- Reference Manager
- Simple TEXT file

People also looked at
Methods article, a review of artificial intelligence and robotics in transformed health ecosystems.

- 1 Institute for Medical Information, Bern University of Applied Sciences, Bern, Switzerland
- 2 Object Management Group, Needham, MA, United States
Health care is shifting toward become proactive according to the concept of P5 medicine–a predictive, personalized, preventive, participatory and precision discipline. This patient-centered care heavily leverages the latest technologies of artificial intelligence (AI) and robotics that support diagnosis, decision making and treatment. In this paper, we present the role of AI and robotic systems in this evolution, including example use cases. We categorize systems along multiple dimensions such as the type of system, the degree of autonomy, the care setting where the systems are applied, and the application area. These technologies have already achieved notable results in the prediction of sepsis or cardiovascular risk, the monitoring of vital parameters in intensive care units, or in the form of home care robots. Still, while much research is conducted around AI and robotics in health care, adoption in real world care settings is still limited. To remove adoption barriers, we need to address issues such as safety, security, privacy and ethical principles; detect and eliminate bias that could result in harmful or unfair clinical decisions; and build trust in and societal acceptance of AI.
The Need for AI and Robotics in Transformed Health Ecosystems
“Artificial intelligence (AI) is the term used to describe the use of computers and technology to simulate intelligent behavior and critical thinking comparable to a human being” ( 1 ). Machine learning enables AI applications to automatically (i.e., without being explicitly programmed for) improving their algorithms through experiences gained by cognitive inputs or by the use of data. AI solutions provide data and knowledge to be used by humans or other technologies. The possibility of machines behaving in such a way was originally raised by Alan Turing and further explored starting in the 1950s. Medical expert systems such as MYCIN, designed in the 1970s for medical consultations ( 2 ), were internationally recognized a revolution supporting the development of AI in medicine. However, the clinical acceptance was not very high. Similar disappointments across multiple domains led to the so-called “AI winter,” in part because rule-based systems do not allow the discovery of unknown relationships and in part because of the limitations in computing power at the time. Since then, computational power has increased enormously.
Over the centuries, we have improved our knowledge about structure and function of the human body, starting with the organs, tissues, cells sub-cell components etc. Meanwhile, we could advance it up to the molecular and sub-molecular level, including protein coding genes, DNA sequences, non-coding RNA etc. and their effects and behavior in the human body. This has resulted in a continuously improving understanding of the biology of diseases and disease progressions ( 3 ). Nowadays, biomedical research and clinical practice are struggling with the size and complexity of the data produced by sequencing technologies, and how to derive from it new diagnoses and treatments. Experiment results, often hidden in clinical data warehouses, must be aggregated, analyzed, and exploited to derive our new, detailed and data-driven knowledge of diseases and enable better decision making.
New tools based on AI have been developed to predict disease recurrence and progression ( 4 ) or response to treatment; and robotics, often categorized as a branch of AI, plays an increasing role in patient care. In a medical context, AI means for example imitating the decision-making processes of health professionals ( 1 ). In contrast to AI that generates data, robotics provides touchable outcomes or realize physical tasks. AI and robotics use knowledge and patient data for various tasks such as: diagnosis; planning of surgeries; monitoring of patient physical and mental wellness; basic physical interventions to improve patient independence during physical or mental deterioration. We will review concrete realizations in a later section of this paper.
These advances are causing a revolution in health care, enabling it to become proactive as called upon by the concept of P5 medicine –a predictive, personalized, preventive, participatory and precision discipline ( 5 ). AI can help interpret personal health information together with other data to stratify the diseases to predict, stop or treat their progression.
In this paper, we describe the impact of AI and robotics on P5 medicine and introduce example use cases. We then discuss challenges faced by these developments. We conclude with recommendations to help AI and robotics transform health ecosystems. We extensively refer to appropriate literature for details on the underlying methods and technologies. Note that we concentrate on applications in the care setting and will not address in more detail the systems used for the education of professionals, logistics, or related to facility management–even though there are clearly important applications of AI in these areas.
Classification of AI and Robotic Systems in Medicine
We can classify the landscape of AI and robotic systems in health care according to different dimensions ( Figure 1 ): use, task, technology. Within the “use” dimension, we can further distinguish the application area or the care setting. The “task” dimension is characterized by the system's degree of autonomy. Finally, regarding the “technology” dimension, we consider the degree of intrusion into a patient and the type of system. Clearly, this is a simplification and aggregation: AI algorithms as such will not be located in a patient etc.
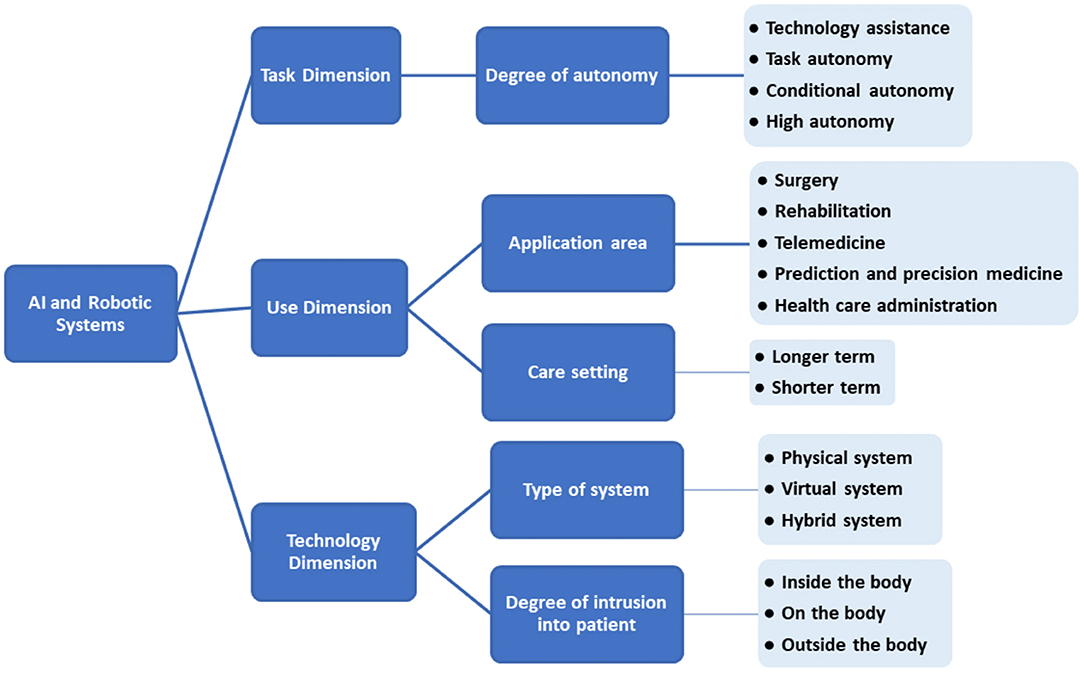
Figure 1 . Categorization of systems based on AI and robotics in health care.
Classification Based on Type of System
We can distinguish two types of such systems: virtual and physical ( 6 ).
• Virtual systems (relating to AI systems) range from applications such as electronic health record (EHR) systems, or text and data mining applications, to systems supporting treatment decisions.
• Physical systems relate to robotics and include robots that assist in performing surgeries, smart prostheses for handicapped people, and physical aids for elderly care.
There can also be hybrid systems combining AI with robotics, such as social robots that interact with users or microrobots that deliver drugs inside the body.
All these systems exploit enabling technologies that are data and algorithms (see Figure 2 ). For example, a robotic system may collect data from different sensors–visual, physical, auditory or chemical. The robot's processor manipulates, analyzes, and interprets the data. Actuators enable the robot to perform different functions including visual, physical, auditory or chemical responses.
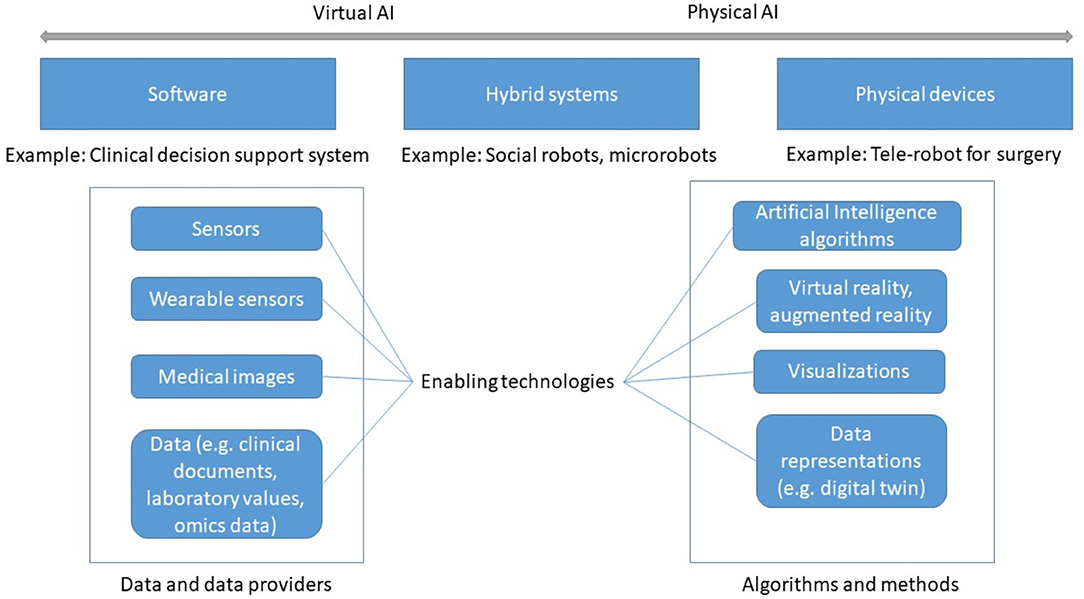
Figure 2 . Types of AI-based systems and enabling technologies.
Two kinds of data are required: data that captures the knowledge and experience gained by the system during diagnosis and treatment, usually through machine learning; and individual patient data, which AI can assess and analyze to derive recommendations. Data can be obtained from physical sensors (wearable, non-wearable), from biosensors ( 7 ), or from other information systems such as an EHR application. From the collected data, digital biomarkers can be derived that AI can analyze and interpret ( 8 ).
AI-specific algorithms and methods allow data analysis, reasoning, and prediction. AI consists of a growing number of subfields such as machine learning (supervised, unsupervised, and reinforcement learning), machine vision, natural language processing (NLP) and more. NLP enables computers to process and understand natural language (written or spoken). Machine vision or computer vision extracts information from images. An authoritative taxonomy of AI does not exist yet, although several standards bodies have started addressing this task.
AI methodologies can be divided into knowledge-based AI and data-driven AI ( 9 ).
• Knowledge-based AI models human knowledge by asking experts for relevant concepts and knowledge they use to solve problems. This knowledge is then formalized in software ( 9 ). This is the form of AI closest to the original expert systems of the 1970s.
• Data-driven AI starts from large amounts of data, which are typically processed by machine learning methods to learn patterns that can be used for prediction. Virtual or augmented reality and other types of visualizations can be used to present and explore data, which helps understand relations among data items that are relevant for diagnosis ( 10 ).
To more fully exploit the knowledge captured in computerized models, the concept of digital twin has gained traction in the medical field ( 11 ). The terms “digital patient model,” “virtual physiological human,” or “digital phenotype” designate the same idea. A digital twin is a virtual model fed by information coming from wearables ( 12 ), omics, and patient records. Simulation, AI and robotics can then be applied to the digital twin to learn about the disease progression, to understand drug responses, or to plan surgery, before intervening on the actual patient or organ, effecting a significant digital transformation of the health ecosystems. Virtual organs (e.g., a digital heart) are an application of this concept ( 13 ). A digital twin can be customized to an individual patient, thus improving diagnosis.
Regardless of the specific kind of AI, there are some requirements that all AI and robotic systems must meet. They must be:
• Adaptive . Transformed health ecosystems evolve rapidly, especially since according to P5 principles they adapt treatment and diagnosis to individual patients.
• Context-aware . They must infer the current activity state of the user and the characteristics of the environment in order to manage information content and distribution.
• Interoperable . A system must be able to exchange data and knowledge with other ones ( 14 ). This requires common semantics between systems, which is the object of standard terminologies, taxonomies or ontologies such as SNOMED CT. NLP can also help with interoperability ( 15 ).
Classification Based on Degree of Autonomy
AI and robotic systems can be grouped along an assistive-to-autonomous axis ( Figure 3 ). Assistive systems augment the capabilities of their user by aggregating and analyzing data, performing concrete tasks under human supervision [for example, a semiautonomous ultrasound scanner ( 17 )], or learning how to perform tasks from a health professional's demonstrations. For example, a robot may learn from a physiotherapist how to guide a patient through repetitive rehabilitation exercises ( 18 ).
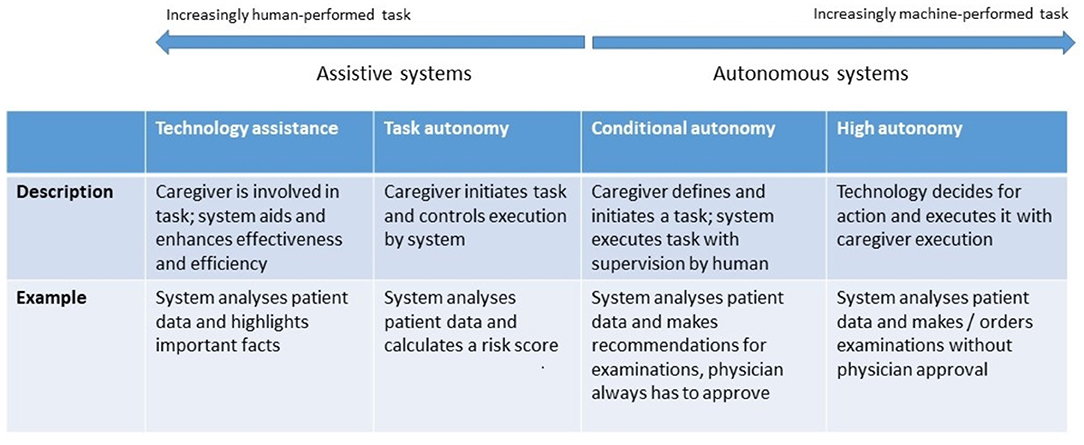
Figure 3 . Levels of autonomy of robotic and AI systems. [following models proposed by ( 16 )].
Autonomous systems respond to real world conditions, make decisions, and perform actions with minimal or no interaction with a human ( 19 ). They be encountered in a clinical setting (autonomous implanted devices), in support functions to provide assistance 1 (carrying things around in a facility), or to automate non-physical work, such as a digital receptionist handling patient check-in ( 20 ).
Classification Based on Application Area
The diversity of users of AI and robotics in health care implies an equally broad range of application areas described below.
Robotics and AI for Surgery
Robotics-assisted surgery, “the use of a mechanical device to assist surgery in place of a human-being or in a human-like way” ( 21 ) is rapidly impacting many common general surgical procedures, especially minimally invasive surgery. Three types of robotic systems are used in surgery:
• Active systems undertake pre-programmed tasks while remaining under the control of the operating surgeon;
• Semi-active systems allow a surgeon to complement the system's pre-programmed component;
• Master–slave systems lack any autonomous elements; they entirely depend on a surgeon's activity. In laparoscopic surgery or in teleoperation, the surgeon's hand movements are transmitted to surgical instruments, which reproduce them.
Surgeons can also be supported by navigation systems, which localize positions in space and help answer a surgeon's anatomical orientation questions. Real-time tracking of markers, realized in modern surgical navigation systems using a stereoscopic camera emitting infrared light, can determine the 3D position of prominent structures ( 22 ).
Robotics and AI for Rehabilitation
Various AI and robotic systems support rehabilitation tasks such as monitoring, risk prevention, or treatment ( 23 ). For example, fall detection systems ( 24 ) use smart sensors placed within an environment or in a wearable device, and automatically alert medical staff, emergency services, or family members if assistance is required. AI allows these systems to learn the normal behavioral patterns and characteristics of individuals over time. Moreover, systems can assess environmental risks, such as household lights that are off or proximity to fall hazards (e.g., stairwells). Physical systems can provide physical assistance (e.g., lifting items, opening doors), monitoring, and therapeutic social functions ( 25 ). Robotic rehabilitation applications can provide both physical and cognitive support to individuals by monitoring physiological progress and promoting social interaction. Robots can support patients in recovering motions after a stroke using exoskeletons ( 26 ), or recovering or supplementing lost function ( 27 ). Beyond directly supporting patients, robots can also assist caregivers. An overview on home-based rehabilitation robots is given by Akbari et al. ( 28 ). Virtual reality and augmented reality allow patients to become immersed within and interact with a 3D model of a real or imaginary world, allowing them to practice specific tasks ( 29 ). This has been used for motor function training, recovery after a stroke ( 30 ) and in pain management ( 31 ).
Robotics and AI for Telemedicine
Systems supporting telemedicine support among others the triage, diagnostic, non-surgical treatment, surgical treatment, consultation, monitoring, or provision of specialty care ( 32 ).
• Medical triage assesses current symptoms, signs, and test results to determine the severity of a patient's condition and the treatment priority. An increasing number of mobile health applications based on AI are used for diagnosis or treatment optimization ( 33 ).
• Smart mobile and wearable devices can be integrated into “smart homes” using Internet-of-Things (IoT) technologies. They can collect patient and contextual data, assist individuals with everyday functioning, monitor progress toward individualized care and rehabilitation goals, issue reminders, and alert care providers if assistance is required.
• Telemedicine for specialty care includes additional tools to track mood and behavior (e.g., pain diaries), AI-based chatbots can mitigate social isolation in home care environments 2 by offering companionship and emotional support to users, noting if they are not sleeping well, in pain or depressed, which could indicate a more complex mental condition ( 34 ).
• Beyond this, there are physical systems that can deliver specialty care: Robot DE NIRO can interact naturally, reliably, and safely with humans, autonomously navigate through environments on command, intelligently retrieve or move objects ( 35 ).
Robotics and AI for Prediction and Precision Medicine
Precision medicine considers the individual patients, their genomic variations as well as contributing factors (age, gender, ethnicity, etc.), and tailors interventions accordingly ( 8 ). Digital health applications can also incorporate data such as emotional state, activity, food intake, etc. Given the amount and complexity of data this requires, AI can learn from comprehensive datasets to predict risks and identify the optimal treatment strategy ( 36 ). Clinical decision support systems (CDSS) that integrate AI can provide differential diagnoses, recognize early warning signs of patient morbidity or mortality, or identify abnormalities in radiological images or laboratory test results ( 37 ). They can increase patient safety, for example by reducing medication or prescription errors or adverse events and can increase care consistency and efficiency ( 38 ). They can support clinical management by ensuring adherence to the clinical guidelines or automating administrative functions such as clinical and diagnostic encoding ( 39 ), patient triage or ordering of procedures ( 37 ).
AI and Agents for Management and Support Tasks
NLP applications, such as voice transcription, have proved helpful for clinical note-taking ( 40 ), compiling electronic health records, automatically generating medical reports from patient-doctor conversations or diagnostic reports ( 41 ). AI algorithms can help retrieving context-relevant patient data. Concept-based information retrieval can improve search accuracy and retrieval speed ( 42 ). AI algorithms can improve the use and allocation of hospital resources by predicting the length of stay of patients ( 43 ) or risk of re-admission ( 44 ).
Classification Based on Degree of Intrusion Into a Patient
Robotic systems can be used inside the body, on the body or outside the body. Those applied inside the body include microrobots ( 45 ), surgical robots and interventional robots. Microrobots are sub-millimeter untethered devices that can be propelled for example by chemical reactions ( 46 ), or physical fields ( 47 ). They can move unimpeded through the body and perform tasks such as targeted therapy (localized delivery of drugs) ( 48 ).
Microrobots can assist in physical surgery, for example by drilling through a blood clot or by opening up obstructions in the urinary tract to restore normal flow ( 49 ). They can provide directed local tissue heating to destroy cancer cells ( 50 ). They can be implanted to provide continuous remote monitoring and early awareness of an emerging disease.
Robotic prostheses, orthoses and exoskeletons are examples of robotic systems worn on the body. Exoskeletons are wearable robotic systems that are tightly physically coupled with a human body to provide assistance or enhance the wearer's physical capabilities ( 51 ). While they have often been developed for applications outside of health care, they can help workers with physically demanding tasks such as moving patients ( 52 ) or assist people with muscle weakness or movement disorders. Wearable technology can also be used to measure and transmit data about vital signs or physical activity ( 19 ).
Robotic systems applied outside the body can help avoid direct contact when treating patients with infectious diseases ( 53 ), assist in surgery (as already mentioned), including remote surgical procedures that leverage augmented reality ( 54 ) or assist providers when moving patients ( 55 ).
Classification Based on Care Setting
Another dimension of AI and robotics is the duration of their use, which directly correlates with the location of use. Both can significantly influence the requirements, design, and technology components of the solution. In a longer-term care setting, robotics can be used in a patient's home (e.g., for monitoring of vital signs) or for treatment in a nursing home. Shorter-term care settings include inpatient hospitals, palliative care facilities or inpatient psychiatric facilities. Example applications are listed in Table 1 .
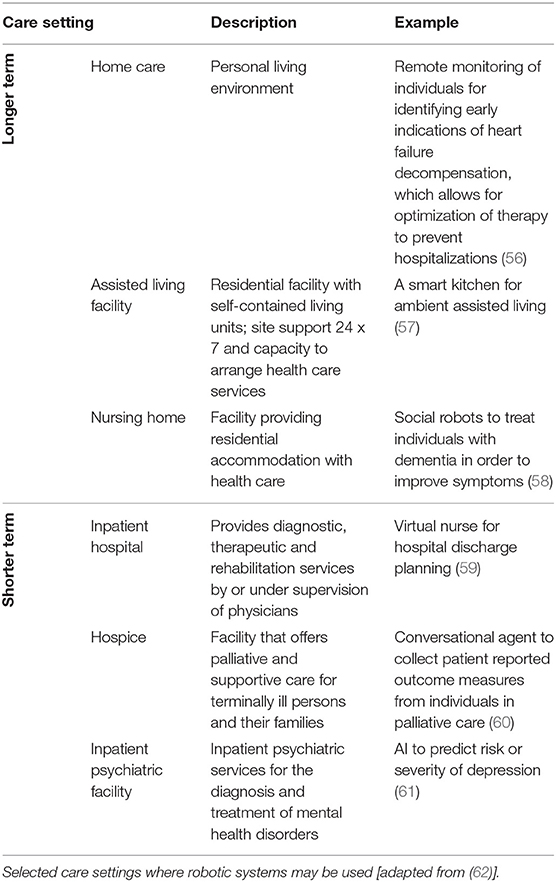
Table 1 . Classification by care setting.
Sample Realizations
Having seen how to classify AI and robotic systems in health care, we turn to recent concrete achievements that illustrate their practical application and achievements already realized. This list is definitely not exhaustive, but it illustrates the fact that we're no longer purely at the research or experimentation stage: the technology is starting to bear fruit in a very concrete way–that is, by improving outcomes–even when only in the context of clinical trials prior to regulatory approval for general use.
Sepsis Onset Prediction
Sepsis was recently identified as the leading cause of death worldwide, surpassing even cancer or cardiovascular diseases. 3 And while timely diagnosis and treatment are difficult in other care settings, it is also the leading cause of death in hospitals in the United States (Sepsis Fact Sheet 4 ) A key reason is the difficulty of recognizing precursor symptoms early enough to initiate effective treatment. Therefore, early onset prediction promises to save millions of lives each year. Here are four such projects:
• Bayesian Health 5 , a startup founded by a researcher at Johns Hopkins University, applied its model to a test population of hospital patients and correctly identified 82% of the 9,800 patients who later developed sepsis.
• Dascena, a California startup, has been testing its software on large cohorts of patients since 2017, achieving significant improvements in outcomes ( 63 ).
• Patchd 6 uses wearable devices and deep learning to predict sepsis in high-risk patients. Early studies have shown that this technology can predict sepsis 8 h earlier, and more accurately, than under existing standards of care.
• A team of researchers from Singapore developed a system that combines clinical measures (structured data) with physician notes (unstructured data), resulting in improved early detection while reducing false positives ( 64 ).
Monitoring Systems in the Intensive Care Unit
For patients in an ICU, the paradox is that large amounts of data are collected, displayed on monitors, and used to trigger alarms, but these various data streams are rarely used together, nor can doctors or nurses effectively observe all the data from all the patients all the time.
This is an area where much has been written, but most available information points to studies that have not resulted in actual deployments. A survey paper alluded in particular to the challenge of achieving effective collaboration between ICU staff and automated processes ( 65 ).
In one application example, machine learning helps resolving the asynchrony between a mechanical ventilator and the patient's own breathing reflexes, which can cause distress and complicate recovery ( 66 ).
Tumor Detection From Image Analysis
This is another area where research has provided evidence of the efficacy of AI, generally not employed alone but rather as an advisor to a medical professional, yet there are few actual deployments at scale.
These applications differ based on the location of the tumors, and therefore on the imaging techniques used to observe them. AI makes the interpretation of the images more reliable, generally by pinpointing to the radiologists areas they might otherwise overlook.
• In a study performed in Korea, AI appeared to improve the recognition of lung cancer in chest X-rays ( 67 ). AI by itself performed better than unaided radiologists, and the improvement was greater when AI was used as an aid by radiologists. Note however that the sample size was fairly small.
• Several successive efforts aimed to use AI to classify dermoscopic images to discriminate between benign nevi and melanoma ( 68 ).
AI for COVID-19 Detection
The rapid and tragic emergence of the COVID-19 disease, and its continued evolution at the time of this writing, have mobilized many researchers, including the AI community. This domain is naturally divided into two areas, diagnostic and treatment.
An example of AI applied to COVID-19 diagnostic is based on an early observation that the persistent cough that is one of the common symptoms of the disease “sounds different” from the cough caused by other ailments, such as the common cold. The MIT Opensigma project 7 has “crowdsourced” sound recordings of coughs from many people, most of whom do not have the disease while some know that they have it or had it. Several similar projects have been conducted elsewhere ( 69 ).
Another effort used AI to read computer tomography images to provide a rapid COVID-19 test, reportedly achieving over 90% accuracy in 15 s ( 70 ). Curiously, after this news was widely circulated in February-March 2020, nothing else was said for several months. Six months later, a blog post 8 from the University of Virginia radiology and medical department asserted that “CT scans and X-rays have a limited role in diagnosing coronavirus.” The approach pioneered in China may have been the right solution at a specific point in time (many cases concentrated in a small geographical area, requiring a massive detection effort before other rapid tests were available), thus overriding the drawbacks related to equipment cost and patient exposure to radiation.
Patient Triage and Symptom Checkers
While the word triage immediately evokes urgent decisions about what interventions to perform on acutely ill patients or accident victims, it can also be applied to remote patient assistance (e.g., telehealth applications), especially in areas underserved by medical staff and facilities.
In an emergency care setting, where triage decisions can result in the survival or death of a person, there is a natural reluctance to entrust such decisions to machines. However, AI as a predictor of outcomes could serve as an assistant to an emergency technician or doctor. A 2017 study of emergency room triage of patients with acute abdominal pain only showed an “acceptable level of accuracy” ( 71 ), but more recently, the Mayo Clinic introduced an AI-based “digital triage platform” from Diagnostic Robotics 9 to “perform clinical intake of patients and suggest diagnoses and hospital risk scores.” These solutions can now be delivered by a website or a smartphone app, and have evolved from decision trees designed by doctors to incorporate AI.
Cardiovascular Risk Prediction
Google Research announced in 2018 that it has achieved “prediction of cardiovascular risk factors from retinal fundus photographs via deep learning” with a level of accuracy similar to traditional methods such as blood tests for cholesterol levels ( 72 ). The novelty consists in the use of a neural network to analyze the retina image, resulting in more power at the expense of explainability.
In practice, the future of such a solution is unclear: certain risk factors could be assessed from the retinal scan, but those were often factors that could be measured directly anyway–such as from blood pressure.
Gait Analysis
Many physiological and neurological factors affect how someone walks, given the complex interactions between the sense of touch, the brain, the nervous system, and the muscles involved. Certain conditions, in particular Parkinson's disease, have been shown to affect a person's gait, causing visible symptoms that can help diagnose the disease or measure its progress. Even if an abnormal gait results from another cause, an accurate analysis can help assess the risk of falls in elderly patients.
Compared to other applications in this section, gait analysis has been practiced for a longer time (over a century) and has progressed incrementally as new motion capture methods (film, video, infrared cameras) were developed. In terms of knowledge representation, see for example the work done at MIT twenty years ago ( 73 ). Computer vision, combined with AI, can considerably improve gait analysis compared to a physician's simple observation. Companies such as Exer 10 offer solutions that physical therapists can use to assess patients, or that can help monitor and improve a home exercise program. This is an area where technology has already been deployed at scale: there are more than 60 clinical and research gate labs 11 in the U.S. alone.
Home Care Robots
Robots that provide assistance to elderly or sick persons have been the focus of research and development for several decades, particularly in Japan due to the country's large aging population with above-average longevity. “Elder care robots” can be deployed at home (with cost being an obvious issue for many customers) or in senior care environments ( 74 ), where they will help alleviate a severe shortage of nurses and specialized workers, which cannot be easily addressed through the hiring of foreign help given the language barrier.
The types of robots used in such settings are proliferating. They range from robots that help patients move or exercise, to robots that help with common tasks such as opening the front door to a visitor or bringing a cup of tea, to robots that provide psychological comfort and even some form of conversation. PARO, for instance, is a robotic bay seal developed to provide treatment to patients with dementia ( 75 ).
Biomechatronics
Biomechatronics combines biology, mechanical engineering, and electronics to design assistive devices that interpret inputs from sensors and send commands to actuators–with both sensors and actuators attached in some manner to the body. The sensors, actuators, control system, and the human subject form together a closed-loop control system.
Biomechatronic applications live at the boundary of prosthetics and robotics, for example to help amputees achieve close-to-normal motion of a prosthetic limb. This work has been demonstrated for many years, with impressive results, at the MIT Media Lab under Prof. Hugh Herr 12 However, those applications have rarely left the lab environment due to the device cost. That cost could be lowered by production in large quantities, but coverage by health insurance companies or agencies is likely to remain problematic.
Mapping of Use Cases to Classification
Table 2 shows a mapping of the above use cases to the classification introduced in the first section of this paper.
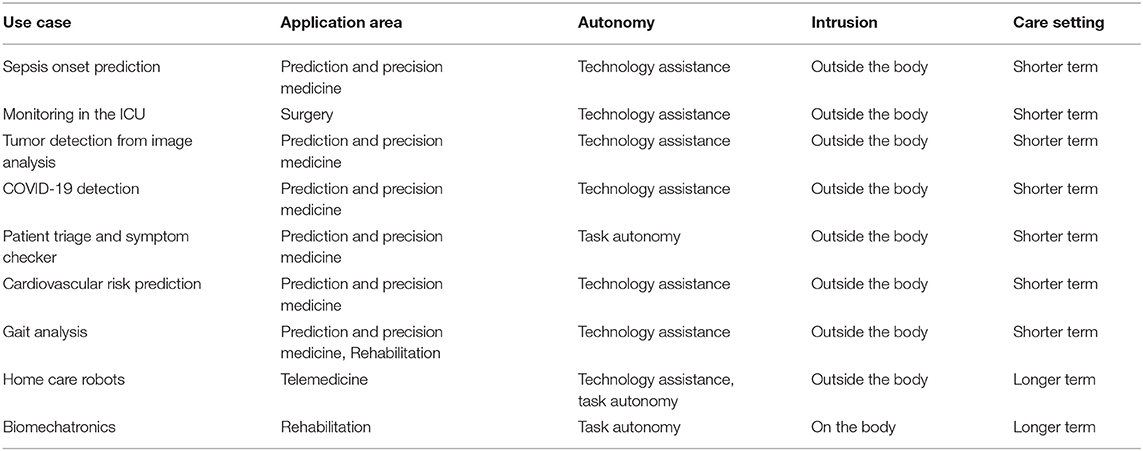
Table 2 . Mapping of use cases to our classification.
Adoption Challenges to AI and Robotics in Health Care
While the range of opportunities, and the achievements to date, of robotics and AI are impressive as seen above, multiple issues impede their deployment and acceptance in daily practice.
Issues related to trust, security, privacy and ethics are prevalent across all aspects of health care, and many are discussed elsewhere in this issue. We will therefore only briefly mention those challenges that are unique to AI and robotics.
Resistance to Technology
Health care professionals may ignore or resist new technologies for multiple reasons, including actual or perceived threats to professional status and autonomy ( 76 ), privacy concerns ( 77 ) or the unresolved legal and ethical questions of responsibility ( 78 ). The issues of worker displacement by robots are just as acute in health care as in other domains. Today, while surgery robots operate increasingly autonomously, humans still perform many tasks and play an essential role in determining the robot's course of operation (e.g., for selecting the process parameters or for the positioning of the patient) ( 79 ). This allocation of responsibilities is bound to evolve.
Transparency and Explainability
Explainability is “a characteristic of an AI-driven system allowing a person to reconstruct why a certain AI came up with the presented prediction” ( 80 ). In contrast to rule-based systems, AI-based predictions can often not be explained in a human-intelligible manner, which can hide errors or bias (the “black box problem” of machine learning). The explainability of AI models is an ongoing research area. When information on the reasons for an AI-based decision is missing, physicians cannot judge the reliability of the advice and there is a risk to patient safety.
Responsibility, Accountability and Liability
Who is responsible when the AI or robot makes mistakes or creates harm in patients? Is it the programmer, manufacturer, end user, the AI/robotic system itself, the provider of the training dataset, or something (or someone) else? The answer depends on the system's degree of autonomy. The European Parliament's 2017 Resolution on AI ( 81 ) assigns legal responsibility for an action of an AI or robotic system to a human actor, which may be its owner, developer, manufacturer or operator.
Data Protection
Machine learning requires access to large quantities of data regarding patients as well as healthy people. This raises issues regarding the ownership of data, protection against theft, compliance with regulations such as HIPAA in the U.S. ( 82 ) or GDPR for European citizens ( 83 ), and what level of anonymization of data is necessary and possible. Regarding the last point, AI models could have unintended consequences, and the evolution of science itself could make patient re-identification possible in the future.
Data Quality and Integration
Currently, the reliability and quality of data received from sensors and digital health devices remain uncertain ( 84 )–a fact that future research and development must address. Datasets in medicine are naturally imperfect (due to noise, errors in documentation, incompleteness, differences in documentation granularities, etc.), hence it is impossible to develop error-free machine learning models ( 80 ). Furthermore, without a way to quickly and reliably integrate the various data sources for analysis, there is lost potential for fast diagnosis by AI algorithms.

Safety and Security
Introducing AI and robotics into the delivery of health care is likely to create new risks and safety issues. Those will exist even under normal functioning circumstances, when they may be due to design, programming or configuration errors, or improper data preparation ( 85 ).
These issues only get worse when considering the probability of cyberattacks:
• Patient data may be exposed or stolen, perhaps by scammers who want to exploit it for profit.
• Security vulnerabilities in robots that interact directly with patients may cause malfunctions that physically threaten the patient or professional. The robot may cause harm directly, or indirectly by giving a surgeon incorrect feedback. In case of unexpected robot behavior, it may be unclear to the user whether the robot is functioning properly or is under attack ( 86 ).
The EU Commission recently drafted a legal framework 13 addressing the risks of AI (not only in health care) in order to improve the safety of and trust in AI. The framework distinguishes four levels of risks: unacceptable risk, high risk, limited risk and minimal risk. AI systems with unacceptable risks will be prohibited, high-risk ones will have to meet strict obligations before release (e.g., risk assessment and mitigation, traceability of results). Limited-risk applications such as chatbots (which can be used in telemedicine) will require “labeling” so that users are made aware that they are interacting with an AI-powered system.
While P5 medicine aims at considering multiple factors–ethnicity, gender, socio-economic background, education, etc.–to come up with individualized care, current implementations of AI often demonstrate potential biases toward certain patient groups of the population. The training datasets may have under-represented those groups, or important features may be distributed differently across groups–for example, cardiovascular disease or Parkinson's disease progress differently in men and women ( 87 ), so the corresponding features will vary. These causes result in undesirable bias and “unintended of unnecessary discrimination” of subgroups ( 88 ).
On the flip side, careful implementations of AI could explicitly consider gender, ethnicity, etc. differences to achieve more effective treatments for patients belonging to those groups. This can be considered “desirable bias” that counteracts the undesirable kind ( 89 ) and gets us closer to the goals of P5 medicine.
Trust–An Evolving Relationship
The relationship between patients and medical professionals has evolved over time, and AI is likely to impact it by inserting itself into the picture (see Figure 4 ). Although AI and robotics are performing well, human surveillance is still essential. Robots and AI algorithms operate logically, but health care often requires acting empathically. If doctors become intelligent users of AI, they may retain the trust associated with their role, but most patients, who have a limited understanding of the technologies involved, would have much difficulty in trusting AI ( 90 ). Conversely, reliable and accurate diagnosis and beneficial treatment, and appropriate use of AI and robotics by the physician can strengthen the patient's trust ( 91 ).
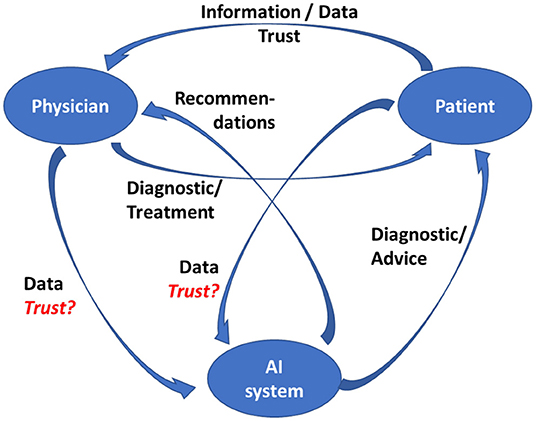
Figure 4 . Physician-patient-AI relationship.
This assumes of course that the designers of those systems adhere to established guidelines for trustworthy AI in the first place, which includes such requirements as creating systems that are lawful, ethical, and robust ( 92 , 93 ).
AI and Robotics for Transformed Health Care–A Converging Path
We can summarize the previous sections as follows:
1. There are many types of AI applications and robotic systems, which can be introduced in many aspects of health care.
2. AI's ability to digest and process enormous amounts of data, and derive conclusions that are not obvious to a human, holds the promise of more personalized and predictive care–key goals of P5 medicine.
3. There have been, over the last few years, a number of proof-of-concept and pilot projects that have exhibited promising results for diagnosis, treatment, and health maintenance. They have not yet been deployed at scale–in part because of the time it takes to fully evaluate their efficacy and safety.
4. There is a rather daunting list of challenges to address, most of which are not purely technical–the key one being demonstrating that the systems are effective and safe enough to warrant the confidence of both the practitioners and their patients.
Based on this analysis, what is the roadmap to success for these technologies, and how will they succeed in contributing to the future of health care? Figure 5 depicts the convergent approaches that need to be developed to ensure safe and productive adoption, in line with the P5 medicine principles.
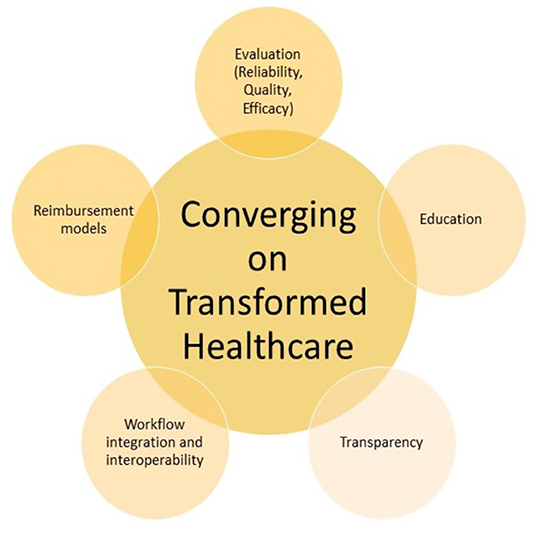
Figure 5 . Roadmap for transformed health care.
First, AI technology is currently undergoing a remarkable revival and being applied to many domains. Health applications will both benefit from and contribute to further advances. In areas such as image classification or natural language understanding, both of which have obvious utility in health care, the rate of progress is remarkable. Today's AI techniques may seem obsolete in ten years.
Second, the more technical challenges of AI–such as privacy, explainability, or fairness–are being worked on, both in the research community and in the legislative and regulatory world. Standard procedures for assessing the efficacy and safety of systems will be needed, but in reality, this is not a new concept: it is what has been developed over the years to approve new medicines. We need to be consistent and apply the same hard-headed validation processes to the new technologies.
Third, it should be clear from our exploration of this subject that education –of patients as well as of professionals–is key to the societal acceptance of the role that AI and robotics will be called upon to play. Every invention or innovation–from the steam engine to the telephone to the computer–has gone through this process. Practitioners must learn enough about how AI models and robotics work to build a “working relationship” with those tools and build trust in them–just as their predecessors learned to trust what they saw on an X-ray or CT scan. Patients, for their part, need to understand what AI and robotics can or cannot do, how the physician will remain in the loop when appropriate, and what data is being collected about them in the process. We will have a responsibility to ensure that complex systems that patients do not sufficiently understand cannot be misused against them, whether accidentally or deliberately.
Fourth, health care is also a business, involving financial transactions between patients, providers, and insurers (public or private, depending on the country). New cost and reimbursement models will need to be developed, especially given that when AI is used to assist professionals, not replace them, the cost of the system is additive to the human cost of assessing the data and reviewing the system's recommendations.
Fifth and last, clinical pathways have to be adapted and new role models for physicians have to be built. Clinical paths can already differ and make it harder to provide continuity of care to a patient who moves across care delivery systems that have different capabilities. This issue is being addressed by the BPM+ Health Community 14 using the business process, case management and decision modeling standards of the Object Management Group (OMG). The issue will become more complex by integrating AI and robotics: every doctor has similar training and a stethoscope, but not every doctor or hospital will have the same sensors, AI programs, or robots.
Eventually, the convergence of these approaches will help to build a complete digital patient model–a digital twin of each specific human being – generated out of all the data gathered from general practitioners, hospitals, laboratories, mHealth apps, and wearable sensors, along the entire life of the patient. At that point, AI will be able to support superior, fully personal and predictive medicine, while robotics will automate or support many aspects of treatment and care.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author Contributions
KD came up with the classification of AI and robotic systems. CB identified concrete application examples. Both authors contributed equally, identified adoption challenges, and developed recommendations for future work. Both authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. ^ https://cmte.ieee.org/futuredirections/2019/07/21/autonomous-systems-in-healthcare/
2. ^ https://emag.medicalexpo.com/ai-powered-chatbots-to-help-against-self-isolation-during-covid-19/
3. ^ https://www.med.ubc.ca/news/sepsis-leading-cause-of-death-worldwide/
4. ^ https://www.sepsis.org/wp-content/uploads/2017/05/Sepsis-Fact-Sheet-2018.pdf
5. ^ https://medcitynews.com/2021/07/johns-hopkins-spinoff-looking-to-build-better-risk-prediction-tooing,ls-emerges-with-15m/
6. ^ https://www.patchdmedical.com/
7. ^ https://hisigma.mit.edu
8. ^ https://blog.radiology.virginia.edu/covid-19-and-imaging/
9. ^ https://hitinfrastructure.com/news/diagnostic-robotics-mayo-clinic-bring-triage-platform-to-patients
10. ^ https://www.exer.ai
11. ^ https://www.gcmas.org/map
12. ^ https://www.media.mit.edu/groups/biomechatronics/overview/
13. ^ https://digital-strategy.ec.europa.eu/en/policies/regulatory-framework-ai
14. ^ https://www.bpm-plus.org/
1. Amisha Malik P, Pathania M, Rathaur VK. Overview of artificial intelligence in medicine. J Fam Med Prim Care. (2019) 8:2328–31. doi: 10.4103/jfmpc.jfmpc_440_19
PubMed Abstract | CrossRef Full Text | Google Scholar
2. van Melle W, Shortliffe EH, Buchanan BG. EMYCIN: a knowledge engineer's tool for constructing rule-based expert systems. In: Buchanan BG, Shortliffe EH, editors. Rule-Based Expert Systems . Reading, MA: Addison-Wesley Publishing Company (1984). p. 302–13.
3. Tursz T, Andre F, Lazar V, Lacroix L, Soria J-C. Implications of personalized medicine—perspective from a cancer center. Nat Rev Clin Oncol. (2011) 8:177–83. doi: 10.1038/nrclinonc.2010.222
4. van't Veer LJ, Dai H, van de Vijver MJ, He YD, Hart AAM, Mao M, et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature. (2002) 415:530–6. doi: 10.1038/415530a
5. Auffray C, Charron D, Hood L. Predictive, preventive, personalized and participatory medicine: back to the future. Genome Med. (2010) 2:57. doi: 10.1186/gm178
6. Hamet P, Tremblay J. Artificial intelligence in medicine. Metabolism. (2017) 69:S36–40. doi: 10.1016/j.metabol.2017.01.011
7. Kim J, Campbell AS, de Ávila BE-F, Wang J. Wearable biosensors for healthcare monitoring. Nat Biotechnol. (2019) 37:389–406. doi: 10.1038/s41587-019-0045-y
8. Nam KH, Kim DH, Choi BK, Han IH. Internet of things, digital biomarker, and artificial intelligence in spine: current and future perspectives. Neurospine. (2019) 16:705–11. doi: 10.14245/ns.1938388.194
9. Steels L, Lopez de, Mantaras R. The Barcelona declaration for the proper development and usage of artificial intelligence in Europe. AI Commun. (2018) 31:485–94. doi: 10.3233/AIC-180607
10. Olshannikova E, Ometov A, Koucheryavy Y, Olsson T. Visualizing big data with augmented and virtual reality: challenges and research agenda. J Big Data. (2015) 2:22. doi: 10.1186/s40537-015-0031-2
CrossRef Full Text
11. Björnsson B, Borrebaeck C, Elander N, Gasslander T, Gawel DR, Gustafsson M, et al. Digital twins to personalize medicine. Genome Med. (2019) 12:4. doi: 10.1186/s13073-019-0701-3
12. Bates M. Health care chatbots are here to help. IEEE Pulse. (2019) 10:12–4. doi: 10.1109/MPULS.2019.2911816
13. Corral-Acero J, Margara F, Marciniak M, Rodero C, Loncaric F, Feng Y, et al. The “Digital Twin” to enable the vision of precision cardiology. Eur Heart J. (2020) 41:4556–64. doi: 10.1093/eurheartj/ehaa159
14. Montani S, Striani M. Artificial intelligence in clinical decision support: a focused literature survey. Yearb Med Inform. (2019) 28:120–7. doi: 10.1055/s-0039-1677911
15. Oemig F, Blobel B. natural language processing supporting interoperability in healthcare. In: Biemann C, Mehler A, editors. Text Mining. Cham: Springer International Publishing (2014). p. 137–56. (Theory and Applications of Natural Language Processing). doi: 10.1007/978-3-319-12655-5_7
16. Bitterman DS, Aerts HJWL, Mak RH. Approaching autonomy in medical artificial intelligence. Lancet Digit Health. (2020) 2:e447–9. doi: 10.1016/S2589-7500(20)30187-4
17. Carriere J, Fong J, Meyer T, Sloboda R, Husain S, Usmani N, et al. An Admittance-Controlled Robotic Assistant for Semi-Autonomous Breast Ultrasound Scanning. In: 2019 International Symposium on Medical Robotics (ISMR). Atlanta, GA: IEEE (2019). p. 1–7. doi: 10.1109/ISMR.2019.8710206
CrossRef Full Text | Google Scholar
18. Tao R, Ocampo R, Fong J, Soleymani A, Tavakoli M. Modeling and emulating a physiotherapist's role in robot-assisted rehabilitation. Adv Intell Syst. (2020) 2:1900181. doi: 10.1002/aisy.201900181
19. Tavakoli M, Carriere J, Torabi A. Robotics, smart wearable technologies, and autonomous intelligent systems for healthcare during the COVID-19 pandemic: an analysis of the state of the art and future vision. Adv Intell Syst. (2020) 2:2000071. doi: 10.1002/aisy.202000071
20. Ahn HS, Yep W, Lim J, Ahn BK, Johanson DL, Hwang EJ, et al. Hospital receptionist robot v2: design for enhancing verbal interaction with social skills. In: 2019 28th IEEE International Conference on Robot and Human Interactive Communication (RO-MAN). New Delhi: IEEE (2019). p. 1–6. doi: 10.1109/RO-MAN46459.2019.8956300
21. Lane T. A short history of robotic surgery. Ann R Coll Surg Engl . (2018) 100:5–7. doi: 10.1308/rcsann.supp1.5
22. Mezger U, Jendrewski C, Bartels M. Navigation in surgery. Langenbecks Arch Surg. (2013) 398:501–14. doi: 10.1007/s00423-013-1059-4
23. Luxton DD, June JD, Sano A, Bickmore T. Intelligent mobile, wearable, and ambient technologies for behavioral health care. In: Artificial Intelligence in Behavioral and Mental Health Care . Elsevier (2016). p. 137–62. Available online at: https://linkinghub.elsevier.com/retrieve/pii/B9780124202481000064
Google Scholar
24. Casilari E, Oviedo-Jiménez MA. Automatic fall detection system based on the combined use of a smartphone and a smartwatch. PLoS ONE. (2015) 10:e0140929. doi: 10.1371/journal.pone.0140929
25. Sriram KNV, Palaniswamy S. Mobile robot assistance for disabled and senior citizens using hand gestures. In: 2019 International Conference on Power Electronics Applications and Technology in Present Energy Scenario (PETPES) . Mangalore: IEEE (2019). p. 1–6. doi: 10.1109/PETPES47060.2019.9003821
26. Nibras N, Liu C, Mottet D, Wang C, Reinkensmeyer D, Remy-Neris O, et al. Dissociating sensorimotor recovery and compensation during exoskeleton training following stroke. Front Hum Neurosci. (2021) 15:645021. doi: 10.3389/fnhum.2021.645021
27. Maciejasz P, Eschweiler J, Gerlach-Hahn K, Jansen-Troy A, Leonhardt S. A survey on robotic devices for upper limb rehabilitation. J NeuroEngineering Rehabil. (2014) 11:3. doi: 10.1186/1743-0003-11-3
28. Akbari A, Haghverd F, Behbahani S. Robotic home-based rehabilitation systems design: from a literature review to a conceptual framework for community-based remote therapy during COVID-19 pandemic. Front Robot AI. (2021) 8:612331. doi: 10.3389/frobt.2021.612331
29. Howard MC. A meta-analysis and systematic literature review of virtual reality rehabilitation programs. Comput Hum Behav. (2017) 70:317–27. doi: 10.1016/j.chb.2017.01.013
30. Gorman C, Gustafsson L. The use of augmented reality for rehabilitation after stroke: a narrative review. Disabil Rehabil Assist Technol . (2020) 17:409–17. doi: 10.1080/17483107.2020.1791264
31. Li A, Montaño Z, Chen VJ, Gold JI. Virtual reality and pain management: current trends and future directions. Pain Manag. (2011) 1:147–57. doi: 10.2217/pmt.10.15
32. Tulu B, Chatterjee S, Laxminarayan S. A taxonomy of telemedicine efforts with respect to applications, infrastructure, delivery tools, type of setting and purpose. In: Proceedings of the 38th Annual Hawaii International Conference on System Sciences . Big Island, HI: IEEE (2005). p. 147.
33. Lai L, Wittbold KA, Dadabhoy FZ, Sato R, Landman AB, Schwamm LH, et al. Digital triage: novel strategies for population health management in response to the COVID-19 pandemic. Healthc Amst Neth. (2020) 8:100493. doi: 10.1016/j.hjdsi.2020.100493
34. Valtolina S, Marchionna M. Design of a chatbot to assist the elderly. In: Fogli D, Tetteroo D, Barricelli BR, Borsci S, Markopoulos P, Papadopoulos GA, Editors. End-User Development . Cham: Springer International Publishing (2021). p. 153–68. (Lecture Notes in Computer Science; Bd. 12724).
PubMed Abstract | Google Scholar
35. Falck F, Doshi S, Tormento M, Nersisyan G, Smuts N, Lingi J, et al. Robot DE NIRO: a human-centered, autonomous, mobile research platform for cognitively-enhanced manipulation. Front Robot AI. (2020) 7:66. doi: 10.3389/frobt.2020.00066
36. Bohr A, Memarzadeh K, . (Eds.) The rise of artificial intelligence in healthcare applications. In: Artificial Intelligence in Healthcare . Oxford: Elsevier (2020). p. 25–60. doi: 10.1016/B978-0-12-818438-7.00002-2
37. Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med. (2020) 3:17. doi: 10.1038/s41746-020-0221-y
PubMed Abstract | CrossRef Full Text
38. Saddler N, Harvey G, Jessa K, Rosenfield D. Clinical decision support systems: opportunities in pediatric patient safety. Curr Treat Options Pediatr. (2020) 6:325–35. doi: 10.1007/s40746-020-00206-3
39. Deng H, Wu Q, Qin B, Chow SSM, Domingo-Ferrer J, Shi W. Tracing and revoking leaked credentials: accountability in leaking sensitive outsourced data. In: Proceedings of the 9th ACM Symposium on Information, Computer and Communications Security . New York, NY: Association for Computing Machinery (2014). p. 425–34. (ASIA CCS'14). doi: 10.1145/2590296.2590342
40. Leventhal R. How Natural Language Processing is Helping to Revitalize Physician Documentation . Cleveland, OH: Healthc Inform (2017). Vol. 34, p. 8–13.
41. Gu Q, Nie C, Zou R, Chen W, Zheng C, Zhu D, et al. Automatic generation of electromyogram diagnosis report. In: 2020 IEEE International Conference on Bioinformatics and Biomedicine (BIBM) . Seoul: IEEE (2020). p. 1645–50.
42. Jain V, Wason R, Chatterjee JM, Le D-N, editor. Ontology-Based Information Retrieval For Healthcare Systems. 1 st ed . Wiley-Scrivener (2020). doi: 10.1002/9781119641391
43. Awad A, Bader–El–Den M, McNicholas J. Patient length of stay and mortality prediction: a survey. Health Serv Manage Res. (2017) 30:105–20. doi: 10.1177/0951484817696212
44. Mahajan SM, Mahajan A, Nguyen C, Bui J, Abbott BT, Osborne TF. Predictive models for identifying risk of readmission after index hospitalization for hip arthroplasty: a systematic review. J Orthop. (2020) 22:73–85. doi: 10.1016/j.jor.2020.03.045
45. Ceylan H, Yasa IC, Kilic U, Hu W, Sitti M. Translational prospects of untethered medical microrobots. Prog Biomed Eng. (2019) 1:012002. doi: 10.1088/2516-1091/ab22d5
46. Sánchez S, Soler L, Katuri J. Chemically powered micro- and nanomotors. Angew Chem Int Ed Engl. (2015) 54:1414–44. doi: 10.1002/anie.201406096
47. Schuerle S, Soleimany AP, Yeh T, Anand GM, Häberli M, Fleming HE, et al. Synthetic and living micropropellers for convection-enhanced nanoparticle transport. Sci Adv. (2019) 5:eaav4803. doi: 10.1126/sciadv.aav4803
48. Erkoc P, Yasa IC, Ceylan H, Yasa O, Alapan Y, Sitti M. Mobile microrobots for active therapeutic delivery. Adv Ther. (2019) 2:1800064. doi: 10.1002/adtp.201800064
49. Yu C, Kim J, Choi H, Choi J, Jeong S, Cha K, et al. Novel electromagnetic actuation system for three-dimensional locomotion and drilling of intravascular microrobot. Sens Actuators Phys. (2010) 161:297–304. doi: 10.1016/j.sna.2010.04.037
50. Chang D, Lim M, Goos JACM, Qiao R, Ng YY, Mansfeld FM, et al. Biologically Targeted magnetic hyperthermia: potential and limitations. Front Pharmacol. (2018) 9:831. doi: 10.3389/fphar.2018.00831
51. Phan GH. Artificial intelligence in rehabilitation evaluation based robotic exoskeletons: a review. EEO. (2021) 20:6203–11. doi: 10.1007/978-981-16-9551-3_6
52. Hwang J, Kumar Yerriboina VN, Ari H, Kim JH. Effects of passive back-support exoskeletons on physical demands and usability during patient transfer tasks. Appl Ergon. (2021) 93:103373. doi: 10.1016/j.apergo.2021.103373
53. Hager G, Kumar V, Murphy R, Rus D, Taylor R. The Role of Robotics in Infectious Disease Crises. ArXiv201009909 Cs (2020).
54. Walker ME, Hedayati H, Szafir D. Robot teleoperation with augmented reality virtual surrogates. In: 2019 14th ACM/IEEE International Conference on Human-Robot Interaction (HRI) . Daegu: IEEE (2019). p. 202–10. doi: 10.1109/HRI.2019.8673306
55. Ding M, Matsubara T, Funaki Y, Ikeura R, Mukai T, Ogasawara T. Generation of comfortable lifting motion for a human transfer assistant robot. Int J Intell Robot Appl. (2017) 1:74–85. doi: 10.1007/s41315-016-0009-z
56. Mohebali D, Kittleson MM. Remote monitoring in heart failure: current and emerging technologies in the context of the pandemic. Heart. (2021) 107:366–72. doi: 10.1136/heartjnl-2020-318062
57. Blasco R, Marco Á, Casas R, Cirujano D, Picking R. A smart kitchen for ambient assisted living. Sensors. (2014) 14:1629–53. doi: 10.3390/s140101629
58. Valentí Soler M, Agüera-Ortiz L, Olazarán Rodríguez J, Mendoza Rebolledo C, Pérez Muñoz A, Rodríguez Pérez I, et al. Social robots in advanced dementia. Front Aging Neurosci. (2015) 7:133. doi: 10.3389/fnagi.2015.00133
59. Bickmore TW, Mitchell SE, Jack BW, Paasche-Orlow MK, Pfeifer LM, O'Donnell J. Response to a relational agent by hospital patients with depressive symptoms. Interact Comput. (2010) 22:289–98. doi: 10.1016/j.intcom.2009.12.001
60. Chatzimina M, Koumakis L, Marias K, Tsiknakis M. Employing conversational agents in palliative care: a feasibility study and preliminary assessment. In: 2019 IEEE 19th International Conference on Bioinformatics and Bioengineering (BIBE) . Athens: IEEE (2019). p. 489–96. doi: 10.1109/BIBE.2019.00095
61. Cecula P, Yu J, Dawoodbhoy FM, Delaney J, Tan J, Peacock I, et al. Applications of artificial intelligence to improve patient flow on mental health inpatient units - narrative literature review. Heliyon. (2021) 7:e06626. doi: 10.1016/j.heliyon.2021.e06626
62. Riek LD. Healthcare robotics. Comm ACM. (2017) 60:68–78. doi: 10.1145/3127874
63. Burdick H, Pino E, Gabel-Comeau D, McCoy A, Gu C, Roberts J, et al. Effect of a sepsis prediction algorithm on patient mortality, length of stay and readmission: a prospective multicentre clinical outcomes evaluation of real-world patient data from US hospitals. BMJ Health Care Inform. (2020) 27:e100109. doi: 10.1136/bmjhci-2019-100109
64. Goh KH, Wang L, Yeow AYK, Poh H, Li K, Yeow JJL, et al. Artificial intelligence in sepsis early prediction and diagnosis using unstructured data in healthcare. Nat Commun. (2021) 12:711. doi: 10.1038/s41467-021-20910-4
65. Uckun S. Intelligent systems in patient monitoring and therapy management. a survey of research projects. Int J Clin Monit Comput. (1994) 11:241–53. doi: 10.1007/BF01139876
66. Gholami B, Haddad WM, Bailey JM. AI in the ICU: in the intensive care unit, artificial intelligence can keep watch. IEEE Spectr. (2018) 55:31–5. doi: 10.1109/MSPEC.2018.8482421
67. Nam JG, Hwang EJ, Kim DS, Yoo S-J, Choi H, Goo JM, et al. Undetected lung cancer at posteroanterior chest radiography: potential role of a deep learning–based detection algorithm. Radiol Cardiothorac Imaging. (2020) 2:e190222. doi: 10.1148/ryct.2020190222
68. Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. (2017) 542:115–8. doi: 10.1038/nature21056
69. Scudellari M. AI Recognizes COVID-19 in the Sound of a Cough . Available online at: https://spectrum.ieee.org/the-human-os/artificial-intelligence/medical-ai/ai-recognizes-covid-19-in-the-sound-of-a-cough (accessed November 4, 2020).
70. Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. (2020) 296:E32–40. doi: 10.1148/radiol.2020200642
71. Farahmand S, Shabestari O, Pakrah M, Hossein-Nejad H, Arbab M, Bagheri-Hariri S. Artificial intelligence-based triage for patients with acute abdominal pain in emergency department; a diagnostic accuracy study. Adv J Emerg Med. (2017) 1:e5. doi: 10.22114/AJEM.v1i1.11
72. Poplin R, Varadarajan AV, Blumer K, Liu Y, McConnell MV, Corrado GS, et al. Prediction of cardiovascular risk factors from retinal fundus photographs via deep learning. Nat Biomed Eng. (2018) 2:158–64. doi: 10.1038/s41551-018-0195-0
73. Lee L. Gait analysis for classification . (Bd. Thesis Ph. D.)–Massachusetts Institute of Technology, Department of Electrical Engineering and Computer Science (2002). Available online at: http://hdl.handle.net/1721.1/8116
74. Foster M. Aging Japan: Robots May Have Role in Future of Elder Care . Healthcare & Pharma. Available online at: https://www.reuters.com/article/us-japan-ageing-robots-widerimage-idUSKBN1H33AB (accessed March 28, 2018).
75. Pu L, Moyle W, Jones C. How people with dementia perceive a therapeutic robot called PARO in relation to their pain and mood: a qualitative study. J Clin Nurs February. (2020) 29:437–46. doi: 10.1111/jocn.15104
76. Walter Z, Lopez MS. Physician acceptance of information technologies: role of perceived threat to professional autonomy. Decis Support Syst. (2008) 46:206–15. doi: 10.1016/j.dss.2008.06.004
77. Price WN, Cohen IG. Privacy in the age of medical big data. Nat Med. (2019) 25:37–43. doi: 10.1038/s41591-018-0272-7
78. Lamanna C, Byrne L. Should artificial intelligence augment medical decision making? the case for an autonomy algorithm. AMA J Ethics. (2018) 20:E902–910. doi: 10.1001/amajethics.2018.902
79. Fosch-Villaronga E, Drukarch H. On Healthcare Robots . Leiden: Leiden University (2021). Available online at: https://arxiv.org/ftp/arxiv/papers/2106/2106.03468.pdf
80. The The Precise4Q consortium, Amann J, Blasimme A, Vayena E, Frey D, Madai VI. Explainability for artificial intelligence in healthcare: a multidisciplinary perspective. BMC Med Inform Decis Mak . (2020) 20:310. doi: 10.1186/s12911-020-01332-6
81. European Parliament. Resolution with Recommendations to the Commission on Civil Law Rules on Robotics (2015/2103(INL)). (2017). Available online at: http://www.europarl.europa.eu/
82. Mercuri RT. The HIPAA-potamus in health care data security. Comm ACM. (2004) 47:25–8. doi: 10.1145/1005817.1005840
83. Marelli L, Lievevrouw E, Van Hoyweghen I. Fit for purpose? the GDPR and the governance of European digital health. Policy Stud. (2020) 41:447–67. doi: 10.1080/01442872.2020.1724929
84. Poitras I, Dupuis F, Bielmann M, Campeau-Lecours A, Mercier C, Bouyer L, et al. Validity and reliability of wearable sensors for joint angle estimation: a systematic review. Sensors. (2019) 19:1555. doi: 10.3390/s19071555
85. Macrae C. Governing the safety of artificial intelligence in healthcare. BMJ Qual Saf June. (2019) 28:495–8. doi: 10.1136/bmjqs-2019-009484
86. Fosch-Villaronga E, Mahler T. Cybersecurity, safety and robots: strengthening the link between cybersecurity and safety in the context of care robots. Comput Law Secur Rev. (2021) 41:105528. doi: 10.1016/j.clsr.2021.105528
87. Miller IN, Cronin-Golomb A. Gender differences in Parkinson's disease: clinical characteristics and cognition. Mov Disord Off J Mov Disord Soc. (2010) 25:2695–703. doi: 10.1002/mds.23388
88. Cirillo D, Catuara-Solarz S, Morey C, Guney E, Subirats L, Mellino S, et al. Sex and gender differences and biases in artificial intelligence for biomedicine and healthcare. Npj Digit Med. (2020) 3:81. doi: 10.1038/s41746-020-0288-5
89. Wolff RF, Moons KGM, Riley RD, Whiting PF, Westwood M, Collins GS, et al. PROBAST: a tool to assess the risk of bias and applicability of prediction model studies. Ann Intern Med. (2019) 170:51–8. doi: 10.7326/M18-1376
90. LaRosa E, Danks D. Impacts on trust of healthcare AI. In: Proceedings of the 2018 AAAI/ACM Conference on AI, Ethics, and Society . New Orleans, LA: ACM (2018). p. 210–5. doi: 10.1145/3278721.3278771
91. Lee D, Yoon SN. Application of artificial intelligence-based technologies in the healthcare industry: opportunities and challenges. Int J Environ Res Public Health. (2021) 18:271. doi: 10.3390/ijerph18010271
92. Smuha NA. Ethics guidelines for trustworthy AI. Comput Law Rev Int. (2019) 20:97–106. doi: 10.9785/cri-2019-200402
93. Grinbaum A, Chatila R, Devillers L, Ganascia J-G, Tessier C, Dauchet M. Ethics in robotics research: CERNA mission and context. IEEE Robot Autom Mag. (2017) 24:139–45. doi: 10.1109/MRA.2016.2611586
Keywords: artificial intelligence, robotics, healthcare, personalized medicine, P5 medicine
Citation: Denecke K and Baudoin CR (2022) A Review of Artificial Intelligence and Robotics in Transformed Health Ecosystems. Front. Med. 9:795957. doi: 10.3389/fmed.2022.795957
Received: 15 October 2021; Accepted: 15 June 2022; Published: 06 July 2022.
Reviewed by:
Copyright © 2022 Denecke and Baudoin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kerstin Denecke, kerstin.denecke@bfh.ch
This article is part of the Research Topic
Managing Healthcare Transformation Towards P5 Medicine
Robotics in HealthCare
Ieee account.
- Change Username/Password
- Update Address
Purchase Details
- Payment Options
- Order History
- View Purchased Documents
Profile Information
- Communications Preferences
- Profession and Education
- Technical Interests
- US & Canada: +1 800 678 4333
- Worldwide: +1 732 981 0060
- Contact & Support
- About IEEE Xplore
- Accessibility
- Terms of Use
- Nondiscrimination Policy
- Privacy & Opting Out of Cookies
A not-for-profit organization, IEEE is the world's largest technical professional organization dedicated to advancing technology for the benefit of humanity. © Copyright 2024 IEEE - All rights reserved. Use of this web site signifies your agreement to the terms and conditions.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(5); 2023 May
- PMC10287569

Artificial Intelligence With Robotics in Healthcare: A Narrative Review of Its Viability in India
1 Medical School, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, IND
Ashish Anjankar
2 Biochemistry, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, IND
This short review focuses on the emerging role of artificial intelligence (AI) with robotics in the healthcare sector. It may have particular utility for India, which has limited access to healthcare providers for a large growing population and limited health resources in rural India. AI works with an amalgamation of enormous amounts of data using fast and complex algorithms. This permits the software to quickly adapt the pattern of the data characteristics. It has the possibility to collide with most of the facets of the health system which may range from discovery to prediction and deterrence. The use of AI with robotics in the healthcare sector has shown a remarkable rising trend in the past few years. Functions like assistance with surgery, streamlining hospital logistics, and conducting routine checkups are some of the tasks that may be managed with great efficiency using artificial intelligence in urban and rural hospitals across the country. AI in the healthcare sector is advantageous in terms of ensuring exclusive patient care, safe working conditions where healthcare providers are at a lower risk of getting infected, and perfectly organized operational tasks. As the healthcare segment is globally recognized as one of the most dynamic and biggest industries, it tends to expedite development through modernization and original approaches. The future of this lucrative industry is looking forward to a great revolution aiming to create intelligent machines that work and respond like human beings. The future perspective of AI and robotics in the healthcare sector encompasses the care of elderly people, drug discovery, diagnosis of deadly diseases, a boost in clinical trials, remote patient monitoring, prediction of epidemic outbreaks, etc. However, the viability of using robotics in healthcare may be questionable in terms of expenditure, skilled workforce, and the conventional mindset of people. The biggest challenge is the replication of these technologies to the smaller towns and rural areas so that these facilities may reach the larger segment of the entire population of the country. This review aims to examine the adaptability and viability of these new technologies in the Indian scenario and identify the major challenges.
Introduction and background
The status of the healthcare sector in India is far from providing universal healthcare coverage to the entire population and lags behind many developing and few least developed countries in terms of health indicators. In addition to this, there are large disparities among various states in achieving the desired health outcomes, as well as the establishment of a sound information system. The adoption of the National Health Policy of India in 2017 has largely facilitated the bridging of the gap among various stakeholders of National Healthcare through the digital corridor. The policy recognizes the significant role of technology in healthcare delivery. It advocates the setting up of a National Digital health authority (NDHA) to regulate, develop and deploy digital health within the field of care. National Institution for Transforming India (NITI) Aayog, after being authorized by the Government of India to draft a National Strategy on Artificial Intelligence (AI) emphasized five sectors that would benefit the most from AI in 2018, of which healthcare is one [ 1 ].
The application of AI in healthcare may be classified into four broad categories, i.e. expressive, analytical, prognostic, and prescriptive. The gap created by a lack of skilled healthcare professionals can only be bridged by enhancing the use of AI in the health sector. Usual health issues can easily be diagnosed with the help of AI, thus reducing the workload of expert health professionals as well as reducing the cost of treatment in India [ 2 ]. It is envisaged that by the year 2035, AI would be able to enhance the economy of India by adding 957 billion USD to it (Accenture, 2017) [ 2 ]. AI will also prove to be a medium for reducing the economic disparity in the country. A report of the TCS global survey (TCS, 2017) projects that the visible reduction of jobs by AI could possibly be replaced by the creation of new jobs in the upcoming AI-integrated healthcare projects [ 2 ].
As a matter of fact, the healthcare setup in India is not perfect. It is deficient in terms of the availability of doctors, nurses, medical technicians, and healthcare facilities needed to attend to the community. The number of qualified doctors is insufficient for the rapidly growing needs of the Indian healthcare system. At the same time, these doctors are concentrated in urban areas and there is a huge gap in medical personnel in rural areas as compared to urban settings. Approximately 74% of the graduate doctors in India work in urban areas which cater to only about one-fourth of the population [ 3 ]. Because of the maldistribution of resources, each doctor serves 19,000 people [ 4 ]. India will need 2.3 million doctors by 2030 to reach the minimum doctor-patient ratio of 1:1000, which the World Health Organization recommends. The early ideas by a few dozen of healthcare startups have the potential to boost the Indian healthcare systems in the future and also have the capability to reduce the burden of the healthcare system.
Recently the coronavirus disease 2019 (COVID-19) pandemic posed a great challenge to the healthcare sector creating a huge demand for equipment, medicines AI-based applications, and robotics. Many reputed hospitals all over the world have switched over to AI and robotic procedures during the COVID-19 pandemic for functions like disinfection and screening of patients and employees at the entry point. Measures such as distantly supervised surgeries, distance education, telemedicine, and video conferencing with doctors were used during the recent pandemic. The experience gained during the pandemic has primarily enhanced the adaptability for use of robotics in the healthcare sector [ 5 ].
AI's major forms of relevance in healthcare are as follows: 1. Machine learning: The use and development of complete systems that are able to learn and adapt without explicit instructions to analyze and draw inferences from data patterns; 2. Natural language processing: A specialized branch of AI focused on the interpretation and manipulation of human-generated written or spoken data; 3. Robotic process automation: An automation technology that uses software to mimic the back office tasks of human workers, such as extracting data, filling the forms, moving files, etc.
In addition, AI also supports the healthcare system in diagnosis and treatment applications, patient engagement and adherence, and administrative applications [ 6 ]. AI not only simplifies the work of doctors, nurses, and other healthcare workers but also saves an ample amount of time. Thus the adoption of digital solutions for the prevention, diagnosis, and cure of various ailments is the wise route for India to deal with the aim of providing health for all.
Research methodology
The present study was conducted between the months of April to June 2022. Databases like Pubmed and Google Scholar were mainly used to search the literature. Databases like Scopus and Web of Science were excluded. Most of the research publications taken into account for gathering the data were from 2013 to 2022. Research papers related to the use of robotics and artificial intelligence in healthcare were thoroughly studied with special emphasis on its viability in the Indian scenario. The relevant search terms used were artificial intelligence, robotics, healthcare, India, etc. It was a difficult task to explore the required information, as meager data is available regarding the use of robotics in the Indian healthcare sector which requires enhanced attention of researchers.
Functioning of robotics in healthcare
Working of robotics in healthcare comprises AI applications like machine learning and deep learning. AI works with an amalgamation of vast amounts of data using fast and intelligent algorithms. This permits the software to quickly adapt the pattern of the data characteristics. Execution of AI is basically program oriented and the designed program consists of the basic information as to how it has to work. All the data is fed into web platforms such as the “cloud” which have the potential to store massive data and information to be used through the internet. There are immense possibilities for development in the healthcare sector through the use of AI in the future [ 7 ].
The main objective of AI is to solve problems by gathering and analyzing the information provided by the program and sensors. Another goal is to learn and respond in uncommon situations by taking alternate ways and remembering the successful alternative to be used in similar situations. It works for creating proficient arrangements so that it can learn, think, and suggest the best possible ways to the users. They work towards accomplishing intellect in machines so that they can perform just like human beings [ 8 ].
Artificial intelligence has the possibility to collide with most of the facets of the health system which may range from discovery to forecast and deterrence. Although the rate of adherence to the new technologies is much lower than their appearance, it is needed that all healthcare professionals be trained uniformly to adopt these new technologies which include techniques like robotic process automation, natural language processing, machine learning, etc. [ 9 ]. The interplay between artificial intelligence, machine learning, and deep learning ultimately leads to the working of robotics in healthcare, which can be seen in Figure Figure1 1 .

Use of robotics in healthcare
Assistance in Surgery
The application of robotics in surgery was first imagined in 1967, but it was just a dream for about 30 years until the United States defense department set up research organizations that gradually developed the first surgical robot designed to conduct different types of tasks. Initially, these robots were used during wars on the battlefields [ 10 ].
Today the most rapidly growing field with the application of robotics in healthcare is surgery. It aims to enhance the capabilities of humans and overcome human limitations in the field of surgery [ 11 ]. In India, the first urologic robot named da Vinci S was set up at the All India Institute of Medical Sciences, New Delhi in 2006. This initiation was followed by an exceptional expansion of robotic surgery in the country. Till July 2019 there were 66 centers and more than 500 skilled robotic surgeons in India who had successfully performed more than 12,800 surgeries with the assistance of robots [ 12 ]. This unexpected expansion of robotic surgery shows that the future of robotic surgery in India is very bright. The introduction of the da Vinci Surgical System is one of the biggest inventions in surgery [ 8 ]. The use of high-definition computer vision enables surgeons to get detailed information about the inner condition of the patients which enhances their performance during the surgery [ 13 ].
For many years engineers and medical researchers, are constantly trying to invent ways in which robotics can be used in surgery, as it has advantages like mechanical accuracy, permanence, and the ability to work in unsafe surroundings [ 14 ]. In the past few years, surgeries assisted by robots have played a significant role in boosting the Indian healthcare system. Reports show that hundreds of robotic surgeons are positioned at different hospitals in India. Surgeries performed with the help of robotics are thought to be better in comparison to other conventional methods due to their precision, shorter recovery periods, lesser pain, and blood loss. These kinds of surgeries are also preferred because they save traveling and boarding costs [ 15 ].
Robotic surgery has successfully sorted the limitations of laparoscopic surgery which is a big leap toward surgery with minimal access. As it may be predicted that almost all surgeries will be performed with robotic assistance in the future, a realistic training approach will be required to enhance the skills of surgeons, thus reshaping the knowledge curvature of the trainees by exposure to new methods like robotic surgical simulators and robotic telementoring [ 16 ]. The role of robotics is increasingly becoming crucial in surgeon training. For example, virtual reality simulators provide realistic situations and real training experiences to the trainees. Practicing the procedures becomes easy within the virtual environment [ 17 ].
Surgical robots are widely being used in over a million surgical actions related to various departments of the healthcare sector. AI helps the surgeon to get actual warnings and suggest appropriately during the process. Profound learning data helps a lot to provide the best surgical application suitable for the patient [ 18 ]. Robotics is also helpful in facilitating experts who are often concentrated in big cities and are not available for patients residing in small towns and rural areas.
Support to Healthcare Workers
In addition to assistance in the operating room, robotics are also useful in clinics and Outdoor Patient Departments to enhance patient care. For example, robots were used to screen suspected patients at the entrance of health facilities during the COVID-19 pandemic. The use of automation and robots can also be seen in research laboratories where they are used to conduct many manual and repetitive tasks so that scientists can focus on more deliberate tasks and move faster towards discoveries. Remedial treatment after strokes, paralysis, traumatic brain injuries, etc. can be ensured with the help of therapeutic robots. These robots can monitor the patients as they perform prescribed exercises, and measure degrees of motion in various positions in a better way compared to the human eye. Social robots can also be used to interact with patients and also encourage them [ 19 ].
Logistic Arrangements
Medical robots efficiently streamline workflows and reduce risk which makes them more feasible to be used for many purposes. For example, robots can clean and organize patients' rooms autonomously, thus lowering the risk of interpersonal contact in infectious disease wards. Thus, for cleaning purposes, human support robots (HSR) are used [ 20 ]. Enabled medicine identifier software in robots helps in the distribution of medicines to patients in hospitals. Due to this kind of support hospital staff can devote more time to giving direct care to the patients.
Advantages of using robotics in healthcare
Exclusive Patient Care
Socially assistive robots (SARs) are the result of the development of AI along with physically assisted technologies. SARs are emotionally intelligent machines that lead to exclusive patient care, as these are capable of communicating with patients through a communicative range that makes them respond emotionally. The different types of response include interaction, communication, companionship, and emotional attachment [ 12 ]. Judicious use of robotics in the healthcare system ensures excellent patient care, perfect processes in medical surroundings, and a secure atmosphere for patients and medical professionals. Chances of human error and negligence are meager with the use of automated robots in healthcare. The health and social care sector is redefined by the invention and continuous development of SARs [ 12 ].
Protected Working Conditions
The role of nurses, ward boys, receptionists, and other healthcare workers can be easily performed by robots. The different types of robots: (i) receptionist robots, (ii) medical servers, (iii) nurse robots, etc., are capable of performing the above-mentioned roles very efficiently [ 15 ]. Automated mobile robots (AMRs) are used in many health facilities such as to distribute medical supplies and linen, collect data and information about patients, and serve food and water to patients in hospitals in order to keep medical professionals safe from pathogen exposure and thus prevent the spread of infections. Therefore, these robots were vigorously used during the recent COVID-19 pandemic. According to Podpora et al., hospitality robots like Wegree and Pepper developed by SoftBank Robotics in Japan were the most used robots during the pandemic, as they were helpful to control the rate of spreading of disease [ 15 ]. During the COVID-19 pandemic, excellent work was done for pandemic preparedness, screening, contact tracing, disinfecting, and enforcing quarantine and social distancing. The Arogya Setu app which was developed by National Informatics Centre and Information Technology Ministry has proven to be a boon in the management of the COVID-19 pandemic. Social robots are used for doing strenuous work like lifting heavy beds or transferring patients, thus reducing the physical strain on healthcare workers.
Organized Operational Tasks
Automated mobile robots (AMRs) regularize regular tasks, decrease the physical burden on health workers, and make sure that more precise procedures are used. These robots can address the shortage of staff, keep a trail of records and place orders on time. They ensure that medicines and other equipment are available as and when needed. Rooms can be quickly cleaned and sanitized and are timely ready for incoming patients by automated robots which enable health professionals to perform other important patient-related jobs. Robots can be efficiently used for making diagnoses of different diseases by using artificial intelligence. The radiologist robots, which are equipped with computational imaging capabilities, are used for making diagnoses with the help of AI through deep learning. These robots are also used for doing diagnosis procedures like MRIs and X-rays and hence are of great advantage for healthcare workers, as it protects them from harmful radiations used in these procedures [ 15 ].
Future perspective
The healthcare segment is globally recognized as one of the most dynamic and biggest industries. It aims to expedite development through modernization and original approaches. Previously this sector was reliant upon manual processes which required more time and were prone to human errors. The latest discoveries in machine learning have brought a revolution in the health sector which aims to create intelligent machines that work and respond like actual persons [ 8 ]. Although the application of AI and robotics in the healthcare sector is still in its infant stage, the future seems to be very bright in terms of acceptability and viability [ 21 ]. The fields prone to fast adaptability of AI and robotics in healthcare are as follows:
Care for Elderly People
It is predicted that the population of elderly people will double globally by 2050. Socially assistive robot technology may emerge as a solution to this growing demand. The major factors that enhance loneliness among older people living alone are ownership of the house, marital status, bad health, and lack of people to support. A study conducted by Abdi et al. has revealed that the role of social robots is crucial in healthcare of the elderly people [ 22 ]. Although many participants of the study were hesitant to accept the significance of robots taking their care, it was quite evident that they were equally apprehensive about having humans as caretakers. Many participants accepted that humanoid robots are programmed with positive human qualities and therefore are more reliable than humans. It can be said that role of robots in taking care of elderly people will prove to be a milestone in the present scenario where the number of elderly people is increasing in India due to improved health services and there is an apparent gap between the demand and supply of trained professionals in hospitals to address the surging need [ 22 ].
Mental commit robots are being developed for the therapy of elderly patients in hospitals. These robots are capable of providing a psychological, physiological, and social impact on human beings through physical contact. It was observed that the mood of elderly people improved with this input [ 23 ]. Several studies are underway to explore the possibilities of expanding the capabilities of social robots to improve their communication with human beings. The physical appearance of the robot largely influences its acceptability by elderly people. Positive results have been seen in older adults suffering from dementia when they were provided with companion animal robots. Studies demonstrate that companion animal robots of appropriate size, weight, and shape are capable of providing cognitive stimulation to elderly people having dementia [ 24 ]. Animal robot like seal PARO developed by Japan's National Institute of Advanced Industrial Science and Technology (AIST) have proven to be quite advantageous for improving the cognitive abilities and sleeping patterns of older adults [ 25 ].
Drug Discovery
One of the major areas where the use of AI can prove to be a boon is the field of drug discovery. It takes about 14 years and an average of 2.6 billion dollars for a new drug to reach the market through conventional procedures, whereas the same can be done using AI in a lesser amount of time. Recently in 2015, the outbreak of the Ebola virus in West Africa and some European countries were controlled with the application of AI which helped to discover an appropriate drug in a very meager time and prevented the outbreak from becoming a global pandemic [ 8 ]. In addition to this, it has been proven that it takes very little time to conduct clinical trials of newly discovered drugs using AI [ 8 ]. AI can also be used to recognize cardiotoxic and non-cardiotoxic drugs of the anticancer group. It is also capable of identifying probable antibiotics from a list of thousands of molecules and can be used as a medium to discover new antibiotics. These algorithms are also being used to identify the molecule with the potential to combat antimicrobial resistance leading to resistance from antibiotics. Studies are underway to explore the role of AI in combating fast-growing antibiotic resistance [ 26 ].
AI in Diagnosis
Reports say that about 80,000 people die every year due to wrong diagnoses of illnesses. Loads of excessive cases with partial details have led to severe mistakes in the past. As AI is resistant to these errors, it is capable of predicting and diagnosing diseases at a faster pace [ 27 ]. The use of AI is extensively explored in the detection of cancer where early detection and prediction are very important. Many companies are using AI-supported tools for diagnosing and detecting different kinds of cancer [ 28 ].
Boost in Clinical Trials
Previously the process of clinical trials was very slow and success rates were very poor. Before the year 2000, the success rate of completing the clinical trials via all three stages, for the candidates was only 13.8% [ 29 ]. The execution of AI has reduced the cycle time and has also impacted the production cost and outcome in a positive direction. The AI helps in ensuring the continuous flow of clinical trial data and also coding, storing, and managing them. Details of patients saved in the computer can be analyzed and the lessons learned can be used for future trials, thus saving time and cost [ 30 ]. It also works efficiently to observe the patients consistently and share the data across different computers. The self-learning capacity of AI enhances the accuracy of the trial and foresees the chances of dropouts [ 31 ].
Consultation in Digital Mode
The idea of digital consultation is aimed at lessening hospital visits for minor ailments, which can be cured easily at home with the guidance of a medical professional. Several apps are using AI for collecting information from patients based on a questionnaire and then facilitating the consultation with a medical practitioner [ 32 ]. In the future, digital consultation through AI will be the most viable and efficient way for the treatment of common diseases. It would also help people to find good doctors near their houses with the help of AI and internet hospitals.
Remote Patient Monitoring
The concept of remote patient monitoring has evolved very fast with the application of AI sensors and advanced predictive analysis. Apart from personal sensors and devices for monitoring health like glucometers, blood pressure monitors, etc., more advanced systems are now coming up like smart implants and smart prosthetics which are used for post-operative rehabilitation purposes to avoid complications after surgery. Smart implants help in monitoring the patient's conditions such as movements, muscle strength, etc which are important parameters for assessing the rate of recovery. Sensors implanted within the muscles or nerves are quite helpful in providing consistent information about the healing process of the patient.
In recent times many new forms are coming up for patient monitoring, such as digital pills, nanorobots, smart fabrics, etc. These monitoring tools are used for ensuring regular medication, wound management, and management of cardiac diseases by keeping track of patients' emotional, physiological, and mental status [ 33 ]. It is calculated that by 2025 the market of AI-based monitoring tools and other wearables will be widely accepted by 50% of the population in developed countries [ 34 ]. The initial data and the details during the time of discharge are collected through cell phones having Wi-Fi or Bluetooth. It is further stored in the cloud and constant monitoring is done to avoid complications and readmissions to the hospitals. The review is shared with the patient with recommendations through the internet [ 35 ].
AI in Nanotechnology Research
Recent advances have been made in the field of medicine using nanotechnology. AI tools can be successfully merged with nanotechnology to understand the various events happening in the nanosystems. This can help in designing and developing drugs by developing the nanosystems [ 36 ]. The field of nanomedicine has grown and continues to develop, numerous approaches have been experimented with successfully to provide several curative instruments in predetermined doses. This advancement has greatly helped in getting efficient results in combination therapy [ 37 ].
Prediction of an Epidemic Outbreak
One of the most amazing tasks of AI in healthcare is that it is capable of forecasting the outbreak of an epidemic. Although it cannot control or mitigate the outbreak, it can warn us beforehand to make preparations in time. It gathers, analyses and monitors the inflow of data through machine learning or social networking sites to locate the epicenter of the endemic. The calculation is done by generating an algorithm by collecting all the data from the news bulletins in all languages, airline ticketing, and reports related to plant and animal diseases [ 38 ]. On 30th December 2019, the AI engine Blue Dot found groups of uncommon pneumonia cases occurring in the wet and dry markets of Wuhan, China, and alerted the government and other stakeholders. This was the first warning signal of the novel COVID-19 pandemic [ 39 ]. Figure Figure2 2 depicts the various future perspectives of AI and robotics in the field of healthcare.

Barriers to using AI in India
Besides the innumerable benefits of employing robotics in health facilities, there are chances of errors and mechanical failures too. One mechanical breakdown can cost a precious human life. Apparently, there are several disadvantages of robots in the healthcare sector, especially in the Indian scenario.
High cost is the major limitation of introducing robotics in healthcare. In India priority is given to the large burden of contagious diseases like tuberculosis and malaria. The introduction of robotics will be an additional load on the meager budget of the healthcare sector for non-prioritized work. The cost of buying and maintaining the robots is very high. Besides this, the expenditure is very huge for setting up a unit appropriate for robotic operations.
Another drawback of the present robotic systems used for different healthcare applications is their narrow spectrum for customization. Every patient is different and hence, customization of the healthcare service systems is the need of the hour, for both patients as well as healthcare professionals. Hence, the current healthcare system needs to be more flexible in respect of providing robotic services that can be easily acceptable as per the patient's needs [ 40 ]. The use of surgical robots is practically limited to developed countries, advanced research centers, and super specialty hospitals. Practically it is out of reach for patients from a very big section of society in India who actually need it. Expensive robotic interventions are not feasible at the small town and village hospitals where they are actually needed due to excessive workload and lack of health professionals in government-owned health facilities.
Studies related to adverse events in robotic surgery show that several undesirable events were recorded including injuries and deaths due to device fault. Robots are mechanical devices and are susceptible to breakdowns and errors. Shortage of power and lack of other infrastructural facilities do not permit access to the use of robotics universally in the Indian healthcare system. In addition to this, positions of medical professionals at the grass root level are largely vacant and the lack of a trained and skilled workforce for operating and maintaining the robotics and AI system is a challenge. The interconnection between AI and computer programming has a major impact on health and care innovation, where benevolent service delivery systems are increasingly becoming important. These mechanical systems focus on affinity, including the essence of passionate and moral relationships along with therapeutic considerations [ 12 ].
Due to its growing popularity, there is also a threat of an increase in irrational demand for robotic surgery in India where the literacy rate and awareness about health are poor. This may lead to hospitals buying robots for commercial publicity and push doctors into unethical use of robotics.
The use of robotics in healthcare also has major medico-legal problems. Like other computers, the surgical robot may also be affected by virus threats and may not adhere to the surgeon's commands, thus leading to a hazardous situation. The government has taken steps to strengthen the medical education system and the delivery of healthcare in rural areas. The introduction of robotics working with mechanical procedures in the healthcare sector in India will possibly deduct the empathy and humanitarian aspect of treatment which is highly appreciated in the Indian scenario where a big percentage of the population is illiterate with low socio-economic status.
Apart from this, there are insufficient laws to address security and privacy issues arising out of data storage through artificial intelligence in the healthcare sector in India [ 2 ]. Quality training of the huge and diversified workforce related to the use of AI and robotics in healthcare is another major challenge that needs to be addressed. More and more simulation-based trainings are required to be performed at all levels to enhance the skills of surgeons regarding minimally invasive and robotic colorectal surgery [ 18 ].
Conclusions
Although the introduction of robots in healthcare is in its infant stage, it offers a lot of opportunities for medical professionals, especially in the urban setting. The significant role of AI in areas like drug discovery, diagnosis of diseases, digital medical consultations, robotic surgeries, remote patient monitoring and prediction of epidemic outbreaks cannot be denied. The emerging role of robotics in care of elderly people has been recognized and is gradually being accepted by Indian society. In the present scenario it is not possible to think about implementation and monitoring of health services in the absence of AI and robotics. Many new techniques are underway in the use of robotics in the health sector which may be more cost-effective in the future. But the quality of robotic procedures needs to be controlled by establishing a stringent and continuous monitoring system. Use of AI and robotics in healthcare sector in India may prove to be a milestone in improving the present status of healthcare services. It has certainly helped in bridging the gap created by lack of skilled health professionals as well as the huge vacancies of doctors, nurses and paramedical staff. The main challenge is to reach the remote regions of the country with poor infrastructural facilities and lack of advanced technologies. The high cost of using AI and robotics in the healthcare sector stands as the major barrier in the path of reaching the disadvantaged community. Besides this, there are chances of errors and mechanical failures due to improper maintenance arrangements resulting in fatal consequences. The Indian government should support companies to invest in AI and encourage public-private partnership (PPP) in the domain of AI and health. The ethical issues must be addressed by the policy makers to enhance the use of AI and robotics in the healthcare sector. After considering the various facts and practicality, it can be said that the use of robotics in India should be expanded in a phased manner initiating with the reputed and equipped hospitals. It is viable only if used judiciously with a standardized reporting and monitoring system in place.
The authors have declared that no competing interests exist.
Advertisement
Robotics in Medical Domain: The Future of Surgery, Healthcare and Imaging
- Published: 04 October 2023
- Volume 132 , pages 2885–2903, ( 2023 )
Cite this article

- Anisha Halder Roy 1 ,
- Sanchita Ghosh 2 &
- Bharat Gupta ORCID: orcid.org/0000-0002-4705-700X 3
358 Accesses
Explore all metrics
Robotics is a popular branch of Machine Learning that has grown the interest of researchers for many years. Machine learning is used for developing various robotic systems which find their applications in different sectors specially in medical domain. This paper shows how robotics have evolved over the years and how robots are helping doctors as a medical assistant in their everyday work like surgeries, medical imaging, healthcare, manufacturing Prosthetics and patients aids, rehabilitation etc. Even major surgeries like Eye Surgery, Heart Surgery, Soft Surgery Operations, Abdominal Surgeries, and Orthopaedics etc. can be done by medical robots to make life easier for both doctors and patients. The main reasons of increasing robotic helps in healthcare sector are (a) robots are tireless, (b) they don’t take stress, (c) their hand never shakes, (d) can do repetitive work effortlessly, (e) can perform precise surgeries. Here, we have reviewed few of robotics application in medical field and discussed all the merits, demerits and future aspects in this regards.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

Application of Robotics in the Healthcare Industry
Surgical robotics beyond enhanced dexterity instrumentation: a survey of machine learning techniques and their role in intelligent and autonomous surgical actions.

Contribution of Robotics in Medical Applications A Literary Survey
Data availability.
No data set is used.
Denecke, K., & Baudoin, C. R. (2022). A Review of Artificial Intelligence and Robotics in Transformed Health Ecosystems. Frontiers in Medicine (Lausanne), 9 , 795957. https://doi.org/10.3389/fmed.2022.795957
Article Google Scholar
Lanfranco, A. R., Castellanos, A. E., Desai, J. P., & Meyers, W. C. (2004). Robotic surgery: A current perspective. Annals of Surgery, 239 (1), 14–21. https://doi.org/10.1097/01.sla.0000103020.19595.7d
Ngu, J. C., Tsang, C. B., & Koh, D. C. (2017). The da Vinci Xi: A review of its capabilities, versatility, and potential role in robotic colorectal surgery. Robotic Surgery, 4 , 77–85. https://doi.org/10.2147/RSRR.S119317
Kraft, B. M., Jäger, C., Kraft, K., Leibl, B. J., & Bittner, R. (2004). The AESOP robot system in laparoscopic surgery: Increased risk or advantage for surgeon and patient? Surgical Endoscopy, 18 (8), 1216–1223. https://doi.org/10.1007/s00464-003-9200-z
Dardona, T., Eslamian, S., Reisner, L. A., & Pandya, A. (2019). Remote presence: Development and usability evaluation of a head-mounted display for camera control on the da Vinci Surgical system. Robotics, 8 (2), 31. https://doi.org/10.3390/robotics8020031
Miura, K., Kadone, H., Koda, M., Abe, T., Endo, H., Murakami, H., Doita, M., Kumagai, H., Nagashima, K., Fujii, K., Noguchi, H., Funayama, T., Kawamoto, H., Sankai, Y., & Yamazaki, M. (2018). The hybrid assisted limb (HAL) for Care Support, a motion assisting robot providing exoskeletal lumbar support, can potentially reduce lumbar load in repetitive snow-shoveling movements. Journal of Clinical Neuroscience, 49 , 83–86. https://doi.org/10.1016/j.jocn.2017.11.020
Gardner, A. D., Potgieter, J. & Noble, F. K. (2017). A review of commercially available exoskeletons’ capabilities. In 2017 24th International Conference on Mechatronics and Machine Vision in Practice (M2VIP) (pp. 1–5). https://doi.org/10.1109/M2VIP.2017.8211470
González-Jiménez, J., Galindo, C., & Ruiz-Sarmiento, J. R. (2012). Technical improvements of the Giraff telepresence robot based on users’ evaluation. Proceedings—IEEE International Workshop on Robot and Human Interactive Communication . https://doi.org/10.1109/ROMAN.2012.6343854
Qureshi, M. O., & Syed, R. S. (2014). The impact of robotics on employment and motivation of employees in the service sector, with special reference to health care. Safety and Health at Work, 5 (4), 198–202. https://doi.org/10.1016/j.shaw.2014.07.003
Kim, J., Gu, G. M., & Heo, P. (2016). Robotics for healthcare. In H. Jo, H. W. Jun, J. Shin, & S. Lee (Eds.), Biomedical engineering: Frontier research and converging technologies. Biosystems & biorobotics. (Vol. 9). Springer. https://doi.org/10.1007/978-3-319-21813-7_21
Chapter Google Scholar
Coleman-Wood, K., Lathan, C., & Kaufman, K. (2009). Development of an interactive upper extremity gestural robotic feedback system: From bench to reality. In Conference proceedings: ... Annual international conference of the IEEE engineering in medicine and biology society . IEEE Engineering in Medicine and Biology Society. Conference (pp. 5973–5976). https://doi.org/10.1109/IEMBS.2009.5333523 .
Palagi, S., & Fischer, P. (2018). Bioinspired microrobots. Nature Reviews Materials, 3 , 113–124. https://doi.org/10.1038/s41578-018-0016-9
Soriano, G. P., Yasuhara, Y., Ito, H., Matsumoto, K., Osaka, K., Kai, Y., Locsin, R., Schoenhofer, S., & Tanioka, T. (2022). Robots and robotics in nursing. Healthcare, 10 (8), 1571. https://doi.org/10.3390/healthcare10081571
Guru, K. A., Esfahani, E. T., Raza, S. J., Bhat, R., Wang, K., Hammond, Y., Wilding, G., Peabody, J. O., & Chowriappa, A. J. (2015). Cognitive skills assessment during robotic-assisted surgery: Separating the wheat from the chaff. BJU International, 115 (1), 166–174. https://doi.org/10.1111/bju.12657
Hung, A. J., Chen, J., & Gill, I. S. (2018). Automated performance metricsand machine learning algorithms to measure surgeon performance and anticipate clinical outcomes in robotic surgery. JAMA Surgery, 153 (8), 770–771. https://doi.org/10.1001/jamasurg.2018.1512
Habuza, T., Navaz, A. N., Hashim, F., Alnajjar, F., Zaki, N., Serhani, M. A., & Statsenko, Y. (2021). AI applications in robotics, diagnostic image analysis and precision medicine: Current limitations, future trends, guidelines on CAD systems for medicine. Informatics in Medicine Unlocked . https://doi.org/10.1016/j.imu.2021.100596
Grischke, J., Johannsmeier, L., Eich, L., Griga, L., & Haddadin, S. (2020). Dentronics: Towards robotics and artificial intelligence in dentistry. Dental Materials, 36 (6), 765–778. https://doi.org/10.1016/j.dental.2020.03.021
Raabe, D., Alemzadeh, K., Harrison, A. J. L., & Ireland, A. J. (2009). The chewing robot: A new biologically-inspired way to evaluate dental restorative materials. In 2009 Annual international conference of the IEEE engineering in medicine and biology society (pp. 6050–6053). https://doi.org/10.1109/IEMBS.2009.5332590
Carvalho, A., Brito, P., Santos, J., Caramelo, F. J., Veiga, G., Vasconcelos, B., et al. (2011). Evaluation of two dental impression materials using a robot arm. Bulletin du GIRSO, 50 , 36–37.
Google Scholar
Mohammad, S. (2013). Robotic surgery. Journal of Oral Biology and Craniofacial Research., 3 (1), 2. https://doi.org/10.1016/j.jobcr.2013.03.002
Zhang, Y. D., Jiang, J. G., Liang, T., & Hu, W. P. (2011). Kinematics modeling and experimentation of the multi-manipulator tooth-arrangement robot for full denture manufacturing. Journal of Medical Systems, 35 , 1421–1429.
Zhu, Z. A., Lu, Y. C., You, C. H., & Chiang, C. K. (2019). Deep learning for sensor-based rehabilitation exercise recognition and evaluation. Sensors (Basel)., 19 (4), 887. https://doi.org/10.3390/s19040887
Hamidah, A., Adiono, T., Syafalni, I., Andriana, M., Kurnia, M., Ratunanda, S. (2019). Review on machine learning applications in assisted treadmill for stroke rehabilitation. In 2019 International symposium on electronics and smart devices (ISESD) (pp. 1–5). https://doi.org/10.1109/ISESD.2019.8909416
Jamin, P., Duret, C., Hutin, E., Bayle, N., Koeppel, T., Gracies, J.-M., & Pila, O. (2022). Using robot-based variables during upper limb robot-assisted training in subacute stroke patients to quantify treatment dose. Sensors, 22 (8), 2989. https://doi.org/10.3390/s22082989
Zhang, W., Su, C., & He, C. (2020). Rehabilitation exercise recognition and evaluation based on smart sensors with deep learning framework. IEEE Access, 8 , 77561–77571. https://doi.org/10.1109/ACCESS.2020.2989128
Liu, Z., Liu, Q., Xu, W., Wang, L., & Zhou, Z. (2020). Robot learning towards smart robotic manufacturing: A review. Robotics and Computer-Integrated Manufacturing, 77 , 102360.
Shoushtari, A. L., Dario, P., & Mazzoleni, S. (2016). A review on the evolvement trend of robotic interaction control. Industrial Robot: An International Journal, 43 (5), 535.
Krebs, H. I., & Hogan, N. (2006). Therapeutic robotics: A technology push. Proceedings of the IEEE, 94 (9), 1727–1738. https://doi.org/10.1109/JPROC.2006.880721
Kong, K., & Tomizuka, M. (2009). Control of exoskeletons inspired by fictitious gain in human model. IEEE/ASME Transactions on Mechatronics, 14 (6), 689–698.
Atashzar, S. F., Shahbazi, M., Tavakoli, M., & Patel, R. V. (2017). A grasp-based passivity signature for haptics-enabled human–robot interaction: Application to design of a new safety mechanism for robotic rehabilitation. The International Journal of Robotics Research, 36 (5–7), 778.
Miyake, H., Motoyama, D., Matsushita, Y., Watanabe, H., Tamura, K., Otsuka, A., & Fujisawa, M. (2023). Initial experience of robot-assisted partial nephrectomy using hinotori surgical robot system: Single institutional prospective assessment of perioperative outcomes in 30 cases. Journal of Endourology . https://doi.org/10.1089/end.2022.0775,37,5,(531-534)
Qian, L., Wu, J. Y., DiMaio, S. P., Navab, N., & Kazanzides, P. (2020). A review of augmented reality in robotic-assisted surgery. IEEE Transactions on Medical Robotics and Bionics, 2 (1), 1–16. https://doi.org/10.1109/TMRB.2019.2957061
Choi, P. J., Oskouian, R. J., & Tubbs, R. S. (2018). Telesurgery: Past, present, and future. Cureus., 10 (5), e2716. https://doi.org/10.7759/cureus.2716
Xiong, L., Chng, C. B., Chui, C. K., Yu, P., & Li, Y. (2017). Shared control of a medical robot with haptic guidance. International Journal of Computer Assisted Radiology and Surgery, 12 (1), 137–147. https://doi.org/10.1007/s11548-016-1425-0
Almujalhem, A., & Rha, K. H. (2020). Surgical robotic systems: What we have now? A urological perspective. Buji Compasss, 1 (5), 152–159. https://doi.org/10.1002/bco2.31
http://bme240.eng.uci.edu/students/10s/sgupta1/Developments.html
Mirbagheri, A., Farahmand, F., Sarkar, S., Alamdar, A., Moradi, M., & Afshari, E. (2020). The sina robotic telesurgery system. In Handbook of robotic and image-guided surgery (pp. 107–121). Elsevier. https://doi.org/10.1016/B978-0-12-814245-5.00007-4
Wang, G., Zeng, Y., & Sheng, X. (2021). Instructions for use of Da Vinci surgical robots. In G. Wang, Y. Zeng, & X. Sheng (Eds.), Robotic surgery and nursing. Springer. https://doi.org/10.1007/978-981-16-0510-9_2
Gorpas, D., Phipps, J., Bec, J., et al. (2019). Autofluorescence lifetime augmented reality as a means for real-time robotic surgery guidance in human patients. Science and Reports, 9 , 1187. https://doi.org/10.1038/s41598-018-37237-8
Winata, S. (2018). Wireless teleoperation control interface of articulated forceps for minimally invasive surgery. https://doi.org/10.13140/RG.2.2.16450.43201
Pakkasjärvi, N., Luthra, T., & Anand, S. (2023). Artificial intelligence in surgical learning. Surgeries, 4 (1), 86–97. https://doi.org/10.3390/surgeries4010010
Morgan, A. A., Abdi, J., Syed, M. A. Q., Kohen, G. E., Barlow, P., & Vizcaychipi, M. P. (2022). Robots in healthcare: A scoping review. Current Robotics Reports, 3 (4), 271–280. https://doi.org/10.1007/s43154-022-00095-4
Kyrarini, M., Lygerakis, F., Rajavenkatanarayanan, A., et al. (2021). A survey of robots in healthcare. Technologies, 9 , 8. https://doi.org/10.3390/technologies9010008
Eto, M., & Naito, S. (2005). Robotic surgery assisted by the ZEUS system. In H. Kumon, M. Murai, & S. Baba (Eds.), Endourooncology. Recent advances in endourology. (Vol. 6). Springer. https://doi.org/10.1007/4-431-27173-2_4
Muradore, R., Bresolin, D., Geretti, L., Fiorini, P., & Villa, T. (2011). Robotic surgery. IEEE Robotics & Automation Magazine, 18 (3), 24–32. https://doi.org/10.1109/MRA.2011.942112
Article MATH Google Scholar
Masamune, K., & Hong, J. (2014). Advanced imaging and robotics technologies for medical applications. International Journal of Optomechatronics, 4 (5), 299–321. https://doi.org/10.1080/15599612.2011.633210
Erin, O., Boyvat, M., Tiryaki, M. E., Phelan, M., & Sitti, M. (2019). Magnetic resonance imaging system–driven medical robotics. Advanced Intelligent Systems . https://doi.org/10.1002/aisy.201900110
Spin-Neto, R., Mudrak, J., Matzen, L. H., Christensen, J., Gotfredsen, E., & Wenzel, A. (2013) Cone beam CT image artefacts related to head motion simulated by a robot skull: Visual characteristics and impact on image quality.
Burdea, G. C., Dunn, S. M., Elmendorf, C. H., & Mallik, M. (1991). Real-time sensing of tooth position for dental digital subtraction radiography. IEEE Transactions on Biomedical Engineering, 38 , 366–378.
Ebert, L. C., Ptacek, W., Naether, S., Fürst, M., Ross, S., Buck, U., Weber, S., & Thali, M. (2010). Virtobot—A multi-functional robotic system for 3D surface scanning and automatic post mortem biopsy. The International Journal of Medical Robotics Computer Assisted Surgery: MRCAS, 6 , 18–27.
Won, H. J., Kim, N., Kim, G. B., Seo, J. B., & Kim, H. (2017). Validation of a CT-guided intervention robot for biopsy and radiofrequency ablation: Experimental study with an abdominal phantom. Diagnostic and Interventional Radiology., 23 (3), 233–237. https://doi.org/10.5152/dir.2017.16422
Frutiger, D. R., Vollmers, K., Kratochvil, B. E., & Nelson, B. J. (2010). Small, fast, and under control: wireless resonant magnetic micro-agents. Int. J. Rob. Res., 29 , 613.
Spin-Neto, R., Matzen, L. H., Schropp, L. W., Sørensen, T. S., & Wenzel, A. (2018). An ex vivo study of automated motion artefact correction and the impact on cone beam CT image quality and interpretability. Dentomaxillofacial Radiology., 47 (5), 20180013. https://doi.org/10.1259/dmfr.20180013
Kummer, M. P., Abbott, J. J., Kratochvil, B. E., Borer, R., Sengul, A., & Nelson, B. J. (2010). OctoMag: An electromagnetic system for 5-DOF wireless micromanipulation. IEEE Transactions on Robotics, 26 , 1006.
Son, D., Dogan, M. D., & Sitti, M. (2017) In IEEE International Conference on Robotics and Automation (p. 1132). IEEE
Niravkumar, P., Jiawen, Y., Gang, L., Reza, M., Lukasz, P., Helen, D.-S., Joyce, J., Andrew, D., Andreas, M., Karun, S., Iulian, I., & Kevin, C. (2021). Body-mounted robotic system for MRI-guided shoulder arthrography: Cadaver and clinical workflow studies. Frontiers in Robotics and AI . https://doi.org/10.3389/frobt.2021.667121
Hashem, J. A., Pryor, M., Landsberger, S., Hunter, J., & Janecky, D. R. (2018). Automating high-precision X-ray and neutron imaging applications with robotics. IEEE Transactions on Automation Science and Engineering, 15 (2), 663–674. https://doi.org/10.1109/TASE.2017.2675709
Von Haxthausen, F., Böttger, S., Wulff, D., et al. (2021). Medical robotics for ultrasound imaging: Current systems and future trends. Curr Robot Rep, 2 , 55–71. https://doi.org/10.1007/s43154-020-00037-y
MGIUS-R3 robotic ultrasound system [Internet]. Available from: https://en.mgitech.cn/products/instruments_info/11/
Adams, S. J., Burbridge, B. E., Badea, A., Kanigan, N., Bustamante, L., Babyn, P., et al. (2018). A crossover comparison of standard and telerobotic approaches to prenatal sonography. Journal of Ultrasound in Medicine, 37 , 2603–2612. https://doi.org/10.1002/jum.14619
Georgescu, M., Sacccomandi, A., Baudron, B., & Arbeille, P. L. (2016). Remote sonography in routine clinical practice between two isolated medical centers and the university hospital using a robotic arm: A 1-year study. Telemedicine Journal and E-Health, 22 , 276–281. https://doi.org/10.1089/tmj.2015.0100
Avgousti, S., Panayides, A. S., Jossif, A. P., Christoforou, E. G., Vieyres, P., Novales, C., et al. (2016). Cardiac ultrasonography over 4G wireless networks using a tele-operated robot. Healthcare Technology Letters, 3 , 212–217. https://doi.org/10.1049/htl.2016.0043
Mathiassen, K., Fjellin, J. E., Glette, K., Hol, P. K., & Elle, O. J. (2016). An ultrasound robotic system using the commercial robot UR5. Frontiers in Robotics AI, 3 , 1. https://doi.org/10.3389/frobt.2016.00001
Geng, C., Xie, Q., Chen, L., Li, A., & Qin, B. (2020) Study and analysis of a remote robot-assisted ultrasound imaging system. In 2020 IEEE 4th information technology, networking, electronic and automation control conference (ITNEC) (pp. 389–393) IEEE. https://doi.org/10.1109/ITNEC48623.2020.9084796
Huang, Q., & Lan, J. (2019). Remote control of a robotic prosthesis arm with six-degree-of-freedom for ultrasonic scanning and three-dimensional imaging. Biomedical Signal Processing and Control, 54 , 101606. https://doi.org/10.1016/j.bspc.2019.101606
Merouche, S., Allard, L., Montagnon, E., Soulez, G., Bigras, P., & Cloutier, G. (2016). A robotic ultrasound scanner for automatic vessel tracking and three-dimensional reconstruction of b-mode images. IEEE Transactions on Ultrasonics, Ferroelectrics, and Frequency Control, 63 , 35–46. https://doi.org/10.1109/TUFFC.2015.2499084
Holland, J., Kingston, L., McCarthy, C., Armstrong, E., O’Dwyer, P., Merz, F., & McConnell, M. (2021). Service robots in the healthcare sector. Robotics, 10 (1), 47. https://doi.org/10.3390/robotics10010047
Bezerra Junior, J. E., Queiroz, P. G. G., & de Lima, R. W. (2018). A study of the publications of educational robotics: A systematic review of literature. IEEE Latin America Transactions, 16 (4), 1193–1199. https://doi.org/10.1109/TLA.2018.8362156
Cesta, A., Cortellessa, G., Orlandini, A., & Tiberio, L. (2016). Long-term evaluation of a telepresence robot for the elderly: Methodology and ecological case study. International Journal of Social Robotics . https://doi.org/10.1007/s12369-016-0337-z
Nickelsen, N. C. M., & Abildgaard, J. S. (2022). The entwinement of policy, design and care scripts: Providing alternative choice-dependency situations with care robots. Sociology of Health and Illness . https://doi.org/10.1111/1467-9566.13434
Malik, N., Hanapiah, F., Rahman, R. A. A., & Yussof, H. (2016). Emergence of socially assistive robotics in rehabilitation for children with cerebral palsy: A review. International Journal of Advanced Robotic Systems . https://doi.org/10.5772/64163
https://www.medlabmag.com/article/1094/Fall_2012/RoboCourier_from_Swisslog/
Hang, Su., & De Momi, E. (2023). Towards human activity recognition enhanced robot assisted surgery. Robot Design, 123 , 143.
Hashimoto, D. A., Rosman, G., Witkowski, E. R., Stafford, C., Navarette- Welton, A. J., Rattner, D. W., Lillemoe, K. D., Rus, D. L., & Meireles, O. R. (2019). Computer vision analysis of intraoperative video: Automated recognition of operative steps in laparoscopic sleeve gastrectomy. Annals of Surg, 270 , 414–421. https://doi.org/10.1097/SLA.0000000000003460
Vedula, S. S., Ishii, M., & Hager, G. D. (2017). Objective assessment of surgical technical skill and competency in the operating room. Annual Review of Biomedical Engineering, 19 (1), 301–325. https://doi.org/10.1146/annurev-bioeng-071516-044435
Gomez, E. D., Aggarwal, R., McMahanW, B. K., & Kuchenbecker, K. J. (2016). Objective assessment of robotic surgical skill using instrument contact vibrations. Surgical Endoscopy, 30 , 1419–1431. https://doi.org/10.1007/s00464-015-4346-z
Egert, M., Steward, J. E., & Sundaram, C. P. (2020). Machine learning and artificial intelligence in surgical fields. Indian Journal of Surgical Oncology, 11 , 573–577. https://doi.org/10.1007/s13193-020-01166-8
Carpenter, B. T., & Sundaram, C. P. (2017). Training the next generation of surgeons in robotic surgery. Robotics Surgery, 4 , 39–44. https://doi.org/10.2147/RSRR/S70552
Sridhar, A. N., Briggs, T. P., Kelly, J. D., et al. (2017). Training in robotic surgery—An overview. Current Urology Reports, 18 , 58. https://doi.org/10.1007/s11934-017-0710-y
Kim, B., & Deshpande, A. D. (2017). An upper-body rehabilitation exoskeleton Harmony with an anatomical shoulder mechanism: Design, modeling, control, and performance evaluation. The International Journal of Robotics Research, 36 , 414–435.
Yang, B., Huang, J., Chen, X., Xiong, C., & Hasegawa, Y. (2021). Supernumerary robotic limbs: A review and future outlook. IEEE Transactions on Medical Robotics and Bionics, 3 (3), 623–639. https://doi.org/10.1109/TMRB.2021.3086016
https://www.jhuapl.edu/prosthetics
Tran, P., Jeong, S., Herrin, K. R., & Desai, J. P. (2021). Review: Hand exoskeleton systems, clinical rehabilitation practices, and future prospects. IEEE Transactions on Medical Robotics and Bionics, 3 (3), 606–622. https://doi.org/10.1109/TMRB.2021.3100625
https://news.brown.edu/articles/2012/05/braingate2
Laut, J., Porfiri, M., & Raghavan, P. (2016). The present and future of robotic technology in rehabilitation. Current Physical Medicine and Rehabilitation Reports, 4 (4), 312.
https://www.physiopedia.com/Robotic_Rehabilitation_for_the_Lower_Extremity
https://www.hocoma.com/
Ogata, T., Abe, H., Samura, K., Hamada, O., Nonaka, M., Iwaasa, M., Higashi, T., Fukuda, H., Shiota, E., Tsuboi, Y., & Inoue, T. (2015). Hybrid assistive limb (HAL) rehabilitation in patients with acute hemorrhagic stroke. Neurologia Medico-Chirurgica (Tokyo)., 55 (12), 901–906. https://doi.org/10.2176/nmc.oa.2015-0209
https://ir.eksobionics.com/press-releases/detail/570/ekso-gt-robotic-exoskeletoncleared-by-fda-for-use-with
Buettner, R., Renner, A., & Boos, A. (2020) A systematic literature review of research in the surgical field of medical robotics. In 2020 IEEE 44th annual computers, software, and applications conference (COMPSAC) (pp. 517–522). https://doi.org/10.1109/COMPSAC48688.2020.0-200
Goh, E. Z., & Ali, T. (2022). Robotic surgery: An evolution in practice. Journal of Surgical Protocols and Research Methodologies, 2022 (1), snac003. https://doi.org/10.1093/jsprm/snac003
Habuza, T., Navaz, A. N., Hashim, F., Alnajjar, F., Zaki, N., Serhani, M. A., & Statsenko, Y. (2021). AI applications in robotics, diagnostic image analysis and precision medicine: Current limitations, future trends, guidelines on CAD systems for medicine. Informatics in Medicine Unlocked, 24 , 100596.
Chang, K. D., Raheem, A. A., & Rha, K. H. (2018). Novel robotic systems and future directions. Indian Journal of Urology, 34 (2), 110–114. https://doi.org/10.4103/iju.IJU_316_17
Salcudean, S. E., Moradi, H., Black, D. G., & Navab, N. (2022). Robot-assisted medical imaging: A review. Proceedings of the IEEE, 110 (7), 951–967. https://doi.org/10.1109/JPROC.2022.3162840
Burdea, G. C., Dunn, S. M., & Levy, G. (1999). Evaluation of robot-based registration for subtraction radiography. Medical Image Analysis, 3 , 265–274.
Morgan, A. A., Abdi, J., Syed, M. A. Q., et al. (2022). Robots in healthcare: A scoping review. Current Robotics Reports, 3 , 271–280. https://doi.org/10.1007/s43154-022-00095-4
Download references
All authors have no sources of funding to report.
Author information
Authors and affiliations.
Radio Physics and Electronics Department, University of Calcutta, Kolkata, India
Anisha Halder Roy
IT Department, Institute of Engineering and Management, Kolkata, India
Sanchita Ghosh
ECE Department, NIT Patna, Patna, India
Bharat Gupta
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Bharat Gupta .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Halder Roy, A., Ghosh, S. & Gupta, B. Robotics in Medical Domain: The Future of Surgery, Healthcare and Imaging. Wireless Pers Commun 132 , 2885–2903 (2023). https://doi.org/10.1007/s11277-023-10747-z
Download citation
Accepted : 03 September 2023
Published : 04 October 2023
Issue Date : October 2023
DOI : https://doi.org/10.1007/s11277-023-10747-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Surgical robots
- Patients aid
- Rehabilitation
- Machine learning
- Find a journal
- Publish with us
- Track your research
Robotics in Healthcare

CITATION: Alvey, R. (2021). Robotics in Healthcare. Online Journal of Nursing Informatics (OJNI), 25 (2). https://www.himss.org/resources/online-journal-nursing-informatics
The healthcare field is constantly looking for ways to support and evolve the care that is being delivered to patients. In recent years, these efforts have included the incorporation of various technologies into healthcare delivery. While one such technological advancement -robotics- has yet to become a standard fixture of any healthcare organization, it is reasonable to believe that this will not remain the case for much longer. As such, it is important to understand how robots are currently being used throughout the healthcare field, as well as how they are being received by patients and healthcare professionals. Identifying any potential issues that could impact the current or future use of robots in the healthcare field is vital for the continued growth of these technologies.
The purpose of this literature review is to investigate and identify the ways in which robots are currently being utilized to reinforce or supplement the provision of patient care. In addition, this review will collect and analyze data related to the prevailing attitudes regarding the use of robots in patient care settings. This analysis will include the viewpoints of both healthcare professionals and patients.
Literature Review
Search Process
Research for this review was performed by searching the following databases: ProQuest and CINAHL Complete. The following keywords were used to guide these searches: robot, robotics, nurse, patients, and healthcare . Initial search results were then filtered to include only peer-reviewed, full text articles. Additional filters were applied to ensure that the articles were written in the English language and published in the past three years. The search of the ProQuest database returned 200 results, while the search of the CINAHL Complete database returned 33 results, for a total of 233 articles.
After the initial 233 articles were identified, the articles were screened for possible inclusion or exclusion. Of the 200 articles identified in the search of the ProQuest database, only the 50 most relevant were considered for this screening process, while all the articles identified in the search of the CINAHL Complete database were screened. In total, 287 articles were excluded, leaving 17 articles eligible for inclusion in the literature review. Most of these articles were excluded because they were not relevant to the study, while others were removed from consideration due to the brevity of the article.
As the assembled literature was reviewed, two distinct themes began to present themselves. The first of these themes involved the various ways in which robotics is being leveraged in the modern healthcare field. The second theme that emerged had to do with the way in which certain populations of people regard the addition of robots and related technologies to the healthcare field.
Current Utilization of Robots in Healthcare
The literature review revealed that there are robots of different shapes and sizes that are currently being utilized in some healthcare settings (Grobbel et al., 2019). One setting that has been profoundly impacted by robotics is the operating room (Suriaga, 2019). Robot-assisted surgeries have been performed since 1985. Over the years, the associated technologies have continued to improve and provide benefits, such as increased dexterity and decreased fatigue, to surgeons. Other common healthcare-related uses for robots involve the delivery of medical supplies or medications to nursing units, the cleaning and sanitation of the healthcare environment, and the provision of companionship to patients (Grobbel et al., 2019). Other studies are being conducted to determine their effectiveness in other clinical situations. For example, feasibility studies have been conducted in Denmark to determine the benefits of using robots to provide passive mobilization to elderly hospitalized patients (Bertelsen et al., 2020).
Other studies have been conducted that were aimed at determining if the use of robots can increase the effectiveness of clinical education and training. An example of this is the study performed by Shaw et al. (2018) that involved the use of robots to act as physical surrogates for nursing students during clinical simulations. The nursing students involved in this study were required to remotely control the actions of a mobile robot that was outfitted with video and audio capabilities. This was done to identify any issues that might arise if this kind of robot were to be used to provide inclusion in clinical simulations for geographically distant students.
Current Attitudes Towards Robots
The literature also showed that there were a few ways in which the utilization of robots in the healthcare field is being perceived, by both the clinicians that provide these services, and by the patients that receive them. One article detailed a study that was conducted in an urban area of the western United States. This study found that older adult patients did not hold as many negative attitudes about robots as the researchers had hypothesized (Backonja, 2018). The researchers also discovered that most of the older adult patients involved in the study shared these feelings. A study was conducted in Portugal to help evaluate interactions between older adult patients and robots (Pereira et al., 2018). The results of this study were then planned to be incorporated into the technology, to strengthen future patient-robot social algorithms.
One particularly interesting fact is that most of the studies that involved patient perspectives on robots were conducted in countries other than the United States. For example, a study in Korea found that some nurses believed that robots can assist in specific efforts, such as with the prevention of falls or pressure ulcers (Lee et al., 2020). Similar studies were conducted in Taiwan (Liang et al, 2019). The nurses involved in that study also believed that robots could be of assistance to their practice, especially when they were used for repetitive tasks or treatments, or as playmates for pediatric patients. These nurses also cited specific concerns about their use, such as the potential for robots to reduce the number of employment opportunities for nursing staff.
A third study conducted in Finland was intended to assist in determining the readiness of healthcare professionals to incorporate robots into their existing practice and workflows (Turja et al., 2018). While healthcare professionals involved in this study did cite specific tasks such as lifting as being ones that the robots might be useful for, some admitted to having a lack of experience with robot-related technologies. This was important, as the participants’ acceptance of these technologies was directly related to their experience with them; the participants who had more experience with robots were more accepting of them.
Other studies were also used to measure acceptance of robots from one culture to another. For example, Coco et al. (2018) conducted a study that found healthcare professionals living in Japan were more receptive to the incorporation of robots into practice than the individuals that resided in Finland. The researchers attributed this level of acceptance to both cultural differences and the fact that Japan has a higher level of incorporation of robots in their healthcare processes than Finland currently has.
A review of the literature shows that, while the utilization of robots in the healthcare field is not widespread, it is something that will most likely propagate throughout the field in the coming years. Many of the articles included information related to the variety of ways that robots are currently being utilized. This includes providing surgical assistance, delivering supplies, performing cleaning and sterilizing duties, and providing companionship to patients.
As these roles and responsibilities of robots continues to expand and evolve, it is important to consider the feelings and perspectives of the patients, and the healthcare professionals, who will be encountering these machines. To this end, the literature review included information related to several studies that were conducted to ascertain the points of view of the aforementioned populations. Possessing this information can help to ease the transition to increased adoption of robotic technologies, as it allows for modification to the technologies, or to implementation strategies, to attempt to gain acceptance from those groups.
The overall strength of this collection of literature lies in the depth of the information provided; however, there are some weaknesses noted. Most importantly, many of the studies that measured the attitudes of patients and personnel toward robots were conducted in other countries, such as Korea, Taiwan, Japan, Portugal, and Finland (Lee et al., 2020; Liang et al., 2019; Turja et al., 2018; Pereira et al., 2018) . While this information was helpful in identifying potential attitudes that might be present in patients and personnel in the United States, it does not account for the variability that might exist based on the differing cultures found in these countries. In order to address this identified weakness, it will be necessary to perform another targeted literature search, to see if there are similar articles that contain information related to studies that were conducted in the United States.
Online Journal of Nursing Informatics
Powered by the HIMSS Foundation and the HIMSS Nursing Informatics Community, the Online Journal of Nursing Informatics is a free, international, peer reviewed publication that is published three times a year and supports all functional areas of nursing informatics.
Read the Latest Edition
References & Bio
Backonja, U., Hall, A. K., Painter, I., Kneale, L., Lazar, A., Cakmak, M., Thompson, H., & Demiris, G. (2018). Comfort and attitudes towards robots among young, middle-aged, and older adults: A cross-sectional study. Journal of Nursing Scholarship , 50 (6), 623– 633. https://doi.org/10.1111/jnu.12430
Bertelsen, A. S., Storm, A., Minet, L., & Ryg, J. (2020). Use of robot technology in passive mobilization of acute hospitalized geriatric medicine patients: A pilot test and feasibility study. Pilot and Feasibility Studies , 6 (1), 1–9 https://doi.org/10.1186/s40814-019-0545-z
Carter-Templeton, H., Frazier, R. M., Wu, L., & Wyatt, T. H. (2018). Robotics in nursing: A bibliometric analysis. Journal of Nursing Scholarship , 50 (6), 582–589. https://doi.org/10.1111/jnu.12399
Coco, K., Kangasniemi, M., & Rantanen, T. (2018). Care personnel's attitudes and fears toward care robots in elderly care: A comparison of data from the care personnel in Finland and Japan. Journal of Nursing Scholarship , 50 (6), 634–644. https://doi.org/10.1111/jnu.12435
Frazier, R. M., Carter-Templeton, H., Wyatt, T. H., & Wu, L. (2019). Current trends in robotics in nursing patents - A glimpse into emerging innovations. CIN - Computers Informatics Nursing , 37 (6), 290–297. https://doi.org/10.1097/CIN.0000000000000538
Grobbel, C., Poly-Droulard, L., van, W. A., & Davis, R. (2019). Designing nursing care practices complemented by robots: Ethical implications and application of caring frameworks. International Journal for Human Caring , 23 (2), 132–140. https://doi.org/10.20467/1091-5710.23.2.132
King, B. M., & Barry, C. D. (2019). “Caring between” the nurse, the one nursed, and the healthcare robot: an interpreted nursing situation using the Barry, Gordon, King framework. International Journal for Human Caring , 23 (2), 168–177. https://doi.org/10.20467/1091-5710.23.2.168
Lee, H., Piao, M., Lee, J., Byun, A., & Kim, J. (2020). The purpose of bedside robots: exploring the needs of inpatients and healthcare professionals. CIN - Computers Informatics Nursing , 38 (1), 8–17. https://doi.org/10.1097/CIN.0000000000000558
Lee, J., Song, Y. A., Jung, J. Y., Kim, H. J., Kim, B. R., Do, H., & Lim, J. (2018). Nurses’ needs for care robots in integrated nursing care services. Journal of Advanced Nursing , 74 (9), 2094–2105. https://doi.org/10.1111/jan.13711
Liang, H. F., Wu, K. M., Weng, C. H., & Hsieh, H. W. (2019). Nurses' views on the potential use of robots in the pediatric unit. Journal of Pediatric Nursing , 47 , 58–64. https://doi.org/10.1016/j.pedn.2019.04.027 Maalouf, N., Sidaoui, A., Elhajj, I. H., & Asmar, D. (2018). Robotics in nursing: A scoping review. Journal of Nursing Scholarship , 50 (6), 590–600. https://doi.org/10.1111/jnu.12424
Pereira, C., Pinheira, V., & Moreira Maria, M. J. G., Goncalves, P., & Silva, S. A. (2018). A methodological approach to evaluate elderly-robot interactions. European Journal of Social & Behavioural Sciences , 23 (3), 2746–2752.
Schoenhofer, S. O., van, W. A., & Boykin, A. (2019). Engaging robots as nursing partners in caring: Nursing as caring meets care-centered value-sensitive design. International Journal for Human Caring , 23 (2), 157–167. https://doi.org/10.20467/1091-5710.23.2.157
Shaw, R. J., Molloy, M., Vaughn, J., Crego, N., Kuszajewski, M., Brisson, R., & Hueckel, R. (2018). Telepresence robots for pediatric clinical simulations: Feasibility and acceptability. Pediatric Nursing , 44 (1), 39–43.
Suriaga, A. (2019). Nurse caring: From robotic surgeries to healthcare robots. International Journal for Human Caring , 23 (2), 178–184. https://doi.org/10.20467/1091-5710.23.2.178
Turja, T., Van, A. L., Särkikoski T, & Oksanen, A. (2018). Finnish healthcare professionals' attitudes towards robots: Reflections on a population sample. Nursing Open , 5 (3), 300– 309. https://doi.org/10.1002/nop2.138
Yasuhara, Y., Tanioka, T., Ito, H., Tanioka, R., & Tsujigami, Y. (2019). Ethico-legal issues with humanoid caring robots and older adults in Japan. International Journal for Human Caring , 23 (2), 141–148. https://doi.org/10.20467/1091-5710.23.2.141
Author Bio:
Robert S. Alvey, RN-BC, BSN is currently enrolled in the Jacksonville University Keigwin School of Nursing’s Master of Science program, with a specialization in nursing informatics. He is also presently employed as an informatics nurse for a hospital in Southern Maryland. Prior to obtaining his current position, Robert worked as a clinical analyst and obtained informatics nursing board certification through ANCC.


IMAGES
VIDEO
COMMENTS
It is important to understand the landscape of roles that robots have in healthcare to inform the research and development of the future. This scoping review aims to establish the types of robots being used in healthcare and identify where they are deployed by way of qualitative analysis of the literature. Through this, predictions can be made ...
Summary. This review found that robots have played 10 main roles across a variety of clinical environments. The two predominant roles were surgical and rehabilitation and mobility. Although robots were mainly studied in the surgical theatre and rehabilitation unit, other settings ranged from the hospital ward to inpatient pharmacy.
Results. We conducted 21 interviews and these accounts suggested that there are significant opportunities for improving the safety, quality, and efficiency of health care through robotics, but our analysis identified 4 major barriers that need to be effectively negotiated to realize these: (1) no clear pull from professionals and patients, (2) appearance of robots and associated expectations ...
In this paper, we analyse patients' perspectives on the introduction of artificial intelligence (AI) and robotic systems in healthcare. Based on citizens' experiences when hospitalised for COVID-19, we explore how the opinions and concerns regarding healthcare automation could not be disassociated from a context of high pressure on the health system and lack of resources, and a political ...
Throughout the paper, we point out the encouraging confluence of ideas between the expectations of healthcare providers and research trends in the human-robot interaction (HRI) literature. As AI-enabled robots enter the realm of healthcare and caregiving, it is important to consider how they will address the dimensions of care and how they wi
Springer Nature supports a reasonable amount of sharing of research papers by authors, subscribers and authorised users ("Users"), for small- ... [20] or healthcare robots [21, 22]. For ...
This paper investigates the use of robotics and artificial intelligence-based technologies and their applications in healthcare to fight against the COVID-19 pandemic. A systematic search following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) method is conducted to accumulate such literature, and an extensive ...
This article presents a broad contextualization of robots in health-care by identifying key stakeholders, care settings, and tasks; re-viewing recent advances in healthcare robotics; and outlining major ... to help fill care gaps and help aid health care workers. In both the research and commercial space, robotics technology has been used for ...
This paper surveys the state-of-the-art in robotics in healthcare and well-being, with particular attention to the key barriers and enablers to the implementation of this technology in real-world settings. Desktop research was used to identify available and emerging robotic technology currently in use (or with potential use) in healthcare settings.
This paper surveys the state-of-the-art in robotics in healthcare and well-being, with particular attention to the key barriers and enablers to the implementation of this technology in real-world settings. Desktop research was used to identify available and emerging robotic technology currently in use (or with potential use) in healthcare settings.
Humanoid service robots made swift progress in extending a helping hand to the strained global healthcare during the COVID-19 pandemic. This case provides an overview of the robots' inclusion in healthcare regarding pre- and intra-pandemic contexts. Specific focus is devoted to humanoid service robots as their shape, size, and mobility make ...
This paper highlights the critical role of humanoid Robots in the healthcare sector. This article also discusses the future trends of humanoid robots for the health sector. Published in: 2022 International Conference on Machine Learning, Big Data, Cloud and Parallel Computing (COM-IT-CON)
Health care is shifting toward become proactive according to the concept of P5 medicine-a predictive, personalized, preventive, participatory and precision discipline. This patient-centered care heavily leverages the latest technologies of artificial intelligence (AI) and robotics that support diagnosis, decision making and treatment. In this paper, we present the role of AI and robotic ...
Socially interactive robots for behavioral therapy, personalized care, and wellness/health promotion. (a) Paro, a huggable baby harp seal robot designed for use in hospitals and nursing homes.
In this survey paper, the recent advances in robotic technology applied in the healthcare domain are discussed. The paper provides detailed information about state-of-the-art research in care, hospital, assistive, rehabilitation, and walking assisting robots. The paper also discusses the open challenges healthcare robots face to be integrated ...
The use of robotics is already there in healthcare, but it's not main-stream yet and it would take some time for that to become a reality. The main goal of this research paper would be to shed some light on the same. I have proposed some ideas on how robotics can be used in some niche in healthcare, and how it can be made easy to spread and ...
Research papers related to the use of robotics and artificial intelligence in healthcare were thoroughly studied with special emphasis on its viability in the Indian scenario. The relevant search terms used were artificial intelligence, robotics, healthcare, India, etc.
This paper aims to review the existing work on the application of robot technology in the healthcare of older adults. The focus. is on research projects from 2008 to 2021 that h ave resulted in ...
AI and robotics in health care using artificial intelligence develops quickly, especially for early detection and diagnostic application. 3 Ai is becoming more powerful at the same time. It enables them to do what humans perform — often more efficiently, easily, and at reduced cost. ... The research type of this paper includes five journals 1 ...
Robotics is a popular branch of Machine Learning that has grown the interest of researchers for many years. Machine learning is used for developing various robotic systems which find their applications in different sectors specially in medical domain. This paper shows how robotics have evolved over the years and how robots are helping doctors as a medical assistant in their everyday work like ...
It can be observed that the expected global sales to industrialized robots will grow by 18 percent. to around 346,800 units during the year of 2017. The above trends showed that worldwide ...
Current Utilization of Robots in Healthcare. The literature review revealed that there are robots of different shapes and sizes that are currently being utilized in some healthcare settings (Grobbel et al., 2019). One setting that has been profoundly impacted by robotics is the operating room (Suriaga, 2019). Robot-assisted surgeries have been ...