- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- Auto Racing
- 2024 Paris Olympic Games
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media

Trans kids’ treatment can start younger, new guidelines say

This photo provided by Laura Short shows Eli Bundy on April 15, 2022 at Deception Pass in Washington. In South Carolina, where a proposed law would ban transgender treatments for kids under age 18, Eli Bundy hopes to get breast removal surgery next year before college. Bundy, 18, who identifies as nonbinary, supports updated guidance from an international transgender health group that recommends lower ages for some treatments. (Laura Short via AP)
FILE - Dr. David Klein, right, an Air Force Major and chief of adolescent medicine at Fort Belvoir Community Hospital, listens as Amanda Brewer, left, speaks with her daughter, Jenn Brewer, 13, as the teenager has blood drawn during a monthly appointment for monitoring her treatment at the hospital in Fort Belvoir, Va., on Sept. 7, 2016. Brewer is transitioning from male to female. (AP Photo/Jacquelyn Martin, File)
- Copy Link copied

A leading transgender health association has lowered its recommended minimum age for starting gender transition treatment, including sex hormones and surgeries.
The World Professional Association for Transgender Health said hormones could be started at age 14, two years earlier than the group’s previous advice, and some surgeries done at age 15 or 17, a year or so earlier than previous guidance. The group acknowledged potential risks but said it is unethical and harmful to withhold early treatment.
The association provided The Associated Press with an advance copy of its update ahead of publication in a medical journal, expected later this year. The international group promotes evidence-based standards of care and includes more than 3,000 doctors, social scientists and others involved in transgender health issues.
The update is based on expert opinion and a review of scientific evidence on the benefits and harms of transgender medical treatment in teens whose gender identity doesn’t match the sex they were assigned at birth, the group said. Such evidence is limited but has grown in the last decade, the group said, with studies suggesting the treatments can improve psychological well-being and reduce suicidal behavior.
Starting treatment earlier allows transgender teens to experience physical puberty changes around the same time as other teens, said Dr. Eli Coleman, chair of the group’s standards of care and director of the University of Minnesota Medical School’s human sexuality program.
But he stressed that age is just one factor to be weighed. Emotional maturity, parents’ consent, longstanding gender discomfort and a careful psychological evaluation are among the others.
“Certainly there are adolescents that do not have the emotional or cognitive maturity to make an informed decision,” he said. “That is why we recommend a careful multidisciplinary assessment.”
The updated guidelines include recommendations for treatment in adults, but the teen guidance is bound to get more attention. It comes amid a surge in kids referred to clinics offering transgender medical treatment , along with new efforts to prevent or restrict the treatment.
Many experts say more kids are seeking such treatment because gender-questioning children are more aware of their medical options and facing less stigma.
Critics, including some from within the transgender treatment community, say some clinics are too quick to offer irreversible treatment to kids who would otherwise outgrow their gender-questioning.
Psychologist Erica Anderson resigned her post as a board member of the World Professional Association for Transgender Health last year after voicing concerns about “sloppy” treatment given to kids without adequate counseling.
She is still a group member and supports the updated guidelines, which emphasize comprehensive assessments before treatment. But she says dozens of families have told her that doesn’t always happen.
“They tell me horror stories. They tell me, ‘Our child had 20 minutes with the doctor’” before being offered hormones, she said. “The parents leave with their hair on fire.’’
Estimates on the number of transgender youth and adults worldwide vary, partly because of different definitions. The association’s new guidelines say data from mostly Western countries suggest a range of between a fraction of a percent in adults to up to 8% in kids.
Anderson said she’s heard recent estimates suggesting the rate in kids is as high as 1 in 5 — which she strongly disputes. That number likely reflects gender-questioning kids who aren’t good candidates for lifelong medical treatment or permanent physical changes, she said.
Still, Anderson said she condemns politicians who want to punish parents for allowing their kids to receive transgender treatment and those who say treatment should be banned for those under age 18.
“That’s just absolutely cruel,’’ she said.
Dr. Marci Bowers, the transgender health group’s president-elect, also has raised concerns about hasty treatment, but she acknowledged the frustration of people who have been “forced to jump through arbitrary hoops and barriers to treatment by gatekeepers ... and subjected to scrutiny that is not applied to another medical diagnosis.’’
Gabe Poulos, 22, had breast removal surgery at age 16 and has been on sex hormones for seven years. The Asheville, North Carolina, resident struggled miserably with gender discomfort before his treatment.
Poulos said he’s glad he was able to get treatment at a young age.
“Transitioning under the roof with your parents so they can go through it with you, that’s really beneficial,’’ he said. “I’m so much happier now.’’
In South Carolina, where a proposed law would ban transgender treatments for kids under age 18, Eli Bundy has been waiting to get breast removal surgery since age 15. Now 18, Bundy just graduated from high school and is planning to have surgery before college.
Bundy, who identifies as nonbinary, supports easing limits on transgender medical care for kids.
“Those decisions are best made by patients and patient families and medical professionals,’’ they said. “It definitely makes sense for there to be fewer restrictions, because then kids and physicians can figure it out together.’’
Dr. Julia Mason, an Oregon pediatrician who has raised concerns about the increasing numbers of youngsters who are getting transgender treatment, said too many in the field are jumping the gun. She argues there isn’t strong evidence in favor of transgender medical treatment for kids.
“In medicine ... the treatment has to be proven safe and effective before we can start recommending it,’’ Mason said.
Experts say the most rigorous research — studies comparing treated kids with outcomes in untreated kids — would be unethical and psychologically harmful to the untreated group.
The new guidelines include starting medication called puberty blockers in the early stages of puberty, which for girls is around ages 8 to 13 and typically two years later for boys. That’s no change from the group’s previous guidance. The drugs delay puberty and give kids time to decide about additional treatment; their effects end when the medication is stopped.
The blockers can weaken bones, and starting them too young in children assigned males at birth might impair sexual function in adulthood, although long-term evidence is lacking.
The update also recommends:
—Sex hormones — estrogen or testosterone — starting at age 14. This is often lifelong treatment. Long-term risks may include infertility and weight gain, along with strokes in trans women and high blood pressure in trans men, the guidelines say.
—Breast removal for trans boys at age 15. Previous guidance suggested this could be done at least a year after hormones, around age 17, although a specific minimum ag wasn’t listed.
—Most genital surgeries starting at age 17, including womb and testicle removal, a year earlier than previous guidance.
The Endocrine Society, another group that offers guidance on transgender treatment, generally recommends starting a year or two later, although it recently moved to start updating its own guidelines. The American Academy of Pediatrics and the American Medical Association support allowing kids to seek transgender medical treatment, but they don’t offer age-specific guidance.
Dr. Joel Frader, a Northwestern University a pediatrician and medical ethicist who advises a gender treatment program at Chicago’s Lurie Children’s Hospital, said guidelines should rely on psychological readiness, not age.
Frader said brain science shows that kids are able to make logical decisions by around age 14, but they’re prone to risk-taking and they take into account long-term consequences of their actions only when they’re much older.
Coleen Williams, a psychologist at Boston Children’s Hospital’s Gender Multispecialty Service, said treatment decisions there are collaborative and individualized.
“Medical intervention in any realm is not a one-size-fits-all option,” Williams said.
Follow AP Medical Writer Lindsey Tanner at @LindseyTanner.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Department of Science Education. The AP is solely responsible for all content.

- For Journalists
- News Releases
- Latest Releases
- News Release
Age restriction lifted for gender-affirming surgery in new international guidelines
'Will result in the need for parental consent before doctors would likely perform surgeries'
Media Information
- Release Date: September 16, 2022
Media Contacts
Kristin Samuelson
- (847) 491-4888
- Email Kristin
- Expert can speak to transgender peoples’ right to bodily autonomy, how guidelines affect insurance coverage, how the U.S. gender regulations compare to other countries, more
CHICAGO --- The World Professional Association for Transgender Health (WPATH) today today announced its updated Standards of Care and Ethical Guidelines for health professionals. Among the updates is a new suggestion to lift the age restriction for youth seeking gender-affirming surgical treatment, in comparison to previous suggestion of surgery at 17 or older.
Alithia Zamantakis (she/her), a member of the Institute of Sexual & Gender Minority Health at Northwestern University Feinberg School of Medicine, is available to speak to media about the new guidelines. Contact Kristin Samuelson at [email protected] to schedule an interview.
“Lifting the age restriction will greatly increase access to care for transgender adolescents, but will also result in the need for parental consent for surgeries before doctors would likely perform them,” said Zamantakis, a postdoctoral fellow at Northwestern, who has researched trans youth and resilience. “Additionally, changes in age restriction are not likely to change much in practice in states like Alabama, Arkansas, Texas and Arizona, where gender-affirming care for youth is currently banned.”
Zamantakis also can speak about transgender peoples’ right to bodily autonomy, how guidelines affect insurance coverage and how U.S. gender regulations compare to other countries.
Guidelines are thorough but WPATH ‘still has work to do’
“The systematic reviews conducted as part of the development of the standards of care are fantastic syntheses of the literature on gender-affirming care that should inform doctors' work,” Zamantakis said. “They are used by numerous providers and insurance companies to determine who gets access to care and who does not.
“However, WPATH still has work to do to ensure its standards of care are representative of the needs and experiences of all non-cisgender people and that the standards of care are used to ensure that individuals receive adequate care rather than to gatekeep who gets access to care. WPATH largely has been run by white and/or cisgender individuals. It has only had three transgender presidents thus far, with Marci Bower soon to be the second trans woman president.
“Future iterations of the standards of care must include more stakeholders per committee, greater representation of transgender experts and stakeholders of color, and greater representation of experts and stakeholders outside the U.S.”
Transgender individuals’ right to bodily autonomy
“WPATH does not recommend prior hormone replacement therapy or ‘presenting’ as one's gender for a certain period of time for surgery for nonbinary people, yet it still does for transgender women and men,” Zamantakis said. “The reality is that neither should be requirements for accessing care for people of any gender.
“The recommendation of requiring documentation of persistent gender incongruence is meant to prevent regret. However, it's important to ask who ultimately has the authority to determine whether individuals have the right to make decisions about their bodily autonomy that they may or may not regret? Cisgender women undergo breast augmentation regularly, which is not an entirely reversible procedure, yet they are not required to have proof of documented incongruence. It is assumed that if they regret the surgery, they will learn to cope with the regret or will have an additional surgery. Transgender individuals also deserve the right to bodily autonomy and ultimately to regret the decisions they make if they later do not align with how they experience themselves.”
Putting numbers on the rise in children seeking gender care
By ROBIN RESPAUT and CHAD TERHUNE
Filed Oct. 6, 2022, 11 a.m. GMT

Thousands of children in the United States now openly identify as a gender different from the one they were assigned at birth, their numbers surging amid growing recognition of transgender identity and rights even as they face persistent prejudice and discrimination.
As the number of transgender children has grown, so has their access to gender-affirming care, much of it provided at scores of clinics at major hospitals.
Reliable counts of adolescents receiving gender-affirming treatment have long been guesswork – until now. Reuters worked with health technology company Komodo Health Inc to identify how many youths have sought and received care. The data show that more and more families across the country are grappling with profound questions about what type of care to pursue for their children, placing them at the center of a vitriolic national political debate over what it means to protect youth who identify as transgender.
Diagnoses of youths with gender dysphoria surge
In 2021, about 42,000 children and teens across the United States received a diagnosis of gender dysphoria, nearly triple the number in 2017, according to data Komodo compiled for Reuters. Gender dysphoria is defined as the distress caused by a discrepancy between a person’s gender identity and the one assigned to them at birth.
Overall, the analysis found that at least 121,882 children ages 6 to 17 were diagnosed with gender dysphoria from 2017 through 2021. Reuters found similar trends when it requested state-level data on diagnoses among children covered by Medicaid, the public insurance program for lower-income families.
Gender-affirming care for youths takes several forms, from social recognition of a preferred name and pronouns to medical interventions such as hormone therapy and, sometimes, surgery. A small but increasing number of U.S. children diagnosed with gender dysphoria are choosing medical interventions to express their identity and help alleviate their distress.
These medical treatments don’t begin until the onset of puberty, typically around age 10 or 11.
For children at this age and stage of development, puberty-blocking medications are an option. These drugs, known as GnRH agonists, suppress the release of the sex hormones testosterone and estrogen. The U.S. Food and Drug Administration has approved the drugs to treat prostate cancer, endometriosis and central precocious puberty, but not gender dysphoria. Their off-label use in gender-affirming care, while legal, lacks the support of clinical trials to establish their safety for such treatment.
Over the last five years, there were at least 4,780 adolescents who started on puberty blockers and had a prior gender dysphoria diagnosis.
This tally and others in the Komodo analysis are likely an undercount because they didn’t include treatment that wasn’t covered by insurance and were limited to pediatric patients with a gender dysphoria diagnosis. Practitioners may not log this diagnosis when prescribing treatment.
By suppressing sex hormones, puberty-blocking medications stop the onset of secondary sex characteristics, such as breast development and menstruation in adolescents assigned female at birth. For those assigned male at birth, the drugs inhibit development of a deeper voice and an Adam’s apple and growth of facial and body hair. They also limit growth of genitalia.
Without puberty blockers, such physical changes can cause severe distress in many transgender children. If an adolescent stops the medication, puberty resumes.
The medications are administered as injections, typically every few months, or through an implant under the skin of the upper arm.
After suppressing puberty, a child may pursue hormone treatments to initiate a puberty that aligns with their gender identity. Those for whom the opportunity to block puberty has already passed or who declined the option may also pursue hormone therapy.
At least 14,726 minors started hormone treatment with a prior gender dysphoria diagnosis from 2017 through 2021, according to the Komodo analysis.
Hormones – testosterone for adolescents assigned female at birth and estrogen for those assigned male – promote development of secondary sex characteristics. Adolescents assigned female at birth who take testosterone may notice that fat is redistributed from the hips and thighs to the abdomen. Arms and legs may appear more muscular. The brow and jawline may become more pronounced. Body hair may coarsen and thicken. Teens assigned male at birth who take estrogen may notice the hair on their body softens and thins. Fat may be redistributed from the abdomen to the buttocks and thighs. Their testicles may shrink and sex drive diminish. Some changes from hormone treatment are permanent.
Hormones are taken in a variety of ways: injections, pills, patches and gels. Some minors will continue to take hormones for many years well into adulthood, or they may stop if they achieve the physical traits they want.
Hormone treatment may leave an adolescent infertile, especially if the child also took puberty blockers at an early age. That and other potential side effects are not well-studied, experts say.
The ultimate step in gender-affirming medical treatment is surgery, which is uncommon in patients under age 18. Some children’s hospitals and gender clinics don’t offer surgery to minors, requiring that they be adults before deciding on procedures that are irreversible and carry a heightened risk of complications.
The Komodo analysis of insurance claims found 56 genital surgeries among patients ages 13 to 17 with a prior gender dysphoria diagnosis from 2019 to 2021. Among teens, “top surgery” to remove breasts is more common. In the three years ending in 2021, at least 776 mastectomies were performed in the United States on patients ages 13 to 17 with a gender dysphoria diagnosis, according to Komodo’s data analysis of insurance claims. This tally does not include procedures that were paid for out of pocket.
A note on the data
Komodo’s analysis draws on full or partial health insurance claims for about 330 million U.S. patients over the five years from 2017 to 2021, including patients covered by private health plans and public insurance like Medicaid. The data include roughly 40 million patients annually, ages 6 through 17, and comprise health insurance claims that document diagnoses and procedures administered by U.S. clinicians and facilities.
To determine the number of new patients who initiated puberty blockers or hormones, or who received an initial dysphoria diagnosis, Komodo looked back at least one year prior in each patient’s record. For the surgery data, Komodo counted multiple procedures on a single day as one procedure.
For the analysis of pediatric patients initiating puberty blockers or hormones, Komodo searched for patients with a prior gender dysphoria diagnosis. Patients with a diagnosis of central precocious puberty were removed. A total of 17,683 patients, ages 6 through 17, with a prior gender dysphoria diagnosis initiated either puberty blockers or hormones or both during the five-year period. Of these, 4,780 patients had initiated puberty blockers and 14,726 patients had initiated hormone treatment.
Youth in Transition
By Robin Respaut and Chad Terhune
Photo editing: Corrine Perkins
Art direction: John Emerson
Edited by Michele Gershberg and John Blanton
- Follow Reuters Investigates
Other Reuters investigations

Young Children Do Not Receive Medical Gender Transition Treatment
By Kate Yandell
Posted on May 22, 2023
SciCheck Digest
Families seeking information from a health care provider about a young child’s gender identity may have their questions answered or receive counseling. Some posts share a misleading claim that toddlers are being “transitioned.” To be clear, prepubescent children are not offered transition surgery or drugs.
Some children identify with a gender that does not match their sex assigned at birth. These children are referred to as transgender, gender-diverse or gender-expansive. Doctors will listen to children and their family members, offer information, and in some cases connect them with mental health care, if needed.
But for children who have not yet started puberty, there are no recommended drugs, surgeries or other gender-transition treatments.
Recent social media posts shared the misleading claim that medical institutions in North Carolina are “transitioning toddlers,” which they called an “experimental treatment.” The posts referenced a blog post published by the Education First Alliance, a conservative nonprofit in North Carolina that says many schools are engaging in “ideological indoctrination” of children and need to be reformed.

The group has advocated the passage of a North Carolina bill to restrict medical gender-transition treatment before age 18. There are now 18 states that have taken action to restrict medical transition treatments for minors .
A widely shared article from the Epoch Times citing the blog post bore the false headline: “‘Transgender’ Toddlers as Young as 2 Undergoing Mutilation/Sterilization by NC Medical System, Journalist Alleges.” The Epoch Times has a history of publishing misleading or false claims. The article on transgender toddlers then disappeared from the website, and the Epoch Times published a new article clarifying that young children are not receiving hormone blockers, cross-sex hormones or surgery.
Representatives from all three North Carolina institutions referenced in the social media posts told us via emailed statements that they do not offer surgeries or other transition treatments to toddlers.
East Carolina University, May 5: ECU Health does not offer gender affirming surgery to minors nor does the health system offer gender affirming transition care to toddlers.
ECU Health elaborated that it does not offer puberty blockers and only offers hormone therapy after puberty “in limited cases,” as recommended in national guidelines and with parental or guardian consent. It also said that it offers interdisciplinary gender-affirming primary care for LGBTQ+ patients, including access to services such as mental health care, nutrition and social work.
“These primary care services are available to any LGBTQ+ patient who needs care. ECU Health does not provide gender-related care to patients 2 to 4 years old or any toddler period,” ECU said.
University of North Carolina, May 12: To be clear: UNC Health does not offer any gender-transitioning care for toddlers. We do not perform any gender care surgical procedures or medical interventions on toddlers. Also, we are not conducting any gender care research or clinical trials involving children. If a toddler’s parent(s) has concerns or questions about their child’s gender, a primary care provider would certainly listen to them, but would never recommend gender treatment for a toddler. Gender surgery can be performed on anyone 18 years old or older .
Duke Health, May 12: Duke Health has provided high-quality, compassionate, and evidence-based gender care to both adolescents and adults for many years. Care decisions are made by patients, families and their providers and are both age-appropriate and adherent to national and international guidelines. Under these professional guidelines and in accordance with accepted medical standards, hormone therapies are explicitly not provided to children prior to puberty and gender-affirming surgeries are, except in exceedingly rare circumstances, only performed after age 18.
Duke and UNC both called the claims that they offer gender-transition care to toddlers false, and ECU referred to the “intentional spreading of dangerous misinformation online.”
Nor do other medical institutions offer gender-affirming drug treatment or surgery to toddlers, clinical psychologist Christy Olezeski , director of the Yale Pediatric Gender Program, told us, although some may offer support to families of young children or connect them with mental health care.
The Education First Alliance post also states that a doctor “can see a 2-year-old girl play with a toy truck, and then begin treatment for gender dysphoria.” But simply playing with a certain toy would not meet the criteria for a diagnosis of gender dysphoria, according to the medical diagnostic manual used by health professionals.
“With all kids, we want them to feel comfortable and confident in who they are. We want them to feel comfortable and confident in how they like to express themselves. We want them to be safe,” Olezeski said. “So all of these tenets are taken into consideration when providing care for children. There is no medical care that happens prior to puberty.”
Medical Transition Starts During Adolescence or Later
The Education First Alliance blog post does not clearly state what it means when it says North Carolina institutions are “transitioning toddlers.” It refers to treatment and hormone therapy without clarifying the age at which it is offered.
Only in the final section of the piece does it include a quote from a doctor correctly stating that children are not offered surgery or drugs before puberty.
To spell out the reality of the situation: The North Carolina institutions are not providing surgeries or hormone therapy to prepubescent children, nor is this standard practice in any part of the country.
Programs and physicians will have different policies, but widely referenced guidance from the World Professional Association for Transgender Health and the Endocrine Society lays out recommended care at different ages.
Drugs that suppress puberty are the first medical treatment that may be offered to a transgender minor, the guidelines say. Children may be offered drugs to suppress puberty beginning when breast buds appear or testicles increase to a certain volume, typically happening between ages 8 to 13 or 9 to 14, respectively.
Generally, someone may start gender-affirming hormone therapy in early adolescence or later, the American Academy for Pediatrics explains . The Endocrine Society says that adolescents typically have the mental capacity to participate in making an informed decision about gender-affirming hormone therapy by age 16.
Older adolescents who want flat chests may sometimes be able to get surgery to remove their breasts, also known as top surgery, Olezeski said. They sometimes desire to do this before college. Guidelines do not offer a specific age during adolescence when this type of surgery may be appropriate. Instead, they explain how a care team can assess adolescents on a case-by-case basis.
A previous version of the WPATH guidelines did not recommend genital surgery until adulthood, but the most recent version, published in September 2022, is less specific about an age limit. Rather, it explains various criteria to determine whether someone who desires surgery should be offered it, including a person’s emotional and cognitive maturity level and whether they have been on hormone therapy for at least a year.
The Endocrine Society similarly offers criteria for when someone might be ready for genital surgery, but specifies that surgeries involving removing the testicles, ovaries or uterus should not happen before age 18.
“Typically any sort of genital-affirming surgeries still are happening at 18 or later,” Olezeski said.
There are no comprehensive statistics on the number of gender-affirming surgeries performed in the U.S., but according to an insurance claims analysis from Reuters and Komodo Health Inc., 776 minors with a diagnosis of gender dysphoria had breast removal surgeries and 56 had genital surgeries from 2019 to 2021.
Research Shows Benefits of Affirming Gender Identity
Young children do not get medical transition treatment, but they do have feelings about their gender and can benefit from support from those around them. “Children start to have a sense of their own gender identity between the ages of 2 1/2 to 3 years old,” Olezeski said.
Programs vary in what age groups they serve, she said, but some do support families of preschool-aged children by answering questions or providing mental health care.
Transgender children are at increased risk of some mental health problems, including anxiety and depression. According to the WPATH guidelines, affirming a child’s gender through day-to-day changes — also known as social transition — may have a positive impact on a child’s mental health. Social transition “may look different for every individual,” Olezeski said. Changes could include going by a different name or pronouns or altering one’s attire or hair style.

Two studies of socially transitioned children — including one with kids as young as 3 — have found minimal or no difference in anxiety and depression compared with non-transgender siblings or other children of similar ages.
“Research substantiates that children who are prepubertal and assert an identity of [transgender and gender diverse] know their gender as clearly and as consistently as their developmentally equivalent peers who identify as cisgender and benefit from the same level of social acceptance,” the AAP guidelines say, adding that differences in how children identify and express their gender are normal.
Social transitions largely take place outside of medical institutions, led by the child and supported by their family members and others around them. However, a family with questions about their child’s gender or social transition may be able to get information from their pediatrician or another medical provider, Olezeski said.
Although not available everywhere, specialized programs may be particularly prepared to offer care to a gender-diverse child and their family, she said. A child may get a referral to one of these programs from a pediatrician, another specialty physician, a mental health care professional or their school, or a parent may seek out one of these programs.
“We have created a space where parents can come with their youth when they’re young to ask questions about how to best support their child: what to do if they have questions, how to get support, what do we know about the best research in terms of how to allow kids space to explore their identity, to explore how they like to express themselves, and then if they do identify as trans or nonbinary, how to support the parents and the youth in that,” Olezeski said of specialized programs. Parents benefit from the support, and then the children also benefit from support from their parents.
WPATH says that the child should be the one to initiate a social transition by expressing a “strong desire or need” for it after consistently articulating an identity that does not match their sex assigned at birth. A health care provider can then help the family explore benefits and risks. A child simply playing with certain toys, dressing a certain way or enjoying certain activities is not a sign they would benefit from a social transition, the guidelines state.
Previously, assertions children made about their gender were seen as “possibly true” and support was often withheld until an age when identity was believed to become fixed, the AAP guidelines explain. But “more robust and current research suggests that, rather than focusing on who a child will become, valuing them for who they are, even at a young age, fosters secure attachment and resilience, not only for the child but also for the whole family,” the guidelines say.
Mental Health Care Benefits
A gender-diverse child or their family members may benefit from a referral to a psychologist or other mental health professional. However, being transgender or gender-diverse is not in itself a mental health disorder, according to the American Psychological Association , WPATH and other expert groups . These organizations also note that people who are transgender or gender-diverse do not all experience mental health problems or distress about their gender.
Psychological therapy is not meant to change a child’s gender identity, the WPATH guidelines say .
The form of therapy a child or a family might receive will depend on their particular needs, Olezeski said. For instance, a young child might receive play-based therapy, since play is how children “work out different things in their life,” she said. A parent might work on strategies to better support their child.
One mental health diagnosis that some gender-diverse people may receive is gender dysphoria . There is disagreement about how useful such a diagnosis is, and receiving such a diagnosis does not necessarily mean someone will decide to undergo a transition, whether social or medical.
UNC Health told us in an email that a gender dysphoria diagnosis “is rarely used” for children.
Very few gender-expansive kids have dysphoria, the spokesperson said. “ Gender expansion in childhood is not Gender Dysphoria ,” UNC added, attributing the explanation to psychiatric staff (emphasis is UNC’s). “The psychiatric team’s goal is to provide good mental health care and manage safety—this means trying to protect against abuse and bullying and to support families.”
Social media posts incorrectly claim that toddlers are being diagnosed with gender dysphoria based on what toys they play with. One post said : “Three medical schools in North Carolina are diagnosing TODDLERS who play with stereotypically opposite gender toys as having GENDER DYSPHORIA and are beginning to transition them!!”
There are separate criteria for diagnosing gender dysphoria in adults and adolescents versus children, according to the Diagnostic and Statistical Manual of Mental Disorders. For children to receive this diagnosis, they must meet six of eight criteria for a six-month period and experience “clinically significant distress” or impairment in functioning, according to the diagnostic manual.
A “strong preference for the toys, games or activities stereotypically used or engaged in by the other gender” is one criterion, but children must also meet other criteria, and expressing a strong desire to be another gender or insisting that they are another gender is required.
“People liking to play with different things or liking to wear a diverse set of clothes does not mean that somebody has gender dysphoria,” Olezeski said. “That just means that kids have a breadth of things that they can play with and ways that they can act and things that they can wear . ”
Editor’s note: SciCheck’s articles providing accurate health information and correcting health misinformation are made possible by a grant from the Robert Wood Johnson Foundation. The foundation has no control over FactCheck.org’s editorial decisions, and the views expressed in our articles do not necessarily reflect the views of the foundation.
Rafferty, Jason. “ Gender-Diverse & Transgender Children .” HealthyChildren.org. Updated 8 Jun 2022.
Coleman, E. et al. “ Standards of Care for the Health of Transgender and Gender Diverse People, Version 8 .” International Journal of Transgender Health. 15 Sep 2022.
Rachmuth, Sloan. “ Transgender Toddlers Treated at Duke, UNC, and ECU .” Education First Alliance. 1 May 2023.
North Carolina General Assembly. “ Senate Bill 639, Youth Health Protection Act .” (as introduced 5 Apr 2023).
Putka, Sophie et al. “ These States Have Banned Youth Gender-Affirming Care .” Medpage Today. Updated 17 May 2023.
Davis, Elliott Jr. “ States That Have Restricted Gender-Affirming Care for Trans Youth in 2023 .” U.S. News & World Report. Updated 17 May 2023.
Montgomery, David and Goodman, J. David. “ Texas Legislature Bans Transgender Medical Care for Children .” New York Times. 17 May 2023.
Ji, Sayer. ‘ Transgender’ Toddlers as Young as 2 Undergoing Mutilation/Sterilization by NC Medical System, Journalist Alleges .” Epoch Times. Internet Archive, Wayback Machine. Archived 6 May 2023.
McDonald, Jessica. “ COVID-19 Vaccines Reduce, Not Increase, Risk of Stillbirth .” FactCheck.org. 9 Nov 2022.
Jaramillo, Catalina. “ Posts Distort Questionable Study on COVID-19 Vaccination and EMS Calls .” FactCheck.org. 15 June 2022.
Spencer, Saranac Hale. “ Social Media Posts Misrepresent FDA’s COVID-19 Vaccine Safety Research .” FactCheck.org. 23 Dec 2022.
Jaramillo, Catalina. “ WHO ‘Pandemic Treaty’ Draft Reaffirms Nations’ Sovereignty to Dictate Health Policy .” FactCheck.org. 2 Mar 2023.
McCormick Sanchez, Darlene. “ IN-DEPTH: North Carolina Medical Schools See Children as Young as Toddlers for Gender Dysphoria .” The Epoch Times. 8 May 2023.
ECU health spokesperson. Emails with FactCheck.org. 12 May 2023 and 19 May 2023.
UNC Health spokesperson. Emails with FactCheck.org. 12 May 2023 and 19 May 2023.
Duke Health spokesperson. Email with FactCheck.org. 12 May 2023.
Olezeski, Christy. Interview with FactCheck.org. 16 May 2023.
Hembree, Wylie C. et al. “ Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline .” The Journal of Clinical Endocrinology and Metabolism. 1 Nov 2017.
Emmanuel, Mickey and Bokor, Brooke R. “ Tanner Stages .” StatPearls. Updated 11 Dec 2022.
Rafferty, Jason et al. “ Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents .” Pediatrics. 17 Sep 2018.
Coleman, E. et al. “ Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7 .” International Journal of Transgenderism. 27 Aug 2012.
Durwood, Lily et al. “ Mental Health and Self-Worth in Socially Transitioned Transgender Youth .” Journal of the American Academy of Child and Adolescent Psychiatry. 27 Nov 2016.
Olson, Kristina R. et al. “ Mental Health of Transgender Children Who Are Supported in Their Identities .” Pediatrics. 26 Feb 2016.
“ Answers to Your Questions about Transgender People, Gender Identity, and Gender Expression .” American Psychological Association website. 9 Mar 2023.
“ What is Gender Dysphoria ?” American Psychiatric Association website. Updated Aug 2022.
Vanessa Marie | Truth Seeker (indivisible.mama). “ Three medical schools in North Carolina are diagnosing TODDLERS who play with stereotypically opposite gender toys as having GENDER DYSPHORIA and are beginning to transition them!! … ” Instagram. 7 May 2023.
- New Hampshire
- North Carolina
- Pennsylvania
- West Virginia
- Online hoaxes
- Coronavirus
- Health Care
- Immigration
- Environment
- Foreign Policy
- Kamala Harris
- Donald Trump
- Mitch McConnell
- Hakeem Jeffries
- Ron DeSantis
- Tucker Carlson
- Sean Hannity
- Rachel Maddow
- PolitiFact Videos
- 2024 Elections
- Mostly True
- Mostly False
- Pants on Fire
- Biden Promise Tracker
- Trump-O-Meter
- Latest Promises
- Our Process
- Who pays for PolitiFact?
- Advertise with Us
- Suggest a Fact-check
- Corrections and Updates
- Newsletters
Stand up for the facts!
Our only agenda is to publish the truth so you can be an informed participant in democracy. We need your help.
I would like to contribute

- Facebook Fact-checks
- Viral image

No, young children cannot take hormones or change their sex
If your time is short.
• Professional medical organizations recommend against puberty blockers for children who have not reached puberty, which typically begins between ages 10 and 12.
• Hormone treatment for feminization or masculinization of the body is typically not considered until patients are at least 16 years old.
• Gender reassignment surgery is typically only available to those 18 and older in the United States.
Misinformation about medical treatments for transgender patients has proliferated in recent weeks, as a spate of events brought transgender rights into the spotlight.
The social media backlash was swift following executive actions from President Joe Biden to expand transgender rights, his nomination of a transgender woman for assistant health secretary and the U.S. House of Representatives’ passing of the Equality Act to prohibit discrimation based on sexual orientation and gender identity.
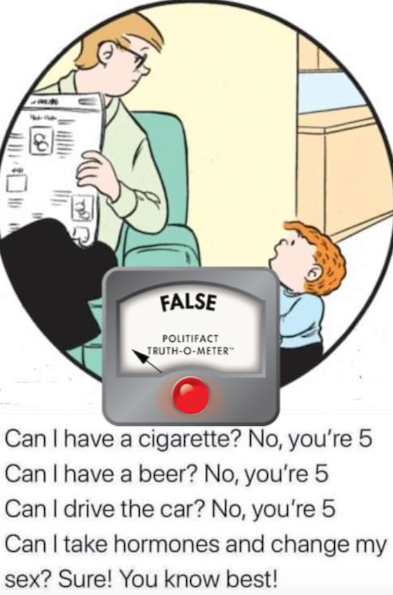
One Facebook post features an image of a father and son from the comic strip "The Family Circus," with text that reads, "Can I have a cigarette? No, you’re 5. Can I have a beer? No, you’re 5. Can I drive the car? No, you’re 5. Can I take hormones and change my sex? Sure! You know best."
The onset of puberty is the baseline for medical intervention. Puberty typically occurs between ages 10 and 14 for girls and 12 and 16 for boys.
Guidelines for the medical care of transgender patients, developed by organizations such as the Endocrine Society and the World Professional Association for Transgender Health, begin with counseling and psychological evaluation by a team of medical professionals before any physical interventions are considered.
If patients have begun to go through puberty, and they have "demonstrated a long-lasting and intense pattern of gender nonconformity or gender dysphoria," then treatments such as puberty blockers can be considered, according to the standards of care for transgender people by the World Professional Association for Transgender Health. Gender dysphoria refers to distress people may experience as a result of the discrepancy between their gender identity and the sex assigned to them at birth.
Puberty blockers, which suppress the release of testosterone and estrogen during puberty, allow adolescents "more time to explore their gender nonconformity and other developmental issues," and can be used for a few years, the standards of care say. One guideline for giving the medication says parents or guardians must consent to the treatment and also provide support to the youth during the process.
Featured Fact-check

If a patient decides to continue transitioning, hormone therapy for feminization or masculinization of the body can follow the use of puberty blockers. But, again, the Endocrine Society’s guidelines say patients should be at least 16 years old to receive hormone treatment, which is partly irreversible. Many hospitals, such as the Duke Health Center for Gender Care for Children and Adolescents , will only offer hormone replacement therapies for adolescents 16 or older.
The World Professional Association for Transgender Health reports that gender dysphoria in childhood "does not inevitably continue into adulthood." One study showed that children who had not yet reached puberty who were referred to clinics for assessment of gender dysphoria had a 12% to 27% persistence rate of gender dysphoria into adulthood.
By comparison, adolescents with gender dysphoria are much more likely to have it persist into adulthood, the association reports, though no formal studies have been conducted for adolescents.
A cartoon on Facebook implies that a child who is 5 can "take hormones and change my sex."
The information is unsubstantiated. The guidelines for the medical care of transgender patients, developed by organizations such as the Endocrine Society and the World Professional Association for Transgender Health, do not recommend puberty blockers for children who have not reached puberty; do not recommend hormone treatment for those under 16 years old; and typically restrict genital reassignment surgery to those 18 and older, who also meet other criteria.
We rate this claim False.
RELATED: What the Equality Act debate gets wrong about gender, sex
RELATED: Rachel Levine does not support gender confirmation surgery for all children
Read About Our Process
The Principles of the Truth-O-Meter
Our Sources
Comics Kingdom, " The Family Circus ," accessed March 3, 2021
Endocrine Society, " Gender Dysphoria/Gender Incongruence Guideline Resources ," Sept. 1, 2017
PolitiFact, " Rachel Levine does not support gender confirmation surgery for all children ," March 2, 2021
U.S. National Library of Medicine, Medline Plus, " Puberty ," accessed March 3, 2021
World Professional Association for Transgender Health, " Standards of Care ," 2012
Browse the Truth-O-Meter
More by monique curet.

Support independent fact-checking. Become a member!
- Follow us on Facebook
- Follow us on Twitter
- Criminal Justice
- Environment
- Politics & Government
- Race & Gender
Expert Commentary
What the research says about hormones and surgery for transgender youth
Researchers and physicians point to a growing body of peer-reviewed academic scholarship in support of gender-affirming medical treatment for transgender youth.

Republish this article

This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License .
by Chloe Reichel, The Journalist's Resource August 7, 2019
This <a target="_blank" href="https://journalistsresource.org/politics-and-government/gender-confirmation-surgery-transgender-youth-research/">article</a> first appeared on <a target="_blank" href="https://journalistsresource.org">The Journalist's Resource</a> and is republished here under a Creative Commons license.<img src="https://journalistsresource.org/wp-content/uploads/2020/11/cropped-jr-favicon-150x150.png" style="width:1em;height:1em;margin-left:10px;">
In the interest of examining this important news topic through a research lens, Journalist’s Resource collaborated on this story with The Burlington Free Press, where it first appeared . This piece is part of the newspaper’s series of stories about transgender youth in the state.
As Vermont regulators consider changes to Medicaid that would expand access to gender confirmation surgery for transgender youth, researchers and physicians point to a growing body of peer-reviewed academic scholarship in support of the new proposal.
Among other changes, the proposed rules would eliminate the requirement that transgender individuals on Medicaid must wait until the age of 21 to receive surgery. Individuals over the age of 18 and minors — with informed parental consent — would be eligible.
Such changes are in line with current thinking among academics and physicians in the field. It’s still a fledgling field, as Marci Bowers, a California-based gynecologist and surgeon who specializes in gender confirmation and serves as a professorial lecturer at the Icahn School of Medicine at Mount Sinai points out.
“Kids are coming out very young. A generation ago, they were driven into the closet,” Bowers said. “It’s only these last 20 years or so where instead of that happening, people are getting professional help.”
How common are gender confirmation surgeries in the U.S.?
Estimates suggest that in the U.S., between 2000 and 2014, 10.9% of inpatient visits for transgender people involved gender confirmation surgery. This figure comes from an analysis of inpatient visits for a nationally representative sample that includes, but is not limited to, transgender patients, which was published in 2018 in the medical journal JAMA Surgery . Over the study period, the number of patients who sought gender confirmation surgery increased annually.
Further, the percentage of gender confirmation surgeries that are “genital surgeries” — commonly referred to as bottom surgeries — has increased over time. Between 2000 and 2005, 72% of gender confirmation surgeries were bottom surgeries; from 2006 to 2011, that number increased to 84%. And the number of patients insured by Medicare or Medicaid seeking these procedures increased threefold between 2012-2013 and 2014.
As societal acceptance of gender diversity has grown, medical thinking has changed, too, Bowers notes.
“At least in the academic circles, in the medical circles, we realize that yes, it’s valid, that yes, kids do better after treatment, yes, surgery is appropriate, and why wait till 21?” Bowers said. “That’s really completely arbitrary. In fact, it’s probably cruel.”
“Most of the research is on older patients,” Elizabeth Boskey, a social worker at the Center for Gender Surgery at Boston Children’s Hospital and co-author of several research papers on gender confirmation gender-affirming surgery in youth, notes. “But there is evidence in the literature about just overall improved health, reduced anxiety, increased ability to function, for individuals after they have these gender-affirming surgeries.”
What does research say about treatment of transgender youth?
A review of the latest research on gender-affirming hormones and surgery in transgender youth , published in a June 2019 edition of The Lancet Diabetes & Endocrinology , supports Bowers’ assertions that gender confirmation surgery benefits adolescents, though it does not go as far as to recommend specific age guidelines.
“Several preliminary studies have shown benefits of gender-affirming surgery in adolescents, particularly regarding bilateral mastectomy in transgender adolescent males, but there is a scarcity of literature to guide clinical practice for surgical vaginoplasty in transgender adolescent females,” the authors write. “The optimal age and developmental stage for initiating [cross sex hormones] and performing gender-affirming surgeries remains to be clarified.”
The World Professional Association for Transgender Health (WPATH), a leading organization for transgender health worldwide whose membership consists of physicians and educators, publishes Standards of Care and Ethical Guidelines for the treatment of transgender patients.
Though WPATH’s Standards of Care was last updated in 2011 and is under revision, even the current standards suggest that individuals at the age of majority in a given country (for the United States, that’s 18) who have lived for at least 12 months in accordance with their gender identity should be eligible for genital surgery, and that chest surgeries can be done earlier.
“I think it’s important to recognize for all of these standards of care, these are flexible guidelines,” says Loren Schechter, director of the Center for Gender Confirmation Surgery at Weiss Memorial Hospital , clinical professor of surgery at the University of Illinois at Chicago, and co-lead for the revision of the WPATH standards of care surgery chapter for adolescents and adults. “It is not necessarily uncommon that we will currently perform bottom surgeries under the legal age of majority now.”
Schechter also indicated that the revision of the standards will likely include lowered age guidelines.
One reason to give transgender youth access to surgery
Schechter maintains that there are many reasons why minors should be eligible to receive gender confirmation surgery.
“One of them is that post-operative care in a supportive environment is very important,” Schechter said. “So, for example, for those individuals going off to college, the ability to recuperate while at home in a supportive environment and parents during that post-operative period is quite important. Trying to have your post-operative care in a dorm room after surgery is it is not necessarily an ideal scenario.”
This reasoning was echoed in a paper published in the Journal of Sexual Medicine in April 2017 . For the study, researchers asked 20 WPATH-affiliated surgeons practicing in the U.S. about whether and why they performed genital surgery on transgender female minors.
Respondents noted the beneficial recovery environment some minor patients may have.
“Some surgeons viewed timing the procedure before college attendance as a harm reduction measure: Younger patients who have the support of their families, support of their parents, and can have the operation while they are still at home, as opposed to being alone at school or at work, anecdotally tend to do much better than someone who is alone and doesn’t have appropriate support.”
Others suggest that receiving surgery as a minor might allow the patient to “fully socially transition” in their next phase, such as in college.
Who is ready for surgery? Considerations beyond age
Physicians involved in the study also noted that while the number of minors requesting information about genital surgery had increased, psychological maturity is their main criteria for approval.
As one interviewed surgeon put it, “Age is arbitrary. The true measures of how well a patient will do are based on maturity, discipline and support.”
Eleven of the 20 surgeons interviewed had performed such surgeries. Minors ranged in age from 15 to “a day before 18.” About two-thirds of surgeons interviewed believe that such decisions should be made on a case-by-case basis rather than in strict adherence with current WPATH guidelines, which advises to wait until 18 in the U.S.
Boskey, who works for the Center for Gender Surgery at Boston Children’s Hospital, notes: “Just setting the age guidelines in place doesn’t remove the need to appropriately assess whether the surgery is something that should be happening,” she said.
“They’re going to need to make certain that the patient is appropriate for that surgery, that they are being diagnosed with gender dysphoria, that they are taking hormones as appropriate, that they are living in their affirmed gender, that they are aware of all of the life-changing nature of these surgeries,” she said. “These are surgeries that require pretty intense assessment to make certain that they’re appropriate. But that needs to come from the clinical side, rather than the insurance side.”
Will trans youth regret surgery? What the research says
Research supports the benefits of early interventions.
A 2018 study published in JAMA Pediatrics of 136 transmasculine youth and young adults between the ages of 13 and 25 receiving care at Children’s Hospital of Los Angeles finds that, on average, chest dysphoria, or distress caused by one’s chest, was significantly higher among participants who had not received chest reconstruction surgery as compared with those who did .
Serious complications among the surgery group were rare, and only one of the 68 patients who received surgery reported experiencing regret sometimes, with the other 67 reporting no regret over the procedure. The time that had elapsed between surgery and the survey ranged from less than 1 year to 5 years.
“Given these findings,” the authors conclude, “professional guidelines and clinical practice should consider patients for chest surgery based on individual need rather than chronologic age.”
Those who study the impact of early access to gender confirming surgeries often point to research from the Netherlands, home to one of the earliest comprehensive gender clinics.
“[T]hey’ve probably got the most data on transgender, gender non-conforming adolescents, who have been followed longitudinally, prospectively in the most rigorous way — that data indicates that people do well with early access and early interventions,” Schechter says. “By early, I mean late adolescence — we’re not, of course, talking about operating on children.”
Adolescents who were the first 22 people to receive gender confirming surgery at the clinic in the Netherlands showed after surgery that they no longer experienced distress over their gender, according to a 1997 publication in the Journal of the American Academy of Child & Adolescent Psychiatry .
The study also showed that the 22 adolescents scored within the normal range for a number of psychological measures.
Further, the authors note, “Not a single subject expressed feelings of regret concerning the decision to undergo sex reassignment.”
A follow-up study, published four years later, of another group of 20 adolescents receiving surgery after the first group of 22 confirmed the initial findings .
Another, later study in the Netherlands focused on the outcomes of 55 transgender young adults who received gender confirmation surgery between 2004 and 2011. The participants all “were generally satisfied with their physical appearance and none regretted treatment.”
Moreover, gender dysphoria was alleviated, mental health improved, and well-being among those studied was similar to or better than their peers in the general population.
About The Author
Chloe Reichel
- Share full article

Doctors Debate Whether Trans Teens Need Therapy Before Hormones
Clinicians are divided over new guidelines that say teens should undergo mental health screenings before receiving hormones or gender surgeries.
Laura Edwards-Leeper, a child clinical psychologist in Beaverton, Ore., who works with transgender adolescents, said they “absolutely have to be treated differently” than adults. Credit... Kristina Barker for The New York Times
Supported by
By Azeen Ghorayshi
- Jan. 13, 2022
An upsurge in teenagers requesting hormones or surgeries to better align their bodies with their gender identities has ignited a debate among doctors over when to provide these treatments.
An international group of experts focused on transgender health last month released a draft of new guidelines, the gold standard of the field that informs what insurers will reimburse for care.
Many doctors and activists praised the 350-page document, which was updated for the first time in nearly a decade, for including transgender people in its drafting and for removing language requiring adults to have psychological assessments before getting access to hormone therapy.
But the guidelines take a more cautious stance on teens. A new chapter dedicated to adolescents says that they must undergo mental health assessments and must have questioned their gender identity for “several years” before receiving drugs or surgeries.
Experts in transgender health are divided on these adolescent recommendations, reflecting a fraught debate over how to weigh conflicting risks for young people, who typically can’t give full legal consent until they are 18 and who may be in emotional distress or more vulnerable to peer influence than adults are.
Some of the drug regimens bring long-term risks, such as irreversible fertility loss. And in some cases, thought to be quite rare, transgender people later “detransition” to the gender they were assigned at birth. Given these risks, as well as the increasing number of adolescents seeking these treatments, some clinicians say that teens need more psychological assessment than adults do.
“They absolutely have to be treated differently,” said Laura Edwards-Leeper, a child clinical psychologist in Beaverton, Ore., who works with transgender adolescents.
Dr. Edwards-Leeper was one of seven authors of the new adolescent chapter, but the organization that publishes the guidelines, the World Professional Association for Transgender Health, did not authorize her to comment publicly on the draft’s proposed wording.
On the other side of the debate are clinicians who say the guidelines are calling for unnecessary barriers to urgently needed care. Transgender teens have a high risk of attempting suicide, according to the Centers for Disease Control and Prevention . And preliminary studies have suggested that adolescents who receive drug treatments to affirm their gender identity have improved mental health and well-being. Considering those data, some clinicians are opposed to any mental health requirements.
“I’m really not a believer in requiring that for people,” said Dr. Alex Keuroghlian, a clinical psychiatrist at Fenway Health in Boston and the director of the Massachusetts General Hospital Psychiatry Gender Identity Program. “Being trans isn’t a mental health problem,” he later added.
The public is invited to comment on the guidelines until Sunday, with a final version expected by spring.
As clinicians debate the intricacies of the new health standards, state legislatures across the country are trying to ban gender-affirming medical care for adolescents. According to the Williams Institute at the UCLA School of Law, 21 states introduced such bills last year. Gov. Greg Abbott of Texas has described gender surgeries as “genital mutilation” and “child abuse.”
Professional medical groups and transgender health specialists have overwhelmingly condemned these legal attempts as dangerous. So far, two have passed into law, in Tennessee and Arkansas, though the latter has temporarily been blocked because of legal appeals.
Some clinicians worry that public disagreement over the best way to care for transgender adolescents will add fuel to this simmering political movement.
“It’s a stressful environment to be in,” said Dr. Cassie Brady, a pediatric endocrinologist at Vanderbilt University Medical Center who provided legislative testimony to make the bill in Tennessee less restrictive. “It not only puts fear in us as providers, but way more fear I think for families who might be trying to balance this.”

“A real shift”
The first version of the guidelines, called the Standards of Care, was released by a small group of doctors at a San Diego meeting in 1979. At the time, there was little public acknowledgment of transgender people, and they had scant options for medical care.
The document “was a real shift,” said Beans Velocci, a historian at the University of Pennsylvania.
But those first guidelines characterized gender nonconformity as a psychological disorder . They stated that transgender people could be delusional or unreliable, and required two letters from psychiatrists before adults could access surgeries. That focus on psychology set a lasting precedent, experts said.
“The establishment medical world didn’t even understand it — they were still treating it as a mental health concern — just 20 years ago,” said Dr. Joshua Safer, an endocrinologist and executive director of the Center for Transgender Medicine and Surgery at Mt. Sinai, who contributed to the guidelines’ chapter on hormone therapy.
Children and teenagers struggling with their gender identities did not get much attention from the medical community until the 1990s, when two contrasting models emerged.
In one approach, clinicians in the Netherlands suggested that parents wait for puberty to make decisions about their children transitioning to another gender, pioneering the use of drugs that suppress the production of hormones like testosterone and estrogen. The Dutch model argued that these puberty blockers, which are reversible, would buy adolescents time to further explore their gender before starting hormones with more lasting consequences.
In another model, which was developed in Canada and is now considered a form of “conversion therapy,” children were pushed to live in the gender they were assigned at birth, in order to avoid drugs or surgeries down the line for those who might later change their minds.
Around the late 2000s, clinicians in the United States introduced the “gender affirming” approach, which has since been endorsed by several major medical groups . Its basic philosophy: Minors should be able to live out their gender identities freely, without clinicians or parents imposing unnecessary delays. Their path might involve medications and surgeries, or no medical treatments at all.
“Children are not short adults — but they have autonomy as well, and they can know their gender,” said Dr. Diane Ehrensaft, director of mental health at the University of California, San Francisco Child and Adolescent Gender Center. Dr. Ehrensaft is one of the key early proponents of the gender-affirming model and helped write a new chapter on prepubescent children in the draft guidelines.
Data on the number of transgender or gender nonconforming adolescents and adults in the United States are limited . About 1.8 percent of high school students surveyed in 19 state or urban school districts in 2017 described themselves as transgender , according to the C.D.C.
Adolescent gender clinics like Dr. Ehrensaft’s have seen a rapid growth in referral rates, and more sites have sprung up to meet demand. Today there are more than 50 such specialty clinics in the United States, she said, up from just four in 2012.
Few studies have followed adolescents receiving puberty blockers or hormones into adulthood. Dr. Ehrensaft and others are now working on large, long-term studies of patients in the United States.
An emerging divide
The new standards state that clinicians should facilitate an “open exploration” of gender with adolescents and their families, without pushing them in one direction or another. But the guidelines recommend restricting the use of medications and surgeries, partly because of their medical risks.
Puberty blockers, for example, can impede bone development , though evidence so far suggests it resumes once puberty is initiated. And if taken in the early phase of puberty, blockers and hormones lead to fertility loss. Patients and their families should be counseled about these risks, the standards say, and if preserving fertility is a priority, drugs should be delayed until a more advanced stage of puberty.
The guidelines suggest minimum ages, lower than those in the previous version, for each treatment: 14 for starting hormone therapy, 15 for chest masculinization and at least 17 for more invasive genital operations.
But the most contentious parts of the new standards among clinicians are the mental health requirements. Before discussing any medical treatment, they say, adolescents must get a “comprehensive assessment” led by mental health providers, and must have consistently questioned their gender identity for “several years.”
Although mental health counseling should be offered as needed, it should not be a requirement for medical care, said Dr. Keuroghlian of Fenway Health. He pointed out that therapy is not required for cisgender patients who get breast augmentation, hysterectomies or rhinoplasties.
“To make that a requirement for everybody is inherently unnecessary gatekeeping and also stigmatizing and pathologizing and a waste of resources,” he said.
What’s more, some of the mental health problems commonly seen in trans adolescents, such as depression and anxiety, may resolve after gender-affirming medical care, Dr. Keuroghlian said.
And some doctors have also argued that waiting several years to initiate medical treatments could itself be harmful.
“Forcing trans and gender diverse youth to go through an incongruent puberty can cause long-term trauma and physical harm,” said Dr. AJ Eckert, medical director of Anchor Health Initiative’s Gender and Life-Affirming Medicine Program in Stamford, Conn.
But other trans health specialists are concerned by the sharp increase in adolescents who are referred to gender clinics, and worry that the desire for hormones and surgeries may be driven partly by peer influence on social media platforms like TikTok and YouTube.
“The kids presenting these days are very different than what I was seeing in the early days,” said Dr. Edwards-Leeper, who in 2007 helped set up one of the first youth gender clinics in the United States, in Boston.
Dr. Edwards-Leeper said that now she was more likely to see adolescents who had recently begun to question their gender, whereas a decade ago her patients were more likely to have longstanding distress about their bodies.
These seemingly abrupt changes — as well as other mental health issues or a history of trauma — should be flags for providers to slow down, she said. Instead, some gender clinics with long wait lists are “blindly affirming” adolescent patients, she said, offering them hormones without taking these potential issues seriously.
And although it’s unclear how often it happens, some people who transitioned as teenagers have reported detransitioning later on. Although some people who detransition continue living with a more fluid gender identity, others are upset about living with the irreversible changes caused by hormones or surgeries.
“These issues of inadequate assessment and what I sometimes called hasty or sloppy care have resulted in potential harm,” said Erica Anderson, a clinical psychologist who works with transgender adolescents in Berkeley, Calif.
Dr. Anderson, 70, said she understood the trauma of being denied care. She first realized she was transgender in her 30s, but didn’t approach an endocrinologist about hormone treatments until age 45. “The doctor’s response was, ‘I can’t help you,’” she said. Despondent, she waited several more years before pursuing a medical transition again.
“I don’t want any young person to go without the care that they need,” Dr. Anderson said. “But the question is, are there new things going on that weren’t going on 10 or 15 years ago?”
Other doctors say they haven’t seen evidence to suggest that clinics are hastily providing medical treatments, or that many patients are experiencing regret about taking hormones. But they agree that teenagers require more mental health precautions than adults do.
“With kids, you’re more conservative,” said Dr. Safer of Mt. Sinai. But, he added, “I guess time and data will tell.”
Advertisement
Educate your inbox
Subscribe to Here’s the Deal, our politics newsletter for analysis you won’t find anywhere else.
Thank you. Please check your inbox to confirm.

Lindsey Tanner, Associated Press Lindsey Tanner, Associated Press
Leave your feedback
- Copy URL https://www.pbs.org/newshour/health/what-medical-treatments-do-transgender-youth-get
What medical treatments do transgender youth get?
Transgender medical treatment for children and teens is increasingly under attack in many states, labeled child abuse and subject to criminalizing bans. But it has been available in the United States for more than a decade and is endorsed by major medical associations.
Many clinics use treatment plans pioneered in Amsterdam 30 years ago, according to a recent review in the British Psych Bulletin. Since 2005, the number of youth referred to gender clinics has increased as much as tenfold in the U.S., U.K, Canada and Finland, the review said.
The World Professional Association for Transgender Health, a professional and educational organization, and the Endocrine Society, which represents specialists who treat hormone conditions, both have guidelines for such treatment . Here’s a look at what’s typically involved.
Puberty blockers
Children who persistently question the sex they were designated at birth are often referred to specialty clinics providing gender-confirming care. Such care typically begins with a psychological evaluation to determine whether the children have “gender dysphoria,” or distress caused when gender identity doesn’t match a person’s assigned sex.
Children who meet clinical guidelines are first offered medication that temporarily blocks puberty . This treatment is designed for youngsters diagnosed with gender dysphoria who have been counseled with their families and are mature enough to understand what the regimen entails.
‘I know who I am’: Transgender youth on the value of support, respect for their identities
The medication isn’t started until youngsters show early signs of puberty — enlargement of breasts or testicles. This typically occurs around age 8 to 13 for girls and a year or two later for boys.
The drugs, known as GnRH agonists, block the brain from releasing key hormones involved in sexual maturation. They have been used for decades to treat precocious puberty, an uncommon medical condition that causes puberty to begin abnormally early.
The drugs can be given as injections every few months or as arm implants lasting up to year or two. Their effects are reversible — puberty and sexual development resume as soon as the drugs are stopped.
Some kids stay on them for several years. One possible side effect: They may cause a decrease in bone density that reverses when the drugs are stopped.
After puberty blockers, kids can either go through puberty while still identifying as the opposite sex or begin treatment to make their bodies more closely match their gender identity.
For those choosing the second option, guidelines say the next step is taking manufactured versions of estrogen or testosterone — hormones that prompt sexual development in puberty . Estrogen comes in skin patches and pills. Testosterone treatment usually involves weekly injections.
READ MORE: The history behind International Transgender Day of Visibility
Guidelines recommend starting these when kids are mature enough to make informed medical decisions. That is typically around age 16, and parents’ consent is typically required, said Dr. Gina Sequiera, co-director of Seattle Children’s Hospital’s Gender Clinic.
Many transgender patients take the hormones for life, though some changes persist if medication is stopped.
In girls transitioning to boys, testosterone generally leads to permanent voice-lowering, facial hair and protrusion of the Adam’s apple, said Dr. Stephanie Roberts, a specialist at Boston Children’s Hospital’s Gender Management Service. For boys transitioning to girls, estrogen-induced breast development is typically permanent, Roberts said.
Research on long-term hormone use in transgender adults has found potential health risks including blood clots and cholesterol changes.
Gender-altering surgery in teens is less common than hormone treatment, but many centers hesitate to give exact numbers.
Guidelines say such surgery generally should be reserved for those aged 18 and older. The World Professional Association for Transgender Health says breast removal surgery is OK for those under 18 who have been on testosterone for at least a year. The Endocrine Society says there isn’t enough evidence to recommend a specific age limit for that operation.
Studies have found some children and teens resort to self-mutilation to try to change their anatomy. And research has shown that transgender youth and adults are prone to stress, depression and suicidal behavior when forced to live as the sex they were assigned at birth.
Opponents of youth transgender medical treatment say there’s no solid proof of purported benefits and cite widely discredited research claiming that most untreated kids outgrow their transgender identities by their teen years or later. One study often mentioned by opponents included many kids who were mistakenly identified as having gender dysphoria and lacked outcome data for many others.
READ MORE: Giving homeless transgender youth a safe haven from the streets
Doctors say accurately diagnosed kids whose transgender identity persists into puberty typically don’t outgrow it. And guidelines say treatment shouldn’t start before puberty begins.
Many studies show the treatment can improve kids’ well-being, including reducing depression and suicidal behavior. The most robust kind of study — a trial in which some distressed kids would be given treatment and others not — cannot be done ethically. Longer term studies on treatment outcomes are underway.
Support Provided By: Learn more

2021 set a record for anti-transgender bills. Here’s how you can support the community
Nation Dec 30
- Introduction
- Conclusions
- Article Information
Error bars represent 95% CIs. GAS indicates gender-affirming surgery.
Percentages are based on the number of procedures divided by number of patients; thus, as some patients underwent multiple procedures the total may be greater than 100%. Error bars represent 95% CIs.
eTable. ICD-10 and CPT Codes of Gender-Affirming Surgery
eFigure. Percentage of Patients With Codes for Gender Identity Disorder Who Underwent GAS
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Wright JD , Chen L , Suzuki Y , Matsuo K , Hershman DL. National Estimates of Gender-Affirming Surgery in the US. JAMA Netw Open. 2023;6(8):e2330348. doi:10.1001/jamanetworkopen.2023.30348
Manage citations:
© 2024
- Permissions
National Estimates of Gender-Affirming Surgery in the US
- 1 Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, New York, New York
- 2 Department of Obstetrics and Gynecology, University of Southern California, Los Angeles
Question What are the temporal trends in gender-affirming surgery (GAS) in the US?
Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
Meaning These findings suggest that there will be a greater need for clinicians knowledgeable in the care of transgender individuals with the requisite expertise to perform gender-affirming procedures.
Importance While changes in federal and state laws mandating coverage of gender-affirming surgery (GAS) may have led to an increase in the number of annual cases, comprehensive data describing trends in both inpatient and outpatient procedures are limited.
Objective To examine trends in inpatient and outpatient GAS procedures in the US and to explore the temporal trends in the types of GAS performed across age groups.
Design, Setting, and Participants This cohort study includes data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. Patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified, and the performance of GAS, including breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures, were identified.
Main Outcome Measures Weighted estimates of the annual number of inpatient and outpatient procedures performed and the distribution of each class of procedure overall and by age were analyzed.
Results A total of 48 019 patients who underwent GAS were identified, including 25 099 (52.3%) who were aged 19 to 30 years. The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years. When stratified by the type of procedure performed, breast and chest procedures made up a greater percentage of the surgical interventions in younger patients, while genital surgical procedures were greater in older patients.
Conclusions and Relevance Performance of GAS has increased substantially in the US. Breast and chest surgery was the most common group of procedures performed. The number of genital surgical procedures performed increased with increasing age.
Gender dysphoria is characterized as an incongruence between an individual’s experienced or expressed gender and the gender that was assigned at birth. 1 Transgender individuals may pursue multiple treatments, including behavioral therapy, hormonal therapy, and gender-affirming surgery (GAS). 2 GAS encompasses a variety of procedures that align an individual patient’s gender identity with their physical appearance. 2 - 4
While numerous surgical interventions can be considered GAS, the procedures have been broadly classified as breast and chest surgical procedures, facial and cosmetic interventions, and genital reconstructive surgery. 2 , 4 Prior studies 2 - 7 have shown that GAS is associated with improved quality of life, high rates of satisfaction, and a reduction in gender dysphoria. Furthermore, some studies have reported that GAS is associated with decreased depression and anxiety. 8 Lastly, the procedures appear to be associated with acceptable morbidity and reasonable rates of perioperative complications. 2 , 4
Given the benefits of GAS, the performance of GAS in the US has increased over time. 9 The increase in GAS is likely due in part to federal and state laws requiring coverage of transition-related care, although actual insurance coverage of specific procedures is variable. 10 , 11 While prior work has shown that the use of inpatient GAS has increased, national estimates of inpatient and outpatient GAS are lacking. 9 This is important as many GAS procedures occur in ambulatory settings. We performed a population-based analysis to examine trends in GAS in the US and explored the temporal trends in the types of GAS performed across age groups.
To capture both inpatient and outpatient surgical procedures, we used data from the Nationwide Ambulatory Surgery Sample (NASS) and the National Inpatient Sample (NIS). NASS is an ambulatory surgery database and captures major ambulatory surgical procedures at nearly 2800 hospital-owned facilities from up to 35 states, approximating a 63% to 67% stratified sample of hospital-owned facilities. NIS comprehensively captures approximately 20% of inpatient hospital encounters from all community hospitals across 48 states participating in the Healthcare Cost and Utilization Project (HCUP), covering more than 97% of the US population. Both NIS and NASS contain weights that can be used to produce US population estimates. 12 , 13 Informed consent was waived because data sources contain deidentified data, and the study was deemed exempt by the Columbia University institutional review board. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We selected patients of all ages with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision ( ICD-10 ) diagnosis codes for gender identity disorder or transsexualism ( ICD-10 F64) or a personal history of sex reassignment ( ICD-10 Z87.890) from 2016 to 2020 (eTable in Supplement 1 ). We first examined all hospital (NIS) and ambulatory surgical (NASS) encounters for patients with these codes and then analyzed encounters for GAS within this cohort. GAS was identified using ICD-10 procedure codes and Common Procedural Terminology codes and classified as breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures. 2 , 4 Breast and chest surgical procedures encompassed breast reconstruction, mammoplasty and mastopexy, or nipple reconstruction. Genital reconstructive procedures included any surgical intervention of the male or female genital tract. Other facial and cosmetic procedures included cosmetic facial procedures and other cosmetic procedures including hair removal or transplantation, liposuction, and collagen injections (eTable in Supplement 1 ). Patients might have undergone procedures from multiple different surgical groups. We measured the total number of procedures and the distribution of procedures within each procedural group.
Within the data sets, sex was based on patient self-report. The sex of patients in NIS who underwent inpatient surgery was classified as either male, female, missing, or inconsistent. The inconsistent classification denoted patients who underwent a procedure that was not consistent with the sex recorded on their medical record. Similar to prior analyses, patients in NIS with a sex variable not compatible with the procedure performed were classified as having undergone genital reconstructive surgery (GAS not otherwise specified). 9
Clinical variables in the analysis included patient clinical and demographic factors and hospital characteristics. Demographic characteristics included age at the time of surgery (12 to 18 years, 19 to 30 years, 31 to 40 years, 41 to 50 years, 51 to 60 years, 61 to 70 years, and older than 70 years), year of the procedure (2016-2020), and primary insurance coverage (private, Medicare, Medicaid, self-pay, and other). Race and ethnicity were only reported in NIS and were classified as White, Black, Hispanic and other. Race and ethnicity were considered in this study because prior studies have shown an association between race and GAS. The income status captured national quartiles of median household income based of a patient’s zip code and was recorded as less than 25% (low), 26% to 50% (medium-low), 51% to 75% (medium-high), and 76% or more (high). The Elixhauser Comorbidity Index was estimated for each patient based on the codes for common medical comorbidities and weighted for a final score. 14 Patients were classified as 0, 1, 2, or 3 or more. We separately reported coding for HIV and AIDS; substance abuse, including alcohol and drug abuse; and recorded mental health diagnoses, including depression and psychoses. Hospital characteristics included a composite of teaching status and location (rural, urban teaching, and urban nonteaching) and hospital region (Northeast, Midwest, South, and West). Hospital bed sizes were classified as small, medium, and large. The cutoffs were less than 100 (small), 100 to 299 (medium), and 300 or more (large) short-term acute care beds of the facilities from NASS and were varied based on region, urban-rural designation, and teaching status of the hospital from NIS. 8 Patients with missing data were classified as the unknown group and were included in the analysis.
National estimates of the number of GAS procedures among all hospital encounters for patients with gender identity disorder were derived using discharge or encounter weight provided by the databases. 15 The clinical and demographic characteristics of the patients undergoing GAS were reported descriptively. The number of encounters for gender identity disorder, the percentage of GAS procedures among those encounters, and the absolute number of each procedure performed over time were estimated. The difference by age group was examined and tested using Rao-Scott χ 2 test. All hypothesis tests were 2-sided, and P < .05 was considered statistically significant. All analyses were conducted using SAS version 9.4 (SAS Institute Inc).
A total of 48 019 patients who underwent GAS were identified ( Table 1 ). Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged 12 to 18 years. Private insurance coverage was most common in 29 064 patients (60.5%), while 12 127 (25.3%) were Medicaid recipients. Depression was reported in 7192 patients (15.0%). Most patients (42 467 [88.4%]) were treated at urban, teaching hospitals, and there was a disproportionate number of patients in the West (22 037 [45.9%]) and Northeast (12 396 [25.8%]). Within the cohort, 31 668 patients (65.9%) underwent 1 procedure while 13 415 (27.9%) underwent 2 procedures, and the remainder underwent multiple procedures concurrently ( Table 1 ).
The overall number of health system encounters for gender identity disorder rose from 13 855 in 2016 to 38 470 in 2020. Among encounters with a billing code for gender identity disorder, there was a consistent rise in the percentage that were for GAS from 4552 (32.9%) in 2016 to 13 011 (37.1%) in 2019, followed by a decline to 12 818 (33.3%) in 2020 ( Figure 1 and eFigure in Supplement 1 ). Among patients undergoing ambulatory surgical procedures, 37 394 (80.3%) of the surgical procedures included gender-affirming surgical procedures. For those with hospital admissions with gender identity disorder, 10 625 (11.8%) of admissions were for GAS.
Breast and chest procedures were most common and were performed for 27 187 patients (56.6%). Genital reconstruction was performed for 16 872 patients (35.1%), and other facial and cosmetic procedures for 6669 patients (13.9%) ( Table 2 ). The most common individual procedure was breast reconstruction in 21 244 (44.2%), while the most common genital reconstructive procedure was hysterectomy (4489 [9.3%]), followed by orchiectomy (3425 [7.1%]), and vaginoplasty (3381 [7.0%]). Among patients who underwent other facial and cosmetic procedures, liposuction (2945 [6.1%]) was most common, followed by rhinoplasty (2446 [5.1%]) and facial feminizing surgery and chin augmentation (1874 [3.9%]).
The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020 ( Figure 1 ). Similar trends were noted for breast and chest surgical procedures as well as genital surgery, while the rate of other facial and cosmetic procedures increased consistently from 2016 to 2020. The distribution of the individual procedures performed in each class were largely similar across the years of analysis ( Table 3 ).
When stratified by age, patients 19 to 30 years had the greatest number of procedures, 25 099 ( Figure 2 ). There were 10 476 procedures performed in those aged 31 to 40 years and 4359 in those aged 41 to 50 years. Among patients younger than 19 years, 3678 GAS procedures were performed. GAS was less common in those cohorts older than 50 years. Overall, the greatest number of breast and chest surgical procedures, genital surgical procedures, and facial and other cosmetic surgical procedures were performed in patients aged 19 to 30 years.
When stratified by the type of procedure performed, breast and chest procedures made up the greatest percentage of the surgical interventions in younger patients while genital surgical procedures were greater in older patients ( Figure 2 ). Additionally, 3215 patients (87.4%) aged 12 to 18 years underwent GAS and had breast or chest procedures. This decreased to 16 067 patients (64.0%) in those aged 19 to 30 years, 4918 (46.9%) in those aged 31 to 40 years, and 1650 (37.9%) in patients aged 41 to 50 years ( P < .001). In contrast, 405 patients (11.0%) aged 12 to 18 years underwent genital surgery. The percentage of patients who underwent genital surgery rose sequentially to 4423 (42.2%) in those aged 31 to 40 years, 1546 (52.3%) in those aged 51 to 60 years, and 742 (58.4%) in those aged 61 to 70 years ( P < .001). The percentage of patients who underwent facial and other cosmetic surgical procedures rose with age from 9.5% in those aged 12 to 18 years to 20.6% in those aged 51 to 60 years, then gradually declined ( P < .001). Figure 2 displays the absolute number of procedure classes performed by year stratified by age. The greatest magnitude of the decline in 2020 was in younger patients and for breast and chest procedures.
These findings suggest that the number of GAS procedures performed in the US has increased dramatically, nearly tripling from 2016 to 2019. Breast and chest surgery is the most common class of procedure performed while patients are most likely to undergo surgery between the ages of 19 and 30 years. The number of genital surgical procedures performed increased with increasing age.
Consistent with prior studies, we identified a remarkable increase in the number of GAS procedures performed over time. 9 , 16 A prior study examining national estimates of inpatient GAS procedures noted that the absolute number of procedures performed nearly doubled between 2000 to 2005 and from 2006 to 2011. In our analysis, the number of GAS procedures nearly tripled from 2016 to 2020. 9 , 17 Not unexpectedly, a large number of the procedures we captured were performed in the ambulatory setting, highlighting the need to capture both inpatient and outpatient procedures when analyzing data on trends. Like many prior studies, we noted a decrease in the number of procedures performed in 2020, likely reflective of the COVID-19 pandemic. 18 However, the decline in the number of procedures performed between 2019 and 2020 was relatively modest, particularly as these procedures are largely elective.
Analysis of procedure-specific trends by age revealed a number of important findings. First, GAS procedures were most common in patients aged 19 to 30 years. This is in line with prior work that demonstrated that most patients first experience gender dysphoria at a young age, with approximately three-quarters of patients reporting gender dysphoria by age 7 years. These patients subsequently lived for a mean of 23 years for transgender men and 27 years for transgender women before beginning gender transition treatments. 19 Our findings were also notable that GAS procedures were relatively uncommon in patients aged 18 years or younger. In our cohort, fewer than 1200 patients in this age group underwent GAS, even in the highest volume years. GAS in adolescents has been the focus of intense debate and led to legislative initiatives to limit access to these procedures in adolescents in several states. 20 , 21
Second, there was a marked difference in the distribution of procedures in the different age groups. Breast and chest procedures were more common in younger patients, while genital surgery was more frequent in older individuals. In our cohort of individuals aged 19 to 30 years, breast and chest procedures were twice as common as genital procedures. Genital surgery gradually increased with advancing age, and these procedures became the most common in patients older than 40 years. A prior study of patients with commercial insurance who underwent GAS noted that the mean age for mastectomy was 28 years, significantly lower than for hysterectomy at age 31 years, vaginoplasty at age 40 years, and orchiectomy at age 37 years. 16 These trends likely reflect the increased complexity of genital surgery compared with breast and chest surgery as well as the definitive nature of removal of the reproductive organs.
This study has limitations. First, there may be under-capture of both transgender individuals and GAS procedures. In both data sets analyzed, gender is based on self-report. NIS specifically makes notation of procedures that are considered inconsistent with a patient’s reported gender (eg, a male patient who underwent oophorectomy). Similar to prior work, we assumed that patients with a code for gender identity disorder or transsexualism along with a surgical procedure classified as inconsistent underwent GAS. 9 Second, we captured procedures commonly reported as GAS procedures; however, it is possible that some of these procedures were performed for other underlying indications or diseases rather than solely for gender affirmation. Third, our trends showed a significant increase in procedures through 2019, with a decline in 2020. The decline in services in 2020 is likely related to COVID-19 service alterations. Additionally, while we comprehensively captured inpatient and ambulatory surgical procedures in large, nationwide data sets, undoubtedly, a small number of procedures were performed in other settings; thus, our estimates may underrepresent the actual number of procedures performed each year in the US.
These data have important implications in providing an understanding of the use of services that can help inform care for transgender populations. The rapid rise in the performance of GAS suggests that there will be a greater need for clinicians knowledgeable in the care of transgender individuals and with the requisite expertise to perform GAS procedures. However, numerous reports have described the political considerations and challenges in the delivery of transgender care. 22 Despite many medical societies recognizing the necessity of gender-affirming care, several states have enacted legislation or policies that restrict gender-affirming care and services, particularly in adolescence. 20 , 21 These regulations are barriers for patients who seek gender-affirming care and provide legal and ethical challenges for clinicians. As the use of GAS increases, delivering equitable gender-affirming care in this complex landscape will remain a public health challenge.
Accepted for Publication: July 15, 2023.
Published: August 23, 2023. doi:10.1001/jamanetworkopen.2023.30348
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Wright JD et al. JAMA Network Open .
Corresponding Author: Jason D. Wright, MD, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, 161 Fort Washington Ave, 4th Floor, New York, NY 10032 ( [email protected] ).
Author Contributions: Dr Wright had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Wright, Chen.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Wright.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Wright, Chen.
Administrative, technical, or material support: Wright, Suzuki.
Conflict of Interest Disclosures: Dr Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

The Evidence for Trans Youth Gender-Affirming Medical Care
Research suggests gender-affirming medical care results in better mental health..
Posted January 24, 2022 | Reviewed by Abigail Fagan
- Sixteen studies to date have examined the impact of gender-affirming medical care for transgender youth.
- Existing evidence suggests that gender-affirming medical care results in favorable mental health outcomes.
- All major medical organizations oppose legislation that would ban gender-affirming medical care for transgender adolescents.
NOTE: This post was updated on October 11, 2022. In discussions of studies 5, 7, 8 and 10, the final sentence was appended to include further information about the study.
I'm a physician-scientist who studies the mental health of transgender and gender diverse youth. I also spend a lot of time on Twitter . And yes I know, that's my first mistake. I've noticed there seem to be hundreds if not thousands of Twitter accounts that will repeatedly post that there is no evidence that gender-affirming medical care results in good mental health outcomes for transgender youth.
Since several U.S. states are introducing legislation to outlaw gender-affirming medical care this year (despite opposition from just about every major medical organization including The American Medical Association, The American Academy of Pediatrics, and The American Psychiatric Association), I thought this was a good time to review the relevant research for you all. So buckle up — here we go. The studies are in chronological order. I'll provide a brief summary of each and provide the citation for people who want to read more. I'll plan on updating this post as new studies become available. As you read, please keep in mind that all studies have methodological strengths and weaknesses and conclusions must be drawn from all of these studies together.
The Studies
Study 1: De Vries, A. L., Steensma, T. D., Doreleijers, T. A., & Cohen‐Kettenis, P. T. (2011). Puberty suppression in adolescents with gender identity disorder: A prospective follow‐up study. The Journal of Sexual Medicine, 8(8), 2276-2283.
This study from the Netherlands followed 70 transgender adolescents and measured their mental health before and after pubertal suppression. Study participants had improvements in depression and global functioning following treatment. However, feelings of anxiety and anger , gender dysphoria , and body satisfaction did not change.
Study 2: De Vries, A. L., McGuire, J. K., Steensma, T. D., Wagenaar, E. C., Doreleijers, T. A., & Cohen-Kettenis, P. T. (2014). Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics, 134(4), 696-704.
Another study from the Netherlands. This one followed 55 transgender adolescents through pubertal suppression, gender-affirming hormone treatment ( estrogen or testosterone ), and gender-affirming genital surgery (as adults). Of note, many of these participants were also participants in study 1 (this study followed them for longer). The researchers found that psychological functioning steadily improved over the course of the study and by adulthood these now young adults had global functioning scores similar to or better than age-matched peers in the general population. Of note, one patient in this study died from a surgical complication of vaginoplasty (necrotizing fasciitis), but little additional information is provided.
Study 3: Costa, R., Dunsford, M., Skagerberg, E., Holt, V., Carmichael, P., & Colizzi, M. (2015). Psychological support, puberty suppression, and psychosocial functioning in adolescents with gender dysphoria. The Journal of Sexual Medicine, 12(11), 2206-2214.
This study is from the United Kingdom. They followed 101 adolescents who received pubertal suppression at the beginning of the study and 100 adolescents who, for a range of reasons, were deemed by the team not ready to start pubertal suppression and thus did not receive it over the course of the study. Both groups received supportive psychotherapy . Both groups saw improvement in mental health. While the pubertal suppression group had a 5-point higher mean score on the study's psychological functioning scale at the end of the study, the difference was not statistically significant. This could have been due to the small sample size by the end of the study (the researchers only had data from 36 participants in the therapy-only group and 35 participants in the pubertal suppression group at the final time point of the study). We will see that later studies were able to obtain larger sample sizes so that statistically significant differences between those who did and did not receive pubertal suppression could be detected.
Study 4: Allen, L. R., Watson, L. B., Egan, A. M., & Moser, C. N. (2019). Well-being and suicidality among transgender youth after gender-affirming hormones. Clinical Practice in Pediatric Psychology, 7(3), 302.
This study was from researchers at Children's Mercy Hospital Gender Pathway Services Clinic in Missouri. They followed 47 transgender adolescents who received gender-affirming hormones (estrogen or testosterone) to a mean 349 days after starting treatment. They found statistically significant increases in general well-being and a statistically significant decrease in suicidality. Of note, the adolescents also received psychotherapy.
Study 5: Kaltiala, R., Heino, E., Työläjärvi, M., & Suomalainen, L. (2020). Adolescent development and psychosocial functioning after starting cross-sex hormones for gender dysphoria. Nordic Journal of Psychiatry, 74(3), 213-219.
This study is from Finland. Researchers conducted a retrospective chart review of 52 adolescents who received gender-affirming hormones (estrogen or testosterone) and found statistically significant decreases in need for specialist level psychiatric treatment for depression (decreased from 54% to 15%), anxiety (decreased from 48% to 15%), and suicidality or self-harm (decreased from 35% to 4%) following treatment. However, the authors note that gender reassignment is "not enough to improve functioning and relieve psychiatric comorbidities among adolescents with gender dysphoria."
Study 6: de Lara, D. L., Rodríguez, O. P., Flores, I. C., Masa, J. L. P., Campos-Muñoz, L., Hernández, M. C., & Amador, J. T. R. (2020). Psychosocial assessment in transgender adolescents. Anales de Pediatría (English Edition), 93(1), 41-48.
This study is from Spain. It followed 23 transgender adolescents who received gender-affirming hormones (estrogen or testosterone) and 30 cisgender controls for approximately one year. They found the transgender adolescents at baseline had worse measures of mental health than the cisgender control adolescents but that this difference equalized by the end of the study. The transgender adolescents in the study who received gender-affirming hormones had statistically significant improvements in several mental health measures, including anxiety and depression.
Study 7: van der Miesen, A. I., Steensma, T. D., de Vries, A. L., Bos, H., & Popma, A. (2020). Psychological functioning in transgender adolescents before and after gender-affirmative care compared with cisgender general population peers. Journal of Adolescent Health, 66(6), 699-704.
This was another Dutch study, with an impressive sample size. Researchers compared 272 transgender adolescents referred to the gender clinic who had not yet received pubertal suppression with 178 transgender adolescents who had received pubertal suppression. They found those who received pubertal suppression had better mental health outcomes than those who did not receive pubertal suppression. However, because subjects received psychotherapy, the authors note that the study does not provide "direct evidence" that pubertal suppression improves mental health in transgender youth.

Study 8: Achille, C., Taggart, T., Eaton, N. R., Osipoff, J., Tafuri, K., Lane, A., & Wilson, T. A. (2020). Longitudinal impact of gender-affirming endocrine intervention on the mental health and well-being of transgender youths: preliminary results. International Journal of Pediatric Endocrinology, 2020(1), 1-5.
This study was from Stony Brook Children's Hospital in New York. It followed 50 transgender adolescents longitudinally. Over the course of the study, 23 received pubertal suppression only, 35 received gender-affirming hormones only, and 11 received both. Three participants received no gender-affirming medical interventions. Over the course of the study, there was a statistically significant decrease in depression scores in one group: Male-to-female transitioners who underwent puberty suppression only.
Study 9: Kuper, L. E., Stewart, S., Preston, S., Lau, M., & Lopez, X. (2020). Body dissatisfaction and mental health outcomes of youth on gender-affirming hormone therapy. Pediatrics, 145(4).
This study was from a gender clinic in Dallas, Texas. The researchers followed 148 transgender adolescents who were receiving gender-affirming medical treatment. 25 received pubertal suppression only, 93 received gender-affirming hormones (estrogen or testosterone) only, and 30 received both. 15 participants received gender-affirming chest surgery. When examining all participants together, the study found statistically significant improvements in body dissatisfaction, depressive symptoms, and anxiety symptoms.
Study 10: Turban, J. L., King, D., Carswell, J. M., & Keuroghlian, A. S. (2020). Pubertal suppression for transgender youth and risk of suicidal ideation. Pediatrics, 145(2).
This study was conducted by myself along with several other researchers from Harvard Medical School. It utilized data from a non-probability sample of 20,619 transgender adults who reported ever wanting pubertal suppression. Of these, 89 actually received pubertal suppression. After adjusting for potentially confounding variables , access to pubertal suppression was associated with a lower odds of lifetime suicidal ideation. Of note, this study did not identify psychotherapy as a potentially confounding variable.
Study 11: Carmichael, P., Butler, G., Masic, U., Cole, T. J., De Stavola, B. L., Davidson, S., ... & Viner, R. M. (2021). Short-term outcomes of pubertal suppression in a selected cohort of 12 to 15 year old young people with persistent gender dysphoria in the UK. PLoS One, 16(2), e0243894.
This is another study from the United Kingdom. Researchers presented data for transgender adolescents who had received pubertal suppression. They had data for 44 patients after 12 months of treatment, 24 patients after 24 months of treatment, and 14 patients after 36 months of treatment. They were unable to detect any changes on their mental health measures (positive or negative).
Study 12: Grannis, C., Leibowitz, S. F., Gahn, S., Nahata, L., Morningstar, M., Mattson, W. I., ... & Nelson, E. E. (2021). Testosterone treatment, internalizing symptoms, and body image dissatisfaction in transgender boys. Psychoneuroendocrinology, 132, 105358.
This study recruited 42 birth-assigned female adolescents from a gender clinic in Ohio. Nineteen were receiving testosterone and 23 were not. Those not receiving testosterone were not receiving it due to a number of reasons (referred to endocrinology but hadn't started, parents not providing consent, and one was not interested in testosterone). The adolescents who were receiving testosterone treatment had lower scores on measures of generalized anxiety, social anxiety , depression, and body image dissatisfaction.
Study 13: Hisle-Gorman, E., Schvey, N. A., Adirim, T. A., Rayne, A. K., Susi, A., Roberts, T. A., & Klein, D. A. (2021). Mental healthcare utilization of transgender youth before and after affirming treatment. The Journal of Sexual Medicine, 18(8), 1444-1454.
This study utilized military healthcare data from transgender youth who received medical care through the U.S. military healthcare system. The researchers identified 963 transgender adolescents who had received some form of gender-affirming medical treatment. The mean age of starting any gender-affirming medical care was 18.2 (so this study may not technically qualify for our review of studies of adolescents). Their outcomes of interest were number of mental healthcare visits after gender-affirming medical care and number of days taking a psychiatric medication after starting gender-affirming medical care. In their adjusted models, there was no change in number of annual mental healthcare visits and an increase in days taking psychiatric medication from a mean 120 days per year to a mean 212 days per year. It's difficult to make firm conclusions based on this study, given the unusual outcome measure of number of days per year taking a psychiatric medication. The authors present a range of possible interpretations in the discussion section of the manuscript for those who are interested.
Study 14: Green, A. E., DeChants, J. P., Price, M. N., & Davis, C. K. (2021). Association of gender-affirming hormone therapy with depression, thoughts of suicide, and attempted suicide among transgender and nonbinary youth. Journal of Adolescent Health.
This study was conducted by researchers from The Trevor Project. They recruited 5,753 transgender adolescents who said they wanted gender-affirming hormone treatment (estrogen or testosterone). Of these, 1,216 had accessed gender-affirming hormones treatment. To focus on the results for only participants who were under 18: After adjusting for potential confounding variables, access to gender-affirming hormones was associated with lower odds of recent depression and suicide attempts when compared to those who desired but did not access gender-affirming hormones.
Study 15: Turban, J. L., King, D., Kobe, J., Reisner, S. L., & Keuroghlian, A. S. (2022). Access to gender-affirming hormones during adolescence and mental health outcomes among transgender adults. PLoS One, 17(1), e0261039.
This study was also conducted by me and other researchers at Harvard Medical School. We examined 21,598 adults who reported ever desiring gender-affirming hormones (estrogen or testosterone). Of these, 481 accessed gender-affirming hormones during adolescence, 12,257 accessed gender-affirming hormones as adults, and 8,860 were never able to access gender-affirming hormones. We found that regardless of age of initiation, accessing gender-affirming hormones was associated with lower odds of past-year suicidal ideation and past year severe psychological distress. We also found that access to gender-affirming hormones during adolescence was associated with a lower odds of these same adverse mental health outcomes when compared to not accessing gender-affirming hormones until adulthood. Because the study was cross-sectional, we created a variable for people who had suicidal ideation in the past but did not have it in the past year (a proxy for mental health improving over time). We found that people who accessed gender-affirming hormones were more likely to meet this criterion than people who desired but did not access gender-affirming hormones, arguing against reverse causation (a common problem with cross-sectional studies).
Study 16: Tordoff, D. M., Wanta, J. W., Collin, A., Stephney, C., Inwards-Breland, D. J., Ahrens, K. (2022) Mental Health Outcomes in Transgender and Nonbinary Youths Receiving Gender-Affirming Care. JAMA Network Open, 5(2), e220978.
This study was a prospective cohort study from Seattle Children's Gender Clinic. The researchers followed 104 transgender and non-binary youth who were receiving gender-affirming medical treatment. After adjusting for temporal trends and potential confounders, they found lower odds of depression and suicidality among young people who had started gender-affirming medical care, when compared to those who did not.
No Randomized Controlled Trials
One will notice that there have not been any randomized controlled trials. There is a general consensus in the field that such a trial would be unethical given the body of literature we have so far indicating that those in the control group would be likely to suffer adverse mental health outcomes compared to those randomized to the treatment groups. For this reason, it appears that no institutional review board would approve a randomized controlled trial at this time, under the principle of "equipoise" to which some bioethicists refer.
In summary, there have been, to my knowledge, 16 studies to date studying the impact of gender-affirming medical care for transgender adolescents. Taken together, the body of research indicates that these interventions result in favorable mental health outcomes. I will continue to update this post as new studies become available. Please feel free to contact me if you are aware of any new studies I have not yet included.
De Vries, A. L., Steensma, T. D., Doreleijers, T. A., & Cohen‐Kettenis, P. T. (2011). Puberty suppression in adolescents with gender identity disorder: A prospective follow‐up study. The Journal of Sexual Medicine, 8(8), 2276-2283.
De Vries, A. L., McGuire, J. K., Steensma, T. D., Wagenaar, E. C., Doreleijers, T. A., & Cohen-Kettenis, P. T. (2014). Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics, 134(4), 696-704.
Costa, R., Dunsford, M., Skagerberg, E., Holt, V., Carmichael, P., & Colizzi, M. (2015). Psychological support, puberty suppression, and psychosocial functioning in adolescents with gender dysphoria. The Journal of Sexual Medicine, 12(11), 2206-2214.
Allen, L. R., Watson, L. B., Egan, A. M., & Moser, C. N. (2019). Well-being and suicidality among transgender youth after gender-affirming hormones. Clinical Practice in Pediatric Psychology, 7(3), 302.
Kaltiala, R., Heino, E., Työläjärvi, M., & Suomalainen, L. (2020). Adolescent development and psychosocial functioning after starting cross-sex hormones for gender dysphoria. Nordic Journal of Psychiatry, 74(3), 213-219.
de Lara, D. L., Rodríguez, O. P., Flores, I. C., Masa, J. L. P., Campos-Muñoz, L., Hernández, M. C., & Amador, J. T. R. (2020). Psychosocial assessment in transgender adolescents. Anales de Pediatría (English Edition), 93(1), 41-48.
van der Miesen, A. I., Steensma, T. D., de Vries, A. L., Bos, H., & Popma, A. (2020). Psychological functioning in transgender adolescents before and after gender-affirmative care compared with cisgender general population peers. Journal of Adolescent Health, 66(6), 699-704.
Achille, C., Taggart, T., Eaton, N. R., Osipoff, J., Tafuri, K., Lane, A., & Wilson, T. A. (2020). Longitudinal impact of gender-affirming endocrine intervention on the mental health and well-being of transgender youths: preliminary results. International Journal of Pediatric Endocrinology, 2020(1), 1-5.
Kuper, L. E., Stewart, S., Preston, S., Lau, M., & Lopez, X. (2020). Body dissatisfaction and mental health outcomes of youth on gender-affirming hormone therapy. Pediatrics, 145(4).
Turban, J. L., King, D., Carswell, J. M., & Keuroghlian, A. S. (2020). Pubertal suppression for transgender youth and risk of suicidal ideation. Pediatrics, 145(2).
Carmichael, P., Butler, G., Masic, U., Cole, T. J., De Stavola, B. L., Davidson, S., ... & Viner, R. M. (2021). Short-term outcomes of pubertal suppression in a selected cohort of 12 to 15 year old young people with persistent gender dysphoria in the UK. PLoS One, 16(2), e0243894.
Grannis, C., Leibowitz, S. F., Gahn, S., Nahata, L., Morningstar, M., Mattson, W. I., ... & Nelson, E. E. (2021). Testosterone treatment, internalizing symptoms, and body image dissatisfaction in transgender boys. Psychoneuroendocrinology, 132, 105358.
Hisle-Gorman, E., Schvey, N. A., Adirim, T. A., Rayne, A. K., Susi, A., Roberts, T. A., & Klein, D. A. (2021). Mental healthcare utilization of transgender youth before and after affirming treatment. The Journal of Sexual Medicine, 18(8), 1444-1454.
Green, A. E., DeChants, J. P., Price, M. N., & Davis, C. K. (2021). Association of gender-affirming hormone therapy with depression, thoughts of suicide, and attempted suicide among transgender and nonbinary youth. Journal of Adolescent Health.
Turban, J. L., King, D., Kobe, J., Reisner, S. L., & Keuroghlian, A. S. (2022). Access to gender-affirming hormones during adolescence and mental health outcomes among transgender adults. PLoS One, 17(1), e0261039.
Tordoff, D. M., Wanta, J. W., Collin, A., Stephney, C., Inwards-Breland, D. J., Ahrens, K. (2022) Mental Health Outcomes in Transgender and Nonbinary Youths Receiving Gender-Affirming Care. JAMA Network Open, 5(2), e220978.

Jack Turban MD MHS is a writer and fellow in child and adolescent psychiatry at Stanford University School of Medicine, where he researches the mental health of transgender and gender diverse youth.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Preparing for Gender Affirmation Surgery: Ask the Experts
Featured Expert:

Romy Smith, LMSW
Preparing for your gender affirmation surgery can be daunting. To help provide some guidance for those considering gender affirmation procedures, our team from the Johns Hopkins Center for Transgender and Gender Expansive Health (JHCTGEH) answered some questions about what to expect before and after your surgery.
What kind of care should I expect as a transgender individual?
What kind of care should I expect as a transgender individual? Before beginning the process, we recommend reading the World Professional Association for Transgender Health Standards Of Care (SOC). The standards were created by international agreement among health care clinicians and in collaboration with the transgender community. These SOC integrate the latest scientific research on transgender health, as well as the lived experience of the transgender community members. This collaboration is crucial so that doctors can best meet the unique health care needs of transgender and gender-diverse people. It is usually a favorable sign if the hospital you choose for your gender affirmation surgery follows or references these standards in their transgender care practices.
Can I still have children after gender affirmation surgery?
Many transgender individuals choose to undergo fertility preservation before their gender affirmation surgery if having biological children is part of their long-term goals. Discuss all your options, such as sperm banking and egg freezing, with your doctor so that you can create the best plan for future family building. JHCTGEH has fertility specialists on staff to meet with you and develop a plan that meets your goals.
Are there other ways I need to prepare?
It is very important to prepare mentally for your surgery. If you haven’t already done so, talk to people who have undergone gender affirmation surgeries or read first-hand accounts. These conversations and articles may be helpful; however, keep in mind that not everything you read will apply to your situation. If you have questions about whether something applies to your individual care, it is always best to talk to your doctor.
You will also want to think about your recovery plan post-surgery. Do you have friends or family who can help care for you in the days after your surgery? Having a support system is vital to your continued health both right after surgery and long term. Most centers have specific discharge instructions that you will receive after surgery. Ask if you can receive a copy of these instructions in advance so you can familiarize yourself with the information.
An initial intake interview via phone with a clinical specialist.
This is your first point of contact with the clinical team, where you will review your medical history, discuss which procedures you’d like to learn more about, clarify what is required by your insurance company for surgery, and develop a plan for next steps. It will make your phone call more productive if you have these documents ready to discuss with the clinician:
- Medications. Information about which prescriptions and over-the-counter medications you are currently taking.
- Insurance. Call your insurance company and find out if your surgery is a “covered benefit" and what their requirements are for you to have surgery.
- Medical Documents. Have at hand the name, address, and contact information for any clinician you see on a regular basis. This includes your primary care clinician, therapists or psychiatrists, and other health specialist you interact with such as a cardiologist or neurologist.
After the intake interview you will need to submit the following documents:
- Pharmacy records and medical records documenting your hormone therapy, if applicable
- Medical records from your primary physician.
- Surgical readiness referral letters from mental health providers documenting their assessment and evaluation
An appointment with your surgeon.
After your intake, and once you have all of your required documentation submitted you will be scheduled for a surgical consultation. These are in-person visits where you will get to meet the surgeon. typically include: The specialty nurse and social worker will meet with you first to conduct an assessment of your medical health status and readiness for major surgical procedures. Discussion of your long-term gender affirmation goals and assessment of which procedures may be most appropriate to help you in your journey. Specific details about the procedures you and your surgeon identify, including the risks, benefits and what to expect after surgery.
A preoperative anesthesia and medical evaluation.
Two to four weeks before your surgery, you may be asked to complete these evaluations at the hospital, which ensure that you are healthy enough for surgery.
What can I expect after gender affirming surgery?
When you’ve finished the surgical aspects of your gender affirmation, we encourage you to follow up with your primary care physician to make sure that they have the latest information about your health. Your doctor can create a custom plan for long-term care that best fits your needs. Depending on your specific surgery and which organs you continue to have, you may need to follow up with a urologist or gynecologist for routine cancer screening. JHCTGEH has primary care clinicians as well as an OB/GYN and urologists on staff.
Among other changes, you may consider updating your name and identification. This list of resources for transgender and gender diverse individuals can help you in this process.
The Center for Transgender and Gender Expansive Health Team at Johns Hopkins
Embracing diversity and inclusion, the Center for Transgender and Gender Expansive Health provides affirming, objective, person-centered care to improve health and enhance wellness; educates interdisciplinary health care professionals to provide culturally competent, evidence-based care; informs the public on transgender health issues; and advances medical knowledge by conducting biomedical research.
Find a Doctor
Specializing In:
- Gender Affirmation Surgery
- Transgender Health
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
- Center for Transgender and Gender Expansive Health
Find Additional Treatment Centers at:

Request an Appointment

Facial Feminization Surgery (FFS)

Gender Affirmation: Do I Need Surgery?

Gender Affirmation Nonsurgical Services
Related Topics
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Preparation and Procedures Involved in Gender Affirmation Surgeries
If you or a loved one are considering gender affirmation surgery , you are probably wondering what steps you must go through before the surgery can be done. Let's look at what is required to be a candidate for these surgeries, the potential positive effects and side effects of hormonal therapy, and the types of surgeries that are available.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender.
A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery.
The term "transexual" was previously used by the medical community to describe people who undergo gender affirmation surgery. The term is no longer accepted by many members of the trans community as it is often weaponized as a slur. While some trans people do identify as "transexual", it is best to use the term "transgender" to describe members of this community.
Transitioning
Transitioning may involve:
- Social transitioning : going by different pronouns, changing one’s style, adopting a new name, etc., to affirm one’s gender
- Medical transitioning : taking hormones and/or surgically removing or modifying genitals and reproductive organs
Transgender individuals do not need to undergo medical intervention to have valid identities.
Reasons for Undergoing Surgery
Many transgender people experience a marked incongruence between their gender and their assigned sex at birth. The American Psychiatric Association (APA) has identified this as gender dysphoria.
Gender dysphoria is the distress some trans people feel when their appearance does not reflect their gender. Dysphoria can be the cause of poor mental health or trigger mental illness in transgender people.
For these individuals, social transitioning, hormone therapy, and gender confirmation surgery permit their outside appearance to match their true gender.
Steps Required Before Surgery
In addition to a comprehensive understanding of the procedures, hormones, and other risks involved in gender-affirming surgery, there are other steps that must be accomplished before surgery is performed. These steps are one way the medical community and insurance companies limit access to gender affirmative procedures.
Steps may include:
- Mental health evaluation : A mental health evaluation is required to look for any mental health concerns that could influence an individual’s mental state, and to assess a person’s readiness to undergo the physical and emotional stresses of the transition.
- Clear and consistent documentation of gender dysphoria
- A "real life" test : The individual must take on the role of their gender in everyday activities, both socially and professionally (known as “real-life experience” or “real-life test”).
Firstly, not all transgender experience physical body dysphoria. The “real life” test is also very dangerous to execute, as trans people have to make themselves vulnerable in public to be considered for affirmative procedures. When a trans person does not pass (easily identified as their gender), they can be clocked (found out to be transgender), putting them at risk for violence and discrimination.
Requiring trans people to conduct a “real-life” test despite the ongoing violence out transgender people face is extremely dangerous, especially because some transgender people only want surgery to lower their risk of experiencing transphobic violence.
Hormone Therapy & Transitioning
Hormone therapy involves taking progesterone, estrogen, or testosterone. An individual has to have undergone hormone therapy for a year before having gender affirmation surgery.
The purpose of hormone therapy is to change the physical appearance to reflect gender identity.
Effects of Testosterone
When a trans person begins taking testosterone , changes include both a reduction in assigned female sexual characteristics and an increase in assigned male sexual characteristics.
Bodily changes can include:
- Beard and mustache growth
- Deepening of the voice
- Enlargement of the clitoris
- Increased growth of body hair
- Increased muscle mass and strength
- Increase in the number of red blood cells
- Redistribution of fat from the breasts, hips, and thighs to the abdominal area
- Development of acne, similar to male puberty
- Baldness or localized hair loss, especially at the temples and crown of the head
- Atrophy of the uterus and ovaries, resulting in an inability to have children
Behavioral changes include:
- Aggression
- Increased sex drive
Effects of Estrogen
When a trans person begins taking estrogen , changes include both a reduction in assigned male sexual characteristics and an increase in assigned female characteristics.
Changes to the body can include:
- Breast development
- Loss of erection
- Shrinkage of testicles
- Decreased acne
- Decreased facial and body hair
- Decreased muscle mass and strength
- Softer and smoother skin
- Slowing of balding
- Redistribution of fat from abdomen to the hips, thighs, and buttocks
- Decreased sex drive
- Mood swings
When Are the Hormonal Therapy Effects Noticed?
The feminizing effects of estrogen and the masculinizing effects of testosterone may appear after the first couple of doses, although it may be several years before a person is satisfied with their transition. This is especially true for breast development.
Timeline of Surgical Process
Surgery is delayed until at least one year after the start of hormone therapy and at least two years after a mental health evaluation. Once the surgical procedures begin, the amount of time until completion is variable depending on the number of procedures desired, recovery time, and more.
Transfeminine Surgeries
Transfeminine is an umbrella term inclusive of trans women and non-binary trans people who were assigned male at birth.
Most often, surgeries involved in gender affirmation surgery are broken down into those that occur above the belt (top surgery) and those below the belt (bottom surgery). Not everyone undergoes all of these surgeries, but procedures that may be considered for transfeminine individuals are listed below.
Top surgery includes:
- Breast augmentation
- Facial feminization
- Nose surgery: Rhinoplasty may be done to narrow the nose and refine the tip.
- Eyebrows: A brow lift may be done to feminize the curvature and position of the eyebrows.
- Jaw surgery: The jaw bone may be shaved down.
- Chin reduction: Chin reduction may be performed to soften the chin's angles.
- Cheekbones: Cheekbones may be enhanced, often via collagen injections as well as other plastic surgery techniques.
- Lips: A lip lift may be done.
- Alteration to hairline
- Male pattern hair removal
- Reduction of Adam’s apple
- Voice change surgery
Bottom surgery includes:
- Removal of the penis (penectomy) and scrotum (orchiectomy)
- Creation of a vagina and labia
Transmasculine Surgeries
Transmasculine is an umbrella term inclusive of trans men and non-binary trans people who were assigned female at birth.
Surgery for this group involves top surgery and bottom surgery as well.
Top surgery includes :
- Subcutaneous mastectomy/breast reduction surgery.
- Removal of the uterus and ovaries
- Creation of a penis and scrotum either through metoidioplasty and/or phalloplasty
Complications and Side Effects
Surgery is not without potential risks and complications. Estrogen therapy has been associated with an elevated risk of blood clots ( deep vein thrombosis and pulmonary emboli ) for transfeminine people. There is also the potential of increased risk of breast cancer (even without hormones, breast cancer may develop).
Testosterone use in transmasculine people has been associated with an increase in blood pressure, insulin resistance, and lipid abnormalities, though it's not certain exactly what role these changes play in the development of heart disease.
With surgery, there are surgical risks such as bleeding and infection, as well as side effects of anesthesia . Those who are considering these treatments should have a careful discussion with their doctor about potential risks related to hormone therapy as well as the surgeries.
Cost of Gender Confirmation Surgery
Surgery can be prohibitively expensive for many transgender individuals. Costs including counseling, hormones, electrolysis, and operations can amount to well over $100,000. Transfeminine procedures tend to be more expensive than transmasculine ones. Health insurance sometimes covers a portion of the expenses.
Quality of Life After Surgery
Quality of life appears to improve after gender-affirming surgery for all trans people who medically transition. One 2017 study found that surgical satisfaction ranged from 94% to 100%.
Since there are many steps and sometimes uncomfortable surgeries involved, this number supports the benefits of surgery for those who feel it is their best choice.
A Word From Verywell
Gender affirmation surgery is a lengthy process that begins with counseling and a mental health evaluation to determine if a person can be diagnosed with gender dysphoria.
After this is complete, hormonal treatment is begun with testosterone for transmasculine individuals and estrogen for transfeminine people. Some of the physical and behavioral changes associated with hormonal treatment are listed above.
After hormone therapy has been continued for at least one year, a number of surgical procedures may be considered. These are broken down into "top" procedures and "bottom" procedures.
Surgery is costly, but precise estimates are difficult due to many variables. Finding a surgeon who focuses solely on gender confirmation surgery and has performed many of these procedures is a plus. Speaking to a surgeon's past patients can be a helpful way to gain insight on the physician's practices as well.
For those who follow through with these preparation steps, hormone treatment, and surgeries, studies show quality of life appears to improve. Many people who undergo these procedures express satisfaction with their results.
Bizic MR, Jeftovic M, Pusica S, et al. Gender dysphoria: Bioethical aspects of medical treatment . Biomed Res Int . 2018;2018:9652305. doi:10.1155/2018/9652305
American Psychiatric Association. What is gender dysphoria? . 2016.
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender-nonconforming people . 2012.
Tomlins L. Prescribing for transgender patients . Aust Prescr . 2019;42(1): 10–13. doi:10.18773/austprescr.2019.003
T'sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine . Endocr Rev . 2019;40(1):97-117. doi:10.1210/er.2018-00011
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877-884. doi:10.21037/tau.2016.09.04
Seal LJ. A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria . Ann Clin Biochem . 2016;53(Pt 1):10-20. doi:10.1177/0004563215587763
Schechter LS. Gender confirmation surgery: An update for the primary care provider . Transgend Health . 2016;1(1):32-40. doi:10.1089/trgh.2015.0006
Altman K. Facial feminization surgery: current state of the art . Int J Oral Maxillofac Surg . 2012;41(8):885-94. doi:10.1016/j.ijom.2012.04.024
Therattil PJ, Hazim NY, Cohen WA, Keith JD. Esthetic reduction of the thyroid cartilage: A systematic review of chondrolaryngoplasty . JPRAS Open. 2019;22:27-32. doi:10.1016/j.jpra.2019.07.002
Top H, Balta S. Transsexual mastectomy: Selection of appropriate technique according to breast characteristics . Balkan Med J . 2017;34(2):147-155. doi:10.4274/balkanmedj.2016.0093
Chan W, Drummond A, Kelly M. Deep vein thrombosis in a transgender woman . CMAJ . 2017;189(13):E502-E504. doi:10.1503/cmaj.160408
Streed CG, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: A narrative review . Ann Intern Med . 2017;167(4):256-267. doi:10.7326/M17-0577
Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: A review of guidelines and literature . Fed Pract . 2018;35(7):30-37.
Van de grift TC, Elaut E, Cerwenka SC, Cohen-kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming aurgery: A follow-up atudy . J Sex Marital Ther . 2018;44(2):138-148. doi:10.1080/0092623X.2017.1326190
American Society of Plastic Surgeons. Gender confirmation surgeries .
American Psychological Association. Transgender people, gender identity, and gender expression .
Colebunders B, Brondeel S, D'Arpa S, Hoebeke P, Monstrey S. An update on the surgical treatment for transgender patients . Sex Med Rev . 2017 Jan;5(1):103-109. doi:10.1016/j.sxmr.2016.08.001
States That Have Restricted Gender-Affirming Care for Trans Youth
As the issue of trans rights has become more political, states are increasingly banning gender-affirming care for trans minors.
States Restricting Gender-Affirming Care

Sue Ogrocki | AP
Trans-rights activists protest outside the House chamber at the Oklahoma state Capitol on Feb. 6, 2023, in Oklahoma City.
A large majority of transgender adults in the United States – 78% – say living with a gender different from the one assigned to them at birth has made them more satisfied with their lives, according to a survey from The Washington Post and Kaiser Family Foundation .
Among respondents, more than three-quarters had changed their type of clothing, hairstyle or grooming habits to align with their preferred gender, while 31% had used hormone treatments and 16% had undergone gender-affirming surgery or a related surgical treatment to alter their appearance.
But such options are becoming available on a more limited basis, as politicians in multiple states have attempted to restrict trans Americans’ ability to seek gender-affirming medical treatments.
What Is Gender-Affirming Care?
The Human Rights Campaign, a LGBTQ+ advocacy group, defines gender-affirming care as “age-appropriate care that is medically necessary for the well-being of many transgender and non-binary people who experience symptoms of gender dysphoria, or distress that results from having one’s gender identity not match their sex assigned at birth.” The organization notes both the American Medical Association and the American Academy of Pediatrics support “age-appropriate, gender-affirming care for transgender and non-binary people.”
Conservatives often oppose the concept of gender-affirming care – which may or may not include surgery or other interventions – for various reasons, including religious beliefs and concerns about child abuse. “You don’t disfigure 10-, 12-, 13-year-old kids based on gender dysphoria,” Florida Gov. Ron DeSantis, a Republican, said at an August news conference.
Some have expressed concern about a lack of data on the possible long-term consequences of gender-affirming medical treatment for minors. A 2022 Reuters investigation , for example, found “no large-scale studies have tracked people who received gender-related medical care as children to determine how many remained satisfied with their treatment as they aged and how many eventually regretted transitioning.” Others, according to the article, have raised alarms about children who are not appropriately evaluated before receiving gender-affirming medical care.
These States Have Banned Gender-Affirming Care for Minors
Mississippi
North Carolina
North Dakota
South Dakota
West Virginia
Below are the states that have moved to restrict some form of gender-affirming care for minors in 2023 and so far in 2024, based largely on legislation tracking from the Equality Federation, an advocacy accelerator that works with a network of state-based LGBTQ+ organizations.
Some states, such as Arizona and Alabama , passed bans prior to 2023 and are not included on the list.
Dozens of bills are still being considered by lawmakers in other states, according to the federation. And officials elsewhere, including in Florida and Missouri, have bypassed state legislatures altogether.
Signed into law by new Republican Gov. Sarah Huckabee Sanders in March, Arkansas’ law will make health care providers liable for civil action for up to 15 years after a minor turns 18 if they performed a gender transition procedure on that minor – essentially making it easier to file malpractice lawsuits in these situations. On that note, experts say the law acts as a de facto ban on gender-affirming care for children because it makes it nearly impossible for providers to get malpractice insurance, according to the AP . In 2021, state lawmakers passed the nation’s first ban on gender-affirming care for minors. The move was temporarily blocked shortly after, but on June 20, 2023, a federal judge issued a permanent injunction against it, ruling the ban unconstitutional. It marked the first time such a state ban was overturned, but the more recent law signed by Sanders was still set to go into effect.
The state Department of Health’s Board of Medicine announced a new rule in March that prohibits several types of treatment and procedures – such as sex reassignment surgeries and puberty blockers – for treating gender dysphoria in minors. Then, on May 17, DeSantis signed into law a similar gender-affirming care ban from the state legislature , which, in addition to prohibiting procedures from being performed on minors, also grants Florida courts “temporary emergency jurisdiction” over a child if they have been subjected to or “threatened” with sex-reassignment prescriptions or procedures. The law also requires transgender adults to get written consent before undergoing such procedures by using a form adopted by the Board of Medicine and Board of Osteopathic Medicine, according to Reuters. But on June 6, a district court judge in Florida issued a preliminary injunction that temporarily blocked enforcement of some parts of the law on behalf of several young plaintiffs. Months later, the same judge ruled that the parts of the law that apply to transgender adults can still be enforced while it is challenged in court.
Senate Bill 140 was signed into law by Georgia Republican Gov. Brian Kemp in late March. The legislation , pushed forward by the Republican majority in the state’s General Assembly, prohibits “certain surgical procedures for the treatment of gender dysphoria in minors from being performed in hospitals and other licensed healthcare facilities.” There are exceptions, including treatments that are deemed “medically necessary” and situations covering continued treatment for minors undergoing “irreversible hormone replacement therapies” prior to July 1, 2023. A federal judge on Sept. 5 allowed Georgia to resume enforcing the portion of the law banning doctors from starting hormone therapy for transgender minors, weeks after blocking it with a preliminary injunction. The prohibition on surgical procedures was not covered by the legal challenges.
The state’s GOP Gov. Brad Little approved a bill that criminalizes providing gender-affirming care for youth. Signed on April 4, 2023, and set to go into effect in January 2024, the law was intended to make it a felony to provide hormones, puberty blockers or other gender-affirming medical care to minors. But in December 2023, a federal judge issued a temporary injunction blocking the law’s enforcement. Then the U.S. Supreme Court in April 2024 ruled that the state could enforce the ban against everyone except the plaintiffs who challenged it. Even before that ruling, Little in March signed a new law which will prevent transgender people in Idaho from using publicly funded programs to help cover the cost of gender-affirming care. The ban included in the legislation, which is scheduled to go into effect on July 1, 2024, extends to state employees on work health insurance and adults using Medicaid.
Republican Gov. Eric Holcomb signed into law on April 5 a bill banning all gender-affirming care for minors, after previously saying there was “some vagueness to it,” according to the AP. The governor said in a statement that “permanent gender-changing surgeries with lifelong impacts and medically prescribed preparation for such a transition should occur as an adult, not as a minor.” The parts of the law banning puberty blockers and hormone treatments for minors were blocked by a federal judge on June 16, 2023, following a request for a preliminary injunction by the American Civil Liberties Union of Indiana. But a federal appeals court ruling on Feb. 27, 2024, allowed those restrictions to go into effect.
Iowa’s ban , signed into law on March 22, prohibits health care professionals from “knowingly” performing certain medical practices on minors if they are “for the purpose of attempting to alter the appearance of, or affirm the minor’s perception of, the minor's gender or sex, if that appearance or perception is inconsistent with the minor's sex.” Practices covered by the law include hormone therapies and surgical procedures. As with other states’ laws, there are some exceptions, including a “medically verifiable disorder of sex development.”
The state on March 29 joined others in banning gender-affirming medical care for minors when the Republican-led Kentucky General Assembly voted to override Democratic Gov. Andy Beshear’s veto, becoming the first state led by a Democrat to approve such a ban in 2023. The law notes that any health provider who violates the prohibition can have their license or certificate revoked. A federal judge on June 28 temporarily blocked the portion of the law that would have banned transgender youth from accessing puberty blockers and hormone therapy, but that same judge lifted the injunction on July 14 – allowing the restrictions to go into effect. A federal appeals court panel on July 31 allowed the state to continue enforcing the law – and so did another in September.
With a successful override attempt of former Democratic Gov. John Bel Edwards’ veto by the state’s Republican supermajority legislature, Louisiana approved a ban on gender-affirming care for minors on July 18. The law , which went into effect on Jan. 1, 2024, covers procedures such as hormone therapies, puberty blockers and gender-reassignment surgeries. The ban’s ultimate approval came after a Republican lawmaker cast a tie-breaking vote to kill the legislation in May. But it was eventually resurrected and passed before Edwards’ veto. New Gov. Jeff Landry, a Republican, has supported the ban, saying in a post in X in May 2023, “Pediatric sex changes should have no place in our society.”
Mississippi’s law – among the first to be enacted in 2023 – bans any person from knowingly providing or engaging in conduct that aids and abets the performance of gender transition procedures on a minor in the state. The ban also prohibits the use of public funds or tax deductions for such procedures. Republican Gov. Tate Reeves said when he signed the bill into law that “radical activists” are telling children they are “just a surgery away from happiness,” according to the AP .
GOP Gov. Mike Parson on June 7 signed a bill that will restrict gender-affirming health care for minors and some adults in Missouri starting in late August. The law prevents the state’s Medicaid division from covering such treatment for people of any age, and prohibits providers from prescribing puberty-blockers or cross-sex hormones to minors until Aug. 28, 2027, unless they were being treated prior to the bill’s effective date. Missouri initially banned gender-affirming care in April through an emergency regulation from state Attorney General Andrew Bailey that limited treatments for both minors and adults, the latter of which was believed to be a first in the country . But Bailey terminated the rule – which had already been on pause due to a lawsuit – on May 16, citing the state legislature’s imminent ban. A circuit judge on Aug. 25 allowed the law to take effect.
Signed into law on April 28 by Republican Gov. Greg Gianforte, Montana’s ban on gender-affirming care for minors covers both surgical procedures and medications such as puberty blockers and testosterone. As with other state laws, the prohibition has exceptions including for someone “diagnosed with a disorder of sexual development.” Any physician who performs a banned procedure can be also sued in the 25 years following it if the after-effects result in any injury, “including physical, psychological, emotional or physiological harms.” Democratic state Rep. Zooey Zephyr, a transgender woman, was exiled from the Montana House floor after she said her fellow Republican lawmakers would have “blood on their hands” if they passed the bill. The law was set to take effect on Oct. 1, but a state judge issued a preliminary injunction on Sept. 27 that blocked its enforcement, according to the AP.
Republican Gov. Jim Pillen signed into law on May 22, 2023, a bill that limits gender-affirming medical care for minors, which covers people under the age of 19 in Nebraska. The law , which also bans abortions at 12 weeks of pregnancy, includes a ban on surgical procedures and limitations on “prescribed drugs related to gender alteration.” The regulations for hormone therapies – recommended by the state’s chief medical officer, a political appointee – were later approved by Pillen on March 12, 2024, and include a seven-day waiting period to start puberty-blocking medications or hormone treatments and a requirement for transgender patients under 19 to meet several therapy benchmarks. The gender-affirming care portion of the new law went into effect on Oct. 1, 2023.
Looking Back at 2023

The state’s Republican-dominated legislature on Aug. 16 voted to successfully override a veto from Democratic Gov. Roy Cooper and approve a ban on gender-affirming care for minors in North Carolina. The bill’s language covers both transition surgeries and puberty-blocking drugs or cross-sex hormones. The law goes into effect immediately, but as with other state bans that have been approved, there are some exceptions to the prohibition.
Republican Gov. Doug Burgum on April 19 signed a veto-proof bill into law that criminalizes providing gender-affirming medical care to minors. The law , which went into effect immediately as an “emergency measure,” makes performing sex reassignment surgery on a minor a felony, and makes providing gender-affirming medication such as puberty blockers to minors a misdemeanor. Burgum recommended in a statement that “thoughtful debate around these complex medical policies should demonstrate compassion and understanding for all North Dakota youth and their families,” according to the AP.
Republican Gov. Mike DeWine on Jan. 5, 2024, signed an executive order that prohibits young Ohioans from getting gender-affirming surgeries done before they turn 18. The order, which took effect immediately, came just a week after DeWine vetoed a bill from the state legislature that would have instituted a broader restriction on gender-affirming care for minors, including hormone therapies. But on Jan. 24, the state Senate successfully voted to override the governor’s veto, meaning the more wide-reaching ban – which also prohibits transgender girls and women from girls’ and women’s sports teams at both the K-12 and collegiate level – was expected to take effect in 90 days. That was until a judge on April 16 blocked the law by issuing a temporary restraining order.
GOP Gov. Kevin Stitt on May 1 signed into law a ban on gender-affirming care for minors in Oklahoma, saying he was “thrilled” to do so and “protect our kids.” The bill allows for any physician who knowingly provides gender transition procedures to be charged with a felony, but the prosecution must occur before the minor patient turns 45. The law went into effect immediately, but on May 18 the state agreed to not enforce it while opponents sought a temporary court order blocking it. A federal judge in October later declined to stop the law from taking effect.
Signed into law on Feb. 13, House Bill 1080 prohibits South Dakotan health care professionals from administering various types of gender-affirming procedures on minors. If a provider violates the law, the legislation requires a professional or occupational licensing board to revoke any license or certificate held by the provider. GOP Gov. Kristi Noem strongly supported the bill before signing it, according to the AP .
Tennessee’s legislation , which was signed by Gov. Bill Lee in March but was set to go into effect on July 1, bans health care providers from performing or offering to perform a medical procedure on a minor if its purpose is to enable that minor “to identify with, or live as, a purported identity inconsistent with the immutable characteristics of the reproductive system that define the minor as male or female.” It also prohibits such procedures if the purpose is to treat “purported discomfort or distress from a discordance between the minor's sex and asserted identity.” There are exceptions, and the law establishes penalties for providers who violate it. Just days before its July 1 effective date, a federal judge on June 28 temporarily blocked the portion of the law that would have banned transgender youth from accessing puberty blockers and hormone therapy. U.S. District Judge Eli Richardson, however, did not block the law’s ban on surgical procedures. A federal appeals court on July 8 temporarily reversed Richardson’s ruling, meaning the law can take effect at least until the court conducts a full review.
GOP Gov. Greg Abbott on June 2 signed a bill banning gender-affirming care for minors in Texas. The law contains exceptions similar to other states’ efforts at restricting transition care. The Texas Supreme Court on Aug. 31 allowed the law to go into effect on Sept. 1, overruling a state district judge who had issued a temporary injunction against the ban a week prior. The law’s passage was not Texas’ first attempt at limiting gender-affirming care: Abbott in 2022 ordered the investigation of families who were receiving such care, but the order was halted by a judge in the state.
Republican Gov. Spencer Cox signed into law on Jan. 28 the first gender-affirming care ban of the year. The Utah legislature’s Senate Bill 16 restricts health providers from performing “sex characteristic surgical procedures on a minor for the purpose of effectuating a sex change” or hormonal transgender treatment on minors who weren’t diagnosed with gender dysphoria before July 1, 2023. Cox said his approval of the law was an effort at least in part to pause “these permanent and life-altering treatments for new patients until more and better research can help determine the long-term consequences,” the AP reported .
A new law signed by GOP Gov. Jim Justice on March 29 prohibits minors from being prescribed hormone therapy and puberty blockers, or from receiving gender-affirming surgery. The law , which will take effect in January 2024, contains an exception geared toward youth for whom “treatment with pubertal modulating and hormonal therapy is medically necessary to treat the minor’s psychiatric symptoms and limit self-harm, or the possibility of self-harm.” In these cases, the minor must receive consent from their parents or guardians along with two medical providers.
Republican Gov. Mark Gordon on March 22 signed into law a measure that prohibits gender-affirming medical care for transgender minors. The ban , which is set to go into effect on July 1, 2024, covers treatment such as surgeries and puberty-blockers. While he did sign the bill, Gordon added that the legislation means the government is “straying into the personal affairs of families,” according to the AP.
Join the Conversation
Tags: Arkansas , Florida , Georgia , Iowa , Mississippi , South Dakota , Tennessee , Utah , transgender people
Related Articles
Best states.

America 2024

Best States Rankings
- # 2 New Hampshire
- # 3 Nebraska
- # 4 Minnesota
Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 best states in america.
Elliott Davis Jr. May 7, 2024

Why Utah Is the Best State
Elliott Davis Jr. and Julia Haines May 7, 2024

Why Florida Is No. 1 in Education
Tim Smart May 7, 2024

Severe Storms Kill at Least 4 in Houston, Knock Out Power to 850,000 Homes and Businesses
Associated Press May 16, 2024

California's Water Tunnel to Cost $20 Billion. State Officials Say the Benefits Are Worth It

Repeal of a Dead Law to Use Public Funds for Private School Tuition Won't Be on Nebraska's Ballot

Kansas Governor Vetoes a Third Plan for Cutting Taxes. One GOP Leader Calls It 'Spiteful'

Judge Dismisses Lawsuit by Georgia Court Candidate Who Sued to Keep Talking About Abortion

Nevada Supreme Court Denies Appeal of Conservative Activist Seeking to Oust County Election Official

Man Convicted of Killing 4 People at Ex-Girlfriend's Home Near Denver

Treatment - Gender dysphoria
Treatment for gender dysphoria aims to help people live the way they want to, in their preferred gender identity or as non-binary.
What this means will vary from person to person, and is different for children, young people and adults. Waiting times for referral and treatment are currently long.
Treatment for children and young people
If your child may have gender dysphoria, they'll usually be referred to one of the NHS Children and Young People's Gender Services .
Your child or teenager will be seen by a multidisciplinary team including a:
- clinical psychologist
- child psychotherapist
- child and adolescent psychiatrist
- family therapist
- social worker
The team will carry out a detailed assessment, usually over 3 to 6 appointments over a period of several months.
Depending on the results of the assessment, options for children and teenagers include:
- family therapy
- individual child psychotherapy
- parental support or counselling
- group work for young people and their parents
- regular reviews to monitor gender identity development
- referral to a local Children and Young People's Mental Health Service (CYPMHS) for more serious emotional issues
Most treatments offered at this stage are psychological rather than medical. This is because in many cases gender variant behaviour or feelings disappear as children reach puberty.
Hormone therapy in children and young people
Some young people with lasting signs of gender dysphoria who meet strict criteria may be referred to a hormone specialist (consultant endocrinologist). This is in addition to psychological support.
Puberty blockers and gender-affirming hormones
Puberty blockers (gonadotrophin-releasing hormone analogues) are not available to children and young people for gender incongruence or gender dysphoria because there is not enough evidence of safety and clinical effectiveness.
From around the age of 16, young people with a diagnosis of gender incongruence or gender dysphoria who meet various clinical criteria may be given gender-affirming hormones alongside psychosocial and psychological support.
These hormones cause some irreversible changes, such as:
- breast development (caused by taking oestrogen)
- breaking or deepening of the voice (caused by taking testosterone)
Long-term gender-affirming hormone treatment may cause temporary or even permanent infertility.
However, as gender-affirming hormones affect people differently, they should not be considered a reliable form of contraception.
There is some uncertainty about the risks of long-term gender-affirming hormone treatment.
Children, young people and their families are strongly discouraged from getting puberty blockers or gender-affirming hormones from unregulated sources or online providers that are not regulated by UK regulatory bodies.
Transition to adult gender identity services
Young people aged 17 or older may be seen in an adult gender identity clinic or be referred to one from a children and young people's gender service.
By this age, a teenager and the clinic team may be more confident about confirming a diagnosis of gender dysphoria. If desired, steps can be taken to more permanent treatments that fit with the chosen gender identity or as non-binary.
Treatment for adults
Adults who think they may have gender dysphoria should be referred to a gender dysphoria clinic (GDC).
Find an NHS gender dysphoria clinic in England .
GDCs have a multidisciplinary team of healthcare professionals, who offer ongoing assessments, treatments, support and advice, including:
- psychological support, such as counselling
- cross-sex hormone therapy
- speech and language therapy (voice therapy) to help you sound more typical of your gender identity
For some people, support and advice from the clinic are all they need to feel comfortable with their gender identity. Others will need more extensive treatment.
Hormone therapy for adults
The aim of hormone therapy is to make you more comfortable with yourself, both in terms of physical appearance and how you feel. The hormones usually need to be taken for the rest of your life, even if you have gender surgery.
It's important to remember that hormone therapy is only one of the treatments for gender dysphoria. Others include voice therapy and psychological support. The decision to have hormone therapy will be taken after a discussion between you and your clinic team.
In general, people wanting masculinisation usually take testosterone and people after feminisation usually take oestrogen.
Both usually have the additional effect of suppressing the release of "unwanted" hormones from the testes or ovaries.
Whatever hormone therapy is used, it can take several months for hormone therapy to be effective, which can be frustrating.
It's also important to remember what it cannot change, such as your height or how wide or narrow your shoulders are.
The effectiveness of hormone therapy is also limited by factors unique to the individual (such as genetic factors) that cannot be overcome simply by adjusting the dose.
Find out how to save money on prescriptions for hormone therapy medicines with a prescription prepayment certificate .
Risks of hormone therapy
There is some uncertainty about the risks of long-term cross-sex hormone treatment. The clinic will discuss these with you and the importance of regular monitoring blood tests with your GP.
The most common risks or side effects include:
- blood clots
- weight gain
- dyslipidaemia (abnormal levels of fat in the blood)
- elevated liver enzymes
- polycythaemia (high concentration of red blood cells)
- hair loss or balding (androgenic alopecia)
There are other risks if you're taking hormones bought over the internet or from unregulated sources. It's strongly recommended you avoid these.
Long-term cross-sex hormone treatment may also lead, eventually, to infertility, even if treatment is stopped.
The GP can help you with advice about gamete storage. This is the harvesting and storing of eggs or sperm for your future use.
Gamete storage is sometimes available on the NHS. It cannot be provided by the gender dysphoria clinic.
Read more about fertility preservation on the HFEA website.
Surgery for adults
Some people may decide to have surgery to permanently alter body parts associated with their biological sex.
Based on the recommendations of doctors at the gender dysphoria clinic, you will be referred to a surgeon outside the clinic who is an expert in this type of surgery.
In addition to you having socially transitioned to your preferred gender identity for at least a year before a referral is made for gender surgery, it is also advisable to:
- lose weight if you are overweight (BMI of 25 or over)
- have taken cross-sex hormones for some surgical procedures
It's also important that any long-term conditions, such as diabetes or high blood pressure, are well controlled.
Surgery for trans men
Common chest procedures for trans men (trans-masculine people) include:
- removal of both breasts (bilateral mastectomy) and associated chest reconstruction
- nipple repositioning
- dermal implant and tattoo
Gender surgery for trans men includes:
- construction of a penis (phalloplasty or metoidioplasty)
- construction of a scrotum (scrotoplasty) and testicular implants
- a penile implant
Removal of the womb (hysterectomy) and the ovaries and fallopian tubes (salpingo-oophorectomy) may also be considered.
Surgery for trans women
Gender surgery for trans women includes:
- removal of the testes (orchidectomy)
- removal of the penis (penectomy)
- construction of a vagina (vaginoplasty)
- construction of a vulva (vulvoplasty)
- construction of a clitoris (clitoroplasty)
Breast implants for trans women (trans-feminine people) are not routinely available on the NHS.
Facial feminisation surgery and hair transplants are not routinely available on the NHS.
As with all surgical procedures there can be complications. Your surgeon should discuss the risks and limitations of surgery with you before you consent to the procedure.

Life after transition
Whether you've had hormone therapy alone or combined with surgery, the aim is that you no longer have gender dysphoria and feel at ease with your identity.
Your health needs are the same as anyone else's with a few exceptions:
- you'll need lifelong monitoring of your hormone levels by your GP
- you'll still need contraception if you are sexually active and have not yet had any gender surgery
- you'll need to let your optician and dentist know if you're on hormone therapy as this may affect your treatment
- you may not be called for screening tests as you've changed your name on medical records – ask your GP to notify you for cervical and breast screening if you're a trans man with a cervix or breast tissue
- trans-feminine people with breast tissue (and registered with a GP as female) are routinely invited for breast screening from the ages of 50 up to 71
Find out more about screening for trans and non-binary people on GOV.UK.
NHS guidelines for gender dysphoria
NHS England has published what are known as service specifications that describe how clinical and medical care is offered to people with gender dysphoria:
- Non-surgical interventions for adults
- Surgical interventions for adults
- Interim service specification for specialist gender incongruence services for children and young people
Review of gender identity services
NHS England has commissioned an independent review of gender identity services for children and young people. The review will advise on any changes needed to the service specifications for children and young people.
Page last reviewed: 28 May 2020 Next review due: 28 May 2023
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry
Readiness assessments for gender-affirming surgical treatments: A systematic scoping review of historical practices and changing ethical considerations
Travis amengual.
1 Department of Psychiatry and Behavioral Sciences, Northwestern Medicine, Chicago, IL, United States
Kaitlyn Kunstman
R. brett lloyd, aron janssen.
2 The Pritzker Department of Psychiatry and Behavioral Health, Ann & Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL, United States
Annie B. Wescott
3 Galter Health Science Library, Northwestern University, Chicago, IL, United States
Associated Data
The original contributions presented in this study are included in the article/ Supplementary material , further inquiries can be directed to the corresponding author.
Transgender and gender diverse (TGD) are terms that refer to individuals whose gender identity differs from sex assigned at birth. TGD individuals may choose any variety of modifications to their gender expression including, but not limited to changing their name, clothing, or hairstyle, starting hormones, or undergoing surgery. Starting in the 1950s, surgeons and endocrinologists began treating what was then known as transsexualism with cross sex hormones and a variety of surgical procedures collectively known as sex reassignment surgery (SRS). Soon after, Harry Benjamin began work to develop standards of care that could be applied to these patients with some uniformity. These guidelines, published by the World Professional Association for Transgender Health (WPATH), are in their 8th iteration. Through each iteration there has been a requirement that patients requesting gender-affirming hormones (GAH) or gender-affirming surgery (GAS) undergo one or more detailed evaluations by a mental health provider through which they must obtain a “letter of readiness,” placing mental health providers in the role of gatekeeper. WPATH specifies eligibility criteria for gender-affirming treatments and general guidelines for the content of letters, but does not include specific details about what must be included, leading to a lack of uniformity in how mental health providers approach performing evaluations and writing letters. This manuscript aims to review practices related to evaluations and letters of readiness for GAS in adults over time as the standards of care have evolved via a scoping review of the literature. We will place a particular emphasis on changing ethical considerations over time and the evolution of the model of care from gatekeeping to informed consent. To this end, we did an extensive review of the literature. We identified a trend across successive iterations of the guidelines in both reducing stigma against TGD individuals and shift in ethical considerations from “do no harm” to the core principle of patient autonomy. This has helped reduce barriers to care and connect more people who desire it to gender affirming care (GAC), but in these authors’ opinions does not go far enough in reducing barriers.
Introduction
Transgender and gender diverse (TGD) are terms that refer to any individual whose gender identity is different from their sex assigned at birth. Gender identity can be expressed through any combination of name, pronouns, hairstyle, clothing, and social role. Some TGD individuals wish to transition medically by taking gender-affirming hormones (GAH) and/or pursuing gender-affirming surgery (GAS) ( 1 ). 1 The medical community’s comfort level with TGD individuals and, consequently, their willingness to provide a broad range of gender affirming care (GAC) 2 has changed significantly over time alongside an increasing understanding of what it means to be TGD and increasing cultural acceptance of LGBTQI people.
Historically physicians have placed significant barriers in the way of TGD people accessing the care that we now know to be lifesaving. Even today, patients wishing to receive GAC must navigate a system that sometimes requires multiple mental health evaluations for procedures, that is not required of cisgender individuals.
The medical and psychiatric communities have used a variety of terms over time to refer to TGD individuals. The first and second editions of DSM described TGD individuals using terms such as transvestism (TV) and transsexualism (TS), and often conflated gender identity with sexuality, by including them alongside diagnoses such as homosexuality and paraphilias. Both the DSM and the International Classification of Diseases (ICD) have continuously changed diagnostic terminology and criteria involving TGD individuals over time, from Gender Identity Disorder in DSM-IV to Gender Dysphoria in DSM-5 to Gender Incongruence in ICD-11.
In 1979, the Harry Benjamin International Gender Dysphoria Association 3 , renamed the World Profession Association for Transgender Health (WPATH) in 2006, was the first to publish international guidelines for providing GAC to TGD individuals. The WPATH Standards of Care (SOC) are used by many insurance companies and surgeons to determine an individual’s eligibility for GAC. Throughout each iteration, mental health providers are placed in the role of gatekeeper and tasked with conducting mental health evaluations and providing required letters of readiness for TGD individuals who request GAC ( 1 ). As part of this review, we will summarize the available literature examining the practical and ethical changes in conducting mental health readiness assessments and writing the associated letters.
While the WPATH guidelines specify eligibility criteria for GAC and a general guide for what information to include in a letter of readiness, there are no widely agreed upon standardized letter templates or semi-structured interviews, leading to a variety of practices in evaluation and letter writing for GAC ( 2 ). To our knowledge, this is the first scoping review to summarize the available research to date regarding the evolution of the mental health evaluation and process of writing letters of readiness for GAS. By summarizing trends in these evaluations over time, we aim to identify best practices and help further guide mental health professionals working in this field.
The review authors conducted a comprehensive search of the literature in collaboration with a research librarian (ABW) according to PRISMA guidelines. The search was comprised of database-specific controlled vocabulary and keyword terms for (1) mental health and (2) TGD-related surgeries. Searches were conducted on December 2, 2020 in MEDLINE (PubMed), the Cochrane Library Databases (Wiley), PsychINFO (EBSCOhost), CINAHL (EBSCOhost), Scopus (Elsevier), and Dissertations and Theses Global (ProQuest). All databases were searched from inception to present without the use of limits or filters. In total, 8,197 results underwent multi-pass deduplication in a citation management system (EndNote), and 4,411 unique entries were uploaded to an online screening software (Rayyan) for title/abstract screening by two independent reviewers. In total, 303 articles were included for full text screening ( Figure 1 ), however, 69 of those articles were excluded as they were unable to be obtained online or through interlibrary loan. Both review authors conducted a full text screen of the remaining 234 articles. Articles were included in the final review if they specified criteria used for mental health screening/evaluation and/or letter writing for GAS, focused on TGD adults, were written in English, and were peer-reviewed publications. Any discrepancies were discussed between the two review authors TA and KK and a consensus was reached. A total of 86 articles met full inclusion criteria. Full documentation of all searches can be found in the Supplementary material .

PRISMA flow diagram demonstrating article review process.
In total, 86 articles were included for review. Eleven articles were focused on ethical considerations while the remaining 75 articles focused on the mental health evaluation and process of writing letters of readiness for GAS. Version 8 of the SOC was published in September of 2022 during the review process of this manuscript and is also included as a reference and point of discussion.
Prior to the publication of the standards of care
Fourteen articles were identified in the literature search as published prior to the development of the WPATH SOC version 1 in 1979. Prominent themes included classification, categorization, and diagnosis of TS. Few publications described the components of a mental health evaluation, and inclusion and exclusion criteria, for GAS. Many publications focused exclusively on transgender females, with a paucity of literature examining the experiences of transgender males during this timeframe.
Authors emphasized accurate diagnosis of TS, highlighting elements of the psychosocial history including early life cross-dressing, preference for play with the opposite gender toys and friends, and social estrangement around puberty ( 3 ). One author proposed the term gender dysphoria syndrome, which included the following criteria: a sense of inappropriateness in one’s anatomically congruent sex role, that role reversal would lead to improvement in discomfort, homoerotic interest and heterosexual inhibition, an active desire for surgical intervention, and the patient taking on an active role in exploring their interest in sex reassignment ( 4 ). Many authors attempted to differentiate between the “true transsexual” and other diagnoses, including idiopathic TS; idiopathic, essential, or obligatory homosexuality; neuroticism; TV; schizophrenia; and intersex individuals ( 5 , 6 ).
Money argued that the selection criteria for patients requesting GAS include a psychiatric evaluation to obtain collateral information to confirm the accuracy of the interview, work with the family to foster support of the individual, and proper management of any psychiatric comorbidities ( 5 ). Authors began to assemble a list of possible exclusion criteria for receiving GAS such as psychosis, unstable mental health, ambivalence, and secondary gain (e.g., getting out of the military), lack of triggering major life events or crises, lack of sufficient distress in therapy, presence of marital bonds (given the illegality of same-sex marriage during this period), and if natal genitals were used for pleasure ( 3 – 5 , 7 – 13 ).
Others focused the role of the psychiatric evaluation on the social lives and roles of the patient. They believed the evaluation should include exploring the patient’s motivation for change for at least 6–12 months ( 8 ), facilitating realistic expectations of treatment, managing family issues, providing support during social transition and post-operatively ( 13 ), and encouraging GAH and the “real-life test” (RLT). The RLT is a period in which a person must fully live in their affirmed gender identity, “testing” if it is right for them. In 1970, Green recommended that a primary goal of treatment was that, “the male patient must be able to pass in society as a socially acceptable woman in appearance and to conduct the normal affairs of the day without arousing undue suspicion” ( 14 ). Benjamin also noted concern that “too masculine” features may be a contraindication to surgery so as to not make an “acceptable woman” ( 7 ). Some publications recommended at least 1–2 years of a RLT ( 3 , 7 , 11 , 15 ), while others recommended at least 5 years of RLT prior to considering GAS ( 12 ). Emphasis was placed on verifying the accuracy of reported information from family or friends to ensure “authentic” motivation for GAS and rule out ambivalence or secondary gain (e.g., getting out of the military) ( 10 ).
Ell recommended evaluation to ensure the patient has “adequate intelligence” to understand realistic expectations of surgery and attempted to highlight the patient’s autonomy in the decision to undergo GAS. He wrote, “That is your decision [to undergo surgery]. It’s up to you to prove that you are a suitable candidate for surgery. It’s not for me to offer it to you. If you decide to go ahead with your plans to pass in the opposite gender role, you do it on your own responsibility” ( 8 ). Notably, many authors conceptualized gender transition along a binary, with individuals transitioning from one end to the other.
In these earliest publications, one can start to see the beginning framework of modern-day requirements for accessing GAS, including ensuring an accurate diagnosis of gender incongruence; ruling out other possible causes of presentation such as psychosis; ensuring general mental stability; making sure that the patient has undergone at least some time of living in their affirmed gender; and that they are able to understand the consequences of the procedure.
Standards of care version 1 and 2
Changes to the standards of care.
The first two versions of the WPATH SOC were written in 1979 and 1980, respectively and are substantially similar to one another. SOC version three was the first to be published in an academic journal in 1985 and changes from the first two versions were documented within this publication. The first two versions required that all recommendations for GAC be completed by licensed psychologists or psychiatrists. The first version recommended that patients requesting GAH and non-genital GAS, spend 3 and 6 months, respectively, living full time in their affirmed gender. These recommendations were rescinded in subsequent versions ( 16 ). Figure 2 reviews changes to the recommendations for GAC within the WPATH SOC over time.

Changes to the World Professional Association for Transgender Health (WPATH) standards of care around gender affirming medical and surgical treatments over time.
Results review
Five articles published between 1979 and 1980 were included in this review. Again, emphasis was placed on proper diagnosis, classification and consistency of gender identity over time ( 17 , 18 ).
Wise and Meyer explored the concept of a continuum between TV and TS, describing that those who experienced gender dysphoria often requested GAS, displayed evidence of strong cross-dressing desires with arousal, history of cross-gender roles, and absence of manic-depressive or psychotic illnesses ( 19 ). Requirements for GAS at the Johns Hopkins Gender Clinic included at least 2 years of cross-dressing, working in the opposite gender role, and undergoing treatment with GAH and psychotherapy ( 19 ). Bernstein identified factors correlated with negative GAS outcomes including presence of psychosis, drug abuse, frequent suicide attempts, criminality, unstable relationships, and low intelligence level ( 18 ). Lothstein stressed the importance of correct diagnosis, “since life stressors may lead some transvestites to clinically present as transsexuals desiring SRS” ( 20 ). Levine reviewed the diagnostic process employed by Case Western Reserve University Gender Identity Clinic which involved initial interview by a social worker to collect psychometric testing, followed by two independent psychiatric interviews to obtain the developmental gender history, understand treatment goals, and evaluate for underlying co-morbid mental health diagnoses, with a final multidisciplinary conference to integrate the various evaluations and develop a treatment plan ( 21 ).
Standards of care version 3
Version 3 broadened the definition of the clinician thereby broadening the scope of providers who could write recommendation letters for GAC. Whereas prior SOC required letters from licensed psychologists or psychiatrists, version 3 allowed initial evaluations from providers with at least a Master’s degree in behavioral science, and when required, a second evaluation from any licensed provider with at least a doctoral degree. Version 3 recommended that all evaluators demonstrate competence in “gender identity matters” and must know the patient, “in a psychotherapeutic relationship,” for at least 6 months ( 16 ). Version 3 relied on the definition of TS in DSM-III, which specified the sense of discomfort with one’s anatomic sex be “continuous (not limited to a period of stress) for at least 2 years” and be independently verified by a source other than the patient through collateral or through a longitudinal relationship with the mental health provider ( 16 ). Recommendation of GAS specifically required at least 6–12 months of RLT, for non-genital and genital GAS, respectively ( 16 ).”
Nine articles were published during the timeframe that the SOC version 3 were active (1981–1990). Themes in these publications included increasing focus on selection criteria for GAS and emphasis on the RLT, which was used to ensure proper diagnosis of gender dysphoria. Recommendations for the duration of the RLT ranged anywhere between 1 and 3 years ( 22 , 23 ).
Proposed components of the mental health evaluation for GAS included a detailed assessment of the duration, intensity, and stability of the gender dysphoria, identification of underlying psychiatric diagnoses and suicidal ideation, a mental status examination to rule out psychosis, and an assessment of intelligence (e.g., IQ) to comment on the individual’s “capacity and competence” to consent to GAC. The Minnesota Multiphasic Personality Inventory (MMPI), Weschler Adult Intelligence Scale (WAIS), and Lindgren-Pauly Body Image Scale were also used during assessments ( 24 ).
Authors developed more specific inclusion and exclusion criteria for undergoing GAS with inclusion criteria including age 21 or older, not legally married, no pending litigation, evidence of gender dysphoria, completion of 1 year of psychotherapy, between 1 and 2 years RLT with ability to “pass convincingly” and “perform successfully” in the opposite gender role, at least 6 months on GAH (if medically tolerable), reasonably stable mental health (including absence of psychosis, depression, alcoholism and intellectual disability), good financial standing with psychotherapy fees ( 25 ), and a prediction that GAS would improve personal and social functioning ( 26 – 29 ). A 1987 survey of European psychiatrists identified their most common requirements as completion of a RLT of 1–2 years, psychiatric observation, mental stability, no psychosis, and 1 year of GAH ( 27 ).
Standards of care version 4
World Professional Association for Transgender Health SOC version four was published in 1990. Between version three and version four, DSM-III-R was published in 1987. Version four relied on the DSM-III-R diagnostic criteria for TS as opposed to the DSM-III criteria in version three. The DSM-III-R criteria for TS included a “persistent discomfort and sense of inappropriateness about one’s assigned sex,” “persistent preoccupation for at least 2 years with getting rid of one’s primary and secondary sex characteristics and acquiring the sex characteristics of the other sex,” and that the individual had reached puberty ( 30 ). Notable changes from the DSM-III criteria include specifying a time duration for the discomfort (2 years) and designating that individuals must have reached puberty.
Six articles were published between 1990 and 1998 while version four was active. Earlier trends continued including emphasizing proper diagnosis of gender dysphoria ( 31 , 32 ), however, a new trend emerged toward implementing more comprehensive evaluations, with an emphasis on decision making, a key element of informed consent.
Bockting and Coleman, in a move representative of other publications of this era, advocated for a more comprehensive approach to the mental health evaluation and treatment of gender dysphoria. Their treatment model was comprised of five main components: a mental health assessment consisting of psychological testing and clinical interviews with the individual, couple, and/or family; a physical examination; management of comorbid disorders with pharmacotherapy and/or psychotherapy; facilitation of identity formation and sexual identity management through individual and group therapy; and aftercare consisting of individual, couple, and/or family therapy with the option of a gender identity consolidation support group. Psychoeducation was a main thread throughout the treatment model and a variety of treatment “subtasks” such as understanding decision making, sexual functioning and sexual identity exploration, social support, and family of origin intimacy were identified as important. The authors advocated for “a clear separation of gender identity, social sex role, and sexual orientation which allows a wide spectrum of sexual identities and prevents limiting access to GAS to those who conform to a heterosexist paradigm of mental health” ( 33 ).
This process can be compared with the Italian SOC for GAS which recommend a multidisciplinary assessment consisting of a psychosocial evaluation and informed consent discussion around treatment options, procedures, and risks. Requirements included 6 months of psychotherapy prior to initiating GAH, 1 year of a RLT prior to GAS, and provision of a court order approving GAS, which could not be granted any sooner than 2 years after starting the process of gender transition. Follow-up was recommended at 6, 12, and 24 months post-GAS to ensure psychosocial adjustment to the affirmed gender role ( 34 ).
Other authors continued to refine inclusion and exclusion criteria for GAS by surveying the actual practices of health centers. Inclusion criteria included those who had life-long cross gender identification with inability to live in their sex assigned at birth; a 1–2 years RLT (a nearly universal requirement in the survey); and ability to pass “effortlessly and convincingly in society”; completed 1 year of GAH; maintained a stable job; were unmarried or divorced; demonstrated good coping skills and social-emotional stability; had a good support system; and were able to maintain a relationship with a psychotherapist. Exclusion criteria included age under 21 years old, recent death of a parent ( 35 ), unstable gender identity, unstable psychosocial circumstances, unstable psychiatric illness (such as schizophrenia, suicide attempts, substance abuse, intellectual disability, organic brain disorder, AIDS), incompatible marital status, criminal history/activity or physical/medical disability ( 36 ).
The survey indicated some programs were more lenient around considering individuals with bipolar affective disorder, the ability to pass successfully, and issues around family support. Only three clinics used sexual orientation as a factor in decision for GAS, marking a significant change in the literature from prior decades. Overall, the authors found that 74% of the clinics surveyed did not adhere to WPATH SOC, instead adopting more conservative policies ( 36 ).
Standards of care version 5
Published in 1998, version five defined the responsibilities of the mental health professional which included diagnosing the gender disorder, diagnosing and treating co-morbid psychiatric conditions, counseling around GAC, providing psychotherapy, evaluating eligibility and readiness criteria for GAC, and collaborating with medical and surgical colleagues by writing letters of recommendation for GAC ( Figure 3 ). Eligibility and readiness criteria were more explicitly described in this version to refer to the specific objective and subjective criteria, respectively, that the patient must meet before proceeding to the next step of their gender transition. The seven elements to include in a letter of readiness were more explicitly listed within this version as well including: the patient’s identifying characteristics, gender, sexual orientation, any other psychological diagnoses, duration and nature of the treatment with the letter writer, whether the author is part of a gender team, whether eligibility criteria have been met, the patient’s ability to follow the SOC and an offer of collaboration. Version five removes the requirement that patients undertake psychotherapy to be eligible for GAC ( 37 ).

Changes to the ten tasks of the mental health provider within the World Professional Association for Transgender Health (WPATH) standards of care over time.
Five articles were published between 1998 and 2001 while version five was active. Two of these articles were summaries of the SOC ( 37 , 38 ). Themes in these publications included continued attempts to develop comprehensive treatment models for GAS.
Ma reviewed the role of the social worker in a multidisciplinary gender clinic in Hong Kong. Psychosocial assessment for GAS included evaluation of performance in affirmed social roles, adaptation to the affirmed gender role during the 1-year RLT and understanding the patient’s identified gender role and the response to the new gender role culturally and interpersonally within the individual’s support network and family unit. She noted five contraindications to GAS: a history of psychosis, sociopathy, severe depression, organic brain dysfunction or “defective intelligence,” success in parental or marital roles, “successful functioning in heterosexual intercourse,” ability to function in the pretransition gender role, and homosexual or TV history with genital pleasure. She proposed a social work practice model for patients who apply for GAS with categorization of TGD individuals into “better-adjusted” and “poorly-adjusted” with different intervention goals and methods for each. For those who were “better-adjusted,” treatment focused on psychoeducation, building coping tools, and mobilization into a peer counselor role, while treatment goals for those who were “poorly-adjusted” focused on building support and resources ( 39 ).
Damodaran and Kennedy reviewed the assessment and treatment model used by the Monash gender dysphoria clinic in Melbourne, Australia for patients requesting GAS. All referrals for GAS were assessed independently by two psychiatrists to determine proper diagnosis of gender dysphoria, followed by endocrinology and psychology consultation to develop a comprehensive treatment plan. Requirements included RLT of minimum 18 months and GAH ( 40 ).
Miach reviewed the utility of using the Minnesota Multiphasic Personality Inventory-2 (MMPI-2), a revision of the MMPI which was standardized using a more heterogeneous population, in a gender clinic to assess stability of psychopathology prior to GAS, which was only performed on patients aged 21–55 years old. The authors concluded that while the TGD group had a significantly lower level of psychopathology than the control group, they believed that the MMPI-2 was a useful test in assessing readiness for GAC ( 41 ).
Standards of care version 6
Published in 2001, version six of the WPATH SOC did not include significant changes to the 10 tasks of the mental health professional ( Figure 3 ) or in the general recommendations for content of the letters of readiness. An important change in the eligibility criteria for GAH allowed providers to prescribe hormones even if patients had not undergone RLT or psychotherapy if it was for harm reduction purposes (i.e., to prevent patient from buying black market hormones). A notable change in version six separated the eligibility and readiness criteria for top (breast augmentation or mastectomy) and bottom (any gender-affirming surgical alteration of genitalia or reproductive organs) surgery allowing some patients, particularly individuals assigned female at birth (AFAB), to receive a mastectomy without having been on GAH or completing a 12 month RLT ( 42 , 43 ).
Thirteen articles were published between 2001 and 2012. One is a systematic review of evidence for factors that are associated with regret and suicide, and predictive factors of a good psychological and social functioning outcome after GAC. De Cuypere and Vercruysse note that less than one percent of patients regret having GAS or commit suicide, making detection of negative predictive factors in a study nearly impossible. They identified a wide array of positive predictive factors including age at time of request, sex of partner, premorbid social or psychiatric functioning, adequacy of social support system, level of satisfaction with secondary sexual characteristics, and surgical outcomes. Many of these predictive factors were later disproved. They also noted that there were not enough studies to determine whether following the WPATH guidelines was a positive predictive factor. In the end they noted that the evidence for all established evaluation regimens (i.e., RLT, age cut-off, psychotherapy, etc.) was at best indeterminate. They recommended that changes to WPATH criteria should redirect focus from gender identity to psychopathology, differential diagnosis, and psychotherapy for severe personality disorders ( 44 ).
The literature at this time supports two opposing approaches to requests for GAC, those advocating for a set of strictly enforced eligibility and readiness criteria associated with very thorough evaluations and those who advocate for a more flexible approach. Common approaches to the evaluation for GAC include: taking a detailed social history including current relationships, support systems, income, and social functioning; a sexual development history meant to understand when and how the patient began to identify as TGD and how their transition has affected their life; an evaluation of their coping skills, “psychic functions” and general mental well-being; and a focus on assessing the “correct diagnosis” of gender identity disorder ( 44 – 56 ). The use of a multidisciplinary team was also commonly recommended ( 44 , 47 , 48 , 51 , 54 – 56 ).
Those that advocated for a stricter interpretation of the eligibility and readiness criteria emphasized the importance of the RLT ( 45 , 49 , 51 , 53 , 55 , 56 ). One clinic in the UK required a RLT lasting 2 years prior to starting GAH, twice as long as recommended by the SOC ( 49 ). The prevailing view continued to approach gender as a binary phenomenon, rather than as a spectrum of experiences. As a result, treatment recommendations emphasized helping the patient to “pass” in their chosen gender role and did not endorse patients receiving less than the full spectrum of treatment to transition fully from one sex to the other. Several authors indicated that they required some amount of psychotherapy before recommending GAC ( 46 , 47 , 51 , 52 , 55 , 56 ). One author described requirements in Turkey, which unlike the US has the requirements enshrined in law and defines an important role for the courts in granting permission for GAC ( 51 ). In general, these authors supported the gatekeeping role of the mental health provider as a mechanism to prevent cases of regret.
Among groups supporting a flexible interpretation of the SOC, there was a much stronger emphasis on the supportive role of the mental health provider in the gender transition process ( 44 – 46 , 48 , 52 , 53 ). This role included creating a supportive environment for the patient, asking and using the correct pronouns, and helping to guide them through what may be a difficult transition both socially and physically. They emphasized the importance of the psychosocial evaluation including the patient’s connections to others in the TGD community, their social functioning, substance use, and psychiatric history/psychological functioning. While informed consent was mentioned as part of the evaluation, the process was not thoroughly explored and largely focused on patients’ awareness that GAS is an irreversible procedure which removes healthy tissue ( 53 ). One author suggested that a “consumer handbook outlining such rights and responsibilities” related to GAS be made available, but they made no further comment on the informed consent process ( 44 ). There was no further guidance as to the contents of letters of readiness for GAC.
The lack of emphasis on informed consent by both groups of authors mirrors the discussion of informed consent within the SOC, which up through version six, had a relatively narrow definition and role specifically related to risks and benefits of surgery. As far back as version one, the SOC states “hormonal and surgical sex reassignment are procedures which must be requested by, and performed only with the agreement of, the patient having informed consent…[these procedures] may be conducted or administered only after the patient applicant has received full and complete explanations, preferably in writing, in words understood by the patient applicant, of all risks inherent in the requested procedures ( 16 ). “This reflects the dominant concerns of surgeons at the time that they were removing or damaging healthy tissue, which was unethical, and as such wanted to make sure that patients understood the irreversibility of the procedures. It was not until version 7 that there is a change in the discussion of informed consent.
Standards of care version 7
Standards of care version seven was published in 2013. Publication of version seven coincided with the publication of DSM-5, in which the diagnosis required to receive GAC shifted from Gender Identity Disorder to Gender Dysphoria, in an effort to de-pathologize TGD patients. Version seven highlights that these are guidelines meant to be flexible to account for different practices in different places. Compared to version six, a significantly expanded section on the “Tasks of the Mental Health Provider” was added, offering some instructions on what to include in the assessment of the patient for GAS. For the first time the SOC expand on what it means to obtain informed consent and describe a process where the mental health provider is expected to guide a conversation around gender identity and how different treatments and procedures might affect TGD individuals psychologically, socially, and physically. Other recommendations include “at a minimum, assessment of gender identity and gender dysphoria, history and development of gender dysphoric feelings, the impact of stigma attached to gender non-conformity on mental health, and the availability of support from family, friends, and peers.” There is also a change to the recommended content of the letters: switching from “The initial and evolving gender, sexual, and other psychiatric diagnoses” to “Results of the client’s psychosocial assessment, including any diagnoses”, indicating a shift in the focus away from diagnosis toward the psychosocial assessment. Version 7 also adds two new tasks for the mental health provider including “Educate and advocate on behalf of clients within their community (schools, workplaces, other organizations) and assist clients with making changes in identity documents” and “Provide information and referral for peer support”( 2 ).
There were also significant changes to eligibility criteria for GAC. For GAH, version seven eliminates entirely the requirement for a RLT and psychotherapy and adds requirements for “persistent well documented gender dysphoria” and “reasonably well controlled” medical or mental health concerns. Notably, the SOC do not define the meaning of “reasonably well controlled,” leaving providers to interpret this on their own. Version seven delineates separate requirements for top and bottom surgeries. The criteria for both feminizing and masculinizing top surgeries are identical to each other and identical to those laid out for GAH. Version seven explicitly states that GAH is not required prior to top surgery, although GAH is still recommended prior to gender-affirming breast augmentation. Criteria for bottom surgery are more explicitly defined, namely internal (i.e., hysterectomy, orchiectomy) vs. external (i.e., metoidioplasty, phalloplasty, and vaginoplasty). For internal surgeries, criteria are the same as for top surgery with the addition of a required 12 months of GAH. For external surgeries the criteria are the same as for internal, with the addition of required 12 months of living in the patient’s affirmed gender identity ( 2 , 42 ).
Twenty-three articles were published while version 7 of the SOC have been active. Themes include identifying the role of psychometric testing in GAC evaluations, expanding the discussion around informed consent for GAC, and revising the requirements for letter writers.
A systematic review evaluated the accuracy of psychometric tests in those requesting GAC, identifying only two published manuscripts that met their inclusion criteria, both of which were of poor quality; this led them to question the utility of psychometric tests in in TGD patients ( 57 ). Keo-Meir and Fitzgerald provided a detailed narrative review of psychometric and neurocognitive exams in the TGD population and concluded that psychometric testing should not be done unless there is a question about the capacity of the patient to provide informed consent ( 58 ). The only other manuscripts that include a mention of psychological testing describe processes in Iran and China, both of which require extensive psychological testing prior to approval for GAC ( 59 , 60 ). These two manuscripts, in addition to an ethnographic study of the evaluation process in Turkey ( 61 ), are also the only ones that indicate a requirement for psychotherapy prior to approval for treatment. The three international manuscripts described above plus three manuscripts from the US ( 62 – 64 ) are the only ones to include consideration of a RLT, with authors outside the US preferring a long RLT and US authors considering RLT as part of the informed consent process for GAS, and not required at all prior to the initiation of GAH.
Many authors describe the process of informed consent for GAC ( 1 , 58 , 60 , 62 – 76 ). In China, a signature indicating informed consent from the patient’s family is required in addition to that of the patient ( 60 ). Many authors emphasize evaluating for and addressing social determinants of health including housing status, income, transportation, trauma history, etc. ( 1 , 58 , 60 , 67 , 69 – 71 , 75 – 77 ). Deutsch advocated for the psychosocial evaluation being the most important aspect of the evaluation and suggests that one of the letters required for bottom surgery be replaced by a functional assessment (i.e., ADLs/iADLs), which could be repeated as needed or removed entirely for high functioning patients ( 69 ).
Practice patterns and opinions on who should write letters of readiness and how many letters should be required vary widely. Many letters that surgeons receive are cursory, and short and non-personal letters correlate with poor surgical outcomes ( 1 ). Several authors advocate for eliminating the second letter entirely, for at least some procedures, as it is a barrier to care ( 68 , 69 , 74 ). Some support removing the requirement that both letter writers be therapists or psychiatrists, and even suggesting the second letter be written by a urologist ( 72 ) or a social worker who has performed a detailed social assessment ( 69 , 75 ). The evaluation in Turkey requires a report written by an extensive multidisciplinary team and submitted to a court for approval ( 61 ). Surveys of providers indicate that the SOC are not uniformly implemented leading to huge disparities based on the providers knowledge level and personal beliefs ( 77 , 78 ). Additional recommendations include that providers spend significant time discussing the SOC and diagnosis of gender dysphoria with the patients prior to providing a letter to prepare them for the stigma such a diagnosis may confer ( 65 , 66 ), and dropping gender dysphoria entirely in favor the ICD-11 diagnosis of gender incongruence, as it may be less stigmatizing ( 71 ).
The Mount Sinai Gender Clinic describes an integrated multidisciplinary model where a patient will see a primary care doctor, endocrinologist, social worker, psychiatrist, and obtain any necessary lab work in a single visit, significantly reducing barriers to care. The criteria in this model focus on informed consent, the social determinants of health, being physically ready for surgery, and putting measurable goals on psychiatric stability, while deemphasizing the gender dysphoria diagnosis. Their study showed that people who received their evaluation over a 2-year period were more likely to meet their in-house criteria than they were to meet criteria as set forth in WPATH SOC. The Mount Sinai criteria allowed for significantly decreased barriers to care, allowing more people to progress through desired GAC in a timely fashion ( 75 ).
Standards of care version 8
Standards of care version 8, published in September 2022, includes major updates to the guidelines around GAS. This version explicitly highlights the importance of informed decision making, patient autonomy, and harm reduction models of care, as well as emphasizing the flexibility of the guidelines which the authors note can be modified by the healthcare provider in consultation with the TGD individual.
Version 8 lays out the roles of the assessor which are to identify the presence of gender incongruence and any co-existing mental health concerns, provide information on GAC, support the TGD individual in their decision-making, and to assess for capacity to consent to GAC. The authors emphasize the collaborative nature of this decision-making process between the assessor and the TGD individual, as well as recommending TGD care occur in a multidisciplinary team model when possible.
Version 8 recommends that providers who assess TGD individuals for GAC hold at least a Master’s level degree and have sufficient knowledge in diagnosing gender incongruence and distinguishing it from other diagnoses which may present similarly. These changes allow for non-mental health providers to be the main assessors for GAC.
Version 8 recommends reducing the number of evaluations prior to GAS to a single evaluation in an effort to reduce barriers to care for the TGD population. Notably, the authors have removed the recommendations around content of the letter of readiness for GAC. The guidelines note that the complexity of the assessment process may differ from patient to patient, based on the type of GAC requested and the specific characteristics of the patient. Version eight directly states that psychometric testing and psychotherapy are not requirements to pursue GAC. While evaluations should continue to identify co-existing mental health diagnoses, version 8 highlights that the presence of a mental health diagnosis should not prevent access to GAC unless the mental health symptoms directly interfere with capacity to provide informed consent for treatment or interfere with receiving treatment. Version 8 recommends that perioperative matters, such as travel requirements, presence of stable, safe housing, hygiene/healthy living, any activity restrictions, and aftercare optimization, be discussed by the surgeon prior to GAS. In terms of eligibility criteria, the authors recommend a reduced duration of GAH from 12 months (from version 7) to 6 months (in version 8) prior to pursuing GAS involving reproductive organs ( 79 ).
Ethical discussions
A total of eleven articles explored ethical considerations of conducting mental health evaluations and writing letters of readiness for GAS, including a comparison of the ethical principles prioritized within the “gatekeeping” model vs. the informed consent model for GAC and the differential treatment of TGD individuals compared to cisgender individuals seeking similar surgical procedures.
Many authors compare the informed consent model of care for TGD individuals to the WPATH SOC model. In the informed consent model, the role of the health practitioner is to provide TGD patients with information about risks, side effects, benefits, and possible consequences of undergoing GAC, and to obtain informed consent from the patient ( 80 ). Cavanaugh et al. argue that the informed consent model is more patient-centered and elevates the ethical principle of autonomy above non-maleficence, the principle often prioritized in the “gatekeeping” model ( 81 ). They write, “Through a discussion of risks and benefits of possible treatment options with the patient…clinicians work to assist patients in making decisions. This approach recognizes that patients are the only ones who are best positioned, in the context of their lived experience, to assess and judge beneficence (i.e., the potential improvement in their welfare that might be achieved), and it also affords prescribing clinicians a better and fuller sense of how a particular patient balances principles of non-maleficence and beneficence.” Authors note that mental health providers can be particularly helpful in situations where an individual desires additional mental health treatment, which some argue should remain optional, or when an individual’s capacity is in question ( 81 ). Additional ethical considerations include balancing the respect for the dignity of persons, responsible caring, integrity in relationships, and responsibility to society ( 82 ). Other authors argue for a more systematic approach to ethical issues, including consulting the literature and/or experts in the field of TGD mental health for support in making decisions around GAC ( 74 ).
Hale criticizes the WPATH SOC noting that these guidelines create a barrier between patient and mental health provider in establishing trust and a therapeutic relationship, overly pathologize TGD individuals, and unnecessarily impose financial costs to the TGD individual. As a “gatekeeper,” the mental health provider is placed in the position of either granting or denying GAC and must weigh the competing ethical principles of beneficence, non-maleficence, and autonomy. He argues that mental health providers are not surrogate decision makers and that framing requests for GAS as a “phenomenon of incapacity” is “reflective of the overall incapacitating effects of society at large toward the TGD community” ( 83 ). This reflects the broader approach to determining capacity utilized in other medical contexts, namely that patients have capacity until proven otherwise ( 84 ). Additionally, due to the gatekeeping dynamic between patient and clinician, many TGD patients may not mention concerns or fears surrounding GAS out of concern they will be denied services, thereby limiting the quality and utility of the informed consent discussion. Ashley proposes changes to the informed consent model, specifically that the informed consent process should include not only information about whether to go through with a procedure, but how to go through the procedure including relevant information about timeline, side effects, need for perioperative support, and treatment plan ( 85 ). Gruenweld argues for a bottom-up, TGD-led provision of GAC instead of focusing solely on alleviating gender dysphoria through a top-down, medical expert approach via such systems like the WPATH SOC ( 86 ).
MacKinnon et al. conducted an institutional ethnographic study of both TGD individuals undergoing mental health evaluations for GAC and mental health providers to better understand the process of conducting such evaluations ( 87 ). They found that providers cited three concerns with the evaluation: determining the authenticity of an individual’s TGD identity, determining if the individual has the capacity to consent to treatment, and determining the readiness of the individual to undergo treatment. TGD individuals cited concerns around presenting enough distress to be diagnosed with gender dysphoria (a SOC requirement) versus too much distress, and risk being diagnosed with an uncontrolled mental health condition therefore being ineligible for GAC. The authors conclude, “although they are designed to optimize and universalize care… psychosocial readiness assessments actually create a medically risky and arguably unethical situation in which trans people experiencing mental health issues have to decide what is more important – transitioning at the potential expense of care for their mental health or disclosing significant mental health issues at the expense of being rendered not ready to transition (which in turn may produce or exacerbate mental distress)” ( 87 ).
With regards to writing letters of readiness for GAS, authors comment on the differential treatment of TGD compared to cisgender individuals. Bouman argues that requiring two letters for gender-affirming orchiectomy or hysterectomy is unethical given that orchiectomy and hysterectomy for chronic scrotal pain and dysfunctional uterine bleeding, respectively, do not require any mental health evaluation. Requiring a second letter may cause delays in treatment, increase financial costs, and may be invasive to the patient who must undergo two detailed evaluations, while allowing for diffusion of responsibility for the mental health provider ( 88 ).
Changing standards
Starting in the 1950’s with the first successful gender affirming procedure in the US on Christine Jorgenson, TGD people in the US started seeking surgical treatment of what was then called TS. The medical community’s understanding of TGD people, their mental health, and the role of the mental health provider in their medical and surgical transition has progressed and evolved since this time. Prior to the first iteration of what would later be known as WPATH’s SOC, patients were mostly evaluated within a system that viewed gender and sexual minorities as deviants and thereby largely limited access to GAC. We can also see this reflected in the changes to DSM and ICD diagnostic criteria between 1980 and today which demonstrates a trend from pathologizing identity and conflating sexual and gender identity toward pathologizing the distress experienced due to the discordant identity, and finally removing the relevant diagnosis from the chapter of Mental and Behavioral Disorders altogether in the ICD and instead into a new chapter titled “conditions related to sexual health ( 89 ).” These changes have clearly yielded positive benefits for TGD individuals by reducing stigma and improving access to care, but significant problems remain. Requiring TGD people to have a diagnosis at all to obtain care, no matter the terminology used, is pathologizing. The practice of requiring a diagnosis continues to put mental health and other medical providers in the position of gatekeeping, continuing the vestigial historical focus on “confirming” a person’s gender identity, rather than trusting that TGD people understand their identities better than providers do. Version 8 of the SOC put a much heavier emphasis on shared decision making and informed consent, but continue to maintain the requirement of a diagnosis ( 79 ). Many insurance companies and other health care payers require the diagnosis to justify paying for GAC, but providers should continue to advocate for removing such labels as a gatekeeping mechanism for GAC.
With each version of the SOC, guidelines for GAC become more specific, with more explanation of the reasoning behind each recommendation; more flexible requirements, a broadening of the definition of mental health provider, and elimination of the requirement that at least one letter be written by a doctoral level provider. There has been a notable shift in the conceptualization of gender identity, away from a strict gender binary, with individuals transitioning fully from one end to the other, to gender identity and transition as a spectrum of experiences. Over time the SOC became more flexible by removing requirements for psychotherapy, narrowing requirement for the RLT to only those pursuing bottom surgery, eliminating requirements for a mental health evaluation prior to initiating GAH, and eliminating requirements for GAH prior to top surgery. Version 8 of the SOC was even more explicit about removing requirements for psychotherapy and psychometric testing prior to receiving GAC ( 79 ).
Despite these positive changes, those wishing to access GAC still face significant challenges. Access to providers knowledgeable about GAC remains limited, especially in more rural areas, therefore requiring evaluations and letters of readiness for GAC continues to significantly limit access to treatment. By requiring letters of readiness for GAC, adult TGD individuals are not afforded the same level of autonomy present in almost any other medical context, where capacity to provide informed consent is automatically established ( 84 ). The WPATH SOC continue to perpetuate differential treatment of TGD individuals by requiring extensive, and often invasive, evaluations for procedures that their cisgender peers are able to access without such evaluations ( 88 ). The WPATH guidelines apply a one-size-fits-all approach to an extremely heterogeneous community who have varying levels of needs based on a variety of factors including but not limited to age, socioeconomic status, race, natal sex, and geographic location ( 90 ). It should be noted, however, that the version 8 of the SOC does acknowledge that different patients may require evaluations of varying complexity based on the procedure they are requesting as well as a variety of psychosocial factors, although it remains vague about exactly what those different evaluations should entail ( 79 ). We propose that future work be directed toward three primary goals: conducting research to determine the utility of letters of readiness; to better understand factors that impact GAS outcomes; and to develop easily accessible and understandable guides to conducting readiness evaluations and writing letters. These aims will help to further our goals of advocating for this vastly underserved population by further removing barriers to life-saving GAC.
Changing ethics
Early iterations of the SOC were strict, placing the mental health provider within a gatekeeper role, tasked with distinguishing the “true transsexual” that would benefit from GAS from those who would not, which in effect elevated the ethical principal of non-maleficence above autonomy. This created a barrier to forming a therapeutic alliance between the patient and mental health provider as there was little motivation for patients to give any information outside of the expected gender narrative ( 50 , 65 ). Mistrust flowed both ways leading to longer and more involved evaluations then than what is required today, with many providers requiring patients to undergo extensive psychological testing and psychotherapy, provide extensive collateral, and undergo lengthy RLTs, with some focusing on a patient’s ability to “pass” within the desire gender role, before agreeing to write a letter ( 11 , 15 , 19 , 49 , 57 , 58 ).
As understanding around the experiences of TGD individuals has evolved over time, the emphasis has shifted from the reliance on non-maleficence toward elevating patient autonomy as the guiding principle of care. Evaluations within this informed consent model focus much more on the patient’s ability to understand the treatment, its aftercare, and its potential effect on their lives. Informed consent evaluations also shift focus toward other psychosocial factors that will contribute to successful surgical outcomes, for example, housing, transportation, a support system, and treatment of any underlying mental health symptoms. While there is still a lack of consistency in current evaluations and the SOC are enforced unevenly ( 77 ), the use of the informed consent model by some providers has reduced barriers for some patients. Many authors now agree that psychological or neuropsychological testing should not be used when evaluating for surgical readiness unless there is a concern about the patient’s ability to provide informed consent such as in the case of a neurocognitive or developmental disorder ( 58 ). Also important to note here is that while there is a general shift in the focus of the literature from that of gatekeeping toward one of informed consent, neither the informed consent model nor the WPATH SOC more broadly are evenly applied by providers, leading to continued barriers for many patients ( 77 , 78 ).
Within the literature, there is support for further reducing barriers to care by widening the definition of who can conduct evaluations, write letters, or facilitate the informed consent discussion for GAC. Recommending that the physician providing the GAC be the one to conduct the informed consent evaluation would bring GAC practices more in line with practices in place within the broader medical community. It is very rare for mental health providers to be the gatekeepers for medical or surgical procedures, except for transplant surgery, where mental health providers may have a clearer role given the prominence of substance use disorders and the very limited resource of organs. However, even within transplant psychiatry, a negative psychiatric evaluation would not necessarily preclude the patient from receiving the transplant, but instead may be used to guide a treatment plan to improve chances of a successful recovery post-operatively. We then should consider what it means to embrace patient autonomy as our guiding principle, especially with more than 40 years of evidence of the positive effects around GAC behind us. Future guidelines should focus on making sure that TGD individuals are good surgical candidates, not based on their gender identity, but instead on a more holistic understanding of the factors that lead to good and bad gender-affirming surgical outcomes, along the lines of those proposed by Mt. Sinai’s gender clinic for vaginoplasty ( 75 ). Additionally, the physicians providing the GAC should in most cases be the ones to obtain informed consent, while retaining the ability to request a mental health evaluation if specific concerns related to mental health arise. This would both allow mental health providers to adopt a supportive consultant role rather than that of gatekeeper, as well as provide more individualized rather than one-size-fits-all care to patients.
Version 8 of the SOC go a long way toward changing the ethical focus of evaluations toward one of shared decision making and informed consent by removing the requirement of a second letter and the requirement that the letter be written by a mental health provider. This will, in theory, lower barriers to care by allowing other providers (as long as they have at least a master’s degree) to write letters for surgery ( 79 ). In practice, however, this change is likely to only affect a small portion of the patient population. This is because, as noted in the section below in more detail, insurance companies already do not adhere closely to the SOC ( 91 ) and are unlikely to quickly adopt the new guidelines if at all. Further, it is possible that many surgeons will require that the letter of readiness be written by a mental health provider, especially if the patient has any previous mental health problems. While changes to SOC 8 are a step in the direction we propose in this manuscript, it is important to remember that the primary decision makers of who can access GAC in the US are insurance companies with surgeons, primary care providers, and mental health providers as secondary decision makers; this leaves patients with much less real-world autonomy than the SOC state they should have in the process. While insurance companies hold this effective decision-making power in all of US healthcare, it could be at least partially addressed by developing clear, evidence based guidelines for which patients might require a more in-depth evaluation in the first place. Screening out patients that have little or no mental health or social barriers to care would directly reduce those patients’ barriers to receiving GAC, while freeing up mental health and other providers to provide evaluation, resources, and support to those patients who will actually benefit from these services.
Letter writing
There are few published guides for writing letters of readiness for GAC. The WPATH SOC provide vague guidelines as to the information to include within the letter itself, which, in addition to a lack of consistency in implementation of the SOC, lead to a huge variety in current practices around letter writing and limit their usefulness to surgical providers ( 1 ). There is much debate within the literature about how many letters should be required and who should be able to write them. Guidelines from China, Turkey, and Iran recommend much stricter processes requiring input from a wider variety of specialists to comment on a patient’s readiness ( 59 – 61 ). Within the US, the few recent recommendations include having a frank discussion with patients about the gender dysphoria diagnosis and allowing them to have input into the content of the letter itself ( 65 , 66 , 70 , 71 , 75 ). The heterogeneity of current practices around letter writing demonstrates a reality in which many providers do not uniformly operate within the informed consent model, and do not even uniformly adhere to the SOC as written. This heterogeneity in practice by providers also extends to requirements by insurance companies in the US. The lack of clear guidelines about what should go into a letter, especially across different insurance providers, can lead to increased barriers to care due to insurance denials for incorrectly written letters. While direct data examining insurance denials for incorrectly written letters is not available, we can see this indirect effects in the fact that while 90% of insurance providers in the US provide coverage for GAC, only 5–10% of TGD patients had received bottom surgery even though about 50% of TGD patients have reported wanting it ( 91 ). Version 8 of the SOC reduce some of the letter writing requirements as discussed above, but they still do not give clear instructions on exactly how to write a letter of readiness or perform an evaluation ( 79 ). Given the lack of uniformity and limited benefit of such letters to surgical providers, these authors propose that future research be conducted into the need for letters of readiness for GAC, ways to ensure the content of such letters are evidence-based to improve outcomes of GAC, and improve education to providers by creating an easily accessible and free semi-structured interview with letter template.
Limitations
The reviewed articles included opinion manuscripts, published SOC, and proposed models for how to design and operate GAC clinics, however, this narrative review is limited by a lack of peer reviewed clinical trials that assess the evidence for the GAC practices described here. As a result, it is challenging to comment on the effectiveness of various interventions over time.
The WPATH SOC have evolved significantly over time with regards to their treatment of TGD individuals. Review of the literature shows a clear progression of practices from paternalistic gatekeeping toward increasing emphasis on patient autonomy and informed consent. Mental health evaluations, still required by SOC version eight are almost entirely unique as a requirement for GAS, apart from some bariatric and transplant surgeries. Individuals who wish to pursue GAC are required to get approval for treatments that their cisgender peers may pursue without such evaluations. While there may be some benefits from these evaluations in helping to optimize a patient socially, emotionally, and psychologically for GAC, the increased stigma and burden placed on patients by having a blanket requirement for such evaluations leads us to seriously question the readiness evaluation requirements in SOC version 8, despite a reduction in the requirements compared to previous SOC. This burden is made worse by limited access to providers knowledgeable and competent in conducting GAC evaluations, writing letters of readiness, and a lack of consistency in the application and interpretations of the SOC by both providers and insurance companies. Other barriers to care created by multiple letter requirements include the often-prohibitive cost of getting multiple evaluations and the delay in receiving their medical or surgical treatments due to extensive wait times to see a mental health provider. This barrier will in theory be ameliorated by updates to SOC in version 8, but multiple letters are likely to at least be required by insurance companies for some time. Overall, the shift from gate keeping to informed consent has been a net positive for patients by reducing barriers to care and improving patient autonomy, but the mental health evaluation is still an unnecessary barrier for many people. Further research is necessary to develop a standardized evaluation and letter template for providers to access, as well as further study into who can most benefit from an evaluation in the first place.
Data availability statement
Author contributions.
TA and KK contributed to the conception and design of the study under the guidance of RL and AJ, reviewed and analyzed the literature, and wrote the manuscript. AW organized the literature search and wrote the “Methods” section. RL and AJ assisted in review and revision of the completed manuscript. All authors approved of the submitted version.
Abbreviations
1 Gender affirming surgery has historically been referred to as sexual reassignment surgery (SRS).
2 Gender affirming care is an umbrella term referring to any medical care a TGD individual might pursue that affirms their gender identity, including primary care, mental health care, GAH or GAS.
3 The organization will be referred to as WPATH moving forward, even when referring to time periods before the name change.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.1006024/full#supplementary-material
- Reconstructive Procedures
Gender Confirmation Surgeries Transgender-Specific Facial, Top and Bottom Procedures
What surgical options are available to transgender and gender non-conforming patients? Gender confirmation surgeries, also known as gender affirmation surgeries, are performed by a multispecialty team that typically includes board-certified plastic surgeons. The goal is to give transgender individuals the physical appearance and functional abilities of the gender they know themselves to be. Listed below are many of the available procedures for transwomen (MTF) and transmen (FTM) to aid in their journey.
Facial Feminization Surgery
Transfeminine top surgery, transfeminine bottom surgery, facial masculinization surgery, transmasculine top surgery, transmasculine bottom surgery, on the blog.

Facial feminization surgery is a combination of procedures designed to soften the facial features and feminize the face. There are many procedures that are available to feminize the face.
- Facial feminization surgery improves gender dysphoria in trans women Josef Hadeed, MD, FACS
- The impact of COVID-19 on gender dysphoria patients Cristiane Ueno, MD
On The Vlog

Facial feminization surgery is always tailored to the individual, but as ASPS member Justine Lee, MD, PhD, explains there are general characteristics such as hairline, brow bones, cheeks and jawline that many patients note and plastic surgeons plan for.
- Gender Affirmation Top Surgery with Dr. Julie Hansen
Find Your Surgeon
Patient care center, before & after photos.

Video Gallery
3d animations, patient safety.
Florida's transgender affirming care ban is now law. Here's what SB 254 does:

Florida Gov. Ron DeSantis signed a new bill into law Wednesday that restricts gender-affirming care for transgender adults and children .
Critics of the bill, SB 254, refer to it as the Florida “abduction” bill because they claim it allows children to be “legally kidnapped” by disagreeing parents — even if the opposing parent lives across state lines — if the child is subject to or “threatened” with sex-reassignment prescriptions or procedures.
Senator Clay Yarborough, who introduced the bill, said the bill is meant to protect children from “drastic life-altering gender dysphoria therapies and surgeries” that he said are being prescribed for children. He argued that both parents should have a say in whether their child receives gender-affirming care.
Florida's anti-LGBTQ bills: A rundown of Florida bills causing 'massive panic' in transgender, LGBTQ communities
SB 254 lands on DeSantis' desk: Restrictions on transgender health care pass Florida Legislature, head to DeSantis
The Tallahassee Democrat reported that while the legislation was not as wide-reaching as House members wanted it to be, it will still restrict care for both transgender children and adults. Along with the ban for new youth patients, the bill requires that a physician administer gender affirming care to adult patients in person, barring the use of telehealth and other health care workers, like nurse practitioners and physicians' assistants, to begin care. Doctors who violate those sections could face a first-degree misdemeanor.
Gender-affirming care for youth has support from nearly every mainstream medical organization, including the American Academy of Pediatrics, the World Health Organization, the Endocrine Society and the American Psychiatric Association. Politifact has determined that while the state cannot kidnap children, the law can affect custody disputes.
LGBTQ advocacy groups said last week they plan to ask a judge to block the law as part of an ongoing lawsuit against the Board of Medicine ban.
Here’s a breakdown of what’s in the bill:
Florida courts can receive temporary emergency jurisdiction
The bill would grant Florida courts temporary emergency jurisdiction if a child present in the state has been abandoned; it’s deemed necessary if the child, a sibling or the parent of a child is subjected to or “threatened” with mistreatment or abuse; or if the child is subjected to or “threatened” with sex-reassignment prescriptions or procedures.
Parents can apply for a warrant to receive physical custody of a child
Section 2 of the bill allows parents to file a petition seeking enforcement of a child custody determination. If a parent believes that their child is likely to “imminently suffer serious physical harm or removal of the state,” they can file a verified issuance of a warrant to take physical custody of the child.
The section explicitly states that serious physical harm “includes, but is not limited to,” being subjected to sex-reassignment prescriptions and procedures.
Florida diversity, pronoun bills: Florida bills targeting diversity programs and pronouns in schools heads to DeSantis
Censoring drag shows, Pride events: In one day, three bills targeting transgender Floridians pass House
State funds are prohibited from being used for gender-affirming care
Another section of the bill prohibits any “governmental entity” from expending state funds for sex-reassignment prescriptions or procedures.
State is erasing trans options: What can I do if I'm a transgender person living in Florida?
People under 18 can no longer receive gender-affirming care unless they qualify for an exception
Section 5 of the bill prohibits sex-reassignment prescriptions and procedures for patients younger than 18 years old. The Board of Medicine and the Board of Osteopathic Medicine will have 60 days to adopt emergency rules pertaining to standards of practice where a minor could continue to be treated with a prescription consistent with those defined in Florida Statute 456.001.
That transition-related medical care includes puberty blockers, hormones and surgery. Despite claims by DeSantis that medical care amounts to child mutilation, gender-affirmation surgery is generally only recommended for adults. For children, care doesn't begin until the onset of puberty.
Physicians must be in the room with adults receiving gender-affirming care, barring the use of telehealth services
The same section also requires that physicians prescribing, administering a pharmaceutical product or performing a procedure must be, at minimum, physically present in the same room as the patient.
Further restrictions require that only physicians can administer and perform these procedures, barring other health care workers, like nurse practitioners and physicians' assistants, to begin care.
The Tallahassee Democrat reported that at least one Florida clinic that provides gender-affirming care is staffed only by nurse practitioners, leaving care for those patients uncertain under the bill. SPEKTRUM Health serves patients in Central Florida with locations in Orlando and Melbourne.
"Absolutely gutted," CEO Joey Knoll told the Democrat on Thursday. "I've spent the last year trying to raise awareness, get help, and avoid a catastrophe ... that is now imminent."
- Newsletters
- Instapundit
- News & Politics
Appeals Court Finds a Constitutional Right to Gender Reassignment Surgery

The 14th Amendment to the Constitution is truly a magical amendment. It was used to justify attempts to kick Donald Trump off the 2024 ballot. Through the decades, judges who want to play at social engineering have used it frequently to justify questionable law.
It's even been invoked to bypass Congress to raise the debt limit.
Now, the Fourth Circuit Court of Appeals has decided that the amendment's "equal protection" clause means that state Medicaid programs have to cover gender reassignment surgeries.
The appeals court ruled that West Virginia's Medicaid rules on mastectomies are unconstitutional because they violate the "equal protection standard" by not covering mastectomies for gender dysphoria.
Yes, really.
The ruling also includes a North Carolina Medicaid case that the state government won't cover "sex changes." The Fourth Circuit nullified the state ban on gender change surgeries, citing the 14th Amendment’s guarantee of “equal protection of the laws.”
This was a court looking for an excuse to make law.
Judge Roger Gregory who wrote the majority opinion in Kadel v. Folwell (8-6) asked, “Is removing a patient’s breasts to treat cancer the same procedure as removing a patient’s breasts to treat gender dysphoria?” He continued, “There is no case law to ground this discussion nor obvious first principles.”
Wall Street Journal:
He is undeterred, and he concludes that gender dysphoria and transgender status are intertwined, so that such insurance exclusions are nothing more than a proxy for discriminating against gender identity. Then he goes further, finding that West Virginia’s and North Carolina’s policies also unconstitutionally discriminate based on sex. How so? Imagine, Judge Gregory says, an unidentified patient seeking a vaginoplasty. Is this a biological female with a rare birth defect? Is it a transgender patient? “By virtue of the fact that they are seeking a vaginoplasty, we know that they were born without a vagina,” he writes. “But we do not know what sex they were assigned at birth. Without that information, we cannot say whether the Plan or Program will cover the surgery.” Ergo, sex discrimination.
Gregory gets even nuttier.
The differences in coverage "is rooted in a gender stereotype: the assumption that people who have been assigned female at birth are supposed to have breasts, and that people assigned male at birth are not."
It's not a "gender stereotype." It's a biological fact.
"No doubt, the majority of those assigned female at birth have breasts, and the majority of those assigned male at birth do not. But we cannot mistake what is for what must be.”
Not just a "majority." It's a universal biological fact with a tiny number of exceptions.
Treating different things differently doesn’t violate the 14th Amendment’s Equal Protection Clause, and jurists aren’t supposed to ignore the obvious. Writing in dissent at the Fourth Circuit, Judge Julius Richardson struggles to contain his exasperation. “The states,” he says, “have chosen to cover alterations of a person’s breasts or genitalia only if the person experiences physical injury, disease, or (in West Virginia) congenital absence of genitalia.” That determination does not turn on the patient’s sex or gender. “Christopher Fain—one of the plaintiffs below—received coverage for a hysterectomy based on a diagnosis unrelated to Fain’s transgender status,” the dissent says. Likewise, males with gynecomastia qualify for surgery coverage in West Virginia only “if they have physical symptoms, like breast pain,” meaning that isn’t a procedure done merely “to affirm a patient’s biological sex.”
The ruling that opened this can of worms was Bostock v. Clayton County, a case that "held that Title VII of the Civil Rights Act of 1964 protects employees against discrimination because of sexuality or gender identity." Now, as a dissenting judge in Kadel v. Folwell, Judge J. Harvie Wilkinson III is saying that this ruling could be a Roe v Wade ruling for the transgender community.
“This is imperial judging at its least defensible,” he says, “What plaintiffs propose is nothing less than to use the Constitution to establish a nationwide mandate that States pay for emerging gender dysphoria treatments.”
He's not wrong. But getting the ruling past this Supreme Court would be a stretch.

Rick Moran has been writing for PJ Media for 18 years. His work has appeared in dozens of media outlets including the Washington Times and ABC News. He was an editor at American Thinker for 14 years. His own blog is Right Wing Nut House . For media inquiries, please contact [email protected] .
Recommended

Trending on PJ Media Videos
- Trump Attorney Delivers a Perry Mason Moment Against Michael Cohen
- Time for the Bud Light Treatment: NFL Denounces Player for Advocating Traditional Values
- In Michigan, Leftists Have Started Knocking on Doors in the Middle of the Night
- Advocate Newsletter
Search form
By continuing to use our site, you agree to our Private Policy and Terms of Use .
Denying gender-affirming care coverage violates federal law, says appeals court

The 11th Circuit made the ruling in the case of Houston County, Ga., sheriff's deputy Anna Lange.
A federal appeals court has upheld a lower court’s ruling that the Houston County, Ga. , Sheriff’s Office violated antidiscrimination law by denying transition-related health care to a deputy.
Anna Lange sued in 2019 because she had been repeatedly denied insurance coverage for gender-affirming care under the county’s employee health plan. A U.S. district court in Georgia ruled in 2022 that the denial violated federal civil rights law, and Monday a three-judge panel of the U.S. Court of Appeals for the 11 Circuit affirmed that ruling.
It is only the second decision by a federal appellate court affirming that it is unlawful for an employer to discriminate against transgender people in an employee health plan, the first being a recent decision on North Carolina's plan for state employees. It is immediately binding on employers in Georgia, Florida, and Alabama, the states covered by the 11th Circuit, notes a press release from the Transgender Legal Defense and Education Fund, which is representing Lange along with a private law firm.
In his ruling for the 2-1 majority, Judge Charles Wilson cited the Supreme Court’s 2020 decision in Bostock v. Clayton County, in which the high court ruled that job discrimination based on sexual orientation and gender identity constitutes sex discrimination, banned by Title VII of the Civil Rights Act of 1964.
“Applying Bostock ’s reasoning to the facts in this case, we conclude that the district court was correct in finding that the Exclusion violated Title VII,” he wrote. “There is no genuine dispute of fact or law as to whether the Exclusion unlawfully discriminates against Lange and other transgender persons. The Exclusion is a blanket denial of coverage for gender-affirming surgery. Health Plan participants who are transgender are the only participants who would seek gender-affirming surgery. Because transgender persons are the only plan participants who qualify for gender-affirming surgery, the plan denies health care coverage based on transgender status.”
“Today’s victory is a win not just for me, but for all transgender Southerners who deserve equal access to life-saving transition-related care,” Lange said in the TLDEF press release. “I have proudly served my community for decades and it has been deeply painful to have the county fight tooth and nail, redirecting valuable resources toward denying me basic health care — health care that the courts and a jury of my peers have already agreed I deserve. I’m pleased to see that yet another court has deemed those efforts to be unfair and illegal.”
Lange has spent 26 years in law enforcement, 17 of them with Houston County. She came out as trans in 2017.
“Today, the 11th Circuit upheld the well-reasoned ruling of the U.S. District Court that treating Sgt. Anna Lange differently because she is transgender is discriminatory,” TLDEF Co-Interim Legal Director Gabriel Arkles said in the release “Houston County and Sheriff [Cullen] Talton have once again lost in court, after spending some $2 million on lawyers to try to deprive Sgt. Lange of medically necessary care that costs orders of magnitude less solely to discriminate against transgender people.”
“We are pleased that the 11th Circuit Court came to the same conclusion as the lower courts that denying health care coverage to transgender individuals is wrong and illegal, and affirmed the lower court ruling in Sgt. Lange’s favor,” added Wesley Powell, partner at Willkie Farr & Gallagher LLP, who serves as co-counsel.
- North Carolina and West Virginia can't deny trans health care: federal appeals court ›
- SCOTUS Lets Trans Woman's Discrimination Suit in Virginia Go Forward ›
- Anti-Trans Workplace Discrimination Is OK in Texas, Judge Rules ›
- Trans Woman Wins Employment Discrimination Suit Using Civil Rights Act ›
- Biden Calls Transgender Discrimination Civil Rights Issue of Our Time ›
Want more breaking equality news & trending entertainment stories?
Check out our NEW 24/7 streaming service: the Advocate Channel!
Download the Advocate Channel App for your mobile phone and your favorite streaming device!
APPLE STORE - GOOGLE PLAY
ROKU - APPLE TV - FIRE TV - GOOGLE TV
From our Sponsors
Most popular, meet all 37 of the queer women in this season's wnba.
17 Celebs Who Are Out & Proud of Their Trans & Nonbinary Kids
Which state is the queerest these are the states with the most lgbtq+ people, these 27 senate hearing room gay sex jokes are truly exquisite, 10 cheeky and homoerotic photos from bob mizer's nude films, here are the 15 gayest travel destinations in the world: report, black transgender woman starr brown shot to death in memphis. her coworker has confessed to the killing, 13 lgbtq+ british royals in history, these are the 5 states with the smallest percentage of lgbtq+ people, 25 pics of hot, shirtless celebs just to remind us of warmer weather, latest stories, cdc warns of new mpox outbreak, urges vaccination, billie jean king says a massachusetts challenge to a kids book about her is ‘so very sad’, rep. robert garcia calls out peru for classifying trans, intersex & nonbinary people as mentally ill, a brief history of lgbtq+ representation on broadway, this is why the kansas city chiefs need to do something about harrison butker, lauren boebert didn't show up at her teen son's trial — but she's attending donald trump's, biden administration moves to reclassify marijuana, making it legal with prescriptions, adult lgbtq+ role models are instrumental to queer youth's mental health. here's how, molly cook, texas's first out lgbtq+ state senator, is ready to make change (exclusive), how wayne brady found the courage to come out: 'i finally dealt with all those demons', nfl rejects harrison butker's transphobic, sexist graduation speech remarks, harrison butker’s ‘inaccurate, ill-informed and woefully out of step' sexist speech is fact-checked by glaad, maria bello and dominique crenn tie the knot in 'stunning' mexico ceremony, ‘rupaul’s drag race’ winner nymphia wind performs for taiwan’s outgoing president, when laws fail to protect trans people, harmful medicalized norms creep in, dominate vacation prep shopping with the pride store’s summer travel essentials, most black women don't have access to abortion, and they're going to impact the elections, behind the lens & the drag with ‘queen of new york’ director emma fidel (exclusive), biden challenges trump to debate: ' i hear you’re free on wednesdays', from player to broadcaster, meet the queer black soccer pro breaking down the washington spirit, trending stories.

‘Ozempic babies’: Reports of surprise pregnancies raise new questions about weight loss drugs

Cynthia Erivo opens up about how she & Ariana Grande made their epic Met Gala duet come to life

Marvel's 'Agatha' finally has a REAL title — can you guess what it is? (Updated)

10 thirsty pics celebrating DJ Dani Brasil’s Capital Pride debut

All 6 rogue Mississippi cops got long prison sentences in 'Goon Squad' torture of 2 Black men

‘Bridgerton’ stars Nicola Coughlan & Luke Newton on getting OUT of the friendzone

The Talk: Starting your journey with HIV

Walmart to close all of its health care clinics

Hulu's 'Black Twitter' producers on trailer backlash: 'You got to welcome the smoke'

Kaskade says 'lives will change' during his set at EDC Las Vegas 2024

Which 'Cowboy Carter' track would Orville Peck hop on as a feature?

Justice Dept plans to reschedule marijuana as a lower-risk drug

How climate disasters hurt mental health in young people

France becomes world’s first country to enshrine abortion rights in constitution

'Selling the OC's Sean Palmieri doubles down on Tyler & Austin claims

Joe Biden has tied the record for most LGBTQ+ judges confirmed in federal courts

Kristin Chenoweth defends the LGBTQ+ community: 'God loves us all the same'

'Looking' cast: Where are they now?

Out and About with Joel Kim Booster

Mixed reviews for airlines in the latest J.D. Powers passenger rankings
Elon Musk uses burner accounts on X, doesn’t fact-check: report

30 steamy pics of Matteo Lane that got us all hot & bothered

6 of Jonathan Groff's best (and most iconic) gay roles

Why is a mother’s mental health so important? A doctor explains
Exclusive: ‘Queen of the North’ Brooke Lynn Hytes makes her South Beach Palace Bar debut
Most recent.

Charlotte LGBTQ+ travel: Discover pride in North Carolina

Savor vibrant bites as the best traveling queer food festival continues its journey east
Hulu's 'black twitter' producers dish about sub-communities.

Joe Biden launches ‘Out for Biden-Harris’ campaign initiative to engage & woo LGBTQ+ voters (exclusive)

The menthol diaries: Taking back pride from tobacco

Queer comics take center stage in Netflix's 'Outstanding'

16 Republican AGs threaten Maine over protections for trans care and abortion

How I found my freedom in Frida Kahlo's fashion

The Talk: Thriving with HIV
Before AIDS, gay artist Rex drew hot men on the prowl — then he disappeared

Giselle Byrd is taking center stage — and helping others do the same

Girl Power: The cast of ‘Bridgerton’ dishes on why season 3 is the year of the woman

The Talk: Finding balance with HIV

Election season got you down? This crisis line is soothing LGBTQ+ mental health

The Talk: What HIV isn’t
Matt Bomer's shorty shorts and body-ody-ody just broke the internet

Federal judge grants Casa Ruby founder Ruby Corado pre-trial release from D.C. jail

Carrie Underwood solidifies herself as a can't-miss entertainer in Las Vegas

Adidas announces 2024 Pride Collection co-created with Pabllo Vittar

‘Drag Race’ winner Nymphia Wind made herstory again by performing for Taiwan’s president

Discover endless fun at The Pride Store: Games & electronics for all ages

Emma D'Arcy & Olivia Cooke's sizzling chemistry has 'House of the Dragon' fans thirsty AF

Matt Bomer is bursting out of his shorts & we almost poked an eye out
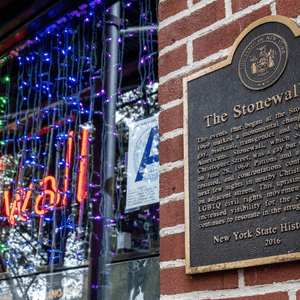
How The Stonewall Gives Back Initiative empowers equality with its impactful legacy
Recommended stories for you.

South Carolina wraps up 2024 legislative session. Here are six key takeaways
T he South Carolina legislature concluded the 2024 session last week. Some widely discussed bills passed through both chambers by the May 9 deadline while several others failed. At least one is in limbo before it can reach Gov. Henry McMaster’s desk.
McMaster signed the permitless “constitutional” firearm carry bill into law on March 7, and the “Help Not Harm” bill banning medical care for transgender youth is headed to the governor’s desk after the House approved Senate amendments to the bill.
Senate Bill 1046, the “judicial reform” measure could become law if a joint conference committee approves it in the coming months, while medical marijuana and an insurance bill related to liquor liability failed to make it that far.
Here are six takeaways from the state General Assembly’s 2024 session.
Permitless “constitutional” firearm carry
McMaster signed H.3594, making permitless firearm carry legal for those 18 and older legally allowed to carry a gun. The new law, dubbed “constitutional carry,” bounced between both chambers of the General Assembly before the finalized version was signed into law.
Days earlier, a joint committee of the House and Senate ultimately decided on the final version of the bill on the morning of March 5. The House approved the committee’s report later that afternoon, and the Senate approved the bill the next day.
The law allows anyone 18 and older, legally eligible to carry a firearm, to do so, openly or concealed, without the need for a permit or registration. It further loosened firearm restrictions after the 2021 Open Carry law allowed a concealed weapons permit (CWP) holder to openly carry handguns.
While CWPs are no longer required under the new permitless carry law, they can still have reciprocity for concealed carry in other states .
With the new law, South Carolina became the 29 th state to legalize permitless carry.
Medical care for transgender youth banned
A House bill outlawing medical care for transgender youth is headed to McMaster to sign into law. On Thursday, the last day of the legislative session, the House agreed to accept the Senate’s amendments to the law.
The bill eliminates puberty-blocking drugs, hormone therapy, and gender-reassignment surgery for those under 18. The bill does make exceptions for people being treated with hormone therapy or puberty blockers that have conditions like precocious puberty or endometriosis.
The Senate's most significant change was an amendment requiring public school principals and vice principals to inform parents if a student reported identifying as a different gender from their assigned sex or using different pronouns.
Opponents of the provision said it was a forced outing and could be dangerous for a child.
Supporters of the bill argued that parents have a right to know if their child is identifying as transgender and said the bill’s goal is to protect children.
If signed into law by the governor, South Carolina would join 25 other states outlawing medical care for transgender youth, according to Human Rights Campaign.
'Judicial reform' bill could become law
The future of S.1046, a bill that would revise the commission that selects judges in the state, remains in limbo as it was referred to a joint conference committee before the legislative session adjourned.
South Carolina and Virginia are the only two states where the legislature appoints judges. Once a judicial merit selection commission screens and approves candidates, they are voted on by the legislature.
However, the two chambers were not able to reconcile their respective versions of the bill, so it is headed to a joint conference committee consisting of three members of the House and three members of the Senate.
Judges appointed by the commission serve six-year terms, except for Supreme Court appointees who serve 10-year terms. The bill looks to establish non-successive terms for commission members. This would, in theory, limit judges from repeatedly appearing before the same lawyer-legislators on the commission.
Currently, the 10-member panel has five Senate appointees and five House appointees. Of those appointees, three are from the Senate and three are from the House. All are practicing attorneys. Each chamber also appoints two members of the general public.
In the conference committee, if two of the three legislators from each body approve a version of the bill, there will still be an opportunity for the Senate and House to agree on the conference report. If they do agree, it will proceed to the governor’s desk.
Rep. Leon Stavrinakis, D-Charleston, is one of the three House members appointed to the committee. Although the legislature adjourned this year’s session “sine die” at 5 p.m. Thursday, Stavrinakis told the Greenville News that if the conference committee comes to an agreed-upon version, both chambers have several opportunities to approve the bill before the end of June.
Insurance bill related to liquor liability fails
House Bill 5066, which would regulate insurance companies and premiums, was one measure that did not reach the conference committee stage. It passed the House in late March but died in committee in the Senate.
Stavrinakis, a co-sponsor of the bill, said it was intended to prevent “blatant” price gouging by insurance companies, especially among bars and restaurants that serve alcohol. He said that some insurance companies charge the businesses “exorbitant” premiums. Some entertainment venues have spoken out against the rising costs of coverage, which has caused some Upstate drinking establishments to shutter.
“The essence of the bill was to create a system that rates risk like we do for automobiles, homes, every other kind of insurance,” Stavrinakis said. “If you think about your automobile policy, people who get in accidents and get tickets pay more money than people that don't. Homeowners claim the same thing, people who make claims pay more money than people who don't.”
Rep. Jason Elliot, R-Greenville, the lead sponsor of the bill, said he hopes the bill can "start over" next legislative session.
"It's a real issue. It's one that's affecting the economic viability of businesses, and it affects jobs," Elliott said.
Medical marijuana killed for a second year in a row
In February, South Carolina’s Senate passed a bill to allow marijuana for medical use 24-19. However, the bill died in a House committee.
Last year, the bill was killed due to a technicality over where the measure must start because it would generate revenue.
Sen. Tom Davis, a Republican representing Beaufort County, has pushed the bill for almost a decade, adamant that it would not be for recreational use.
‘Health czar’ bill squashed
A bill that would have dissolved several departments and combined them into one agency was killed by the South Carolina’s Freedom Caucus in the last minutes of the legislative session.
The bill, introduced in the Senate earlier this year, would have created an Executive Office of Health and Policy by combining the newly created Department of Public Health with five departments.
Last year, South Carolina passed a bill dividing the South Carolina Department of Health and Environment Control (DHEC) into two separate agencies. Effective in July, the two new agencies will be the South Carolina Department of Environmental Services (SCDES) and South Carolina Public Health (DPH.)
The Executive Office of Health Policy bill would have eliminated the Department of Alcohol and Other Drug Abuse Services, Department of Disabilities and Special Needs, Department of Health and Human Services, Department of Mental Health, and Department of Aging and combined them in the Department of Health.
It passed the Senate and made its way out of a House committee but did not pass the House at the last minute. Critics of the bill dubbed the bill the “Health Czar bill.”
“We need medical freedom bills, not more Fauci’s,” said Rep. Adam Morgan, the Republican chairman of the South Carolina Freedom Caucus, on X, formerly Twitter, Thursday night. Morgan, also a candidate for the 4th District Congressional seat, was referring to Anthony Fauci, the nation's former chief medical advisor to the president.
This article originally appeared on Herald-Journal: South Carolina wraps up 2024 legislative session. Here are six key takeaways


IMAGES
VIDEO
COMMENTS
A leading transgender health association has lowered its recommended minimum age for starting gender transition treatment, including sex hormones and surgeries. The World Professional Association for Transgender Health said hormones could be started at age 14, two years earlier than the group's previous advice, and some surgeries done at age ...
The World Professional Association for Transgender Health (WPATH) today announced its updated Standards of Care and Ethical Guidelines for health professionals. Among the updates is a new suggestion to lift the age restriction for youth seeking gender-affirming surgical treatment, in comparison to previous suggestion of surgery at 17 or older.
A total of 17,683 patients, ages 6 through 17, with a prior gender dysphoria diagnosis initiated either puberty blockers or hormones or both during the five-year period. Of these, 4,780 patients ...
Gender surgery can be performed on anyone 18 years old or older. Duke Health, May 12: Duke Health has provided high-quality, compassionate, and evidence-based gender care to both adolescents and ...
Jennings received genital reassignment surgery at 17. Genital reassignment surgery should be reserved for those 18 and older, according to guidelines for the medical care of transgender patients ...
• Gender reassignment surgery is typically only available to those 18 and older in the United States. ... by a team of medical professionals before any physical interventions are considered ...
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
Among other changes, the proposed rules would eliminate the requirement that transgender individuals on Medicaid must wait until the age of 21 to receive surgery. Individuals over the age of 18 and minors — with informed parental consent — would be eligible. Such changes are in line with current thinking among academics and physicians in ...
Kristina Barker for The New York Times. An upsurge in teenagers requesting hormones or surgeries to better align their bodies with their gender identities has ignited a debate among doctors over ...
The last couple of years have seen burgeoning awareness in society of what it means to be transgender as an adult. But now doctors, like those at Ann and Robert H. Lurie Children's Hospital of ...
Gender-altering surgery in teens is less common than hormone treatment, but many centers hesitate to give exact numbers. Guidelines say such surgery generally should be reserved for those aged 18 ...
These patients subsequently lived for a mean of 23 years for transgender men and 27 years for transgender women before beginning gender transition treatments. 19 Our findings were also notable that GAS procedures were relatively uncommon in patients aged 18 years or younger. In our cohort, fewer than 1200 patients in this age group underwent ...
Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics, 134(4), 696-704. ... and gender-affirming genital surgery (as adults). Of note, many of these ...
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
Request an Appointment. 410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Find a Doctor. To help provide guidance for those considering gender affirmation surgery, two experts from the Johns Hopkins Center for Transgender Health answer questions about what to expect before and after your surgery.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender. A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery. The term "transexual" was previously used by the medical community to describe people ...
Overview of current international guidance. Genital surgery for gender incongruence/dysphoria has not been recommended traditionally until the patient achieves the age of majority [1].The 8th version of the WPATH Standards of Care (SoC8) [2] removed however any age-based recommendation, with a shift towards a more individualised assessment of the patient's best interests.
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Republican Gov. Jim Pillen signed into law on May 22, 2023, a bill that limits gender-affirming medical care for minors, which covers people under the age of 19 in Nebraska. The law, which also ...
Treatment Gender dysphoria. Treatment. Treatment for gender dysphoria aims to help people live the way they want to, in their preferred gender identity or as non-binary. What this means will vary from person to person, and is different for children, young people and adults. Waiting times for referral and treatment are currently long.
Breast augmentation is often performed as an outpatient procedure but some patients may require one night stay in the hospital. 1 of 7. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations, mastectomies and vaginoplasty.
Again, emphasis was placed on proper diagnosis, classification and consistency of gender identity over time (17, 18). ... been referred to as sexual reassignment surgery (SRS). 2 Gender affirming care is an umbrella term referring to any ... a barrier to care than WPATH SOC 7 criteria before transgender-specific surgery. Transg Health. (2020) 5 ...
Gender confirmation surgeries, also known as gender affirmation surgeries, are performed by a multispecialty team that typically includes board-certified plastic surgeons. The goal is to give transgender individuals the physical appearance and functional abilities of the gender they know themselves to be. Listed below are many of the available ...
2:53. Florida Gov. Ron DeSantis signed a new bill into law Wednesday that restricts gender-affirming care for transgender adults and children. Critics of the bill, SB 254, refer to it as the ...
Rick Moran has been writing for PJ Media for 18 years. His work has appeared in dozens of media outlets including the Washington Times and ABC News.He was an editor at American Thinker for 14 years.
Trudy Ring. May 14 2024 10:12 AM EST. A federal appeals court has upheld a lower court's ruling that the Houston County, Ga., Sheriff's Office violated antidiscrimination law by denying ...
The bill eliminates puberty-blocking drugs, hormone therapy, and gender-reassignment surgery for those under 18. The bill does make exceptions for people being treated with hormone therapy or ...
China's first publicly recognised transgender dancer has remarried the love of her life whom she was forced to divorce 18 years ago. Jin Xing, 56, from Liaoning province in northeastern China ...
While Lange put off gender reassignment surgery — which would have cost $20,000 — her endocrinologist, two psychologists and a surgeon recommended the procedure.
Roughly 8% of patients were between the ages of 12 to 18, the study found, and genital surgeries made up about 35% of the procedures performed among all age groups. Another study pegged the median cost of phalloplasty at $148,540. The sex reassignment surgical industry is projected by some financial analysts to become a $5 billion industry by ...