services
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Conceptual framework, evolving definitions of adhd, what are the academic and educational characteristics of children with adhd, are academic and educational problems transient or persistent, what are the academic characteristics of children with symptoms of adhd but without formal diagnoses, how do treatments affect academic and educational outcomes, how should we design future research to determine which treatments improve academic and educational outcomes of children with adhd.
- < Previous
Academic and Educational Outcomes of Children With ADHD
ADHD Special Issue, reprinted by permission from Ambulatory Pediatrics, Vol. 7, Number 2 (Supplement), Jan./Feb. 2007,
- Article contents
- Figures & tables
- Supplementary Data
Irene M. Loe, Heidi M. Feldman, Academic and Educational Outcomes of Children With ADHD, Journal of Pediatric Psychology , Volume 32, Issue 6, July 2007, Pages 643–654, https://doi.org/10.1093/jpepsy/jsl054
- Permissions Icon Permissions
Attention-deficit/hyperactivity disorder (ADHD) is associated with poor grades, poor reading and math standardized test scores, and increased grade retention. ADHD is also associated with increased use of school-based services, increased rates of detention and expulsion, and ultimately with relatively low rates of high school graduation and postsecondary education. Children in community samples who show symptoms of inattention, hyperactivity, and impulsivity with or without formal diagnoses of ADHD also show poor academic and educational outcomes. Pharmacologic treatment and behavior management are associated with reduction of the core symptoms of ADHD and increased academic productivity, but not with improved standardized test scores or ultimate educational attainment. Future research must use conceptually based outcome measures in prospective, longitudinal, and community-based studies to determine which pharmacologic, behavioral, and educational interventions can improve academic and educational outcomes of children with ADHD.
Problems in school are a key feature of attention-deficit/hyperactivity disorder (ADHD), often bringing the child with ADHD to clinical attention. It is important to establish the nature, severity, and persistence of these school difficulties in children with ADHD. It is also critical to learn how various treatments affect academic and educational outcomes. These findings inform clinical practice, public health, public education, and public policy. This review of academic and educational outcomes of ADHD is organized around 5 questions: (1) What are the academic and educational characteristics of children with ADHD? (2) Are academic and educational problems transient or persistent? (3) What are the academic characteristics of children with symptoms of ADHD but without formal diagnoses? (4) How do treatments affect academic and educational outcomes? (5) How should we design future research to determine which treatments improve academic and educational outcomes of children with ADHD?
We used the International Classification of Functioning, Disability, and Health (ICF) 1 as the conceptual framework for describing the functional problems associated with ADHD. The World Health Organization developed the ICF to provide a systematic and comprehensive framework and common language for describing and assessing functional implications of health conditions, regardless of the specific disease or disorder. Use of this model facilitates comparisons of health-related states across conditions, studies, interventions, populations, and countries.
In the underlying ICF conceptual framework, health conditions impact function at 3 mutually interacting levels of analysis ( Figure 1 ): body functions and structures, activities of daily living, and social participation. Problems of body functions and structures are called impairments , a more specific and narrow meaning for the term than that used in DSM-IV. 2 Problems of activities of daily living are called limitations . Problems of social participation are called restrictions. Environmental and personal factors can also affect functioning. Treatments may address the health condition directly, may be aimed at one or more domains within the levels of functioning, or may be designed to change the environment. Because of the bidirectional influences within and among these levels of analysis, treatments directed at one problem may indirectly improve problems at other levels.
Conceptual model of International Classification of Functioning, Disability, and Health.
Figure 2 applies the ICF model to school functioning in children with ADHD using the specific codes and terminology of the classification system. At the level of body functions, ADHD affects several global and specific mental functions: intellectual function; impulse control; sustaining and shifting attention; memory; control of psychomotor functions; emotion regulation; higher level cognition, including organization, time management, cognitive flexibility, insight, judgment, and problem solving; and sequencing complex movements. At the level of activities, ADHD may result in limitations in at least 2 domains relevant to this review (and other domains addressed by other chapters in this volume): (1) learning and applying knowledge, including reading, writing, and calculation; and (2) general tasks and demands, including completing single or multiple tasks, handling one's own behavior, and managing stress and frustration. Here, we will differentiate between academic underachievement , which will refer to problems in learning and applying knowledge, including earning poor grades and low standardized test scores, and academic performance , which includes completing classwork or homework. At the level of social participation, ADHD can compromise the major life area of education, including creating restrictions in moving in and across educational levels, succeeding in the educational program, and ultimately leaving school to work. Any one of these functional problems may have many contributors, including the health condition and functional problems at other levels of analysis. We will refer to the restrictions in participation as educational problems. Environmental factors relevant to outcomes in ADHD include general and special education services and policies.
Functional problems associated with attention-deficit/hyperactivity disorder using the International Classification of Functioning, Disability, and Health conceptual model.
The clinical criteria for ADHD have evolved over the last 25 years. Studies from the 1980s and 1990s often used different inclusion and exclusion criteria than were used in more recent studies. Some studies carefully differentiate between children with what we now label as ADHD-Combined subtype (ADHD-C) and attention deficit disorder or ADHD-predominantly Inattentive subtype (ADHD-I). We will address briefly the outcomes of the subtypes specifically. Many children with ADHD have comorbid conditions, including anxiety, depression, disruptive behavior disorders, tics, and learning problems. The contributions of these co-occurring problems to the functional outcomes of ADHD have not been well established. Therefore, in this review, we will consider the academic and educational outcomes of ADHD without subdividing the population on the basis of coexisting neurobehavioral problems in affected children.
Children with ADHD show significant academic underachievement, poor academic performance, and educational problems. 3–8 In terms of impairment of body functions, children with ADHD show significant decreases in estimated full-scale IQ compared with controls but score on average within the normal range. 9 In terms of activity limitations, children with ADHD score significantly lower on reading and arithmetic achievement tests than controls. 9 In terms of restrictions in social participation, children with ADHD show increases in repeated grades, use of remedial academic services, and placement in special education classes compared with controls. 9 Children with ADHD are more likely to be expelled, suspended, or repeat a grade compared with controls. 10
Children with ADHD are 4 to 5 times more likely to use special educational services than children without ADHD. 10, 11 Additionally, children with ADHD use more ancillary services, including tutoring, remedial pull-out classes, after-school programs, and special accommodations.
The literature reports conflicting data about whether the academic and educational characteristics of ADHD-I are substantially different from the characteristics of ADHD-C. 12, 13 Some studies have not found different outcomes in terms of academic attainment, use of special services, and rates of high school graduation. 14 However, a large survey of elementary school students found children with ADHD-I were more likely to be rated as below average or failing in school compared with the children with ADHD-C and ADHD–predominantly hyperactive-impulsive subtype. 15 A subset of children with ADHD-I are described as having a sluggish cognitive tempo, leading to the assumption that there is a higher prevalence of learning disorders in the ADHD-I than the ADHD-C populations. One study supporting this claim found more children with ADHD-I than children with ADHD-C in classrooms for children with learning disabilities. 16 Comparative long-term outcome studies of the subtypes in terms of academic and educational outcomes have not been conducted. 17
Longitudinal studies show that the academic underachievement and poor educational outcomes associated with ADHD are persistent. Academic difficulties for children with ADHD begin early in life. Symptoms are commonly reported in children aged 3 to 6 years, 18 and preschool children with ADHD or symptoms of ADHD are more likely to be behind in basic academic readiness skills. 19, 20
Several longitudinal studies follow school-age children with ADHD into adolescence and young adulthood. Initial symptoms of hyperactivity, distractibility, impulsivity, and aggression tend to decrease in severity over time but remain present and increased in comparison to controls. 21 In terms of activity limitations, subjects followed into adolescence fail more grades, achieve lower ratings on all school subjects on their report cards, have lower class rankings, and perform more poorly on standardized academic achievement tests than matched normal controls. 22–26 School histories indicate persistent problems in social participation, including more years to complete high school, lower rates of college attendance, and lower rates of college graduation for subjects than controls. 27–30
The subjects with ADHD in the longitudinal studies generally fall into 1 of 3 main groups as young adults: (1) approximately 25% eventually function comparably to matched normal controls; (2) the majority show continued functional impairment, limitations in learning and applying knowledge, and restricted social participation, particularly poor progress through school; and (3) less than 25% develop significant, severe problems, including psychiatric and/or antisocial disturbance. 31 It is unclear what factors determine the long-term outcomes. Persistent difficulties may be due to ADHD per se or may be due to a combination of ADHD and coexisting conditions, including learning, internalizing, and disruptive behavior disorders. The contribution of environmental factors to outcomes is also unclear.
Studies of outcome in children diagnosed with ADHD suffer from a potentially serious logical problem: circularity. 32 The clinical definition of ADHD in the DSM-IV requires the presence of functional impairment, typically defined in terms of behavior and performance at home and school. School problems are almost always present to make the diagnosis and therefore are more likely to be present at follow-up. Another problem in the use of clinic-referred samples is the selection bias in who gets referred to diagnostic clinics. One research strategy to complement the longitudinal studies of clinic-referred samples and avoid these problems is to evaluate children from community-based samples who demonstrate symptoms of ADHD but who have not necessarily been formally diagnosed with ADHD. In general, these studies find that children with symptoms of ADHD and without formal diagnoses also have adverse outcomes.
An early community-based study that charted the natural history of ADHD 33 followed subjects who were diagnosed and treated during childhood and children with symptoms and/or behavior indications who were never diagnosed or treated. Both groups were far more likely to attend special education schools and far less likely to graduate from high school or go to college than the asymptomatic controls. The magnitude of the difference was greater for the children with formal diagnosis than for those with pervasive symptoms.
Another community-based study on the relationship between symptoms of ADHD, scores on academic standardized tests, and grade retention found a linear relationship between the number of behavioral symptoms and academic achievement, even among children whose scores were generally below the clinical threshold for the diagnosis of ADHD. 34 Similar findings have been found in studies from Britain 35 and New Zealand. 36 Taken together, these findings suggest that the symptoms and associated features of ADHD are associated with adverse outcomes.
By using the ICF framework, treatments can be evaluated in terms of whether they improve body functions, including intelligence, sustained attention, memory, or executive functions; affect activities, including increasing learning and applying knowledge (such as raising standardized test scores or grades in reading, mathematics, or writing) and improving attending and completing tasks; or enhance participation, including moving across educational levels, succeeding in the educational program, and leaving school for work.
Medical Treatments
Psychopharmacological treatments, particularly with stimulant medications, reduce the core symptoms of ADHD 37 at the level of body functions. In addition, psychopharmacological treatments have been shown to improve children's abilities to handle general tasks and demands; for example, medication has been shown to improve academic productivity as indicated by improvements in the quality of note-taking, scores on quizzes and worksheets, the amount of written-language output, and homework completion. 38 However, stimulants are not associated with normalization of skills in the domain of learning and applying knowledge. 39 For example, stimulant medications have not generally been associated with improvements in reading abilities. 40, 41 In longitudinal studies, subjects demonstrated poor outcomes compared with controls whether or not they received medication. 24 , ,25 ,27 ,42–44 One caution in interpreting these findings is that it cannot be determined if outcomes would have been even worse without treatment because studies often lacked a true nontreatment group with ADHD. Another problem was attrition; subjects lost to follow-up may include those with worse outcomes. A third caution is that most children receive medication for only 2 to 3 years, 45 and it remains unclear whether steady treatment over many years would be associated with improved outcomes.
Behavior Management of ADHD
Behavioral interventions for ADHD, including behavioral parent training, behavioral classroom interventions, positive reinforcement and response cost contingencies, are effective in reducing core ADHD symptoms. 17 , ,30 ,46 However, in head-to-head comparisons behavior management techniques are less effective than psychostimulant medications 37 in reducing core symptoms. It has been shown that behavior management is equivalent or better than medication in improving aspects of functioning, such as parent-child interactions and reduction in oppositional-defiant behavior. However, the problem with this literature is that most behavior management intervention studies evaluate the impact on short-term behavior outcomes, not academic and educational outcomes. The impact of behavioral treatments on long-term academic and educational outcomes must be carefully studied.
Combined Management of ADHD
Given the chronic nature of ADHD and its impact on multiple domains of function, it is likely that multiple treatment approaches are needed. However, the impact of such combined treatments on long-term academic and educational outcomes has not been well studied. Combined treatment (medication and behavioral treatment) in the Multimodal Treatment Study of Children With ADHD was better than behavioral treatment and community care for reading achievement; however, the differences were small and of questionable clinical significance. 37 In addition, children with ADHD and co-occurring anxiety or environmental adversity derived benefit from the combination of medication and behavior management. 47, 48 We need studies to determine whether combined treatment has a larger impact on academic and educational outcomes in some subpopulations than others.
In terms of academic achievement and performance, a 2-year study comparing therapy with methylphenidate to therapy with methylphenidate plus multimodal psychosocial treatments found no advantage of combined treatment over medication alone on any academic measures. 49 The multimodal treatment included academic assistance, organizational skills training, individual psychotherapy, social skills training, and, if needed, reading remediation using phonics. In these studies, medication and/or behavior management, whether used alone or in combination, did not improve academic and educational outcomes of ADHD.
Educational Interventions and Services
The impact of remedial educational services on academic and educational outcomes is not known. Most available treatment outcome studies have not been conducted in general education classroom settings 50 and have focused on reducing problematic behavior rather than on improving scholastic status. 51 Even current rates of utilization are difficult to determine because ADHD itself is not an eligibility criterion for special education. 52 Although advocates pursued making ADHD a category of disability under the Individuals with Disabilities Education Act of 1990 (IDEA), this attempt was not successful. 53 Instead, the US Department of Education issued a policy memorandum 54 stating that students with ADHD were eligible for special education services under the Other Health Impairment category if problems of limited alertness negatively affected academic performance. Children with ADHD may qualify for special education services if they are eligible for another IDEA category, such as emotional disturbance or specific learning disability, but the children with ADHD are not disaggregated from students without ADHD in these categories. 55
Educational services are also provided to students with ADHD who do not meet IDEA eligibility requirements under Section 504 of the Vocational Rehabilitation Act of 1973 if the condition substantially limits a major life activity, such as learning. 53 Services include accommodations and related services in the general education setting, such as preferential seating, modified instructions, reduced classroom and homework assignments, and increased time or environmental modification for test taking. There is wide variability in the knowledge and application of Section 504 services among parents and educators. 53
For both special education and Section 504 services, the children most likely to obtain services are those with the most severe functional limitations. Therefore, it would be difficult to interpret associations among use of services and outcomes. There are no data regarding effectiveness of many commonly recommended accommodations, such as preferential seating, on outcomes.
The evidence that ADHD is associated with poor academic and education outcomes is overwhelming. However, studies thus far find that treatments are associated with relatively narrow improvements in core symptoms of inattention, hyperactivity, and impulsivity at the level of body functions and attending and completing tasks at the level of activities. We need prospective, controlled, and large-scale studies to investigate whether existing or new treatments will improve reading, writing, and mathematics skills; reduce grade retention; reduce expulsions and detentions; improve graduation rates; and increase completion of postsecondary education. In a literate, information-age society, these improved outcomes are vital to the economic and personal well-being of individuals with ADHD.
Because of the limitations of previous research, we recommend that future research incorporate several features. In terms of the subjects, the study must specify clear inclusion criteria, including diagnostic criteria for ADHD, subtypes, and coexisting conditions. Given the research history to date, we favor community- or school-based samples as opposed to clinic-referred samples to avoid selection bias. Studies should be conducted in general education as well as secondary school settings, given the lack of data from these settings. In terms of the outcome variables, we support use of standardized definitions of functional outcomes following the conceptualization of function provided by the ICF framework. We specifically favor repeated measures of academic achievement. Unfortunately, measures such as grades may vary across school systems. For this reason, the use of achievement tests may be preferable in large-scale studies. In addition, measures relevant to educational promotion, such as college entrance examinations, may provide more standardized information than graduation rates. In local or regional studies, other repeated measures may be possible, including analysis of portfolios. Another sensitive measure that could be collected on a continuous basis is curriculum-based measurement, 56 which involves probes of reading and math performance relative to the instructed curriculum and permits examination of relative trajectories over time as a measure of treatment outcome.
Designing convincing studies on the long-term impact of medication or behavior management on academic and educational outcomes is challenging because it is unethical to withhold standard treatments for long periods of time from an affected sample to create a control group. To circumvent this problem, we suggest large-scale studies that evaluate rates of change in the outcomes as a function of treatment strategy (or intensity) and that use statistical methods such as hierarchical linear modeling. 57 In this approach, individual students are nested in hierarchies that are defined by grade and diagnosis and also by treatment type and intensity. Repeated measures for outcomes, such as reading or math standard scores, are collected over time. The statistical methods estimate the effects of each factor—age and treatment intensity—on the rate of change. This method can demonstrate if the rate of change increases more rapidly in some groups than other groups and more rapidly than would have been predicted on the basis of status at study entry. The hierarchical linear modeling method is also helpful with differentiating rates of progress among children who adhere to treatment recommendations over long periods of time versus those who discontinue treatment after a few months or years.
We also recommend that the research strategy incorporate a 2-tiered approach. First, improvements in instruction/teaching methods, curriculum design, school physical designs, and environmental modifications should be offered to all students. We can call this phase improved universal design. Schools often try to change the child with ADHD to fit the school environment. Attempts to “normalize” behavior include pulling a child out of the classroom, perhaps applying a remedial strategy, and then putting the child back into the original setting, with the hope that the child will now be successful. 58 This strategy identifies the child as the problem, serves to isolate and potentially stigmatize the child, and precludes the exploration of environment-based solutions. 59 The advantage of universal design is that most children with ADHD are educated in general education settings. Improved universal design in the classroom could potentially benefit all children in the classroom, particularly those with ADHD. Such interventions may not decrease the differences between children with ADHD and their peers without ADHD on some measures, such as standardized test scores. However, more important is whether the children with ADHD reach a higher threshold of achievement, such as improved reading scores or higher rates of high school graduation.
The second tier for research is specific interventions for children with ADHD, layered on top of the basic reforms. These interventions can include teaching methods, new curricula, specific behavior management, and school-based intervention approaches. 60
We will focus on 6 different options that warrant further investigation in this 2-tiered research design: (1) small class size; (2) reducing distractions; (3) specific academic intervention strategies; (4) increased physical activity; (5) alternative methods of discipline; and (6) systems change.
Small Class Size
A study based in London schools of regular education students found that variations in average class size in the 25- to 35-student range are of little consequence in affecting student progress, probably because of a lack of opportunity for differences in classroom management techniques. 61 However, small classes of approximately 8 to 15 students have been beneficial for younger children and children with special needs. 62 Because children with ADHD are reported to do better with one-on-one instruction, smaller class size makes intuitive sense. Teachers perceive class size to be one of the major barriers to inclusion of ADHD students in regular education. 63 Empiric investigation on reduced class size is therefore warranted for all children, and also for children with ADHD. Small class sizes will probably result in use of innovative educational approaches that are precluded in the current system.
Reducing Distractions
Classrooms are often noisy and distracting environments. Children perform more poorly in noisy situations than do adults, and researchers have reported that the ability to listen in noise is not completely developed until adolescence or adulthood. 64–66 If an acoustic environment can be provided that allows +15 dB signal-to-noise ratio throughout the entire classroom, then all participants can hear well enough to receive the spoken message fully. 64 Accommodations in Section 504 plans often include repeating instructions and providing quiet test-taking areas that are free of distractions. Repetition of instructions alone is not likely to increase the attention of children with ADHD. Thus, methods for reducing noise and other distractions should be studied.
Specific Academic Intervention Strategies
As reviewed by Hoffman and DuPaul, 51 the so-called antecedent-oriented management strategies are good universal design features that hold promise for improving outcomes for children with ADHD. Antecedent interventions include choice making, peer tutoring, and computer-aided instruction, all reviewed below. Such strategies are proactive, support appropriate adaptive behavior, and prevent unwanted, challenging behaviors. These strategies make tasks more stimulating and provide students with opportunities to make choices related to academic work. 67 They may be particularly helpful for children with ADHD who demonstrate avoidance and escape behaviors.
Choice-making strategies allow students to select work from a teacher-developed menu. In a study of choice making with children with emotional and behavioral difficulties in a special education classroom, students demonstrated increased academic engagement and decreased behavior problems. 68 Another study demonstrated decreased disruptive behavior in a general education setting, 69 although more variable academic and behavioral performance occurred in a study of 4 students with ADHD in a general education setting. 51 A related concept is project-based learning, which capitalizes on student interests and provides a dynamic, interactive way to learn.
Studies of Class Wide Peer Tutoring, a widely used form of peer tutoring, have demonstrated enhanced task-related attention and academic accuracy in elementary school students with ADHD, 70, 71 as well as positive changes in behavior and academic performance in students without ADHD. 72 Teachers perceive time requirements of specialized interventions as a significant barrier to the inclusion of ADHD students. 63 Peer tutoring reduces the demands on teachers to provide one-on-one instruction. At the same time, it gives students with ADHD the opportunity to practice and refine academic skills, as well as to enhance peer social interactions, promoting self-esteem. Peer tutoring may be particularly effective when students are using disruptive behavior to gain peer attention. 51
Computer-aided instruction has intuitive appeal as a universal design feature and for children with ADHD because of its interactive format, use of multiple sensory modalities, and ability to provide specific instructional objectives and immediate feedback. Computer-aided instruction has not been well studied in children with ADHD. 51, 73 Studies with small numbers of subjects showed promising initial results 74, 75 but did not examine the effects on academic achievement. A small study of 3 children with ADHD that used a game-format math program found increases in academic achievement and increased task engagement. 76
Increased Physical Activity
Given that fidgeting and out-of-seat behavior are common in children with ADHD, increased use of recess and physical exercise might reduce overactivity. A study on the effects of a traditional recess on the subsequent classroom behavior of children with ADHD showed that levels of inappropriate behavior were consistently higher on days when participants did not have recess, compared with days when they did have recess. 77 A meta-analysis of studies on the effects of regular, noncontingent exercise showed reductions in disruptive behavior with greater effects in participants with hyperactivity. 78 Increased physical exercise would be beneficial for long-term health and for behavioral regulation in both children developing typically and children with ADHD.
Alternative Methods of Discipline
Many students receive suspensions or are sent to the principal's office for disruptive behavior. For those children who are avoiding work, these approaches are equivalent to positive reinforcement. Such avoidant or escape behavior could be countered with in-school as opposed to out-of-school suspensions. The use of interventions that teach children how to replace disruptive behaviors with appropriate behaviors is less punitive than suspensions and more effective in promoting academic productivity and success. 17
Systems Change
Classroom changes are unlikely to create adequate improvements without concomitant changes in the educational system. Three potential areas under the category of systems change are improved education of teachers and educational administrators; enhanced collaborations among family members, school professionals, and health care professionals; and improved tracking of child outcomes. Teacher surveys demonstrate that teachers perceive the need for more training about ADHD. 63 The optimal management of children with ADHD requires close collaboration of their parents, teachers, and health care providers. Currently there is no organized system to support this collaboration.
At the policy level, we need mechanisms to track the outcome of children with ADHD in relation to educational reform and utilization of special services. Federally supported surveys could focus on services and treatments for mental health conditions, including ADHD, and their impact on outcomes. Relevant data for the relationship of interventions and outcomes may also exist at the local and state level. Building on existing local and state databases to include health and mental health statistics could provide valuable information on this issue.
We remain ill informed about how to improve academic and educational outcomes of children with ADHD, despite decades of research on diagnosis, prevalence, and short-term treatment effects. We urge research on this important topic. It may be impossible to conduct long-term randomized, controlled trials with medication or behavior management used as treatment modalities for practical and ethical reasons. However, large-scale studies that use modern statistical methods, such as hierarchical linear modeling, hold promise for teasing apart the impact of various treatments on outcomes. Such methods can take into account the number and types of interventions, duration of treatment, intensity of treatment, and adherence to protocols. Educational interventions for children with ADHD must be studied. We recommend large-scale, prospective studies to evaluate the impact of educational interventions. These studies should be tiered, introducing universal design improvements and specific interventions for ADHD. They must include multiple outcomes, with emphasis on academic skills, high school graduation, and successful completion of postsecondary education. Such studies will be neither cheap nor easy. A broad-based coalition of parents, educators, and health care providers must work together to advocate for an ambitious research agenda and then design, implement, and interpret the resulting research. Changes in local, state, and federal policies might facilitate these efforts by creating meaningful databases and collaborations.
Google Scholar
Google Preview
Author notes
| Month: | Total Views: |
|---|---|
| January 2017 | 86 |
| February 2017 | 497 |
| March 2017 | 953 |
| April 2017 | 699 |
| May 2017 | 908 |
| June 2017 | 398 |
| July 2017 | 320 |
| August 2017 | 486 |
| September 2017 | 853 |
| October 2017 | 1,185 |
| November 2017 | 1,555 |
| December 2017 | 7,259 |
| January 2018 | 7,071 |
| February 2018 | 7,647 |
| March 2018 | 9,722 |
| April 2018 | 11,538 |
| May 2018 | 11,623 |
| June 2018 | 9,227 |
| July 2018 | 9,231 |
| August 2018 | 9,640 |
| September 2018 | 9,861 |
| October 2018 | 10,292 |
| November 2018 | 12,081 |
| December 2018 | 10,112 |
| January 2019 | 8,693 |
| February 2019 | 9,796 |
| March 2019 | 11,377 |
| April 2019 | 11,802 |
| May 2019 | 10,238 |
| June 2019 | 9,489 |
| July 2019 | 10,306 |
| August 2019 | 9,639 |
| September 2019 | 8,407 |
| October 2019 | 5,118 |
| November 2019 | 4,340 |
| December 2019 | 3,297 |
| January 2020 | 3,230 |
| February 2020 | 3,306 |
| March 2020 | 3,051 |
| April 2020 | 4,211 |
| May 2020 | 2,244 |
| June 2020 | 2,715 |
| July 2020 | 2,452 |
| August 2020 | 2,155 |
| September 2020 | 2,710 |
| October 2020 | 4,188 |
| November 2020 | 4,178 |
| December 2020 | 3,533 |
| January 2021 | 2,815 |
| February 2021 | 3,538 |
| March 2021 | 4,706 |
| April 2021 | 4,990 |
| May 2021 | 3,827 |
| June 2021 | 2,143 |
| July 2021 | 1,856 |
| August 2021 | 1,964 |
| September 2021 | 2,667 |
| October 2021 | 4,113 |
| November 2021 | 4,304 |
| December 2021 | 3,076 |
| January 2022 | 2,565 |
| February 2022 | 3,070 |
| March 2022 | 4,239 |
| April 2022 | 4,198 |
| May 2022 | 3,807 |
| June 2022 | 2,379 |
| July 2022 | 2,045 |
| August 2022 | 2,037 |
| September 2022 | 2,990 |
| October 2022 | 3,962 |
| November 2022 | 4,435 |
| December 2022 | 3,102 |
| January 2023 | 3,038 |
| February 2023 | 3,088 |
| March 2023 | 4,001 |
| April 2023 | 4,006 |
| May 2023 | 3,401 |
| June 2023 | 2,123 |
| July 2023 | 1,902 |
| August 2023 | 2,095 |
| September 2023 | 2,630 |
| October 2023 | 3,442 |
| November 2023 | 3,321 |
| December 2023 | 2,441 |
| January 2024 | 2,649 |
| February 2024 | 2,902 |
| March 2024 | 3,348 |
| April 2024 | 3,142 |
| May 2024 | 2,911 |
| June 2024 | 2,213 |
| July 2024 | 160 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1465-735X
- Print ISSN 0146-8693
- Copyright © 2024 Society of Pediatric Psychology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Understanding and Supporting Attention Deficit Hyperactivity Disorder (ADHD) in the Primary School Classroom: Perspectives of Children with ADHD and their Teachers
- Original Paper
- Open access
- Published: 01 July 2022
- Volume 53 , pages 3406–3421, ( 2023 )
Cite this article
You have full access to this open access article

- Emily McDougal ORCID: orcid.org/0000-0001-7684-7417 1 , 3 ,
- Claire Tai 1 ,
- Tracy M. Stewart ORCID: orcid.org/0000-0002-8807-1174 2 ,
- Josephine N. Booth ORCID: orcid.org/0000-0002-2867-9719 2 &
- Sinéad M. Rhodes ORCID: orcid.org/0000-0002-8662-1742 1
41k Accesses
16 Altmetric
Explore all metrics
Children with Attention Deficit Hyperactivity Disorder (ADHD) are more at risk for academic underachievement compared to their typically developing peers. Understanding their greatest strengths and challenges at school, and how these can be supported, is vital in order to develop focused classroom interventions. Ten primary school pupils with ADHD (aged 6–11 years) and their teachers (N = 6) took part in semi-structured interviews that focused on (1) ADHD knowledge, (2) the child’s strengths and challenges at school, and (3) strategies in place to support challenges. Thematic analysis was used to analyse the interview transcripts and three key themes were identified; classroom-general versus individual-specific strategies, heterogeneity of strategies, and the role of peers. Implications relating to educational practice and future research are discussed.
Similar content being viewed by others

An overview on neurobiology and therapeutics of attention-deficit/hyperactivity disorder

Evidence-Based Practices for Children, Youth, and Young Adults with Autism: Third Generation Review

The positive aspects of attention deficit hyperactivity disorder: a qualitative investigation of successful adults with ADHD
Avoid common mistakes on your manuscript.
Characterised by persistent inattention, hyperactivity and impulsivity (APA, 2013), ADHD is a neurodevelopmental disorder thought to affect around 5% of children (Russell et al., 2014 ) although prevalence estimates vary (Sayal et al., 2018 ). Although these core symptoms are central to the ADHD diagnosis, those with ADHD also tend to differ from typically developing children with regards to cognition and social functioning (Coghill et al., 2014 ; Rhodes et al., 2012 ), which can negatively impact a range of life outcomes such as educational attainment and employment (Classi et al., 2012 ; Kuriyan et al., 2013 ). Indeed, academic outcomes for children with ADHD are often poor, particularly when compared with their typically developing peers (Arnold et al., 2020 ) but also compared to children with other neurodevelopmental disorders, such as autism (Mayes et al., 2020 ). Furthermore, children with ADHD can be viewed negatively by their peers. For example, Law et al. ( 2007 ) asked 11–12-year-olds to read vignettes describing the behaviour of a child with ADHD symptoms, and then use an adjective checklist to endorse those adjectives that they felt best described the target child. The four most frequently ascribed adjectives were all negative (i.e. ‘careless’, ‘lonely’, ‘crazy’, and ‘stupid’). These negative perceptions can have a significant impact on the wellbeing of individuals with ADHD, including self-stigmatisation (Mueller et al., 2012 ). There is evidence that teachers with increased knowledge of ADHD report more positive attitudes towards children with ADHD compared to those with poor knowledge (Ohan et al., 2008 ) and thus research that identifies the characteristics of gaps in knowledge is likely to be important in addressing stigma.
Previous research of teachers' ADHD knowledge is mixed, with the findings of some studies indicating that teachers have good knowledge of ADHD (Mohr-Jensen et al., 2019 ; Ohan et al., 2008 ) and others suggesting that their knowledge is limited (Latouche & Gascoigne, 2019 ; Perold et al., 2010 ). Ohan et al. ( 2008 ) surveyed 140 primary school teachers in Australia who reported having experience of teaching at least one child with ADHD. Teachers completed the ADHD Knowledge Scale which consisted of 20 statements requiring a response of either true or false (e.g. “A girl/boy can be appropriately labelled as ADHD and not necessarily be over-active ”). They found that, on average, teachers answered 76.34% of items correctly, although depth of knowledge varied across the sample. Almost a third of the sample (29%) had low knowledge of ADHD (scoring less than 69%), with just under half of teachers (47%) scoring in the average range (scores of 70–80%). Only a quarter (23%) had “high knowledge” (scores above 80%) suggesting that knowledge varied considerably. Furthermore, Perold et al. ( 2010 ) asked 552 teachers in South Africa to complete the Knowledge of Attention Deficit Disorders Scale (KADDS) and found that on average, teachers answered only 42.6% questions about ADHD correctly. Responses of “don’t know” (35.4%) and incorrect responses (22%) were also recorded, indicating gaps in knowledge as well as a high proportion of misconceptions. Similar ADHD knowledge scores were reported in Latouche and Gascoigne’s ( 2019 ) study, who found that teachers enrolled into their ADHD training workshop in Australia had baseline KADDS scores of below 50% accuracy (increased to above 80% accuracy after training).
The differences in ADHD knowledge reported between Ohan et al. ( 2008 ) and the more recent studies could be due to the measures used. Importantly, when completing the KADDS, respondents can select a “don’t know” option (which receives a score of 0), whereas the ADHD Knowledge Scale requires participants to choose either true or false for each statement. The KADDS is longer, with a total of 39 items, compared to the 20-item ADHD Knowledge Scale, offering a more in-depth knowledge assessment. The heterogeneity of measures used within the described body of research is also highlighted within Mohr-Jensen et al. ( 2019 ) systematic review; the most frequently used measure (the KADDS) was only used by 4 out of the 33 reviewed studies, showing little consensus on the best way to measure ADHD knowledge. Despite these differences in measurement, the findings from most studies indicate that teacher ADHD knowledge is lacking.
Qualitative methods can provide rich data, facilitating a deeper understanding of phenomena that quantitative methods alone cannot reveal. Despite this, there are very few examples in the literature of qualitative methods being used to understand teacher knowledge of ADHD. In one example, Lawrence et al. ( 2017 ) interviewed fourteen teachers in the United States about their experiences of working with pupils with ADHD, beginning with their knowledge of ADHD. They found that teachers tended to focus on the external symptoms of ADHD, expressing knowledge of both inattentive and hyperactive symptoms. Although this provided key initial insights into the nature of teachers’ ADHD knowledge, only a small section of the interview schedule (one out of eight questions/topics) directly focused on ADHD knowledge. Furthermore, none of the questions asked directly about strengths, with answers focusing on difficulties. It is therefore difficult to determine from this study whether teachers are aware of strengths and difficulties outside of the triad of symptoms. A deeper investigation is necessary to fully understand what teachers know, and to identify areas for targeted psychoeducation.
Importantly, improved ADHD knowledge may impact positively on the implementation of appropriate support for children with ADHD in school. For example, Ohan et al. ( 2008 ) found that teachers with high or average ADHD knowledge were more likely to perceive a benefit of educational support services than those with low knowledge, and teachers with high ADHD knowledge were also more likely to endorse a need for, and seek out, those services compared to those with low knowledge. Furthermore, improving knowledge through psychoeducation may be important for improving fidelity to interventions in ADHD (Dahl et al., 2020 ; Nussey et al., 2013 ). Indeed, clinical guidelines recommend inclusion of psychoeducation in the treatment plan for children with ADHD and their families (NICE, 2018 ). Furthermore, Jones and Chronis-Tuscano ( 2008 ) found that educational ADHD training increased special education teachers’ use of behaviour management strategies in the classroom. Together, these findings suggest that understanding of ADHD may improve teachers’ selection and utilisation of appropriate strategies.
Child and teacher insight into strategy use in the classroom on a practical, day-to-day level may provide an opportunity to better understand how different strategies might benefit children, as well as the potential barriers or facilitators to implementing these in the classroom. Previous research with teachers has shown that aspects of the physical classroom can facilitate the implementation of effective strategies for autistic children, for example to support planning with the use of visual timetables (McDougal et al., 2020 ). Despite this, little research has considered the strategies that children with ADHD and their teachers are using in the classroom to support their difficulties and improve learning outcomes. Moore et al. ( 2017 ) conducted focus groups with UK-based educators (N = 39) at both primary and secondary education levels, to explore their experiences of responding to ADHD in the classroom, as well as the barriers and facilitators to supporting children. They found that educators mostly reflected on general inclusive strategies in the classroom that rarely targeted ADHD symptoms or difficulties specifically, despite the large number of strategies designed to support ADHD that are reported elsewhere in the literature (DuPaul et al., 2012 ; Richardson et al., 2015 ). Further to this, when interviewing teachers about their experiences of teaching pupils with ADHD, Lawrence et al. ( 2017 ) specifically asked about interventions or strategies used in the classroom with children with ADHD. The reported strategies were almost exclusively behaviourally based, for example, allowing children to fidget or move around the classroom, utilising rewards, using redirection techniques, or reducing distraction. This lack of focus on cognitive strategies is surprising, given the breadth of literature focusing on the cognitive difficulties in ADHD (e.g. Coghill, et al., 2014 ; Gathercole et al., 2018 ; Rhodes et al., 2012 ). Furthermore, to our knowledge research examining strategy use from the perspective of children with ADHD themselves, or strengths associated with ADHD, is yet to be conducted.
Knowledge and understanding of ADHD in children with ADHD has attracted less investigation than that of teachers. In a Canadian sample of 8- to 12-year-olds with ADHD (N = 29), Climie and Henley ( 2018 ) found that ADHD knowledge was highly varied between children; scores on the Children ADHD Knowledge and Opinions Scale ranged from 5 to 92% correct (M = 66.53%, SD = 18.96). The authors highlighted some possible knowledge gaps, such as hyperactivity not being a symptom for all people with ADHD, or the potential impact upon social relationships, however the authors did not measure participant’s ADHD symptoms, which could influence how children perceive ADHD. Indeed, Wiener et al ( 2012 ) has shown that children with ADHD may underestimate their symptoms. If this is the case, it would also be beneficial to investigate their understanding of their own strengths and difficulties, as well as of ADHD more broadly. Furthermore, if children do have a poor understanding of ADHD, they may benefit from psychoeducational interventions. Indeed, in their systematic review Dahl et al. ( 2020 ) found two studies in which the impact of psychoeducation upon children’s ADHD knowledge was examined, both of which reported an increase in knowledge as a consequence of the intervention. Understanding the strengths and difficulties of the child, from the perspective of the child and their teacher, will also allow the design of interventions that are individualised, an important feature for school-based programmes (Richardson et al., 2015 ). Given the above, understanding whether children have knowledge of their ADHD and are aware of strategies to support them would be invaluable.
Teacher and child knowledge of ADHD and strategies to support these children is important for positive developmental outcomes, however there is limited research evidence beyond quantitative data. Insights from children and teachers themselves is particularly lacking and the insights which are available do not always extend to understanding strengths which is an important consideration, particularly with regards to implications for pupil self-esteem and motivation. The current study therefore provides a vital examination of the perspectives of both strengths and weaknesses from a heterogeneous group of children with ADHD and their teachers. Our sample reflects the diversity encountered in typical mainstream classrooms in the UK and the matched pupil-teacher perspectives enriches current understandings in the literature. Specifically, we aimed to explore (1) child and teacher knowledge of ADHD, and (2) strategy use within the primary school classroom to support children with ADHD. This novel approach, from the dual perspective of children and teachers, will enable us to identify potential knowledge gaps, areas of strength, and insights on the use of strategies to support their difficulties.
Participants
Ten primary school children (3 female) aged 7 to 11 years (M = 8.7, SD = 1.34) referred to Child and Adolescent Mental Health Services (CAMHS) within the NHS for an ADHD diagnosis were recruited to the study. All participant characteristics are presented in Table 1 . All children were part of the Edinburgh Attainment and Cognition Cohort and had consented to be contacted for future research. Children who were under assessment for ADHD or who had received an ADHD diagnosis were eligible to take part. Contact was established with the parent of 13 potential participants. Two had undergone the ADHD assessment process with an outcome of no ADHD diagnosis and were therefore not eligible to take part, and one could not take part within the timeframe of the study. The study was approved by an NHS Research Ethics Committee and parents provided informed consent prior to their child taking part. Co-occurrences data for all participants was collected as part of a previous study and are reported here for added context. All of the children scored above the cut-off (T-score > 70) for ADHD on the Conners 3 rd Edition Parent diagnostic questionnaire (Conners, 2008 ). The maximum possible score for this measure is 90. At the point of interview, seven children had received a diagnosis of ADHD, two children were still under assessment, and one child had been referred for an ASD diagnosis (Table 1 ). The ADHD subtype of each participant was not recorded, however all children scored above the cut-off for both inattention (M = 87.3, SD = 5.03) and hyperactivity (M = 78.6, SD = 5.8) which is indicative of ADHD combined type. Use of stimulant medication was not recorded at the time of interview.
Following the child interview and receipt of parental consent, each child’s school was contacted to request their teacher’s participation in the study. Three teachers could not take part within the timeframe of the study, and one refused to take part. Six teachers (all female) were successfully contacted and gave informed consent to participate.
Due to the increased likelihood of co-occurring diagnoses in the target population, we also report Autism Spectrum Disorder (ASD) symptoms and Developmental Co-ordination Disorder (DCD) symptoms using the Autism Quotient 10-item questionnaire (AQ-10; Allison et al., 2012 ) and Movement ABC-2 Checklist (M-ABC2; Henderson et al., 2007 ) respectively, both completed by the child’s parent.
Scores of 6 and above on the AQ-10 indicates referral for diagnostic assessment for autism is advisable. All but one of the participants scored below the cut-off on this measure (M = 3.6, SD = 1.84).
The M-ABC2 checklist categorises children as scoring green, amber or red based on their scores. A green rating (up to the 85th percentile) indicates no movement difficulty, amber ratings (between 85 and 95th percentile) indicate risk of movement difficulty, and red ratings (95th percentile and above) indicate high likelihood of movement difficulty. Seven of the participants received a red rating, one an amber rating, and two green ratings.
Socioeconomic status (SES) is also known to impact educational outcomes, therefore the SES of each child was calculated using the Scottish Index of Multiple Deprivation (SIMD), which is an area-based measure of relative deprivation. The child’s home postcode was entered into the tool which provided a score of deprivation on a scale of 1 to 5. A score of 1 is given to the 20% most deprived data zones in Scotland, and a score of 5 indicates the area was within the 20% least deprived areas.
Semi-Structured Interview
The first author, who is a psychologist, conducted interviews with each participant individually, and then a separate interview with their teacher. This was guided by a semi-structured interview schedule (see Appendix A, Appendix B) developed in line with our research questions, existing literature, and using authors (T.S. and J.B.) expertise in educational practice. The questions were adapted to be relevant for the participant group. For example, children were asked “If a friend asked you to tell them what ADHD is, what would you tell them?” and teachers were asked, “What is your understanding of ADHD or can you describe a typical child with ADHD?”. The schedule comprised two key sections for both teachers and children. The first section focused on probing the participant’s understanding and knowledge of ADHD broadly. The second section focused on the participating child’s academic and cognitive strengths and weaknesses, and the strategies used to support them. Interviews with children took place in the child’s home and lasted between 19 and 51 min (M = 26.3, SD = 10.9). Interviews with teachers took place at their school and were between 28 and 50 min long (M = 36.5, SD = 7.61). Variation in interview length was mostly due to availability of the participant and/or age of the child (i.e. interviews with younger children tended to be shorter). All interviews were recorded on an encrypted voice recorder and transcribed by the first author prior to data analysis. Pseudonyms were randomly generated for each child to protect anonymity.
Reflexive thematic analysis was used to analyse the data (Braun & Clarke, 2019 ). This flexible approach allows the data to drive the analysis, putting the participant at the centre of the research and placing high value on the experiences and perspectives of individual participants (Braun & Clarke, 2006 ). The six phases of reflexive thematic analysis as outlined by Braun and Clarke were followed: (1) familiarisation, (2) generating codes, (3) constructing themes, (4) revising themes, (5) defining themes, (6) producing the report. Due to the exploratory nature of this study, bottom-up inductive coding was used. Two of the authors (E.M. and C.T.) worked collaboratively to construct and subsequently define the themes using the process described above. More specifically, one author (E.M.) generated codes, with support from another author (C.T.). Collated codes and data were then abstracted into potential themes, which were reviewed and refined using relevant literature, as well as within the wider context of the data. This process continued until all themes were agreed upon.
In the first part of the analysis, focus was placed on summarising the participants’ understanding of ADHD, as well as what they thought their biggest strengths and challenges were at school. Following this, an in-depth analysis of the strategies used in the classroom was conducted, taking into account the perspective of both teachers and children, aiming to generate themes from the data.
Knowledge of ADHD
Children and teachers were asked about their knowledge of ADHD. When asked if they had ever heard of ADHD, the majority of children said yes. Some of the children could not explain to the interviewer what ADHD was or responded in a way that suggested a lack of understanding ( “it helps you with skills” – Niall, 7 years; “ Well it’s when you can’t handle yourself and you’re always crazy and you can just like do things very fast”— Nathan, 8 years). Very few of the children were able to elaborate accurately on their understanding of ADHD, which exclusively focused on inattention. For example, Paige (8 years) said “ its’ kinda like this thing that makes it hard to concentrate ” and Finn (10 years) said “ they get distracted more just in different ways that other people would ”. This suggests that children with ADHD may lack or have a limited awareness or understanding of their diagnosis.
When asked about their knowledge of ADHD, teachers tended to focus on the core symptoms of ADHD. All teachers directly mentioned difficulties with attention, focus or concentration, and most directly or indirectly referred to hyperactivity (e.g. moving around, being in “ overdrive ”). Most teachers also referred to social difficulties as a feature of ADHD, including not following social rules, reacting inappropriately to other children and appearing to lack empathy, which they suggested could be linked to impulsivity. For example, “ reacting in social situations where perhaps other children might not react in a similar way” (Paige’s teacher) and “ They can react really really quickly to things and sometimes aggressively” (Eric’s teacher). Although no teachers directly mentioned cognitive difficulties, some referred to behaviours indicative of cognitive difficulties, for example, “ they can’t store a lot of information at one time” (Eric’s teacher) and, “ it’s not just the concentration it’s the amount they can take in at a time as well” (Nathan’s teacher), which may reflect processing or memory differences. Heterogeneity was mentioned, in that ADHD can mean different things for different children (e.g., “ I think ADHD differs from child to child and I think that’s really important” —Nathan’s teacher). Finally, academic difficulties as a feature of ADHD were also mentioned (e.g., “ a child… who finds some aspects of school life, some aspects of the curriculum challenging ”—Jay’s teacher).
After being asked to give a general description of ADHD, each child was asked about their own strengths at school and teachers were also asked to reflect on this topic for the child taking part.
When asked what they like most about school, children often mentioned art or P.E. as their preferred subjects. A small number of children said they enjoyed maths or reading, but this was not common and the majority described these subjects as a challenge or something they disliked. There was also clear link between the aspects of school children enjoyed, and what they perceived to be a strength for them. For example, when asked what he liked about school, Eric (10 years) said, “ Math, I’m pretty good at that”, or when later asked what they were good at, most children responded with the same answers they gave when asked what they liked about school. It is interesting to note that subjects such as art or P.E. generally have a different format to more traditionally academic subjects such as maths or literacy. Indeed, Felicity (11 years) said, “ I quite like art and drama because there’s not much reading…and not really too much writing in any of those” . Children also tended to mention the non-academic aspects of school, such as seeing their friends, or lunch and break times.
Teachers’ descriptions of the children’s strengths were much more variable compared to strengths mentioned by children. Like the children, teachers tended to consider P.E and artistic activities to be a strength for the child with ADHD. Multiple teachers referred to the child having a good imagination and creative skills. For example, “ she’s a very imaginative little girl, she has a great ability to tell stories and certainly with support write imaginative stories” (Paige’s teacher) . Teachers referred to other qualities or characteristics of the child as strengths, although these varied across teachers. These included openness, both socially but also in the context of willingness to learn or being open to new challenges, being a hard worker, or an enjoyable person to be around (e.g., “ he is the loveliest little boy, I’ve got a lot of time for [Nathan]. He makes me smile every day, you know, he just comes out with stuff he’s hilarious”— Nathan’s teacher). The most noticeable theme that emerged from this data was that when some teachers began describing one of the child’s strengths, it was suffixed with a negative. For example, Henry’s teacher said, “ He’s got a very good imagination, his writing- well not so much the writing of the stories, he finds writing quite a challenge, but his verbalising of ideas he’s very imaginative”. This may reflect that while these children have their own strengths, these can be limited by difficulties. Indeed, Paige’s teacher said, “ I think she’s a very able little girl without a doubt, but there is a definite barrier to her learning in terms of her organisation, in terms of her focus” , which reinforces this notion.
Children were asked directly about what they disliked about school, and what they found difficult. Children tended to focus more on specific subjects, with maths and aspects of literacy being the most frequently mentioned of these. Children referred to difficulties with or a dislike for reading, writing and/or spelling activities, for example, Rory (9 years) said “ Well I suppose spelling because … sometimes we have to do some boring tasks like we have to write it out three times then come up with the sentence for each one which takes forever and it’s hard for me to think of the sentences if I’m not ready” . Linking this with known cognitive difficulties in ADHD, it is interesting to note that both memory and planning are implicated in this quote from Rory about finding spelling challenging. In terms of writing, children referred to both the physical act of writing (e.g., “ probably writing cause sometimes I forget my finger spaces ”—Paige, 8 years; “ [writing the alphabet is] too hard… like the letters joined together … [and] I make mistakes” —Jay, 7 years) as well as the planning associated with writing a longer piece of work (e.g. “ when I run out of ideas for it, it’s really hard to think of some more so I don’t usually get that much writing done ”—Rory (9 years) .
Aside from academic subjects, several children referred to difficulties with focus or attention (e.g. “ when I find it hard to do something I normally kind of just zone out ”—Felicity, 11 years, “ probably concentrating sometimes ”—Rory, 9 years), but boredom was also a common and potentially related theme (e.g. “ Reading is a bit hard though … it just sometimes gets a bit boring” —Finn, 10 years, “ I absolutely hate maths … ‘cause it’s boring ”—Paige, 8 years). It could be that children with ADHD find it more difficult to concentrate during activities they find boring. Indeed, when Jay (7 years) was asked how it made him feel when he found something boring, he said “ it made me not do my work ”. Some children also alluded to the social difficulties faced at school, which included bullying and difficulties making friends (e.g. “ just making all kind of friends [is difficult] ‘cause the only friend that I’ve got is [name redacted] ”—Nathan, 8 years; “ sometimes finding a friend to play with at break time [is difficult] ” – Paige, 8 years; “ there’s a lot of people in my school that they bully me” —Eric, 10 years).
When asked what they thought were the child’s biggest challenges at school, teachers' responses were relatively variable, although some common themes were identified. As was the case for children, teachers reflected on difficulties with attention, which also included being able to sit at the table for long periods of time (e.g. “ I would say he struggles the most with sitting at his table and focusing on one piece of work ”—Henry’s teacher). Teachers did also mention difficulties with subjects such as maths and literacy, although this varied from child to child, and often they discussed these in the context of their ADHD symptom-related difficulties. For example, Eric’s teacher said, “ we’ve struggled to get a long piece of writing out of him because he just can’t really sit for very long ”. This quote also alludes to difficulties with evaluating the child’s academic abilities, due to their ADHD-related difficulties, which was supported by other teachers (e.g. “ He doesn’t particularly enjoy writing and he’s slow, very slow. And I don’t know if that’s down to attention or if that’s something he actually does find difficult to do ” —Henry’s teacher). Furthermore, some teachers reflected on the child’s confidence as opposed to a direct academic difficulty. For example, Luna’s teacher said, “ I think it’s she lacks the confidence in maths and reading like the most ” and later, elaborated with “ she’ll be like “I can’t do it” but she actually can. Sometimes she’s … even just anxious at doing a task where she thinks … she might not get it. But she does, she’s just not got that confidence”.
Teachers also commonly mentioned social difficulties, and referred to these difficulties as a barrier to collaborative learning activities (e.g. “ he doesn’t always work well with other people and other people can get frustrated” —Henry’s teacher; “ [during] collaborative group work [Paige] perhaps goes off task and does things she shouldn’t necessarily be doing and that can cause friction within the group” —Paige’s teacher). Teachers also mentioned emotion regulation, mostly in relation to the child’s social difficulties. For example, Eric’s teacher said “ I think as well he does still struggle with his emotions like getting angry very very quickly, and being very defensive when actually he’s taken the situation the wrong way” , which suggests that the child’s difficulty with regulating emotions may impact on their social relationships.
Strategy Use in the Classroom
Strategies to support learning fell into one of four categories: concrete or visual resources, information processing, seating and movement, and support from or influence of others. Examples of codes included in each of these strategy categories are presented in Table 2 .
Concrete or visual resources were the most commonly mentioned type of strategy by teachers and children, referring to the importance of having physical representations to support learning. Teachers spoke about the benefit of using visual aids (e.g. “ I think [Henry] is quite visual so making sure that there is visual prompts and clues and things like that to help him ”—Henry’s teacher), and teachers and children alluded to these resources supporting difficulties with holding information in mind. For example, when talking about the times table squares he uses, Rory said “ sometimes I forget which one I’m on…and it’s easier for me to have my finger next to it than just doing it in my head because sometimes I would need to start doing it all over again ”.
Seating and movement were also commonly mentioned, which seemed to be specific to children with ADHD in that it was linked to inattention and hyperactivity symptoms. For example, teachers referred to supporting attention or avoiding distraction by the positioning of a child’s location in the classroom (e.g. “ he’s so easily distracted, so he has an individual desk in the room and he’s away from everyone else because he wasn’t coping at a table [and] he’s been so much more settled since we got him an individual desk” —Eric’s teacher). Some teachers also mentioned the importance of allowing children to move around the room where feasible, as well as giving them errands to perform as a movement break (e.g. “ if I need something from the printer, [Nathan] is gonna go for it for me…because that’s down the stairs and then back up the stairs so if I think he’s getting a bit chatty or he’s not focused I’ll ask him to go and just give him that break as well” —Nathan’s teacher). Children also spoke about these strategies but didn’t necessarily describe why or how these strategies help them.
Information processing and cognitive strategies included methods that supported children to process learning content or instructions. For example, teachers frequently mentioned breaking down tasks or instructions into more manageable chunks (e.g. “ with my instructions to [Eric] I break them down … I’ll be like “we’re doing this and then we’re doing this” whereas the whole class wouldn’t need that ”—Eric’s teacher). Teachers and children also mentioned using memory strategies such as songs, rhymes or prompts. For example, Jay’s teacher said, “ if I was one of the other children I could see why it would be very distracting but he’s like he’s singing to himself little times table songs that we’ve been learning in class” , and Paige (8 years) referred to using mnemonics to help with words she struggles to spell, “ I keep forgetting [the word] because. But luckily we got the story big elephants can always understand little elephants [which helps because] the first letter of every word spells because” .
Both groups of participants mentioned support from and influence of others, and referred to working with peers, the teacher–child relationship, and one-to-one teaching. Peer support was a common theme across the data and is discussed in more detail in the thematic analysis findings, where teachers and children referred to the importance of the role of peers during learning activities. Understanding the child well and adapting to them was also seen as important, for example, Luna’s teacher said, “ with everything curricular [I] try and have an art element for her, just so I know it’ll engage her [because] if it’s like a boring old written worksheet she’s not gonna do it unless you’re sitting beside her and you’re basically telling her the answers” . As indicated in this quote, teachers also referred to the effectiveness of one-to-one or small group work with the child (e.g. “ when somebody sits beside her and explains it, and goes “come on [Paige] you know how to do this, let’s just work through a couple of examples”… her focus is generally better ” – Paige’s teacher), however this resource is not always available (e.g. “ I’d love for someone to be one-to-one with [Luna] but it’s just not available, she doesn’t meet that criteria apparently ” – Luna’s teacher). Children also referred to seeking direct support from their teacher (e.g. “if I can’t get an idea of what I’m doing then I ask the teacher for help” – Paige, 8 years), but were more likely to mention seeking support from their peers than the teacher.
Thematic Analysis
In addition to summarising the types of strategies that teachers and children reported using in the classroom, the data were also analysed using thematic analysis to generate themes. These are now presented. The theme names, definitions, and example quotes for each theme are presented in Table 3 .
Theme 1: Classroom-General Versus Individual-Specific Strategies
During the interviews, teachers spoke about strategies that they use as part of their teaching practice for the whole class but that are particularly helpful for the child/children with ADHD. These tended to be concrete or visual resources that are available in the classroom for anyone, for example, a visual timetable or routine checklist (e.g. “ there’s also a morning routine and listing down what’s to be done and where it’s to go … it’s very general for the class but again it’s located near her” —Paige’s teacher).
Teachers also mentioned using strategies that have been implemented specifically for that child, and these strategies tended to focus on supporting attention. For example, Nathan’s teacher spoke about the importance of using his name to attract his attention, “ maybe explaining to the class but then making sure that I’m saying “[Nathan], you’re doing this”, you know using his name quite a lot so that he knows it’s his task not just the everybody task ”, and this was a strategy that multiple teachers referred to using with the individual child and not necessarily for other children. Other strategies to support attention with a specific child also tended to be seating and movement related, such as having an individual desk or allowing them to fidget. For example, Luna’s teacher said, “ she’s a fidgeter so she’ll have stuff to fidget with … [and] even if she’s wandering around the classroom or she’s sitting on a table, I don’t let other kids do that, but as long as she’s listening, it’s fine [with me]” .
Similar to teachers, children spoke about strategies or resources that were in place for them specifically as well as about general things in the classroom that they find helpful. That said, it was less common for children to talk about why particular strategies were in place for them and how they helped them directly.
In addition to recognising strategies that teachers had put in place for them, children also referred to using their own strategies in the classroom. The most frequently mentioned strategy was fidgeting, and although some of the younger children spoke about having resources available in the classroom for fidgeting, some of the older children referred to using their own toy or an object that was readily available to them but not intended for fidgeting. For example, Finn (10 years) and Rory (9 years) both spoke about using items from their pencil case to fiddle with, and explained that this would help them to focus. (“ Sometimes I fidget with something I normally just have like a pencil holder under the table moving about … [and] it just keeps my mind clear and not from something else ”—Rory; “ Sometimes I fiddle with my fingers and that sometimes helps, but if not I get one of my coloured pencils and have a little gnaw on it because that actually takes my mind off some things and it’s easier for me to concentrate when I have something to do ”—Finn). Henry (9 years) spoke about being secretive with his fidgeting as it was not permitted in class, “ if you just bring [a fidget toy] in without permission [the teacher will] just take it off of you, so it has to be something that’s not too big. I bring in a little Lego ray which is just small enough that she won’t notice ”. Although some teachers did mention having fidget toys available, not all teachers seemed to recognise the importance of this for the child, and some children viewed fidgeting as a behaviour they should hide from the teacher.
Another strategy mentioned uniquely by children was seeing their peers as a resource for ideas or information. This is discussed in more detail in Theme 3—The role of peers , but reinforces the notion that children also develop their own strategies, independently from their teacher, rather than relying only on what is made available to them.
Theme 2: Heterogeneity of Strategies
Teachers spoke about the need for a variety of strategies in the classroom, for two reasons: (1) that different strategies work for different children (e.g. “ some [strategies] will work for the majority of the children and some just don’t seem to work for any of them ”—Jay’s teacher), and (2) what works for a child on one occasion may not work consistently for the same child (e.g. “ I think it’s a bit of a journey with him, and some things have worked and then stopped working, so I think we’re constantly adapting and changing what we’re doing ”—Eric’s teacher). One example of both of these challenges of strategy use came from Luna’s teacher, who spoke about using a reward chart with Luna and another child with ADHD, “ [Luna] and another boy in my class [with ADHD] both had [a reward chart]… but I think whereas the boy loved his and still loves his, she was getting a bit “oh I’m too cool for this” or that sort of age… so I stopped doing that for her and she’s not missing that at all” . These quotes demonstrate that strategies can work differently for different children, highlighting the need for a variety of strategies for teachers to access and trial with children.
Some children also referred to the variability of whether a strategy was helpful or not; for example, Henry (9 years) said that he finds it helpful to fidget with a toy but that sometimes it can distract him and prevent him from listening to the teacher. He said, “ Well, [the fidget toy] helps but it also gets me into trouble when the teacher spots me building it when I’m listening…but then sometimes I might not listen in maths and [use the fidget toy] which might make it worse”. This highlights that both children and teachers might benefit from support in understanding the contexts in which to use particular strategies, as well as why they are helpful from a psychological perspective.
For teachers, building a relationship with and understanding the child was also highly important in identifying strategies that would work. Luna’s teacher reflected upon the difference in Luna’s behaviour at the start of the academic year, compared to the second academic term, “ at the start of the year, we would just clash the whole time. I didn’t know her, she didn’t know me … and then when we got that bond she was absolutely fine so her behaviour has got way better ”. Eric’s teacher also reflected on how her relationship with Eric had changed, particularly after he received his diagnosis of ADHD, “ I think my approach to him has completely changed. I don’t raise my voice, I speak very calmly, I give him time to calm down before I even broach things with him. I think our relationship’s just got so much better ‘cause I kind of understand … where he’s coming from ”. She also said, “ it just takes a long time to get to know the child and get to know what works for them and trialling different things out ”, which demonstrates that building a relationship with and understanding the child can help to identify the successful strategies that work with different children.
Theme 3: The Role of Peers
Teachers and children spoke about the role of the child’s peers in their learning. Teachers talked about the benefit of partnering the child with good role models (e.g. “ I will put him with a couple of good role models and a couple of children who are patient and who will actually maybe get on with the task, and if [Jay] is not on task or not on board with what they’re doing at least he’s hearing and seeing good behaviour ”—Jay’s teacher), whereas children spoke more about their peers as a source of information, idea generation, or guidance on what to do next. For example, when asked what he does to help him with his writing, Henry (9 years) said, “ [I] listen to what my partner’s saying… my half of the table discuss what they’re going to do so I can literally hear everything they’re doing and steal some of their ideas ”. Henry wasn’t the only child to use their peers as a source of information, for example, Niall (7 years) said, “ I prefer working with the children because some things I might not know and the children might help me give ideas ”, and with a more specific example, Rory (9 years) said, “ somebody chose a very good character for their bit of writing, and I was like “I think I might choose that character”, and somebody else said “my setting was going to be the sea”, and I chose that and put that in a tiny bit of my story ”.
Some children also spoke about getting help from their peers in other ways, particularly when completing a difficult task. Paige (8 years) said, “ if the question isn’t clear I try and figure it out, and if I can’t figure it out then… don’t tell my teacher this but I sometimes get help from my classmates ”, which suggests some guilt associated with asking for help from her peers. This could be related to confidence and self-esteem, which teachers mentioned as a difficulty for some children with ADHD. In some instances, children felt it necessary to directly copy their peers’ work; for example, Nathan (8 years) spoke about needing a physical resource (i.e. “ fuzzies ”) to complete maths problems, but that when none were available he would “ just end up copying other people ”. This could also be related to a lack of confidence, as he may feel as though he may not be able to complete the task on his own. Indeed, Nathan’s teacher mentioned that when he is given the option to choose a task from different difficulty levels, Nathan would typically choose something easier, and that it was important to encourage him to choose something more difficult to build his confidence, “ I quite often say to him “come on I think you can challenge yourself” and [will] use that language”.
Peers clearly play an important role for the children with ADHD, and this is recognised both by the children themselves, and by their teachers. Teachers also mentioned that children with ADHD respond well to one-to-one learning with staff, indicating that it is important for these children to have opportunities to learn in different contexts: whole classroom learning, small group work and one-to-one.
In this study, a number of important topics surrounding ADHD in the primary school setting were explored, including ADHD knowledge, strengths and challenges, and strategy use in the classroom, each of which will now be discussed in turn before drawing together the findings and outlining the implications.
ADHD Knowledge
Knowledge of ADHD varied between children and their teachers. Whilst most of the children claimed to have heard of ADHD, very few could accurately describe the core symptoms. Previous research into this area is limited, however this finding supports Climie and Henley’s ( 2018 ) finding that children’s knowledge of ADHD can be limited. By comparison, all of the interviewed teachers had good knowledge about the core ADHD phenotype (i.e. in relation to diagnostic criteria) and some elaborated further by mentioning social difficulties or description of behaviours that could reflect cognitive difficulties. This supports and builds further upon existing research into teachers’ ADHD knowledge, demonstrating that although teachers understanding may be grounded in a focus upon inattention and hyperactivity, this is not necessarily representative of the range of their knowledge. By interviewing participants about their ADHD knowledge, as opposed to asking them to complete a questionnaire as previous studies have done (Climie & Henley, 2018 ; Latouche & Gascoigne, 2019 ; Ohan et al., 2008 ; Perold et al., 2010 ), the present study has demonstrated the specific areas of knowledge that should be targeted when designing psychoeducation interventions for children and teachers, such as broader aspects of cognitive difficulties in executive functions and memory. Improving knowledge of ADHD in this way could lead to increased positive attitudes and reduction of stigma towards individuals with ADHD (Mueller et al., 2012 ; Ohan et al., 2008 ), and in turn improving adherence to more specified interventions (Bai et al., 2015 ).
Strengths and Challenges
A range of strengths and challenges were discussed, some of which were mentioned by both children and teachers, whilst others were unique to a particular group. The main consensus in the current study was that art and P.E. tended to be the lessons in which children with ADHD thrive the most. Teachers elaborated on this notion, speaking about creative skills, such as a good imagination, and that these skills were sometimes applied in other subjects such as creative writing in literacy. Little to no research has so far focused on the strengths of children with ADHD, therefore these findings identify important areas for future investigation. For example, it is possible that these strengths could be harnessed in educational practice or intervention.
Although a strength for some, literacy was commonly mentioned as a challenge by both groups, specifically in relation to planning, spelling or the physical act of writing. Previous research has repeatedly demonstrated that literacy outcomes are poorer for children with ADHD compared to their typically developing peers (DuPaul et al., 2016; Mayes et al., 2020 ), however in these studies literacy tended to be measured using a composite achievement score, where the nuance of these difficulties can be lost. Furthermore, in line with a recent systematic review and meta-analysis (McDougal et al., 2022 ) the present study’s findings suggest that cognitive difficulties may contribute to poor literacy performance in ADHD. This issue was not unique to literacy, however, as teachers also spoke about academic challenges in the context of ADHD symptoms being a barrier to learning, such as finding it difficult to remain seated long enough to complete a piece of work. Children also raised this issue of engagement, who referred to the most challenging subjects being ‘boring’ for them. This link between attention difficulties and boredom in ADHD has been well documented (Golubchik et al., 2020 ). The findings here demonstrate the need for further research into the underlying cognitive difficulties leading to academic underachievement.
Both children and teachers also mentioned social and emotional difficulties. Research has shown that many different factors may contribute to social difficulties in ADHD (for a review see Gardner & Gerdes, 2015 ), making it a complex issue to disentangle. That said, in the current study teachers tended to attribute the children’s relationship difficulties to behaviour, such as reacting impulsively in social situations, or going off task during group work, both of which could be linked to ADHD symptoms. Despite these difficulties, peers were also considered a positive support. This finding adds to the complexity of understanding social difficulties for children with ADHD, demonstrating the necessity and value of further research into this key area.
The three key themes of classroom-general versus individual-specific strategies , heterogeneity of strategies and the role of peers were identified from the interview transcripts with children and their teachers. Within the first theme, classroom-general versus individual-specific strategies, it was clear that teachers utilise strategies that are specific to the child with ADHD, as well as strategies that are general to the classroom but that are also beneficial to the child with ADHD. Previously, Moore et al. ( 2017 ) found that teachers mostly reflected on using general inclusive strategies, rather than those targeted for ADHD specifically, however the methods differ from the current study in two key ways. Firstly, Moore et al.’s sample included secondary and primary school teachers, for whom the learning environment is very different. Secondly, focus groups were used as opposed to interviews where the voices of some participants can be lost. The merit of the current study is that children were also interviewed using the same questions as teachers; we found that children also referred to these differing types of strategies, and reported finding them useful, suggesting that the reports of teachers were accurate. Interestingly, children also mentioned their own strategies that teachers did not discuss and may not have been aware of. This finding highlights the importance of communication between the child and the teacher, particularly when the child is using a strategy considered to be forbidden or discouraged, for example copying a peer’s work or fidgeting with a toy. This communication would provide an understanding of what the child might find helpful, but more importantly identify areas of difficulty that may need more attention. Further to this, most strategies specific to the child mentioned by teachers aimed to support attention, and few strategies targeted other difficulties, particularly other aspects of cognition such as memory or executive function, which supports previous findings (Lawrence et al., 2017 ). The use of a wide range of individualised strategies would be beneficial to support children with ADHD.
Similarly, the second theme, heterogeneity of strategies , highlighted that some strategies work with some children and not others, and some strategies may not work for the same child consistently. Given the benefit of a wide range of strategy use, for both children with ADHD and their teachers, the development of an accessible tool-kit of strategies would be useful. Importantly, and as recognised in this second theme, knowing the individual child is key to identifying appropriate strategies, highlighting the essential role of the child’s teacher in supporting ADHD. Teachers mostly spoke about this in relation to the child’s interests and building rapport, however this could also be applied to the child’s cognitive profile. A tool-kit of available strategies and knowledge of which difficulties they support, as well as how to identify these difficulties, would facilitate teachers to continue their invaluable support for children and young people with ADHD. This links to the importance of psychoeducation; as previously discussed, the teachers in our study had a good knowledge of the core ADHD phenotype, but few spoke about the cognitive strengths and difficulties of ADHD. Children and their teachers could benefit from psychoeducation, that is, understanding ADHD in more depth (i.e., broader cognitive and behavioural profiles beyond diagnostic criteria), what ADHD and any co-occurrences might mean for the individual child, and why certain strategies are helpful. Improving knowledge using psychoeducation is known to improve fidelity to interventions (Dahl et al., 2020 ; Nussey et al., 2013 ), suggesting that this would facilitate children and their teachers to identify effective strategies and maintain these in the long-term.
The third theme, the role of peers , called attention to the importance of classmates for children with ADHD, and this was recognised by both children and their teachers. As peers play a role in the learning experience for children with ADHD, it is important to ensure that children have opportunities to learn in small group contexts with their peers. This finding is supported by Vygotsky’s ( 1978 ) Zone of Proximal Development; it is well established in the literature that children can benefit from completing learning activities with a partner, especially a more able peer (Vygotsky, 1978 ).
Relevance of Co-Occurrences
Co-occurring conditions are common in ADHD (Jensen & Steinhausen, 2015 ), and there are many instances within the data presented here that may reflect these co-occurrences, in particular, the overlap with DCD and ASD. For ADHD and DCD, the overlap is considered to be approximately 50% (Goulardins et al., 2015 ), whilst ADHD and autism also frequently co-occur with rates ranging from 40 to 70% (Antshel & Russo, 2019 ). It was not an aim of the current study to directly examine co-occurrences, however it is important to recognise their relevance when interpreting the findings. Indeed, in the current sample, scores for seven children (70%) indicated a high likelihood of movement difficulty. One child scored above the cut-off for autism diagnosis referral on the AQ-10, indicating heightened autism symptoms. Further to this, some of the discussions with children and teachers seemed to be related to DCD or autism, for example, the way that they can react in social situations, or difficulties with the physical act of handwriting. This finding feeds into the ongoing narrative surrounding heterogeneity within ADHD and individualisation of strategies to support learning. Recognising the potential role of co-occurrences should therefore be a vital part of any psychoeducation programme for children with ADHD and their teachers.
Limitations
Whilst a strong sample size was achieved for the current study allowing for rich data to be generated, it is important to acknowledge the issue of representativeness. The heterogeneity of ADHD is recognised throughout the current study, however the current study represents only a small cohort of children and young people with ADHD and their teachers which should be considered when interpreting the findings, particularly in relation to generalisation. Future research should investigate the issues raised using quantitative methods. Also on this point of heterogeneity, although we report some co-occurring symptoms for participants, the number of co-occurrences considered here were limited to autism and DCD. Learning disabilities and other disorders may play a role, however due to the qualitative nature of this study it was not feasible to collect data on every potential co-occurrence. Future quantitative work should aim to understand the complex interplay of diagnosed and undiagnosed co-occurrences.
Furthermore, only some of the teachers of participating children took part in the study; we were not able to recruit all 10. It may be, for example, that the six teachers who did take part were motivated to do so based on their existing knowledge or commitment to understanding ADHD, and the fact that not all child-teacher dyads are represented in the current study should be recognised. Another possibility is the impact of time pressures upon participation for teachers, particularly given the increasing number of children with complex needs within classes. Outcomes leading from the current study could support teachers in this respect.
It is also important to recognise the potential role of stimulant medication. Although it was not an aim of the current study to investigate knowledge or the role of stimulant medication in the classroom setting, it would have been beneficial to record whether the interviewed children were taking medication for their ADHD at school, particularly given the evidence to suggest that stimulant medication can improve cognitive and behavioural symptoms of ADHD (Rhodes et al., 2004 ). Examining strategy use in isolation (i.e. with children who are drug naïve or pausing medication) will be a vital aim of future intervention work.
Implications/Future Research
Taking the findings of the whole study together, one clear implication is that children and their teachers could benefit from psychoeducation, that is, understanding ADHD in more depth (i.e., broader cognitive and behavioural profiles beyond diagnostic criteria), what ADHD might mean for the individual child, and why certain strategies are helpful. Improving knowledge using psychoeducation is known to improve fidelity to interventions (Dahl et al., 2020 ; Nussey et al., 2013 ), suggesting that this would facilitate children and their teachers to identify effective strategies and maintain these in the long-term.
To improve knowledge and understanding of both strengths and difficulties in ADHD, future research should aim to develop interventions grounded in psychoeducation, in order to support children and their teachers to better understand why and in what contexts certain strategies are helpful in relation to ADHD. Furthermore, future research should focus on the development of a tool-kit of strategies to account for the heterogeneity in ADHD populations; we know from the current study’s findings that it is not appropriate to offer a one-size-fits-all approach to supporting children with ADHD given that not all strategies work all of the time, nor do they always work consistently. In terms of implications for educational practice, it is clear that understanding the individual child in the context of their ADHD and any co-occurrences is important for any teacher working with them. This will facilitate teachers to identify and apply appropriate strategies to support learning which may well result in different strategies depending on the scenario, and different strategies for different children. Furthermore, by understanding that ADHD is just one aspect of the child, strategies can be used flexibly rather than assigning strategies based on a child’s diagnosis.
This study has provided invaluable novel insight into understanding and supporting children with ADHD in the classroom. Importantly, these insights have come directly from children with ADHD and their teachers, demonstrating the importance of conducting qualitative research with these groups. The findings provide clear scope for future research, as well as guidelines for successful intervention design and educational practice, at the heart of which we must acknowledge and embrace the heterogeneity and associated strengths and challenges within ADHD.
Allison, C., Auyeung, B., & Baron-Cohen, S. (2012). Autism spectrum quotient: 10 items (AQ-10). Journal of the American Academy of Child and Adolescent Psychiatry., 51 (2), 202–212.
Article PubMed Google Scholar
Antshel, K. M., & Russo, N. (2019). Autism spectrum disorders and ADHD: Overlapping phenomenology, diagnostic issues, and treatment considerations. Current Psychiatry Reports, 21 (5), 34. https://doi.org/10.1007/s11920-019-1020-5
Arnold, L. E., Hodgkins, P., Kahle, J., Madhoo, M., & Kewley, G. (2020). Long-term outcomes of ADHD: Academic achievement and performance. Journal of Attention Disorders, 24 (1), 73–85. https://doi.org/10.1177/1087054714566076
Bai, G., Yang, L., Wang, Y., & Niu, W.-Y. (2015). Effectiveness of a focused, brief psychoeducation program for parents of ADHD children: Improvement of medication adherence and symptoms. Neuropsychiatric Disease and Treatment, . https://doi.org/10.2147/NDT.S88625
Article PubMed PubMed Central Google Scholar
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3 (2), 77–101. https://doi.org/10.1191/1478088706qp063oa
Article Google Scholar
Braun, V., & Clarke, V. (2019). Reflecting on reflexive thematic analysis. Qualitative Research in Sport, Exercise and Health, 11 (4), 589–597. https://doi.org/10.1080/2159676X.2019.1628806
Classi, P., Milton, D., Ward, S., Sarsour, K., & Johnston, J. (2012). Social and emotional difficulties in children with ADHD and the impact on school attendance and healthcare utilization. Child and Adolescent Psychiatry and Mental Health, 6 (1), 33. https://doi.org/10.1186/1753-2000-6-33
Climie, E. A., & Henley, L. (2018). Canadian parents and children’s knowledge of ADHD. Vulnerable Children and Youth Studies, 13 (3), 266–275. https://doi.org/10.1080/17450128.2018.1484975
Coghill, D. R., Seth, S., & Matthews, K. (2014). A comprehensive assessment of memory, delay aversion, timing, inhibition, decision making and variability in Attention Deficit Hyperactivity Disorder: Advancing beyond the three-pathway models. Psychological Medicine, 44 (9), 1989–2001. https://doi.org/10.1017/S0033291713002547
Conners, C. K., & Multi-Health Systems Inc. (2008). Conners Comprehensive Behavior Rating Scales (Conners CBRS): Manual . North Tonawanda, N.Y: Multi-Health Systems.
Dahl, V., Ramakrishnan, A., Spears, A. P., Jorge, A., Lu, J., Bigio, N. A., & Chacko, A. (2020). Psychoeducation interventions for parents and teachers of children and adolescents with ADHD: A systematic review of the literature. Journal of Developmental and Physical Disabilities, 32 (2), 257–292. https://doi.org/10.1007/s10882-019-09691-3
DuPaul, G. J., Eckert, T. L., & Vilardo, B. (2012). The effects of school-based interventions for Attention Deficit Hyperactivity Disorder: A meta-analysis. School Psychology Review, 41 (4), 387412. https://doi.org/10.1080/02796015.2012.12087496
Gardner, D. M., & Gerdes, A. C. (2015). A review of peer relationships and friendships in youth with ADHD. Journal of Attention Disorders, 19 (10), 844–855. https://doi.org/10.1177/1087054713501552
Gathercole, S. E., Astle, D. A., Manly, T., the CALM Team, & Holmes, J. (2018). Cognition and behaviour in learning difficulties and ADHD: A dimensional approach [Preprint]. Animal Behavior and Cognition . https://doi.org/10.1101/260265
Golubchik, P., Manor, I., Shoval, G., & Weizman, A. (2020). Levels of proneness to boredom in children with Attention-Deficit/Hyperactivity Disorder on and off methylphenidate treatment. Journal of Child and Adolescent Psychopharmacology, 30 (3), 173–176. https://doi.org/10.1089/cap.2019.0151
Goulardins, J. B., Rigoli, D., Licari, M., Piek, J. P., Hasue, R. H., Oosterlaan, J., & Oliveira, J. A. (2015). Attention Deficit Hyperactivity Disorder and developmental coordination disorder: Two separate disorders or do they share a common etiology. Behavioural Brain Research, 292 , 484–492. https://doi.org/10.1016/j.bbr.2015.07.009
Henderson, S. E., Sugden, D. A., & Barnett, A. L. (2007). Movement assessment battery for children – (2nd ed.). Harcourt Assessment.
Google Scholar
Jensen, C. M., & Steinhausen, H.-C. (2015). Comorbid mental disorders in children and adolescents with Attention-Deficit/Hyperactivity Disorder in a large nationwide study. ADHD Attention Deficit and Hyperactivity Disorders, 7 (1), 27–38. https://doi.org/10.1007/s12402-014-0142-1
Jones, H. A., & Chronis-Tuscano, A. (2008). Efficacy of teacher in-service training for attention-deficit/hyperactivity disorder: Teacher in-service training for ADHD. Psychology in the Schools, 45 (10), 918–929. https://doi.org/10.1002/pits.20342
Kuriyan, A. B., Jr., Molina, B. S. G., Waschbusch, D. A., Gnagy, E. M., Sibley, M. H., Babinski, D. E., Walther, C., Cheong, J., Yu, J., & Kent, K. M. (2013). Young adult educational and vocational outcomes of children diagnosed with ADHD. Journal of Abnormal Child Psychology, 41 , 27–41. https://doi.org/10.1007/s10802-012-9658-z
Latouche, A. P., & Gascoigne, M. (2019). In-service training for increasing teachers’ ADHD knowledge and self-efficacy. Journal of Attention Disorders, 23 (3), 270–281. https://doi.org/10.1177/1087054717707045
Law, G. U., Sinclair, S., & Fraser, N. (2007). Children’s attitudes and behavioural intentions towards a peer with symptoms of ADHD: Does the addition of a diagnostic label make a difference? Journal of Child Health Care, 11 (2), 98–111. https://doi.org/10.1177/1367493507076061
Lawrence, K., Estrada, R. D., & McCormick, J. (2017). Teachers’ experiences with and perceptions of students with Attention Deficit/hyperactivity Disorder. Journal of Pediatric Nursing, 36 , 141–148. https://doi.org/10.1016/j.pedn.2017.06.010
Mayes, S. D., Waschbusch, D. A., Calhoun, S. L., & Mattison, R. E. (2020). Correlates of academic overachievement, nondiscrepant achievement, and learning disability in ADHD, autism, and general population samples. Exceptionality, 28 (1), 60–75. https://doi.org/10.1080/09362835.2020.1727324
McDougal, E., Gracie, H., Oldridge, J., Stewart, T. M., Booth, J. N., & Rhodes, S. M. (2022). Relationships between cognition and literacy in children with attention‐deficit/hyperactivity disorder: A systematic review and meta‐analysis. British Journal of Developmental Psychology , 40 (1), 130–150. https://doi.org/10.1111/bjdp.12395
McDougal, E., Riby, D. M., & Hanley, M. (2020). Teacher insights into the barriers and facilitators of learning in autism. Research in Autism Spectrum Disorders, 79 , 101674. https://doi.org/10.1016/j.rasd.2020.101674
Mohr-Jensen, C., Steen-Jensen, T., Bang-Schnack, M., & Thingvad, H. (2019). What do primary and secondary school teachers know about ADHD in children? Findings from a systematic review and a representative, nationwide sample of Danish teachers. Journal of Attention Disorders, 23 (3), 206–219. https://doi.org/10.1177/1087054715599206
Moore, D. A., Russell, A. E., Arnell, S., & Ford, T. J. (2017). Educators’ experiences of managing students with ADHD: A qualitative study: Educators’ management of ADHD. Child: Care, Health and Development, 43 (4), 489–498. https://doi.org/10.1111/cch.12448
Mueller, A. K., Fuermaier, A. B., Koerts, J., & Tucha, L. (2012). Stigma in attention deficit hyperactivity disorder. Attention Deficit and Hyperactivity Disorders, 4 (3), 101–114. https://doi.org/10.1007/s12402-012-0085-3
National Institute for Health and Care Excellence (NICE). (2018). Attention deficit hyperactivity disorder: Diagnosis and management . Retrieved August 2021, from https://www.nice.org.uk/guidance/ng87/chapter/Recommendations#managing-adhd .
Nussey, C., Pistrang, N., & Murphy, T. (2013). How does psychoeducation help? A review of the effects of providing information about Tourette syndrome and attention-deficit/hyperactivity disorder: A review of psychoeducational approaches in TS and ADHD. Child Care, Health and Development, 39 (5), 617–627. https://doi.org/10.1111/cch.12039
Ohan, J. L., Cormier, N., Hepp, S. L., Visser, T. A. W., & Strain, M. C. (2008). Does knowledge about attention-deficit/hyperactivity disorder impact teachers’ reported behaviors and perceptions? School Psychology Quarterly, 23 (3), 436–449. https://doi.org/10.1037/1045-3830.23.3.436
Perold, M., Louw, C., & Kleynhans, S. (2010). Primary school teachers’ knowledge and misperceptions of attention deficit hyperactivity disorder (ADHD). South African Journal of Education, 30 (3), 457–473.
Rhodes, S. M., Coghill, D. R., & Matthews, K. (2004). Methylphenidate restores visual memory, but not working memory function in attention deficit-hyperkinetic disorder. Psychopharmacology (berl), 175 (3), 319–330. https://doi.org/10.1007/s00213-004-1833-7
Rhodes, S. M., Park, J., Seth, S., & Coghill, D. R. (2012). A comprehensive investigation of memory impairment in attention deficit hyperactivity disorder and oppositional defiant disorder: Memory in ADHD and ODD. Journal of Child Psychology and Psychiatry, 53 (2), 128–137. https://doi.org/10.1111/j.1469-7610.2011.02436.x
Richardson, M., Moore, D. A., Gwernan-Jones, R., Thompson-Coon, J., Ukoumunne, O., Rogers, M., Whear, R., Newlove-Delgado, T. V., Logan, S., Morris, C., Taylor, E., Cooper, P., Stein, K., Garside, R., & Ford, T. J. (2015). Non-pharmacological interventions for attention-deficit/hyperactivity disorder (ADHD) delivered in school settings: Systematic reviews of quantitative and qualitative research. Health Technology Assessment, 19 (45), 1–470. https://doi.org/10.3310/hta19450
Russell, G., Rodgers, L. R., Ukoumunne, O. C., & Ford, T. (2014). Prevalence of parent-reported ASD and ADHD in the UK: Findings from the millennium cohort Study. Journal of Autism and Developmental Disorders, 44 (1), 31–40. https://doi.org/10.1007/s10803-013-1849-0
Sayal, K., Prasad, V., Daley, D., Ford, T., & Coghill, D. (2018). ADHD in children and young people: Prevalence, care pathways, and service provision. The Lancet. Psychiatry, 5 (2), 175–186. https://doi.org/10.1016/S2215-0366(17)30167-0
Vygotsky, L. S. (1978). Mind in society: The development of higher psychological processes . Harvard University Press.
Wiener, J., Malone, M., Varma, A., Markel, C., Biondic, D., Tannock, R., & Humphries, T. (2012). Children’s perceptions of their ADHD symptoms: Positive illusions, attributions, and stigma. Canadian Journal of School Psychology, 27 (3), 217–242. https://doi.org/10.1177/0829573512451972
Download references
The funding was provided by Waterloo Foundation Grant Nos. (707-3732, 707-4340, 707-4614).
Author information
Authors and affiliations.
Centre for Clinical Brain Sciences, Child Life and Health, University of Edinburgh, Edinburgh, United Kingdom
Emily McDougal, Claire Tai & Sinéad M. Rhodes
Moray House School of Education and Sport, University of Edinburgh, Edinburgh, United Kingdom
Tracy M. Stewart & Josephine N. Booth
School of Psychology, University of Surrey, Guildford, United Kingdom
Emily McDougal
You can also search for this author in PubMed Google Scholar
Contributions
E.M. Conceptualization, Methodology, Investigation, Data Curation, Formal Analysis, Writing - original draft, C.T. Formal Analysis, Writing - review & editing, T.M.S., J.N.B. and S.M.R. Conceptualization, Methodology, Writing - review & editing.
Corresponding author
Correspondence to Sinéad M. Rhodes .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Interview Schedule—Teacher
Demographic/experience.
How many years have you been teaching?
Are you currently teaching pupils with ADHD and around how many?
If yes, do you feel competent/comfortable/equipped teaching pupils with ADHD?
If no, how competent/comfortable/equipped would you feel to teach pupils with ADHD?
Would you say your experience of teaching pupils with ADHD is small/moderate/significant?
Psychoeducation
What is your understanding of ADHD/Can you describe a typical child with ADHD?
Probe behaviour knowledge
Probe cognition knowledge
Probe impacts of behaviour/cognition difficulties
Probe knowledge that children with ADHD differ from each other
Probe knowledge that children with ADHD have co-occurring difficulties as the norm
(If they do have some knowledge) Where did you learn about ADHD?
e.g. specific training, professional experience, personal experience, personal interest/research
Cognitive skills and strategies
Can you tell me about the pupil’s strengths?
Can you tell me about the pupil’s biggest challenges/what they need most support with?
When you are supporting the pupil with their learning, are there any specific things you do to help them? (i.e. strategies)
Probe internal
Probe external
Probe whether they think those not mentioned might be useful/feasible/challenges
Probe if different for different subjects/times of the day
In your experience, which of these you have mentioned are the most useful for the pupil?
Probe for examples of how they apply it to their learning
Probe whether these strategies are pupil specific or broadly relevant
Probe if specific to particular subjects/times of the day
In your experience, which of these you have mentioned are the least useful for the pupil?
What would you like to be able to support the pupil with that you don’t already do?
Probe why they can’t access this currently e.g. lack of training, resources, knowledge, time
Is there anything you would like to understand better about ADHD?
Probe behaviour
Probe cognition
Interview Schedule—Child
Script: We’re going to have a chat about a few different things today, mostly about your time at school. This will include things like how you get on, how you think, things you’re good at and things you find more difficult. I’ve got some questions here to ask you but try to imagine that I’m just a friend that you’re talking to about these things. There are no right or wrong answers, I’m just interested in what you’ve got to say. Do you have any questions?
Script: First we’re going to talk about ADHD (Attention Deficit Hyperactivity Disorder).
Have you ever heard of/has anyone ever told you what ADHD is?
(If yes) If a friend asked you to tell them what ADHD is, what would you tell them?
Is there anything you would like to know more about ADHD?
Cognition/strategy use
Script: Now we’re going to talk about something a bit different. Everyone has things they are good at, and things they find more difficult. For example, I’m quite good at listening to what people have to say, but I’m not so good at remembering people’s names. I’d like you to think about when you’re in school, and things you’re good at and things you are not so good at. It doesn’t just have to be lessons, it can be anything.
Do you like school?
Probe why/why not?
Probe favourite lessons
What sort of things do you find you do well at in school?
Is there anything you think that you find more difficult in school?
Probe: If I asked your teacher/parent what you find difficult, what would they say?
Probe: Is there anything at school you need extra help with?
Probe: Is there anything you do to help yourself with that?
Script: Some people do things to try to help themselves do things well. For example, when someone tells me a number to remember, I repeat it in my head over and over again.
Can you try to describe to me what you do to help you do these things?
Solving a maths problem
Planning your writing
Doing spellings
Trying to remember something
Concentrating/ignoring distractions
Listening to the teacher
Remaining seated in class when doing work
Working with other children in the class
Probe: Do you use anything in lessons to help you with your work?
Probe: What kind of things do you think could help you with your work?
Probe: Is there anything you do at home, such as when you’re doing your homework, to help you finish what you are doing to do it well?
Probe: Does someone help you with your homework at home? If yes, what do they do that helps? If no, what do you think someone could do to help?
Script: In this last part we’re going to talk about your time at school.
How many teachers are in your class?
Is there anyone who helps you with your work?
Do you work mostly on your own or in groups?
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
McDougal, E., Tai, C., Stewart, T.M. et al. Understanding and Supporting Attention Deficit Hyperactivity Disorder (ADHD) in the Primary School Classroom: Perspectives of Children with ADHD and their Teachers. J Autism Dev Disord 53 , 3406–3421 (2023). https://doi.org/10.1007/s10803-022-05639-3
Download citation
Accepted : 06 June 2022
Published : 01 July 2022
Issue Date : September 2023
DOI : https://doi.org/10.1007/s10803-022-05639-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Child and teacher interviews
- Strengths and difficulties
- Learning strategies
- Find a journal
- Publish with us
- Track your research
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
The impact of psychological theory on the treatment of Attention Deficit Hyperactivity Disorder (ADHD) in adults: A scoping review
Contributed equally to this work with: Rebecca E. Champ
Roles Conceptualization, Data curation, Formal analysis, Writing – original draft
* E-mail: [email protected]
Affiliation Department of Nursing and Midwifery, School of Human and Health Sciences, University of Huddersfield, Huddersfield, United Kingdom
Roles Supervision
¶ ‡ These authors also contributed equally to this work.
Affiliation School of Health and Life Sciences, Teeside University, Middlesbrough, United Kingdom
- Rebecca E. Champ,
- Marios Adamou,
- Barry Tolchard

- Published: December 21, 2021
- https://doi.org/10.1371/journal.pone.0261247
- Peer Review
- Reader Comments
Psychological theory and interpretation of research are key elements influencing clinical treatment development and design in Attention Deficit Hyperactivity Disorder (ADHD). Research-based treatment recommendations primarily support Cognitive Behavioural Therapy (CBT), an extension of the cognitive behavioural theory, which promotes a deficit-focused characterisation of ADHD and prioritises symptom reduction and cognitive control of self-regulation as treatment outcomes. A wide variety of approaches have developed to improve ADHD outcomes in adults, and this review aimed to map the theoretical foundations of treatment design to understand their impact. A scoping review and analysis were performed on 221 documents to compare the theoretical influences in research, treatment approach, and theoretical citations. Results showed that despite variation in the application, current treatments characterise ADHD from a single paradigm of cognitive behavioural theory. A single theoretical perspective is limiting research for effective treatments for ADHD to address ongoing issues such as accommodating context variability and heterogeneity. Research into alternative theoretical characterisations of ADHD is recommended to provide treatment design opportunities to better understand and address symptoms.
Citation: Champ RE, Adamou M, Tolchard B (2021) The impact of psychological theory on the treatment of Attention Deficit Hyperactivity Disorder (ADHD) in adults: A scoping review. PLoS ONE 16(12): e0261247. https://doi.org/10.1371/journal.pone.0261247
Editor: Gerard Hutchinson, University of the West Indies at Saint Augustine, TRINIDAD AND TOBAGO
Received: May 21, 2021; Accepted: November 25, 2021; Published: December 21, 2021
Copyright: © 2021 Champ et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The combination of psychological theory and interpretation of research have been highlighted as critical influencers guiding decision-making for clinical treatment design and development for Attention Deficit Hyperactivity Disorder (ADHD) [ 1 , 2 ]. ADHD is a neurodevelopmental disorder of self-regulation with symptoms negatively affecting daily functioning at work and at home, with long-term impacts in academic, occupational, social and emotional areas of functioning [ 3 – 8 ]. Effective, long-term treatment outcomes benefit both the individual with ADHD and society as a whole as undiagnosed and untreated adults with ADHD may become an economic burden due to increased health care costs and decreased productivity at work [ 9 , 10 ].
Russell Barkley [ 11 ] postulated the first unifying theory of ADHD, which places a core deficit of behavioural inhibition at the source of ADHD behaviours. Several theoretical models attribute additional and alternative cognitive sources for the development of ADHD symptoms [ 12 – 14 ]. While a variety of different interventions are available and the benefit of other forms of support is acknowledged (e.g. psychotherapy or coaching), only Cognitive Behavioural Therapy (CBT), Mindfulness, Dialectical Behavioural Therapy (DBT) and potentially Neurofeedback have the most empirical support [ 15 ]. Results of non-pharmacological intervention studies suggest these interventions have a positive effect on core behavioural symptoms of ADHD (inattention, hyperactivity/impulsivity), particularly when compared to inactive control conditions [ 15 , 16 ]. However, recent systematic reviews of non-pharmacological treatment highlight that different classes of intervention design take similar approaches; that heterogeneity in sample size, study design, quality and symptom outcome measurement makes meta-analysis difficult, and there is a high risk of bias [ 15 – 17 ]. Additionally, the National Institute for Health and Care Excellence (NICE) [ 18 ] only recommends interventions that match a similar protocol to medications: Randomised Controlled Trials (RCTs), primarily based in CBT [ 15 ], despite a growing wider evidence base.
It is hypothesised that much of current research for the characterisation of ADHD is based on a cognitive behavioural theoretical paradigm that does not account comprehensively for the broad spectrum of ADHD presentation [ 1 , 19 – 24 ]. This paradigm is deficit-focused with primary treatment outcomes of symptom reduction and control of maladaptive behaviours. Recent research in psychology suggests that this may not be the best approach to improving mental health, and it may be necessary to develop positive psychological factors and emotions that cultivate health and wellbeing [ 25 , 26 ]. This scoping review aims to map the evidence and understand the influence of current psychological theories on design and treatment recommendations in adult ADHD by answering the following questions:
- Are characterisations of ADHD dominated by a cognitive behavioural paradigm?
- Does that paradigm influence treatment design and outcomes?
- Are there any alternative characterisations of ADHD that present a different perspective to the cognitive behavioural paradigm?
A broad approach was considered most effective to identify gaps in the literature, as data regarding supportive psychological theories would likely be identified in publications beyond specific study designs. To our knowledge, this is the first scoping review providing an overview of the theoretical characterisations of ADHD and their impact on available treatments.
Search strategy
The scoping review was carried out over three months: February, March and April 2020. The scoping review protocol was published on the Open Science Framework ( https://osf.io/ ). Search design and criteria were formulated based on guidance and recommendations by Arksey & O’Malley [ 27 ], Colquhoun et al. [ 28 ], O’Brien et al. [ 29 ] and the Joanna Briggs Institute [ 30 ]. A starting timeframe from the publication of Barkley’s [ 11 ] theory was selected as the foundation for current theoretical characterisations of ADHD. Papers were reviewed from multiple countries, including the United States, the United Kingdom, The Netherlands, Canada, Argentina, Brazil, Colombia, Iceland, Ireland, Portugal, Spain, Belgium, Germany, Switzerland, Finland, Sweden, Israel, Iran, China, Hong Kong, India and Australia, and multiple languages including English, Dutch, German, French, and Spanish.
Research evidence was identified by conducting searches across web-based databases with pre-determined search terms. Table 1 outlines the search terms and syntax used in primary and secondary searches.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0261247.t001
Additional searches were in generic search engines Google and Google Scholar, and checks of references from guidance documents and systematic reviews for additional material. Once identified, these references were collected through additional database searches or a direct search in the specific journal or publication.
Inclusion criteria
Titles and abstracts of materials were reviewed for eligibility. Materials were considered appropriate if they met the following criteria:
- Studies involving research on a pilot, efficacy, or applicability of a treatment intervention for adults with ADHD (19–65+, male and female)
- Systematic reviews of treatment literature or specific approaches to treatment for adults with ADHD
- Thesis, conference papers, or reports reviewing, presenting, or recommending treatment approaches for adults with ADHD
- Documents, articles, books, or consensus statements presenting guidance or recommendations for treatment for adults with ADHD
Exclusion criteria
In addition to meeting the inclusion criteria, materials were excluded if they met one of the following exclusion criteria:
- Treatment approaches designed for a specific subset of participants (couples, military, substance abuse)
- Treatment approaches designed to treat specific comorbidities (Autism, Bi-polar, Learning Disabilities, Tourette’s, Oppositional Defiant Disorder, Personality Disorder, Traumatic Brain Injury)
- Treatment approaches designed for the inclusion of younger age groups (children, adolescents) or their parents
- Materials summarising and updating recent developments in the field of treatment for adult ADHD (general practice journals, nursing practice journals, medical student journals)
- Characterisations of adult ADHD that were not empirically researched
A large body of literature has been published over the years which present different characterisations of adult ADHD and subsequent recommendations for treatment. Predominantly based in the US, these biopsychosocial models range from origin theories of genetic strengths [ 31 ], diversity [ 32 ] and developmental impairment of the prefrontal cortex due to issues with attachment and trauma [ 33 ], to identifying multiple presentations of ADHD diagnosed individually with SPECT imaging [ 34 ]. While these models do present alternative characterisations of ADHD, they are not empirically researched and therefore will be excluded from this review.
The following PRISMA flowchart ( Fig 1 ) presents the search process details, including the number of articles located, those eliminated and those included in the final analysis.
https://doi.org/10.1371/journal.pone.0261247.g001
Results and analysis
The 221 articles were subdivided into the following categories according to their primary content: Cognitive Behavioural Therapy (122), Coaching (36), Psychotherapy (16), and Other (47). All articles were assessed for quality against the relevant Critical Appraisals Skills Programme (CASP) checklists. Results summary of the ADHD characterisation cited for each intervention category is displayed in a mosaic plot ( Fig 2 ).
https://doi.org/10.1371/journal.pone.0261247.g002
An overview of interventions published by year is displayed in a column chart ( Fig 3 ).
https://doi.org/10.1371/journal.pone.0261247.g003
Due to the number and variety of materials, a narrative analysis was performed to review the publications’ composition. Systematic reviews were also analysed separately to see if any review of the characterisation of ADHD had been completed previously.
Systematic reviews
Over the years, several systematic reviews of treatments for adult ADHD have been published. Searches were undertaken through Joanna Briggs Institute Evidence Synthesis, The Cochrane Database of Systematic Reviews, and the Campbell Library show some of these reviews are specific to the efficacy of a particular intervention approach, such as psychodynamic therapy [ 35 ], homoeopathy [ 36 ], Cognitive Behavioural Therapy (CBT) [ 37 – 41 ], Mindfulness [ 42 , 43 ], and Meditation [ 44 , 45 ]. Others have been focused on efficacy [ 2 , 15 , 16 , 46 – 48 ], long term outcomes [ 10 , 49 ], or guidance [ 50 ]. Only one systematic review investigated the characterisation of adult ADHD but failed to find evidence of neurocognitive disfunction as a predictor of persistence [ 51 ]. Interestingly, one systematic review investigated how adults with ADHD experience and manage their symptoms [ 52 ]. Therefore, it seems that no recent attempt has reviewed the psychological theories for the characterisation of adult ADHD.
Data extraction
Articles were reviewed, and data extracted into categorised excel spreadsheets for comparison. Each document was examined for the following criteria:
- Research Purpose/Outcome
- Treatment Approach
- ADHD Characterisation
- ADHD Theory
Intervention analysis
Research studies and guidance documents present treatment approaches in various environments, contexts and skill levels of delivery. The following interventions present a wide range of delivery in clinical and non-clinical environments; therapeutic, academic, and social contexts; and professionals including psychiatrists, clinical psychologists, nurses, occupational therapists, psychotherapists, as well as counsellors, coaches, and mentors.

Cognitive Behavioural Therapy (CBT).
Due to the involvement of cognitive behavioural theory in establishing the characterisation of ADHD, the bulk of research in the field has used this intervention model. While recommended as the primary treatment modality, treatment goals and methodologies have changed over time. Due to this shift in focus, some early research references non-empirical anecdotal work. This analysis will use the delineation of “waves” as seen in the current theoretical literature to demonstrate these changes [ 53 ] ( S1 Appendix ).
First wave : Behaviourism . Before 1990, ADHD was still considered a disorder of childhood. Although considerable research exists regarding “first wave” treatments in children, the few approaches developed for adults apply pure behavioural theory and techniques. A case study of three subjects focused on improving attentional behaviour in psychiatric patients [ 54 ], and the design utilises operant theory and models used for brain injury [ 55 ]. Guidance documents for teachers, parents and counsellors [ 56 ] and psychotherapists [ 57 ] highlight the importance of behavioural skill development. The conceptualisation of ADHD in these treatment models is a disorder of attention [ 54 ] and a neurobiological disorder of self-regulation, executive function deficits and disinhibition [ 56 , 57 ]. Burgess et al. [ 54 ] exemplify the transition of the conceptualisation of attentional deficits in ADHD from mental illness to mental disorder.
The therapist’s role in these models is to assist the client in learning and practising practical behavioural strategies for task attention, organisation, listening and scheduling, and planning and organising daily activities. Treatment designs are varied, with only one specifying weekly sessions from 6–10 weeks [ 54 ]. Characterisation of ADHD aetiology highlight issues with inability to maintain vigilance (attention deficit) and distractibility [ 54 ], self-regulation, impaired inhibition, developmental delay, and deficits in executive function, referencing Barkley [ 56 , 57 ].
Rational Emotive Behaviour Therapy (REBT) . A single case study for ADHD specifically used REBT [ 58 ]. REBT approaches ADHD as a combination of neurobiological deficits [ 59 ] and developed secondary psychological personality disorders. Failure to develop cognitive structures leads to a lack of connection between thoughts, emotions and feelings, leading to deeply held distorted convictions and beliefs. The therapist’s role in this model is to assist the individual to dispute evaluative cognitions (“musts”) to develop a more rational philosophical orientation to the world. The approach incorporates independent “experiments” by clients outside of therapy, problem-solving methodology, and gentle introduction of rational self-statements for clients who lack the cognitive sophistication to engage in disputing of irrational beliefs [58, p. 95]. Treatment design has a developmental and longitudinal focus, in this case eight years. Characterisation of ADHD is described as DSM-IV core symptoms of attentional difficulties, impulsivity and hyperactivity [ 60 ] and references both Douglas’s [ 61 ] cognitive processing deficit model and Barkley’s [ 59 ] model of response inhibition and executive function deficits contributing to deficient self-regulation, impaired cross-temporal organisation of behaviour, and diminished social effectiveness and adaptation.
Second wave : Cognitive and cognitive behavioural therapy model . Cognitive and Cognitive Behavioural approaches are the primary and recommended treatment for working with ADHD and therefore make up the bulk of studies reviewed for this analysis. Considered “second wave” cognitive behavioural therapies, they consist of systematic reviews [ 2 , 37 , 38 , 41 ], randomised controlled trials (RCT) [ 62 – 80 ], group interventions [ 81 – 87 ], individual interventions [ 88 – 90 ], quantitative analysis [ 91 ], qualitative analysis [ 92 ], a cohort study [ 93 ], case-control studies [ 69 , 94 – 98 ], single case studies [ 99 – 102 ], multiple case studies [ 103 – 106 ], and psychotherapeutic treatment guidance [ 8 , 106 – 138 ]. Many of these studies deliver CBT as a standalone intervention, however multimodal treatment is recommended, and several treatment models include individual coaching or mentoring support alongside or in between CBT sessions [ 57 , 72 , 77 , 86 , 103 , 112 , 127 , 131 , 137 , 139 ]. One intervention also includes hypnosis and CBT [ 140 ].
Second wave interventions for ADHD recognise the neurobiological deficits as specific to the disorder and not brain injury. While they stress there is no “cure” for ADHD and the literature is clear that ADHD does not arise from distorted cognitions, cognitive treatment models focus primarily on improving, strengthening, or retraining cognitive abilities to increase awareness of behaviour and behavioural control. Early research identified cognitive distortions and maladaptive strategies and beliefs as interfering with skills acquisition and therefore needed support [ 104 , 136 ]. Further research shifted this view slightly to perceive the development of a negative self-concept as the core issue for maladaptive schema or “secondary symptoms” of stress, anxiety, depression, and chronic perceived failure attributed to a history of unachieved potential and negative feedback resulting from a lack of recognition of the disorder. [ 122 , 141 , 142 ]. Aims of treatment reduce deficit-based symptoms, develop environmental restructuring and accommodations, improve self-esteem and negative self-concept through disorder psychoeducation, and increase confidence in capabilities through supported skills practice and repetition. Approaches vary widely, including cognitive rehabilitation, cognitive and metacognitive remediation, and cognitive restructuring. However, most treatment approaches in this area are defined as Cognitive Behavioural Therapy (CBT) ( S1 Appendix ).
The therapists’ role in these models is more a “partner”, “expert teacher-motivator” [ 122 ] and collaborator than the traditional medical expert role [ 117 , 121 , 129 ]. Originally defined by Hallowell & Ratey [ 143 ] as “coaching”, therapists are encouraged to be active and directive in providing structure and redirection to goals or session topics [ 83 , 87 , 101 , 108 , 129 , 135 , 137 , 144 ]. Failure to initiate behavioural changes or maintain new habits and strategies, or “procrastivity”, is attributed to motivational problems due to the nature of the disorder [ 8 , 108 , 121 , 145 ]. CBT for ADHD identifies the ADHD client’s difficulty with delayed gratification and generation of positive emotions as the reason for lack of engagement or “Coping Drift”, where individuals stop implementing the skills taught in treatment [ 121 , 145 ]. Professionals are cautioned that repetition is key, and strategies must be reinforced, or relapse is likely. Therefore relapse prevention is included in practice as well as model design [ 8 , 70 , 71 , 74 , 83 , 86 , 93 , 94 , 108 , 121 , 126 , 136 , 145 , 146 ]. Recommendations for resistance or avoidance of aversive emotional states is to provide therapist support to develop tolerance [ 107 , 122 , 135 ], reframe past experiences [ 112 , 128 , 147 ], and build resilience when encountering setbacks [ 8 , 111 , 118 , 137 , 138 , 146 ]. Treatment designs are limited in length, either by the number of sessions (3 to 16) or by relevance (academic year) except for single case studies [ 99 – 102 , 104 ]. Intervention delivery methods vary from individual or group therapy and didactic teaching with therapeutic support to a computerised program and self-help manuals ( S1 Appendix ).
Characterisation of ADHD and aetiology highlight issues with attentional and behavioural control (hyperactivity, impulsivity, disorganisation) initially, but broadens to give a higher priority to executive dysfunction deficits, motivation and sustained attention, issues with emotional control and self-regulation. Guidance documents definitions of ADHD are often cited: of the 84 papers in this Second Wave analysis, 29 reference DSM-IV [ 60 ], seven reference DSM-IV-TR [ 148 ], and eight reference DSM-V [ 149 ]. Several studies reference alternative characterisations of ADHD, such as similarity to brain injury [ 117 ] and Brown’s Executive Function model [ 83 , 94 ]. However, Barkley is cited in 70 documents.
Third Wave : Mindfulness and acceptance . Third Wave cognitive behavioural interventions take a different treatment approach to traditional CBT. While they are similar in the practical application of behavioural techniques, they differ in their theoretical approach and the focus on cognitive change. Third-wave approaches explore context: the relationship between a person’s thoughts and emotions rather than content alone. This relationship includes a more holistic perspective of health beyond the reduction of disorders [ 53 ]. Therefore, this analysis will review them separately. These approaches include Metacognitive Therapy (MCT), Dialectical Behavioural Therapy (DBT), and Mindfulness Cognitive Behavioural Therapy (MCBT).
Metacognitive Therapy (MC) . Four documents used a metacognitive approach (MC), divided into group metacognitive therapy [ 5 , 76 , 150 ] and metacognitive remedial psychotherapeutic guidance [ 151 ]. Metacognitive interventions conceptualise ADHD as neurobiological dysfunction in the corticostriatal pathways, displayed as deficits in executive functions [ 151 ]. MC highlights the importance of awareness of cognitions or thinking about thinking to strengthen executive functions to enhance functioning and improve self-control. Borrowing from the psychoanalytic frame [ 152 ], treatment of this hybrid model aims to develop an “observing ego” or self-awareness, increasing the ability to be conscious of maladaptive thoughts and behaviours and confront them via self-analysis. The therapist’s role is to focus on cognitive and behavioural aspects of treatment and only address motivational or unconscious elements if they remain unexplained by neurobehavioural origins. Individual treatment plans are designed on a case-by-case basis to capture the individual’s unique problems and strengths. Analysis of authentic and emotionally charged experiences facilitates self-awareness using metaphoric problem identification, followed by strategy design and modification [ 151 ]. In group therapy, the therapist acts as an educator and facilitator, assisting with goal identification, the leading theme focused or problem assessment discussion, and offering support and encouragement [ 76 ]. Characterisation of ADHD focuses primarily on executive function deficits, followed by inattention and memory. This focus is reflected practically in treatment design as hyperactivity/impulsivity is considered less prevalent in adults [ 76 ]. Barkley is a primary citation in all four documents.
Dialectical Behavioural Therapy (DBT) . Ten studies identified an adapted model of Dialectical Behavioural Therapy (DBT) for ADHD. These consist of randomised controlled trials [ 21 , 153 – 155 ], a pragmatic open study [ 156 ], and group interventions [ 157 – 161 ]. This treatment model recognises ADHD neurobiological deficits but is grounded in a phenomenological conceptualisation, perceiving the nature of ADHD as a personality disorder. This conceptualisation is supported by similarities in symptoms and the positive response to the treatment of ADHD with comorbid Borderline Personality Disorder (BPD) [ 158 ]. Linehan [ 162 ] characterises BPD as a disorder of self-regulation from biological irregularities combined with dysfunctional environments, including their interaction and transaction. Experiences of invalidating environments impair childhood ability to learn to label experiences and emotions, modulate emotional arousal, tolerate distress, or form realistic goals and expectations, resulting in a child who invalidates their own experiences, generating a lack of self-trust. The adapted model is presented in group format of 13 weeks of 2-hour sessions. The design prioritises ADHD symptom-oriented modules, highlights non-empirically researched resources of ADHD [ 163 ], and includes DBT “mindfulness” training explicitly. The therapist’s role in the DBT adapted model for ADHD supports treatment aims of learning to “control ADHD—instead of being controlled by ADHD” through psychoeducation and provision of session structure and flexibility for individuals. A key therapist practice adopted from DBT is the dialectical balance between validating symptoms, aiming for a stabilising effect and encouragement of motivation, and skills training for behavioural change [ 158 ]. These models characterise ADHD as a deficit of attention and emotional control with hyperactive and impulsive behaviour, but later papers highlight issues with executive function and self-regulation [ 157 ]. Four studies cite Wender [ 164 ] as diagnostic criteria [ 153 , 158 – 160 ], two studies cite DSM-IV [ 154 , 155 ], and four studies cite Barkley specifically [ 21 , 156 , 157 , 161 ].
Mindfulness . Twenty-two documents included mindfulness in treatment options for ADHD. These included systematic reviews [ 42 , 165 – 167 ], randomised controlled trials [ 168 – 174 ], a pragmatic open study [ 156 ], group interventions [ 98 , 175 , 176 ], a case-control study [ 177 ], a multiple case study [ 178 ], and psychotherapeutic guidance [ 8 , 179 – 182 ]. Only two studies presented mindfulness treatment alone [ 98 , 156 ]. In Edel et al. [ 156 ], mindfulness was used as a comparator to DBT.
Mindfulness-based approaches conceptualise ADHD as a neurobiological disorder of self-regulation with deficits in executive function. Issues with sustained and selective attention are addressed by mindfulness meditation, which is presented as a self-regulatory practice recognised as mental training to strengthen and improve regulation of attention, emotions and brain function [ 167 , 175 , 177 , 181 ]. The therapist’s role is primarily to introduce and support developing the new skill set of “mindful awareness” or cognitive defusion to facilitate the ability to decrease emotional responses while continuing to act [ 8 ]. Interestingly, Zylowska’s [ 175 , 176 ] Mindfulness-Based Cognitive Therapy treatment model includes within its psychoeducation a characterisation of ADHD as a “neurobiological difference” with both evolutionary non-adaptive and potentially adaptive aspects [ 183 – 185 ]. However, within the treatment approach, the ADHD characterisation remains based on cognitive behavioural theory.
Treatment is in a group format, and length varies from 8 to 12 weeks of 2 to 3-hour sessions. The characterisation is reasonably consistent across this group, focusing primarily on poor sustained attention, inhibition and emotional dysregulation attributed to executive dysfunction, with one study highlighting impairments in performance monitoring [ 173 ]. Two papers cite DSM IV [ 42 , 168 ], two cite DSM V [ 167 , 170 ], and sixteen cite Barkley specifically [ 8 , 98 , 156 , 165 , 166 , 169 , 171 – 173 , 175 , 176 – 180 , 182 ].
Thirty-six documents presented coaching as a beneficial intervention for ADHD. These include a systematic review [ 186 ], a randomised controlled trial [ 187 ], individual interventions [ 188 – 199 ], qualitative studies [ 200 – 204 ], quantitative studies [ 205 – 207 ], and psychotherapeutic guidance [ 118 , 143 , 208 – 218 ]. It is important to note that nineteen studies were conducted at university for students, and therefore have academic goal achievement as a focus [ 187 – 195 , 197 – 199 , 201 , 204 , 206 , 208 , 212 ].
The term “coaching therapy” was coined by Hallowell and Ratey [ 143 ] to highlight the need for a therapist to take a more “active, encouraging role” with ADHD patients. The role of the “therapist-coach” was to provide a structuring force, maintaining focus and reminding patients of goals and objectives through directive interaction, as opposed to open-ended psychoanalysis. ADHD Coaching has since developed into an independent modality, which can be delivered alone or as part of a multi-modal approach. The ADHD Coaches Organisation (ACO) defines ADHD Coaching as a blending of three elements: Life Coaching, Skills Coaching, and Education [ 218 ]. Life coaching separates ADHD Coaching from therapy by highlighting the therapist-client relationship’s collaborative nature, where the coach supports client self-awareness and achievement of self-identified goals, providing structure and accountability as needed. The client is viewed as a creative and resourceful expert with individual strengths which are leveraged in skills coaching to design systems and strategies to strengthen clients’ ability to manage daily life. Education is provided through relevant ADHD research and tools, as requested by the client or as needed.
Conceptualisations of ADHD within coaching models focus almost exclusively on working with neurobiological deficits in executive function, with the primary treatment aim to set and achieve goals and develop skill sets to support practical day to day management. Some models even define themselves specifically as “Executive Function Coaching” [ 191 , 195 , 198 , 204 , 206 , 208 ]. However, some models highlight ADHD Coaching as based on or similar to CBT [ 186 , 196 , 199 , 208 ]. The role of the coach is to support clients to improve self-regulation, defined as the ability to persist in goal-directed behaviour through time [ 204 , 209 ], by modelling cognitive strategies, practising non-judgement, offering pragmatic support and guidance, and holding clients accountable by reflection in session or monitoring progress via between session check-ins. Negative emotions are addressed as barriers to goal achievement and confidence, but models are specific that ADHD coaching is practical [ 186 ], dealing with “what, when and how–never why” [ 213 ].
Six documents mention self-determination models as part of a wider ADHD Coaching treatment model [ 190 , 191 , 194 , 195 , 204 , 206 ]. These are functional theory models designed to assist students, particularly those with learning disabilities, to develop internal or dispositional characteristics of self-determined behaviour and goal acquisition [ 219 – 221 ]. Field & Hoffman’s model [ 221 ] defines self-determination as the ability to define and achieve goals grounded in knowing and valuing oneself, which can be supported or thwarted by internal variables and environmental factors. The model specifically focuses on internal controllable variables to assist individuals to adapt to environments with unpredictable support. The core theory is that to be self-determined, one must develop internal awareness and the skills and strength to act on this internal foundation. The model has five major components:
- “Know Yourself”: Increase awareness of one’s preferences, strengths, weaknesses and needs by “dreaming” or overcoming barriers in socialised expectations for individuals with disabilities that limit options and perceptions of self-efficacy, building on a foundation for self-determined decision making.
- “Value Yourself”: Develop affective variables of self-esteem, including identifying strengths in areas commonly perceived as weakness, supporting the self-acceptance of disability and motivation for self-advocacy, increasing the ability to be self-determined.
- Plan: Learn planning skills and visual rehearsal of creative and effective actions for short-range steps leading to long term goals.
- Act: Awareness of how to assertively communicate goals, desires and intentions to others and access relevant resources. Understanding persistence, negotiation, and conflict resolution around risk-taking and barriers that may result from taking action.
- Experience Outcomes and Learn: Learn skills in evaluation of progress based on experience of change and comparison to expected outcomes. Recognition and celebration of successes crystallises the self-determination process.
Wehmeyer et al.’s model [ 219 , 222 ] is a teaching model to help students become causal agents. Based on cognitive behavioural theory [ 223 , 224 ], social cognitive theory [ 225 ] and research in self-management and self-control [ 226 ], this model defines self-determination as the abilities necessary to act as one’s primary causal agent and make choices and decisions about the quality of life free from external influence and interference [ 227 ]. Developed from a model designed to teach students decision making, independent performance, self-evaluation, and adjustment skills, the updated model includes defining those who are self-determined to persistently regulate problem-solving to meet self-directed personal goals using student-directed learning strategies [ 219 ]. This ability is developed through a learned problem-solving sequence of thoughts and actions to reduce the discrepancy between what students want or need and what they have or know. The sequence requires the students to 1) identify the problem; 2) identify potential solutions; 3) identify barriers to solving the problem; and 4) identify consequences to each solution, thereby enabling the student to regulate problem-solving by setting goals to meet needs, constructing plans to meet goals, and adjusting actions to complete plans [ 219 ]. A comprehensive combined curriculum of these frameworks was later developed [ 220 ]. While they provide support for client autonomy and causal agency within the design of these ADHD Coaching models, these models prioritise goal setting and identification as regulators for human behaviour and recommend student-directed learning strategies based on operant psychology, applied behavioural analysis and positive reinforcement techniques. Thus, treatment approaches for ADHD remain based on cognitive behavioural theory.
Treatment approaches in ADHD Coaching models are primarily cognitive behavioural, including reframing negative self-talk [ 228 ], continuous reinforcement [ 189 , 209 ], implementing rewards and consequences [ 188 , 189 , 192 , 196 , 212 ], and between-session assignments [ 192 , 196 , 209 , 217 ]. These models focus on the characterisation of ADHD as deficits in executive function relating to goal-directed behaviour, disorganisation and planning, motivation, and ultimately self-regulation. Citations for characterisation in ADHD Coaching models include one referencing DSM IV [ 211 ], three reference DSM-IV-TR [ 191 , 202 , 214 ], one reference to Brown’s Executive Function Model [ 195 ], and twenty-eight reference Barkley specifically [ 118 , 128 , 143 , 186 , 188 , 189 , 191 – 194 , 196 – 201 , 203 – 207 , 209 , 212 , 214 – 218 ].
Other interventions.
Fourty-seven documents describe non-pharmacological interventions not based on psychotherapy. These include Neurofeedback, Transcranial Stimulation, Hypnotherapy, Light Therapy, Computer-Based, Mentoring, Self-Monitoring, Binaural Beat Auditory Stimulation, and Movement-related interventions.
Neurofeedback . Twelve documents explored Neurofeedback as an intervention for ADHD. These include randomised controlled trials [ 229 – 231 ], individual interventions [ 232 , 233 ], case-control studies [ 234 , 235 ], a single case study [ 236 ], and treatment guidance [ 118 , 237 – 239 ]. Neurofeedback (NF) treatment models focus heavily on neurocognitive deficits as being the origin of ADHD behaviours. The research uses Electroencephalography (EEG) measures to study the correspondences between intracranial electrical currents and responding voltages on the scalp. These measures indicate aspects of brain electrical function and processing, such as the electrical activity of various brain regions and their response to stimuli during cognitive tasks. EEG activity is quantified by computation of amplitude and power values for specific frequency bands of activity, source localization, and brain electrical activity mapping. Frequency refers to the number of oscillations, or waveforms, within a given time period. Analysis of waveforms, or a mixture of frequency bands, is a relational and complex process of examining frequency bands associated with both regions of the brain and cognitive or behavioural characteristics.
Characterisations of ADHD are presented as disturbances in cortical arousal, executive function, and self-regulation. Theta/beta and theta/alpha waveform ratios (TBR) are considered a measure of differences in excess, slow-wave activity and epileptiform spike and wave activity [ 240 ], interpreted as abnormal brain processes indicating cortical under arousal, insufficient inhibitory control, and maturational delay in ADHD [ 241 ]; however recent studies have challenged TBR as a marker for ADHD diagnosis [ 235 ]. Sensory-motor rhythm (SMR) or low beta waveform ratios are thought to indicate cortical hypo-arousal, interpreted as deficiencies in the early stages of information processing [ 230 ]. Decreased contingent negative variation (CNV), a steady, slow, negative-going waveform associated with cognitive energy in anticipation of task performance, is considered indicative of dysfunctional regulation of energetical resources in ADHD [ 234 ].
Based on research in children, two treatment approaches reflect changes in the conceptualisation of ADHD and, therefore, treatment aims. Traditionally, the focus of treatment has been based on a “conditioning and repair model” [ 242 ]. Treatment aims to address dysfunctions and see behavioural improvement and remediation of symptoms following NF application [ 243 ]. Skill acquisition and learning are implicit, automatic, and unconscious. Changes in activity indicate positive results: the ability to decrease slow-wave activity (theta) and/or increase fast wave EEG activity (beta) should correlate with symptom improvement; or modulation of slow cortical potentials (SCP), changes of cortical electrical activity, indicate improved cortical regulatory processes [ 244 ]. The role of the therapist is to act as a model for affect regulation [ 236 ] as well as use behavioural principles such as operant conditioning (i.e., positive reinforcement) in the training process resulting in normalisation and stable change in resting EEG, or “EEG trait” [ 245 ], and behaviour [ 231 , 233 , 234 ].
More recently, the NF treatment focus has developed into a “skills acquisition model” [ 242 ]. Rather than simply improving neuropsychological deficits, it is thought that NF may be used as a tool for enhancing or optimising specific cognitive or attentional states [ 246 , 247 ]. This model recognises the bio-psycho-social model of neurodevelopmental disorders, characterising ADHD as impairments in attention, executive functions and self-regulation [ 229 , 230 ]. In this model, self-regulation, or neuro-regulation, is defined as explicit learning of controlled cognitive processes of cortical regulation evidenced by normalised shifts in EEG amplitudes [ 242 , 248 , 249 ]. Performance optimisation is evidenced by improved skill in changing the “EEG state” via self-initiated effort during task performance [ 243 , 250 ]. The therapist’s role is to use cognitive behavioural therapy elements such as positive feedback and coaching and operant procedures as active support within treatment sessions to enhance self-efficacy and self-confidence to support neuro-regulation [ 244 , 251 ]. Citations for characterisation of ADHD in NF models include two citations for DSM-IV-TR [ 231 , 238 ], two for DSM -V [ 232 , 233 ], one for Sonuga-Barke’s Delay Aversion Model [ 237 ], three for Sergeant’s Cognitive-Energic Model [ 230 , 234 , 237 ], and four citations for Barkley [ 118 , 229 , 237 , 239 ].
Transcranial stimulation . Four documents present Transcranial Stimulation as a treatment approach for ADHD. These include a systematic review [ 252 ], two randomised controlled trials of Transcranial Direct Stimulation (tDCS) [ 253 , 254 ], and a randomised controlled trial of Transcranial Magnetic Stimulation (rTMS) [ 255 ]. Both forms of transcranial stimulation conceptualise ADHD as a neurobiological disorder with deficits in executive functions, including attention, working memory, impulsivity, and inhibitory control. The treatment aims to increase cortical excitability in the area of stimulation, leading to improved neuropsychological and cognitive functions.
Treatment approaches are non-invasive but differ in their application. Transcranial Magnetic Stimulation uses a coil placed on the subjects head to deliver brief, intense pulses of current (up to 50 Hz) to generate a sizeable electromagnetic induction field initiating neurotransmitter release in the cortex and subcortical white matter of the brain [ 255 , 256 ]. Transcranial Direct Current Stimulation uses conductive sponge electrodes applied to the scalp in specific locations to deliver a weak electrical current (1–2 mA or milliamps) for up to 20 minutes. It is hypothesised that the electrical current changes the polarisation of the neurons, affecting their average level of discharge [ 253 , 254 , 256 ]. Multiple treatments are administered daily for 3–4 weeks. Protocols suggest two applications of stimulation: “online”, or while a patient is completing a task, or “offline” where the treatment is applied before or without specific targeted tasks. Citations for characterisation of ADHD in these models include DSM-IV [ 252 ], DSM-IV-TR [ 254 ], DSM V [ 255 ] and Barkley [ 253 ].
Hypnotherapy . Two RCTs examined hypnotherapy as a treatment approach for ADHD [ 74 , 257 ]. These studies conceptualise ADHD as a developmental neurobiological disability with deficits in attention, issues with hyperactivity/impulsivity and problems in executive function, including processing speed, regulating alertness, modulating emotions, and utilizing memory. Treatment aims to improve symptoms, mood, quality of life and cognitive performance. Treatment design is based on symptoms outlined in the DSM-IV and Brown’s Executive Dysfunction Model [ 258 ]. The therapist’s role was to follow a semi-structured manual to review the previous session, present the theme for the current session, perform induction and guided hypnotherapy with a post-hypnotic suggestion, and lead discussion. Treatment length was ten weekly sessions of 40 to 60 minutes. Citations for characterisation of ADHD were the DSM-IV [ 257 ] and Brown’s Executive Dysfunction Model [ 74 ].
Light therapy . Five documents present light therapy as a treatment approach for ADHD: a systematic review [ 259 ], an individual intervention [ 260 ], a quantitative study [ 261 ], a literature review [ 262 ], and treatment guidance [ 263 ]. These documents conceptualise ADHD as a neuropsychiatric disorder with primary symptoms of impulsivity, inattention, and hyperactivity impacted by mood regulation difficulties, maintaining arousal and sleep disturbances that contribute to pathophysiology. This conceptualisation is supported by links between ADHD, seasonal affective disorder (SAD) and circadian rhythms and highlighted by similarities in symptoms between sleep deprivation and ADHD [ 261 , 263 ]. Research indicates abnormalities in circadian related physiological measures such as heart rate increase relevant to autonomic function, dysregulation in melatonin rhythm leading to delays in melatonin onset, which may affect the modulation of the sleep/wake cycle [ 263 , 264 ], as well as some evidence of low cortisol impacting wakening times [ 259 ]. Also, a later diurnal preference, or evening chronotype, is highly prevalent in the ADHD population. Its association with shorter night sleep periods is believed to generate sleep debt, delay the sleep phase, and exacerbate symptoms or potentially play a causal role in ADHD symptoms [ 262 , 263 ].
Light Therapy (LT) treatment aims to assist with phase-shifting abnormal circadian rhythms through light exposure to achieve sleep onset to improve alignment with work, academic, or social norms. Treatment outcomes are improved sleep and improved ability to maintain effort, arousal and attention [ 260 , 262 ]. The treatment has been trialled as a three-week self-administered daily dose of 10,000 lux at a distance of 24 inches using a full-spectrum fluorescent lightbox [ 260 ]. Citations for the characterisation of ADHD in these documents include DSM-IV [ 260 ], DSM-V [ 259 ], Douglas [ 262 ], Brown’s Executive Dysfunction Theory [ 261 ], and Barkley [ 261 ].
Computer-based interventions . Eight documents presented computer-based interventions as a treatment approach for ADHD. These include randomised controlled trials [ 265 – 268 ], individual interventions [ 269 , 270 ], and case-control studies [ 271 , 272 ]. These approaches characterise ADHD as a neurobiological disorder with executive function deficits, including difficulties in sustained attention, response inhibition, goal persistence, and working memory. Computer-based interventions take two approaches: supportive or training. Supportive interventions aim to target specific symptoms and facilitate functioning via supportive software. Individuals are given access to tools used independently following training for a set timeframe. In Hecker et al. [ 271 ], a software tool designed to reduce internal and external distractions aimed to reduce effort and improve engagement, resulting in increased time reading and comprehension. In Irvine [ 269 ], a smartphone app for time management aimed to reduce the discrepancy between the perception of time and actual time spent by providing immediate real-time feedback on the current status and time use, leading to adjustments of future tasks according to behavioural therapeutic principles.
Training interventions aim to strengthen cognitive skills and/or remediate deficiencies via cognitive behavioural learning strategies of repetition and positive reinforcement. Working Memory Training [ 265 , 266 , 268 ] aimed to enhance auditory-verbal and visual-space working memory through intensive training with increasing task difficulty leading to improved cognitive and academic performance and attentional self-regulation. Cognitive ability training [ 272 ] aimed to improve cognitive skills of decision making, attention, organisation and time management through simulated activities in a gaming environment, providing immediate real-time rewards. Cognitive training for executive function [ 267 , 270 ] aimed to remediate cognitive processes deficiencies by repeated and graded exposure to neutral and universal stimuli and feedback. Training is self-administered, hierarchical and adjusted to individual performance with outcomes for improvements in daily executive functioning, occupational performance, and quality of life. Treatment length varied in frequency and intensity, from 20-minute sessions 3–5 times a week for 12 weeks to 45-minute sessions five days a week for five weeks and included weekly check-ins or supportive coaching. Citations for characterisation of ADHD in these approaches include DSM-IV [ 265 , 266 , 268 , 270 ], DSM V [ 271 ], Brown’s Executive Dysfunction Model [ 267 , 270 ], Nigg’s Integrative Theory [ 267 ], and Barkley [ 266 , 267 , 269 , 270 ].
Mentoring . One study presented mentoring as an individual intervention for ADHD [ 273 ]. Based in a university environment, ADHD is characterised as deficits in basic cognitive skills, such as attention, concentration, and memory and higher-level cognitive skills or “executive functioning”, such as planning, organization, judgment, problem-solving, and cognitive flexibility. These can negatively affect the university experience, as more independent self-management and a complex skill set are required for success, particularly time management and organization, academic skills, and social skills.
The mentoring program pairs second-year master’s level occupational therapy (MSOT) students (mentors) with undergraduate college students (mentees) for one-to-one support twice weekly for 2-hour sessions in the fall and spring semesters. This mentoring is a credit-bearing course that addresses skill development in time management and organization, academic skills, and social skills for college success. Mentees are graded on attendance, professional behaviours, compliance on a weekly to-do list, a presentation on academic resources, and a 4-part written paper on an academic skill. Mentors are participating as part of a professional Occupational Therapy training programme with an overall goal to facilitate student success in college, and if factors overwhelmingly interfere with this goal, to identify an alternate, suitable plan. As part of the training, mentors meet in discussion groups to brainstorm ways to overcome the mentoring process’s challenges. The citation for the characterisation of ADHD in this intervention is primarily the DSM V [ 273 ].
Self-monitoring . One study presented individual self-monitoring as an intervention for ADHD [ 274 ]. Based in a university environment, ADHD is characterised as a neurobehavioral disorder with symptoms of inattention, hyperactivity, and impulsivity, which increases the risk of academic failure or underachievement.
A checklist tool is co-designed and supported with integrity checks and email reminders every 2–4 days, with face-to-face check-in sessions every two weeks. The self-monitoring intervention aims to teach participants to observe and record behaviours to change the behaviour in the future. Outcomes are to obtain higher grades, endorse fewer ADHD symptoms, engage in more positive study skills, further attain goals, and improve medication adherence. Citations for characterisation of ADHD is DSM IV [ 274 ].
Binaural beat auditory stimulation . Two documents present binaural beat auditory stimulation as a treatment for ADHD. These include an individual intervention [ 275 ] and a literature review [ 276 ]. These approaches characterise ADHD as a disorder with core deficits in behavioural inhibition and sustained attention, highlighting a decrease in beta wave states interfering with maintenance of attention as a contributing factor.
Binaural beat auditory stimulation generates tones of two frequencies presented separately in each ear which are synthesised by the medulla into a single low-frequency tone. The pulse frequency from this binaural beat is the difference between the two tones and generates electrical activity that EEG can record. Treatment aims to match the difference between the tones to a particular brain-wave state, such as the beta range, which will correspondingly be maintained by overall brain activity and affect cognition levels [ 277 ]. Treatment involves exposure to auditory stimulus via headphones during an active task. Citations for characterisation of ADHD only directly reference Barkley [ 275 ].
Movement-related interventions . Twelve documents present movement-related interventions as a treatment for ADHD, including a systematic review [ 278 ], a pilot study [ 279 ], case-control studies [ 280 – 285 ], and treatment guidance [ 286 – 289 ]. In these approaches, ADHD is a disorder with core issues in special working memory, attention control, response inhibition, motor control, delay aversion, emotional self-regulation, and executive dysfunction. Movement-related interventions approach treatment in two ways: passive and active.
One document presented a passive intervention. Whole Body Vibration (WBV) devices deliver sinusoidal or oscillating wave vibrations at low frequencies to enhance mechanical muscular performance [ 290 ], improve balance and proprioception [ 291 ], and increase vigilance [ 292 ], potentially by inducing muscle contractions and increasing tension through the stretch reflex. Treatment is passive, delivered while sitting still, and aims to improve attention, inhibitory control, and cognitive performance in ADHD [ 280 ].
Active movement-related interventions aim to improve neurobiological factors such as increased cerebral blood flow, enhance neuroplasticity [ 288 , 289 ], assist the development of cortical and subcortical brain regions through activity [ 287 ], reduce the impact of comorbid anxiety, depression, stress and negative affect [ 279 , 288 ], and improve cognitive function and performance [ 282 – 286 ]. There is a specific focus on hypodopominergic functioning in ADHD and the upregulation of a brain-derived neurotrophic factor (BDNF) protein in several studies. [ 281 , 283 , 286 , 288 , 289 ]. Research shows that BDNF is linked to differentiation and survival of dopaminergic neurons, and decreased levels of BDNF have been suggested as being involved in ADHD pathology [ 293 ]. As well as improved cognition, one of the benefits of acute exercise is elevated levels of BDNF, which these models argue makes exercise an important intervention for ADHD. Treatment varies both in approach and length, from vigorous physical activity for 30 minutes, such as cycling, to fine motor movement stimulation using an anti-stress ball during a task. Citations for the characterisation of ADHD in these approaches include DSM IV [ 287 ], DSM V [ 285 ], Nigg [ 281 , 286 ], Sergeant [ 282 ], Sonuga-Barke [ 282 , 286 ], and Barkley [ 278 – 280 , 283 , 284 , 286 , 288 , 289 ].
Alternative models.
Psychoanalysis and Psychodynamic . There are very few studies in Psychoanalysis and Psychodynamic approaches for adult ADHD. A group intervention [ 294 ], single [ 295 , 296 ] or double case studies [ 297 – 299 ] were reviewed, as well as an evaluation study [ 300 ]. Much of the literature consists of literature reviews [ 35 , 301 – 304 ] and guidance pieces [ 152 , 305 , 306 ], which demonstrate considerable debate in the characterisation and aetiology of ADHD. Early papers reflect issues in clinical approaches by highlighting the importance of considering ADHD diagnosis as defined by DSM-IV in light of epidemiological evidence [ 301 , 307 ]. Both Psychoanalysis and Psychodynamic approaches present alternative models to Barkley, with distinct variation in characterisation.
Historically, Psychoanalysis does not recognise neurobiological deficits. Behaviours associated with ADHD are conceptualized as disturbances in the ego, identified as the organising force responsible for synthesis and integration of internal and external stimuli, internalisation of object relations and structure and development of the superego, and integral to facilitating the capacity for self-observation and self-reflection. Early presentations of these disturbances in childhood lead to attachment issues and interfere with sibling relationship development [ 301 ]. Behaviours are perceived as defence mechanisms, identified as an internal struggle for control [ 296 , 300 ]. Psychodynamic perspectives differ in that behaviours are conceptualized as a reaction to neurobiological deficits [ 152 , 302 , 306 ], facilitating engagement with Barkley’s model. Executive functioning deficits are presented as synonymous with self-regulation deficits, interfering with the development of personality structure and an internal representation of self about others. Self-regulation deficits disrupt the ability to empathise, which distorts the capacity to mentalise and develop a coherent sense of self [ 304 ].
The therapist’s role in these models is to act as the organising force for the client, assisting them to develop ego capacities via therapeutic relationship and transference. This enables the client to experience empathy, recognise mental states, and identify self in relation to others [ 35 , 301 , 304 ]. With the exception of the group intervention [ 294 ], treatment designs are intensive, up to four times a week [ 301 , 304 ] and long term, between 2 and 12 years [ 295 , 296 , 298 , 301 , 304 ]. Despite the alternative model to characterise ADHD, four studies reference international guidance [ 297 , 301 , 302 , 307 ], seven studies mention executive function or cognitive control [ 35 , 152 , 295 , 297 , 299 , 304 , 306 ], and seven reference Barkley specifically [ 35 , 294 , 295 , 297 – 299 , 304 ].
A review of 221 documents confirmed that treatment approaches for ADHD are based on a dominant cognitive behavioural paradigm for conceptualising ADHD, which attributes symptoms solely to neurobiological and developmental deficits leading to challenges with cognitive function, behavioural control, and management of self-regulation. This is reflected in descriptions of treatment aims, approaches and outcomes ( S1 Appendix ).
While this scoping review aimed for as broad a scope as possible, it is important to acknowledge the limitations of this study. First, while translation services were used as much as possible, the material identified in the results were primarily published in English. Further, the majority of the documents presented were published in the US, Canada and European countries. This may be due to documents being presented or published by journals not listed by the major search engines, and therefore not identified in the search strategies. Alternatively, there may not be a large existent body of published research in other countries, as the official diagnosis criteria for adults with ADHD was only recognised in 2013 [ 149 ]. Secondly, this scoping review was an enormous undertaking, and results are only up to date as of April 2020. However, searches did not reveal any other recent reviews of the theoretical charactarisation of ADHD, therefore it is believed this is the most current comprehensive scoping review on the topic.
This review reflects current research understanding that ADHD is complex and multidimensional in its presentation and impact. Clearly, it shows a broad, cross-disciplinary interest in developing treatment approaches to support individuals with ADHD to reduce symptoms, improve functioning and achieve a better quality of life. Critically, it highlights that a single theoretical perspective limits research into effective treatments for ADHD. Existing aetiological theories of ADHD have been challenged for their refutability [ 308 ], and other issues such as accounting for context variability, or inability to fully link or account for the full aspects of the symptomology [ 19 – 21 ], and heterogeneity [ 1 , 22 – 24 ] including specific links between domains and outcome [ 22 ] and cognition and motivation to select actions for a given context [ 309 ]. Recent recommendations for resolving challenges with heterogeneity in ADHD emphasise the importance of theoretical guidance in decision-making and recognise the critical role of beliefs, assumptions, and goals in preventing misapplication of conclusions to clinical circumstances or populations [ 1 ]. It is proposed that treatments based on approaches from a singular perspective on processes of self-regulation and a deficit-based origin of impairments in ADHD may be limited in scope and capacity to identify and support positive psychological factors for well-being and growth. Hence, the findings in this scoping review identify a gap in research and practice for alternative theoretical perspectives of ADHD.
This review concludes that further research into additional theoretical models of self-regulation would provide opportunities to develop alternative treatment approaches and benefit research and understanding of the symptomology of ADHD.
Supporting information
S1 appendix. analysis of treatment approaches..
https://doi.org/10.1371/journal.pone.0261247.s001
S1 File. PRISMA scoping review checklist.
https://doi.org/10.1371/journal.pone.0261247.s002
- View Article
- Google Scholar
- PubMed/NCBI
- 6. Barkley RA. Executive functions: What they are, how they work, and why they evolved. New York, NY: Guildford Press; 2012.
- 7. Brown TE. A new understanding of ADHD in children and adults: Executive function and impairments. New York, NY: Routledge; 2013.
- 8. Ramsay JR. Rethinking adult ADHD. Washington D.C.: American Psychological Association; 2020.
- 11. Barkley RA. ADHD and the nature of self control. London: Guildford Press; 1997.
- 18. NICE, editor. Attention deficit hyperactivity disorder: diagnosis and management. In National Institute for Health Care and Excellence; 2019. Available from: https://www.nice.org.uk/guidance/cg72
- 19. Brown TE. Differential diagnosis of ADD versus ADHD in adults. In: Nadeau KG, editor. A comprehensive guide to attention deficit disorder in adults. New York: Brunner/Mazel Inc.; 1995. p. 93–108.
- 20. Brown TE. Smart but stuck: Emotions in teens and adults with ADHD. San Francisco: Jossey-Bass; 2014.
- 26. Liberman RP. Recovery from disability: Manual of psychiatric rehabilitation. Arlington, VA: American Psychiatric Publishing, Inc.; 2008.
- 30. Aromataris E, Munn Z. Johanna Briggs Institute reviewer’s manual. The Joanna Briggs Institute. 2017.
- 31. Hartmann T, Popkin M. ADHD: a hunter in a farmer’s world. Rochester, Vermont: Healing Arts Press; 2019.
- 32. Weiss L. Embracing ADHD: A healing perspecive. Lanham, MD: Taylor Trade Publishing; 2015.
- 33. Maté G. Scattered minds: The origin and healing of Attention Deficit Disorder. London, UK: Vermilion; 1999.
- 34. Amen D. Healing ADD: The breakthrough program that allows you to see and heal the 7 types of Attention Deficit Disorder. New York, NY: Berkley Publishing Group; 2013.
- 55. Wood RL. Head trauma rehabilitation: A neurobehavioural approach. London: Croom Helm; 1987.
- 56. Jordan DR. Attention Deficit Disorder: ADHD and ADD syndromes. Third. Austin, TX: Pro-Ed; 1998.
- 58. Yankura J, Dryden W. Using REBT with common psychological problems: A therapist’s casebook. New York: Springer Publishing Co.; 1997.
- 59. Barkley RA. Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment. New York: Guildford Press; 1990.
- 60. American Psychiatric Association. The diagnostic and statistical manual of mental disorders. 4th ed. Washington D.C.: American Psychiatric Association; 1994.
- 61. Douglas VI. Higher mental processess in hyperactive children: implications for training. In: Knights RM, Bakker DJ, editors. Treatment of hyperactive and learning disordered children. Baltimore: University Park Press; 1980. p. 65–92.
- 108. Safren SA, Perlman C, Sprich S, Otto M. Mastering your adult ADHD. New York: Oxford University Press; 2005.
- 111. Young S, Bramham J. ADHD in adults: a psychological guide to practice. Chichester, West Sussex: John Wiley & Sons, Inc; 2007.
- 112. Young SJ, Ross RR. R&R2 for ADHD youths and adults: a prosocial competence training program. Ottawa, Canada: Cognitive Centre of Canada; 2007.
- 118. Ramsay JR. Nonmedication treatments for adult ADHD. Washington D.C.: American Psychological Association; 2010.
- 121. Young S, Bramham J. Cognitive-behavioural therapy for ADHD in adolescents and adults: A psychological guide to practice. 2nd ed. Chichester, West Sussex: Wiley-Blackwell; 2012.
- 122. Knouse LE. Cognitive behavioural therapies for ADHD. In: Barkley RA, editor. Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment. 4th ed. New York: Guilford Press; 2014. p. 757–94.
- 125. Jeavons A, Bishop T, French B, Bastable S, Harpham-Salter A. The adult ADHD treatment handbook. Abington, Oxon: Routledge; 2018.
- 128. Nadeau K. The clinician’s role in the treatment of ADHD. In: Goldstein S, Ellison AT, editors. Clinician’s guide to adult ADHD: assessment and intervention. San Diego, CA: Academic Press; 2002. p. 107–26.
- 129. Nadeau KG. Life management skills for the adult with ADHD. In: Nadeau KG, editor. A comprehensive guide to attention deficit disorder in adults. New York, NY: Brunner/Mazel Inc.; 1995. p. 191–217.
- 130. Murphy K. Empowering the adult with ADHD. In: Nadeau KG, editor. A comprehensive guide to attention deficit disorder in adults. New York, NY: Brunner/Mazel Inc.; 1995. p. 135–45.
- 135. Young S. A model of psychotherapy for adults with ADHD. In: Goldstein S, Ellison T, editors. Clinician’s guide to adult ADHD: assessment and intervention. San Diego, CA: Academic Press; 2002. p. 147–63.
- 136. McDermott S. Cognitive Therapy for adults with attention-deficit/hyperactivity disorder. In: Brown TE, editor. Attention-deficit disorders and comorbidities in children, adolescents, and adults. Arlington, VA: American Psychiatric Publishing, Inc.; 2000. p. 569–606.
- 137. Murphy K. Psychological counselling of adults with ADHD. In: Barkley RA, editor. Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment. 3rd ed. New York, NY: Guildford Press; 2006.
- 138. Brooks RB. Changing the mindset of adults with ADHD: strategies for fostering hope, optimism, and resilience. In: Goldstein S, Ellison AT, editors. Clinician’s guide to adult ADHD: assessment and intervention. San Diego, CA: Academic Press; 2002. p. 127–46.
- 143. Hallowell E, Ratey J. Driven to distraction. New York: Touchstone; 1994. https://doi.org/10.1080/14640749408401099 pmid:7809399
- 145. Ramsay JR, Rostain AL. The adult ADHD toolkit. New York: Routledge; 2015.
- 148. American Psychiatric Association [APA]. The diagnostic and statistical manual of mental disorders. IV-TR. Washington D.C.: American Psychiatric Publishing, Inc.; 2000.
- 149. American Psychiatric Association [APA]. The diagnostic and statistical manual of mental disorders. 5th ed. Washington D.C.: American Psychiatric Association; 2013.
- 150. Solanto M V. Cognitive-behavioural therapy for adult ADHD. New York: Guildford Press; 2010.
- 157. Fleming AP, Fleming AP. Randomized controlled trial of group cognitive-behavioral therapy for ADHD among college students. University of Washington; 2013.
- 162. Linehan MM. Cognitive-behavioural treatment of borderline personality disorder. 14th ed. New York: Guildford Press; 1993.
- 163. Hartmann T. ADD: a different perception. Grass Valley, California: Underwood Books; 1997.
- 164. Wender PH. Attention deficit hyperactivity disorder in adults. New York: Oxford University Press; 1995.
- 182. Zylowska L. The mindfulness prescription for adult ADHD. Boulder, CO: Trumpeter; 2012.
- 189. Reaser AL. ADHD coaching and college students. Florida State University; 2008. https://doi.org/10.1111/j.1863-2378.2008.01123.x pmid:18399943
- 191. Farmer JL. The development of the Personal Strengths Intervention (PSI) to improve self- determination and social-emotional levels in postsecondary students with learning disabilities and/or ADHD: A multiple baseline study. [Internet]. Available in ProQuest Dissertations and Theses database. (UMI No. 3466210). 2011. Available from: http://search.ebscohost.com.proxy-ub.rug.nl/login.aspx?direct=true&db=psyh&AN=2012-99070-067&site=ehost-live&scope=site
- 195. Bomar R. The role of online academic coaching on levels of self-determination of college students with learning disabilities. Texas Woman’s University; 2017.
- 210. Nadeau KG. Non-medication treatments for women with ADHD: working with coaches and organizers. In: Nadeau KG, Quinn P, editors. Understanding women with ADHD. Washington D.C.: Advantage Books; 2002. p. 124–32.
- 211. Jaksa P, Ratey N. Therapy and ADD coaching: similarities, differences, and collaboration [Internet]. 1999 [cited 2016 Feb 7]. p. http://www.nancyratey.com/adhdcoaching/therapy-add . Available from: http://www.nancyratey.com/adhdcoaching/therapy-addcoaching
- 212. Quinn P, Ratey N, Maitland TL. Coaching college students with ADHD. Silver Spring, MD: Advantage Books; 2000.
- 213. Ratey N. Life coaching for adult ADHD. In: Goldstein S, Ellison AT, editors. Clinician’s guide to adult ADHD: assessment and intervention. San Diego, CA: Academic Press; 2002. p. 261–77.
- 217. Bowles VM. A survey of the methods and processes involved in interventions with ADHD clients from a psychologist and ADHD coach perspective. Florida State University; 2012.
- 218. Wright SD. ADHD coaching matters: the definitive guide. College Station, TX: ACO Books; 2014.
- 220. Wehmeyer ML, Field S. Self-Determination: instructional and assessment strategies. Thousand Oaks, CA: Corwin Press; 2007.
- 222. Mithaug DE, Wehmeyer ML, Agran M, Martin JE, Palmer S. The self-determined learning model of instruction: Engaging students to solve their learning problems. In: Wehmeyer ML, Sands DJ, editors. Making it happen: student involvement in educational planning, decision-making and instruction. Baltimore: Paul H. Brookes; 1998. p. 299–328.
- 223. Agran M, Martin JE. Applying a technology of self-control in community environments for individuals who are mentally retarded. In: Hersen M, Eisler RM, Miller PM, editors. Progress in behavior modification. Newbury Park, CA: SAGE; 1987. p. 108–51. pmid:3588360
- 224. Kanfer R, Goldstein AP. Helping people change: A textbook of methods. New York: Pergamon Press; 1986.
- 225. Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs: Prentice-Hall; 1986.
- 226. Martin JE, Burger D, Elias-Burger S, Mithaug DE. Applications of self-control strategies to facilitate independence in vocational and instructional settings. In: Bray NW, editor. International review of research in mental retardation. San Diego: Academic Press; 1988. p. 155–93.
- 258. Brown TE. Attention deficit disorder: The unfocused mind in children and adults. New Haven, CT: Yale University Press; 2005.
- 269. Irvine MJD. Outcome evaluation of a time management smartphone application: a pilot study [Internet]. George Fox University; 2013. Available from: http://digitalcommons.georgefox.edu/psyd/118
- 276. Peterson O. Rhythm as an intervention for health and mental health difficulties: a comprehensive literature review. Doctoral Thesis. Alliant International University; 2012.
ORIGINAL RESEARCH article
Experience of cbt in adults with adhd: a mixed methods study.

- 1 School of Psychology, University of Nottingham, Nottingham, United Kingdom
- 2 School of Health Sciences, University of Nottingham, Nottingham, United Kingdom
- 3 Institute of Mental Health, University of Nottingham, Nottingham, United Kingdom
- 4 School of Social Sciences and Humanities, University of Suffolk, Ipswich, United Kingdom
Introduction: The National Institute for Health and Care Excellence (NICE) recommends Cognitive-Behavioural therapy (CBT) as the psychotherapeutic treatment of choice for adults with Attention Deficit Hyperactivity Disorder (ADHD) in the UK. However, the literature often refers to adapted CBT programs tailored for ADHD and provides limited insight into how adults with ADHD experience and perceive this form of treatment in routine clinical practice.
Methods: This mixed-methods study aims to explore ADHD individuals’ experience and perception of CBT delivered in routine clinical practice, to gain a better understanding of this treatment’s helpfulness and perceived effectiveness.
Results: A survey (n=46) and semi-structured in-depth interviews (n=10) were conducted to explore the experience of CBT and its perceived effectiveness in managing ADHD. The interviews were analysed using thematic analysis and the survey was synthesised using descriptive narratives. The thematic analysis highlighted three key themes: difficulties with the CBT framework, difficulties with CBT therapists, and consequences of CBT. The survey highlighted similar findings. Participants described the CBT framework as, generic, rigid, and too short, and described the CBT therapist as unspecialised, unempathetic, and not sufficiently adapting CBT to ADHD-related difficulties.
Discussions: Overall, participants found non-adapted, generic CBT in the UK to be unhelpful, overwhelming, and at times harmful to their mental well-being. Therefore, it is necessary for clinical bodies in the UK, while following the indicated NICE guidelines, to be mindful of adapting CBT delivery of CBT, to be most effective for people with ADHD and to mitigate potential harm.
1 Introduction
Attention-Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental condition characterised by symptoms of persistent inattention and/or hyperactivity-impulsivity, that causes clinical impairment in academic and social functioning ( 1 ) affecting approximately 5% of children ( 2 ) and 2.5% of adults ( 3 ). While this suggests that ADHD attenuates over time, the prevalence of symptomatic adults is estimated to be 6.7% ( 3 ).
ADHD is centrally a disorder of impaired executive functions (EFs) creating a devastating effect on self-regulation ( 4 ), inhibition, planning and working memory ( 5 ). These impairments impact many different aspects of life such as education, employment and mental well-being ( 6 ) Barkley ( 7 ) argued that inhibition is the central EF impairment in ADHD, that hinders the utilisation of other functions. Moreover, a body of research reports significant deficits in the EFs of shifting and working memory for ADHD adults ( 8 – 10 ). Furthermore, Bailey & Jones ( 11 ) argued that the EF processes of inhibition, updating, and shifting are closely linked to emotional regulation. Henceforth, ADHD is also described as a disorder of emotional dysregulation ( 12 ). In a systematic review by Soler-Gutiérrez et al. ( 13 ), adults with ADHD demonstrated the consistent use of non-adaptive emotion regulation strategies when compared to controls. Bodalski et al. ( 14 ), also reported emotion regulation deficits in adults with ADHD including the use of avoidance strategies. Adults with ADHD demonstrate increased use of experiential and cognitive-behavioural avoidance strategies which mediates the relationship between ADHD, deficits in emotion regulation, and internalising disorder outcomes ( 14 ).
The National Institute for Health and Care Excellence ( 15 ) considers pharmacological treatment as the first-line treatment for adults with persisting ADHD symptoms. However, Ramsay ( 16 ) attests that individuals with ADHD who experience symptom improvement from medications still experience difficulties in academic and social functioning, due to ADHD’s high comorbidity with other psychological disorders, such as anxiety, depression, and substance abuse. For this reason, the NICE guideline (2018) recommends a structured psychological intervention in the form of cognitive-behavioural therapy (CBT) for individuals with ADHD as the first psychotherapeutic treatment of choice.
CBT is an umbrella term for a range of related therapies, including for instance cognitive therapy, behavioural therapy, and metacognitive therapy ( 17 ). These therapies share a strong commitment to developing clinical interventions grounded in empirical evidence, with CBT described as the most researched form of psychological therapy ( 18 ). The therapies encapsulated by the term CBT aim to reduce client’s experience of distress by helping the person to explore patterns in their behaviour, thinking processes and thought content, ( 19 ). Probably the most commonly practised form of non-adapted CBT in the UK, derives from a mixture of behavioural therapy principles and Beck’s cognitive therapy, to employ an active goal-oriented problem-solving approach ( 20 ). CBT is highly structured, present-oriented, and time-limited, usually lasting from 5–20 sessions ( 21 ). Typically, a CBT therapist may seek to address an individual’s cognitive distortions by challenging maladaptive core beliefs, dysfunctional assumptions, and negative automatic thoughts using techniques including Guided discovery, Socratic questioning, positive data logs, and thought records ( 21 ). Additionally, CBT therapists may employ behavioural techniques such as activity scheduling, where tasks are reduced to a controllable list, or behavioural experiments to try responding differently to identified situations or stimuli. The CBT therapeutic relationship is based on genuineness, rapport and empathy between the patient and the therapist ( 21 ).
In England, CBT is predominantly provided through the National Health Service (NHS) Increasing Access to Psychological Therapies Programme (IAPT), recently rebranded as NHS Talking Therapies for Anxiety and Depression (NHSTTAD). This programme was developed in 2008 in an attempt to radically increase the availability of CBT in primary care, in response to a range of NICE guidelines increasingly recommending CBT and other psychological therapies as the first-line interventions for anxiety and depression ( 21 , 22 ). This programme commissions a range of primary care psychological therapies services across England, with one-to-one CBT the most frequently provided therapy ( 23 ). Therapists are trained in accordance with a competency-based curriculum ( 24 ), which does not include specific content on adapting CBT for ADHD. This potentially leads to therapists having high variability in their knowledge, skills and ability to support ADHD patients. Access to NHSTTAD services is often by self-referral, with no separate formal diagnostic assessment of presenting problems required as a precursor to treatment. While the NHSTTAD programme is mainly designed for individuals with mild to moderate depression and anxiety, therapists working in NHSTTAD services often find they are working with complex cases, for which they may have insufficient training and knowledge ( 22 ) including ADHD. According to Ramsay ( 4 , 25 ), individuals with ADHD often seek treatment for comorbid depression and/or anxiety, therefore they may be highly likely to receive CBT treatment through the NHSTTAD service. Whilst statistics of the number of people accessing NHSTTAD who have an existing ADHD diagnosis, or who experience ADHD-related difficulties are not recorded, more than thirty-three thousand people seeking help from NHSTTAD services during the year 2021–22, were assessed as experiencing problems with memory, and concentration, learning and understanding ( 26 ).
Previous evidence from empirical studies reported that adults with ADHD found adapted CBT helpful for their symptoms ( 27 , 28 ). Virta and colleagues ( 27 ) reported a pilot RCT of short-term outpatient adapted CBT to adults with ADHD (n=10), delivered over 10 weekly appointments. Participants in this study reported significantly reduced symptoms as a result of engaging in adapted CBT. Two patients (20%) dropped out of adapted CBT. Solanto and Scheres ( 28 ) reported a cohort study of adapted CBT for college students (n=18) delivered in a group format, over 12 weekly sessions. Clinician’s ratings and participants’ self-report data evidenced a reduction in ADHD symptoms and student’s perceived self-efficacy in managing ADHD. One participant dropped out of group adapted CBT. These studies suggest that adapted CBT is acceptable to ADHD patients.
Numerous studies have also highlighted the efficacy of adapted CBT in reducing symptoms of ADHD and EF ( 27 – 31 ) as well as mental well-being and general functioning ( 32 , 33 ). A randomised controlled trial by Safren et al. ( 34 ) highlighted the efficacy of an ADHD-adapted CBT treatment in providing significantly better outcomes for participants over an active control treatment based on relaxation and educational support. Additionally, studies comparing CBT to treatment as usual control groups, have shown the treatment’s efficacy compared with medication-only groups ( 35 , 36 ). A meta-analysis by Knouse et al. ( 37 ) reported that studies with active control groups indicated significantly smaller effect sizes for CBT treatment, than studies without active controls. The differences in these results could be due to variations in the CBT interventions applied in each study, which varied by treatment type, format, length, and the medication status of the participants, which can arguably moderate the effect of treatment ( 37 ). Finally, Solanto and Scheres reported the effectiveness of a CBT program in reducing inattention and EF in college student with ADHD.
Additionally, there are a number of studies which have shown the efficacy and acceptability of adapted Dialectical Behaviour Therapy (DBT) for ADHD patients ( 38 – 43 ). DBT ( 44 ) is an empirically validated approach for working with distress tolerance and coping behaviours. Early DBT papers focused on reducing self-harm and suicide attempts in individuals diagnosed with personality disorder ( 45 ), whereas more recent work has applied modified DBT to diagnostically heterogenous groups ( 46 ). DBT is often considered part of the ‘third wave’ of CBT, given its focus on emotional and behavioural regulation ( 47 ). As applied to ADHD treatment, adapted DBT includes acceptance, mindfulness, functional behavioural analysis, psychoeducation and distress tolerance techniques ( 42 , 43 ). Many of the studies of adapted DBT for ADHD, have utilised group level interventions ( 38 – 43 ). The reliance on group interventions is at odds with the dominant model of one-to-one CBT used within NHSTTAD services. Furthermore, within the English context, DBT is a psychological therapy approach rarely delivered within primary care in England, given low numbers of DBT trained therapists and supervisors. The English NHS has plans to rapidly expand the availability of DBT by commissioning additional training ( 48 ), but there are still few DBT trained practitioners working with primary care populations.
Moreover, it is important to note that the majority of studies reporting on the efficacy and acceptability of CBT, have delivered ADHD adapted DBT or adapted CBT, rather than generic CBT, which is essential for treatment efficacy but the title and often content of these studies do not always reflect this important nuance. Ramsay ( 4 ) suggested the adaptation of CBT to accommodate for the executive and emotional dysfunctions experienced by adults with ADHD, using environmental engineering and EF training. This entails changing work, home, and personal settings by implementing systems to lessen dysfunction as well as delivering organisation and time management skills, ( 4 ). As adults with ADHD often have a history of negative experiences related to their EF deficits, which may foster negative cognitions about themselves or their abilities and maladaptive emotional strategies, these must be addressed in CBT to motivate change and encourage appropriate coping ( 4 , 19 ).
Knouse & Ramsay ( 49 ) argued that non-adapted CBT could be harmful to adults with ADHD, as negative experiences of therapy can occur in relation to the experience of therapy in interaction with ADHD symptoms and individuals’ sense of self. While the benefits can outweigh the negative experiences, therapists must be aware of the possibility of certain negative experiences which might occur during all stages of a CBT treatment course, and any such experiences of therapy must be managed appropriately to reduce harm and barriers to treatment.
CBT therefore appears an efficacious treatment for people with ADHD, yet one that could cause side effects, or iatrogenic harm, if not delivered in a way that is responsive to the needs of people with ADHD. However, the existing literature provides limited indepth, qualitative insight as to how adults with ADHD experience and perceive CBT treatment. In response to this gap in the literature, the present mixed-methods study aims to record and collate the CBT experiences (adapted or non adapted) of adults with ADHD, to capture and analyse the perceived impact of this form of therapy and its value for ADHD individuals. A mixed-method approach lends itself well in capturing user experiences and understanding social phenomena better ( 50 ). This study aims to explore the following research question, ‘How do individuals with ADHD experience CBT therapy in the UK?’
An explanatory sequential mixed methods design ( 51 ) was employed, consisting of an online survey, followed by in-depth, semi-structured interviews with a sub-sample of survey respondents. The survey data was collected over 3 months (June-August) in 2023. Interviews were conducted and recorded over one month in August 2023. The survey and interviews took place online and followed data protection procedures and best practices for record-keeping, and storage of personal data, in accordance with the BPS Code of Human Research Ethics ( 52 ). The study received ethical approval from the University of Nottingham School of Psychology (ethics reference number: FMHS 81–0922).
2.2 Material
The survey and interview questions were developed by the authors (who include CBT practitioners and researchers). The surveys took on average 15 minutes and included 28 questions in the form of multiple choice, 10-point Likert-scale, and free text box questions ( Supplementary Material 1 ). A demographic questionnaire gathered demographic data from the samples. On average, the interviews lasted for 30 minutes and encompassed 23 questions exploring the participants’ experience of CBT and its effectiveness in addressing their ADHD difficulties ( Supplementary Material 2 ).
2.3 Participants
Participants were recruited from across different regions of the UK, using a database of adults with a diagnosis of ADHD, collated at the University of Nottingham’s ADHD research lab. The database had been created from previous research studies with individuals who have an ADHD diagnosis who previously indicated a willingness to participate in future research studies. Additionally, participants were also recruited from, ‘The ADHD Collective’, an online community of adults with ADHD based in the UK.
Inclusion criteria were that participants were aged 18 years old or greater, had an existing diagnosis of ADHD before receiving CBT, and the course of CBT was delivered within the UK by any provider (NHS, private or others).
Participants who reported receiving CBT within a mixed, integrative or eclectic psychotherapeutic approach, such as those mixing CBT concepts with other concepts drawn from other psychotherapy approaches (e.g. psychodynamic or humanistic approaches), were excluded from the study.
2.4 Procedure
Details of the studies were sent to mailing lists by the research team. Participants in the survey were entered in a £10 Amazon voucher prize draw. Additionally, interview participants were provided with a £20 Amazon voucher code after the completion of the interview.
Participants in both the survey and interviews who wished to participate signed an online consent form. Participants who responded to the semi-structured interview invitation were interviewed over Microsoft Teams at a time of their convenience.
2.5 Analysis
The interviews were analysed using an inductive approach to thematic analysis ( 53 ), which employed an essentialist perspective in extracting codes. The thematic analysis consisted of a six-stage process ( 53 ). The analytic process began by transcribing each interview verbatim shortly after being conducted. Following this process, the lead investigator first familiarized herself with the interview data and made notes in a diary of preliminary thoughts on the content of the interviews. From this, initial codes were identified in a coding manual that was then collated and combined to be classified into broader themes using constant comparative analysis, both within and between transcripts. Finally, as the analysis evolved, these broader themes were reviewed and refined to generate the final themes proposed. An ongoing analysis allowed for a clear definition of the final themes. Semantic themes were developed using participants’ descriptions of their own experiences. Themes were then reviewed by a second researcher (BF) to ensure that they mapped to the original transcripts. Interrater reliability of themes was tested on a small proportion (2/10, 20% of interviews) of the transcripts. The results were validated collectively as a team, and any discrepancies were discussed and reconciled. The survey responses were reported descriptively and were used to triangulate the responses from the interviews.
Ten participants took part in the interviews (70% female) and 46 in the surveys (71% female). Tables 1 , 2 (Interview) and 2 (survey) describe the demographics of each group.
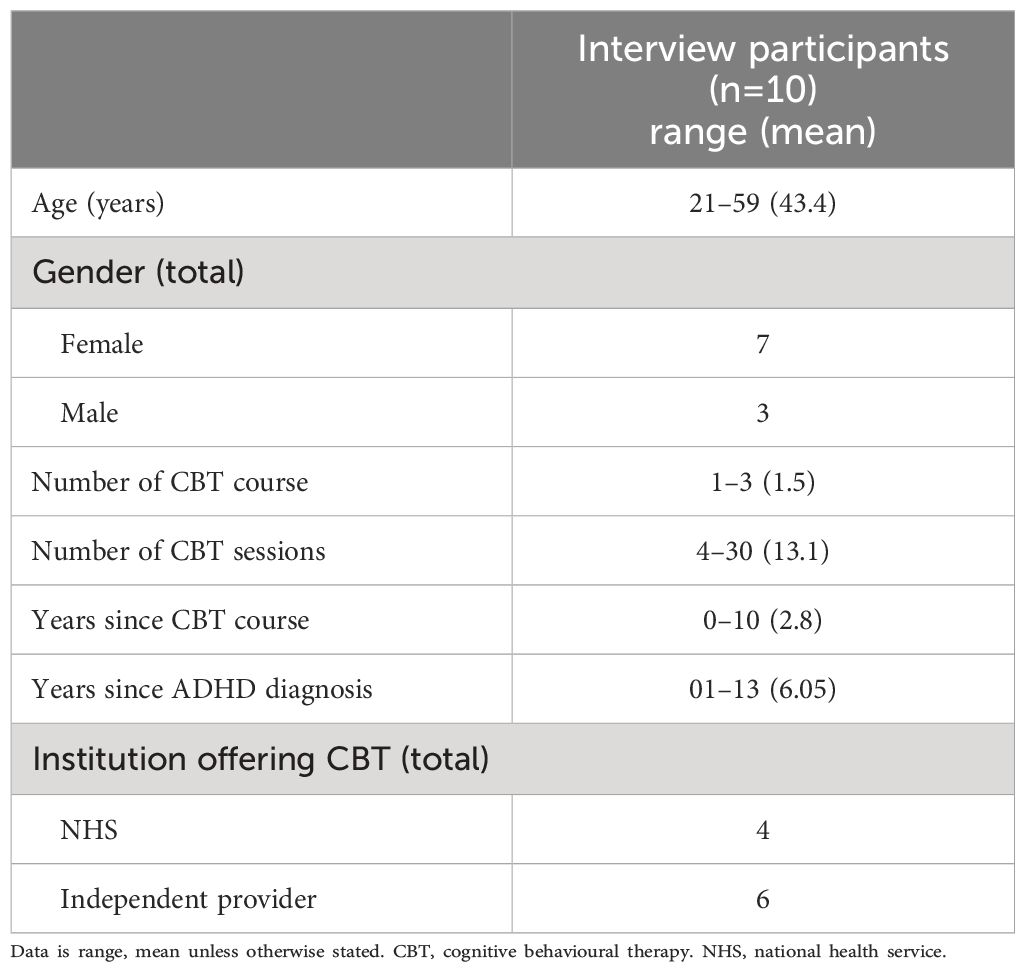
Table 1 Interview participants demographic characteristics.
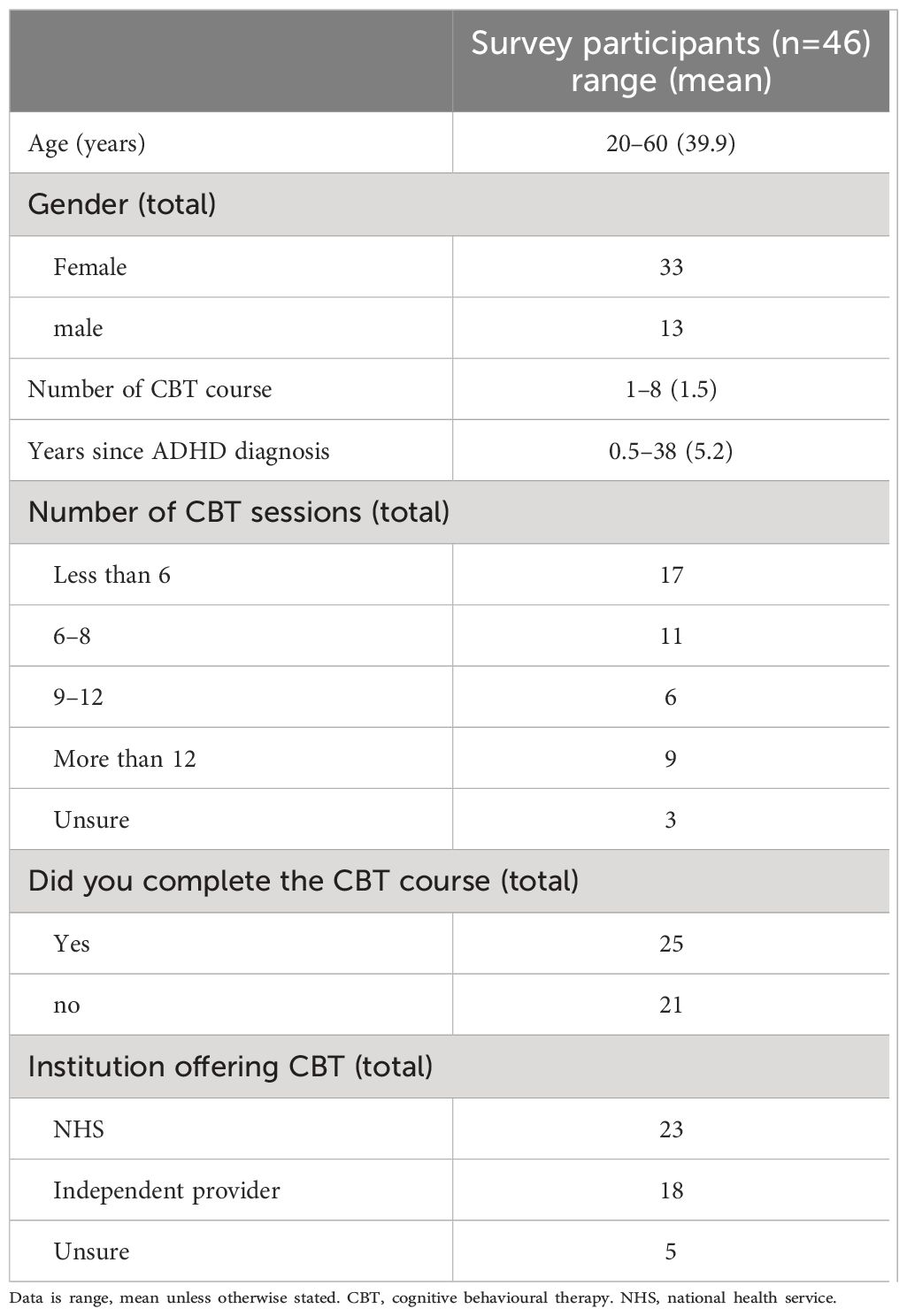
Table 2 Survey participants demographic characteristics.
3.1 Semi-structured interviews
The codes from the thematic analysis captured three main themes: The complex structure of the CBT framework, the intricacy of the therapist relationship, Consequences of CBT.
3.1.1 The complex structure of the CBT Framework
Participants reported that the overall framework of CBT was unhelpful due to several factors. Firstly, the generic nature of CBT sessions was usually not adapted to individuals with ADHD, making therapy ineffective and experienced as highly frustrating. Secondly, the CBT sessions followed a rigid structure that was not personalised to the participants’ needs. Thirdly, the timeframe of the therapy was experienced as too short to be of benefit to the ADHD participants.
Participants reported that the CBT they received was essentially incompatible with their experience of ADHD, as it did not take into consideration the inherent EF and emotional dysregulation difficulties they experienced. Working memory deficits were not accommodated in sessions, leading to a cycle of unnecessary pressure and ineffective treatment. Moreover, participants described that the content of therapy did not account for ADHD symptoms of inconsistency, distractibility, and inattention. As a result, ADHD participants reported feeling overwhelmed and frustrated by the approach, which they found unhelpful in managing their ADHD difficulties.
“I think there’s core things about CBT that are just seen on the face of it to me to be incompatible with ADHD. So, there is an element of having, decent working metacognition, working memory and things like that [ … ] I might discuss a technique with my therapist, but I would not remember to remember that technique. It just wasn’t going to happen.” (P5).
Only one participant reported receiving adapted CBT, with a therapist who also had ADHD. This participant reported that their CBT sessions allowed for self-acceptance of their EF difficulties, which moderated their approach to facing ADHD-related difficulties. For instance, they were able to moderate their time and chunk activities to avoid resistance and boredom. Overall, through the adapted CBT course, they were able to adopt cognitive strategies in their daily life, easing their day-to-day activities.
In contrast, however, most participants reported that the goals set in generic CBT were unspecific and unhelpful in managing ADHD symptoms. They explained that there was often no obvious relation between the CBT process and the management of their ADHD difficulties. They reported that ADHD topics such as understanding ADHD, time management, organization, and emotion regulation were often not discussed.
“ In the sense of actually managing ADHD symptoms [ … ]like time management, procrastination, achieving goal, it wasn’t really helpful for that kind of stuff, which is initially what I was hoping for” (P3) .
Furthermore, participants commented on the learning aids or physical resources offered in sessions. Some participants reported an absence of any learning aids or physical resources to summarize sessions, which caused an unhelpful dependence on memory, that led to forgetfulness. Conversely, other participants reported that they received an overwhelming amount of generic CBT resources which required high levels of literacy and concentration to comprehend, and which were not adequately adapted to ADHD individuals.
“I got sent a whole load of files and stuff to read and it was just volumes and volumes and volumes and stuff [ … ] Reading stuff is something I don’t do very well, and just the thought of doing all of that just overwhelmed me. I kept losing them as well” (P6) .
Participants reported that they needed CBT to offer an acceptance and management of their ADHD condition, rather than a fixing of their condition. Some participants reported that the sessions were too focused on symptom reduction, which did not allow for an appreciation of their strengths. This focus on just part of the person’s experience was sometimes experienced as unfair, with elements of their identity as a person with ADHD being ignored, or repressed, akin to being ‘dampened down’.
Conversely, the one participant who received adapted CBT reported that this course explained the behavioural irregularities as well as the strengths of having ADHD, fostering their acceptance of the condition.
“What I liked about it was that I understood how my mind worked [ … ] So it was really kind of understanding what the strengths I think of ADHD were. I just felt that I’m more accepting of myself and I’m more aware of myself and I’m more aware of my kind of behaviours if that makes sense” (P4) .
Participants also reported that the CBT objectives were not focused on the client’s needs but followed an unhelpful systematic approach. Participants who had undergone multiple courses of CBT reported that sessions felt like a pre-written script. Moreover, other participants reported that the CBT approach did not view the participant as an individual requiring personalised treatment.
“I felt the therapist had got their own set of exercises both times that they wanted to do from their own training, and I felt that I needed a much more bespoke approach” (P9) .
However, one participant expressed that their adapted CBT course was personalised in relation to their current situational difficulties, rather than being a generic application of CBT strategies. They reported sessions not being highly structured or systematic, but rather following an organic and client-centered approach, where the direction and flow of the therapy coincided with their feelings and needs.
Participants also reported that the generic CBT courses were too short to be helpful for their ADHD. They described that the number of offered sessions was inappropriate for individuals with ADHD who require more time to process information.
“It’d have to be extended because not only are you meeting someone new … you still got to bring the courage to open up to that person and then the sessions end, don’t last long enough, and then the overall course doesn’t last long enough. And I feel like something that takes that much would need to have more time for it” (P7) .
3.1.2 The intricacy of the therapist relationship and its impact on therapy
Participants reported multiple difficulties with their therapists affecting the overall experience. Firstly, almost all therapists were reported to be unspecialised in working with ADHD symptoms and seemed to have little knowledge about the condition, demotivating participants. Secondly, many therapists were experienced as unempathetic, affecting the participants’ healing and learning. Thirdly, many participants described their therapists’ approach as non-accommodative and inflexible.
Therapists appeared to lack a genuine understanding of ADHD, which affected participants’ treatment and motivation to continue with therapy. Some participants commented that they believe therapists with extensive ADHD experience should be delivering the CBT to ADHD individuals, for it to be maximally effective. Several participants reported that they had to explain multiple times to their therapists that the techniques they were assigned would not work with their ADHD, creating a lack of being understood and their experiences invalidated. Additionally, participants reported that their therapists seemed to assume their mental health difficulties could be treated in the same way as neurotypicals, disregarding that the myriad difficulties participants experienced were intricately linked to ADHD.
“I couldn’t see the link with ADHD and she didn’t see it either. [ … ] She knew nothing [about ADHD], and she told me that straight away. So, I think it impacted every single aspect of the therapy because she would just look on the surface of the problem and never be able to understand the deeper-rooted issues and difficulties” (P8) .
In contrast, tailored CBT facilitated participants understanding of the relationship between anxiety experiences and ADHD, and this was further aided by therapist’s disclosure of personal experience and knowledge of difficulties inherent in the condition.
“I felt very comfortable with her. I felt I could be very open and felt that she understood me, which was really important. I don’t know what it would be like to have that experience with a therapist who didn’t have ADHD … but I think unless you really know somatically how it feels that might be difficult to really know what someone else is experiencing” (P4) .
Participants reported that their therapist was unempathetic during treatment. They often felt judged and dismissed, which worsened their emotional state and affected the healing process.
“I always felt like quite dictated, like talking at me when I feel like, no one can be healed or learn about themselves or anything if they feel like they’re being judged or talked down to” (P7) .
Several participants felt that their therapist was not accommodating of their difficulties, nor their explicit feedback, resulting in feeling dismissed and demotivating their activation participation in CBT.
“I was sharing things that I thought were relevant, associated with ADHD and she didn’t really embrace it. She acknowledged it and she read it and said it was interesting, but she then didn’t necessarily adapt for it. So, I felt like it was listened to but not understood and acted upon. At the end I sort of gave up sharing my thoughts, trying to prepare for it” (P6) .
Some participants reported situations where the therapist was extremely rigid and inflexible with the timing of sessions. For instance, one participant reported that their therapist asked them to leave the room very abruptly because their time had ended, whilst they were severely distressed from recalling a traumatic event. Another participant reported that their therapist cancelled the appointment due to a five-minute bus delay.
“The therapist changed the time and he kept scheduling times that I couldn’t make, So, in the end, he wasn’t able to accommodate the time that I had available for the sessions, he ended up just discharging me” (P3) .
3.1.3 Consequences of unadapted CBT
The majority of participants reported little gain from or feeling worse off after the course of CBT.
Participants reported feeling worse off due to lowered self-esteem, increased sense of failure, frustration with self, increased emotional dysregulation and hopelessness with the future. One participant reported that their inability to perform the required techniques frustrated them greatly and lowered their self-esteem. Similarly, another commented that CBT made them feel responsible for their inability to benefit from the sessions, leading to a sense of failure. Other participants felt the CBT sessions left their emotional dysregulation even worse, not knowing how else they could move forward or be helped.
“I kept forgetting to practice, so by the time I come to the next session, they would have asked me how it went with the practice and I wouldn’t have practised, I wouldn’t have had time or I would’ve forgotten. And then it felt that if I didn’t do that, we couldn’t move forward. [ … ] So it felt like I was being punished and I couldn’t do the therapy properly because I couldn’t do those exercises” (P8) .
Some participants also felt at times that CBT sessions were a complete waste of time for them and that the lack of available alternative treatments for managing ADHD, led them feeling hopeless for the future.
“It was just such a waste of time for everyone, and it’s a shame, [ … ] it made me feel worse going there, and that’s not what you hope when you do therapy, you expect to feel better afterwards. But I felt worse and it’s just not very nice” (P8) .
Conversely, Participant Four described their adapted CBT experience as,
“… very transformational … because it really helped me to understand my mind and how to kind of work, I guess with my mind more. That made me feel happier about being me rather than trying to fit into what I believe the world sort of expected of me” (P4) .
All participants completed 11 Likert-scale questions on their experience of CBT from a scale of 1 to 10, where 1 indicated ‘strongly disagree’ and 10 indicated ‘strongly agree’. The results of the Likert-scale questions are presented in Table 3 .

Table 3 Experience of CBT questionnaire.
Additionally, 41 participants responded to the remaining short-answer questions. When asked, ‘What were you hoping to get out of your CBT sessions?’ participants responded that they wanted to receive help in managing their ADHD symptoms and executive functioning and to feel better about themselves. Moreover, most participants commented that they needed help understanding their thought processes and managing their emotional regulation, anxiety, self-esteem, organization, and low motivation. In addition, many participants expressed their need for actionable tools and effective coping strategies. When asked whether the CBT sessions met these expectations, participants responded that they did not. Participants commented that they felt blamed, not understood by their therapist, and constantly needed to explain themselves. For instance, one participant replied,
“No. ADHD wasn’t understood, and I constantly felt I had to explain why some the things being asked of me were a challenge”(P124) .
When asked about the challenges of accessing CBT, most participants argued that the sessions were too time-consuming. In addition, some participants noted that the waiting time to access CBT was too long and did not allow the patient to choose their own therapist. When asked what accommodations were made to support the participants’ access and engagement with CBT, most participants noted that no accommodations were made. Only a few participants commented that they were alerted prior to their appointments and that they were given extra time. When asked what the participants had liked or disliked, found helpful or unhelpful about CBT, many participants responded that it was unhelpful because it was manualised, repetitive, and did not address the underlying causes of symptoms. Moreover, some participants commented that they found the homework, tools, and therapists unhelpful, increasing their frustration. For example, one participant wrote,
“I struggled with speaking to someone who didn’t understand ADHD and didn’t seem to want to make any effort to. Some of the tasks required more forward planning or future thinking than I’m able to engage with. I came away feeling I’d need a much more intense level of interaction and support than I could afford or was on offer”(P106) .
When asked what the CBT course included, most participants responded that the course included working on unhelpful thinking styles, managing multiple tasks, organisation and planning, and managing distractibility. Moreover, when asked whether they had anything else to add about their experiences with CBT, some participants responded that they did not find it suitable and would not recommend this form of therapy to individuals with ADHD. For instance, one participant said,
“Overall, it made me feel more inadequate as I felt I couldn’t do the stuff I was supposed to. You can’t change how you think when your brain is wired differently. ADHD isn’t a thinking or positivity problem, and CBT seemed to assume it was”(P121) .
4 Discussion
The present study aimed to explore how individuals with ADHD experienced CBT in the UK. In this study, individuals with ADHD experienced several difficulties with CBT, that was not adapted to ADHD, which could have a negative impact on their overall wellbeing. These difficulties encompassed nonalignment of an unadapted CBT framework with specific aspects of ADHD, alongside a perceived unspecialised, unempathetic and non-accommodative CBT therapist, collectively resulting in suboptimal therapeutic experiences.
Participants expressed frustrations with the generic CBT framework due to its inconsideration of the EF and emotional dysregulation impairments experienced by individuals with ADHD. Participants described being forgetful, distracted, inconsistent, and inattentive, which pertained to impairments in their EF processes of updating, shifting, and inhibition, supporting previous research highlighting these difficulties in ADHD adults ( 8 – 10 ). Moreover, the participants’ emphasis on emotional regulation difficulties further supports previous research describing ADHD as a disorder of emotional dysregulation ( 14 , 54 ). Sadly, the generic, non-adapted CBT framework was not experienced as helpful, causing a counterproductive effect where participants felt overwhelmed, frustrated, and hopeless.
Research shows that when CBT is adapted specifically for ADHD symptoms, it can provide concrete strategies for managing the core symptoms of inattention, hyperactivity and impulsivity, and the associated personal interpersonal, social and occupational concomitants of the condition ( 55 ). Additionally, adapted DBT group interventions have demonstrated high effectiveness and acceptability, in helping people manage ADHD related symptoms ( 38 – 43 ). Group delivery of therapy is not commonplace within NHSTTAD services for patients with higher levels of distress or complexity, with one to one CBT being the primary treatment option. Moreover, as previously highlighted, there are few DBT trained therapists and supervisors currently working in primary care within England, giving rise to current plans to increase numbers of DBT trained therapists ( 48 ). The implication is that at this present time, adapted DBT maybe unlikely to be delivered in primary care with fidelity to the empirical studies.
Hayes and Hoffman ( 47 ), make the point that ‘third wave’ and traditional CBT approaches are often blended in reality, and this may be reflected in the range of empirically validated key adaptations to CBT for ADHD, which include helping the person to develop and review strategies to improve attentional focus, impulse control, planning and problem-solving, cognitive restructuring in the context of ADHD, managing emotional arousal in conflict and ensuing emotional or behavioural responses (e.g. managing anger and anxiety) and pro-social skills, e.g. empathy skills including perspective taking, recognition of the thoughts and feeling of others, critical reasoning, evaluating options and negotiation skills ( 28 , 34 , 56 ).
This is consistent with a body of research showing the efficacy of CBT in reducing ADHD symptoms and improving EF ( 29 , 31 , 34 , 56 ). Moreover, in a recent meta-analysis by Young et al. ( 19 ), CBT was shown to be an effective psychotherapeutic treatment for reducing ADHD symptoms.
Potential inconsistency in results across included studies is affected by stark differences in the implementation and delivery of CBT. Ramsay ( 4 ) described the impeding effect of ADHD symptoms on standard CBT and the need for an adapted approach to CBT to accommodate the EF and emotional dysregulation difficulties in participants with ADHD. Additionally, previous studies reported CBT content targeted to address ADHD symptoms, in countries outside the UK ( 19 , 31 , 34 , 56 , 57 ). The English NHSTTAD system is unique as it is a single point of access for CBT for all resident adults seeking support with mental health, following a prescribed competency-based approach to CBT for a limited range of presenting problems ( 58 ). Therefore, CBT in NHSTTAD is not necessarily easily tailored to or adapted for specific conditions outside of its core focus on anxiety and depression. CBT programs in other countries and published studies have often been adapted for ADHD and therefore do not represent the same form of care.
The difference in outcome between adapted and generic CBT is demonstrated in the striking disparity between Participant Four’s account and those of the other participants. They received a form of CBT specifically adapted for individuals with ADHD, by a therapist who was reported as having specialist expertise in working with clients with ADHD and who also had lived experience of ADHD. This experience of CBT was found extremely helpful and meaningfully tailored to their experiences by explaining their cognitive processes and behavioural responses in the context of their ADHD diagnosis. Psychoeducation of ADHD and an adapted approach allowed for an understanding of the client’s strengths and promoted self-acceptance and moderation of their ADHD-related difficulties. This mirrors previous studies which have highlighted the benefits of psychoeducation in cognitive interventions ( 43 ). Conversely, most participants, reported that there was no obvious accounting for ADHD symptoms within their CBT sessions. Therapists appeared to lack cursory knowledge of ADHD and did not seem to understand ADHD as a root cause behind symptoms experienced, and therefore could not appropriately adapt CBT or provide relevant techniques to help clients accept and moderate ADHD-related difficulties. Similar experiences of CBT delivered in routine practice in NHSTTAD services, as not being adequately tailored to the needs of clients are reported in the literature. Omylinska-Thurston et al. ( 59 ) reported similar findings in a group of participants with severe mental health disorders, where generic CBT was not experienced as adequately addressing underlying core issues, and was delivered inflexibly, leading to CBT being perceived as a waste of time and financial resources. The pressure on NHSTTAD therapists is significant, including considerations such as measurement against key performance indicators relating to client and service recovery rates, ‘throughput’ of clients, limited session numbers, high caseloads, and a range of client problems that are less likely to respond to time-limited CBT, such as experiences of poverty, social exclusion, or systematic oppression and social injustice ( 22 ). Against such a demanding context, several studies report significant levels of stress and psychological disturbance among the NHSTTAD workforce ( 60 – 62 ). It is possible, that against this context of background stress, therapists may be struggling to provide personalised formulation and therapy adapted to the presenting needs of their clients.
Indeed, in this study, most participants reported not receiving behavioural components of CBT for ADHD, meaning that they were not given graded task assignments, activity scheduling, or other behavioural tools to help manage procrastination and anxiety. The exclusion of valid behavioural elements of CBT has been previously noted by Binnie ( 22 ), who argued that CBT delivered in NHSTTAD often tended to focus on cognitive interventions, neglecting valid behavioural components.
Participants argued that the structure of therapy was not client-centred but followed a rigid and systematic approach which neglected their feelings, needs, and self-expression. Decades of research highlight the importance of a therapeutic relationship in which the therapist is experienced as empathic and attuned to the needs of the client, (e.g. 63 ), however, this crucial element of therapy was not experienced by several participants in the present study. Omylinska-Thurston et al. ( 59 ) reported that when participants felt their therapists were unempathetic and adhered to a rigid CBT protocol, instead of attending to the participant’s individual needs, therapy was unhelpful. Binnie ( 22 ) supported this by arguing that the delivery of CBT in NHSTTAD services may omit collaborative empiricism and guided discovery where the therapist works compassionately with the client, and instead overly focuses on manualised treatment for a restrictive range of presenting problems.
In contrast, Participant Four’s, specialised therapist idiosyncratically formulated the participant’s current situational difficulties and meaningfully personalised the treatment plan to the participant’s feelings and needs. This was experienced as crucial and helpful by the participant, who was able to learn from and manage undesirable situations, supporting Omylinska-Thurston et al. ( 59 ) who argued that an adjusted client-centred (i.e. idiosyncratically formulated) CBT process can improve the therapeutic relationship and outcome of therapy.
Overall, most participants reported feeling discontent or disappointed with therapy, which led to an increased sense of failure, increased emotional dysregulation, low self-esteem and a sense of self-blame. The ineffectiveness of therapy increased their feelings of hopelessness and disappointment in themselves. According to Ramsay ( 4 ), individuals with ADHD are more inclined to have pessimistic thoughts and expectations of failure due to their past unsuccessful experiences, which runs the risk of being amplified by therapy not adjusted to consider the person’s experiences of ADHD.
The survey results further supported the insights gleaned from the conducted interviews. Similar to the interviews, participants responded that they found the non-adapted form of CBT unhelpful and challenging, further deploring their self-esteem and increasing their frustration. Moreover, the therapists’ lack of knowledge of ADHD was apparent from most survey responses, demonstrating a need for additional training for therapists, on working with people who have ADHD.
4.1 Limitations
While the present study addresses an important research gap on the experience of generic, non-adapted CBT in adults with ADHD, there are limitations to the study. A convenience sample was used to recruit participants. The sample was predominantly female, which may not be an adequate representation of the predominantly male ADHD population, limiting the generalisability of the results. Moreover, convenience sampling may attract participants with charged emotional experiences, who may deliver a more negatively, or positively exaggerated account than that of the rest of the ADHD population. Additionally, the impact of the different ADHD presentations (inattentive, hyperactive-impulsive, and combined) on participants’ experiences of CBT was not analysed, which may have left an interesting variable unexplored. Finally, it is important to acknowledge that the findings refer to a vast range of non-adapted CBT treatment episodes experienced across the UK and therefore refers to a heterogeneous form of therapy. While we could discern between private, adapted CBT programs and NHS delivered generic programs, we cannot generalise the findings broadly as we lack details on these specific programs. Finally, we did not explore the different types of CBT that might have been received. The study aimed to look into how adults with ADHD experienced CBT, adopting a broad definition of what CBT is, as we did not want to be too prescriptive, believing that individuals might not always know the exact type of CBT they have received. This variance in the nature of CBT delivered, and understanding of what type of CBT is received may reflect naturalistic practice in the NHS, however through this omission, we might have missed important information about different nuances.
4.2 Future considerations
4.2.1 implications for practice.
This study highlights that routine delivery of CBT in the UK, may not be adapted appropriately for many adults with ADHD, negatively impacting their experiences. To combat this counterproductive effect of therapy, CBT therapists treating ADHD adults must receive additional training on adapting CBT to work with the array of symptoms and common experiences of people with ADHD, to more appropriately adapt CBT techniques and resources ( 4 ). Through this adaptive framework, necessary considerations regarding the EF and emotional dysregulation difficulties of ADHD individuals should be considered, transforming the nature of standard CBT to being more explicitly aligned with the experiences of people with ADHD.
4.2.2 Implications for research
The present study illustrates the potential negative impact of CBT on adults with ADHD revealing the need for more research in this topic area. Further investigation on the difference between adapted versus non-adapted CBT would further the important nuance in how beneficial CBT may be as a first line of psychotherapy treatment. Additionally, future research should consider the effect of different ADHD presentations on the effectiveness of CBT treatments, since research suggests improvement for clients with the predominantly inattentive ADHD sub-type ( 64 ). Moreover, specific post-qualification training on adapting CBT to work with ADHD symptoms appears indicated, and the authors are developing such training packages in association with people with lived experience of ADHD.
5 Conclusion
In conclusion, the present study portrays how adults with ADHD experienced CBT in the UK, with most ADHD participants reporting negative experiences when CBT programs were not adapted. This evidence prompts future research and clinical practice to address the issues highlighted in this study for a deeper understanding of how best to accommodate adults with ADHD in therapy. Moreover, this prompts therapists and service providers in the UK to consider the current implementation of CBT to ensure CBT can be appropriately adapted and delivered by therapists with relevant training, who understand the difficulties of ADHD, to ensure that treatment is helpful, efficient and meaningful to adults with ADHD, and to mitigate against the possibility of iatrogenic harm.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by University of Nottingham School of Psychology ethics committee (ethics reference number: FMHS 81-0922. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SW: Formal analysis, Investigation, Writing – original draft, Writing – review & editing. MH: Conceptualization, Methodology, Supervision, Writing – review & editing. JR: Conceptualization, Methodology, Supervision, Writing – review & editing. CH: Conceptualization, Investigation, Supervision, Writing – review & editing. BF: Conceptualization, Investigation, Methodology, Project administration, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. BR received funding from the Economic and Social Research Council (Grant number: ES/X000141/1).
Conflict of interest
BF reports personal fees and nonfinancial support from Takeda and Medice.
All remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1341624/full#supplementary-material
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders , 5th ed. (2013). doi: 10.1176/appi.books.9780890425596.
CrossRef Full Text | Google Scholar
2. Sayal K, Prasad V, Daley D, Ford T, Coghill D. ADHD in children and young people: prevalence, care pathways, and service provision. Lancet Psychiatry . (2018) 5:175–86. doi: 10.1016/S2215-0366(17)30167-0
3. Song P, Zha M, Yang Q, Zhang Y, Li X, Rudan I. The prevalence of adult attention-deficit hyperactivity disorder: A global systematic review and meta-analysis. J Global Health . (2021) 11:1–9. doi: 10.7189/jogh.11.04009
4. Ramsay JR. CBT for adult ADHD: adaptations and hypothesized mechanisms of change. J Cogn Psychother . (2010) 24:37–45. doi: 10.1891/0889–8391.24.1.37
5. Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol Psychiatry . (2005) 57:1336–46. doi: 10.1016/j.biopsych.2005.02.006
6. Gjervan B, Torgersen T, Nordahl HM, Rasmussen K. Functional impairment and occupational outcome in adults with ADHD. J attention Disord . (2012) 16:544–52. doi: 10.1177/1087054711413074
7. Barkley RA. Behavioral inhibition, sustained attention, and executive functions. psychol Bull . (1997) 121:65–94. doi: 10.1037/0033–2909.121.1.65
8. Boonstra AM, Kooij JJS, Oosterlaan J, Sergeant JA, Buitelaar JK. To act or not to act, that’s the problem. Neuropsychology . (2010) 24:209–21. doi: 10.1037/a0017670
9. Pazvantoğlu O, Aker AA, Karabekiroğlu K, Akbaş S, Sarısoy G, Baykal S, et al. Neuropsychological weaknesses in adult ADHD; cognitive functions as core deficit and roles of them in persistence to adulthood. J Int Neuropsychol Soc . (2012) 18:819–26. doi: 10.1017/S1355617712000574
10. Alderson RM, Kasper LJ, Hudec KL, Patros CHG. Attention-deficit/hyperactivity disorder (ADHD) and working memory in adults. Neuropsychology . (2013) 27:287–302. doi: 10.1037/a0032371
11. Bailey R, Jones SM. An integrated model of regulation for applied settings. Clin Child Family Psychol Rev . (2019) 22:2–23. doi: 10.1007/s10567-019-00288-y
12. Beheshti A, Chavanon ML, Christiansen H. Emotion dysregulation in adults with attention deficit hyperactivity disorder: a meta-analysis. BMC Psychiatry . (2020) 20:1–11. doi: 10.1186/s12888-020-2442-7
13. Soler-Gutiérrez A-M, Pérez-González J-C, Mayas J. Evidence of emotion dysregulation as a core symptom of adult ADHD: A systematic review. PloS One . (2023) 18:e0280131–e0280131. doi: 10.1371/journal.pone.0280131
14. Bodalski EA, Knouse LE, Kovalev D. Adult ADHD, emotion dysregulation, and functional outcomes: examining the role of emotion regulation strategies. J Psychopathol Behav Assess . (2019) 41:81–92. doi: 10.1007/s10862–018-9695–1
15. NICE. Attention deficit hyperactivity disorder: diagnosis and management (2018). Available online at: https://www.nice.org.uk/guidance/ng87 .
Google Scholar
16. Ramsay JR. Current status of cognitive-behavioral therapy as a psychosocial treatment for adult attention-deficit/hyperactivity disorder. Curr Psychiatry Rep . (2007) 9:427–33. doi: 10.1007/s11920–007-0056–0
17. McMain S, Newman MG, Segal ZV, DeRubeis RJ. Cognitive behavioral therapy: current status and future research directions. Psychother Res . (2015) 25:321–9. doi: 10.1080/10503307.2014.1002440
18. David D, Cristea I, Hofmann SG. Why cognitive behavioral therapy is the current gold standard of psychotherapy. Front Psychiatry (2018) 9:333730.
19. Young Z, Moghaddam N, Tickle A. The efficacy of cognitive behavioral therapy for adults with ADHD: A systematic review and meta-analysis of randomized controlled trials. J Attention Disord . (2020) 24:875–88. doi: 10.1177/1087054716664413
20. Gaudiano BA. Cognitive-behavioural therapies: achievements and challenges. BMJ Ment Health (2008) 11(1):5–7.
21. Fenn K, Byrne M. The key principles of cognitive behavioural therapy. InnovAiT . (2013) 6:579–85. doi: 10.1177/1755738012471029
22. Binnie J. Do you want therapy with that? A critical account of working within IAPT. Ment Health Rev J . (2015) 20:79–83. doi: 10.1108/MHRJ-11–2014-0044
23. NHS Benchmarking Network. Health Education England NHS Talking Therapies for Anxiety and Depression Workforce Census: National Report January 2023 . (2023).
24. Health Education England. National Curriculum for High Intensity Cognitive Behavioural Therapy Courses . London: NHS England (2022). Available at: https://www.hee.nhs.uk/sites/default/files/documents/HIT%20CBT%20Curriculum%204th%20Edition%202022_10%20Nov%202022.pdf .
25. Ramsay JR. CBT is effective in reducing symptoms in adults with ADHD whose symptoms persist following pharmacotherapy. Evidence-Based Ment Health . (2011) 14:28–8. doi: 10.1136/ebmh1144
26. NHS Digital. Psychological Therapies Annual report on the use of IAPT services 2021–22 (2022). Available online at: https://digital.nhs.uk/data-and-information/publications/statistical/psychological-therapies-annual-reports-on-the-use-of-iapt-services/annual-report-2021–22 .
27. Virta M, Salakari A, Antila M, Chydenius E, Partinen M, Kaski M, et al. Short cognitive behavioral therapy and cognitive training for adults with ADHD–a randomized controlled pilot study. Neuropsychiatr Dis Treat . (2010), 443–53. doi: 10.2147/NDT
28. Solanto MV, Scheres A. Feasibility, acceptability, and effectiveness of a new cognitive-behavioral intervention for college students with ADHD. J Attention Disord . (2021) 25:2068–82. doi: 10.1177/1087054720951865
29. Solanto MV, Marks DJ, Mitchell KJ, Wasserstein J, Kofman MD. Development of a new psychosocial treatment for adult ADHD. J Attention Disord . (2008) 11:728–36. doi: 10.1177/1087054707305100
30. Ramsay JR, Rostain AL. CBT without medications for adult ADHD: an open pilot study of five patients. J Cogn Psychother . (2011) 25:277–86. doi: 10.1891/0889–8391.25.4.277
31. Huang F, Tang Y, Zhao M, Wang Y, Pan M, Wang Y, et al. Cognitive-behavioral therapy for adult ADHD: A randomized clinical trial in China. J Attention Disord . (2019) 23:1035–46. doi: 10.1177/1087054717725874
32. López-Pinar C, Martínez-Sanchís S, Carbonell-Vayá E, Sánchez-Meca J, Fenollar-Cortés J. Efficacy of nonpharmacological treatments on comorbid internalizing symptoms of adults with attention-deficit/hyperactivity disorder: A meta-analytic review. J Attention Disord . (2020) 24:1–23. doi: 10.1177/1087054719855685
33. Guo C, Assumpcao L, Hu Z. Efficacy of non-pharmacological treatments on emotional symptoms of children and adults with attention-deficit/hyperactivity disorder: A meta-analysis. J Attention Disord . (2021) 26:2318. doi: 10.1177/10870547211001953
34. Safren SA, Sprich S, Mimiaga MJ, Surman C, Knouse L, Groves M, et al. Cognitive behavioral therapy vs relaxation with educational support for medication-treated adults with ADHD and persistent symptoms: A randomized controlled trial. JAMA: J Am Med Assoc . (2010) 304:875–80. doi: 10.1001/jama.2010.1192
35. Weiss M, Murray C, Wasdell M, Greenfield B, Giles L, Hechtman L. A randomized controlled trial of CBT therapy for adults with ADHD with and without medication. BMC Psychiatry . (2012) 12:30–0. doi: 10.1186/1471–244X-12–30
36. Jensen CM, Amdisen BL, Jørgensen KJ, Arnfred SMH. Cognitive behavioural therapy for ADHD in adults: systematic review and meta-analyses. Attention Deficit Hyperactivity Disord . (2016) 8:3–11. doi: 10.1007/s12402–016-0188–3
37. Knouse LE, Teller J, Brooks MA. Meta-analysis of cognitive-behavioral treatments for adult ADHD. J Consulting Clin Psychol . (2017) 85:737–50. doi: 10.1037/ccp0000216
38. López-Pinar C, Rosen H, Selaskowski B, Staerk C, Jans T, Retz W, et al. Exploring the relationship between adherence to therapy, treatment acceptability, and clinical outcomes in adults with attention-deficit/hyperactivity disorder: results from the COMPAS multicenter randomized controlled trial. Psychother Psychosomatics . (2023) 93:46–64. doi: 10.1159/000532043
39. Hesslinger B, Ludger Tebartz van E, Nyberg E, Dykierek P, Richter H, Berner M, et al. Psychotherapy of attention deficit hyperactivity disorder in adults: A pilot study using a structured skills training program. Eur Arch Psychiatry Clin Neurosci . (2002) 252:177–84. doi: 10.1007/s00406–002-0379–0
40. Hirvikoski T, Waaler E, Alfredsson J, Pihlgren C, Holmström A, Johnson A, et al. Reduced ADHD symptoms in adults with ADHD after structured skills training group: Results from a randomized controlled trial. Behav Res Ther . (2011) 49:175–85. doi: 10.1016/j.brat.2011.01.001
41. Fleming AP, McMahon RJ, Moran LR, Peterson AP, Dreessen A. Pilot randomized controlled trial of dialectical behavior therapy group skills training for ADHD among college students. J Attention Disord . (2015) 19:260–71. doi: 10.1177/1087054714535951
42. Morgensterns E, Alfredsson J, Hirvikoski T. Structured skills training for adults with ADHD in an outpatient psychiatric context: an open feasibility trial. ADHD Attention Deficit Hyperactivity Disord . (2016) 8:101–11. doi: 10.1007/s12402–015-0182–1
43. Nasri B, Castenfors M, Fredlund P, Ginsberg Y, Lindefors N, Kaldo V. Group treatment for adults with ADHD based on a novel combination of cognitive and dialectical behavior interventions. J Attention Disord . (2017) 24:1–13. doi: 10.1177/1087054717690231
44. Linehan MM. Cognitive-behavioral treatment of borderline personality disorder . Guilford Press (1993).
45. Linehan MM. Dialectical behavioral therapy: A cognitive behavioral approach to parasuicide. J Pers Disord . (1987) 1:328–33. doi: 10.1521/pedi.1987.1.4.328
46. Seow LLY, Collins KRL, Page AC, Hooke GR. Outcomes of brief versions of Dialectical Behaviour Therapy for diagnostically heterogeneous groups in a routine care setting. Psychother Res . (2022) 32:179–94. doi: 10.1080/10503307.2021.1933240
47. Hayes SC, Hofmann SG. The third wave of cognitive behavioral therapy and the rise of process-based care. World Psychiatry . (2017) 16:245–6. doi: 10.1002/wps.20442
48. Health Education England. Psychological Professions Workforce Plan for England . London: Health Education England (2021). Available at: https://www.hee.nhs.uk/sites/default/files/documents/Psychological%20Professions%20Workforce%20Plan%20for%20England%20-%20Final.pdf .
49. Knouse LE, Ramsay JR. Managing side effects in CBT for adult ADHD. ADHD Rep . (2018) 26:6–10. doi: 10.1521/adhd.2018.26.2.6
50. Krawczyk P, Topolewski M, Pallot M. (2017). Towards a reliable and valid mixed methods instrument in user eXperience studies, in: In 2017 International Conference on Engineering, Technology and Innovation (ICE/ITMC), . pp. 1455–64. IEEE.
51. Creswell JW, Plano Clark VL. Designing and conducting mixed methods research (3rd ed.) . Sage (2018).
52. Oates J, Carpenter D, Fisher M, Goodson S, Hannah B, Kwiatowski R, et al. BPS code of human research ethics. Br psychol Soc (2021).
53. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol . (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
54. Barkley RA. Attention-Deficit Hyperactivity Disorder . 4th ed. Guilford Publications (2014).
55. Solanto MV. Cognitive-behavioral therapy for adult ADHD: Targeting executive dysfunction. Guilford Press (2011).
56. Emilsson B, Gudjonsson G, Sigurdsson JF, Baldursson G, Einarsson E, Olafsdottir H, et al. Cognitive behaviour therapy in medication-treated adults with ADHD and persistent symptoms: a randomized controlled trial. BMC Psychiatry . (2011) 11:116–6. doi: 10.1186/1471–244X-11–116
57. Solanto MV, Marks DJ, Wasserstein J, Mitchell K, Abikoff H, Alvir JMJ, et al. Efficacy of meta-cognitive therapy for adult ADHD. Am J Psychiatry (2010) 167(8):958–68.
58. Roth AD, Pilling S. A competence framework for the supervision of psychological therapies . (2008).
59. Omylinska-Thurston J, McMeekin A, Walton P, Proctor G. Clients’ perceptions of unhelpful factors in CBT in IAPT serving a deprived area of the UK. Counselling Psychother Res . (2019) 19:455–64. doi: 10.1002/capr.12249
60. Owen J, Cross S, Mergia V, Fisher P. Stress, resilience and coping in psychological wellbeing practitioner trainees: a mixed-methods study. Cogn Behav Therapist (2021) 15:e38.
61. Steel C, Macdonald J, Schröder T, Mellor-Clark J. Exhausted but not cynical: burnout in therapists working within Improving Access to Psychological Therapy Services. J Ment Health (2015) 24(1):33–7.
62. Westwood S, Morison L, Allt J, Holmes N. Predictors of emotional exhaustion, disengagement and burnout among improving access to psychological therapies (IAPT) practitioners. J Ment Health (2017) 26(2):172–9.
63. Baier AL, Kline AC, Feeny NC. Therapeutic alliance as a mediator of change: A systematic review and evaluation of research. Clin Psychol Rev (2020) 82:101921.
64. Strålin EE, Thorell LB, Szybek K, Lundgren T, Bölte S, Bohman B. (2022).
Keywords: attention-deficit hyperactivity disorder (ADHD), cognitive-behavioural therapy (CBT), adapted CBT, psychotherapy, interviews
Citation: William S, Horrocks M, Richmond J, Hall CL and French B (2024) Experience of CBT in adults with ADHD: a mixed methods study. Front. Psychiatry 15:1341624. doi: 10.3389/fpsyt.2024.1341624
Received: 20 November 2023; Accepted: 24 May 2024; Published: 19 June 2024.
Reviewed by:
Copyright © 2024 William, Horrocks, Richmond, Hall and French. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Blandine French, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Introduction
- Conclusions
- Article Information
ADHD indicates attention-deficit/hyperactivity disorder; OR, odds ratio.
eAppendix 1. MoBa genetic data generation and quality control
eAppendix 2. Polygenic risk score thresholds
eAppendix 3. Pregnancy-related factors
eAppendix 4. Principal Component Analysis (PCA)
eAppendix 5. Inverse Probability Weighting (IPW)
eAppendix 6. Multiple Imputation (MI)
eAppendix 7. ADHD symptom measures in adulthood in MoBa
eAppendix 8. Paternal PGS sample overview and results
eAppendix 9. PGS associations at different P value thresholds
eAppendix 10. Comparison of complete case, inverse probability weighted and multiple imputation results
eReferences
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Havdahl A , Wootton RE , Leppert B, et al. Associations Between Pregnancy-Related Predisposing Factors for Offspring Neurodevelopmental Conditions and Parental Genetic Liability to Attention-Deficit/Hyperactivity Disorder, Autism, and Schizophrenia : The Norwegian Mother, Father and Child Cohort Study (MoBa) . JAMA Psychiatry. 2022;79(8):799–810. doi:10.1001/jamapsychiatry.2022.1728
Manage citations:
© 2024
- Permissions
Associations Between Pregnancy-Related Predisposing Factors for Offspring Neurodevelopmental Conditions and Parental Genetic Liability to Attention-Deficit/Hyperactivity Disorder, Autism, and Schizophrenia : The Norwegian Mother, Father and Child Cohort Study (MoBa)
- 1 Nic Waals Institute, Lovisenberg Diaconal Hospital, Oslo, Norway
- 2 Department of Mental Disorders, Norwegian Institute of Public Health, Oslo, Norway
- 3 PROMENTA, Department of Psychology, University of Oslo, Oslo, Norway
- 4 MRC (Medical Research Council) Integrative Epidemiology Unit, University of Bristol, Bristol, United Kingdom
- 5 Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, United Kingdom
- 6 Division of Psychological Medicine and Clinical Neurosciences, MRC Centre for Neuropsychiatric Genetics and Genomics, Cardiff University, Cardiff, United Kingdom
- 7 Wolfson Centre for Young People’s Mental Health, Cardiff University, Cardiff, United Kingdom
- 8 NORMENT, Institute of Clinical Medicine, University of Oslo, Oslo, Norway
- 9 Division of Mental Health and Addiction, Oslo University Hospital, Oslo, Norway
- 10 Institute of Clinical Medicine, University of Oslo, Oslo, Norway
Question Does maternal genetic liability for attention-deficit/hyperactivity disorder, autism, and schizophrenia predict exposure to pregnancy factors hypothesized to be causal for neurodevelopmental conditions in offspring?
Findings In this cohort study of 14 539 mothers and 14 897 fathers, associations between polygenic scores for attention-deficit/hyperactivity disorder, autism, and schizophrenia and 37 pregnancy-related predisposing factors were assessed. Higher genetic liability in mothers was found to be modestly but robustly associated with likelihood of experiencing several of the pregnancy-related factors associated with offspring neurodevelopmental conditions.
Meaning Observed associations between some pregnancy-related factors and offspring neurodevelopmental conditions are likely subject to genetic confounding and may not be causal.
Importance Several maternal exposures during pregnancy are considered predisposing factors for offspring neurodevelopmental conditions. However, many of these exposures may be noncausal and biased by maternal genetic liability.
Objective To assess whether pregnancy-related predisposing factors for offspring neurodevelopmental conditions are associated with maternal genetic liability for attention-deficit/hyperactivity disorder (ADHD), autism, and schizophrenia and to compare associations for maternal genetic liability with those for paternal genetic liability, which could indicate that paternal exposures are not suitable negative controls for maternal exposures.
Design, Setting, and Participants The Norwegian Mother, Father and Child Cohort Study (MoBa) is a population-based pregnancy cohort that recruited parents from June 1999 to December 2008. Polygenic scores (PGS) for ADHD, autism, and schizophrenia were derived in mothers and fathers. The associations between maternal PGS and 37 pregnancy-related measures were estimated, and these results were compared with those from paternal PGS predicting paternal measures during the mother’s pregnancy. Analysis took place between March 2021 and March 2022.
Exposures PGS for ADHD, autism, and schizophrenia, calculated (using discovery effect size estimates and threshold of P < .05) from the largest available genome-wide association studies.
Main Outcomes and Measures Self-reported pregnancy-related measures capturing lifestyle behaviors, metabolism, infectious and autoimmune diseases, other physical health conditions, and medication use.
Results Data were available for up to 14 539 mothers (mean [SD] age, 30.00 [4.45] years) and 14 897 fathers (mean [SD] age, 32.46 [5.13] years) of European ancestry. Modest but robust associations were observed between specific pregnancy-related measures and maternal PGS, including ADHD PGS with asthma (odds ratio [OR], 1.15 [95% CI, 1.06-1.25]), smoking (OR, 1.26 [95% CI, 1.19-1.33]), prepregnancy body mass index (β, 0.25 [95% CI, 0.18-0.31]), pregnancy weight gain (β, 0.20 [95% CI, 0.10-0.30]), taking folate (OR, 0.92 [95% CI, 0.88-0.96]), and not taking supplements (OR, 1.09 [95% CI, 1.04-1.14]). Schizophrenia PGS was associated with coffee consumption (OR, 1.09 [95% CI, 1.05-1.12]), smoking (OR, 1.12 [95% CI, 1.06-1.19]), prepregnancy body mass index (β, −0.18 [95% CI, −0.25 to −0.11]), and pregnancy weight gain (β, 0.17 [95% CI, 0.07-0.27]). All 3 PGSs associated with symptoms of depression/anxiety (ADHD: OR, 1.15 [95% CI, 1.09-1.22]; autism: OR, 1.13 [95% CI, 1.06-1.19]; schizophrenia: OR, 1.13 [95% CI, 1.07-1.20]). Associations were largely consistent for maternal and paternal PGS, except ADHD PGS and smoking (fathers: OR, 1.13 [95% CI, 1.09-1.17]).
Conclusions and Relevance In this study, genetic liability to neurodevelopmental conditions that is passed from mothers to children was associated with several pregnancy-related factors and may therefore confound associations between these pregnancy-related factors and offspring neurodevelopment that have previously been thought to be causal. It is crucial that future study designs account for genetic confounding to obtain valid causal inferences so that accurate advice can be given to pregnant individuals.
Attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (hereafter, autism) are common neurodevelopmental conditions. 1 Schizophrenia, although with later onset, shares many of the same features, and is hypothesized to have a neurodevelopmental origin. ADHD, autism, and schizophrenia are all highly heritable, 2 although their etiology is complex and likely to include a combination of genetic, environmental, and stochastic factors. 1 As development of these conditions is thought to begin early, prenatal factors have been investigated widely as potential predisposing factors, often through observational studies. 3 - 8 However, it is unclear whether the observed associations are causal. Observed associations may reflect confounding by unknown or unmeasured shared familial factors that influence maternal exposure and offspring neurodevelopmental outcomes. 9 , 10 Genetic confounding, when the same genetic factors are independently associated with both the exposure and outcome, has consistently been shown to explain the association between smoking during pregnancy and risk for ADHD in children using different causally informative designs. 11 - 15 Determining if exposure to prenatal factors is causal is important because misleading evidence about the causes of neurodevelopmental conditions can result in unnecessary worry for pregnant individuals and hinder attention to more appropriate intervention targets.
Genome-wide association studies (GWAS) have revealed ADHD, autism, and schizophrenia to be highly polygenic. 16 - 18 Individual common genetic liability can be expressed by a composite measure, called a polygenic score (PGS), summarizing the association of all the risk-increasing genetic variants identified in the GWAS. 19 By using PGS for genetic liability to neurodevelopmental conditions to predict pregnancy exposures, we can test whether shared genetics transmitted from mother to offspring can partially explain associations in observational studies. 20
Comparison of maternal and paternal PGS associations with the same pregnancy-related factors is informative given that paternal exposures are commonly used as negative controls to strengthen causal inference about intrauterine effects of maternal exposures. 21 Under the assumption that maternal and paternal associations between exposures and neurodevelopmental outcomes in the child are similarly influenced by shared genetics between parent and offspring (and other confounding familial factors, eg, socioeconomic status), similar magnitudes of parental factor–offspring outcome associations would suggest that the maternal factor does not have a causal intrauterine effect. However, different magnitudes of association between maternal vs paternal PGS with exposures would suggest that the use of paternal exposures as a negative control may not be appropriate. For example, some negative control studies have found stronger associations between prenatal substance use (smoking, alcohol, and caffeine) and offspring ADHD for mothers compared with fathers, 15 , 22 despite broader triangulation of evidence suggesting no causal effects. 12 , 13 , 15 During pregnancy, the substance use of the pregnant individual is a more severe phenotype than that of their nonpregnant partner, owing to the strong pressure on pregnant individuals to quit. Therefore, a higher genetic liability for substance use might be required for pregnant individuals to continue to smoke compared with their partners.
In the current study, we tested for the association between maternal and paternal PGS for ADHD, autism, and schizophrenia with maternal pregnancy-related exposures and co-occurring paternal exposures in the Norwegian Mother, Father and Child Cohort Study (MoBa). 23 The large sample size of mothers and fathers with genetic data allows us to include rare pregnancy-related factors such as vitamin B 12 insufficiency and use of depression medication. We also compare PGS associations with maternal exposures before and during pregnancy.
We used data from MoBa, a population-based pregnancy cohort study conducted by the Norwegian Institute of Public Health. 23 Participants were recruited from all over Norway from June 1999 to December 2008. Individuals were classified as mothers or fathers based on whether they returned the questionnaire for mothers or fathers. The genetic data quality control identified all of the mothers and fathers in the sample used in this article as chromosomally female and male, respectively. Mothers consented in writing to participate in 41% of the pregnancies. The cohort includes approximately 114 500 children, 95 200 mothers, and 75 200 fathers. The current study is based on version 12 of the quality-assured data files released for research in January 2019. The establishment of MoBa and initial data collection was based on a license from the Norwegian Data Protection Agency and approval from the Regional Committees for Medical and Health Research Ethics. The MoBa cohort is now based on regulations related to the Norwegian Health Registry Act. The current study was approved by the Regional Committees for Medical and Health Research Ethics (2016/1702). Blood samples were collected from both parents during pregnancy and from children (umbilical cord) at birth. 24 A range of pregnancy-related factors have been captured through questionnaires and the Medical Birth Registry of Norway, a national health registry containing information about all births in Norway. Genotyping and quality control are described in eAppendix 1 in the Supplement and previously. 25 Quality-controlled genotype data were available for 14 804 mothers and 15 198 fathers of European ancestry.
Of the neurodevelopmental conditions, only ADHD and autism had available GWAS summary statistics of large sample sizes (>10 000 cases). Schizophrenia was additionally included because of its commonly shared features of atypical attention, activity and impulse regulation, social communication and behavioral flexibility, hypothesized neurodevelopmental origin, and shared observational associations with prenatal exposures and to allow comparison with results from a study in the Avon Longitudinal Study of Parents and Children (ALSPAC) cohort. 26
Maternal and paternal PGS for ADHD, autism, and schizophrenia were calculated using PRSice version 2.0 27 as the weighted sum of single-nucleotide variants (only common sequence variants, ie, single-nucleotide polymorphisms) associated with ADHD, autism and schizophrenia in the discovery GWAS. 20 We excluded single-nucleotide variants in approximate linkage disequilibrium ( r 2 < 0.25 within a 500-kb sliding window) and in the major histocompatibility complex region owing to complex linkage disequilibrium structure. PGSs were adjusted for genotyping batch and the top 10 principal components to adjust for population stratification. Standardized residual scores were used in all analyses. Risk alleles were identified in GWAS for ADHD (individuals with ADHD, n = 20 183; controls, n = 35 191), 16 autism (individuals with autism, n = 18 381; controls, n = 27 969) 17 and schizophrenia (individuals with schizophrenia, n = 36 989; controls, n = 113 075). 18 Our primary single-nucleotide variant inclusion P value threshold was less than .05, selected for comparability with relevant previous studies of these PGS. 20 , 28 eAppendix 2 in the Supplement shows the number of single-nucleotide variants included in each PGS and histograms and correlations between PGS.
Pregnancy-related factors were chosen after a literature review of early life exposures that have been reported to be associated with neurodevelopmental conditions ( Table 1 ; eAppendix 3 in the Supplement ). Broadly, these exposures related to maternal lifestyle and health behaviors, metabolism, immune system, other physical health conditions, and medication use. We excluded pregnancy-related factors with fewer than 100 cases based on our power calculation (eAppendix 3 in the Supplement ). Where the same measures were reported by the fathers (during the mother’s pregnancy), we included these in the father’s analysis (eAppendix 3 in the Supplement ).
We restricted the sample to 1 observation per mother, keeping the firstborn child in MoBa. The multiple testing corrected threshold for significance was determined to be P < .002 for all analyses (eAppendix 4 in the Supplement ). Analysis took place between March 2021 and March 2022.
We assessed whether the ADHD PGS predicted ADHD behaviors in the MoBa parents (eAppendix 7 in the Supplement ). No direct phenotypic measure of autism or schizophrenia behaviors was available for the parents. However, autism and schizophrenia PGSs have both been validated in previous samples. 29 - 31
Associations of maternal ADHD, autism, and schizophrenia PGS with pregnancy-related factors were assessed using linear regression for continuous measures and logistic regression for binary outcomes in Stata version 15.1 (StataCorp). Effect estimates are presented per 1-SD increase in PGS. Analyses were repeated for paternal PGS on available paternal pregnancy-related factors.
To assess consistency, where possible, we estimated the association between maternal neurodevelopmental PGS and relevant exposures before pregnancy and at specific trimesters of the pregnancy.
PGS constructed using P value thresholds .0005, .005, .05, .10, and .50 were derived for sensitivity analyses as they provide different balance between levels of variance explained and inclusion of pleiotropic variants. We also conducted 2 analyses to investigate the potential effect of missing data. First, inverse probability weighting on missing maternal genetic data was applied to account for sampling bias in the genotyped data set (eAppendix 5 in the Supplement ). Second, we used multiple imputation (n = 100) with chained equations to impute missing data in the PGS and pregnancy-related factors (eAppendix 6 in the Supplement ).
Data were available for up to 14 539 mothers and 14 897 fathers. To account for differences between the genotyped and nongenotyped samples ( Table 1 ) and missing data, additional analyses were conducted (eAppendices 5 and 6 in the Supplement ).
Effect sizes for all associations of maternal PGS with maternal pregnancy-related exposures are shown in Table 2 . Maternal ADHD PGS was associated with younger age at childbirth (of first included MoBa child), higher odds of smoking during pregnancy, higher body mass index (BMI) before pregnancy, and higher pregnancy weight gain. Higher maternal ADHD PGS was associated with lower odds of taking supplements (including folate) during pregnancy. Additionally, mothers with higher ADHD PGS were more likely to have asthma and depression/anxiety symptoms. There was weak evidence of association with higher odds of migraine and pain during pregnancy.
Maternal autism PGS was associated with higher odds of experiencing depression/anxiety symptoms (and weak evidence for migraine and urinary tract infection) during pregnancy. There was little evidence for other associations of autism PGS with maternal health or lifestyle during pregnancy.
Maternal schizophrenia PGS was associated with higher odds of coffee consumption and cigarette smoking during pregnancy, lower prepregnancy BMI, and higher pregnancy weight gain. Schizophrenia PGS was associated with higher odds of depression/anxiety symptoms during pregnancy and of taking medication for depression/anxiety. There was only weak evidence of association between schizophrenia PGS and higher odds of taking supplements during pregnancy.
Sixteen of the pregnancy-related exposures were also measured in fathers during the mother’s pregnancy. We compared the magnitude of the maternal exposure PGS association with the magnitude of the paternal exposure PGS association ( Figure and eAppendix 8 in the Supplement ). Nonoverlapping confidence intervals were observed only for 2 associations: (1) maternal ADHD PGS was associated with higher odds of maternal smoking in pregnancy compared with paternal ADHD PGS predicting odds of father smoking and (2) maternal schizophrenia PGS was associated with higher maternal coffee consumption during pregnancy, while there was no association in fathers.
The associations of ADHD PGS with smoking, migraine, and depression before pregnancy were consistent with the associations during pregnancy ( Table 3 ). However, mothers with higher ADHD PGS were more likely to have ever drank alcohol, whereas there was little evidence for an association with alcohol consumption during pregnancy. The associations of schizophrenia PGS with smoking and depression during pregnancy were also seen for ever smoking and lifetime depression. Autism PGS was associated with lifetime depression and depression/anxiety symptoms during pregnancy. Stratifying by trimester, differences were found for pain, with evidence that mothers with high ADHD PGS were more likely to experience pain only during the first trimester.
Results using PGSs derived at different P value thresholds were consistent with our primary analysis of using a P value threshold of less than .05 (eAppendix 9 in the Supplement ). Results from inverse probability weighting and multiple imputation analyses were consistent with our primary results using complete case data (eAppendices 3, 5, 6, and 10 in the Supplement ).
We examined the association between parental genetic liability to ADHD, autism, and schizophrenia and a wide range of pregnancy-related factors previously observed to be associated with these conditions in offspring. Mothers with a higher ADHD PGS were more likely to be younger at age of childbirth, smoke during pregnancy, have higher BMI, gain more weight during pregnancy, have asthma and depression/anxiety symptoms, and less likely to take folate or other supplements. Our findings were broadly in line with findings from ALSPAC 20 and the UK Biobank. 28 Concordant results across these 2 UK-based cohorts represent a cross-cultural replication, strengthening the evidence that some pregnancy-related factors are associated with ADHD genetic liability and emphasizing the need to consider genetic confounding as a potential explanation for parent-offspring associations.
Evidence for an association with PGS does not exclude a causal effect. Genetic liability for neurodevelopmental conditions in parents might increase liability in their offspring through direct genetic effects and increase the likelihood of causal pregnancy-related exposures. Future study designs should attempt to partition genetic confounding from causal effects, triangulating different genetically informative approaches such as within-family Mendelian randomization, sibling comparison, and children-of-twins designs. 32 - 34 Our findings suggest potential effects of parental genetic liability to ADHD, autism, and schizophrenia on pregnancy-related factors. Even if these pregnancy-related factors are not causal for offspring neurodevelopment, many of them are still known to be causal for other offspring health outcomes (eg, low birth weight 35 ). Consequently, future studies should determine whether expecting parents with neurodevelopmental conditions require specific support during pregnancy (eg, to quit smoking and regulate weight gain).
In the case of smoking, studies using different causally informative designs have found that smoking during pregnancy is unlikely to increase the likelihood of ADHD outcomes in offspring via causal mechanisms. 12 , 36 - 38 Current findings suggest that ADHD is more likely to increase the risk of smoking during pregnancy, rather than the other way around.
The paternal ADHD PGS association with paternal smoking during pregnancy was of smaller magnitude than the maternal ADHD PGS association with maternal smoking during pregnancy. Thus, for smoking (and caffeine consumption, where disparity was also observed), there are implications for the validity of paternal negative control studies. Such studies assume that associations between maternal and paternal smoking with offspring outcomes will be similarly biased by familial factors such as shared genetics, and therefore any difference between the 2 is likely due to intrauterine effects. 13 However, we show that associations between maternal and offspring outcomes are more at risk of bias by genetic confounding than associations involving paternal smoking.
Maternal schizophrenia PGS was associated with higher likelihood of smoking and coffee consumption during pregnancy. There is both phenotypic and genetic correlation between coffee consumption and smoking, 39 making it challenging to account for pleiotropy. Schizophrenia PGS was also associated with lower BMI, consistent with findings from ALSPAC 20 and the UK Biobank. 28 We found a novel association between schizophrenia PGS and increased pregnancy weight gain. These findings are important given that exposures such as smoking during pregnancy were thought to play a causal role in schizophrenia. 40 The findings suggest that observational studies of pregnancy-related exposures and offspring schizophrenia need to be regarded with caution.
Autism PGS, as well as ADHD PGS and schizophrenia PGS, were associated with higher odds of experiencing depression/anxiety symptoms during pregnancy, as reported previously in ALSPAC. 20 Major depression is also genetically correlated with neurodevelopmental conditions. 41 The associations we found between schizophrenia PGS and depression/antidepressant medication use in pregnancy highlight the importance of genetically informative designs in studies of prenatal exposure to antidepressants and child neurodevelopment. 42
There was evidence for an association between ADHD PGS and an increased risk of asthma. Comorbidity between asthma and ADHD has been demonstrated previously. 43 , 44 Asthma and ADHD are also genetically correlated, 45 with ADHD PGS previously found to predict asthma risk in the UK Biobank. 28 Shared genetic liability between asthma and ADHD could be due to immunological mechanisms as ADHD is also positively associated with other allergic diseases. 46
There was some weak evidence of ADHD PGS and autism PGS association with migraine. ADHD-migraine comorbidity has been reported in children and adults, 47 and migraine is genetically correlated with ADHD. 48 Migraine could represent a mediating or confounding mechanism between the association of ADHD and paracetamol use. 49
Our study has several strengths, including large sample size and availability of many pregnancy-related factors. We were able to compare maternal and paternal PGS associations on the same pregnancy-related factors. We found relatively consistent associations, suggesting that genetic confounding may contribute to some associations between pregnancy-related factors and offspring ADHD, autism, and schizophrenia.
Our study was limited by the small amount of variance explained by neurodevelopmental PGS, especially for autism because of its low common single-nucleotide variant heritability. 16 - 18 , 50 Therefore, even where there was no evidence for an association in the current study, it is difficult to exclude associations of small magnitudes. The majority of the prenatal exposure PGS associations identified were of small magnitude. However, given that the PGS only explains a small proportion of the variance in the heritability, these estimates do not capture the full extent of genetic confounding. Consequently, only adjusting for parental PGS in observational studies is unlikely to sufficiently control for genetic confounding. An important next step (when the MoBa offspring are older) is to incorporate offspring phenotypic and genetic information and triangulate different designs to quantify the true extent of genetic confounding in associations between pregnancy exposures and neurodevelopmental outcomes. 51
We confirmed that ADHD PGS was associated with ADHD behaviors in MoBa mothers and fathers, and previous studies have shown that PGS for ADHD, autism, and schizophrenia predict signs of these conditions in the general population. 29 , 31 , 52 Owing to lack of power, we were not able to investigate other neurodevelopmental conditions, such as Tourette syndrome (cases, n = 4819; controls, n = 9488). 53 When larger GWAS become available, these investigations can be extended.
We relied on self-reports for many of the pregnancy-related factors. For some exposures (eg, smoking), this might have led to reporting bias. However, results were consistent with paternal exposures during pregnancy, which does not tend to be considered as harmful. Paternal associations of ADHD PGS with smoking were in fact lower than maternal associations, which might indicate that mother’s reporting was not biased by stigma.
As with all cohort studies, MoBa is subject to certain selection biases, for example, underrepresentation of younger parents and those with less education. 23 , 54 - 56 Thus, generalizability of results to populations not well-represented in MoBa should not be assumed. However, it is also worth noting that most measures used, and the blood samples from which genotype data arise, were collected during pregnancy, meaning that selective attrition is not a likely source of bias in these results. Genotyping in MoBa prioritized full trios, which likely contributed to differences between the full and genotyped sample. We performed sensitivity analyses using inverse probability weighting and multiple imputation and the results were consistent, suggesting this selection bias did not substantially impact our findings.
Our study demonstrates associations of ADHD genetic liability with several pregnancy-related factors that have been considered predisposing factors for offspring ADHD. Schizophrenia genetic liability also showed associations with some pregnancy-related factors, including lower prepregnancy BMI, higher pregnancy weight gain, and increased smoking during pregnancy. Autism genetic liability showed few associations with pregnancy-related factors beyond depression. Our findings suggest that pregnant individuals with high ADHD or schizophrenia genetic liability are at increased risk of adverse pregnancy-related exposures. Furthermore, our results indicate that observed associations between asthma, depression, smoking, BMI, pregnancy weight gain, and reduced likelihood of taking supplements with offspring ADHD as well as coffee consumption, smoking, BMI, and higher pregnancy weight gain with schizophrenia in the offspring are likely to be, at least in part, due to shared genetic liability, highlighting the need for genetically informative study designs for causal inference.
Accepted for Publication: May 10, 2022.
Published Online: July 6, 2022. doi:10.1001/jamapsychiatry.2022.1728
Corresponding Author: Alexandra Havdahl, PhD, Norwegian Institute of Public Health, Department of Mental Disorders, Sandakerveien 24C, 0473 Oslo, Norway ( [email protected] ).
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2022 Havdahl A et al. JAMA Psychiatry .
Author Contributions : Drs Havdahl and Wootton had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Drs Havdahl and Wootton are co–first authors, and Drs Reichborn-Kjennerud and Stergiakouli are co–senior authors.
Concept and design: Havdahl, Leppert, Bugge Askeland, Tilling, Davey Smith, Thapar, Reichborn-Kjennerud, Stergiakouli.
Acquisition, analysis, or interpretation of data: Havdahl, Wootton, Riglin, Ask, Tesli, Bugge Askeland, Hannigan, Corfield, Øyen, Andreassen, Stergiakouli.
Drafting of the manuscript: Havdahl, Wootton, Hannigan, Davey Smith, Stergiakouli.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Havdahl, Wootton, Leppert, Hannigan.
Obtained funding: Havdahl, Andreassen, Thapar, Stergiakouli.
Administrative, technical, or material support: Havdahl, Ask, Bugge Askeland, Corfield, Øyen, Reichborn-Kjennerud.
Supervision: Havdahl, Andreassen, Davey Smith, Thapar, Reichborn-Kjennerud, Stergiakouli.
Conflict of Interest Disclosures: Dr Wootton reported grants from Norwegian South-Eastern Regional Health Authority and Wellcome Trust during the conduct of the study and worked in the Integrative Epidemiology Unit at the University of Bristol, which was funded by the Medical Research Council. Dr Riglin reported grants from Wellcome Trust during the conduct of the study and is supported by the Wolfson Foundation. Ms Bugge Askeland was supported by the Research Council of Norway (grant 274611), awarded to Prof Reichborn-Kjennerud. Dr Corfield received funding from South-Eastern Norway Regional Health Authority Ted’s Research Council of Norway grant. Dr Øyen reports grants from Helse Sør Øst during the conduct of the study. Dr Andreassen reported unrestricted research funding from KG Jebsen Stiftelsen, South East Norway Health Authority, and Research Council of Norway and grants from EU H2020 for the CoMorMent project during the conduct of the study and consultant fees from HealthLytix, speaker’s honorarium fees from Lundbeck and Sunovion, and other funding for hospital clinical trials from Janssen, MAPS, and Boehringer Ingelheim outside the submitted work. Dr Tilling reported grants from MRC and Wellcome Trust during the conduct of the study. Dr Stergiakouli reported grants from Welcome Trust and MRC during the conduct of the study and outside the submitted work. Drs Leppert, Wootton, and Riglin were supported by the Wellcome Trust (grant 204895/Z/16/Z, awarded to Profs Thapar, Tilling, and Davey Smith and Dr Stergiakouli). Dr Havdahl is a member of the Norwegian Research Council–supported PROMENTA Research Centre and REMENTA project and reported grants from South-Eastern Norway Regional Health Authority and the Research Council of Norway during the conduct of the study. Drs Havdahl, Wootton, and Hannigan were supported by South-Eastern Norway Regional Health Authority (grants 2018058, 2018059, 2020024 and 2020022, awarded to Drs Øyen and Havdahl). Drs Wootton, Leppert, Stergiakouli and Profs Tilling and Davey Smith work in a unit that receives funding from the University of Bristol and the UK Medical Research Council (MRC Integrative Epidemiology Unit, University of Bristol) (grants MC_UU_00011/1 and MC_UU_00011/3). No other disclosures were reported.
Funding/Support: The Norwegian Mother, Father and Child Cohort Study is supported by the Norwegian Ministry of Health and Care Services and the Ministry of Education and Research. This research is part of the HARVEST collaboration, supported by the Research Council of Norway (grant 229624). We also thank deCODE Genetics and the NORMENT Centre for providing genotype data, funded by the Research Council of Norway (grant 223273), South East Norway Health Authorities, and Stiftelsen Kristian Gerhard Jebsen. We further thank the Center for Diabetes Research, the University of Bergen, for providing genotype data and performing quality control and imputation of the data funded by the ERC AdG project SELECTion PREDISPOSED, Stiftelsen Kristian Gerhard Jebsen, Trond Mohn Foundation, the Research Council of Norway, the Novo Nordisk Foundation, the University of Bergen, and the Western Norway Health Authorities (Helse Vest).
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: We are grateful to all the participating families in Norway who take part in this ongoing cohort study. We thank the Norwegian Institute of Public Health (NIPH) for generating high-quality genomic data.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

Could ADHD Actually Be A Superpower For Some Athletes?
How high energy, hyperfocus, and little tolerance for the mundane affect sports performance.
Before Molly Seidel was a legendary Olympic medal–winning marathoner, she was a high school student in Wisconsin just trying to make it through pre-calculus.
What her teacher didn’t know, though, was that Seidel had attention deficit/hyperactivity disorder (ADHD) , a neurodevelopmental disorder typically characterized by hyperactivity, compulsive behaviors, and difficulty paying attention. In fact, over the years, no one—not Seidel, and not her parents, coaches, teammates, friends, or doctors—knew she had ADHD. It wasn’t until February 2022 that a therapist with the U.S. Olympic & Paralympic Committee picked up on some signs.
“I thought, I can’t have ADHD, I’m not like that ,” Seidel says.
Up to that point, her life had been marked by major accolades in sports. She’d already become a multiple-time NCAA Division I cross-country and track champion, sailed to bronze in the 2020 Tokyo Olympics (becoming only the third American woman in history to medal in the marathon), and set the American women’s record at the New York City Marathon in 2021. Reddit fans called her “America’s distance sweetheart,” and fellow professional athletes called her a hero.
ADHD hadn’t been holding her back at all—in fact, it seemed to help propel her forward.
“If I had been diagnosed with ADHD when I was a kid and immediately put on medication,” Seidel says, “I don't think I'd be an Olympic athlete .” That’s because, for a while, her sport was her medicine. “When I started running, I immediately was like, ‘Wow, this is something that makes my brain work in a way that I never thought it could work.’”
These days, experts are starting to understand that the disorder is a brain difference that can give rise to frustrating symptoms but also notable strengths. And that can be especially true for athletes. Like the evolutionary “hunters” of society, people with ADHD are “very good at quickly context-switching, routing big bursts of energy to go after a goal and hyperfocusing on it,” says Mimi Winsberg, MD , a psychiatrist in San Francisco and chief medical officer of the online mental health practice Brightside Health . “It’s not so much an attention deficit as it is selective attention.”

Seidel is not alone in her ADHD-accented athletic prowess. Olympic GOATs like Michael Phelps and Simone Biles are on the roster too. In fact, high-level athletics seems to attract people with ADHD, with one research review finding the prevalence may be at least 8 percent in college and elite athletes compared with about 2.5 percent in the general adult population.
The actual estimate of ADHD in athletes may be even higher, since many studies capture only those who openly take medication for their condition. Plenty more, like Olympic gold medal–winning shot putter Michelle Carter , who was diagnosed with ADHD as a child, have never used meds. And others, like Seidel, excelled in their sport long before learning they had ADHD.
“In my world,” Carter says, “ADHD is kind of normal.”
.css-1cugboc{margin:0rem;font-size:2.125rem;line-height:1.2;font-family:Domaine,Domaine-roboto,Domaine-local,Georgia,Times,Serif;color:#f7623b;font-weight:bold;}.css-1cugboc em,.css-1cugboc i{font-style:italic;font-family:inherit;}.css-1cugboc b,.css-1cugboc strong{font-family:inherit;font-weight:bold;} “I’ve thought about what kind of person I would be without ADHD so many times.” —Michelle Carter
Of course, ADHD isn’t all positive. It can exist on a spectrum, manifesting differently in female athletes who may channel their hyperactivity and intense perfectionism via high-performance sports. However, what good is hyperfocus if you can’t get to practice on time? How valuable is extra energy if it drives you toward injury and burnout? Can you ever reach your full potential if you’re also grappling with depression, a substance use disorder, or another mental illness—conditions that frequently co-occur with ADHD ?
For many athletes, it’s hard to know where their personality ends and their disorder begins. But those like Seidel and Carter don’t feel the need to find out.
“I’ve thought about what kind of person I would be without ADHD so many times,” says Carter, 38, who’s now retired from professional sports and runs the mentorship program You Throw Girl . “My path is different, but I wouldn’t change it because I just think that it’s part of my creativity and it’s part of my personality—I think it adds that flair to my life.”
Spotting ADHD In Female Athletes
ADHD is technically characterized by inattention (trouble staying on task), hyperactivity (fidgeting, a racing brain), and impulsivity (risky behaviors or an inability to delay gratification) that negatively interfere with daily life. It’s an executive dysfunction disorder, which means it comes with differences in the brain—likely in the prefrontal cortex, which helps regulate attention and emotion. The ADHD brain also seems to have impaired neurotransmitter activity, including norepinephrine and dopamine, which play roles in stress, motivation, and reward-seeking behavior.
But many experts believe it’s poorly named: An ADHD brain can actually hyper focus on tasks and actions—so long as it finds the object of its attention interesting. “If I’m not interested in it, it’s just not happening,” Seidel says. “But if I am, I’m spending hours on it.”
ADHD also often manifests differently in women (read: not the typical rambunctious, disruptive, rowdy boy in class that most of us think of). Of the three subtypes—inattentive, hyperactive/impulsive, and mixed—women are thought to be more likely to fall into that first category. And this often looks like disorganization, depression, perfectionism, or procrastination.
Women and girls also tend to be socialized to “mask” chaotic inner thoughts and impulses with more “put together” demeanors. So, it’s no surprise that girls and women are frequently undiagnosed or misdiagnosed when it comes to ADHD, research shows. Sometimes, women don’t even recognize it themselves.
“In school, I was doing five things at once, but because I got good grades and I wasn’t causing trouble, I was just passed along,” says Allysa Seely , a Paralympic gold medalist in triathlon who was diagnosed with ADHD about five years ago, around age 30.
Seely, now 35, won gold in both the Tokyo and Rio de Janeiro Paralympics, and as of May 31, was waiting to learn if she made the 2024 Paris team. After her ADHD diagnosis (a surprise result of routine meetings with a psychologist), this was her reaction: “That can’t be right—only little boys have that.”
But as she learned more about how ADHD presents in girls and women, a lot of things clicked into place. For example, she has long felt a sort of “buzzing,” as she describes it, in her body and mind, and has little patience for chitchat. For Seely, “recovery” means foam-rolling while crocheting and listening to an audiobook at double speed.
Seely says her ADHD also presented as a near-irrational need for structure (the disorder often disrupts the cognitive skills involved in planning, decision-making, and sequencing tasks needed to achieve a goal). “I want 10 million things going on, but sometimes I have 10 million things going on and if one thing changes, I cannot rearrange the day,” she says. “If something falls apart, everything falls apart.”
Harnessing ADHD’s Unique Strengths Is Key
ADHD and athletics seem to go hand in hand. A driving decision that may seem impulsive on the highway can be quick thinking on the basketball court. An aloof demeanor at the office can translate to being “in the zone” in the pool. And hyperactivity in a classroom can be pure fuel in the ice rink.
Alli Matlesky, a 33-year-old executive assistant at a Washington, D.C., nonprofit, started running during the pandemic to release her pent-up energy and ended up training for her first triathlon in just eight weeks. She annihilated her goal time—and was diagnosed with ADHD.
“Triathlon gave me an energy outlet and something to focus on and strive for because, at the time, I was struggling with what I know now is ADHD,” Matlesky says.
Similarly, when Seidel is marathon training, she’s running upwards of 130 miles a week. “I’m either preparing to run or running, and for most people, that would sound like hell on earth,” she says. “But there’s nothing I’d rather be doing.”

People with ADHD also tend to find that moving their bodies can calm their racing minds. Michael Phelps, who was diagnosed with ADHD in sixth grade, explained the phenomenon in one of his books : “I could go fast in the pool, it turned out, in part because being in the pool slowed down my mind. In the water, I felt, for the first time, in control.”
Seely can relate. While her teammates tend to be pretty relaxed during training, they stiffen with anxiety on race day. She’s the opposite.
“That’s when I feel like I operate the best—it’s like everything is high stress, high stakes, and I’m just like, ‘All right, let’s do this,’” she says. “It’s this feeling of zen—almost how other people describe meditating. I never get that meditating. But if I’m running till I’m going to puke? Somehow, I’ve found it.”
The ADHD brain’s impulsive tendencies can also benefit athletes, says Scott Kollins, PhD , a clinical psychologist in Chapel Hill, North Carolina, and former chief medical officer at Akili , a digital medicine company that created the first and only FDA-approved video game, EndeavorRx , to treat ADHD. “You have people who are willing to do things others wouldn’t, take some risks, whether it’s with their time or pushing themselves harder,” Kollins says.
If you’re, say, an Olympic diver tasked with somersaulting off a springboard in front of hundreds of fans, it’s helpful to have a brain that doesn’t look too long before you leap.
People with ADHD also often thrive under pressure. Some crave the rush of adrenaline and, on the flip side, sometimes can’t get much done without it. When Matlesky was in college, she’d write papers while baking brownies, cramming to beat the buzzer. These days, that manifests as signing up for a triathlon every two to three months.
But the ultimate superpower for elite athletes with ADHD may be the ability to hyperfocus on something they’re excited about. When they’re “locked in,” a free-throw shooter won’t falter at fans’ jeers, a shot-putter won’t get psyched out that a lifetime of training comes down to a half second, an endurance racer won’t let daily temptations derail their training.
“ADHD honestly does feel like [a superpower] a little bit, especially in something like the marathon, because you’re having to focus on a really intense thing for a long time,” Seidel said. “I feel like I’m able to lock in in a way that I don’t know I could without ADHD.”
Finding A Balance Is Critical
That same superpower can also be someone’s kryptonite. Excess energy can lead to injury and burnout. Hyperfocusing on one thing (making it to the championship game, the Olympics, or that big PR) can mean neglecting another (keeping your academic scholarship, making sure the house is clean, paying your bills on time). Knee-jerk emotional reactions can get you in trouble with referees, coaches, or teammates. The list goes on.
“Even if it [ADHD] might be advantageous in certain ways, it takes both a mental and physical toll on the person,” Dr. Winsberg says.
In fact, being a girl or woman with ADHD can have “additional and unique harms,” says Julia Schechter, PhD , a clinical psychologist and codirector of the Duke Center for Girls & Women with ADHD. “ADHD is so much more than just being late to some meetings or losing your keys. It can contribute to academic difficulties, relationship problems, problems at work, and financial difficulties.”

Many women with ADHD, particularly those without a diagnosis, can drown in internal and external shame and criticism, frustrated by their inability to be on time, control their emotions, or refrain from interrupting. It follows, then, that women with ADHD are at higher risk for anxiety and depression, self-harm, and eating disorders, research shows . One Canadian study from 2020 found a startling one in four women with ADHD have attempted suicide.
“We have to work much harder than somebody with a holistic brain to achieve the same thing, to not be labeled as a problem, a troublemaker, disruptive. And sometimes, a lot of those coping mechanisms are detrimental to our health and our well-being,” says Seely. “There are definitely some great advantages, and there are also some very, very harsh drawbacks.”
Seidel, who, in addition to ADHD, has obsessive-compulsive disorder and is in recovery from an eating disorder, describes her experience like this: “There’s a radio on at full blast, right behind your head at all times, and no matter what you do, it will never turn off. It can drive you crazy if you don’t really handle your shit.”
Often, it’s only when these athletes get sick, injured, or retire that the wheels come off. “The mental health declines, the ADHD symptoms arise, and it can be pretty disastrous,” says Dusty Marie Narducci, MD , a physician in family and sports medicine who studies and treats athletes with ADHD.
That’s why proper diagnosis and management, either with or without medication, is key, says Dr. Narducci. “When you get [the diagnosis] right,” she says, “you change their life.”
While Medication Is Helpful, It’s Not For Everyone—And Some Elite Athletes Are Wary.
Stimulant medications such as Adderall and Ritalin, the most commonly prescribed medications for ADHD, can help. They work by increasing levels of certain neurotransmitters, including dopamine, to improve a person with ADHD’s ability to pay attention.
“I called [Adderall] my ‘adult pills,’ because all of a sudden I just felt like a normal person,” says Seidel, who described the prescription as “life-changing” in an Instagram post in 2022 . “For the first time, I felt like I was able to get the quiet, functioning brain in my day-to-day life that I could previously only achieve with intense physical activity,” she wrote.
But many athletes resist medication due to stigma around mental health conditions, bans against stimulants in competition without a therapeutic-use exemption, and a fear that in corralling their ADHD, they’ll dull their secret weapon, Dr. Narducci says.

There’s also debate in the medical community regarding potential side effects, like weight loss and heart issues , and about whether stimulant-based ADHD drugs could give athletes an unfair advantage. (Case in point: Despite having a therapeutic-use exemption, Simone Biles faced some heat after a media report exposed her ADHD diagnosis and Ritalin prescription. She responded: “Taking medicine for it is nothing to be ashamed of.”) But the reality, Dr. Narducci says, is “some of these meds can kind of flatten you out.”
In fact, that’s exactly why Seidel—who pulled out of a race in 2022 after her therapeutic-use exemption (which took months to process) wasn’t approved in time—stopped taking her medication. “For me, I feel like it takes away a little bit of what allows me to get into that zone that I need to perform at a world-class level,” she says.
The Good News: Treatment Options Are Increasing
Stimulants can be long- or short-acting and don’t necessarily need to be taken daily, Dr. Winsberg says, so some athletes use them to focus on life tasks like work or chores but avoid them ahead of competition.
Nonstimulant ADHD meds exist too, though they don’t tend to be as effective . Matlesky has had success on a form of Strattera, the brand name for atomoxetine, a nonstimulant ADHD treatment that increases noradrenaline (a neurotransmitter involved in attention) levels in the brain. With the drug and four weekly workouts, “I can handle what’s thrown at me,” she says.
“This is what makes me me . It allows me to process things really quickly. It allows me to do the sport I love.” —Molly Seidel
There are also nonpharmacological treatments, including psychotherapy, the Akili company's video game developed to treat ADHD, and neurofeedback therapy, which helps people train their brains to better focus by analyzing brain wave data in real time.
Seidel swears by mindfulness techniques like meditation and breath work. She’s a fan of near-daily naps—or at least how they make her feel afterward: less agitated, more calm. While quiet time and therapy are more tedious than medication, especially for the ADHD brain, the drug-free strategies work best for Seidel at the moment.
“There have been times where I’m just like, ‘I can’t do this anymore.’ It can be really, really hard,” she says. “But then at other times, I’m like, ‘Man, this is what makes me me .’ It allows me to process things really quickly. It allows me to do the sport I love. It makes me feel like the fullest version of myself.”

Anna Medaris is a freelance health and lifestyle journalist with nearly 15 years of experience writing features, narratives, explainers, and news hits for publications including the Washington Post, Business Insider, Cosmopolitan, and US News & World Report. She lives in Brooklyn with her husband and basset hound. Follow her at @AnnaMedaris on X and Instagram.

Sports & Athletes

Who Is Sha'Carri Richardson's Mom? Aunt, Grandma

All About Jade Carey's Parents, Brian And Danielle

Seine River Has High Levels Of E.Coli Pre-Olympics

All About Jordan Chiles' Parents, Gina And Timothy

Meet Simone Biles' Supportive Parents

Everything to Know About Jasmine Paolini’s Parents

All About Shilese Jones’ Training, Injury Recovery

Does Coco Gauff Have A Boyfriend?

Suni Lee‘s Incurable Kidney Disease Diagnosis

Where Is Dallas Cowboys Cheerleader Kelly Now?

Sabrina Ionescu Breaks Down The Sabrina 2 Sneaker
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Environmental Factor
Your online source for niehs news, how can you reduce health effects of endocrine-disrupting chemicals.
Nearly 300 researchers, clinicians, and community members gathered to share research, steps people can take to reduce exposure to EDCs.
By Caroline Stetler
National Institutes of Health (NIH) scientists recently gathered with researchers, clinicians, and community members to discuss emerging research focused on interventions — simple, accessible, and safe steps people can take — to mitigate exposures to endocrine-disrupting chemicals (EDCs). These chemicals interfere with hormones produced by the endocrine system, which controls metabolism, heart rate, growth, reproduction, and other biological processes.
During the two-day workshop held June 10-11 in Bethesda, Maryland, panelists called for more solutions-focused research, clinical trials to assess benefits of holistic interventions such as diet and physical activity, and health care provider education.
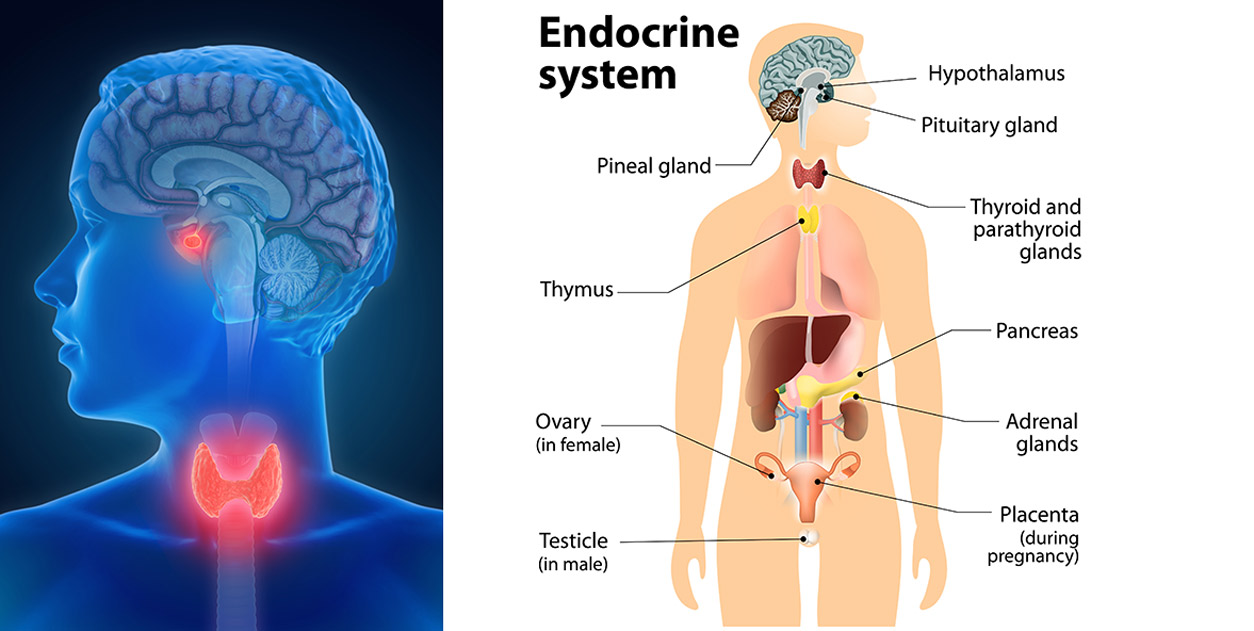
“We’ve discovered many different chemicals that are used widely — such as PFAS, pesticides like DDT, and plastic-related chemicals like phthalates and bisphenol A [BPA] — can all impact health and the health of future generations through endocrine-disrupting effects,” said NIEHS Director Rick Woychik, Ph.D. , during the workshop jointly organized by the National Center for Complementary and Integrative Health (NCCIH) and NIEHS.

“Every day there seems to be a new headline about EDCs and forever chemicals having an effect on our health and well-being, and possible links between EDCs and obesity, cancers, ADHD, immune dysfunction, or fertility problems,” said Sekai Chideya, M.D. , program director at NCCIH. “We must find ways to clear EDCs from our bodies, block their effects, or build defenses and resiliency because trying to avoid these chemicals is unlikely to prevent the health effects EDCs may cause.”
The goal, according to Chideya: Help the public feel empowered to do something about EDC exposure and risk reduction, as well as inspire researchers and the public to collaborate with NIH so we all stay healthy and thrive in the face of EDCs.
What are EDCS?

“EDCs are a little bit different than overt poisons in that they perturb our endocrine system,” said Heather Patisaul, Ph.D. , the scientific director for the NIEHS Division of Translational Toxicology. “And there isn’t an organ or cell in your body that the endocrine system doesn’t touch.”
According to Patisaul, the term “endocrine disruption” was coined in 1991, marking the beginning of an era when scientists began further understanding how chemicals can affect our bodies and health. The timing of EDC exposure, particularly during critical windows such as pregnancy and even at low doses, can significantly perturb the endocrine system and other organ systems.
However, regulation of these chemicals has lagged.
“Consumer demand, not a regulatory action, got BPA out of baby bottles and flame retardants out of furniture,” Patisaul explained. “There’s a lot of power when groups come together and ask for change.”
Diet, probiotics, supplements, and sweating chemicals out
NCCIH Director Helene M. Langevin, M.D. , applauded efforts to figure out how to mitigate the effects of these toxic chemicals, especially through lifestyle changes, such as nutrition education, physical activity, and stress management, that have wide- ranging benefits.
Key takeaways from research presented during the workshop include the following.
- Eating a diet high in fruits, vegetables, and whole grains, as well as low in sugar, along with physical activity and sufficient sleep, is known to improve overall health. Emerging research shows the benefits may also extend to a person’s ability to reduce EDCs’ effects.
- Consuming higher quality diets and decreasing exposures to nonpersistent EDCs improved pregnancy and maternal metabolic health outcomes, according to studies conducted by Rita Strakovsky, Ph.D., R.D., Michigan State University.
- Karen Peterson, D.Sc., University of Michigan, and a longtime NIEHS grantee, shared research showing lower intake of ultra-processed foods may reduce EDC exposure levels and cardiometabolic risk among women in midlife.
- Eating probiotic yogurt or fermented foods may help boost gut microbes that act as a barrier of protection against heavy metals that are EDCs, such as arsenic, mercury, and lead, according to studies conducted by Jordan Bisanz, Ph.D., Penn State.
- Regularly induced sweating can reduce the levels of EDCs, said Detlef Birkholz, Ph.D., an analytical consultant. His team found levels of BPA that were consistently higher in a person’s sweat than urine, suggesting sweat may be a better indicator of toxicant levels and more accurately capture the true burden of some EDCs.
- Emerging research indicates supplements such as fish oil, folate, and probiotics to support the gut microbiome, and stress management using mindfulness techniques, could provide benefits.
- If possible, avoid and reduce exposure to consumer products containing EDCs (see sidebar).
The human cost of EDCs
Community members representing firefighters, farmworkers, and veterans, who have been disproportionately exposed to EDCs in the workplace, as well as those affected by polluted drinking water, shared their perspectives during the workshop.
Hormis Bedolla, of the Alianza Nacional de Campesinas, shared photos of injuries she sustained after applying pesticides at an apple orchard. She also shared photos of her children. All were born premature and underweight, including one child who underwent heart surgery and another who was in the Neonatal Intensive Care Unit for two months, which she attributes to her decades-long work using pesticides that contain EDCs.
“As farmworkers, we are the ones feeding the nation, but we are not being seen or recognized,” said Amy Tamayo, J.D., Bedolla’s colleague who acted as her interpreter. “We are continuously facing the horrible consequences of pesticide exposures.”
Calls for health care provider education
“Our institute has been studying endocrine disruptors for a long time,” said Thad Schug, Ph.D. , program director at NIEHS. “We know the many ways the chemicals can harm our bodies, we know we should reduce exposure, and we know many of the bad chemicals, but how to proceed from here is the big question.”

Sheela Sathyanarayana, M.D., University of Washington, called on workshop participants to write an open letter to the Association of American Medical Colleges advocating for incorporating environmental components into the curriculum for all medical students. The goal would be to educate health care practitioners on EDC exposures and impacts on human health.
“Hearing from the impacted communities was very powerful and underscored the critical importance of interfacing with and talking to them even more,” Patisaul said. “It is their needs and priorities, after all, that we are tasked with addressing. NIH needs to do a better job of learning from them, responding to their needs, and prioritizing their health.”
Patisaul said she is hopeful the engaging and stimulating meeting leads to new partnerships and initiatives.
“We have reason to hope that so much of the outstanding research discussed in the last two days is pointing us in the right direction,” said Langevin.
The complete list of workshop speakers and their bios can be found here . Don’t miss a minute of the conference by checking out the NIH VideoCast .
(Caroline Stetler is Editor-in-Chief of the Environmental Factor, produced monthly by the NIEHS Office of Communications and Public Liaison.)
Steps you can take
Carmen Messerlian, Ph.D., Harvard T.H. Chan School of Public Health and an NIEHS grantee, shared a few concrete and sustainable steps people can take today to reduce their exposure to EDCs.
- Mop floors to reduce dust, chemicals picked up in the dust.
- Reduce screen time.
- Reduce the number of personal care products you put on your body (e.g., go from 10 to seven.)
- Reduce the number of times you eat takeout per week.
- Invest in a water filtration system, whether low-cost, over-the-counter water filters, or a reverse osmosis system.
Moving the needle down to create a new habit is the key, says Messerlian.
“What couples do today in the preconception window of vulnerability [to decrease exposures and enhance health and nutrition] affects their grandchild’s health and lifespan and helps us achieve generational health,” she said.
Related Articles

NIEHS News in Brief

How do PFAS, HIV drugs interact and affect health?

The microbiome’s influence on human health explored by NIEHS grantee
Improving PFAS filters with charged molecules
Ask the Expert: How does NIEHS research on PFAS affect me?
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 21 March 2022
Pursuing a scientific career with ADHD
- James E. Brown ORCID: orcid.org/0000-0002-3504-7373 1
Nature Reviews Endocrinology volume 18 , pages 325–326 ( 2022 ) Cite this article
2257 Accesses
16 Altmetric
Metrics details
- Medical research
- Neuroscience
Attention deficit hyperactivity disorder presents considerable barriers to a successful research career. Universities need to start taking this into account to ensure that talented researchers are retained in the sector and given an equal opportunity to succeed.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Acknowledgements
I would like to thank Dr A. C. Conner, University of Birmingham, for supporting the preparation of this article and for advocating for more support for ADHD in academia.
Author information
Authors and affiliations.
School of Biosciences, College of Health & Life Sciences, Aston University, Birmingham, UK
James E. Brown
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to James E. Brown .
Ethics declarations
Competing interests.
J.E.B. is co-founder of the registered charity ADHDadultUK.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Brown, J.E. Pursuing a scientific career with ADHD. Nat Rev Endocrinol 18 , 325–326 (2022). https://doi.org/10.1038/s41574-022-00664-9
Download citation
Published : 21 March 2022
Issue Date : June 2022
DOI : https://doi.org/10.1038/s41574-022-00664-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.119(5); Sep-Oct 2022

ADHD Diagnostic Trends: Increased Recognition or Overdiagnosis?
The prevalence of Attention Deficit Hyperactivity Disorder (ADHD) has seen a consistent rise in recent years. These numbers spark a debate over the reason for the observed trends, with some concerned about over diagnosis and over prescription of stimulant medications, and others raising the issue of diagnostic disparities, particularly in underrepresented populations. In this paper we look at both sides, starting with the history of ADHD and its diagnostic criteria changes, from early concepts of alterations in attention and hyperactivity in the 19th and 20th century, to its introduction in the Diagnostical and Statistical Manual of Mental Disorders (DSM), and its evolution into how it is defined today. The general broadening of ADHD diagnostically over time plays a role in the increased prevalence over the years, but it is not the only reason. Increased awareness of physicians and the public is also believed to play a big role, particularly in underrepresented minorities and women. However, there continues to be disparities in detection of ADHD in these groups. There are significant consequences to a patient’s social, interpersonal, and professional life when ADHD is left unrecognized and untreated. Thoughtful evaluation, accurate diagnosis, and adequate treatment can make a big difference.
Case History
Agatha has been struggling with school work since starting college in the fall. She always had difficulty paying attention in certain subjects, but did fairly well in high school. Lately she has been feeling more anxious because her study habits that worked throughout high school no longer seem to be effective. She feels completely inundated by the sheer volume and difficulty of her current assignments. She finds herself constantly procrastinating, regularly feeling guilty about her inability to adhere to deadlines. Problem sets are riddled with careless errors and papers contain numerous typos and grammatical errors. Sometimes, especially after doing poorly on an exam, guilt and anxiety about school become so high that she simply shuts down and avoids doing any work for the rest of the day. She has seen a lot of ADHD content on TikTok recently, and wonders if she may have ADHD herself. Her college friend has offered her Adderall, and while she hasn’t taken it without a prescription, she wonders if she may benefit from it.
Introduction
The past couple of decades have seen a continuous increase in attention deficit hyperactivity disorder (ADHD) diagnoses. National population surveys reflect an increase in the prevalence from 6.1% to 10.2% in the 20-year period from 1997 to 2016 and experts continue to debate and disagree on the causes for this trend. 1 On the one hand, while there are children whose diagnoses are irrefutable and undeniably require treatment, some experts worry about the risk of overdiagnosis and subsequent over prescription of stimulants and other psychotropics. Like with most psychotropic medications, treatment consideration needs to be carefully weighed with regards to potential adverse outcomes. For stimulants there is also concern for diversion and misuse of the medication for performance enhancement rather than for treatment. On the other hand, diagnostic disparities and underdiagnosis exist in various communities, including women and underrepresented minorities, as seen with Agatha. In this article, we aim to better understand the debate about the growing number of those affected by reviewing how ADHD morphed into the diagnosis we know today, and the variability and disparities observed.
Attention Deficit Hyperactivity Disorder: The Basics
Attention Deficit Hyperactivity Disorder is a neurodevelopmental disorder that globally affects 5% – 7.2% of youth and 2.5% – 6.7% of adults. 2 – 4 Recent estimates indicate that prevalence is even higher in children in the United States (U.S.), around 8.7% or 5.3 million. 5 Although it has long been conceptualized as a disorder of childhood, up to 90% of children with ADHD continue to experience symptoms into adulthood. 6 Obtaining a diagnosis in adulthood is also possible, as in one study, 75% of adults with ADHD were not previously diagnosed in childhood. 7 While in childhood the male to female ratio is 4:1, the ratio is closer to 1:1 in adults. 8
Attention Deficit Hyperactivity Disorder is thought to be caused by a combination of factors: genetic, neurobiologic, and environmental. Twin studies show that ADHD is highly hereditable (60–70%), and scientists have identified a number of genes believed to underlie vulnerability to the disorder. 9 This includes genes that regulate the expression of Brain Derived Neurotrophic Factor, which plays a role in learning and memory, as well as those involved in modulation of the brain’s dopaminergic system. 9 Environmental risk factors like perinatal complications and toxic exposures are also believed to play a role. 9 – 10
ADHD is a clinical diagnosis, which is accomplished through questionnaires, clinical interview, and in some cases, neuropsychiatric testing. While neuroimaging studies suggest a potential correlation between ADHD and white matter volume abnormalities in cortico-striatal pathways and the prefrontal cortex in study samples, biomarkers are not currently sensitive enough to assist with diagnosis.
The treatment for ADHD is often a combination of medication, skill building, and psychotherapy. In the 1930s, Charles Bradley, MD, noticed a drastic improvement in children’s behavior and school performance after administration of amphetamine sulfate—a drug he was hoping would help treat headaches. That serendipitous discovery led to the development of other stimulants, a class of medications that is still considered the gold standard and first line ADHD treatment. Pharmacologic therapy is reported to be effective in up to 70% of cases, yet the benefits are not without risk. 11 The most common side effects are decreased appetite, anxiety, nausea, headaches, and in children in particular, concern about tolerance, weight loss, and insomnia. Data on long-term stimulant use also remains limited. A recent literature review found long-term use to be generally safe, but authors did advise providers to use caution when prescribing stimulants to pre-school age children, adolescents at high risk of abuse, and children with tics and psychosis. 12
There are also many non-pharmacological modalities of treatment for ADHD, including behavioral parent training and mindfulness-based attention training. 13 – 14 Psychotherapy, especially cognitive behavioral techniques, has also been shown to be quite effective. 11 Finally, a newer non-pharmacological approach, neurofeedback, has some benefits, though clinical application remains logistically challenging. More research is required into its efficacy. 15
ADHD: Changes in Diagnostic Criteria Over Time
To understand its diagnostic trends, it is important to consider the origins of ADHD and its diagnostic criteria. In the Eighteenth century, Sir Alexander Crichton wrote one of the earliest documented clinical descriptions of a disorder in attention in his 1798 book On Attention and its Diseases. He described “morbid alterations” of attention that “render [individuals] incapable of attending with constancy to any one object of education.” 16 Although not globally recognized and treated at the time, his observations bear striking similarities to modern descriptions of the inattention domains of ADHD.
In the early 1900s, British physician Sir George Frederic Still described a number of children with a “defect of moral control.” 17 Although more similar to the modern concepts of conduct disorder (CD) or oppositional disorder (ODD), his description identified a number of features typically seen in ADHD like impulsivity and impaired frustration tolerance. Later, in the 1930s, physicians Kramer and Pollnow wrote about children with “hyperkinetic disease of infancy”, a syndrome that more closely resembled modern ADHD descriptions including both hyperactivity, emotional excitability and impulsivity, and inattention. 17
ADHD made its first appearance in the Diagnostic and Statistical Manual of Mental Disorders (or DSM) in 1968, as “Hyperkinetic Reaction of Childhood.” As the name implies, the emphasis was on overactivity and distractibility. In the years that followed, and with subsequent editions of the DSM, there was a clear shift in focus towards attention deficit as the defining feature of the disorder. The publication of the DSM-III in 1980 gave rise to the diagnosis of “attention deficit disorder,” or ADD, a term that remains part of popular vernacular to this day. The DSM-III also introduced a cutoff for the number of symptoms to earn the diagnosis, as well as age at onset, symptom duration, and exclusion of confounding psychiatric disorders and substance use.
The label ADHD that we know and use today first appeared in 1987 with the DSM-III-R, and combined both inattention and hyperactivity domains into one diagnosis. Then, the DSM-IV iteration divided the diagnosis into three subtypes: predominantly inattentive, predominantly hyperactive-impulsive, and combined type. The release of the DSM-V in 2013 saw the definition of ADHD broaden significantly. The changes are summarized in Table 1 . One such change allowed for autism spectrum disorder (ASD) and ADHD to coexist, which was not the case in previous iterations. Given the high comorbidity between ADHD and ASD, it is clear that this change, along with others ( Table 1 ), contributed to the rise in ADHD prevalence, as it added a large group of children who were previously excluded. 18
Changes in diagnostic determination for ADHD between the Diagnostic and Statistical Manual of Mental Disorders (DSM) IV and V editions
| DSM-IV | DSM-V | |
|---|---|---|
| 6 or more in either inattention of hyperactivity domains | 6 or more in either domain if <17 years old, OR 5 or more in either domain if >17 years old | |
| <7 years | <12 years | |
| Onset of impairment <7 years | Not required | |
| “Evidence of in 2 or more settings” | “Evidence of in 2 or more settings” | |
| Yes | No |
Clearly, the evolution of the diagnostic criteria accounts for some of the rise in ADHD. In fact, Polanczyk and his collaborators have done a lot of work on ADHD epidemiology—and they have consistently demonstrated that the observed variability in prevalence rates across various studies was attributed largely to differences in measurement of outcomes, namely the criteria used to diagnose ADHD and the inclusion or exclusion of functional impairment. 19 – 20
The changing criteria only makes clinical diagnosis more difficult. In the absence of biomarkers, diagnosis is made by signs and symptoms. Some helpful questions for screening by clinicians are suggested in Table 2 . However, this leaves a lot up to the clinician, and may lead to under and over diagnosis. Due to the overlapping nature of psychiatric symptoms, ADHD is often missed, and patients end up with inaccurate psychiatric diagnoses and medication regimen. This latter point is important as we now know ADHD has high rates of psychiatric comorbidities, such as behavioral aberrances (52%), anxiety (33%), depression (17%), and autism (14%). While this may lead to overdiagnosis, more likely than not, ADHD can be misdiagnosed as a result, and subsequently inadequately treated. 21 Screening tools have been developed and validated for detection of ADHD in adults such as WHO’s Adult ADHD Self Report Scales or ASRS and many clinicians will ask for reports from schools and loved ones as well. 22 Referring to neuropsychiatric testing is also an option, though it is expensive and not required to make the diagnosis.
Example of questions clinicians can ask when assessing for ADHD. Adapted from “Integrative Treatment for Adult ADHD: A Practical, Easy-to-use Guide for Clinicians” by Ari Tuckman (New Harbinger Publications, 2007). Broader questions can often elicit more information and will allow clinicians to explore more in depth than a memorizable check-list.
| Helpful Diagnostic Questions for Clinicians |
|---|
| Could you describe how it feels when you have to sit through a long movie or meeting? |
| Tell me how you did with being attentive in class in middle school compared to other students? |
| What is your experience when you try to read or focus on work for an extended period of time? |
| Have you ever made a mistake on an exam or at work that could have easily been prevented? |
| Do you often lose things like your keys or cell phone? If so, what do you do to keep track of them? |
| How likely are you to remember to do a task without writing it down (make a phone call, water the plants, do the laundry etc..) |
| What happens when you have a lot of tasks to do and need to get them all done? |
| Tell me about your ability to focus on things you like and want to do as opposed to harder less exciting things. |
| Do your friends and family ever ask you if you are paying attention to them? Do you feel you need to ask them to repeat something? Do you sometimes pretend you heard the conversation but actually didn't? |
| Do you ever feel the urge to say whatever is on your mind right there and then, sometimes interrupt people? Does it ever get you in trouble with others? For example, losing friendships, or having difficulties with your boss? |
| Do you drink coffee? If so, how much and how do you notice it affects you? |
ADHD: Increased Awareness, Increased Prevalence
Outside of simply diagnostic changes, studies have provided other explanations for the rise in ADHD, including increased awareness and familiarity of physicians and the public with the diagnosis, geographic location and cultural differences, as well as other public health related factors such as improved access to care. 23 ADHD has even earned its own Awareness Month as of October of 2004. A quick search on Google Trend shows a steady increase in ADHD-related searches throughout the years, with popularity in March 2022 at the highest it has ever been ( Figure 1 ).

Google search trends for the term “ADHD”, from 2004 to present
ADHD has also become prominent in popular culture. Characters with problems in attention and hyperactivity can be found all over early literary works - physician Heinrich Hoffman wrote short stories in the mid-1800s featuring characters like “Fidgety Philip” and “Johnny Look-in-the-Air,” the names of which alone indicate hyperactivity and inattention as core features of the characters. 24 Today, a number of movies and television characters have ADHD as part of their plotline and defining features - from Barney Stinson on “How I Met Your Mother,” to Phil Dunphy on “Modern Family,” and even Bart Simpson. Social media has also propelled ADHD into popular awareness, as it has taken over platforms like TikTok and Twitter. As of May 2022, the hashtag #adhd has 11.4 billion views on TikTok. Many people credit these platforms with helping them realize they had the diagnosis and subsequently seeking treatment for it. However, as is always the case with the internet and social media, misinformation about ADHD is fairly prevalent. A recent study has found that more than half of ADHD content on TikTok was misleading, most of them posted by non-health care providers. 25 That same study however did show that content posted by health care providers was overwhelmingly more accurate and useful to consumers. 25
ADHD and Undertreatment
While there is concern from rising ADHD diagnoses, a U.S. national survey reported in 2006 that only 11% of adults with ADHD were being treated for it. This is critical as deficits in organization and time management can lead to major educational, professional, or financial problems, with higher drop-out rates, higher unemployment rates, and lower income attainment in adults with ADHD. 26 Deficits can also have major interpersonal implications, with higher rates of divorce documented in adults with ADHD, for example. 27 People with untreated ADHD are also at elevated risk of substance use, car accidents, unintentional injuries, depression, anxiety, and suicide. 28 In other words, underdiagnosis has significant implications, far beyond inability to focus.
Some have raised concerns over non-medical use of stimulants. Non-medical use is most studied in student populations, where medications can function as either a cognitive enhancer, or are used recreationally. However, while some studies reported non-prescribed use of stimulants in about 7% of college students, most of the misuse was in the setting of attentional difficulties impairing the student’s ability to succeed in class. 29 This is a possible indication that said student has undiagnosed ADHD, and not a desire to use the medication to get ahead. More importantly, a recent review has found that pharmacological treatment of ADHD was associated with a decreased risk of substance use, not the opposite. 30
Disparities in ADHD Diagnosis in Minoritized Populations
Any discussion of ADHD diagnostic trends would be incomplete without a review of disparities among minoritized population. Increasing awareness of these disparities might be contributing to the increase in rates of diagnosis. Over the past 20 years, available literature showcases the presence of pervasive disparities in ADHD diagnosis related to both race and gender. For instance, between 2004–2006, Black students were more likely than their White counterparts to have ADHD symptoms (12% vs. 7% respectively), but were less likely to have received a diagnosis (9% vs. 14% respectively). 31 During the following decade, rates of diagnosis among Black individuals grew at a rate 3 times higher than among White individuals. 32 Similar trends have been seen among girls, who demonstrated a 3 times higher increase in diagnosis rates than boys over the past two decades. 32 – 33 In fact, with regard to gender, experts have attributed changes in DSM-IV diagnostic criteria to recent diagnostic trends. Following changes that placed increased focus on inattention, rather than hyperactivity, there was a correspondingly significant increase in ADHD diagnosis among females. 34 Specifically, between 1991 and 2008, diagnosis rates increased by a factor of 5.6 in girls compared to only 3.7 in boys. 35 In other words, knowing girls and underrepresented groups are more likely to have missed diagnoses, and even present with different symptoms, patients and clinicians might be asking more questions as a result. The rise might be due to the fact that these groups are just simply finally diagnosed, rather than over-diagnosed.
Even still, the data suggests we still are missing groups and underdiagnosing ADHD for many. To date, recent findings indicate that ADHD continues to be less frequently diagnosed in youth who are Black Indigenous and Persons of Color (BIPOC) and female, compared to those who are White and male, even after controlling for potential confounders such as socioeconomic status and adverse childhood experiences. 36 – 37 Girls continue to be diagnosed at older ages than boys and tend to endorse higher levels of perceived stress. 38 Reasons for these disparities stem from a multitude of systems level factors, however racial and gender bias is likely to play a major role. For example, diagnosis of any mental illness, especially ADHD, depends on individual interpretations of behavior and the way that a clinician integrates multiple informant reports from parents, caregivers, and teachers. Studies have found that clinicians tend to be more responsive to White parents who solicit an ADHD diagnosis and treatment for their child compared to BIPOC parents. 39 Further, BIPOC youth with ADHD are disproportionately more likely to be misdiagnosed with ODD or CD. 40–41
ADHD manifests differently across gender, as there may be stronger social pressures for girls to sit quietly compared to boys. In fact, studies show that boys have historically been more likely to exhibit hyperactivity and disruptive behaviors, prompting earlier detection of the disorder, compared to those with inattentive symptoms, a group that most often includes girls. 42 Interestingly, other studies have indicated there to be no true difference in level of hyperactivity across gender, rather a bias among teachers leading to under-recognition of hyperactive symptoms among girls. 43 While some are concerned about the overdiagnosis of ADHD, there are still many groups who are underdiagnosed and unaccounted for in the data. Ultimately, focusing on the idea of “overdiagnosis” among providers may be harmful, particularly for these populations, as this may present additional barriers to them receiving appropriate care.
ADHD is not a new phenomenon, however its prevalence has increased significantly in the recent years. Given changing diagnostic criteria and increasing awareness of the disorder in marginalized populations, especially individuals of color and females, this finding is not surprising. The general public has become increasingly more aware of ADHD through the media and social media. People are more likely to bring up their concerns to a physician, which in turn might prompt more numbers of people to be diagnosed. While some may argue that the increase is concerning and due to intentional feigning of symptoms in order to gain access to stimulant medication or test accommodations, the evidence suggests these groups have a negligible impact on diagnostic trends. In fact, as medical providers, focus on the idea of “overdiagnosis” may instead be harmful, create additional barriers to care, and add to the stigma towards their requests for help. It is important, instead, to approach patients holistically, and with an understanding of both the risks of treatment and undertreatment in mind. For those who have been struggling with unrecognized ADHD, there are significant impacts to mental health, social life, and work life. Thoughtful diagnosis and subsequent treatment can make all the difference.

Elie Abdelnour, MD, (above) and Jessica A. Gold, MD, MS , are in the Department of Psychiatry, Washington University School of Medicine, St. Louis, Missouri. Madeline O. Jansen, MD, MPH, is with the Department of Psychiatry, Child and Adolescent Division, University of California-Los Angeles, Los Angeles, California.
None reported.

COMMENTS
1. Introduction. Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder (NDD) presenting with inattention, hyperactivity, and impulsivity. It can be classified in three subtypes, depending on the intensity of the symptoms: predominantly inattentive, predominantly hyperactive-impulsive, and combined [ 1, 2 ].
ADHD increases the risk of substance misuse disorders 1.5-fold (2.4-fold for smoking) and problematic media use 9.3-fold in adolescence 55 56 and increases the risk of becoming obese 1.23-fold for adolescent girls. 57 58 59 It is also associated with different forms of dysregulated eating in children and adolescents.
Attention deficit/hyperactivity disorder (ADHD) is among the most common neurobehavioral disorders presenting for treatment in children and adolescents. ADHD is often chronic with prominent symptoms and impairment spanning into adulthood. ADHD is often associated with co-occurring disorders including disruptive, mood, anxiety, and substance abuse.
Twin and family studies have found that the same genetic factors influence both the disorder of ADHD and lower levels of ADHD symptoms in the general population 61,64, and that shared genetic ...
First broad scientometric analysis of over 50 years of research on ADHD. ... The co-citation reference network reflects the intellectual base combining highly cited papers and research trends evolution, whereas co-citation networks enriched by thematic patterns of citing articles, such as the techniques used in this study, may highlight ...
Overall, while many research questions have been answered, many others need to be addressed. Strengthening multidisciplinary collaborations, relying on large data sets in the spirit of Open Science and supporting research in less advantaged countries will be key to face the challenges ahead.
Attention-deficit hyperactivity disorder (ADHD) is a common childhood behavioural disorder. Systematic reviews indicate that the community prevalence globally is between 2% and 7%, with an average of around 5%. At least a further 5% of children have substantial difficulties with overactivity, inattention, and impulsivity that are just under the threshold to meet full diagnostic criteria for ...
ADHD is the most common neurodevelopmental disorder in children, yet despite a large increase in awareness and in the number of diagnoses, much less is known about how this disorder affects adults.
ADHD - attention deficit hyperactivity disorder - is a neurodevelopmental disorder that involves problems with attention, concentration and/or increased activity levels, resulting in problems ...
We remain ill informed about how to improve academic and educational outcomes of children with ADHD, despite decades of research on diagnosis, prevalence, and short-term treatment effects. We urge research on this important topic. It may be impossible to conduct long-term randomized, controlled trials with medication or behavior management used ...
Previous research of teachers' ADHD knowledge is mixed, with the findings of some studies indicating that teachers have good knowledge of ADHD (Mohr-Jensen et al., 2019; Ohan et al., 2008) and others suggesting that their knowledge is limited (Latouche & Gascoigne, 2019; Perold et al., 2010).Ohan et al. surveyed 140 primary school teachers in Australia who reported having experience of ...
Journal of Attention Disorders (JAD) focuses on basic and applied science concerning attention and related functions in children, adolescents, and adults. JAD publishes articles on diagnosis, comorbidity, neuropsychological functioning, … | View full journal description. This journal is a member of the Committee on Publication Ethics (COPE).
More provocatively, these scholars note the discrepancy between common practices in college disability services offices and the results from careful empirical research. Above all, Weis et al.'s paper reminds us that even when a diagnosis of ADHD is well-documented, the needed accommodations (if any) remain an open question, requiring separate ...
The remaining papers underwent full-text screening by the two reviewers (NB and SWAD) independently. ... routine inclusion of a generic HRQoL measure in health interventions for children with ADHD is encouraged. Future research should also incorporate both parent and child perspectives in HRQoL measures as both appear to be important in ...
Subsequent research led DSM V describing ADHD as a disorder across the lifespan. From there arose the term Adult ADHD, which clinicians are still uncomfortable or unfamiliar with. Till DSM IV-TR, ADHD was recognized as a triad of symptom-clusters of inattention, hyperactivity, and impulsivity, with onset before 7 years of age and causing ...
Introduction. The combination of psychological theory and interpretation of research have been highlighted as critical influencers guiding decision-making for clinical treatment design and development for Attention Deficit Hyperactivity Disorder (ADHD) [1, 2].ADHD is a neurodevelopmental disorder of self-regulation with symptoms negatively affecting daily functioning at work and at home, with ...
The assessment of impairment in every given ADHD evaluation can be seen as a gatekeeper that protects against over-diagnosis. In contrast, the presence of ADHD symptoms without the experience of functional impairment does not fulfill the criteria of a mental disorder (Spitzer et al., 2018) and represents a serious threat for diagnostic validity and common reason for false positives (Sibley, 2021).
Objectives There is limited evidence of the unmet needs and experiences of adults with attention deficit hyperactivity disorder (ADHD). Previous research in this area is predominantly quantitative ...
Systematic Search for and Retrieval of Research Reports. The inclusion criteria (see Table 1) were defined as studies on children's and adolescents' experiences and understanding of their ADHD, whereby qualitative methods were used for collecting and analysing data.The children and adolescents, diagnosed with ADHD, had to be under 19 years of age at the time the study was conducted.
Early DBT papers focused on reducing self-harm and suicide attempts in individuals diagnosed with personality disorder , ... The present study illustrates the potential negative impact of CBT on adults with ADHD revealing the need for more research in this topic area. Further investigation on the difference between adapted versus non-adapted ...
The purpose of this paper is to critically discuss the most up-to-date clinical evidence on the potential benefits and harms of the various approaches to the treatment and management of ADHD, and to identify the limitations of the current evidence base and the impact of these limitations on interpretation and translation into clinical practice.
Association of Maternal PGS for ADHD, Autism, and Schizophrenia With Pregnancy-Related Factors. View Large Download. Table 3. ... This research is part of the HARVEST collaboration, supported by the Research Council of Norway (grant 229624). We also thank deCODE Genetics and the NORMENT Centre for providing genotype data, funded by the Research ...
Research exploring the overlap/distinctiveness between ADHD and ASD has significantly increased in recent years, but direct comparison of the inhibition-related neuronal correlates between these ...
In fact, high-level athletics seems to attract people with ADHD, with one research review finding the prevalence may be at least 8 percent in college and elite athletes compared with about 2.5 ...
This research provides an opportunity to contribute to a deeper understanding of comorbid ADHD and social anxiety disorder (SAD), which can ultimately inform future interventions - and provide ...
Despite this long research history, ADHD is not necessarily well understood among the lay public, given the many controversies and public misconceptions concerning the disorder. 1,2 Longitudinal evidence suggests that childhood ADHD persists into young adulthood in 60-70% of the cases when defined relative to same-age peers and in 58% of the ...
6 Expert Academic Writing Tips for Stronger Papers. Published on July 2, 2024 by Hannah Skaggs. Learn how to improve your academic writing by removing bias, organizing your paper well, adding variety in the words and sentences you use, writing in active voice, editing thoroughly, and taking advantage of smart tools.
National Institutes of Health (NIH) scientists recently gathered with researchers, clinicians, and community members to discuss emerging research focused on interventions — simple, accessible, and safe steps people can take — to mitigate exposures to endocrine-disrupting chemicals (EDCs). These chemicals interfere with hormones produced by the endocrine system, which controls metabolism ...
Research has suggested that 4-5% of adults might have ADHD, with upwards of 90-95% of these people being undiagnosed and therefore untreated. ADHD is a protected disability in the UK under the ...
The past couple of decades have seen a continuous increase in attention deficit hyperactivity disorder (ADHD) diagnoses. National population surveys reflect an increase in the prevalence from 6.1% to 10.2% in the 20-year period from 1997 to 2016 and experts continue to debate and disagree on the causes for this trend. 1 On the one hand, while ...