Bipolar disorders
Affiliations.
- 1 Mood Disorders Psychopharmacology Unit, University Health Network, Toronto, ON, Canada; Department of Psychiatry, University of Toronto, Toronto, ON, Canada; Department of Pharmacology, University of Toronto, Toronto, ON, Canada; Brain and Cognition Discovery Foundation, Toronto, ON, Canada. Electronic address: [email protected].
- 2 Institute for Mental and Physical Health and Clinical Translation Strategic Research Centre, School of Medicine, Deakin University, Melbourne, VIC, Australia; Mental Health Drug and Alcohol Services, Barwon Health, Geelong, VIC, Australia; Orygen, The National Centre of Excellence in Youth Mental Health, Melbourne, VIC, Australia; Centre for Youth Mental Health, Florey Institute for Neuroscience and Mental Health, Melbourne, VIC, Australia; Department of Psychiatry, The University of Melbourne, Melbourne, VIC, Australia.
- 3 Department of Psychiatry, Adult Division, Kingston General Hospital, Kingston, ON, Canada; Department of Psychiatry, Queen's University School of Medicine, Queen's University, Kingston, ON, Canada; Centre for Neuroscience Studies, Queen's University, Kingston, ON, Canada.
- 4 Department of Psychiatry, University of Toronto, Toronto, ON, Canada; Centre for Youth Bipolar Disorder, Sunnybrook Health Sciences Centre, Toronto, ON, Canada.
- 5 Department of Psychiatry, Faculty of Medicine, University of Antioquia, Medellín, Colombia; Mood Disorders Program, Hospital Universitario San Vicente Fundación, Medellín, Colombia.
- 6 Copenhagen Affective Disorders Research Centre, Psychiatric Center Copenhagen, Rigshospitalet, Copenhagen, Denmark; Department of Psychiatry, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark.
- 7 Discipline of Psychiatry, Northern Clinical School, University of Sydney, Sydney, NSW, Australia; Department of Academic Psychiatry, Northern Sydney Local Health District, Sydney, Australia.
- 8 Department of Psychiatry, University of Toronto, Toronto, ON, Canada.
- 9 Mood Disorders Psychopharmacology Unit, University Health Network, Toronto, ON, Canada; Department of Psychiatry, University of Toronto, Toronto, ON, Canada; Dauten Family Center for Bipolar Treatment Innovation, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA.
- 10 Mood Disorders Psychopharmacology Unit, University Health Network, Toronto, ON, Canada.
- 11 Hospital Clinic, Institute of Neuroscience, University of Barcelona, IDIBAPS, CIBERSAM, Barcelona, Spain.
- 12 Department of Psychiatry, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark; Psychiatric Research Unit, Psychiatric Centre North Zealand, Hillerød, Denmark.
- 13 Department of Psychological Medicine, Institute of Psychiatry, Psychology and Neuroscience, King's College London and South London and Maudsley National Health Service Foundation Trust, Bethlem Royal Hospital, London, UK.
- 14 Mood Disorders Psychopharmacology Unit, University Health Network, Toronto, ON, Canada; Department of Psychiatry, University of Toronto, Toronto, ON, Canada.
- PMID: 33278937
- DOI: 10.1016/S0140-6736(20)31544-0
Bipolar disorders are a complex group of severe and chronic disorders that includes bipolar I disorder, defined by the presence of a syndromal, manic episode, and bipolar II disorder, defined by the presence of a syndromal, hypomanic episode and a major depressive episode. Bipolar disorders substantially reduce psychosocial functioning and are associated with a loss of approximately 10-20 potential years of life. The mortality gap between populations with bipolar disorders and the general population is principally a result of excess deaths from cardiovascular disease and suicide. Bipolar disorder has a high heritability (approximately 70%). Bipolar disorders share genetic risk alleles with other mental and medical disorders. Bipolar I has a closer genetic association with schizophrenia relative to bipolar II, which has a closer genetic association with major depressive disorder. Although the pathogenesis of bipolar disorders is unknown, implicated processes include disturbances in neuronal-glial plasticity, monoaminergic signalling, inflammatory homoeostasis, cellular metabolic pathways, and mitochondrial function. The high prevalence of childhood maltreatment in people with bipolar disorders and the association between childhood maltreatment and a more complex presentation of bipolar disorder (eg, one including suicidality) highlight the role of adverse environmental exposures on the presentation of bipolar disorders. Although mania defines bipolar I disorder, depressive episodes and symptoms dominate the longitudinal course of, and disproportionately account for morbidity and mortality in, bipolar disorders. Lithium is the gold standard mood-stabilising agent for the treatment of people with bipolar disorders, and has antimanic, antidepressant, and anti-suicide effects. Although antipsychotics are effective in treating mania, few antipsychotics have proven to be effective in bipolar depression. Divalproex and carbamazepine are effective in the treatment of acute mania and lamotrigine is effective at treating and preventing bipolar depression. Antidepressants are widely prescribed for bipolar disorders despite a paucity of compelling evidence for their short-term or long-term efficacy. Moreover, antidepressant prescription in bipolar disorder is associated, in many cases, with mood destabilisation, especially during maintenance treatment. Unfortunately, effective pharmacological treatments for bipolar disorders are not universally available, particularly in low-income and middle-income countries. Targeting medical and psychiatric comorbidity, integrating adjunctive psychosocial treatments, and involving caregivers have been shown to improve health outcomes for people with bipolar disorders. The aim of this Seminar, which is intended mainly for primary care physicians, is to provide an overview of diagnostic, pathogenetic, and treatment considerations in bipolar disorders. Towards the foregoing aim, we review and synthesise evidence on the epidemiology, mechanisms, screening, and treatment of bipolar disorders.
Copyright © 2020 Elsevier Ltd. All rights reserved.

Publication types
- Research Support, Non-U.S. Gov't
- Anticonvulsants / therapeutic use
- Antidepressive Agents / therapeutic use
- Antimanic Agents / therapeutic use
- Antipsychotic Agents / therapeutic use
- Bipolar Disorder / classification*
- Bipolar Disorder / drug therapy*
- Bipolar Disorder / genetics
- Bipolar Disorder / psychology
- Carbamazepine / therapeutic use
- Cardiovascular Diseases / complications
- Cardiovascular Diseases / mortality
- Child Abuse / psychology
- Comorbidity
- Depressive Disorder, Major / drug therapy*
- Depressive Disorder, Major / genetics
- Depressive Disorder, Major / psychology
- Environmental Exposure / adverse effects
- Lamotrigine / therapeutic use
- Lithium / therapeutic use
- Mania / drug therapy
- Mania / psychology
- Suicide / psychology
- Suicide Prevention*
- Valproic Acid / therapeutic use
- Young Adult
- Anticonvulsants
- Antidepressive Agents
- Antimanic Agents
- Antipsychotic Agents
- Carbamazepine
- Valproic Acid
- Lamotrigine
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Diagnosis and...
Diagnosis and management of bipolar disorders
- Related content
- Peer review
- Fernando S Goes , associate professor of psychiatry and behavioral sciences 1 2
- 1 Precision Medicine Center of Excellence in Mood Disorders, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
- 2 Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA
- Correspondence to: F S Goes fgoes1{at}jhmi.edu
Bipolar disorders (BDs) are recurrent and sometimes chronic disorders of mood that affect around 2% of the world’s population and encompass a spectrum between severe elevated and excitable mood states (mania) to the dysphoria, low energy, and despondency of depressive episodes. The illness commonly starts in young adults and is a leading cause of disability and premature mortality. The clinical manifestations of bipolar disorder can be markedly varied between and within individuals across their lifespan. Early diagnosis is challenging and misdiagnoses are frequent, potentially resulting in missed early intervention and increasing the risk of iatrogenic harm. Over 15 approved treatments exist for the various phases of bipolar disorder, but outcomes are often suboptimal owing to insufficient efficacy, side effects, or lack of availability. Lithium, the first approved treatment for bipolar disorder, continues to be the most effective drug overall, although full remission is only seen in a subset of patients. Newer atypical antipsychotics are increasingly being found to be effective in the treatment of bipolar depression; however, their long term tolerability and safety are uncertain. For many with bipolar disorder, combination therapy and adjunctive psychotherapy might be necessary to treat symptoms across different phases of illness. Several classes of medications exist for treating bipolar disorder but predicting which medication is likely to be most effective or tolerable is not yet possible. As pathophysiological insights into the causes of bipolar disorders are revealed, a new era of targeted treatments aimed at causal mechanisms, be they pharmacological or psychosocial, will hopefully be developed. For the time being, however, clinical judgment, shared decision making, and empirical follow-up remain essential elements of clinical care. This review provides an overview of the clinical features, diagnostic subtypes, and major treatment modalities available to treat people with bipolar disorder, highlighting recent advances and ongoing therapeutic challenges.
Introduction
Abnormal states of mood, ranging from excesses of despondency, psychic slowness, diminished motivation, and impaired cognitive functioning on the one hand, and exhilaration, heightened energy, and increased cognitive and motoric activity on the other, have been described since antiquity. 1 However, the syndrome in which both these pathological states occur in a single individual was first described in the medical literature in 1854, 2 although its fullest description was made by the German psychiatrist Emil Kraepelin at the turn of the 19th century. 3 Kraepelin emphasized the periodicity of the illness and proposed an underlying trivariate model of mood, thought (cognition), and volition (activity) to account for the classic forms of mania and depression and the various admixed presentations subsequently know as mixed states. 3 These initial descriptions of manic depressive illness encompassed most recurrent mood syndromes with relapsing remitting course, minimal interepisode morbidity, and a wide spectrum of “colorings of mood” that pass “without a sharp boundary” from the “rudiment of more severe disorders…into the domain of personal predisposition.” 3 Although Kraepelin’s clinical description of bipolar disorder (BD) remains the cornerstone of today’s clinical description, more modern conceptions of bipolar disorder have differentiated manic depressive illness from recurrent depression, 4 partly based on differences in family history and the relative specificity of lithium carbonate and mood stabilizing anticonvulsants as anti-manic and prophylactic agents in bipolar disorder. While the boundaries of bipolar disorder remain a matter of controversy, 5 this review will focus on modern clinical conceptions of bipolar disorder, highlighting what is known about its causes, prognosis, and treatments, while also exploring novel areas of inquiry.
Sources and selection criteria
PubMed and Embase were searched for articles published from January 2000 to February 2023 using the search terms “bipolar disorder”, “bipolar type I”, “bipolar type II”, and “bipolar spectrum”, each with an additional search term related to each major section of the review article (“definition”, “diagnosis”, “nosology”, “prevalence”, “epidemiology”, “comorbid”, “precursor”, “prodrome”, “treatment”, “screening”, “disparity/ies”, “outcome”, “course”, “genetics”, “imaging”, “treatment”, “pharmacotherapy”, “psychotherapy”, “neurostimulation”, “convulsive therapy”, “transmagnetic”, “direct current stimulation”, “suicide/suicidal”, and “precision”). Searches were prioritized for systematic reviews and meta-analyses, followed by randomized controlled trials. For topics where randomized trials were not relevant, searches also included narrative reviews and key observational studies. Case reports and small observations studies or randomized controlled trials of fewer than 50 patients were excluded.
Modern definitions of bipolar disorder
In the 1970s, the International Classification of Diseases and the Diagnostic and Statistical Manual of Mental Disorders reflected the prototypes of mania initially described by Kraepelin, following the “neo-Kraepelinian” model in psychiatric nosology. To meet the primary requirement for a manic episode, an individual must experience elevated or excessively irritable mood for at least a week, accompanied by at least three other typical syndromic features of mania, such as increased activity, increased speed of thoughts, rapid speech, changes in esteem, decreased need for sleep, or excessive engagement in impulsive or pleasurable activities. Psychotic symptoms and admission to hospital can be part of the diagnostic picture but are not essential to the diagnosis. In 1994, Diagnostic and Statistical Manual of Mental Disorders , fourth edition (DSM-IV) carved out bipolar disorder type II (BD-II) as a separate diagnosis comprising milder presentations of mania called hypomania. The diagnostic criteria for BD-II are similar to those for bipolar disorder type I (BD-I), except for a shorter minimal duration of symptoms (four days) and the lack of need for significant role impairment during hypomania, which might be associated with enhanced functioning in some individuals. While the duration criteria for hypomania remain controversial, BD-II has been widely accepted and shown to be as common as (if not more common than) BD-I. 6 The ICD-11 (international classification of diseases, 11th revision) included BD-II as a diagnostic category in 2019, allowing greater flexibility in its requirement of hypomania needing to last several days.
The other significant difference between the two major diagnostic systems has been their consideration of mixed symptoms. Mixed states, initially described by Kraepelin as many potential concurrent combinations of manic and depressive symptoms, were more strictly defined by DSM as a week or more with full syndromic criteria for both manic and depressive episodes. In DSM-5, this highly restrictive criterion was changed to encompass a broader conception of subsyndromal mixed symptoms (consisting of at least three contrapolar symptoms) in either manic, hypomanic, or depressive episodes. In ICD-11, mixed symptoms are still considered to be an episode, with the requirement of several prominent symptoms of the countervailing mood state, a less stringent requirement that more closely aligns with Kraepelin's broader conception of mixed states. 7
Epidemiology
Using DSM-IV criteria, the National Comorbidity Study replication 6 found similar lifetime prevalence rates for BD-I (1.0%) and BD-II (1.1%) among men and women. Subthreshold symptoms of hypomania (bipolar spectrum disorder) were more common, with prevalence rate estimates of 2.4%. 6 Incidence rates, which largely focus on BD-I, have been estimated at approximately 6.1 per 100 000 person years (95% confidence interval 4.7 to 8.1). 8 Estimates of the incidence and lifetime prevalence of bipolar disorder show moderate variations according to the method of diagnosis (performed by lay interviewers in a research context v clinically trained interviews) and the racial, ethnic, and demographic context. 9 Higher income, westernized countries have slightly higher rates of bipolar disorder, 10 which might reflect a combination of westernized centricity in the specific idioms used to understand and elicit symptoms, as well as a greater knowledge, acceptance, and conceptualization of emotional symptoms as psychiatric disorders.
Causes of bipolar disorder
Like other common psychiatric disorders, bipolar disorder is likely caused by a complex interplay of multiple factors, both at the population level and within individuals, 11 which can be best conceptualized at various levels of analysis, including genetics, brain networks, psychological functioning, social support, and other biological and environmental factors. Because knowledge about the causes of bipolar disorder remains in its infancy, for pragmatic purposes, most research has followed a reductionistic model that will ultimately need to be synthesized for a more coherent view of the pathophysiology that underlies the condition.
Insights from genetics
From its earliest descriptions, bipolar disorder has been observed to run in families. Indeed, family history is the strongest individual risk factor for developing the disorder, with first degree relatives having an approximately eightfold higher risk of developing bipolar disorder compared with the baseline population rates of ~1%. 12 While family studies cannot separate the effects of genetics from behavioral or cultural transmission, twin and adoption studies have been used to confirm that the majority of the familial risk is genetic in origin, with heritability estimates of approximately 60-80%. 13 14 There have been fewer studies of BD-II, but its heritability has been found to be smaller (~46%) 15 and closer to that of more common disorders such as major depressive disorder or generalized anxiety. 15 16 Nevertheless, significant heritability does not necessarily imply the presence of genes of large effect, since the genetic risk for bipolar disorder appears likely to be spread across many common variants of small effect sizes. 16 17 Ongoing studies of rare variations have found preliminary evidence for variants of slightly higher effect sizes, with initial evidence of convergence with common variations in genes associated with the synapse and the postsynaptic density. 18 19
While the likelihood that the testing of single variants or genes will be useful for diagnostic purposes is low, analyses known as polygenic risk studies can sum across all the risk loci and have some ability to discriminate cases from controls, albeit at the group level rather than the individual level. 20 These polygenic risk scores can also be used to identify shared genetic risk factors across other medical and psychiatric disorders. Bipolar disorder has strong evidence for common variant based coheritability with schizophrenia (genetic correlation (r g ) 0.69) and major depressive disorder (r g 0.48). BD-I has stronger coheritability with schizophrenia compared with BD-II, which is more strongly genetically correlated with major depressive disorder (r g 0.66). 16 Lower coheritability was observed with attention deficit hyperactivity disorder (r g 0.21), anorexia nervosa (0.20), and autism spectrum disorder (r g 0.21). 16 These correlations provide evidence for shared genetic risk factors between bipolar disorder and other major psychiatric syndromes, a pattern also corroborated by recent nationwide registry based family studies. 12 14 Nevertheless, despite their potential usefulness, polygenic risk scores must currently be interpreted with caution given their lack of populational representation and lingering concerns of residual confounds such as gene-environment correlations. 21
Insights from neuroimaging
Similarly to the early genetic studies, small initial studies had limited replication, leading to the formation of large worldwide consortiums such as ENIGMA (enhancing neuroimaging genetics through meta-analysis) which led to substantially larger sample sizes and improved reproducibility. In its volumetric analyses of subcortical structures from MRI (magnetic resonance imaging) of patients with bipolar disorder, the ENIGMA consortium found modest decreases in the volume of the thalamus (Cohen’s d −0.15), the hippocampus (−0.23), and the amygdala (−0.11), with an increased volume seen only in the lateral ventricles (+0.26). 22 Meta-analyses of cortical regions similarly found small reductions in cortical thickness broadly across the parietal, temporal, and frontal cortices (Cohen’s d −0.11 to −0.29) but no changes in cortical surface area. 23 In more recent meta-analyses of white matter tracts using diffuse tension imaging, widespread but modest decreases in white matter integrity were found throughout the brain in bipolar disorder, most notably in the corpus callosum and bilateral cinguli (Cohen’s d −0.39 to −0.46). 24 While these findings are likely to be highly replicable, they do not, as yet, have clinical application. This is because they reflect differences at a group level rather than an individual level, 25 and because many of these patterns are also seen across other psychiatric disorders 26 and could be either shared risk factors or the effects of confounding factors such as medical comorbidities, medications, co-occurring substance misuse, or the consequences (rather than causes) of living with mental illness. 27 Efforts to collate and meta-analyze large samples utilizing longitudinal designs 28 task based, resting state functional MRI measurents, 29 as well as other measures of molecular imaging (magnetic resonance spectroscopy and positron emission tomography) are ongoing but not as yet synthesized in large scale meta-analyses.
Environmental risk factors
Because of the difficulty in measuring and studying the relevant and often common environmental risk factors for a complex illness like bipolar disorder, there has been less research on how environmental risk factors could cause or modify bipolar disorder. Evidence for intrauterine risk factors is mixed and less compelling than such evidence in disorders like schizophrenia. 30 Preliminary evidence suggests that prominent seasonal changes in solar radiation, potentially through its effects on circadian rhythm, can be associated with an earlier onset of bipolar disorder 31 and a higher likelihood of experiencing a depressive episode at onset. 31 However, the major focus of environmental studies in bipolar disorder has been on traumatic and stressful life events in early childhood 32 and in adulthood. 33 The effects of such adverse events are complex, but on a broad level have been associated with earlier onset of bipolar disorder, a worse illness course, greater prevalence of psychotic symptoms, 34 substance misuse and psychiatric comorbidities, and a higher risk of suicide attempts. 32 35 Perhaps uniquely in bipolar disorder, evidence also indicates that positive life events associated with goal attainment can also increase the risk of developing elevated states. 36
Comorbidity
Bipolar disorder rarely manifests in isolation, with comorbidity rates indicating elevated lifetime risk of several co-occurring symptoms and comorbid disorders, particularly anxiety, attentional disorders, substance misuse disorders, and personality disorders. 37 38 The causes of such comorbidity can be varied and complex: they could reflect a mixed presentation artifactually separated by current diagnostic criteria; they might also reflect independent illnesses; or they might represent the downstream effects of one disorder increasing the risk of developing another disorder. 39 Anxiety disorders tend to occur before the frank onset of manic or hypomanic symptoms, suggesting that they could in part reflect prodromal symptoms that manifest early in the lifespan. 37 Similarly, subthreshold and syndromic symptoms of attention deficit/hyperactivity disorder are also observed across the lifespan of people with bipolar disorder, but particularly in early onset bipolar disorder. 40 On the other hand, alcohol and substance misuse disorders occur more evenly before and after the onset of bipolar disorder, consistent with a more bidirectional causal association. 41
The association between bipolar disorder and comorbid personality disorders is similarly complex. Milder manifestations of persistent mood instability (cyclothymia) or low mood (dysthymia) have previously been considered to be temperamental variants of bipolar disorder, 42 but are now classified as related but separate disorders. In people with persistent emotional dysregulation, making the diagnosis of bipolar disorder can be particularly challenging, 43 since the boundaries between longstanding mood instability and phasic changes in mood state can be difficult to distinguish. While symptom overlap can lead to artificially inflated prevalence rates of personality disorders in bipolar disorder, 44 the elevated rates of most personality disorders in bipolar disorder, particularly those related to emotional instability, are likely reflective of an important clinical phenomenon that is understudied, particularly with regard to treatment implications. 45 In general, people with comorbidities tend to have greater symptom burden and functional impairment and have lower response rates to treatment. 46 47 Data on approaches to treat specific comorbid disorders in bipolar disorder are limited, 48 49 and clinicians are often left to rely on their clinical judgment. The most parsimonious approach is to treat primary illness as fully as possible before considering additional treatment options for remaining comorbid symptoms. For certain comorbidities, such as anxiety symptoms and disorders of attention, first line pharmacological treatment—namely, antidepressants and stimulants, should be used with caution, since they might increase the long term risks of mood switching or overall mood instability. 50 51
Like other major mental illnesses, bipolar disorder is also associated with an increased prevalence of common medical disorders such as obesity, hyperlipidemia, coronary artery disease, chronic obstructive pulmonary disease, and thyroid dysfunction. 52 These have been attributed to increase risk factors such as physical inactivity, poor nutrition, smoking, and increased use of addictive substances, 53 but some could also be consequences of specific treatments, such as the atypical antipsychotics and mood stabilizers. 54 Along with poor access to care, this medical burden likely accounts for much of the increased standardized mortality (approximately 2.6 times higher) in people with bipolar disorder, 55 highlighting the need to utilize treatments with better long term side effect profiles, and the need for better integration with medical care.
Precursors and prodromes: who develops bipolar disorder?
While more widespread screening and better accessibility to mental health providers should in principle shorten the time to diagnosis and treatment, early manifestation of symptoms in those who ultimately go on to be diagnosed with bipolar disorder is generally non-specific. 56 In particular, high risk offspring studies of adolescents with a parent with bipolar disorder have found symptoms of anxiety and attentional/disruptive disorders to be frequent in early adolescence, followed by higher rates of depression and sleep disturbance in later teenage years. 56 57 Subthreshold symptoms of mania, such as prolonged increases in energy, elated mood, racing thoughts, and mood lability are also more commonly found in children with prodromal symptoms (meta-analytic prevalence estimates ranging from 30-50%). 58 59 Still, when considered individually, none of these symptoms or disorders are sensitive or specific enough to accurately identify individuals who will transition to bipolar disorder. Ongoing approaches to consider these clinical factors together to improve accuracy have a promising but modest ability to identify people who will develop bipolar disorder, 60 emphasizing the need for further studies before implementation.
Screening for bipolar disorder
Manic episodes can vary from easily identifiable prototypical presentations to milder or less typical symptoms that can be challenging to diagnose. Ideally, a full diagnostic evaluation with access to close informants is performed on patients presenting to clinical care; however, evaluations can be hurried in routine clinical care, and the ability to recall previous episodes might be limited. In this context, the use of screening scales can be a helpful addition to clinical care, although screening scales must be regarded as an impetus for a confirmatory clinical interview rather than a diagnostic instrument by themselves. The two most widely used and openly available screening scales are the mood disorders questionnaire (based on the DSM-IV criteria for hypomania) 61 and the hypomania check list (HCL-32), 62 that represent a broader overview of symptoms proposed to be part of a broader bipolar spectrum.
Racial/ethnic disparities
Although community surveys using structured or semi-structured diagnostic instruments, have provided little evidence for variation across ethnic groups, 63 64 observational studies based on clinical diagnoses in healthcare settings have found a disproportionately higher rate of diagnosis of schizophrenia relative to bipolar disorder in black people. 65 Consistent with similar disparities seen across medicine, these differences in clinical diagnoses are likely influenced by a complex mix of varying clinical presentations, differing rates of comorbid conditions, poorer access to care, greater social and economic burden, as well as the potential effect of subtle biases of healthcare professionals. 65 While further research is necessary to identify driving factors responsible for diagnostic disparities, clinicians should be wary of making a rudimentary diagnosis in patients from marginalized backgrounds, ensuring comprehensive data gathering and a careful diagnostic formulation that incorporates shared decision making between patient and provider.
Bipolar disorder is a recurrent illness, but its longitudinal course is heterogeneous and difficult to predict. 46 66 The few available long term studies of BD-I and BD-II have found a consistent average rate of recurrence of 0.40 mood episodes per year in historical studies 67 and 0.44 mood episodes per year in more recent studies. 68 The median time to relapse is estimated to be 1.44 years, with higher relapse rates seen in BD-I (0.81 years) than in BD-II (1.63 years) and no differences observed with respect to age or sex. 1 2 In addition to focusing on episodes, an important development in research and clinical care of bipolar disorder has been the recognition of the burden of subsyndromal symptoms. Although milder in severity, these symptoms can be long lasting, functionally impairing, and can themselves be a risk factor for episode relapse. 69 Recent cohort studies have also found that a substantial proportion of patients with bipolar disorder (20-30%) continue to have poor outcomes even after receiving guideline based care. 46 70 Risk factors that contribute to this poor outcome include transdiagnostic indicators of adversity such as substance misuse, low educational attainment, socioeconomic hardship, and comorbid disorders. As expected, those with more severe past illness activity, including those with rapid cycling, were also more likely to remain symptomatically and psychosocially impaired. 46 71 72
The primary focus of treating bipolar disorder has been to manage the manic, mixed, or depressive episodes that present to clinical care and to subsequently prevent recurrence of future episodes. Owing to the relapse remitting nature of the illness, randomized controlled trials are essential to determine treatment efficacy, as the observation of clinical improvement could just represent the ebbs and flows of the natural history of the illness. In the United States, the FDA (Food and Drug Administration) requires at least two large scale placebo controlled trials (phase 3) to show significant evidence of efficacy before approving a treatment. Phase 3 studies of bipolar disorder are generally separated into short term studies of mania (3-4 weeks), short term studies for bipolar depression (4-6 weeks), and longer term maintenance studies to evaluate prophylactic activity against future mood episodes (usually lasting one year). Although the most rigorous evaluation of phase 3 studies would be to require two broadly representative and independent randomized controlled trials, the FDA permits consideration of so called enriched design trials that follow participants after an initial response and tolerability has been shown to an investigational drug. Because of this initial selection, such trials can be biased against comparator agents, and could be less generalizable to patients seen in clinical practice.
A summary of the agents approved by the FDA for treatment of bipolar disorder is in table 1 , which references the key clinical trials demonstrating efficacy. Figure 1 and supplementary table 1 are a comparison of treatments for mania, depression, and maintenance. Effect sizes reflect the odds ratios or relative risks of obtaining response (defined as ≥50% improvement from baseline) in cases versus controls and were extracted from meta-analyses of randomized controlled trials for bipolar depression 86 and maintenance, 94 as well as a network meta-analysis of randomized controlled trials in bipolar mania. 73 Effect sizes are likely to be comparable for each phase of treatment, but not across the different phases, since methodological differences exist between the three meta-analytic studies.
FDA approved medications for bipolar disorder
- View inline

Summary of treatment response rates (defined as ≥50% improvement from baseline) of modern clinical trials for acute mania, acute bipolar depression, and long term recurrence. Meta-analytic estimates were extracted from recent meta-analyses or network meta-analyses of acute mania, 73 acute bipolar depression, 86 and bipolar maintenance studies 94
- Download figure
- Open in new tab
- Download powerpoint
Acute treatment of mania
As mania is characterized by impaired judgment, individuals can be at risk for engaging in high risk, potentially dangerous behaviors that can have substantial personal, occupational, and financial consequences. Therefore, treatment of mania is often considered a psychiatric emergency and is, when possible, best performed in the safety of an inpatient unit. While the primary treatment for mania is pharmacological, diminished insight can impede patients' willingness to accept treatment, emphasizing the significance of a balanced therapeutic approach that incorporates shared decision making frameworks as much as possible to promote treatment adherence.
The three main classes of anti-manic treatments are lithium, mood stabilizing anticonvulsants (divalproate and carbamazepine), and antipsychotic medications. Almost all antipsychotics are effective in treating mania, with the more potent dopamine D2 receptor antagonists such as risperidone and haloperidol demonstrating slightly higher efficacy ( fig 1 ). 73 In the United States, the FDA has approved the use of all second generation antipsychotics for treating mania except for lurasidone and brexpriprazole. Compared with mood stabilizing medications, second generation antipsychotics have a faster onset of action, making them a first line treatment for more severe manic symptoms that require rapid treatment. 99 The choice of which specific second generation antipsychotic to use depends on a balance of efficacy, tolerability concerns, and cost considerations (see table 1 ). Notably, the FDA has placed a black box warning on all antipsychotics for increasing the risk of cerebral vascular accidents in the elderly. 100 While this was primarily focused on the use of antipsychotics in dementia, this likely class effect should be taken into account when considering the use of antipsychotics in the elderly.
Traditional mood stabilizers, such as lithium, divalproate, and carbamazepine are also effective in the treatment of active mania ( fig 1 ). Since lithium also has a robust prophylactic effect (see section on prevention of mood episodes below) it is often recommended as first line treatment and can be considered as monotherapy when rapid symptom reduction is not clinically indicated. On the other hand, other anticonvulsants such as lamotrigine, gabapentin, topiramate, and oxcarbazepine have not been found to be effective for the treatment of mania or mixed episodes. 101 Although the empirical evidence for polypharmacy is limited, 102 combination treatment in acute mania, usually consisting of a mood stabilizer and a second generation antipsychotic, is commonly used in clinical practice despite the higher burden of side effects. Following resolution of an acute mania, consideration should be given to transitioning to monotherapy with an agent with proven prophylactic activity.
Pharmacological approaches to bipolar depression
Depressed episodes are usually more common than mania or hypomania, 103 104 and often represent the primary reason for individuals with bipolar disorder to seek treatment. Nevertheless, because early antidepressant randomized controlled trials did not distinguish between unipolar and bipolar depressive episodes, it has only been in the past two decades that large scale randomized controlled trials have been conducted specifically for bipolar depression. As such trials are almost exclusively funded by pharmaceutical companies, they have focused on the second generation antipsychotics and newer anticonvulsants still under patent. These trials have shown moderate but robust effects for most recent second generation antipsychotics, five of which have received FDA approval for treating bipolar depression ( table 1 ). No head-to-head trials have been conducted among these agents, so the choice of medication depends on expected side effects and cost considerations. For example, quetiapine has robust antidepressant efficacy data but is associated with sedation, weight gain, and adverse cardiovascular outcomes. 105 Other recently approved medications such as lurasidone, cariprazine, and lumateperone have better side effect profiles but show more modest antidepressant activity. 106
Among the mood stabilizing anticonvulsants, lamotrigine has limited evidence for acute antidepressant activity, 107 possibly owing to the need for an 8 week titration to reach the full dose of 200 mg. However, as discussed below, lamotrigine can still be considered for mild to moderate acute symptoms owing to its generally tolerable side effect profile and proven effectiveness in preventing the recurrence of depressive episodes. Divalproate and carbamazepine have some evidence of being effective antidepressants in small studies, but as there has been no large scale confirmatory study, they should be considered second or third line options. 86 Lithium has been studied for the treatment of bipolar depression as a comparator to quetiapine and was not found to have a significant acute antidepressant effect. 88
Antidepressants
Owing to the limited options of FDA approved medications for bipolar depression and concerns of metabolic side effects from long term second generation antipsychotic use, clinicians often resort to the use of traditional antidepressants for the treatment of bipolar depression 108 despite the lack of FDA approval for such agents. Indeed, recent randomized clinical trials of antidepressants in bipolar depression have not shown an effect for paroxetine, 89 109 bupropion, 109 or agomelatine. 110 Beyond the question of efficacy, another concern regarding antidepressants in bipolar disorder is their potential to worsen the course of illness by either promoting mixed or manic symptoms or inducing more subtle degrees of mood instability and cycle acceleration. 111 However, the risk of switching to full mania while being treated with mood stabilizers appears to be modest, with a meta-analysis of randomized clinical trials and clinical cohort studies showing the rates of mood switching over an average follow-up of five months to be approximately 15.3% in people with bipolar disorder treated on antidepressants compared with 13.8% in those without antidepressant treatment. 111 The risk of switching appears to be higher in the first 1-2 years of treatment in people with BD-I, and in those treated with a tricyclic antidepressant 112 or the dual reuptake inhibitor venlafaxine. 113 Overall, while the available data have methodological limitations, most guidelines do not recommend the use of antidepressants in bipolar disorder, or recommend them only after agents with more robust evidence have been tried. That they remain so widely used despite the equivocal evidence base reflects the unmet need for treatment of depression, concerns about the long term side effects of second generation antipsychotics, and the challenges of changing longstanding prescribing patterns.
Pharmacological approaches to prevention of recurrent episodes
Following treatment of the acute depressive or manic syndrome, the major focus of treatment is to prevent future episodes and minimize interepisodic subsyndromal symptoms. Most often, the medication that has been helpful in controlling the acute episode can be continued for prevention, particularly if clinical trial evidence exists for a maintenance effect. To show efficacy for prevention, studies must be sufficiently long to allow the accumulation of future episodes to occur and be potentially prevented by a therapeutic intervention. However, few long term treatment studies exist and most have utilized enriched designs that likely favor the drug seeking regulatory approval. As shown in figure 1 , meta-analyses 94 show prophylactic effect for most (olanzapine, risperidone, quetiapine, aripiprazole, asenapine) but not all (lurasidone, paliperidone) recently approved second generation antipsychotics. The effect sizes are generally comparable with monotherapy (odds ratio 0.42, 95% confidence interval 0.34 to 0.5) or as adjunctive therapy (odds ratio 0.37, 95% confidence interval 0.25 to 0.55). 94 Recent studies of lithium, which have generally used it as a (non-enriched) comparator drug, show a comparable protective effect (odds ratio 0.46, 95% confidence interval 0.28 to 0.75). 94 Among the mood stabilizing anticonvulsant drugs, a prophylactic effect has also been found for both divalproate and lamotrigine ( fig 1 and supplementary table 1), although only the latter has been granted regulatory approval for maintenance treatment. While there are subtle differences in effect sizes in drugs approved for maintenance ( fig 1 and table 1 ), the overlapping confidence intervals and methodological differences between studies prevent a strict comparison of the effect measures.
Guidelines often recommend lithium as a first line agent given its consistent evidence of prophylaxis, even when tested as the disadvantaged comparator drug in enriched drug designs. Like other medications, lithium has a unique set of side effects and ultimately the decision about which drug to use among those which are efficacious should be a decision carefully weighed and shared between patient and provider. The decision might be re-evaluated after substantial experience with the medication or at different stages in the long term treatment of bipolar disorder (see table 1 ).
Psychotherapeutic approaches
The frequent presence of residual symptoms, often associated with psychosocial and occupational dysfunction, has led to renewed interest in psychotherapeutic and psychosocial approaches to bipolar disorder. Given the impairment of judgment seen in mania, psychotherapy has more of a supportive and educational role in the treatment of mania, whereas it can be more of a primary focus in the treatment of depressive states. On a broad level, psychotherapeutic approaches effective for acute depression, such as cognitive behavioral therapy, interpersonal therapy, behavioral activation, and mindfulness based strategies, can also be recommended for acute depressive states in individuals with bipolar disorder. 114 Evidence for more targeted psychotherapy trials for bipolar disorder is more limited, but meta-analyses have found evidence for decreased recurrence (odds ratio 0.56; 95% confidence interval 0.43 to 0.74) 115 and improvement of subthreshold interepisodic depressive and manic symptoms with cognitive behavioral therapy, family based therapy, interpersonal and social rhythm therapy, and psychoeducation. 115 Recent investigations have also focused on targeted forms of psychotherapy to improve cognition 116 117 118 as well as psychosocial and occupational functioning. 119 120 Although these studies show evidence of a moderate effect, they remain preliminary, methodologically diverse, and require replication on a larger scale. 121
The implementation of evidence based psychotherapy as a treatment faces several challenges, including clinical training, fidelity monitoring, and adequate reimbursement. Novel approaches, leveraging the greater tractability of digital tools 122 and allied healthcare workers, 123 are promising means of lessening the implementation gap; however, these approaches require validation and evidence of clinical utility similar to traditional methods.
Neurostimulation approaches
For individuals with bipolar disorder who cannot tolerate or do not respond well to standard pharmacotherapy or psychotherapeutic approaches, neurostimulation techniques such as repetitive transcranial magnetic stimulation or electric convulsive therapy should be considered as second or third line treatments. Electric convulsive therapy has shown response rates of approximately 60-80% in severe acute depressions 124 125 and 50-60% in cases with treatment resistant depression. 126 These response rates compare favorably with those of pharmacological treatment, which are likely to be closer to ~50% and ~30% in subjects with moderate to severe depression and treatment resistant depression, respectively. 127 Although the safety of electric convulsive therapy is well established, relatively few medical centers have it available, and its acceptability is limited by cognitive side effects, which are usually short term, but which can be more significant with longer courses and with bilateral electrode placement. 128 While there have been fewer studies of electric convulsive therapy for bipolar depression compared with major depressive disorder, it appears to be similarly effective and might show earlier response. 129 Anecdotal evidence also suggests electric convulsive therapy that is useful in refractory mania. 130
Compared with electric convulsive therapy, repetitive transcranial magnetic stimulation has no cognitive side effects and is generally well tolerated. Repetitive transcranial magnetic stimulation acts by generating a magnetic field to depolarize local neural tissue and induce excitatory or inhibitory effects depending on the frequency of stimulation. The most studied FDA approved form of repetitive transcranial magnetic stimulation applies high frequency (10 Hz) excitatory pulses to the left prefrontal cortex for 30-40 minutes a day for six weeks. 131 Like electric convulsive therapy, repetitive transcranial magnetic stimulation has been primarily studied in treatment resistant depression and has been found to have moderate effect, with about one third of patients having a significant treatment response compared with those treated with pharmacotherapy. 131 Recent innovations in transcranial magnetic stimulation have included the use of a novel, larger coil to stimulate a larger degree of the prefrontal cortex (deep transcranial magnetic stimulation), 132 and a shortened (three minutes), higher frequency intermittent means of stimulation known as theta burst stimulation that appears to be comparable to conventional (10 Hz) repetitive transcranial magnetic stimulation. 133 A preliminary trial has recently assessed a new accelerated protocol of theta burst stimulation marked by 10 sessions a day for five days. It found that theta burst stimulation had a greater effect on people with treatment resistant depression compared with treatment as usual, although larger studies are needed to confirm these findings. 134
Conventional repetitive transcranial magnetic stimulation (10 Hz) studies in bipolar disorder have been limited by small sample sizes but have generally shown similar effects compared with major depressive disorder. 135 However, a proof of concept study of single session theta burst stimulation did not show efficacy in bipolar depression, 136 reiterating the need for specific trials for bipolar depression. Given the lack of such trials in bipolar disorder, repetitive transcranial magnetic stimulation should be considered a potentially promising but as yet unproven treatment for bipolar depression.
The other major form of neurostimulation studied in both unipolar and bipolar depression is transcranial direct current stimulation, an easily implemented method of delivering a low amplitude electrical current to the prefrontal area of the brain that could lead to local changes in neuronal excitability. 137 Like repetitive transcranial magnetic stimulation, transcranial direct current stimulation is well tolerated and has been mostly studied in unipolar depression, but has not yet generated sufficient evidence to be approved by a regulatory agency. 138 Small studies have been performed in bipolar depression, but the results have been mixed and require further research before use in clinical settings. 137 138 139 Finally, the evidence for more invasive neurostimulation studies such as vagal nerve stimulation and deep brain stimulation remains extremely limited and is currently insufficient for clinical use. 140 141
Treatment resistance in bipolar disorder
As in major depressive disorder, the use of term treatment resistance in bipolar disorder is controversial since differentiating whether persistent symptoms are caused by low treatment adherence, poor tolerability, the presence of comorbid disorders, or are the result of true treatment resistance, is an essential but often challenging clinical task. Treatment resistance should only be considered after two or three trials of evidence based monotherapy, adjunctive therapy, or both. 142 In difficult-to-treat mania, two or more medications from different mechanistic classes are typically used, with electric convulsive therapy 143 and clozapine 144 being considered if more conventional anti-manic treatments fail. In bipolar depression, it is common to combine antidepressants with anti-manic agents, despite limited evidence for efficacy. 145 Adjunctive therapies such as bright light therapy, 146 the dopamine D2/3 receptor agonist pramipexole, 147 and ketamine 148 149 have shown promising results in small open label trials that require further study.
Treatment considerations to reduce suicide in bipolar disorder
The risk of completed suicide is high across the subtypes of bipolar disorder, with estimated rates of 10-15% across the lifespan. 150 151 152 Lifetime rates of suicide attempts are much higher, with almost half of all individuals with bipolar disorder reporting at least one attempt. 153 Across a population and, often within individuals, the causes of suicide attempts and completed suicides are likely to be multifactorial, 154 affected by various risk factors, such as symptomatic illness, environmental stressors, comorbidities (particularly substance misuse), trait impulsivity, interpersonal conflict, loneliness, or socioeconomic distress. 155 156 Risk is highest in depressive and dysphoric/mixed episodes 157 158 and is particularly high in the transitional period following an acute admission to hospital. 159 Among the available treatments, lithium has potential antisuicidal properties. 160 However, since suicide is a rare event, with very few to zero suicides within a typical clinical trial, moderate evidence for this effect emerges only in the setting of meta-analyses of clinical trials. 160 Several observational studies have shown lower mortality in patients on lithium treatment, 161 but such associations might not be causal, since lithium is potentially fatal in overdose and is often avoided by clinicians in patients at high risk of suicide.
The challenge of studying scarce events has led most studies to focus on the reduction of the more common phenomena of suicidal ideation and behavior as a proxy for actual suicides. A recent such multisite study of the Veterans Affairs medical system included a mixture of unipolar and bipolar disorder and was stopped prematurely for futility, indicating no overall effect of moderate dose lithium. 162 Appropriate limitations of this study have been noted, 163 164 including difficulties in recruitment, few patients with bipolar disorder (rather than major depressive disorder), low levels of compliance with lithium therapy, high rates of comorbidity, and a follow-up of only one year. Nevertheless, while the body of evidence suggests that lithium has a modest antisuicidal effect, its degree of protection and utility in complex patients with comorbidities and multiple risk factors remain matters for further study. Treatment of specific suicidal risk in patients with bipolar disorder must therefore also incorporate broader interventions based on the individual’s specific risk factors. 165 Such an approach would include societal interventions like means restriction 166 and a number of empirically tested suicide focused psychotherapy treatments. 167 168 Unfortunately, the availability of appropriate training, expertise, and care models for such treatments remains limited, even in higher income countries. 169
More scalable solutions, such as the deployment of shortened interventions via digital means could help to overcome this implementation gap; however, the effectiveness of such approaches cannot be assumed and requires empirical testing. For example, a recent large scale randomized controlled trial of an abbreviated online dialectical behavioral therapy skills training program was paradoxically associated with slightly increased risk of self-harm. 170
Treatment consideration in BD-II and bipolar spectrum conditions
Because people with BD-II primarily experience depressive symptoms and appear less likely to switch mood states compared with individuals with BD-I, 50 171 there has been a greater acceptance of the use of antidepressants in BD-II depression, including as monotherapy. 172 However, caution should be exercised when considering the use of antidepressants without a mood stabilizer in patients with BD-II who might also experience high rates of mood instability and rapid cycling. Such individuals can instead respond better to newer second generation antipsychotic agents such as quetiapine 173 and lumateperone, 93 which are supported by post hoc analyses of these more recent clinical trials with more BD-II patients. In addition, despite the absence of randomized controlled trials, open label studies have suggested that lithium and other mood stabilizers can have similar efficacy in BD-II, especially in the case of lamotrigine. 174
Psychotherapeutic approaches such as psychoeducation, cognitive behavioral therapy, and interpersonal and social rhythm therapy have been found to be helpful 115 and can be considered as the primary form of treatment for BD-II in some patients, although in most clinical scenarios BD-II is likely to occur in conjunction with psychopharmacology. While it can be tempting to consider BD-II a milder variant of BD-I, high rates of comorbid disorders, rapid cycling, and adverse consequences such as suicide attempts 175 176 highlight the need for clinical caution and the provision of multimodal treatment, focusing on mood improvement, emotional regulation, and better psychosocial functioning.
Precision medicine: can it be applied to improve the care of bipolar disorder?
The recent focus on precision medicine approaches to psychiatric disorders seeks to identify clinically relevant heterogeneity and identify characteristics at the level of the individual or subgroup that can be leveraged to identify and target more efficacious treatments. 1 177 178
The utility of such an approach was originally shown in oncology, where a subset of tumors had gene expression or DNA mutation signatures that could predict response to treatments specifically designed to target the aberrant molecular pathway. 179 While much of the emphasis of precision medicine has been on the eventual identification of biomarkers utilizing high throughput approaches (genetics and other “omics” based measurements), the concept of precision medicine is arguably much broader, encompassing improvements in measurement, potentially through the deployment of digital tools, as well as better conceptualization of contextual, cultural, and socioeconomic mechanisms associated with psychopathology. 180 181 Ultimately, the goal of precision psychiatry is to identify and target driving mechanisms, be they molecular, physiological, or psychosocial in nature. As such, precision psychiatry seeks what researchers and clinicians have often sought: to identify clinically relevant heterogeneity to improve prediction of outcomes and increase the likelihood of therapeutic success. The novelty being not so much the goals of the overarching approach, but the increasing availability of large samples, novel digital tools, analytical advances, and an increasing armamentarium of biological measurements that can be deployed at scale. 177
Although not unique to bipolar disorder, several clinical decision points along the life course of bipolar disorder would benefit from a precision medicine approach. For example, making an early diagnosis is often not possible based on clinical symptoms alone, since such symptoms are usually non-specific. A precision medicine approach could also be particularly relevant in helping to identify subsets of patients for whom the use of antidepressants could be beneficial or harmful. Admittedly, precision medicine approaches to bipolar disorder are still in their infancy, and larger, clinically relevant, longitudinal, and reliable phenotypes are needed to provide the infrastructure for precision medicine approaches. Such data remain challenging to obtain at scale, leading to renewed efforts to utilize the extant clinical infrastructure and electronic medical records to help emulate traditional longitudinal analyses. Electronic medical records can help provide such data, but challenges such as missingness, limited quality control, and potential biases in care 182 need to be resolved with carefully considered analytical designs. 183
Emerging treatments
Two novel atypical antipsychotics, amilsupride and bifeprunox, are currently being tested in phase 3 trials ( NCT05169710 and NCT00134459 ) and could gain approval for bipolar depression in the near future if these pivotal trials show a significant antidepressant effect. These drugs could offer advantages such as greater antidepressant effects, fewer side effects, and better long term tolerability, but these assumptions must be tested empirically. Other near term possibilities include novel rapid antidepressant treatments, such as (es)ketamine that putatively targets the glutamatergic system, and has been recently approved for treatment resistant depression, but which have not yet been tested in phase 3 studies in bipolar depression. Small studies have shown comparable effects of intravenous ketamine, 149 184 in bipolar depression with no short term evidence of increased mood switching or mood instability. Larger phase 2 studies ( NCT05004896 ) are being conducted which will need to be followed by larger phase 3 studies. Other therapies targeting the glutamatergic system have generally failed phase 3 trials in treatment resistant depression, making them unlikely to be tested in bipolar depression. One exception could be the combination of dextromethorphan and its pharmacokinetic (CYP2D6) inhibitor bupropion, which was recently approved for treatment resistant depression but has yet to be tested in bipolar depression. Similarly, the novel GABAergic compound zuranolone is currently being evaluated by the FDA for the treatment of major depressive disorder and could also be subsequently studied in bipolar depression.
Unfortunately, given the general efficacy for most patients of available treatments, few scientific and financial incentives exist to perform large scale studies of novel treatment in mania. Encouraging results have been seen in small studies of mania with the selective estrogen receptor modulator 185 tamoxifen and its active metabolite endoxifen, both of which are hypothesized to inhibit protein kinase C, a potential mechanistic target of lithium treatment. These studies remain small, however, and anti-estrogenic side effects have potentially dulled interest in performing larger studies.
Finally, several compounds targeting alternative pathophysiological mechanisms implicated in bipolar disorder have been trialed in phase 2 academic studies. The most studied has been N -acetylcysteine, a putative mitochondrial modulator, which initially showed promising results only to be followed by null findings in larger more recent studies. 186 Similarly, although small initial studies of anti-inflammatory agents provided impetus for further study, subsequent phase 2 studies of the non-steroidal agent celecoxib, 187 the anti-inflammatory antibiotic minocycline, 187 and the antibody infliximab (a tumor necrosis factor antagonist) 188 have not shown efficacy for bipolar depression. Secondary analyses have suggested that specific anti-inflammatory agents might be effective only for a subset of patients, such as those with elevated markers of inflammation or a history of childhood adversity 189 ; however, such hypotheses must be confirmed in adequately powered independent studies.
Several international guidelines for the treatment of bipolar disorder have been published in the past decade, 102 190 191 192 providing a list of recommended treatments with efficacy in at least one large randomized controlled trial. Since effect sizes tend to be moderate and broadly comparable across classes, all guidelines allow for significant choice among first line agents, acknowledging that clinical characteristics, such as history of response or tolerability, severity of symptoms, presence of mixed features, or rapid cycling can sometimes over-ride guideline recommendations. For acute mania requiring rapid treatment, all guidelines prioritize the use of second generation antipsychotics such as aripiprazole, quetiapine, risperidone, asenapine, and cariprazine. 102 192 193 Combination treatment is considered based on symptom severity, tolerability, and patient choice, with most guidelines recommending lithium or divalproate along with a second generation antipsychotic for mania with psychosis, severe agitation, or prominent mixed symptoms. While effective, haloperidol is usually considered a second choice option owing to its propensity to cause extrapyramidal symptoms. 102 192 193 Uniformly, all guidelines agree on the need to taper antidepressants in manic or mixed episodes.
For maintenance treatment, guidelines are generally consistent in recommending lithium if tolerated and without relative contraindications, such as baseline renal disease. 194 The second most recommended maintenance treatment is quetiapine, followed by aripiprazole for patients with prominent manic episodes and lamotrigine for patients with predominant depressive episodes. 194 Most guidelines recommend considering prophylactic properties when initially choosing treatment for acute manic episodes, although others suggests that acute maintenance treatments can be cross tapered with maintenance medications after several months of full reponse. 193
For bipolar depression, recent guidelines recommend specific second generation antipsychotics such as quetiapine, lurasidone, and cariprazine 102 192 193 For more moderate symptoms, consideration is given to first using lamotrigine and lithium. Guidelines remain cautious about the use of antidepressants (selective serotonin reuptake inhibitors, venlafaxine, or bupropion) in patients with BP-I, restricting them to second or third line treatments and always in the context of an anti-manic agent. However, for patients with BP-II and no rapid cycling, several guidelines allow for the use of carefully monitored antidepressant monotherapy.
Bipolar disorder is a highly recognizable syndrome with many effective treatment options, including the longstanding gold standard therapy lithium. However, a significant proportion of patients do not respond well to current treatments, leading to negative consequences, poor quality of life, and potentially shortened lifespan. Several novel treatments are being developed but limited knowledge of the biology of bipolar disorder remains a major challenge for novel drug discovery. Hope remains that the insights of genetics, neuroimaging, and other investigative modalities could soon be able to inform the development of rational treatments aimed to mitigate the underlying pathophysiology associated with bipolar disorder. At the same time, however, efforts are needed to bridge the implementation gap and provide truly innovative and integrative care for patients with bipolar disorder. 195 Owing to the complexity of bipolar disorder, few patients can be said to be receiving optimized care across the various domains of mental health that are affected in those with bipolar disorder. Fortunately, the need for improvement is now well documented, 196 and concerted efforts at the scale necessary to be truly innovative and integrative are now on the horizon.
Questions for future research
Among adolescents and young adults who manifest common mental disorders such as anxiety or depressive or attentional disorders, who will be at high risk for developing bipolar disorder?
Can we predict the outcomes for patients following a first manic or hypomanic episode? This will help to inform who will require lifelong treatment and who can be tapered off medications after sustained recovery.
Are there reliable clinical features and biomarkers that can sufficiently predict response to specific medications or classes of medication?
What are the long term consequences of lifelong treatments with the major classes of medications used in bipolar disorder? Can we predict and prevent medical morbidity caused by medications?
Can we understand in a mechanistic manner the pathophysiological processes that lead to abnormal mood states in bipolar disorder?
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors
Contributors: FSG performed the planning, conduct, and reporting of the work described in the article. FSG accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Competing interests: I have read and understood the BMJ policy on declaration of interests and declare no conflicts of interest.
Patient involvement: FSG discussed of the manuscript, its main points, and potential missing points with three patients in his practice who have lived with longstanding bipolar disorder. These additional viewpoints were incorporated during the drafting of the manuscript.
Provenance and peer review: Commissioned; externally peer reviewed.
- ↵ . Falret’s discovery: the origin of the concept of bipolar affective illness. Translated by M. J. Sedler and Eric C. Dessain. Am J Psychiatry 1983;140:1127-33. doi: 10.1176/ajp.140.9.1127 OpenUrl CrossRef PubMed Web of Science
- ↵ Kraepelin E. Manic-depressive Insanity and Paranoia. Translated by R. Mary Barclay from the Eighth German. Edition of the ‘Textbook of Psychiatry.’ 1921.
- Merikangas KR ,
- Akiskal HS ,
- Koukopoulos A ,
- Jongsma HE ,
- Kirkbride JB ,
- Rowland TA ,
- Kessler RC ,
- Kazdin AE ,
- Aguilar-Gaxiola S ,
- WHO World Mental Health Survey collaborators
- Bergen SE ,
- Kuja-Halkola R ,
- Larsson H ,
- Lichtenstein P
- Smoller JW ,
- Lichtenstein P ,
- Sjölander A ,
- Mullins N ,
- Forstner AJ ,
- O’Connell KS ,
- Palmer DS ,
- Howrigan DP ,
- Chapman SB ,
- Pirooznia M ,
- Murray GK ,
- McGrath JJ ,
- Hickie IB ,
- ↵ Mostafavi H, Harpak A, Agarwal I, Conley D, Pritchard JK, Przeworski M. Variable prediction accuracy of polygenic scores within an ancestry group. Loos R, Eisen MB, O’Reilly P, eds. eLife 2020;9:e48376. doi: 10.7554/eLife.48376 OpenUrl CrossRef PubMed
- Westlye LT ,
- van Erp TGM ,
- Costa Rica/Colombia Consortium for Genetic Investigation of Bipolar Endophenotypes
- Pauling M ,
- ENIGMA Bipolar Disorder Working Group
- Schnack HG ,
- Ching CRK ,
- ENIGMA Bipolar Disorders Working Group
- Goltermann J ,
- Hermesdorf M ,
- Dannlowski U
- Gurholt TP ,
- Suckling J ,
- Lennox BR ,
- Bullmore ET
- Marangoni C ,
- Hernandez M ,
- Achtyes ED ,
- Agnew-Blais J ,
- Gilman SE ,
- Upthegrove R ,
- ↵ Etain B, Aas M. Childhood Maltreatment in Bipolar Disorders. In: Young AH, Juruena MF, eds. Bipolar Disorder: From Neuroscience to Treatment . Vol 48. Current Topics in Behavioral Neurosciences. Springer International Publishing; 2020:277-301. doi: 10.1007/7854_2020_149
- Johnson SL ,
- Weinberg BZS
- Stinson FS ,
- Costello CG
- Klein & Riso LP DN
- Sandstrom A ,
- Perroud N ,
- de Jonge P ,
- Bunting B ,
- Nierenberg AA
- Hantouche E ,
- Vannucchi G
- Zimmerman M ,
- Ruggero CJ ,
- Chelminski I ,
- Leverich GS ,
- McElroy S ,
- Mignogna KM ,
- Balling C ,
- Dalrymple K
- Kappelmann N ,
- Stokes PRA ,
- Jokinen T ,
- Baldessarini RJ ,
- Faedda GL ,
- Offidani E ,
- Viktorin A ,
- Launders N ,
- Osborn DPJ ,
- Roshanaei-Moghaddam B ,
- De Hert M ,
- Detraux J ,
- van Winkel R ,
- Lomholt LH ,
- Andersen DV ,
- Sejrsgaard-Jacobsen C ,
- Skjelstad DV ,
- Gregersen M ,
- Søndergaard A ,
- Brandt JM ,
- Van Meter AR ,
- Youngstrom EA ,
- Taylor RH ,
- Ulrichsen A ,
- Strawbridge R
- Hafeman DM ,
- Merranko J ,
- Hirschfeld RM ,
- Williams JB ,
- Spitzer RL ,
- Adolfsson R ,
- Benazzi F ,
- Regier DA ,
- Johnson KR ,
- Akinhanmi MO ,
- Biernacka JM ,
- Strakowski SM ,
- Goldberg JF ,
- Schettler PJ ,
- Coryell W ,
- Scheftner W ,
- Endicott J ,
- Zarate CA Jr . ,
- Matsuda Y ,
- Fountoulakis KN ,
- Zarate CA Jr .
- Bowden CL ,
- Brugger AM ,
- The Depakote Mania Study Group
- Calabrese JR ,
- Depakote ER Mania Study Group
- Weisler RH ,
- Kalali AH ,
- Ketter TA ,
- SPD417 Study Group
- Keck PE Jr . ,
- Cutler AJ ,
- Caffey EM Jr . ,
- Grossman F ,
- Eerdekens M ,
- Jacobs TG ,
- Grundy SL ,
- The Olanzipine HGGW Study Group
- Versiani M ,
- Ziprasidone in Mania Study Group
- Sanchez R ,
- Aripiprazole Study Group
- McIntyre RS ,
- Panagides J
- Calabrese J ,
- McElroy SL ,
- EMBOLDEN I (Trial 001) Investigators
- EMBOLDEN II (Trial D1447C00134) Investigators
- Lamictal 606 Study Group
- Lamictal 605 Study Group
- Keramatian K ,
- Chakrabarty T ,
- Nestsiarovich A ,
- Gaudiot CES ,
- Neijber A ,
- Hellqvist A ,
- Paulsson B ,
- Trial 144 Study Investigators
- Schwartz JH ,
- Szegedi A ,
- Cipriani A ,
- Salanti G ,
- Dorsey ER ,
- Rabbani A ,
- Gallagher SA ,
- Alexander GC
- Cerqueira RO ,
- Yatham LN ,
- Kennedy SH ,
- Parikh SV ,
- Højlund M ,
- Andersen K ,
- Correll CU ,
- Ostacher M ,
- Schlueter M ,
- Geddes JR ,
- Mojtabai R ,
- Nierenberg AA ,
- Goodwin GM ,
- Agomelatine Study Group
- Vázquez G ,
- Baldessarini RJ
- Altshuler LL ,
- Cuijpers P ,
- Miklowitz DJ ,
- Efthimiou O ,
- Furukawa TA ,
- Strawbridge R ,
- Tsapekos D ,
- Hodsoll J ,
- Vinberg M ,
- Kessing LV ,
- Forman JL ,
- Miskowiak KW
- Lewandowski KE ,
- Sperry SH ,
- Torrent C ,
- Bonnin C del M ,
- Martínez-Arán A ,
- Bonnín CM ,
- Tamura JK ,
- Carvalho IP ,
- Leanna LMW ,
- Karyotaki E ,
- Individual Patient Data Meta-Analyses for Depression (IPDMA-DE) Collaboration
- Vipulananthan V ,
- Hurlemann R ,
- UK ECT Review Group
- Haskett RF ,
- Mulsant B ,
- Trivedi MH ,
- Wisniewski SR ,
- Espinoza RT ,
- Vazquez GH ,
- McClintock SM ,
- Carpenter LL ,
- National Network of Depression Centers rTMS Task Group ,
- American Psychiatric Association Council on Research Task Force on Novel Biomarkers and Treatments
- Levkovitz Y ,
- Isserles M ,
- Padberg F ,
- Blumberger DM ,
- Vila-Rodriguez F ,
- Thorpe KE ,
- Williams NR ,
- Sudheimer KD ,
- Bentzley BS ,
- Konstantinou G ,
- Toscano E ,
- Husain MM ,
- McDonald WM ,
- International Consortium of Research in tDCS (ICRT)
- Sampaio-Junior B ,
- Tortella G ,
- Borrione L ,
- McAllister-Williams RH ,
- Gippert SM ,
- Switala C ,
- Bewernick BH ,
- Hidalgo-Mazzei D ,
- Mariani MG ,
- Fagiolini A ,
- Swartz HA ,
- Benedetti F ,
- Barbini B ,
- Fulgosi MC ,
- Burdick KE ,
- Diazgranados N ,
- Ibrahim L ,
- Brutsche NE ,
- Sinclair J ,
- Gerber-Werder R ,
- Miller JN ,
- Vázquez GH ,
- Franklin JC ,
- Ribeiro JD ,
- Turecki G ,
- Gunnell D ,
- Hansson C ,
- Pålsson E ,
- Runeson B ,
- Pallaskorpi S ,
- Suominen K ,
- Ketokivi M ,
- Hadzi-Pavlovic D ,
- Stanton C ,
- Lewitzka U ,
- Severus E ,
- Müller-Oerlinghausen B ,
- Rogers MP ,
- Li+ plus Investigators
- Manchia M ,
- Michel CA ,
- Auerbach RP
- Altavini CS ,
- Asciutti APR ,
- Solis ACO ,
- Casañas I Comabella C ,
- Riblet NBV ,
- Young-Xu Y ,
- Shortreed SM ,
- Rossom RC ,
- Amsterdam JD ,
- Brunswick DJ
- Gustafsson U ,
- Marangell LB ,
- Bernstein IH ,
- Karanti A ,
- Kardell M ,
- Collins FS ,
- Armstrong K ,
- Concato J ,
- Singer BH ,
- Ziegelstein RC
- ↵ Holmes JH, Beinlich J, Boland MR, et al. Why Is the Electronic Health Record So Challenging for Research and Clinical Care? Methods Inf Med 2021;60(1-02):32-48. doi: 10.1055/s-0041-1731784
- García Rodríguez LA ,
- Cantero OF ,
- Martinotti G ,
- Dell’Osso B ,
- Di Lorenzo G ,
- REAL-ESK Study Group
- Palacios J ,
- DelBello MP ,
- Husain MI ,
- Chaudhry IB ,
- Subramaniapillai M ,
- Jones BDM ,
- Daskalakis ZJ ,
- Carvalho AF ,
- ↵ Goodwin GM, Haddad PM, Ferrier IN, et al. Evidence-based guidelines for treating bipolar disorder: revised third edition Recommendations from the British Association for Psychopharmacology. J Psychopharmacol 2016;30:495-553. doi: 10.1177/0269881116636545 OpenUrl CrossRef PubMed
- Verdolini N ,
- Del Matto L ,
- Regeer EJ ,
- Hoogendoorn AW ,
- Harris MG ,
- WHO World Mental Health Survey Collaborators
- Research article
- Open access
- Published: 08 February 2021
Bipolar I disorder: a qualitative study of the viewpoints of the family members of patients on the nature of the disorder and pharmacological treatment non-adherence
- Nasim Mousavi 1 ,
- Marzieh Norozpour ORCID: orcid.org/0000-0002-8894-9178 1 ,
- Zahra Taherifar 2 ,
- Morteza Naserbakht 3 &
- Amir Shabani 3
BMC Psychiatry volume 21 , Article number: 83 ( 2021 ) Cite this article
18k Accesses
4 Citations
4 Altmetric
Metrics details
Bipolar disorder is a common psychiatric disorder with a massive psychological and social burden. Research indicates that treatment adherence is not good in these patients. The families’ knowledge about the disorder is fundamental for managing their patients’ disorder. The purpose of the present study was to investigate the knowledge of the family members of a sample of Iranian patients with bipolar I disorder (BD-I) and to explore the potential reasons for treatment non-adherence.
This study was conducted by qualitative content analysis. In-depth interviews were held and open-coding inductive analysis was performed. A thematic content analysis was used for the qualitative data analysis.
The viewpoints of the family members of the patients were categorized in five themes, including knowledge about the disorder, information about the medications, information about the treatment and the respective role of the family, reasons for pharmacological treatment non-adherence, and strategies applied by families to enhance treatment adherence in the patients. The research findings showed that the family members did not have enough information about the nature of BD-I, which they attributed to their lack of training on the disorder. The families did not know what caused the recurrence of the disorder and did not have sufficient knowledge about its prescribed medications and treatments. Also, most families did not know about the etiology of the disorder.
The lack of knowledge among the family members of patients with BD-I can have a significant impact on relapse and treatment non-adherence. These issues need to be further emphasized in the training of patients’ families. The present findings can be used to re-design the guidelines and protocols in a way to improve treatment adherence and avoid the relapse of BD-I symptoms.
Peer Review reports
Bipolar I disorder (BD-I) is a chronic and recurrent psychiatric disorder in which a person has a manic episode for 1 week, which may present before or after hypomanic or major depressive episodes [ 1 ].
BD-I is accompanied by chronic stress, disability, increased risk of sudden mood swings, higher rates of comorbid disorders and moral, financial, and legal problems. The disorder is ranked the sixth debilitating disease according to the World Health Organization (WHO). BD-I is considered the most expensive mental disorder in terms of the health and behavioral care required by the patients and the burden on governmental institutions and insurance companies [ 2 , 3 , 4 ]. According to a report by the Central Bank of the Islamic Republic of Iran, the average annual income of an Iranian household in 2012 was 209,050,000 Rials. The direct annual cost of one BD-I patient consists of 10% of this average family income [ 5 ].
BD-I affects the patient’s life and has long-term consequences that are visible in the patient’s social performance and quality of life [ 6 , 7 ]. Severe impairment in job performance is observed in about 30% of the patients with BD-I. In such cases, functional improvement falls substantially behind symptom improvement [ 1 ].
Pharmacological treatment is the first-line treatment for BD-I. Evidence shows that about 40% of patients with BD-I do not have good medication adherence, which translates into a higher probability of symptom relapse, hospitalization, and increased suicide risk [ 8 ]. In a study in Tehran, Iran, poor treatment adherence was noticed in about 30% of BD-I patients [ 9 ]. Another study from Iran [ 10 ] also reported the prevalence of poor compliance in BD-I patients after the first episode of mania as 38.1% during a 17-month follow-up period. Therefore, it is of great importance to better understand and investigate the underlying reasons for treatment non-adherence in BD-I patients.
Given the changes implemented in health care systems over the last two decades and the resultant focus on community-based services, the role of families in caring for BD-I patients has become more prominent [ 6 ]. The insufficient knowledge of families about the disorder, its symptoms, and medications has made the management of BD-I more difficult and eventually imposes additional costs on them [ 6 ]. The higher is the cost imposed on the family, the more likely is it for the family members to show adverse reactions to the BD-I patients, which itself leads to a higher chance of disorder relapse [ 3 ].
In Iran, the general public is acquainted with various types of psychiatric illnesses through mass media and public educational websites such as the website of the Iranian Psychiatric Association ( https://iranmentalhealth.com ) and other Persian public written sources. Patients with BD-I and their families become familiar with the treatment process after consulting a general practitioner, a psychiatrist, or a psychologist, and, if necessary, the patients are admitted to the hospital through a psychiatrist. In addition to medical treatment, they receive the necessary training and information about their treatment process in the hospital. Furthermore, an association called ABR (Association of Mental Health Promotion), with an active website ( http://abrcharity.ir ), independently monitors patients, including those with bipolar disorder, after discharge.
Many studies have examined the views and roles of patients with BD-I and their caregivers and also the importance of family awareness and its impact on medication adherence. Tacchi & Scott [ 11 ] and Veligan et al. [ 12 ] suggest that the family members’ beliefs about the nature of BD-I and the information they have about the disorder affect the patient’s medication adherence. The review of literature showed no precise studies conducted to explore the knowledge, information, and opinions of family members of BD-I patients about the disorder and the causes of their medication non-adherence.
In a previous study in Iran [ 13 ], the authors held qualitative interviews with the family members of patients with BD-I and reported that treatment non-adherence is a major problem in these patients. They also reported that the patients and their families did not have sufficient knowledge about the nature of this disorder. Considering these findings about the insufficient knowledge of the family members of BD-I patients and the high rate of treatment non-adherence, it is necessary to conduct more studies to investigate the possible causes of treatment non-adherence and families’ knowledge and beliefs about this disorder in Iran. This study was thus carried out to explore the viewpoints of the family members of BD-I patients about the nature of this disorder and the potential causes of treatment non-adherence. The results can be used for revising the psychoeducation guidelines for BD-I patients, as clinical guidelines mandate the inclusion of psychoeducation in the treatment plan adopted for these patients. The results can also be used to design a protocol to address the disorder relapse, which can have substantial consequences in terms of reducing healthcare costs.
The findings of this study are reported according to the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist [ 14 ].
Study samples’ characteristics
The participants were the family members of patients diagnosed with BD-I. The patients had been admitted to Iran Psychiatry Hospital in Tehran, Iran, and were receiving pharmacological treatments.
This study used purposive sampling to select the participants. From November 2017 to April 2018, 12 patients were interviewed by two psychiatrists based on the DSM-5 criteria [ 1 ] and received the diagnosis of BD-I. Then these diagnoses were confirmed by A.SH. and their families were invited to participate in the study.
None of the family members refused to participate in the study and they all completed the entire course of the study. The mean age of the participants was 50.83 years. There were three male (25%) and nine female (75%) participants (Table 1 ). Table 2 shows further details on patients’ characteristics.
Data collection
After diagnosing patients with BD-I, and obtaining the written consent of the family members of patients to participate in this study, data were collected by in-depth interviews from family members of patients, conducted at the hospital’s conference hall. No one else was present at the time of the interviews except for the interviewer and the participant. Each interview lasted approximately 20 min and was digitally recorded for subsequent analyses. Two female PhD candidates (N. M. and M. N.) in clinical psychology at the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran, who had already received training on the implementation of qualitative studies, held the interviews. They did not know any of the participants. The interviewers introduced themselves to the participants before the beginning of each interview. The interview questions were provided by the authors. The interviews were held only once and were not repeated. Data saturation was reached with 12 participants, and no further participants were interviewed after reaching this number. Data saturation occurs when no new information is obtained by conducting further interviews [ 15 ].
Data analysis
Thematic analysis was used for the qualitative data analysis [ 16 , 17 ]. To this end, the six steps proposed by Clark and Brown [ 17 ] were used.
The raw data derived from the interviews were used for the analysis. The content of the interviews were transcribed verbatim immediately after each interview. Field notes were made during the interviews and were reviewed in this stage. Three authors (M. N., N. M., and Z. T.) read the interviews several times for immersing in the data and getting familiar with it. Line-by-line coding was then applied to generate the initial codes. These steps were performed manually by the three authors without using any computer programs. One author encoded each interview and the interview was then read by another author and encoded again. The individually-extracted codes were then integrated and modified, if necessary.
In the next step, by linking the codes together, their common patterns and concepts were extracted and potential themes and subthemes were identified, keeping the research questions in mind. The data related to the themes were then collected and examined to verify the accuracy of the themes and subthemes, which resulted in five final themes.
Several statements were selected from the interviews as examples and are reported in the results section. To preserve participants’ anonymity, their names and ages are not mentioned in the results; instead, they are represented by random numbers.
Taking into account comprehensiveness, homogeneity, and overlap, the components of the family members’ viewpoints on the nature of the disorder and the reasons for pharmacological treatment non-adherence were categorized into five themes, including knowledge about the disorder, information about the medications, information about the treatment and the respective role of the family, reasons for pharmacological treatment non-adherence, and strategies applied by families to enhance treatment adherence in the patients.
Each of the themes contained several subthemes, which were themselves made up of some open codes. These subthemes contained recurrent codes and concepts that shared a common meaning.
Table 3 presents the themes, subthemes and examples of some of the codes.
Theme one: knowledge about the disorder
Most interviewees did not have sufficient or accurate knowledge about the nature of BD-I, the signs and symptoms of depression and mania cycles, and the outcome of the disorder. They mentioned the lack of training or inadequate training (especially by healthcare providers) as the main cause of insufficient knowledge about BD-I. Additionally, most families did not have a good understanding of the etiology of BD-I.
Some of them considered BD-I as a genetic abnormality, while others considered factors such as adolescent maltreatment, parents’ unusual conditions during sexual intercourse, and the lack of proper training before parenthood as potential causes of BD-I.
Participant No. 5 (a patient’s wife): “I was told that he has a nervous problem.” Participant No. 3 (a patient‘s mother): "I have a theory about having babies. I think that not everyone should have children. The husband and wife should be screened and monitored for two years to see if they understand the matter clearly. Do you see these anomalies now? ... These shameful movies they watch … The person is not feeling well when raising their kid … From an Islamic point of view, from a human’s point of view, both the husband and wife need to be monitored. Their food and other things should also be monitored to see if they can have a healthy baby.”
Participant No. 7 (a patient’s mother): "Because this boy is always impressed by me, sometimes I tell myself, maybe I didn’t fully understand him during his puberty. Sometimes I blame myself, as he has said this many times. I always blame myself … . Sometimes he says, ‘You did this to me, that’s why I’m sick now and take drugs’. For example, when hitting puberty, in the first or second year of high school, he used to get up late and so he got to school very late. Then the school’s principal complained to me, ‘Why is he late again?’ And he says, ‘Why did you wake me up early in the morning? You did this to me.” Participant No. 10 (a patient’s mother), referring to her son's divorce: "That's why he's so broken.” Participant No. 11 (a patient’s sister): "Bipolar disorder has a genetic background. I think there would be no one out there who suffered from the disorder unless they got the genes. It is a genetic disorder, but it emerges when a patient experiences a series of shocking events. Well, some have higher potentials, such as those who get very angry. I mean, the anger itself is not part of the disorder, but in angry people, shocking events affect the patient more rapidly.”
Theme two: information about the medications
Many family members had a misconception about the treatment of the disorder and the effects of psychotropic medications on the patients. In other words, they were unable to accurately identify the therapeutic effects of the administered medications and the time it took for the patients to show signs of improvement. Also, some participants were unaware of the side-effects of the prescribed medications. Some mentioned side-effects like memory loss and drug addiction; however, almost all the participants believed that pharmacological treatment is necessary for the patients despite the side-effects.
Participant No. 1 (a patient’s mother): "The problem of her running away from home with her boyfriend was a big burden for us, but as the prescribed meds began to show their effectiveness, this problem was gradually solved and we finally managed to put up with her aggressiveness and other problems. That is, we were saying to ourselves, ‘This is a period of angriness; we had better not said this, not done that’... We thought the medication was working. But now they’ve told me, ‘No, your patient has not recovered at all, has not been cured.”
Participant No. 1 (a patient's mother): "Her first psychiatrist, who has been visiting her for eight years, was frequently asking if she studies, watches TV or goes to work at all. ‘Whenever she goes back to these routines, then she has recovered,’ the therapist would say. Recently, she’s always been saying, ‘I would love to go to work’ and so on. Once, her employer told her to do some cleaning, and she had responded, ‘I’m not your servant.’ She suddenly broke it off and said, ‘I won’t go to work anymore.’ She didn’t sleep at all, saying, ‘I work so much, but I don’t feel exhausted at all.’ We were also excited and thought ‘Yeah, so this doctor's meds have been good; she’s getting back to normal, she’s working,’ She was frequently organizing her closet, like an obsession.”
Participant No. 3 (a patient’s mother): “I can’t remember the side-effects but I’ve heard about them in classes. My daughter is taking lithium now but she gets these chills. Her stomach is not well. Its side-effects are such that they affect her memory. However, when we compare the pros and cons, we have to take it. "
Theme three: information about the treatment
The regular intake of medications, stress control, work, exercise, regular visits to a psychiatrist or psychologist, and the need to provide insight into the patient’s illness through education were noted by the families in this part. Some participants believed that psychotherapy sessions cannot help treat this disorder while some had completely false or superstitious beliefs about treatment of the disorder.
Participant No. 4 (a patient's son): "Our patient doesn’t accept justifications. When you bring them to classes and convince them that ‘You are sick, and you have to take this medication because of this and that, and we have evidence that you have this disorder,’ and then we show it to them, prove it like in the movies, say that this disorder is serious because of so and so reasons, I think, it would be much easier.”
Participant No. 1 (a patient’s mother): "They sent us to get counseling. Of course, my daughter did not cooperate and didn’t come with. So, I got an appointment under my name to get information and find out how to deal with this disorder. Then the psychologist said, 'No, your daughter is diagnosed with bipolar disorder; this is an acute illness. Counseling does not work for her. She should take medications –a lot of them. And since the doc said those words, we withdrew from counseling altogether.”
Participant No. 5 (a patient’s wife): "My mother-in-law says, ‘If God gives him a baby, he’ll be fine.’ Because his ex-wife also failed to bear a child for him.”
Theme four: information about the role of the family in the treatment
Most families defined their role as helping the patient recover and adhere to their treatment, reminding them to take the medications, encouraging them to go to the doctor, not leaving them alone, and doing whatever they wanted to do so that things went as the patient wished. The patients also appeared to feel guilty when their families tried to comfort them, and this pattern was observed in several of the participants in this study.
Participant No. 6 (a patient’s husband): "We should put up with her, love her, not argue about what she says, listen to her, get her to do exercise to keep busy. I'm here now and I brought her with me too instead of leaving her alone to think about stuff.”
Participant No. 2 (a patient’s mother): "You should be good to them, listen to them, make home a peaceful environment, and not argue.”
Participant No. 8 (a patient’s wife): “I don't know. If he just thinks that everything is okay, all will be okay; but such feelings don’t last forever.”
Participant No. 2 (a patient’s mother): "I tell him to take his meds on time … Say, ‘Let's go to the park to take a look around ... Don't stay at home too much. God is merciful; it won’t be that bad’ … I talk to him, I comfort him sometimes, tell him that I’m ill too because I feel your pain.’ I really do. I’ve been crying alone at home many times. God, what will happen at the end?"(She cries).
Theme five: reasons for pharmacological treatment non-adherence
As for this theme, the participants noted issues that were mostly about the comments made by other people, including relatives or care-providers, such as doctors or specialists in other disciplines. An interesting observation was made by a participant who mentioned a celebrity talking on TV about the inefficiency of medications; following these comments, the patient had stopped taking his medications. Another issue was that the families’ constant changing of the patient’s physician contributed to their medication non-adherence. Another reason noted for non-adherence was that the patients did not suffer from mania symptoms and found that it was not so crucial for them to take the medications. Additionally, some patients reported the physical discomfort and weakness (e.g., impotence) experienced as side-effects of the prescribed medications a reason for their medication non-adherence.
Participant No. 2 (a patient’s mother): "She didn't take the meds for seven to eight months. Her friend had told her ‘Your eyes look different. When you take the medicine, your eyes turn into a strange shape. Get rid of them.’ After seven months, her disease relapsed.”
Participant No. 6 (a patient’s husband): "If we go to a party somewhere and someone asks her, ‘Oh, you take drugs?’ … But that person is not aware of the matter, cause she might look all well, and that person doesn’t know what’s actually happening in my wife’s mind, who then has to admit that she is alright."
Participant No. 7 (a patient’s mother): "At one point at work, some colleagues told him, ‘You will become addicted to the medicines, you will get sick.’ Then, he put the medicines aside and became pessimistic about his work. ‘This job has made me sick,’ so he said and left his job all of a sudden. He had a great job, not a difficult one. He could manage it by himself very easily.”
Participant No. 3 (a patient’s mother): “My son had gone to a doctor to remove the corn on his feet. The doctor had checked his medicine prescriptions and asked, ‘What are these you’re taking? You won’t be able to conceive a baby in the future. It’ll affect you poorly’ and so on. My son keeps repeating what the doctor told him.”
Participant No. 1 (a patient’s mother): "That emergency nurse who came to our house told us to change her doctor. Since then, she has kept repeating this sentence. She threw out all her medicines.”
Participant No. 3 (a patient’s mother): “Since the beginning of the new year, he’s began to no longer take his medications. In Khandevaneh, Footnote 1 Mr. Mehran Ghafourian (a famous Iranian actor) said, ‘I was in a bad mood ... I had depression. I put the medications aside and started exercising.’ My son stopped taking his medicines on hearing those words. I asked him many times to go see a doctor but he said no. He continued to not take his medicines and then his disorder worsened. He was frequently beating us up until we took him to the hospital with the help of the police.”
Participant No. 3 (a patient’s mother): “There was a child psychiatrist on a TV talk. We took our son to her office. We used to visit a counselor as well. The psychiatrist prescribed him some medications. We didn’t know what the medications were. He was taking his medicines. In the middle of therapy, we stopped it. Then, my son-in-law, who is a doctor, said ‘Dr. A -his professor- is a very good doctor.’ My son used to go to Dr. A. earlier when he was a college student. He was taking medicines and he believed in him so much. Then again, my eldest daughter, who is a physician, said ‘Dr. B. is a very helpful therapist. All the doctors, engineers, and educated people go to visit him.’ Then he went there ... And two years ago, I took him to Dr. S. too, to help him get rid of his substance abuse." (This participant named seven different doctors).
Participant No. 4 (a patient’s son) discussed the reasons for the patient’s refusal to take the medications and said: "Well, he doesn't actually believe in the disorder being a real one (in the manic episode). Maybe now he takes the pill in front of you, but you know that it is not something that bothers him. You take pills more easily if you have actual pain, but when you don’t, you ask yourself ‘Why do I have to take all these pills?”
Participant No. 11 (a patient’s sister): “We can note the poor behaviors of those around him. He considers any weaknesses he experiences (e.g., sexual problems) a side-effect of the medicines he’s taking. And he’s linking everything to the medicines and thinking they’re going to make him different from the others.”
The findings of this study regarding the viewpoints of the family members of patients with BD-I were categorized into five themes. Although qualitative studies do not allow for the identification of the extent and relative importance of every condition, recurrent themes and concepts stated by the participants at different individual and social levels were extracted.
Research suggests that there is a relationship between families’ knowledge and beliefs about the disorder and the patients’ medication adherence [ 12 ]. The attitudes and knowledge of the family members have a significant influence on the patient’s own beliefs and attitudes and affect the patient’s decision about treatment compliance [ 18 ]. In agreement with previous studies [ 19 , 20 ], the family caretakers in this study were shown to lack sufficient information and knowledge about the nature of BD-I. In addition, many participants had inaccurate or false information and insisted on these false beliefs. A review study on treatment acceptance found that brief interventions focused on relapse prevention and psychoeducation-based interventions have the greatest impact on relapse prevention [ 21 ]. Maintaining the patients’ circadian rhythms (especially sleep rhythm), controlling activity levels, verifying and controlling initial symptoms of mania and depressive episodes, and not using narcotics or stimulants have been recommended in approved psychotherapy protocols for bipolar patients [ 22 ]. Nonetheless, the participants in this study did not discuss any of these important factors. The lack of knowledge about these important issues among families can have a significant impact on relapse and treatment non-adherence in the patients. These points need to be further emphasized in training patients’ families.
In a qualitative study on bipolar patients and their families, Peters, Pontin, Lobban, and Morriss [ 23 ] found that the viewpoints of patients and their families play an important role in managing the disorder; however, the families usually get despondent about participating in this process, and their perception was that some mental health workers believe that family involvement makes their work more complicated. Meanwhile, the present study showed that, in Iran, families do not have enough information about their role in preventing disorder relapse and attribute their patient’s relapse only to factors such as medication withdrawal, unemployment, lack of community support, and financial problems. Most of them believed that if everything goes as the patient wishes, the disorder will not relapse.
Furthermore, the participants did not have adequate information about the non-pharmacological treatment options available for this disorder and the role that psychologists can play in helping the patients enhance their medication adherence and prevent the symptoms of relapse. A variety of behavioral, cognitive, and emotion-focused interventions are used in the management of bipolar disorders [ 22 ]. Nevertheless, the participants did not have sufficient knowledge about these treatments. The observation that many psychologists in Iran appear unwilling to participate in the treatment of bipolar disorder patients seems to play a role in this lack of knowledge. According to Farhoudian et al. [ 24 ], only about 1.5% of all the studies on psychiatric disorders conducted in Iran between 1973 and 2003 involved bipolar and cyclothymic patients. In a qualitative study on bipolar-II patients and their families, Fisher et al. [ 25 ] found that the number of resources available to patients for deciding about their treatment has increased and their priorities have been given increasing attention; yet, the patients’ and their families’ preferences are not fully considered.
Similar to the studies carried out by Jönsson, Wijk, Skärsäter & Danielson [ 26 ] and Shamsaei, Mohamad Khan Kermanshahi, and Vanaki [ 27 ], in the present study, the patients and their families were struggling with the acceptance, understanding, and management of the disorder. According to the participants, the families’ lack of insight into the patients’ disorder contributed significantly to their medication non-adherence. This finding is in line with Scott and Pope’s [ 28 ] research, but Delmas, Proudfoot, Parker, and Manicavasagar [ 29 ] stated that the rejection of treatment is a complex issue that depends on various factors.
Some of the results of this study are consistent with the findings reported by Clatworthy, Bowskill, Rank, Parham, and Horne [ 8 ], who noted that deliberate treatment non-adherence is associated with factors such as patients’ concerns about the prescribed medications and their side-effects in the case of continuous consumption. Proudfoot et al. [ 30 ] stated that the side-effects of medications, coping with unpleasant symptoms, the extent of awareness about the nature of the disorder, and the reactions to it as well as the stigma associated with the disorder affect the patient’s life path. Besides, these symptoms have a permanent impact on the disorder relapse [ 31 ]. The findings showed that the interaction of the disorder, patient, medications, psychiatric attitude, and cultural attitude with non-compliance is very complex [ 32 ].
In addition to the themes mentioned, there were some interesting results concerning the response process in all the interviews. For example, the majority of the participants only reported symptoms of the manic episode, while two major studies [ 33 , 34 ] have shown that people with bipolar I and II (especially type II) disorders spend most of their symptomatic days with depression. Patients suffer greatly during the depressive episodes but have elevated or irritable moods during the manic episode; in contrast, families find the mania symptoms more annoying and disruptive to themselves. This duality can negatively impact reaching a common understanding with the patient about visiting the doctor and taking medications. Moreover, the fact that some families do not have enough information about the depressive episode can eventuate in neglecting the patient’s need to take medications during this phase, which can then adversely affect medication adherence. These results are somewhat contradictory to the results of a previous study [ 29 ], which reported that both patients and their family members report symptoms of mania and hypomania to their physicians less often, as some of them enjoy the manic symptoms. Family members feel relieved when they see that their patient is happy and shows mania symptoms. A major cause of this discrepancy in findings may be the differences in the study populations. While Delmas et al. [ 29 ] studied patients with bipolar I and II, the present study examined only patients with BD-I. The discrepancy may also partially originate from cultural differences. It seems that when there is a pattern of greater attention to objective and apparent symptoms, very important mental symptoms such as suicidal thoughts, whether during the mania or depressive episode, are neglected by families.
This study showed that families with a higher educational and socioeconomic status tend to seek psychiatric care from different psychiatrists. Frequently changing the treating psychiatrist can cause treatment non-adherence in the patients. Furthermore, as the family members of such patients falsely think that they have greater medical information, they are more likely to encourage the patient to stop taking their prescribed medications.
A major limitation of this study was that most participants were the mothers of the patients, as it was hard to find other family members of the patients to participate in the study. For example, only one child of a patient and one sister were among the participants. Also, all the participants were from Tehran and were selected from one hospital; therefore, the generalization of the results to other cities in Iran should be pursued with caution.
The authors suggest using the findings of this qualitative study regarding the knowledge of the family members of patients with bipolar I disorder (BD-I) as well as the dominating cultural beliefs to design further quantitative studies. The quantitative assessment of individual, familial, and social reasons for treatment non-adherence is also a recommendation for future research. Conducting similar studies on the family members of patients with other types of bipolar disorder with an attention to the different processes and outcomes involved is also recommended. Since there are different ethnicities and subcultures in Iran, the results obtained by examining the residents of the country’s capital city cannot be generalized to the population of other cities and towns, and it is necessary to repeat the study in other populations in order to get familiar with other viewpoints in Iran.
Overall, the results of this study contribute to the emerging qualitative research on bipolar disorder and provide the readers with an insight into the viewpoints of the family members of patients with BD-I. Some inaccurate information might have been observed in participants’ statements due to some deeply-rooted cultural attitudes and beliefs and their correction may require extensive interventions.
The results of this study can be used to compile educational content for patients with bipolar disorder and their families as well as for psychologists, psychiatrists, psychiatry assistants, and hospital health workers.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
A popular comedy show on Iranian television
Diagnostic and statistical manual of mental disorders. Fifth edition (DSM-5). Arlington: American Psychiatric Association; 2013.
Kaushik P, Bhatia M. Burden and quality of life in spouses of patients with schizophrenia and bipolar disorder. Delhi Psychiatry J. 2013;16(1):83-9.
Maji KR SMSRKS, Maji KR, Sood M, Sagar R, Khandelwal SK. No Title. 2012 Mar 18 [cited 2020 mar 16];58(2). Available from: http://www.ncbi.nlm.nih.gov/pubmed/21421638 .
Zergew A, Hailemariam D, Alem A, Kebede D. A longitudinal comparative analysis of economic and family caregiver burden due to bipolar disorder. Afr J Psychiatry. 2008;11(3):191–8.
Article Google Scholar
Shirkhoda SA. The investigation of the amount of cost for bipolar disorder type I and its related factors during the 1-year follow-up for the hospitalized patients in Iran educational-therapeutic psychiatric center [dissertaion]. Iran University of Medical Sciences ;2014.
Jönsson PD, Skärsäter I, Wijk H, Danielson E. Experience of living with a family member with bipolar disorder. Int J Ment Health Nurs. 2011;20(1):29–37.
Shabani A, Ahmadzad-Asl M, Zangeneh K, Teimurinejad S, Kokar S, Taban M, et al. Quality of life in patients with bipolar I disorder: is it related to disorder outcome? Acta Med Iran 2013:51(6):386-93.
Clatworthy J, Bowskill R, Rank T, Parham R, Horne R. Adherence to medication in bipolar disorder: a qualitative study exploring the role of patients’ beliefs about the condition and its treatment. Bipolar Disord 2007;9(6):656-64.
Sharifi A, Shabani A, Ahmadzadasl M. The pattern of adherence in patients with bipolar I disorder; an eight weeks study: Iranian Journal of Psychiatry and Behav Sci 2009;3(2):39-43.
Shabani A, Eftekhar M. Non Compliance After First Episode of Manic or Mixed Mood State: A 17-Month Follow-up. 2007;1(2):46-49.
Tacchi M-J, Scott J. Improving adherence in schizophrenia and bipolar disorders: Wiley; 2005;7:24-31.
Velligan D, Weiden P, Sajatovic M, Scott J, Carpenter D, Ross R, et al. Expert Consensus Panel on Adherence Problems in Serious and Persistent Mental Illness. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. J Clin Psychiatry 2009;70(suppl 4):1-46.
Shabani A, Sobhani S, Tahmasebi N, Ghahramani S, Dejman M: How family caregivers of patients with bipolar disorder conceptualize caring problems: a qualitative study, unpublished.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19(6):349-57.
Fusch PI, Ness LR. Are we there yet? Data saturation in qualitative research. Qual Rep. 2015;20(9):1408.
Clarke V, Braun V. Using thematic analysis in counselling and psychotherapy research: A critical reflection. Couns Psychother Res 2018;18(2):107-10.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3(2):77-101.
Chakrabarti S. Treatment-adherence in bipolar disorder: a patient-centred approach. World J Psychiatry 2016;6(4):399.
Shamsaei F, Mohammadkhan Kermanshahi S, Vanaki Z. Survey of Family Caregiver Needs of Patients with Bipolar Disorder. Avicenna J Clin Med 2010;17(3):57-63.
Rahmani F, Ebrahimi H, Ranjbar F, Asghari E. The effect of group psychoeducational program on attitude toward mental illness in family caregivers of patients with bipolar disorder. Hayat. 2016;21(4):65-79.
MacDonald L, Chapman S, Syrett M, Bowskill R, Horne R. Improving medication adherence in bipolar disorder: A systematic review and meta-analysis of 30 years of intervention trials. J Affect Disord 2016;194:202-21.
Wright JH. Cognitive-behavior therapy for severe mental illness: An illustrated guide: American Psychiatric Pub; 2009.
Peters S, Pontin E, Lobban F, Morriss R. Involving relatives in relapse prevention for bipolar disorder: a multi-perspective qualitative study of value and barriers. BMC Psychiatry 2011;11(1):172.
Farhoudian A, Rad Goodarzi R, Rahimi Movaghar A, Sharifi V, Mohammadi MR, Sahimi Izadian E, et al. Trend of Researches in the Field of Psychiatric Disorders in Iran. Iran J Psychiatry Clin Psychol 2007;12(4):327-36.
Fisher A, Manicavasagar V, Sharpe L, Laidsaar-Powell R, Juraskova I. A qualitative exploration of patient and family views and experiences of treatment decision-making in bipolar II disorder. J Ment Health 2018;27(1):66-79.
Jönsson PD, Wijk H, Skärsäter I, Danielson E. Persons living with bipolar disorder—their view of the illness and the future. Issues Mental Health Nurs 2008;29(11):1217-36.27.
Shamsaei F, Mohamad khan Kermanshahi S, Vanaki Z. Meaning of Health from the Perspective of Family Member Caregiving to Patients with Bipolar Disorder. Journal of Mazandaran University of Medical Sciences. 2012;22(90):52-65.
Scott J, Pope M. Nonadherence with mood stabilizers: prevalence and predictors. J Clin Psychiatry 2002;63(5):384-390.
Delmas K, Proudfoot J, Parker G, Manicavasagar V. Recoding past experiences: A qualitative study of how patients and family members adjust to the diagnosis of bipolar disorder. J Nerv Ment Dis 2011;199(2):136-9.
Proudfoot JG, Parker GB, Benoit M, Manicavasagar V, Smith M, Gayed A. What happens after diagnosis? Understanding the experiences of patients with newly-diagnosed bipolar disorder. Health Expect 2009;12(2):120-9.
Crowe M, Inder M, Carlyle D, Wilson L, Whitehead L, Panckhurst A, et al. Feeling out of control: a qualitative analysis of the impact of bipolar disorder. J Psychiatr Ment Health Nurs 2012;19(4):294-302.
Weiss RD, Greenfield SF, Najavits LM, Soto JA, Wyner D, Tohen M, et al. Medication compliance among patients with bipolar disorder and substance use disorder. J Clin Psychiatry 1998;59(4):172-4.
Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry 2002;59(6):530-7.
Judd LL, Schettler PJ, Akiskal HS, Maser J, Coryell W, Solomon D, et al. Long-term symptomatic status of bipolar I vs. bipolar II disorders. Int J Neuropsychopharmacol 2003;6(2):127-37.
Download references
Acknowledgements
The authors express their gratitude to all the staff of Iran Psychiatry Hospital for their generous cooperation in the study.
This research is funded by the Mental Health Research Center of Iran University of Medical Sciences (grant number 95–01–121-27963).
The views expressed are those of the authors and not necessarily those of the Mental Health Research Center of Iran University of Medical Sciences. The funders had no role in the study design, data collection and analysis, interpretation, decision to publish or the writing and preparation of the manuscript.
Author information
Authors and affiliations.
Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences, Tehran, Islamic Republic of Iran
Nasim Mousavi & Marzieh Norozpour
Department of Psychology, Faculty of Psychology and Educational Sciences, University of Tehran, Tehran, Islamic Republic of Iran
Zahra Taherifar
Faculty of Behavioral Sciences and Mental Health, Tehran Psychiatry Institute, Iran University of Medical Sciences, Tehran, Islamic Republic of Iran
Morteza Naserbakht & Amir Shabani
You can also search for this author in PubMed Google Scholar
Contributions
NM, MN and ASH conceived the study idea and design. NM, and MN conducted the interviews. NM, MN and ZT conducted transcription and data analysis. NM, MNA and ZT interpreted and presented the results, and contributed to the manuscript. ASH supervised the research activities and contributed to the interpretation of results. NM, MN and ZT wrote the manuscript. All authors have read, edited and approved the final manuscript for submission.
Corresponding author
Correspondence to Marzieh Norozpour .
Ethics declarations
Ethics approval and consent to participate.
This research has been approved by the Research Ethics Committee of Iran University of Medical Sciences (Code of Ethics: IR.IUMS.REC 1395.95–01–121-27963). Written informed consent was obtained from all the research participants prior to participating in the study.
Consent for publication
Not applicable as no personal information is provided in the manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mousavi, N., Norozpour, M., Taherifar, Z. et al. Bipolar I disorder: a qualitative study of the viewpoints of the family members of patients on the nature of the disorder and pharmacological treatment non-adherence. BMC Psychiatry 21 , 83 (2021). https://doi.org/10.1186/s12888-020-03008-x
Download citation
Received : 20 March 2020
Accepted : 08 December 2020
Published : 08 February 2021
DOI : https://doi.org/10.1186/s12888-020-03008-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Bipolar I disorder
- Treatment non-adherence
- Family psychological education
- Qualitative study
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Media Center
- Events & Webinars
- Healthy Minds TV
- Email Signup
- Get Involved
- Anxiety Disorders
- Attention-Deficit Hyperactivity Disorder (ADHD)
- Autism Spectrum Disorder (ASD)
Bipolar Disorder
- Borderline Personality Disorder (BPD)
- Eating Disorders
- Mental Illness (General)
- Inaccessible
- Obsessive-Compulsive Disorder (OCD)
- Post-Traumatic Stress Disorder (PTSD)
- Schizophrenia
- Suicide Prevention
- Other Brain-Related Illnesses
- Basic Research
- New Technologies
- Early Intervention/ Diagnostic Tools
- Next Generation Therapies
- Donate Today
- Make a Memorial/Tribute Gift
- Create an Event/Memorial Page
- Find an Event/Memorial Page
- Make a Stock/Securities Gift/IRA Charitable Rollover Gift
- Donate Cryptocurrency
- Other Giving Opportunities
- Monthly Giving
- Planned Giving
- Research Partners
- Donor Advised Funds
- Workplace Giving
- Team Up for Research!
- Sponsorship Opportunities
$35.4M Awarded to Bipolar Disorder Research since 1987
The Latest Research Discoveries
Posted: May 09, 2024
Neural Activation Patterns That May Help Distinguish Elevated Mania/Hypomania Risk From Depression Risk in Young People

Posted: May 02, 2024
Dialectical Behavior Therapy Decreased Suicide Attempts in Youths With Bipolar Disorder

Posted: February 15, 2024
Unique Neural Activation Pattern in People With Co-Occurring Bipolar Disorder and Alcohol Use Disorder Points to Future Treatment Targets
Posted: February 01, 2024
In Young Psychosis Patients, Study Reveals Changes Over Time in Brain Molecules Called Metabolites

Posted: January 11, 2024
In Trial, Magnetic Seizure Therapy (MST) Was Just as Effective as Electroconvulsive Therapy (ECT) in Treating Severe Depression, and Likely Safer

Posted: May 16, 2023
Research Suggests How Working Memory Retains, Manipulates, and Deletes Specific Items

Posted: December 14, 2022
Lumateperone, an Antipsychotic, is Tested in a Phase 3 Trial for Major Depressive Episodes in Bipolar I and II Disorders

Posted: December 13, 2022
Precise Imaging Reveals How a Key Receptor's Signaling Is Modulated—A Spur to Improving Psychiatric and Other Drugs

Simple Parent Questionnaire Can Help Doctors Track Mood Symptom Trajectory in Youths at High Risk for Bipolar Disorder

Posted: August 12, 2021
Obesity Is a Risk Factor for Brain-Structure Changes in Schizophrenia and Bipolar Disorder, 2 Studies Show

Posted: April 29, 2021
Study Points to Importance of Cognitive Flexibility in Children Diagnosed with Bipolar Disorder

Posted: April 22, 2021
Largest Genome Study to Date of Anxiety Reveals New Risk Variants and Suggests Possible Biological Mechanisms
Posted: February 18, 2021
In Schizophrenia, Differences in the Brain’s Energy Pathways Suggest Possible New Treatment Target

Posted: November 19, 2020
Psychotherapy in Addition to Medication Helps Bipolar Disorder Patients Avoid Relapse and Manage Their Symptoms, Study Determines

Posted: November 12, 2020
Study Reveals Adults With Mental Disorders Are At Significantly Higher Risk of COVID-19 and Have Poorer Outcomes

Posted: July 02, 2020
Study Finds Changes in the Treatment of Bipolar Disorder Over 20 Years

Posted: April 30, 2020
Brain Activity While Anticipating a Working-Memory Task Could Help Distinguish Depression in Bipolar Disorder from Major Depression
Posted: March 31, 2020
Connecting the Dots, From Genes to Brain Biology to Disorders
Taking the Next Step in Understanding the Genetic Roots of Mental Illness

Posted: February 20, 2020
Maternal Inflammation Early in Pregnancy May Raise Offspring’s Psychosis Risk

Posted: November 14, 2019
After 60 Years, Study Finds Children of Mothers with Bacterial Infections During Pregnancy Have Elevated Psychosis Risk

Posted: August 15, 2019
Study Finds Lithium Has Advantages Over Other Mood Stabilizers in Youths with Bipolar Disorder

Posted: August 01, 2019
A Way of Predicting if New Psychosis Patients Will or Won’t Respond to Standard Treatment

Posted: June 27, 2019
A Rarely Studied Brain Structure Provides New Clues About Psychosis

Posted: June 20, 2019
FDA Approves Cariprazine for Depression in Bipolar I Disorder

Posted: March 19, 2019
A Medicine That Treats Mania Also Shows Effectiveness in Treating Depression in Bipolar Disorder

Posted: February 25, 2019
Long-term Study Reveals How Bipolar Disorder Emerges in High-Risk Youth
Posted: October 29, 2018
Researchers Train Computers to Identify a Biological Signature of Bipolar Disorder
Posted: October 17, 2018
A Revealing Genetic Comparison of Schizophrenia and Bipolar Disorder

Posted: September 17, 2018
A New Understanding of Risk for Bipolar Disorder

Posted: August 02, 2018
Evidence Links White Matter Patterns to Cognitive Performance in Bipolar Disorder
Posted: April 10, 2018
Certain Patterns of Brain Activity May Protect Against Bipolar Disorder
Posted: April 03, 2018
Large Gene Expression Study Sheds Light on Causal Factors in Five Brain Disorders

Posted: March 20, 2018
Molecular Picture Points the Way to Better Antipsychotic Medications
Posted: March 12, 2018
NAC Medication Improves Working Memory in Schizophrenia and Bipolar Patients with Psychosis

Posted: February 26, 2018
Social Impairment Levels Remain Stable in Patients with Psychotic Disorders

Posted: January 23, 2018
Animal Studies Suggest a Strategy for Developing New Bipolar Disorder Treatments

Posted: January 18, 2018
Brain Imaging Suggests Visual Processing Is Disrupted in People with Bipolar Disorder

Posted: October 16, 2017
Study Shows Exposure to Bright Light at Midday Reduces Depression in Patients with Bipolar Disorder
Posted: September 07, 2017
New Knowledge about How Lithium Reduces Mania in Bipolar Disorder Opens Research Path to More Effective Treatments

Posted: August 21, 2017
Large Study Showed Lithium Lowered Suicide Risk in Patients with Bipolar Disorder

Posted: July 11, 2017
Brain Structure Study in Children Suggests Biological Overlaps in Disorders Usually Considered Distinct

Posted: June 19, 2017
Trial Finds Rapid Reduction in Suicidal Thoughts after Ketamine Treatment in Patients with Bipolar Disorder
Posted: April 26, 2017
Deep Transcranial Magnetic Stimulation (dTMS) Could Help Treat Bipolar Depression

Posted: April 17, 2017
Study Compares 3 Different Treatments for Bipolar II Disorder
Posted: March 03, 2017
Combinations of Genetic Risks are Linked with Abnormal Processing of Emotional Information in Bipolar Disorder
Posted: February 28, 2017
Parts of the Brain’s Hippocampus are Diminished in Size in People with Bipolar Disorder

Posted: February 21, 2017
Brain Abnormalities Linked to Suicidal Behavior in Young People with Bipolar Disorder

Posted: January 20, 2017
Adolescents With Bipolar Disorder Not More Likely to be Overweight or Obese
Posted: December 02, 2016
Emotional Disorders Share Disruptions to Brain’s White Matter, Imaging Reveals

Posted: November 02, 2016
Researchers Pinpoint Neurons That Cause and Maintain Wakefulness

Posted: September 30, 2016
A Breakthrough in the Effort to Develop a Fast-Acting Antidepressant
Posted: August 30, 2016
Study Finds Some Autism and Schizophrenia Related Genes May Also Be Involved in Bipolar Disorder

Posted: August 19, 2016
New Tool Calculates Patients’ Personal Psychosis Risk
Posted: August 09, 2016
Long-term Lithium Treatment May Prevent Shrinking of Hippocampus in Bipolar Disorder Patients

Posted: August 01, 2016
Study Identifies Separate Brain Network Disturbances in Bipolar Disorder States

Posted: June 23, 2016
Exercise May Treat Cognitive Symptoms in Bipolar Disorder By Restoring Brain Activation Patterns

Posted: May 16, 2016
Blood Markers Indicate High Inflammation Levels in People with Schizophrenia, Bipolar Disorder and Depression
Posted: May 01, 2016
New Biotypes Classify Psychosis Cases According to Measurable Biological Features

Posted: April 05, 2016
Immune Activity During Pregnancy Tied to Neuronal Defects, Anxiety, and Cognitive Impairments
Posted: March 22, 2016
Large Study Ties Genes to Variable Lithium Response in Bipolar Disorder

Posted: February 22, 2016
Enhanced Brain Plasticity May Help Overcome Predisposition to Bipolar Disorder
Posted: November 19, 2015
Antipsychotic Treatment for Bipolar Disorder Not Always Effective After Six Months
Posted: October 06, 2015
Measuring Gene Activity in the Blood Could Help Diagnose Bipolar Disorder
Posted: July 31, 2015
Genes Linked to Abnormal Brain Waves in Schizophrenia, Psychotic Bipolar Disorder
Posted: June 22, 2015
D-Serine, A Potential Schizophrenia Treatment, May Guide Some Early Brain Development
Posted: June 11, 2015
Parent’s History of Suicide Attempts Helps Predict Suicide Attempts In Children
Looking For Clues in Reward Circuits of Bipolar and Depressed Patients
Posted: June 01, 2015
Large-Scale Gene Mutation Disrupts Brain Development During Key Period
Posted: March 03, 2015
Lithium Linked to Lower Incidence of Dementia in Older People with Bipolar Disorder
Posted: February 17, 2015
For Children and Adolescents with Bipolar Disorder, a New Antidepressant Combination Treatment
Posted: February 03, 2015
In Bipolar Disorder, a Chemical Signal of Abnormal Metabolism
Posted: January 30, 2015
Multiple Psychiatric illnesses Share the Same Perturbed Biological Pathways
Posted: December 23, 2014
New Approach Provides Path Toward Functional Recovery in Bipolar Disorder
Posted: October 23, 2014
What Causes the Placebo Effect in Clinical Trials of Antipsychotic Medications?
Posted: October 15, 2014
Fast-Acting Antidepressant Restores Ability to Experience Pleasure in People with Bipolar Disorder
Posted: September 29, 2014
International Collaborative Effort Develops the Beginnings of a Blood Test for Psychosis
Posted: September 09, 2014
Upcoming Keynote at Foundation’s DC Event Featured in Forbes Article
Mother discusses why she raises money for mental health research.

Posted: August 21, 2014
With New Technology, Researchers See How Faulty Human Brain Cells Develop
Posted: June 19, 2014
Gene Linked to Bipolar Disorder, Schizophrenia Plays Key Role in Brain Development
Posted: March 05, 2014
Making the Impossible Possible: The Challenges of Practicing Evidence-Based Psychiatry with a Focus on Bipolar Depression*
Posted: November 04, 2013
Watch Dr. Boris Birmaher’s Video: 2013 Colvin Prize for Outstanding Achievement in Mood Disorders Research
Watch dr. andrew nierenberg’s video: 2013 colvin prize for outstanding achievement in mood disorders research.
Posted: November 01, 2013
New Insight for Difficult-to-Treat Mania in Bipolar Disorder
Posted: October 24, 2013
Electrical Stimulation Can Improve Cognitive Performance―May Help in Schizophrenia, Bipolar Disorder
Posted: October 22, 2013
State of MD Supports Foundation Scientific Council Member’s Early Intervention in Psychosis Program

Posted: October 08, 2013

Defining Psychotic Disorders―Mood Disorders and Schizophrenia―by Symptom Course and Long-Term Outcome
Posted: October 04, 2013
Pre-Term Birth Associated with Higher Risk of Mental Illness, But Also for Siblings
Posted: August 26, 2013
NARSAD Grant-Funded Study Identifies Disrupted Brain Communication in Schizophrenia and Bipolar Disorder
Posted: August 20, 2013
Using Brain Imaging, NARSAD Grantee Identifies Predictor of Psychosis Treatment Effectiveness
Posted: July 31, 2013
Linking Brain Imaging With Genetics Helps Identify New Risk Profile for Depression
Posted: March 12, 2013
NARSAD Grantee Discovers Predictor of Psychosis in Bipolar Disorder, Schizophrenia
Posted: March 01, 2013
Current Progress in Developing More Effective Treatments for Bipolar Disorder
Posted: January 17, 2013
NARSAD Grantees Make New Discoveries About the Brain Circuitry of Bipolar Disorder
Posted: December 03, 2012
Karen Dineen Wagner Wins 2012 Colvin Prize for Mood Disorders Research
Posted: November 06, 2012
Eduard Vieta is Recognized for Outstanding Achievement in Mood Disorders Research
Posted: September 24, 2012
Premature Birth Heightens Risk for Mental Illness
Posted: August 22, 2012
NARSAD Grant-Funded Research Furthers Understanding of Causes of Bipolar Disorder
Posted: August 07, 2012
Addressing the Major Public Health Issue of Vascular Disease in Mood Disorders
Creating a new window to study synaptic (dys)function in brain and behavior disorders.
Posted: July 05, 2012
NARSAD Grant-funded Research Finds Links Between Schizophrenia, Bipolar and Autism
Posted: July 03, 2012
NARSAD Grantee Discusses Innovative Work to Understand and Better Treat Mental Illnesses
Posted: June 04, 2012
NARSAD Grant-Funded Research Finds Premature Birth Increases Risk for Mental Illness
Posted: April 18, 2012
Off-Balance Circadian Clocks and the Risk of Mood Disorders
Building careers, changing lives; q&a with david j. miklowitz, ph.d..
Posted: April 03, 2012
NARSAD Grantees Learning to Predict Likelihood of Mental Illness in Teenagers
Posted: January 23, 2012
Research News Update – Deep Brain Stimulation
Posted: January 11, 2012
NARSAD Grants Fund Breakthrough Bipolar & Depression Treatment
Posted: January 06, 2012
Foundation-funded Discovery: Early Childhood Immigration Linked to Psychotic Disorders
Posted: December 30, 2011
Basic Research and Novel Therapeutic Treatments Pave the Road to Cures for Mental Illness
Posted: November 22, 2011
VIDEO: 2011 Gloria Neidorf Memorial Lecture on Bipolar Disorder
Posted: November 15, 2011
The Challenge of Co-Morbidity: How to Treat Patients with Multiple Brain and Behavior Disorders
Posted: September 26, 2011
Understanding Why Identical Twins Are Not Carbon Copies in Mental Illness
Posted: September 22, 2011
Foundation Honors Scientists For Outstanding Achievements in Mental Illness Research
Posted: August 26, 2011
An Overview of Treatment Options for Bipolar Disorder
The diagnostic challenge: is it depression or bipolar disorder, new approach leads toward more effective bipolar treatments, using other disorders with similar symptoms to help unravel the genetic code of bipolar disorder.
Posted: July 14, 2011
Sharing Knowledge as We Unlock the Mysteries of Mental Illness
Posted: March 11, 2011
The NARSAD Feed: NARSAD Researchers in the News, Research Finds Bipolar Disorder is Under-Diagnosed in Some Countries, Talk Therapy Doesn’t Pay
Posted: February 01, 2011
New York Times Profiles NARSAD Investigator as ‘Master Virus Hunter’
Posted: December 09, 2010
The Most Avant-Garde Bipolar Disorder Researcher Found in Denmark … the NARSAD Outstanding Achievement in Mood Disorder Research Awarded to Dr. Lars Kessing
Posted: December 01, 2010
Understanding the Brain Physiology of Bipolar Disorder
Posted: April 01, 2010
Kiki Chang and Tara Peris: Helping Families Cope with Childhood Mental Illness
Key figures.

Bipolar disorder affects approximately 5.7 million adult Americans or about 2.8% of the U.S. population age 18 and older every year.*
* Source: National Institute of Mental Health

* Source: World Health Organization (WHO)
Featured Tweet
Brain imaging study reveals hippocampus shrinks in people with #bipolar disorder. TWEET
Meet a Researcher

Peter L. Franzen, Ph.D.
Associate Professor of Psychiatry, Psychology, and Clinical and Translational Science
University of Pittsburgh
2016 Independent Investigator Grant
Ask an Expert

Huda Akil, Ph.D.
Gardner Quarton Distinguished University Professor of Neuroscience and Psychiatry
Co-Director, Molecular and Behavioral Neuroscience Institute
2007 Goldman-Rakic Prize for Outstanding Achievement in Cognitive Neuroscience
In your work with the Pritzker Neuropsychiatric Research Consortium, have you uncovered any new genes that you think might be related to mental illnesses besides major depression?
- More Questions
Learn More About the Foundation
The Brain & Behavior Research Foundation is a global nonprofit organization focused on improving the understanding, prevention and treatment of psychiatric and mental illnesses.
Beginning in 1987, the Brain & Behavior Research Foundation was providing seed money to neuroscientists to invest in “out of the box” research that the government and other sources were unwilling to fund. Today, Brain & Behavior Research Foundation is still the leading, private philanthropy in the world in this space.
Meet the people who make up the Brain & Behavior Research Foundation. Our staff of experts, passionate Board of Directors, and Scientific Council which includes Nobel prize winners and chairs of psychiatric departments around the world.
Annual Report & Financials
We take our responsibility to our donors seriously and believe that our financial operations must be transparent. We're proud to say that 100% of your contribution for research is invested directly in research grants.
Frequently Asked Questions about the Brain & Behavior Research Foundation.
The latest news on brain and behavior research and issues that matter most to you.
Donations are welcome
100% of every dollar donated for research is invested in our research grants. Our operating expenses are covered by separate foundation grants.
The Brain & Behavior Research Foundation is a 501(c)(3) nonprofit organization, our Tax ID # is 31-1020010.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 10 May 2024
The role of bipolar disorder and family wealth in choosing creative occupations
- Barbara Biasi 1 , 2 ,
- Michael S. Dahl 3 , 4 , 5 &
- Petra Moser 2 , 6
Scientific Reports volume 14 , Article number: 10703 ( 2024 ) Cite this article
586 Accesses
8 Altmetric
Metrics details
- Human behaviour
- Risk factors
Research in psychology and medicine has linked mental health disorders, and particularly bipolar disorder (BD), to employment in creative professions. Little is known, however, about the mechanisms for this link, which could be due to biology (primarily through a person’s genes) or environmental (through socioeconomic status). Using administrative data on mental health diagnoses and occupations for the population of Denmark, we find that people with BD are more likely to be musicians than the population, but less likely to hold other creative jobs. Yet, we also show that healthy siblings of people with BD are significantly more likely to work in creative professions. Notably, people from wealthy families are consistently more likely to work in creative professions, and access to family wealth amplifies the likelihood that siblings of people with BD pursue creative occupations. Nevertheless, family wealth explains only a small share of the correlation between BD and creative employment.
Similar content being viewed by others
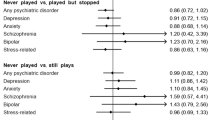
The effects of playing music on mental health outcomes
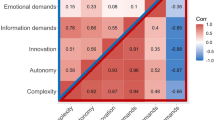
Genetic basis of job attainment characteristics and the genetic sharing with other SES indices and well-being

A comprehensive investigation into the genetic relationship between music engagement and mental health
Research in psychology and medicine has pointed to a link between mental health disorders and creative pursuits, such as employment in creative professions. For instance, studies of Swedish population data have found that writers (but not people in other creative professions) face an elevated risk of bipolar disorder (BD), schizophrenia, and depression 1 , 2 . Similarly, polygenic risk scores for individuals in Iceland indicate that people with an elevated genetic predisposition for BD and schizophrenia are more likely to work in creative professions 3 . [Polygenic risk scores measure a person’s genetic predisposition for a trait or disorder, abstracting from environmental factors ( https://www.genome.gov/Health/Genomics-and-Medicine/Polygenic-risk-scores ).]
Despite this evidence, less is known about the mechanisms that link creativity with mental health. One set of possible causes is neurobiological. Existing studies point to the importance of dopamine, a neurotransmitter that regulates our perception of pleasure and the ability to think and plan. Dopamine regulation is affected in people with mood disorders, such as BD 4 . At the same time, dopamine is related to divergent thinking 3 , 5 , which allows for greater freedom to pursue high-risk projects and fresh ideas that are essential for creative work 6 , 7 .
Another set of possible causes is environmental. There could be aspects of a person’s background—such as socioeconomic status—which influence both their likelihood of being in a creative profession and their mental health. For example children from families with income in the top percentile have been shown to be 10 times as likely to become inventors as those from below-median income families 8 . Similarly, 9 have emphasized the importance of exposure to role models and parental income 9 . Conversely, financial distress has been shown to negatively impact mental health 10 , 11 and increase the incidence of BD 12 , 13 , 14 and other mental health disorders. Access to specialized mental health care has also been shown to depend, at least in part, on a person’s socio-economic status 9 , 15 .
Connecting these insights from psychology and economics, we study the channels behind the observed link between mental health and creativity, with a focus on the role of socioeconomic factors such as parental wealth. We focus on BD, a prevalent “brain disorder that causes unusual shifts in mood, energy, activity levels, and the ability to carry out day-to-day tasks.”[ https://www.nimh.nih.gov/health/topics/bipolar-disorder/index.shtml , accessed November 22, 2019.] BD affects 1 in 11 people in the US population and 40 million people world-wide, creating major career costs for affected individuals 16 , 17 BD, however, has also been strongly and consistently associated with creative employment 2 , 3 , 18 . For instance, biographical evidence suggests that many exceptionally creative individuals were affected by BD, including visual artists such as Vincent van Gogh, writers such as Virginia Woolf, and composers such as Robert Schumann 18 . Our goal is to investigate this tension and explore a potential role of familial wealth in the connection between creativity and BD.
To perform this analysis, we use registry data on mental health diagnoses, creative employment, and parental wealth for the population of Denmark. These data include individual-level administrative records of mental health diagnoses and occupations for all 2,524,325 people who were active in Denmark’s labor force between 1995 and 2015. Family identifiers, available for 71 percent of the population, allow us to identify siblings of people with a mental health condition and observe family wealth. To define employment in creative professions, we implement definitions from psychology which include designers, university teachers (academics), visual artists, architects, display artists, performing artists, musicians, and photographers 2 , 3 , 19 .
We begin by revisiting the association between mental health and creativity. We compare the likelihood of creative employment among people with BD, their siblings, and the population. We find that while people with BD are 20 percent less likely to be active in any creative occupation than the population, they are 50 percent more likely to be composers and musicians. Occupations that people with BD are most likely to pursue, instead, include clerks, librarians, archivists and curators, as well as waiters and bartenders.
Notably, we also find that healthy siblings of people with BD are 11 percent more likely to work in creative professions, confirming the results for Sweden 1 . This finding is consistent with a biological explanation for the link between mental health and creativity. Siblings of people with BD may be affected by a milder (subthreshold) form of BD that eludes diagnosis and experience a greater penchant for divergent thinking, without suffering the adverse health effects of BD, which could lead them to successfully pursue creative employment 20 .
An increased likelihood of creative employment for siblings of people with BD, however, is also consistent with an alternative, socioeconomic explanation: people who grew up in wealthy families have better access to both medical care (including diagnoses for mental health disorders) and employment in creative professions (for instance, because they can afford specialized training required for these jobs). To investigate this alternative channel, we first examine whether people from wealthy families are more likely to hold creative jobs. Then, we test whether the link between mental health and creativity can be explained by differences in parental wealth.
Our results indicate a strong link between parental wealth and employment in creative professions. People from the top decile of the parental wealth distribution are 7 times more likely to work in creative occupations compared with people from the bottom decile. These findings extend existing results for patentees 1 , 2 to a broader set of creative occupations.
Nevertheless, the correlation between wealth and creative employment explains only a small portion of the correlation between BD and creativity. Differences in parental wealth can account for at most 8 percent of the correlation between creativity and mental health. Notably, the gradient between parental wealth and creative employment is stronger for siblings of people with BD than for the population. This suggests that environmental factors can reinforce the biological channel, even though they cannot fully explain the link between mental health and creativity.
Our paper contributes to two main strands of literature. The first has explored the link between mental health and creativity. The channels behind the BD-creativity link are still still poorly understood. Polygenic risk scores for BD and schizophrenia are correlated with elevated odds of creative employment in a sample of 86,000 people in Iceland 3 . Yet, polygenic risk scores explain less than 1 percent of these odds, suggesting a statistically significant but small role for biology. In Swedish administrative data, people who have been hospitalized with BD have been found to be over-represented in creative professions, while those with depression are not 1 . In a similar setting, people in creative professions—and particularly writers—are more likely to have BD, but not other psychiatric disorders 2 . Our study complements these works by analyzing the entire population of Denmark and by considering all people with a BD diagnosis, including those with less severe symptoms, not requiring hospitalization. In addition, the richness of our data and a broader classification of creative professions (which combines definitions previously used in the literature) allow us to explore the link between this condition and each creative occupation individually. Lastly, we investigate the role of what is perhaps the most powerful alternative explanation—socioeconomic status, which has been linked to creativity for inventors 1 , 2 .
Our paper also relates to research on the relationship between health and work, and occupational choice more specifically 21 , 22 . Most of this research considers occupational choice as a factor influencing health (for example through differences in the intensity of work between manual and white-collar jobs). Our research complements these analyses by investigating the link between a particular dimension of health—mental health—and the way it relates to occupational choice through biology and socioeconomic status.
BD and creative employment
People with bd are less likely to work in creative jobs.
First, we test whether people with BD are more likely to work in creative occupations compared with the population. Figure 1 reports occupation-specific estimates and 95-percent confidence intervals for the difference in the likelihood of holding a creative job between people with BD and the population, controlling for variation across calendar years, birth cohorts, and gender. We divide this difference by the population share of each occupation, so that estimates can be interpreted as percent differences (panel A of Table 1 reports the unscaled differences). These estimates indicate that people with BD are − 0.293 percentage points less likely to work in any creative occupation (significant at 1 percent, Table 1 , panel A, column 1). Compared with a population share of 1.474 percent, this implies that people with BD are 20 percent less likely to work in a creative occupation (Fig. 1 ).
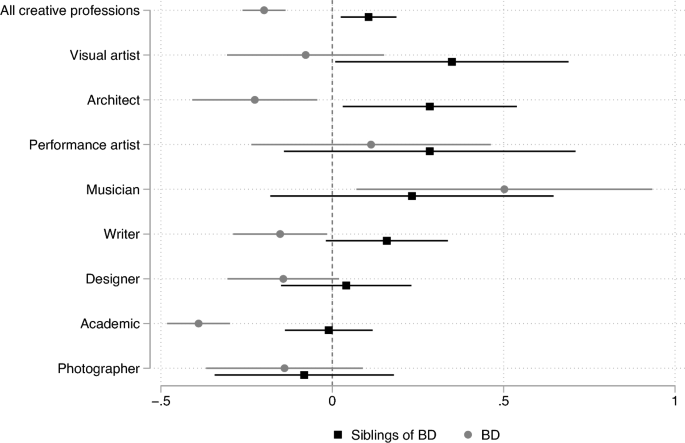
Share in creative occupations: people with BD and their siblings, compared with the population. Note OLS estimates (and 95-percent confidence intervals) of β in the equation creative it = β X i + γ F i + θ c(i) + τ t + ε it where creative it equals one if person i is employed in a creative profession in year t . In the BD series, X i is an indicator for people who have received at least one diagnosis of BD at least once. For siblings of BD , X i indicates siblings of people with BD . The variable F i is an indicator for females. A vector of cohort fixed effects θ c(i) controls for systematic differences in the propensity to hold a creative job across cohorts; a vector of year fixed effects τ t controls for differences over time. We report coefficients and confidence intervals as the share of the mean of the dependent variable. Standard errors are clustered at the individual level. Creative professions are listed in Appendix Table A2 , together with ISCO-4 codes.
Occupation-specific estimates reveal moderate heterogeneity in the share of people with BD across occupations. People with BD are 15 percent less likely to be writers, 39 percent less likely to be academics, 23 percent less likely to be architects, and 14 percent less likely to be designers (significant at 5, 1, 5, and 5 percent, respectively, Fig. 1 and Table 1 , panel A). People with BD are also 14 percent less likely to be photographers and 8 percent less likely to be visual artists, although these estimates are not statistically significant (with p-values of 0.55 and 0.53, respectively).
Notably, people with BD are 50 percent more likely to be musicians and composers (significant at 5 percent). This result is consistent with biographical evidence suggesting that prominent composers (including Berlioz, Brahms, Cherubini, Gluck, Mahler, Mendelssohn, Schubert, and Schumann) may have been affected by bipolar disorder 23 . Interestingly, people with BD are also slightly more likely to be performing artists (actors, dancers, choreographers, and directors), though this estimate is smaller and not statistically significant (11 percent, with a p-value of 0.47). [In contrast to our results and those of others 24 , people who are diagnosed with BD in Sweden are more likely to be writers, but not musicians.]
Healthy siblings of people with BD are more likely to be creative
If BD is associated with creativity through a genetic link, siblings may have a milder “subthreshold” form of BD that allows them to be more creative, without experiencing debilitating symptoms. Models of BD in molecular neuropsychiatry have proposed an inverted U-shaped relationship between the genetic risk for BD and creativity. Greenwood (2016, p. 200) 25 conjectures that “some aspects of the bipolar spectrum may confer advantages, while more severe expressions of symptoms negatively influence creative accomplishment.”
Our data indicate that siblings of people with BD are 11 percent more likely to work in creative professions compared with the population (Fig. 1 and Table 1 , panel B, column 1). Occupation-specific estimates imply that siblings of people with BD are 35 percent more likely to be visual artists, 28 percent more likely to be architects, and 16 percent more likely to be writers (Table 1 , panel B, significant at the 5, 5, and 10 percent level, respectively). Siblings are also 23 percent more likely to be musicians and composers than the population, even though this estimate is imprecise due to the small number of observations (with a p value of 0.27). These findings confirm the higher share of creative employment among siblings of people who have received in-patient treatment for BD in Sweden 1 .
Most frequent occupations for people with BD
Looking beyond creative professions, we investigate what type of jobs people with BD are instead most likely to pursue. Formally, we estimate multinomial models of occupational choice, using the broader 3-digit ISCO08 codes to classify occupations and an indicator for BD as the explanatory variable, together with an indicator for women to account for gender differences. [To define occupations consistently over time, we restrict the analysis to 2010–2015, when ISCO08 codes are available. Following the psychology literature, we use 4-digit codes to examine employment in creative professions in the main specifications. To estimate multinomial choice models of an individual’s choice across all occupations, we use 3-digit ISCO codes. An earlier study 26 estimates a multinomial model of a choice between five occupations, using data from a total of 20,861 interviews in 5 university towns. They find that people with BD and mania are most likely to work in services and show, using a measure of creativity, that services are a creative occupation.]
Multinomial logit estimates also confirm that people with BD are less likely to work in creative professions. For example, people with BD are 34 percent less likely to be “architects, planners, and surveyor designers” and 38 percent less likely to be “artistic, cultural, and culinary associate professionals,” including designers. The largest positive coefficient among creative professions is again for composers, musicians, and performing artists (here included in “creative and performing artists”). People with BD are 27 percent more likely to be employed in this category (significant at 5 percent).
Interestingly, three of the five occupations that people with BD are least likely to pursue relate to management. This is in contrast with the popular idea that BD is a “CEO’s disease” 27 , 28 because entrepreneurs share certain traits that are associated with BD, including overconfidence and an excessive tolerance for risk. [Medical studies document excessive risk tolerance and impulsive behavior in people with BD. In experiments with a balloon analogue risk task (BART) people with BD score higher on self-reported tests of impulsiveness 29 . Overconfidence and tolerance for risk are also consistent with narcissistic personality 30 . Impulsivity—the tendency to pursue rewards without considering negative consequences—has also been shown to be elevated in people who experience mania 31 .] Rejecting the hypothesis that BD is a CEO’s disease, we find that people with BD are 82 percent less likely to be sales, marketing, and development managers, 81 percent less likely to be construction and distribution managers, and 80 percent less likely to be business and administration managers.
Instead, people with BD are 177 percent more likely to be clerks; 50 percent more likely to be librarians, archivists, and curators; and 43 percent more likely to be waiters and bartenders (Fig. 2 ).
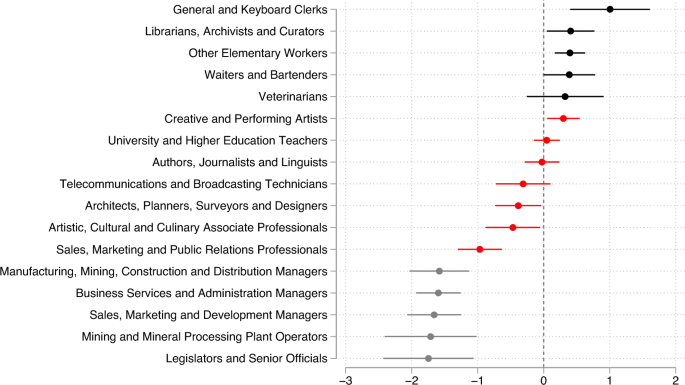
Multinomial logit estimates of occupation: people with BD vs. population. Note Multinomial logit estimates and 95 percent confidence intervals of the parameters β j in equation Pr(Y it = j) = exp(β j BD i + θ j F i )/ Σ k exp(β k BD i + θ k F i ), where Y it is the occupation of person i in year t , BD i equals one for people with BD, and F i is an indicator for females. This figure shows the five largest and the five smallest estimates of β j , along with estimates of β j for creative occupations, defined by 3-digit ISCO08 codes. Standard errors are clustered at the individual level.
Can parental wealth explain the link between BD and creativity?
Our analysis of population data for Denmark indicates a link between mental health and creativity. In this final section we test whether this link can be explained by differences in family backgrounds, and specifically parental wealth.
Children of wealthier parents are more likely to be employed in creative professions
We first test whether the finding that people with wealthy parents are more likely to become inventors extends to other creative occupations. Specifically, we plot the share (and 95-percent confidence interval) of people employed in creative professions by their decile of parental wealth.
We find that people in the top decile of parental wealth are 7 times more likely to work in creative professions (with 2.9 percent, Fig. 3 ) compared with people in the bottom decile (just 0.4 percent). This suggests that earlier findings based on inventors (a profession where financial resources are needed to be able to patent 1 , 2 ) hold more broadly across creative professions: differences in parental income and wealth help shape the link between innate creativity and professional outcomes.
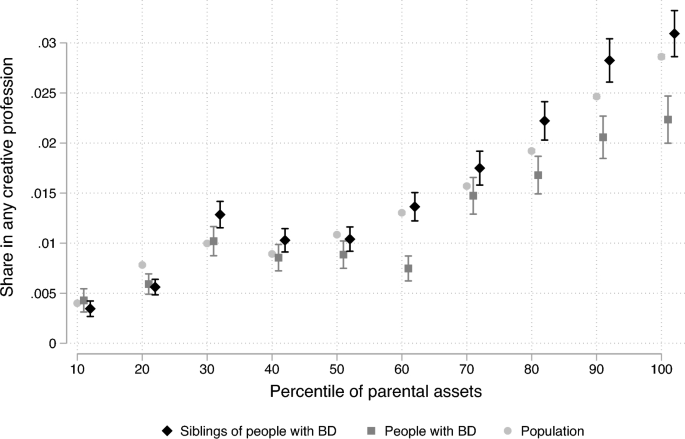
Creative professions and parental wealth: population, people with BD, and their siblings. Note Share of people employed in any of the eight creative professions in Fig. 2 , separately by the median decile of parental asset for people with BD, their siblings, and the population (with 95-percent confidence intervals). Implementing definitions from psychology, we define creative professions to include academics, architects, designers and display artists, musicians, performance artists, photographers, visual artists, and writers (Appendix Table A2 ).
Employment in creative professions for people with BD and their siblings
Higher rates of creative employment for healthy siblings are consistent with a biological link between BD and creativity. Yet, analyses of polygenic risk scores have found that only 1.2 percent of the variance in creative employment can be explained by genes that are associated with BD 3 . Indeed, an increased chance of creative employment for BD siblings is also consistent with an environmental explanation for the link between BD and creativity, as siblings share family backgrounds.
To better quantify the role of environmental factors, we examine whether parental wealth can account for the observed relationship between mental health and creative employment. We have shown above that people with wealthier parents are more likely to hold creative jobs. Differences in income and wealth can also directly impact mental health 10 , 11 . For instance, recipients of large and unconditional cash transfers in rural Kenya experienced significant increases in psychological well-being 10 .
To test this hypothesis, we use information on parental assets and investigate how differences in wealth affect the link between mental health and creativity. We formally test for the influence of parental wealth by re-estimating the difference in the likelihood of holding a creative job between people with BD and the population, controlling for indicators for low (below median) and high (above median) parental wealth.
This exercise indicates that the link between BD and creative employment is robust to controlling for, and cannot be explained by, parental wealth: estimates of the BD-population difference are essentially unchanged when we control for wealth. In these specifications, people with BD are 61 percent more likely to be musicians (Table 2 , panel A, column 5), while they are 50 percent more likely when we do not control for wealth (Fig. 3 , panel A). Across all occupations, people with BD are 19 percent less likely to have a creative job (Table 2 , panel A, column 1, significant at 1 percent), while they are 20 percent less likely not controlling for wealth. These results indicate that only a small share—approximately 6 percent—of the overall association between creativity and mental health can be explained by differences in wealth. All results are robust to alternative definitions of wealth, using of terciles, quartiles or other quantiles of parental assets.
Estimates looking at siblings of people with BD paint a similar picture: controlling for parental wealth in Eq. ( 2 ) leaves the estimates virtually unchanged. Controlling for wealth, siblings of people with BD are 12 percent more likely to work in any creative profession (with an estimated coefficient for BD Sibling equal to 0.00169 and a share of people in creative professions equal to 0.0147, Table 2 , panel B, column 1). Compared with estimates that do not control for wealth, this implies that differences in wealth explain 8 percent of the observed association between creativity and BD among siblings.
Interestingly, we find that the gradient between wealth and creative employment is weaker for people with BD than for the general population (Fig. 2 ). Among people with BD, 2.2 percent of those with the wealthiest parents work in creative professions (compared with 2.9 percent in the population). By comparison, only 0.4 percent of people with BD with the least wealthy parents work in creative professions, the same rate as the population.
At the same time, the gradient between wealth and creative employment is slightly stronger for healthy siblings of people with BD than for the population. Among siblings of people with BD, 3.0 percent of those with the wealthiest parents and only 0.4 percent of those with the least wealthy parents work in creative professions. This finding suggests that differences in wealth may amplify the biological links between mental health and creativity.
Using individual-level data on mental health diagnoses and occupations, we revisit the link between creativity and mental health disorders and study the channels behind this relationship, with a specific focus on biological and environmental forces. We show that people with BD are 50 percent more likely to be musicians, but less likely to be employed in other creative professions. Notably, healthy siblings of people with BD are consistently more likely to work in creative professions. For instance, siblings of people with BD are 16 percent more likely to be writers, 28 percent more likely to be architects, and 28 percent more likely to be visual artists. These findings indicate that family-level traits, either through genes or socioeconomic status, link mental health disorders with creativity.
Consistent with a strong influence of socioeconomic status, we find that people with parents in the top quartile of parental wealth are over 7 times as likely to hold a creative job compared with those in the bottom quartile. This striking correlation, however, explains only a small share—no more than 8 percent—of the observed correlation between mental health and creative employment. Interestingly, we also find that the creativity-wealth gradient is stronger for siblings of people with BD than for the population.
Taken together, our findings indicate that neurobiological factors may be the primary link between mental health and creativity, and that socioeconomic status amplifies this biological link. Siblings people with BD from high-income families may be additionally more likely to pursue creative jobs because their occupational choices are less constrained by financial needs, or because high-income people are more likely to experience positive moods. While comprehensive, our analysis faces a few limitations. First, our measure of creativity is limited to the choice of creative occupations and may therefore miss other expressions of creativity that do not result in creative employment. We may be missing expressions of Big Creativity 32 , 33 , which have been linked to mental health conditions 34 . Empirically, expressions of Big Creativity can be proxied through creative output, e.g., through inventions 8 , publications 31 , or musical creations 37 future analysis could establish such links by linking health records with these measures. Second, it is possible for the set of occupations that have a creative component to change over time, due to changes in the nature of work. Our time-invariant classification of creative occupations makes it possible to compare our results to findings in previous literature 1 , 2 but is not able to explicitly incorporate such changes. Third, our analysis of the relationship between BD, creative employment, and wealth is not causal and there is the possibility of reverse causality. For example, it is possible that BD leads to certain choices of occupation, but it is also possible that the choice of a certain job creates stress, e.g., over financial uncertainty, which may trigger latent pre-dispositions to develop BD and other mood and anxiety disorders 35 .
Data and sample
We use registry data on the population of Denmark, obtained from Statistics Denmark. Our data comprise mental health diagnoses and occupations for 2,524,325 people born between 1946 and 1975. Family identifiers, which we use to link people to their siblings and measure differences in parental wealth, are available for 71 percent of the population. Appendix Table A1 summarizes the variables used in our analysis. While we are not allowed to share the data ourselves, researchers will be able to access it through an application with Statistics Denmark. [ https://sundhedsdatastyrelsen.dk/da/english/health_data_and_registers/research_services/apply/data_statistics_dk ].
Mental health diagnoses
Information on diagnoses is taken from the Central Psychiatric Register ( Landspatientregistret for Psykiatri Diagnoser ), which records all mental health diagnoses in Denmark between January 1, 1995, and December 31, 2015. The Register classifies mental health disorders according to the World Health Organization International Statistical Classification of Diseases and Related Health Problems (ICD-10; see http://apps.who.int/classifications/icd10/browse/2016/en#/F30-F39 ).
Implementing this classification, our variable BD identifies 18,729 people who have received at least one diagnosis of bipolar disorder (ICD-10: F31) or mania (ICD-10: F30). BD is defined as “A disorder characterized by […] some occasions of an elevation of mood and increased energy and activity (hypomania or mania) and on others of a lowering of mood and decreased energy and activity (depression).” Mania is described as “A disorder […] which varies from carefree joviality to almost uncontrollable excitement, […] accompanied by increased energy, resulting in overactivity, pressure of speech, and a decreased need for sleep.”
Creative occupations
In this analysis, we measure a person’s tendency for creativity through employment in creativity professions. Existing economic analyses have measured creativity through output, such as patents 8 , 9 , publications 36 , and musical compositions 37 . By contrast, studies of mental health disorders and creativity in psychology and medicine have treated creativity as an individual-level characteristic, proxied by a person’s choice of occupation 1 , 2 , 19 .
We follow the psychology literature in defining creative occupations. Previous studies have classified creative professions to include designers, writers, academics, visual artists, architects, display artists, performing artists, composers, and musicians 19 . Others have excluded architects but included photographers 1 . We include both architects and photographers among the creative occupations and report results separately by occupation.
Denmark’s registries follow the International Standard Classification of Occupations (ISCO) to classify occupations. Years 1995–2009 use the 1988 classification and years 2010–2015 use the 2008 classification. Using 4-digit ISCO codes we distinguish academics (ISCO code 2310), photographers (3131), visual artists (2452 in 1988; 2651 and 2166 in 2008), designers (3471 in 1988; 3432, 3435, 2163, and 2166 in 2008), performing artists (2454 and 2455 in 1988; 2654 and 2655 in 2008), composers and musicians (2453 in 1988, 2652 in 2008), writers (2451 in 1988; 2431, 2432, 2641, and 2642 in 2008), and architects (2141 in 1998; 2161 and 2162 in 2008; Appendix Table A2 ). In multinomial logit regressions we aggregate ISCO codes to the 3-digit level to reduce the number of choices.
Family identifiers and parental wealth
To match people with their siblings, we use their mother’s or father’s social security number as a family identifier. Family identifiers are available for 1,788,166 people (71 percent of the population); 75 percent of them have one or more siblings. Family identifiers allow us to identify siblings of people with BD.
Data on parental wealth are available for people whose mother or father reported assets for at least one year between 1980 and 2015. We set assets to zero for people whose parents are listed but do not have any financial assets. Assets are reported by banks and other financial institutions and not by the individuals themselves. All results are robust to excluding individuals without information on parental assets from the analyses. To define a person’s position in the distribution of parental wealth, we calculate the percentile of parental assets for each year (from 1980 to 2015) and assign each person to their parents’ median percentile across all years.
Empirical framework
First, we test whether people with BD are more likely to work in creative occupations compared with the population. To avoid picking up differences in labor force participation between people with BD and the population, we restrict attention to people with positive earnings in any given year. We estimate the following equation separately for eight creative occupations, including writers, academics, architects, designers, musicians, photographers, visual artists, and performing artists:
where the variable creative it equals one if person i is employed in any or in a specific creative profession in year t , and BD i equals one if the person has been diagnosed with BD at least once. An indicator for women F i controls for possible gender differences in occupational choices. A vector of cohort fixed effects θ c(i) controls for systematic differences in the propensity to hold a creative job across cohorts. A vector of year fixed effects τ t controls for differences in the same propensity over time. We cluster standard errors at the individual level. The coefficient β estimates the difference in the likelihood of holding a creative job between people with BD and the population, controlling for variation in creative employment across calendar years, birth cohorts, and gender.
Creative employment among siblings of people With BD
If BD is associated with creativity through a genetic link, siblings may have a milder “subthreshold” form of BD that allows them to be more creative, without experiencing debilitating symptoms. Models of BD in molecular neuropsychiatry have proposed an inverted U-shaped relationship between the genetic risk for BD and creativity 25 . Conjectures that “some aspects of the bipolar spectrum may confer advantages, while more severe expressions of symptoms negatively influence creative accomplishment.”
To test whether healthy siblings of people with BD are more likely to pursue creative jobs, we estimate Eq. ( 1 ) with an indicator for BD siblings instead of the indicator for BD:
In this modified equation, the coefficient β S estimates the difference in the likelihood of holding a creative job between siblings of people with BD and other people of the same gender, in the same birth cohort and calendar year.
Most frequent occupations for people with BD: multinomial logit
Looking beyond creative professions, we investigate what type of jobs people with BD are instead most likely to pursue. Formally, we estimate multinomial models of occupational choice, using the broader 3-digit ISCO08 codes to classify occupations. To define occupations consistently over time, we restrict the analysis to 2010–2015, when ISCO08 codes are available. Following the psychology literature, we use 4-digit codes to examine employment in creative professions in the main specifications. To estimate multinomial choice models of an individual’s choice across all occupations, we use 3-digit ISCO codes. [An earlier study estimates a multinomial model of a choice between five occupations, using data from a total of 20,861 interviews in 5 university towns. They find that people with BD and mania are most likely to work in services and show, using a measure of creativity, that services are a creative occupation 28 .]We model the probability that a person works in occupation j at time t as:
where Y it is the occupation of person i in year t and F i is an indicator for women. First, we estimate β j and γ j for 129 occupations via maximum likelihood. We normalize both parameters to zero for “Primary Schools and Early Childhood Teachers” (ISCO08 code 234), the most common occupation (with 6.8 percent of workers). We then compute the excess probability of occupation j for people with BD as exp( β j )− 1.
Data availability
We obtained our data from Statistics Denmark. While we are not allowed to share the data ourselves, researchers will be able to access it through an application with Statistics Denmark. [ https://sundhedsdatastyrelsen.dk/da/english/health_data_and_registers/research_services/apply/data_statistics_dk ].
Kyaga, S. et al. Creativity and mental disorder: Family study of 300 000 people with severe mental disorder. Br. J. Psychiatry 199 (5), 373–379 (2011).
Article PubMed Google Scholar
Kyaga, S. et al. Mental illness, suicide and creativity: 40-year prospective total population study. J. Psychiatr. Res. 47 (1), 84–90 (2013).
Article Google Scholar
Power, R. A. et al. Polygenic risk scores for schizophrenia and bipolar disorder predict creativity. Nat. Neurosci. 18 (7), 953–955 (2015).
Article CAS PubMed Google Scholar
Miklowitz, D. J. & Johnson, S. L. The psychopathology and treatment of bipolar disorder. Annu. Rev. Clin. Psychol. 2 , 199–235 (2006).
Article PubMed PubMed Central Google Scholar
Takeuchi, H. et al. Regional gray matter volume of dopaminergic system associate with creativity: Evidence from voxel-based morphometry. Neuroimage 51 (2), 578–585 (2010).
MacCabe, J. H. et al. Excellent school performance at age 16 and risk of adult bipolar disorder: National cohort study. Br. J. Psychiatry 196 (2), 109–115 (2010).
Runco, M. A. Creativity: Theories and themes: Research, development, and practice (Elsevier, Amsterdam, 2007).
Google Scholar
Bell, A., Chetty, R., Jaravel, X., Petkova, N. & van Reenen, J. Who becomes an inventor in America? The importance of exposure to innovation. Q. J. Econ. 134 (2), 647–713 (2019).
Aghion, Phillipe, Ufuk Akcigit, A. Hyytinen, and Otto Toivanen. 2017. “The social origins of inventors.” NBER Working Paper No. 24110.
Haushofer, J. & Shapiro, J. The short-term impact of unconditional cash transfers to the poor: Experimental evidence from Kenya. Q. J. Econ. 131 (4), 1973–2042 (2016).
Ridley, Matthew W., Gautam Rao, Frank Schilbach and Vikram H. Patel. 2020. “Poverty, Depression, and Anxiety: Causal Evidence and Mechanisms.” NBER Working Paper 27157.
Bauer, Michael, Tasha Glenn, Natalie Rasgon, Wendy Marsh, Kemal Sagduyu, Rodrigo Munoz, Rita Schmid, Sara Haack, and Peter C. Whybrow. 2011. “Association between median family income and self-reported mood symptoms in bipolar disorder.” Comprehensive psychiatry 52, no. 1: 17–25. -treated patients with bipolar disorder,” Biological Psychiatry , 62 (1): 7–16.
Sareen, J., Afifi, T. O., McMillan, K. A. & Asmundson, G. J. G. Relationship between household income and mental disorders: findings from a population-based longitudinal study. Arch. Gen. Psychiatry 68 (4), 419–427 (2011).
Hakulinen, C., Musliner, K. L. & Agerbo, E. Bipolar disorder and depression in early adulthood and long-term employment, income, and educational attainment: A nationwide cohort study of 2,390,127 individuals. Depress. Anxiety 36 (11), 1080–1088 (2019).
Alegría, M., Bijl, R. V., Lin, E., Walters, E. E. & Kessler, R. C. Income differences in persons seeking outpatient treatment for mental disorders: a comparison of the United States with Ontario and The Netherlands. Arch. Gen. Psychiatry 57 (4), 383–391 (2000).
Simpson, S. G. & Jamison, K. R. The risk of suicide in patients with bipolar disorders. J. Clin. Psychiatry 60 (2), 53–56 (1999).
PubMed Google Scholar
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. The Lancet 396 (10258), 1204–1222 (2000).
Jamison, K. R. Touched with fire manic depressive illness and the artistic temperament (Free Press, New York, 1993).
Ludwig, & Arnold, M. Creative achievement and psychopathology: Comparison among professions. Am. J. Psychiatry 46 (3), 330–356 (1992).
MathSciNet CAS Google Scholar
Richards, R., Kinney, D. K., Lunde, I., Benet, M. & Merzel, A. P. C. Creativity in manic-depressives, cyclothymes, their normal relatives, and control subjects. J. Abnormal Psychol. 97 (3), 281 (1988).
Article CAS Google Scholar
Grossman, M. On the concept of health capital and the demand for health. J. Political Econ. 80 (2), 223–255 (1972).
Strulik, H. A health economic theory of occupational choice, aging, and longevity. J. Health Econ. 82 , 102599 (2022).
Mula, M. & Trimble, M. R. Music and madness: Neuropsychiatric aspects of music. Clin. Med. 9 (1), 83 (2009).
Borowiecki, K. How are you, my dearest Mozart? Well-being and creativity of three famous composers based on their letters. Rev. Econ. Stat. 99 (4), 591–605 (2017).
Greenwood, T. A. Positive traits in the bipolar spectrum. The space between madness and genius. Molecular Neuropsychiatry 2 (4), 198–212 (2016).
MathSciNet PubMed PubMed Central Google Scholar
Tremblay, C. H., Grosskopf, S. & Yang, Ke. Brainstorm: Occupational choice, bipolar illness and creativity. Econ. Human Biol. 8 (2), 233–241 (2020).
Elsberry, Richard. 1998. “Bipolar Disorder: Why Are They Calling It the CEO Disease?” Electrical Apparatus.
Gartner, J. D. The hypomanic edge: The link between (A Little) craziness and (A Lot of) success in America (Simon & Schuster, New York, 2011).
Reddy, L. F. et al. Impulsivity and risk taking in bipolar disorder and schizophrenia. Neuropsychopharmacology 39 , 456–463 (2014).
Larcker, David F., Charles A. O'Reilly, Brian Tayan, and Anastasia A. Zakolyukina. 2021. "Are Narcissistic CEOs All That Bad?" Rock Center for Corporate Governance at Stanford University Working Paper.
Swann, A. C. D. M., Dougherty, P. J. P., Pham, M. & Moeller, F. G. Impulsivity: A link between bipolar disorder and substance abuse. Bipolar Disorder 6 , 204–2012 (2004).
Simonton, D. K. What is a creative idea? Little-c versus Big-C creativity. In Handbook of research on creativity (eds Thomas, K. & Chan, J.) (Edward Elgar Publishing, Camberley, 2013). https://doi.org/10.4337/9780857939814.00015 .
Chapter Google Scholar
Simonton, D. K. The mad (creative) genius: What do we know after a century of historiometric research? In Creativity and mental illness (ed. Kaufman, J. C.) 25–41 (Cambridge University Press, Cambridge, 2014).
Simonton, D. K. The mad-genius paradox: Can creative people be more mentally healthy but highly creative people more mentally ill?. Persp. Psychol. Sci. 9 , 470–480 (2014).
Weisberg, R. W. Creativity: Understanding innovation in problem solving, science, invention, and the arts (Wiley, Hoboken, 2006).
Biasi, B. & Moser, P. Effects of copyrights on science – evidence from the wwii book republication program. Am. Econ. J. Microecon. 13 (4), 218–260 (2021).
Giorcelli, M. & Moser, P. Copyright and creativity. Evidence from Italian operas in the neapoleonic age. J. Political Econ. 128 (11), 4163–4210 (2020).
Download references
Author information
Authors and affiliations.
Yale School of Management, New Haven, USA
Barbara Biasi
National Bureau of Economic Research, Cambridge, USA
Barbara Biasi & Petra Moser
Aalborg University, Aalborg, Denmark
Michael S. Dahl
NHH Norwegian School of Economics, Bergen, Norway
Aarhus University, Aarhus, Denmark
New York University Stern School of Business, New York, USA
Petra Moser
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed equally.
Corresponding author
Correspondence to Barbara Biasi .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Biasi, B., Dahl, M.S. & Moser, P. The role of bipolar disorder and family wealth in choosing creative occupations. Sci Rep 14 , 10703 (2024). https://doi.org/10.1038/s41598-024-61320-y
Download citation
Received : 05 July 2023
Accepted : 03 May 2024
Published : 10 May 2024
DOI : https://doi.org/10.1038/s41598-024-61320-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Occupational choice
- Parental wealth
- Bipolar disorder
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Bipolar Disorder Biobank
Researcher information.
Find information about using samples or data from the Mayo Clinic Bipolar Disorder Biobank.
How can I access samples and data from the Bipolar Disorder Biobank?
Contact our senior program coordinator with information about your planned project. Please include what types of samples or data you are requesting.
What data points are available in the dataset?
- Bipolar diagnosis and history.
- Personal background.
- Environment.
- Family history.
What steps are required to become a collaborator?
Contact our senior program coordinator if you are interested in collaborating with us.
More about research at Mayo Clinic
- Research Faculty
- Laboratories
- Core Facilities
- Centers & Programs
- Departments & Divisions
- Clinical Trials
- Institutional Review Board
- Postdoctoral Fellowships
- Training Grant Programs
- Publications
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
- Bipolar Disorder Symptoms and Traits
What Causes Bipolar Disorder?
- Is Bipolar Hereditary?
- How to Diagnose Bipolar Disorder
- Bipolar Disorder Treatments to Manage Symptoms
- When Your Loved One Has Bipolar Disorder
Bipolar Disorder Explained: Everything You Need to Know
What is bipolar disorder, living with bipolar disorder.
- Next in Bipolar Disorder Guide Bipolar Disorder Symptoms and Traits
Bipolar disorder refers to a group of mental health conditions characterized by sudden, dramatic changes in mood, energy, and behavior. Formerly known as manic depression, this condition causes mood episodes lasting days or weeks at a time and hinder day-to-day functioning, school or work performance, and relationships.
This article describes the symptoms , causes, and treatments for bipolar disorder and discusses how to cope if you’re diagnosed with this mental health condition.
FG Trade / Getty Images
Estimated to affect 4.4% of U.S. adults at some point in their lives, bipolar disorder causes distinct periods of extreme emotional states or episodes that can last for days or weeks. Episodes are characterized by manic or depressive behavior.
Manic Episodes
A manic episode is a phase of a week or more during which you have an elevated mood and energy most of the time for most days. In this phase, you may feel abnormally happy, agitated, restless, and don’t need much sleep.
In rare and severe cases, people experience hallucinations and delusions during manic episodes. In addition, some people experience hypomanic episodes—less severe manic episodes lasting four or more days.
Everything You Should Know About Bipolar Disorder
Major depressive episodes.
A major depressive episode is a period of two or more weeks of depressive symptoms, such as sadness, hopelessness, lethargy (lack of energy), and apathy. These episodes can become severe, leading to suicidal thoughts. As with manic episodes, severe depressive episodes can lead to hallucinations or delusions.
What Are the Types of Bipolar Disorder?
Healthcare providers break down bipolar disorder into four primary types : bipolar 1, bipolar 2, cyclothymic disorder, and unspecified bipolar disorder.
Bipolar 1 Disorder
With bipolar 1 disorder, manic episodes last a week or become so severe that you require hospitalization. In most cases, bipolar 1 also causes depressive episodes. Some people have “mixed” episodes that feature both manic and depressive symptoms at the same time. Neutral periods—neither manic nor depressive—are also common with this type.
Bipolar 2 Disorder
Bipolar 2 disorder occurs when you experience one depressive episode and at least one hypomanic episode (milder manic episodes that last four or more days). In between these are symptom-free periods. Those with bipolar 2 disorder often have other mental health conditions, such as anxiety or depression.
Cyclothymic Disorder (Cyclothymia)
Cyclothymic disorder is a milder type of bipolar disorder that causes regular mood swings. Ranging between those of mild depression and hypomania, the symptoms aren’t severe enough to be considered clinically depressive or hypomanic episodes.
Unspecified Bipolar Disorder
Unspecified bipolar disorder is when you have extreme mood fluctuations, but the symptoms aren’t as bad as those of bipolar 1 or 2. Still, with this type, the symptoms are significant enough to affect daily functioning, relationships, and work or school.
Bipolar Disorder Symptoms
Dramatic and intense changes in your mood, emotions, behaviors, and activity level are the primary signs of bipolar disorder. These shifts tend to be noticeable to others and impact your relationships, performance at work or school, or daily functioning.
The symptoms you experience depend on whether you’re having a manic or depressive episode.
Manic Episode Symptoms
During manic episodes, emotion and activity levels are elevated. Manic episode symptoms include the following:
- Abnormal giddiness or happiness
- Changing topics when speaking
- Distractibility
- Feeling energetic despite insufficient sleep
- Increased irritability or agitation
- Racing, uncontrollable thoughts
- Recklessness or risky, impulsive behaviors
- Restlessness, increased activity
- Talking faster or more often
Major Depressive Episode Symptoms
In contrast to manic episodes, during a depressive episode, you feel “low” in terms of energy, mood, and emotion. Symptoms of this type include combinations of the following:
- Despair, thoughts about death or suicide
- Difficulty falling or staying asleep or sleeping excessively
- Difficulty with routine tasks
- Feeling sad, hopeless, or anxious
- Forgetfulness, slowed speech, not knowing what to say
- Loss of energy or motivation
- Loss of interest in activities
- Restlessness
When to Call 911
If you have bipolar disorder, go to an emergency room (ER) if you experience:
- Suicidal thoughts
- Thoughts about hurting yourself or others
- Hallucinations or delusions
- Lithium toxicity symptoms: nausea, vomiting, dizziness, changes in vision, and slurred speech
Researchers don’t know what exactly causes bipolar disorder. The consensus is that genetic factors, brain chemistry and structure, and environmental factors all play a role in this condition.
Genetic Factors
Though more work is needed, researchers have linked genetics with an increased risk of developing bipolar disorder. This condition is heritable, making family history a risk factor; people with a parent or sibling with the condition are more likely to have it.
Brain Chemistry and Structure
Using imaging techniques, researchers have found differences between the brains of those with and without bipolar disorder. Some research shows that people with bipolar disorder have smaller subcortical structures (associated with mood and cognition) and a thinner cortex (the outer layer of the brain).
In addition, researchers have linked imbalances in certain neurotransmitters (brain chemicals), particularly dopamine and serotonin, to bipolar disorder.
Environmental Factors
Stressful or traumatic life events and certain behaviors can also raise your risk of developing bipolar disorder. Examples of traumatic events found to trigger attacks include childbirth, losing a job or a loved one, divorce, misusing or overusing drugs or alcohol, or traumatic head injuries.
How Is Bipolar Disorder Diagnosed?
To diagnose bipolar disorder, a healthcare provider will ask about your medical history, current medications, symptoms, and your family’s mental health history. You’ll also undergo a physical exam and, in some cases, blood tests to rule out other potential causes of bipolar disorder symptoms, such as hypothyroidism, stroke, and substance use disorder.
A healthcare provider or a mental health specialist, like a psychiatrist or psychologist , will perform a mental health evaluation. They will diagnose bipolar disorder and identify the type based on criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
Diagnosing Bipolar 1 Disorder
According to the DSM-5, to be diagnosed with bipolar 1 disorder, you must have had at least one manic episode. This may be followed or preceded by a hypomanic or major depressive episode. While hypomanic or major depressive episodes can occur in bipolar 1, they are not required for a diagnosis.
In bipolar 1 disorder, manic episodes last at least one week or are severe enough to require hospitalization. A healthcare provider will look for at least three (or four if you experience irritability) of the following to diagnose you with bipolar 1 disorder:
- An inflated self-esteem or sense of grandiosity
- Difficulty concentrating; being easily distracted
- Increased activities, agitation, toe-tapping, pacing, or other unnecessary movements
- Increased engagement in unusually risky or self-destructive activities
- Racing thoughts; thoughts in flight
- Reduced need for sleep
Diagnosing Bipolar 2 Disorder
A diagnosis of bipolar 2 disorder is made based on four criteria:
- A current or past episode of hypomania and at least one major depressive episode
- Never having a manic episode
- No other psychological or neurological issues can explain the symptoms
- The mood changes cause impairments in social, personal, and professional life and daily functioning
"Hypomania" is defined as at least four days of manic symptoms that aren’t as severe or numerous as with a full manic episode. Major depressive episodes are defined as having daily or nearly daily symptoms for at least two weeks. According to the DSM-5, these are diagnosed when you display five of the following criteria:
- Agitation, toe-tapping, or pacing
- A lack of interest or enjoyment in life
- Decreased ability to concentrate
- Depression, sadness
- Fatigue, insufficient energy
- Inappropriate guilt or lack of self-worth
- Thinking about suicide without making a concrete plan (suicidal ideation)
- Weight loss without dieting, weight gain, decrease or increase in appetite
Diagnostic Criteria for Cyclothymic Disorder
In the DSM-5, among the criteria for cyclothymic disorder are the following:
- You have neutral, asymptomatic periods for no more than three months at a time.
- Symptoms arise independent of substance use disorder.
- Symptoms hinder your ability to function and impact your work, school, home, or social life.
- Symptoms are inconsistent with bipolar 1 or 2 or another mental health condition.
- You experience two or more years of hypomania and depressive episodes if an adult and at least one year of symptoms if a child.
Bipolar Disorder Treatment
Treating bipolar disorder typically involves adopting multiple strategies, including medications, counseling, and lifestyle changes.
Medications
Antidepressants, mood stabilizers, and atypical antipsychotics are medication types that healthcare providers consider. A healthcare provider may prescribe selective serotonin reuptake inhibitors (SSRIs), a class of antidepressants, for depression associated with bipolar disorder. However, these can cause what is known as cycling—rapid mood shifts—so healthcare providers prescribe them with caution.
Mood-stabilizing drugs, such as Lithobid (lithium) and Depacon (valproate), are indicated alongside SSRIs and help ease or shorten the length of mood episodes. A provider may also prescribe medications to address insomnia (sleep problems) and anxiety, which often accompany bipolar disorder.
Medication Side Effects
The side effects of medications depend on the type you’re taking. For bipolar disorder, the most common of these are unintended weight gain, sedation, restlessness, and changes in metabolism.
Psychotherapy and Counseling
Psychotherapy and counseling involve talk therapy with a psychiatrist, therapist, or trained counselor. This work aims to identify and change problematic behaviors, thoughts, or emotions that set off episodes. Another alternative is cognitive behavioral therapy (CBT), which focuses on changing thought patterns.
Lifestyle Changes
Alongside medical treatments or therapy, lifestyle changes can help you manage bipolar disorder, including:
- Relax : Activities like yoga or meditation may help ease anxiety and help with symptoms.
- Stay active : Regular exercise improves sleep and helps with stress, among other benefits.
- Dietary changes : Poor diet is associated with an increased risk for bipolar disorder and a reduced risk of co-occurring conditions.
- Avoid substances : Drinking alcohol, smoking tobacco, or using recreational drugs can all increase the risk of bipolar symptoms.
- Education : Understand the symptoms of bipolar disorder and keep track of events or things that trigger symptoms; know your medications and their side effects.
Living with bipolar disorder means finding a support system , developing coping mechanisms, and managing the shifts in your mood and behaviors. Strategies that can help include:
- Adding structure to your daily activities
- Enlisting loved ones and/or family members in your care
- Ensuring you’re getting regular exercise and enough sleep
- Making sure to take part in enjoyable activities, staying connected to friends, family, and the local community
- Seeking out social support from online or in-person support groups, social media, or message boards
- Seeking treatment, developing a treatment plan with your healthcare provider
- Tracking and logging your symptoms, medications, and triggers
Bipolar disorder causes dramatic and lasting mood and behavior shifts. People with the condition go through high-energy manic episodes and often also experience depressive episodes. Because of its effects on behavior, bipolar disorder can significantly impact your professional, academic, and/or personal life. If you suspect you or someone you care for has this condition, talk to a healthcare provider for an accurate diagnosis and treatment.
American Psychiatric Association. What are bipolar disorders?
MedlinePlus. Bipolar disorder .
National Institute of Mental Health. Bipolar disorder: definition .
National Institute of Mental Health. Bipolar disorder: overview .
National Alliance on Mental Illness (NAMI). Bipolar disorder .
MedlinePlus. Lithium toxicity .
Rowland TA, Marwaha S. Epidemiology and risk factors for bipolar disorder . Ther Adv Psychopharmacol . 2018 26;8(9):251-269. doi:10.1177/2045125318769235.
Abé C, Liberg B, Klahn AL, Petrovic P, Landén M. Mania-related effects on structural brain changes in bipolar disorder – a narrative review of the evidence. Mol Psychiatry . 2023;28(7):2674-2682. doi:10.1038/s41380-023-02073-4
Lee JG, Woo YS, Park SW, Seog DH, Seo MK, Bahk WM. Neuromolecular etiology of bipolar disorder: possible therapeutic targets of mood stabilizers . Clin Psychopharmacol Neurosci . 2022;20(2):228-239. doi:10.9758/cpn.2022.20.2.228
Substance Abuse and Mental Health Services Administration. DSM-5 changes: implications for child serious emotional disturbance . Substance Abuse and Mental Health Services Administration; 2016. Table 12, DSM-IV to DSM-5 Bipolar I Disorder Comparison.
Perugi G, Hantouche E, Vannucchi G. Diagnosis and treatment of cyclothymia: the "primacy" of temperament . Curr Neuropharmacol . 2017;15(3):372-379. doi:10.2174/1570159X14666160616120157
Marzani G, Neff AP. Bipolar disorders: evaluation and treatment . Am Fam Physician. 2021;103(4):227-239
Bauer IE, Gálvez JF, Hamilton JE, et al. Lifestyle interventions targeting dietary habits and exercise in bipolar disorder: A systematic review . J Psychiatr Res . 2016;74:1-7. doi:10.1016/j.jpsychires.2015.12.006
By Mark Gurarie Gurarie is a freelance writer and editor. He is a writing composition adjunct lecturer at George Washington University.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ther Adv Psychopharmacol
- v.8(9); 2018 Sep

Epidemiology and risk factors for bipolar disorder
Tobias a. rowland.
Unit of Mental Health and Wellbeing, Division of Health Sciences, University of Warwick, Coventry, CV4 7AL, UK
Steven Marwaha
Division of Health Sciences, University of Warwick, Coventry, UK
Coventry and Warwick-shire Partnership Trust, The Caludon Centre, Coventry, UK
Bipolar disorder is a multifactorial illness with uncertain aetiology. Knowledge of potential risk factors enables clinicians to identify patients who are more likely to develop bipolar disorder, which directs further investigation, follow up and caution when prescribing. Ideally, identifying directly causative factors for bipolar disorder would enable intervention on an individual or population level to prevent the development of the illness, and improve outcomes through earlier treatment. This article reviews the epidemiology of bipolar disorder, along with putative demographic, genetic and environmental risk factors, while assessing the strength of these associations and to what extent they might be said to be ‘causative’. While numerous genetic and environmental risk factors have been identified, the attributable risk of individual factors is often small, and most are not specific to bipolar disorder but are associated with several mental illnesses. Therefore, while some genetic and environmental factors have strong evidence supporting their association with bipolar disorder, fewer have sufficient evidence to establish causality. There is increasing interest in the role of specific gene–environment interactions, as well as the mechanisms by which risk factors interact to lead to bipolar disorder.
Introduction
Bipolar affective disorder (bipolar) is a multicomponent illness involving episodes of severe mood disturbance, neuropsychological deficits, immunological and physiological changes, and disturbances in functioning. 1 It is one of the leading causes of disability worldwide 2 and is associated with high rates of premature mortality from both suicide and medical comorbidities. 3 , 4
The aetiology of bipolar is not well understood and research into the disorder lags behind disorders such as psychosis. However, the last decade has seen an expanding evidence into the genetics of the disorder, underlying developmental pathways, risks and vulnerability factors, gene–environment interactions and the putative features of the bipolar prodrome.
This article summarizes the research into demographic, genetic and environmental risk factors for the development of bipolar, with a focus on recent updates and the role of environmental triggers. To identify relevant literature, searches were conducted in PubMed and PsycINFO using the terms ‘Bipolar Disorder’, combined with ‘risk factors’ or ‘epidemiology’. Results were reviewed with a focus on the most recent evidence and systematic reviews or large prospective studies, and further individual searches were then expanded for each risk factor category identified. A summary of the included studies relating to specific risk factors for bipolar are included in Table 1 .
Studies investigating specific risk factors for bipolar disorder.
ADHD, attention deficit hyperactivity disorder; BDNF, brain-derived neurotrophic factor; bipolar, bipolar disorder; CI, confidence interval; COMT, Catechol- O -methyltransferase; 5-HTTL, serotonin system gene; 5-HTTLPR, serotonin-transporter-linked polymorphic region; GWAS, genome-wide association study; HR, hazard ratio; MDD, major depressive disorder; mRNA, messenger ribonucleic acid; OR, odds ratio; SNP, single nucleotide polymorphism; TLR2, toll-like receptor 2.
Epidemiology of bipolar disorder
Epidemiological studies have suggested a lifetime prevalence of around 1% for bipolar type I in the general population. 54 , 55 A large cross-sectional survey of 11 countries found the overall lifetime prevalence of bipolar spectrum disorders was 2.4%, with a prevalence of 0.6% for bipolar type I and 0.4% for bipolar type II. 56 Although findings varied across different countries, this suggested a lower prevalence of bipolar type I and II than previous studies, 55 , 57 while the prevalence of bipolar type I in USA was found to be 1%, slightly higher than the other countries. It is unclear whether differences were due to more stringent diagnostic criteria used in this study, or true differences in rates of bipolar across countries and ethnic groups. In one of the very few epidemiological investigations in England, the recent Adult Psychiatric Morbidity Survey 2014 found lifetime prevalence of likely bipolar was 2%. The measurement method suggests that this was an underestimate, but the study did not distinguish bipolar subtypes. 58 A recent meta-analysis of 25 studies found a pooled lifetime prevalence of 1.06% and 1.57% for bipolar type I and II, respectively, although the majority of the included studies were from North or South America. 59 Nevertheless, a similar prevalence has been found in the UK, Germany and Italy, 60 and a lifetime prevalence between 0.1–1.83% was found in a systematic review of studies from African countries. 61
The reason for international variations in the prevalence of bipolar is not entirely clear, and ethnicity, 49 cultural factors 62 and variations in diagnostic criteria and study methodology 59 may each have an impact. The evidence for differing rates of bipolar in different ethnicities is conflicting, with some studies showing higher rates in Caucasians 63 , 64 and others in nonwhite populations. 65 A systematic review found no clear evidence for differences across ethnic groups, and suggested individual study differences may be related to cultural factors, migration and higher rates of misdiagnosis of black ethnic groups as having schizophrenia rather than bipolar. 49 With regards to sex, several studies report equal distribution in bipolar, 49 while others have identified a higher prevalence of manic episodes and bipolar type I in males and higher rates of bipolar type II in females. 56 Overall, the evidence is not sufficiently strong to deviate from the view that bipolar appears to have a roughly equal distribution across sex and ethnicity.
The mean age of onset for bipolar appears to be in the early twenties, 56 although findings vary between 20–30 years. 55 A bimodal distribution of the incidence of bipolar has been suggested, 66 supported by a large population-based cohort study, which found two peaks in age of onset at 15–24 years and at 45–54 years. 67 However, age of onset estimates are very difficult to define accurately for bipolar, given the long periods of untreated illness, when symptoms can be nascent or apparent without individuals accessing services, which is often used as the measure of onset in many studies. 68 Moreover, there appear to be differences in the presentation and clinical course of bipolar depending on age of onset, 69 with higher rates of psychiatric and medical comorbidities such as suicidality and vascular disease in later-onset mania. 70
A number of studies have investigated rates of bipolar according to sociodemographic variables, with generally inconsistent findings. 49 There is some evidence of higher rates in low income, unemployed and unmarried groups, 49 although the social disruption caused by severe mental illness giving rise to such associations cannot be ruled out. 54 Conversely, an interesting finding among some studies is that higher socioeconomic status and higher occupational level, as well as creativity, 54 , 71 are associated with increased risk of bipolar, 72 , 73 which is opposite to that of unipolar depression and schizophrenia. 54 However, these studies are limited by small sample sizes and a lack of replication. 74 Explanations for this association include the possibility of referral bias for those with higher socioeconomic status, while some have suggested that those with high-functioning creative traits may confer a genetic risk of bipolar. 54
There is also emerging evidence for an association between urban environments and increased rates of bipolar. 49 While the evidence is stronger for schizophrenia, where there have been multiple suggested explanations, 75 the reason for the association between urbanization and bipolar is less clear. However, a cohort study found that there was a strong association between urban residence and the incidence of psychotic bipolar, but no association for bipolar without psychosis. 76 This may suggest that urban residence is a transdiagnostic risk factor for psychotic illness rather than bipolar per se .
Genetics and gene environment interactions
The contribution of genetic factors to bipolar has long been identified, with evidence from twin studies suggesting monozygotic concordance of between 40–70%, and lifetime risk in first-degree relatives is 5–10%; around seven times higher than the general population risk. 5 However, relatives of patients with bipolar are more likely to develop unipolar depression than bipolar themselves, suggesting the genetic risk transcends diagnostic categories. 5 There is also evidence of shared genetic risk between bipolar, schizophrenia and autism. 77 , 78 Nonetheless, bipolar clearly does not follow a Mendelian pattern of inheritance, and linkage studies have not identified individual genes with a strong association with the disorder. 79 The genetic risk for bipolar in part is likely due to multiple single nucleotide polymorphisms, which are highly prevalent in the general population and confer a very small increased risk individually. 80 Technological advances have allowed for genome-wide association studies that have pooled data and identified multiple genetic loci associated with bipolar patients, suggesting aggregated polygenic risk. 6
Whilst many important genetic loci have been identified, how these translate to risk of illness is a second frontier of discovery. Studies have identified polymorphisms in genes coding for brain-derived neurotrophic factor (BDNF) to be associated with bipolar. 7 BDNF is suspected to be involved in the pathogenesis of bipolar as well as being a potential biomarker of disease activity. 81 Associations with catechol- O -methyl transferase (COMT) and monoamine transporters have also been observed. 8 , 82 Genes for voltage-gated calcium channel subunits such as CACNA1C are located near to single nucleotide polymorphisms that have an association with bipolar, as well as proteins involved in cell signalling such as ODZ4, 6 and genes encoding for gamma-aminobutyric acid (GABA) receptor subunits. 83 The fact that many of the medications used as prophylactic agents in bipolar act on calcium channels or GABA receptors 84 suggests these proteins may be involved in the neurobiology of the disorder, and this evidence is guiding the search for new therapeutic targets. 85
However, it is clear that the effect size of each single nucleotide polymorphism is very small. For example, the odds of having bipolar in those with the polymorphism around CACNA1C is 1.14, and the majority of those with this polymorphism do not go on to develop the disorder. 6 , 80 There has therefore been increasing interest in the role of how gene–environment interactions contribute to the onset of bipolar, although this remains an under-researched area, compared with schizophrenia. 86 , 87 Nevertheless, interaction between childhood abuse and BDNF gene polymorphisms have been shown in several studies, 9 , 86 while toll-like receptor 2 polymorphisms may interact with stressful life events and Toxoplasma gondii infection to increase the risk of bipolar. 10 , 11 A COMT polymorphism has been found to interact with stressful life events for bipolar depressive episodes, 12 while serotonin transporter genes have interactions with cannabis use on the presence of psychotic symptoms in bipolar. 13 With the increasing ability of genome-wide association studies to identify polymorphisms conferring a very small increased risk, further study of how these genes interact with environmental factors to trigger bipolar is required.
Environmental risk factors
Prenatal and perinatal factors.
Prenatal viral infections have been implicated in a number of mental illnesses, including bipolar. 88 – 90 A recent review by Barichello and colleagues 14 investigated associations between bipolar and 10 infectious agents. Findings between studies were generally inconsistent, and no association was found for Epstein-Barr virus, human herpesvirus 6 or varicella zoster virus. Five of the eleven studies investigating cytomegalovirus found an association between antibody levels and bipolar, while two studies found an association between maternal influenza infection and bipolar with psychosis, 91 , 92 although other studies found no association. 93 – 95 None of these studies were prospective or longitudinal and it is uncertain whether these infections occurred during pregnancy or subsequently. Therefore, the evidence for maternal viral infection as a risk factor for bipolar remains weak, overall.
However, there is stronger evidence for an association between bipolar and seropositivity for T. gondii infection, demonstrated in two recent meta-analyses. 15 , 16 The first included 11 studies and demonstrated overall increased odds of having bipolar in those with immunoglobulin G (IgG) to T. gondii , with an odds ratio of 1.52 (95% confidence interval 1.06–2.18). 15 A second meta-analysis of eight studies also found a significant association between bipolar and T. gondii seropositivity, with an odds ratio of 1.26 (95% confidence interval 1.08–1.47). 16 However, the included studies were not prospective and it remains uncertain when T. gondii exposure occurred. Notwithstanding, there is preclinical evidence suggestive of a relationship between T. gondii and development of mental illness, with studies showing behavioural changes in mice 96 and humans. 97 , 98 Moreover, there is evidence that infection with T. gondii causes changes in dopamine metabolism leading to increased dopamine production, 99 similar to that suggested as a potential mechanism for manic episodes in bipolar. 100 Furthermore, there is evidence that following T. gondii infection, the local inflammatory response leads to alteration in cytokines, 101 such as IL-6, 102 which have been implicated in mental illness and bipolar specifically, 103 and may be related to cognitive deterioration in this patient group. 102
Evidence regarding other prenatal exposures such as maternal smoking and severe psychological stressors are inconsistent, with only a small number of studies investigating these factors. 50 Obstetric complications have generated interest as a risk factor for later development of bipolar, 104 but a meta-analysis found no significant evidence for this association, 17 and bipolar patients were less likely to have experienced obstetric complications than those with schizophrenia. A systematic review by Marangoni and colleagues 50 identified prospective studies which suggested extreme prematurity (less than 32 weeks’ gestation) conferred a significant risk of developing bipolar.
In general, the evidence for prenatal and perinatal factors as an independent risk factor for developing bipolar is relatively weak and inconsistent, and such factors appear to confer greater risk for developing other mental disorders, such as schizophrenia. 17 The evidence for T. gondii infection is more substantial, while maternal CMV and influenza infection warrant further investigation as to their associations with bipolar.
Postnatal factors
Childhood maltreatment.
Childhood maltreatment is a well-studied environmental risk factor with high-quality evidence that it confers a risk for later development of bipolar, 51 although it is also associated with behavioural problems and other mental illnesses. 105 , 106 When investigating specific subtypes of abuse, several studies have identified a link between emotional abuse or emotional neglect and the later the development of bipolar, 18 , 19 while emotional abuse appears to be the most frequent subtype of abuse experienced in bipolar patients. 20 A recent high quality meta-analysis of childhood adversity in bipolar patients compared with healthy controls found significant associations between development of bipolar and prior physical, sexual and emotional abuse, and physical and emotional neglect. 21 The largest association was for emotional abuse which was four times more likely to have occurred in bipolar patients than in controls. 21 Moreover, higher rates of childhood adversity were found in patients with bipolar compared with unipolar depression, although rates were similar to schizophrenia. 21 Gilman and colleagues 52 also found that a history of childhood abuse increased the risk of transitioning to bipolar following a depressive episode. This suggests that abuse and neglect during childhood confer some specific risk to more severe forms of mental illness.
As well a risk factor, childhood maltreatment appears to be associated with poorer clinical outcomes in bipolar, with more severe and more frequent mood episodes, 22 earlier onset, increased risk of suicide and comorbid substance misuse. 23 The relationship between childhood abuse and the severity of bipolar adds further weight to its position as a potential causative factor for the disorder. Notwithstanding, childhood maltreatment does not appear to be specifically related to psychotic symptoms or a diagnosis of bipolar type I over type II. 21 , 24
Whilst it seems likely that childhood traumatic events increase the risk of bipolar, why or how they do this remains unclear but is the focus of ongoing research. Traumatic events are linked to increased levels of affective instability or emotional dysregulation more generally in people with bipolar and this represents one possible mechanism of action. 107 Other dimensions of psychopathology such as hostility and impulsivity, along with affective instability have been shown to mediate the association between childhood maltreatment and outcomes in bipolar, 108 while alterations in the hypothalamic–pituitary–adrenal (HPA) axis, 109 increased levels of BDNF and inflammatory cytokines 110 and reduced limbic grey matter volume 111 represent possible neurobiological underpinnings of the effect of childhood trauma and how this may lead to later psychopathology and bipolar, in particular.
It should be noted that there is difficulty in determining to what extent childhood maltreatment is a cause or consequence of the predisposition to develop bipolar, as parental psychopathology may confer a genetic risk of the disorder, as well as increased risk of childhood maltreatment. 112 The retrospective nature of these studies introduces the possibility of recall bias with regard to childhood adversity, and at present, there are few prospective studies investigating the association between childhood maltreatment and bipolar.
Psychological stressors
Recent stressful life events are known to affect the course of bipolar, 113 although their relationship with the onset of the disorder has been less extensively investigated compared with unipolar depression. 49 A systematic review by Tsuchiya and colleagues 49 identified four studies investigating stressful life events prior to the onset of bipolar, the three largest of which found an increased risk of onset within 6 months of such events. A meta-analysis found that patients experience more life events prior to relapses into either manic or depressive episodes than during euthymic periods, although the rate of significant life events prior to the onset of bipolar was similar to unipolar depression. 25 Other studies have supported the association between life events and the onset of bipolar, including a large case-control study which found that stressful life events were associated with a first hospitalization for a manic episode, particularly suicide of a first-degree relative, but also recent marriage, divorce, disability or unemployment. 26 There are a number of confounders to these associations, particularly with regard to suicide of a first-degree relative, where genetic factors play a significant role, as death due to other causes was not associated with hospitalization. 26 A bidirectional relationship has also been suggested for stressful life events in bipolar, as there is evidence that these events occur both prior to and following mood episodes. 27
There is also evidence for specific life events conferring a risk for bipolar, such as early parental loss and childbirth. The systematic review by Tsuchiya and colleagues 49 found that only 3 of the 10 studies investigating parental loss identified an association with bipolar, although it is noteworthy that one of these was a very large cohort study which adjusted for a number of confounders, including family history of mental illness. 53 A meta-analysis found that childbirth specifically increased the risk of mood episodes in patients with bipolar, more so than relapses in unipolar depression or schizophrenia. 25 Tsuchiya and colleagues 49 identified only three studies investigating onset of bipolar following childbirth, but each found an association with subsequent bipolar diagnosis within 12 months. This is perhaps unsurprising, considering the association between puerperal psychosis and bipolar, 114 but it is unclear whether the reason for the association is genetic, hormonal or related to childbirth as a life event.
However, life events are relatively nonspecific in relation to mental and physical illness, and appear to be associated not only with the onset of bipolar disorder and unipolar depression, but also psychosis, 115 anxiety disorders, 116 ischaemic stroke 117 and circulatory disorders. 118 While gene–environment interactions have been identified between life events and the onset of specific disorders, 12 the use of checklists to identify life events in such studies has been criticized as lacking sufficient detail with regard to the severity and context of such events. 119 These methodological issues make it difficult to establish causation between life events and development of bipolar.
Substance misuse
Bipolar is frequently comorbid with misuse of substances, including cannabis, opioids, cocaine, sedatives and alcohol, 50 , 52 and causality has been suggested in both directions. 120 While the high level of comorbidity is undeniable, causality it much harder to ascertain as there is often difficulty in establishing the temporal relationship between substance misuse and the onset of mental illness. This is compounded by the relative lack of prospective, longitudinal studies examining the relationship between substance misuse and bipolar. 121
There is increasing evidence that cannabis use can act as a risk factor for the development of bipolar as well as psychotic disorders. A recent systematic review by Gibbs and colleagues 28 identified several studies supporting a link between cannabis use and subsequent relapse of manic symptoms. This review also included a meta-analysis of two large prospective cohort studies 29 , 30 which found that cannabis use almost trebled the risk of new-onset subthreshold manic symptoms after adjusting for potential confounding factors. A further large prospective cohort study found cannabis use increased the risk of first episode bipolar by a factor of 5 after adjusting for confounders, and demonstrated evidence of a dose–response relationship. 31 Other studies were more equivocal, finding increased risk of bipolar only in those with weekly to daily cannabis use and no dose–response relationship, 32 or increased risk only in those with a past year episode of depression. 52 Recently, a prospective analysis has demonstrated cannabis use at age 17 is associated with hypomania in young adulthood independent of psychotic symptoms and other important confounders. Further path analysis indicated cannabis use is one mechanism by which childhood abuse translates to increased risk of bipolar symptoms. 33
Other substances of abuse are also important in the risk of bipolar. Prospective studies have linked opioid use to an increased risk of developing bipolar, which is greater than other mood disorders. 34 , 35 A further study found that alcohol and drug abuse or dependence before the age of 25 increased the odds of developing subsequent bipolar, although differences between specific drugs were not examined. 36 Cocaine use has also been implicated, although is less well studied, 37 and as stimulant use can precipitate mania or similar symptoms, 120 this may lead to inappropriate diagnosis of bipolar, 122 rather than act as a causative factor.
There are significant confounding factors to associations between bipolar and substance misuse, which remain despite attempts at adjustment within the studies. It has been suggested that cannabis may serve as self medication for bipolar illness, 123 and therefore may be used by those with subthreshold symptoms prior to the onset of bipolar. Furthermore, there is evidence that shared genetic factors confer risk for developing both substance misuse disorders and bipolar, 124 , 125 while childhood maltreatment is also associated with both disorders. 20 , 22 , 113
Medical comorbidity
Bipolar is known to be comorbid with a number of medical and psychiatric conditions. 51 , 38 , 39 There are multiple reasons for this, including shared genetic and environmental vulnerabilities, consequences of treatment, recognition bias on the part of clinicians as well as the potential for a direct causal relationship in either direction.
There is strong evidence for the association between bipolar and irritable bowel syndrome (IBS) 51 highlighted in a recent large meta-analysis of retrospective cohort studies. 40 However, potentially important confounders, such as antidepressant use, were not adjusted for. There is also evidence that both disorders may share inflammatory 51 , 126 , 127 and stress-related aetiologies, 25 , 128 which could give rise to this association.
Similarly, recent meta-analyses have shown asthma, 41 obesity, 42 migraine 43 and head injury 44 are associated with bipolar. The evidence for these associations is mediated by the relatively small number of studies included, most of which were cross sectional and lacked data to adjust for confounding factors. However, for asthma, a retrospective cohort 45 and large prospective study 46 also support the association, which may be mediated by shared inflammatory pathways 126 , 127 or the use of corticosteroids during early childhood. 38 , 45 Medication and lifestyle factors significantly confound the association with obesity, for which there are few prospective studies and weak evidence for a directly causal relationship, while the association with traumatic brain injury is potentially confounded by ‘accident proneness’ or physical abuse. 129 There is evidence of increased prevalence of bipolar in patients with multiple sclerosis (MS) 47 , 130 which cannot be completely accounted for by steroid-induced mania, and in some instances, psychiatric symptoms may predate the diagnosis of MS. 131 However, other studies have not supported this association. 38
A meta-analysis reported high lifetime prevalence of anxiety disorders in bipolar patients, 48 while ADHD, conduct disorders, aggression and impulsivity also appeared to increase risk of developing bipolar. 39
Prodromal features and bipolar at-risk criteria
It is becoming increasingly recognised that bipolar, like schizophrenia, has a prodromal phase which can be identified prior to development of the full illness. 132 , 133 However, one issue with research into this area is the potential conflation of the concepts of a prodrome for bipolar, referring to symptoms that can be retrospectively identified as preceding the onset of the disorder, and a ‘risk syndrome’ consisting of clinical features, comorbidities and risk factors which increase the risk of later developing bipolar. 134 At present, neither prodrome nor risk syndrome has been fully defined, although the bipolar at-risk (BAR) assessment tool has demonstrated predictive validity and reliability for identifying those at risk of bipolar, with around 23% of those identified transitioning to mania or hypomania. 135 A study using the BAR assessment tool criteria found that cyclothymia had the best overall clinical utility for case finding and screening when focusing on depressed youths with an early transition to bipolar. The clinical utility profile of subthreshold mania, antidepressant emergent elation, family history of bipolar and atypical depression suggested they were better for screening out noncases. 136 However, other studies have questioned the associations between clinical characteristics of depression and transition to bipolar. 52
The low positive predictive value of these precursors reduces their usefulness, and of the significant proportion of those ‘at risk’ who do not go on to develop bipolar there is limited understanding of what factors are protective against this transition, or how this group differs from those who do develop bipolar. 134 Future research should focus on identifying differences in this group, while continuing to refine screening tools for prodromal identification and risk syndromes in prospective studies. Focusing on transition to first-episode mania may have greater reliability in identifying cases. 134
First-episode bipolar mania has an annual incidence of around 5 per 100,000 of population, 137 and peak incidence occurs between 21–25 years. 138 Although the incidence of first-episode mania is equal between males and females, 137 studies have found that age of onset is around 5 years earlier for men. 139 A meta-analysis of longitudinal studies of first-episode mania found that 87.5% of patients achieve syndromal recovery within the first year, meaning they no longer meet criteria for diagnosis. However, the symptomatic recovery rates (essentially defined as being symptom free) were 62.1% within the first year, while 41% experience a recurrence of a manic, mixed or depressed episode over the same period. 140 Considering the relatively poor outcome in such patients, the potential to identify a risk syndrome or prodromal phase of bipolar in those presenting with a depressive illness offers the opportunity to intervene at an earlier stage, leading to improved outcomes. 68
Risk factors for bipolar are numerous, both genetic and environmental, but low attributable risk, inconsistency of results, inability to identify the temporality of the relationship, lack of a clear biological mechanism and the nonspecific nature of many risk factors means that causation is difficult to assign in an individual patient. Studies of environmental risk were also unable to completely adjust for confounding. However, there is evidence that severity of bipolar is related to childhood emotional abuse and the degree of cannabis misuse, suggesting a dose–response relationship. The association with T. gondii is also strong, with some evidence of biological plausibility, although concerns remain about temporality. Bipolar is associated with medical comorbidities such as IBS and asthma, which may point towards shared inflammatory pathophysiology of the disorders, while other psychiatric disorders and clinical features that predate the onset of bipolar may point towards an identifiable ‘risk syndrome’. Future research into these risk factors should focus on establishing temporality, whether the severity of bipolar is linked to the risk factor, and identifying potential neurobiological and environmental mechanisms to explain the associations. Finally, research into gene–environment interactions is required to link existing evidence on genetic and environmental risks.
Funding: TR is partly funded through the National Institute of Health Research as an academic clinical fellow. The authors received no financial support for the research, authorship, or publication of this article.
Conflict of interest statement: The authors declare that there is no conflict of interest.

Contributor Information
Tobias A. Rowland, Unit of Mental Health and Wellbeing, Division of Health Sciences, University of Warwick, Coventry, CV4 7AL, UK.
Steven Marwaha, Division of Health Sciences, University of Warwick, Coventry, UK. Coventry and Warwick-shire Partnership Trust, The Caludon Centre, Coventry, UK.
- Open access
- Published: 06 November 2018
The challenges of living with bipolar disorder: a qualitative study of the implications for health care and research
- Eva F. Maassen ORCID: orcid.org/0000-0003-0211-0994 1 , 2 ,
- Barbara J. Regeer 1 ,
- Eline J. Regeer 2 ,
- Joske F. G. Bunders 1 &
- Ralph W. Kupka 2 , 3
International Journal of Bipolar Disorders volume 6 , Article number: 23 ( 2018 ) Cite this article
38k Accesses
18 Citations
21 Altmetric
Metrics details
In mental health care, clinical practice is often based on the best available research evidence. However, research findings are difficult to apply to clinical practice, resulting in an implementation gap. To bridge the gap between research and clinical practice, patients’ perspectives should be used in health care and research. This study aimed to understand the challenges people with bipolar disorder (BD) experience and examine what these challenges imply for health care and research needs.
Two qualitative studies were used, one to formulate research needs and another to formulate healthcare needs. In both studies focus group discussions were conducted with patients to explore their challenges in living with BD and associated needs, focusing on the themes diagnosis, treatment and recovery.
Patients’ needs are clustered in ‘disorder-specific’ and ‘generic’ needs. Specific needs concern preventing late or incorrect diagnosis, support in search for individualized treatment and supporting clinical, functional, social and personal recovery. Generic needs concern health professionals, communication and the healthcare system.
Patients with BD address disorder-specific and generic healthcare and research needs. This indicates that disorder-specific treatment guidelines address only in part the needs of patients in everyday clinical practice.
Bipolar disorder (BD) is a major mood disorder characterized by recurrent episodes of depression and (hypo)mania (Goodwin and Jamison 2007 ). According to the Diagnostic and Statistical Manual 5 (DSM-5), the two main subtypes are BD-I (manic episodes, often combined with depression) and BD-II (hypomanic episodes, combined with depression) (APA 2014 ). The estimated lifetime prevalence of BD is 1.3% in the Dutch adult population (de Graaf et al. 2012 ), and BD is associated with high direct (health expenditure) and indirect (e.g. unemployment) costs (Fajutrao et al. 2009 ; Michalak et al. 2012 ), making it an important public health issue. In addition to the economic impact on society, BD has a tremendous impact on patients and their caregivers (Granek et al. 2016 ; Rusner et al. 2009 ). Even between mood episodes, BD is often associated with functional impairment (Van Der Voort et al. 2015 ; Strejilevich et al. 2013 ), such as occupational or psychosocial impairment (Huxley and Baldessarini 2007 ; MacQueen et al. 2001 ; Yasuyama et al. 2017 ). Apart from symptomatic recovery, treatment can help to overcome these impairments and so improve the person’s quality of life (IsHak et al. 2012 ).
Evidence Based Medicine (EBM), introduced in the early 1990s, is a prominent paradigm in modern (mental) health care. It strives to deliver health care based on the best available research evidence, integrated with individual clinical expertise (Sackett et al. 1996 ). EBM was introduced as a new paradigm to ‘de - emphasize intuition’ and ‘ unsystematic clinical experience’ (Guyatt et al. 1992 ) (p. 2420). Despite its popularity in principle (Barratt 2008 ), EBM has also been criticized. One such criticism is the ignorance of patients’ preferences and healthcare needs (Bensing 2000 ). A second criticism relates to the difficulty of adopting evidence-based treatment options in clinical practice (Bensing 2000 ), due to the fact that research outcomes measured in ‘the gold standard’ randomized-controlled trials (RCTs) seldom correspond to the outcomes clinical practice seeks and are not responsive to patients’ needs (Newnham and Page 2010 ). Moreover, EBM provides an overview on population level instead of individual level (Darlenski et al. 2010 ). Thus, adopting research evidence in clinical practice entails difficulties, resulting in an implementation gap.
To bridge the gap between research and clinical practice, it is argued that patients’ perspectives should be used in both health care and research. Patients have experiential knowledge about their illness, living with it in their personal context and their care needs (Tait 2005 ). This is valuable for both clinical practice and research as their knowledge complements that of health professionals and researchers (Tait 2005 ; Broerse et al. 2010 ; Caron-Flinterman et al. 2005 ). This source of knowledge can be used in the process of translating evidence into clinical practice (Schrevel 2015 ). Moreover, patient participation can enhance the clinical relevance of and support for research and the outcomes in practice (Abma and Broerse 2010 ). Hence, it is argued that these perspectives should be explicated and integrated into clinical guidelines, clinical practice, and research (Misak 2010 ; Rycroft-Malone et al. 2004 ).
Given the advantages of including patients’ perspectives, patients are increasingly involved in healthcare services (Bagchus et al. 2014 ; Larsson et al. 2007 ), healthcare quality (e.g. guideline development) (Pittens et al. 2013 ) and health-related research (e.g. agenda setting, research design) (Broerse et al. 2010 ; Boote et al. 2010 ; Elberse et al. 2012 ; Teunissen et al. 2011 ). However, patients’ perspectives on health care and on research are often studied separately. We argue that to be able to provide care focused on the patients and their needs, care and research must closely interact.
We hypothesize that the challenges BD patients experience and the associated care and research needs are interwoven, and that combining them would provide a more comprehensive understanding. We hypothesize that this more comprehensive understanding would help to close the gap between clinical practice and research. For this reason, this study aims to understand the challenges people with BD experience and examine what these challenges imply for healthcare and research needs.
To understand the challenges and needs of people with BD, we undertook two qualitative studies. The first aimed to formulate a research agenda for BD from a patient’s perspective, by gaining insights into their challenges and research needs. A second study yielded an understanding of the care needs from a patient’s perspective. In this article, the results of these two studies are combined in order to investigate the relationship between research needs and care needs. Challenges are defined as ‘difficulties patients face, due to having BD’. Care needs are defined as that what patients ‘desire to receive from healthcare services to improve overall health’ (Asadi-Lari et al. 2004 ) (p. 2). Research needs are defined as that what patients ‘desire to receive from research to improve overall health’.
Study on research needs
In this study, mixed-methods were used to formulate research needs from a patient’s perspective. First six focus group discussions (FGDs) with 35 patients were conducted to formulate challenges in living with BD and hopes for the future, and to formulate research needs arising from these difficulties and aspirations. These research needs were validated in a larger sample (n = 219) by means of a questionnaire. We have reported this study in detail elsewhere (Maassen et al. 2018 ).
Study on care needs
This study was part of a nationwide Dutch project to generate a practical guideline for BD: a translation of the existing clinical guideline to clinical practice, resulting in a standard of care that patients with BD could expect. The practical guideline (Netwerk Kwaliteitsontwikkeling GGZ 2017 ) was written by a taskforce comprising health professionals, patients. In addition to the involvement of three BD patients in the taskforce, a systematic qualitative study was conducted to gain insight into the needs of a broader group of patients.
Participants and data collection
To formulate the care needs of people with BD, seven FGDs were conducted, with a total of 56 participants, including patients (n = 49) and caregivers (n = 9); some participants were both patient and caregiver. The inclusion criteria for patients were having been diagnosed with BD, aged 18 years or older and euthymic at time of the FGDs. Inclusion criteria for caregivers were caring for someone with BD and aged 18 years or older. To recruit participants, a maximum variation sampling strategy was used to collect a broad range of care needs (Kuper et al. 2008 ). First, all outpatient clinics specialized in BD affiliated with the Dutch Foundation for Bipolar Disorder (Dutch: Kenniscentrum Bipolaire Stoornissen) were contacted by means of an announcement at regular meetings and by email if they were interested to participate. From these outpatient clinics, patients were recruited by means of flyers and posters. Second, patients were recruited at a quarterly meeting of the Dutch patient and caregiver association for bipolar disorder. The FGDs were conducted between March and May 2016.
The FGDs were designed to address challenges experienced in BD health care and areas of improvement for health care for people with BD. The FGDs were structured by means of a guide and each session was facilitated by two moderators. The leading moderator was either BJR or EFM, having both extensive experience with FGD’s from previous studies. The first FGD explored a broad range of needs. The subsequent six FGDs aimed to gain a deeper understanding of these care needs, and were structured according to the outline of the practical guideline (Netwerk Kwaliteitsontwikkeling GGZ 2017 ). Three chapters were of particular interest: diagnosis, treatment and recovery. These themes were discussed in the FGDs, two in each session, all themes three times in total. Moreover, questions on specific aspects of care formulated by the members of the workgroup were posed. The sessions took 90–120 min. The FGDs were audiotaped and transcribed verbatim. A summary of the FGDs was sent to the participants for a member check.
Data analysis
To analyze the data on challenges and needs, a framework for thematic analysis to identify, analyze and report patterns (themes) in qualitative data sets by Braun and Clarke ( 2006 ) was used. First, we familiarized ourselves with the data by carefully reading the transcripts. Second, open coding was used to derive initial codes from the data. These codes were provided to quotes that reflected a certain challenge or care need. Third, we searched for patterns within the codes reflecting challenges and within those reflecting needs. For both challenges and needs, similar or overlapping codes were clustered into themes. Subsequently, all needs were categorized as ‘specific’ or ‘generic’. The former are specific to BD and the latter are relevant for a broad range of psychiatric illnesses. Finally, a causal analysis provided a clear understanding of how challenges related to each other and how they related to the described needs.
To analyze the data on needs regarding recovery, four domains were distinguished, namely clinical, functional, social and personal recovery (Lloyd et al. 2008 ; van der Stel 2015 ). Clinical recovery refers to symptomatic remission; functional recovery concerns recovery of functioning that is impaired due to the disorder, particularly in the domain of executive functions; social recovery concerns the improvement of the patient’s position in society; personal recovery concerns the ability of the patient to give meaning to what had happened and to get a grip on their own life. The analyses were discussed between BR and EM. The qualitative software program MAX QDA 11.1.2 was used (MaxQDA).
Ethical considerations
According to the Medical Ethical Committee of VU University Medical Center, the Medical Research Involving Human Subjects Act does not apply to the current study. All participants gave written or verbal informed consent regarding the aim of the study and for audiotaping and its use for analysis and scientific publications. Participation was voluntary and participants could withdraw from the study at any time. Anonymity was ensured.
This section is in three parts. The first presents the participants’ characteristics. The second presents the challenges BD patients face, derived from both studies, and the disorder-specific care and research needs associated with these challenges. The third part describes the generic care needs that patients formulated.
Characteristics of the participants
In the study on care needs, 56 patients and caregivers participated. The mean age of the participants was 52 years (24–75), of whom 67.8% were women. The groups varied from four to sixteen participants, and all groups included men and women. Of all participants 87.5% was diagnosed with BD, of whom 48.9% was diagnosed with BD I. 3.5% was both caregivers and diagnosed with BD. Of 4 patients the age was missing, and from 6 patients the bipolar subtype.
Despite the fact that participants acknowledge the inevitable diagnostic difficulties of a complex disorder like BD, in both studies they describe a range of challenges in different phases of the diagnostic process (Fig. 1 ). Patients explained that the general practitioner (GP) and society in general did not recognize early-warning signs and mood swings were not well interpreted, resulting in late or incorrect diagnosis. Patients formulated a need for more research on what early-warning signs could be and on how to improve GPs’ knowledge about BD. Formulated care needs were associated with GPs using this knowledge to recognize early-warning signs in individual patients. One participant explained that certain symptoms must be noticed and placed in the right context:
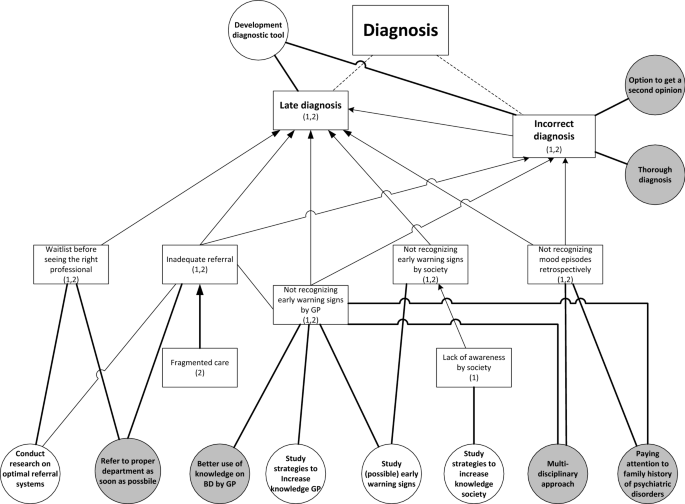
Challenges with diagnosis (squares) including relating research needs (white circles) and care needs (grey circles). (1): mentioned in study on research needs; (2): mentioned in study on care needs. Dotted lines: division of challenges into sub challenges. Arrows: causal relation between challenges
I call it, ‘testing overflow of ideas’. [….] When it happens for the first time you yourself do not recognize it. Someone else close to you or the health professional, who is often not involved yet, must signal it. (FG6)
Moreover, these challenges are associated with the need to pay attention to family history and to use a multidisciplinary approach to diagnosis to benefit from multiple perspectives. The untimely recognition of early symptoms also results in another challenge: inadequate referral to the right specialized health professional. After referral, people often face a waiting list, again causing delay in the diagnostic process. These challenges result in the need for research on optimal referral systems and the care need for timely referral. One participant described her process after the GP decided to refer her:
But, yes, at that moment the communication wasn’t good at all. Because the general practitioner said: ‘she urgently has to be seen by someone’. Subsequently, three weeks went by, until I finally arrived at depression [department]. And at that department they said: ‘well, you are in the wrong place, you need to go to bipolar [department ]’. (FG1)
The challenge of being misdiagnosed is associated with the need to be able to ask for a second opinion and to have a timely and thorough diagnosis. On the one hand, it is important for patients that health professionals quickly understand what is going on, on the other hand that health professionals take the time to thoroughly investigate the symptoms by making several appointments.
From both studies, two main challenges related to the treatment of BD were derived (Fig. 2 ). The first is finding appropriate and satisfactory treatment. Participants explained that it is difficult to find the right medication and dosage that is effective and has acceptable side-effects. One participant illustrates:
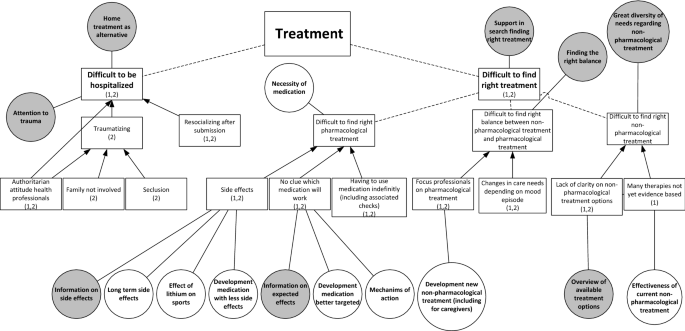
Challenges with treatment (squares) including relating research needs (white circles) and care needs (grey circles). (1): mentioned in study on research needs; (2): mentioned in study on care needs. Dotted lines: division of challenges into sub challenges. Arrows: causal relation between challenges
I think, at one point, we have to choose, either overweight or depressed. (FG1)
Some participants said that they struggle with having to use medication indefinitely, including the associated medical checks. The difficult search for the right pharmacological treatment results in the need for research on long-term side-effects, on the mechanism of action of medicine and on the development of better targeted medication with fewer adverse side-effects. In care, patients would appreciate all the known information on the side-effects and intended effects. One participant explained the importance of being properly informed about medication:
I don’t read anything [about medication], because then I wouldn’t dare taking it. But I do think, when you explain it well, the advantages, the disadvantages, the treatment, the idea behind it, that would help a lot in compliance. (FG1)
A second aspect is the challenge of finding non-pharmacological therapies that fit patients’ needs. They said they and the health professionals often do not know which non-pharmacological therapies are available and effective:
But we found the carefarm ourselves Footnote 1 [….]. You have to search for yourself completely. Yes, I actually hoped that that would be presented to you, like: ‘this would be something for you’. (FG3)
Participants mentioned a variety of non-pharmacological therapies they found useful, namely cognitive behavior therapy (CBT), EMDR, running therapy, social-rhythm training, light therapy, mindfulness, psychotherapy, psychoeducation, and training in living with mood swings. They formulated the care need to receive an overview of all available treatment options in order to find a treatment best suited to their needs. They would appreciate research on the effectiveness of non-pharmacological treatments.
A third aspect within this challenge is finding the right balance between non-pharmacological and pharmacological treatment. Participants differed in their opinion about the need for medication. Whereas some participants stated that they need medication to function, others pointed out that they found non-pharmacological treatments effective, resulting in less or no medication use. They explained that the preferred balance can also change over time, depending on their mood. However, they experience a dominant focus on pharmacological treatment by the health professionals. To address this challenge, patients need support in searching for an appropriate balance.
Next to the challenge of finding appropriate and satisfactory treatment, a second treatment-related challenge is hospitalization. Participants often had a traumatic experience, due to seclusion, the authoritarian attitudes of clinical staff, and not involving their family. Patients therefore found it important to try preventing being hospitalized, for example by means of home treatment, which some participants experienced positively. Despite the challenges relating to hospitalization, participants did acknowledge that in some cases it cannot be avoided, in which case they urged for close family involvement, open communication and being treated by their own psychiatrist. Still, in the study on research needs, hospitalization did not emerge as an important research theme.
In both studies, participants described challenges in all four domains of recovery: clinical, functional, social and personal (Fig. 3 ). In relation to clinical recovery, participants struggled with the symptoms of mood episodes, the psychosis and the fear of a future episode. In contrast, some participants mentioned that they sometimes miss the hypomanic state they had experienced previously due to effective medical treatment. In the domain of functional recovery, participants contended with having to function below their educational level due to residual symptoms, such as cognitive problems, due to the importance of preventing stress in order to reduce the risk of a new episode, and because of low energy levels. This leads to the care need that health professionals should pay attention to the level of functioning of their patients.
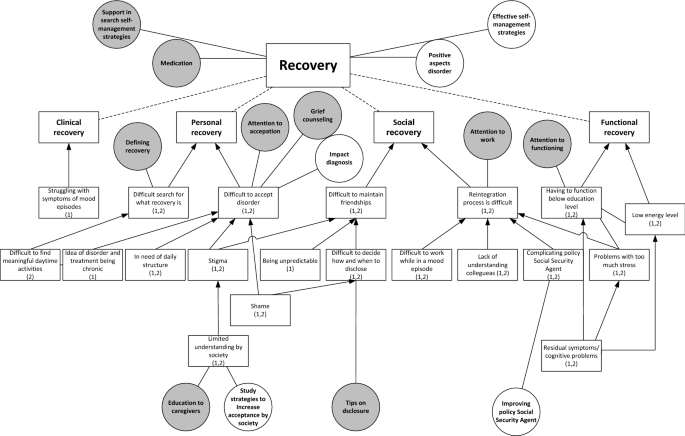
Challenges with recovery (squares) including relating research needs (white circles) and care needs (grey circles). (1): mentioned in study on research needs; (2): mentioned in study on care needs. Dotted lines: division of challenges into sub challenges. Arrows: causal relation between challenges
In the domain of social recovery, participants described challenges with maintaining friendships, due to stigma, being unpredictable and with deciding when to disclose the disorder. The latter resulted in the care need for tips on disclosure. Moreover, patients experienced challenges with reintegration to work, due to colleagues’ lack of understanding, problems with functioning during an episode, the complicating policy of the (Dutch) Employee Insurance Agency Footnote 2 in relation to the fluctuating course of BD and the negative impact of stress. These challenges are associated with the care need that health professionals should pay attention to work and the need for research on how to improve the Social Security Agency’s policy.
For their personal recovery, participants struggled with acceptance of the disorder, due to shame, stigma, having to live by structured rules and disciplines, and the chronic nature of BD. This results in care needs for grief counselling and attention to acceptance and the need for research on the impact of being diagnosed with BD. Limited understanding within society also causes problems with acceptance, corresponding with the care need for education for caregivers and for research on how to increase social acceptance. Another challenge in personal recovery was discovering what recovery means and what constitute meaningful daily activities. Patients appreciated the support of health professionals in this area. One participant described the difficult search for the meaning of recovery:
I have been looking to recover towards the situation [before diagnosis] for a long time; that I could do what I always did and what I liked. But then I was confronted with the fact that I shouldn’t expect that to happen, or only with a lot of effort. (…) Then you start thinking, now what? A compromise. I don’t want to call that recovery, but it is a recovered, partly accepted, situation. But it is not recovery as I expected it to be. (FG5)
In general, participants considered frequent contact with a nurse or psychiatrist supportive, to help them monitor their mood and help them find (efficient) self-management strategies. Most participants appreciated the involvement of caregivers in the treatment and contact with peers.
Generic care needs
We have described BD-specific needs, but patients mentioned also mentioned several generic care needs. The latter are clustered into three categories. The first concerns the health professionals . Participants stressed the importance of a good health professional, who carefully listens, takes time, and makes them feel understood, resulting in a sense of connection. Furthermore, a good health professional treats beyond the guideline, and focuses on the needs of the individual patient. When there is no sense of connection, it should be possible to change to another health professional. The second category concerns communication between the patient and the health professional . Health professionals should communicate in an open, honest and clear way both in the early diagnostic phase and during treatment. Open communication facilitates individualized care, in which the patient is involved in decision making. In addition, participants wanted to be treated as a person, not as a patient, and according to a strength-based approach. The third category concerns needs at the level of the healthcare system . Participants struggled with the availability of the health professionals and preferred access to good care 24/7 and being able to contact their health professional quickly when necessary. Currently, according to the participants, the care system is not geared to the mood swings of BD, because patients often faced waiting lists before they could see a health professional.
Is adequate treatment also having a number from a mental health institution you can always call when you are in need, that you can go there? And not that you can go in three weeks, but on a really short notice. So at least a phone call. (FG3)
Participants were often frustrated by the limited collaboration between health professionals, within their own team, between departments of the organization, and between different organizations, including complementary health professionals. They would appreciate being able to merge their conventional and complementary treatment, with greater collaboration among the different health professionals. Furthermore, they would like continuity of health professionals as this improves both the diagnostic phase and treatment, and because that health professional gets to know the patient.
We hypothesized that research and care needs of patients are closely intertwined and that understanding these, by explicating patients’ perspectives, could contribute to closing the gap between research and care. Therefore, this study aimed to understand the challenges patients with BD face and examine what these imply for both healthcare and research. In the study on needs for research and in the study on care needs, patients formulated challenges relating to receiving the correct diagnosis, finding the right treatment, including the proper balance between non-pharmacological and pharmacological treatment, and to their individual search for clinical, functional, social and personal recovery. The formulated needs in both studies clearly reflected these challenges, leading to closely corresponding needs. Another important finding of our study is that patients not only formulate disorder-specific needs, but also many generic needs.
The needs found in our study are in line with the current literature on the needs of patients with BD, namely for more non-pharmacological treatment (Malmström et al. 2016 ; Nestsiarovich et al. 2017 ), timely recognition of early-warning signs and self-management strategies to prevent a new episode (Goossens et al. 2014 ), better information on treatment and treatment alternatives (Malmström et al. 2016 ; Neogi et al. 2016 ) and coping with grief (Goossens et al. 2014 ). Moreover, the need for frequent contact with health professionals, being listened to, receiving enough time, shared decision-making on pharmacological treatment, involving caregivers (Malmström et al. 2016 ; Fisher et al. 2017 ; Skelly et al. 2013 ), and the urge for better access to health care and continuity of health professionals (Nestsiarovich et al. 2017 ; Skelly et al. 2013 ) are confirmed by the literature. Our study added to this set of literature by providing insights in patients’ needs in the diagnostic process and illustrating the interrelation between research needs and care needs from a patient’s perspective.
The generic healthcare needs patients addressed in this study are clustered into three categories: the health professional , communication between the patient and the health professional and the health system. These categories all fit in a model of patient-centered care (PCC) by Maassen et al. ( 2016 ) In their review, patients’ perspectives on good care are compared with academic perspectives of PCC and a model of PCC is created comprising four dimensions: patient, health professional, patient – professional interaction and healthcare organization. All the generic needs formulated in this study fit into these four dimensions. The need to be treated as a person with strengths fits the dimension ‘patient’, and the need for a good health professional who carefully listens, takes time and makes them feel understood, resulting in a good connection with the professional, fits the dimension ‘health professional’ of this model. Furthermore, patients in this study stressed the importance of open communication in order to provide individualized care, which fits the dimension of ‘patient–professional interaction’. The urge for better access to health care, geared to patients’ mood swings and the need for better collaboration between health professionals and continuity of health professionals fits the dimension of ‘health care organization’ of the model. This study confirms the findings from the review and contributes to the literature stressing the importance of a patient-centered care approach (Mills et al. 2014 ; Scholl et al. 2014 ).
In the prevailing healthcare paradigm, EBM, the best available evidence should guide treatment of patients (Sackett et al. 1996 ; Darlenski et al. 2010 ). This evidence is translated into clinical and practical guidelines, which thus facilitate EBM and could be used as a decision-making tool in clinical practice (Skelly et al. 2013 ). For many psychiatric disorders, treatment is based on such disorder - specific clinical and practical guidelines. However, this disease-focused healthcare system has contributed to its fragmented nature Stange ( 2009 ) argues that this fragmented care system has expanded without the corresponding ability to integrate and personalize accordingly. We argue that acknowledging that disorder - specific clinical and practical guidelines address only parts of the care needs is of major importance, since otherwise important aspects of the patients’ needs will be ignored. Because there is an increasing acknowledgement that health care should be responsive to the needs of patients and should change from being disease-focused towards being patient-focused (Mead and Bower 2000 ; Sidani and Fox 2014 ), currently in the Netherlands generic practical guidelines are written on specific care themes (e.g. co-morbidity, side-effects, daily activity and participation). These generic practical guidelines address some of the generic needs formulated by the patients in our study. We argue that in addition to disorder-specific guidelines, these generic practical guidelines should increasingly be integrated into clinical practice, while health professionals should continuously be sensitive to other emerging needs. We believe that an integration of a disorder-centered and a patient-centered focus is essential to address all needs a patient.
Strengths, limitations and future research
This study has several strengths. First, it contributes to the literature on the challenges and needs of patients with BD. Second, the study is conducted from a patient’s perspective. Moreover, addressing this aim by conducting two separate studies enabled us to triangulate the data.
This study also has several limitations. First, this study reflects the challenges, care needs and research needs of Dutch patient with BD and caregivers. Despite the fact that a maximum variation sampling strategy was used to derive a broad range of challenges and needs throughout the Netherlands, the Dutch setting of the study may limit the transferability to other countries. To understand the overlap and differences between countries, similar research should be conducted in other contexts. Second, given the design of the study, we could not differentiate between patients and caregivers since they participated together in the FGDs. More patients than caregivers participated in the study. For a more in-depth understanding of the challenges and needs faced by caregivers, in future research separate FGDs should be conducted. Third, due to the fixed outline of the practical guideline used to conduct the FGDs, only the healthcare needs for diagnosis, treatment and recovery of BD are studied. Despite the fact that these themes might cover a broad range of health care, it could have resulted in overlooking certain needs in related areas of well-being. Therefore, future research should focus on needs outside of these themes in order to provide a complete set of healthcare needs.
Patients and their caregivers face many challenges in living with BD. Our study contributes to the literature on care and research needs from a patient perspective. Needs specific for BD are preventing late or incorrect diagnosis, support in search for individualized treatment, and supporting clinical, functional, social and personal recovery. Generic healthcare needs concern health professionals, communication and the healthcare system. This explication of both disorder-specific and generic needs indicates that clinical practice guidelines should address and integrate both in order to be responsive to the needs of patients and their caregivers.
Care farm: farms that combine agriculture and services for people with disabilities (Iancu 2013 ). These farms are used as interventions in mental care throughout Europe and the USA to facilitate recovery (Iancu et al. 2014 ).
A government agency involved in the implementation of employee insurance and providing labor market and data services.
Abma T, Broerse J. Patient participation as dialogue: setting research agendas. Health Expect. 2010;13(2):160–73.
Article Google Scholar
APA. Beknopt overzicht van de criteria (DSM-5). Nederlands vertaling van de Desk Reference to the Diagnostic Criteria from DSM-5. Amsterdam: Boom; 2014.
Google Scholar
Asadi-Lari M, Tamburini M, Gray D. Patients’ needs, satisfaction, and health related quality of life: towards a comprehensive model. Health Qual Life Outcomes. 2004;2:1–15.
Bagchus C, Dedding C, Bunders JFG. “I”m happy that I can still walk’—participation of the elderly in home care as a specific group with specific needs and wishes. Health Expect. 2014;18(6):1–9.
Barratt A. Evidence based medicine and shared decision making: the challenge of getting both evidence and preferences into health care. Patient Educ Couns. 2008;73(3):407–12.
Bensing J. Bridging the gap. The separate worlds of evidence-based medicine and patient-centered medicine. Patient Educ Couns. 2000;39:17–25.
Article CAS Google Scholar
Boote J, Baird W, Beecroft C. Public involvement at the design stage of primary health research: a narrative review of case examples. Health Policy. 2010;95(1):10–23.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Broerse J, Zweekhorst M, van Rensen A, de Haan M. Involving burn survivors in agenda setting on burn research: an added value? Burns. 2010;36(2):217–31.
Caron-Flinterman JF, Broerse JEW, Bunders JFG. The experiential knowledge of patients: a new resource for biomedical research? Soc Sci Med. 2005;60(11):2575–84.
Darlenski RB, Neykov NV, Vlahov VD, Tsankov NK. Evidence-based medicine: facts and controversies. Clin Dermatol. 2010;28(5):553–7.
de Graaf R, ten Have M, van Gool C, van Dorsselaer S. Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands Mental Health Survey and Incidence Study-2. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):203–13.
Elberse J, Pittens C, de Cock Buning T, Broerse J. Patient involvement in a scientific advisory process: setting the research agenda for medical products. Health Policy. 2012;107(2–3):231–42.
Fajutrao L, Locklear J, Priaulx J, Heyes A. A systematic review of the evidence of the burden of bipolar disorder in Europe. Clin Pract Epidemiol Ment Health. 2009;5(1):3.
Fisher A, Manicavasagar V, Sharpe L, Laidsaar-Powell R, Juraskova I. A qualitative exploration of patient and family views and experiences of treatment decision-making in bipolar II disorder. J Ment Health. 2017;27(1):66–79.
Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorder and recurrent depression. 2nd ed. New York: Oxford University Press; 2007.
Goossens P, Knoopert-van der Klein E, Kroon H, Achterberg T. Self reported care needs of outpatients with a bipolar disorder in the Netherlands: a quantitative study. J Psychiatr Ment Health Nurs. 2014;14:549–57.
Granek L, Danan D, Bersudsky Y, Osher Y. Living with bipolar disorder: the impact on patients, spouses, and their marital relationship. Bipolar Disord. 2016;18(2):192–9.
Guyatt G, Cairns J, Churchill D, Cook D, Haynes B, Hirsh J, Irvine J, Levine M, Levine M, Nishikawa J, Sackett D, Brill-Edwards P, Gerstein H, Gibson J, Jaeschke R, Kerigan A, Neville A, Panju A, Detsky A, Enkin M, Frid P, Gerrity M, Laupacis A, Lawrence V, Menard J, Moyer V, Mulrow C, Links P, Oxman A, Sinclair J, Tugwell P. Evidence-based medicine: a new approach to teaching the practice of medicine. JAMA. 1992;268(17):2420–5.
Huxley N, Baldessarini R. Disability and its treatment in bipolar disorder patients. Bipolar Disord. 2007;9(1–2):183–96.
Iancu SC. New dynamics in mental health recovery and rehabilitation. Amsterdam: Vu University; 2013.
Iancu SC, Zweekhorst MBM, Veltman DJ, Van Balkom AJLM, Bunders JFG. Mental health recovery on care farms and day centres: a qualitative comparative study of users’ perspectives. Disabil Rehabil. 2014;36(7):573–83.
IsHak WW, Brown K, Aye SS, Kahloon M, Mobaraki S, Hanna R. Health-related quality of life in bipolar disorder. Bipolar Disord. 2012;14(1):6–18.
Kuper A, Lingard L, Levinson W. Critically appraising qualitative research. BMJ. 2008;337(7671):687–9.
Larsson IE, Sahlsten MJM, Sjöström B, Lindencrona CSC, Plos KAE. Patient participation in nursing care from a patient perspective: a grounded theory study. Scand J Caring Sci. 2007;21(3):313–20.
Lloyd C, Waghorn G, Williams PL. Conceptualising recovery in mental health. Br J Occup Ther. 2008;71:321–8.
Maassen EF, Schrevel SJC, Dedding CWM, Broerse JEW, Regeer BJ. Comparing patients’ perspectives of “good care” in Dutch outpatient psychiatric services with academic perspectives of patient-centred care. J Ment Health. 2016;26(1):1–11.
Maassen EF, Regeer BJ, Bunders JGF, Regeer EJ, Kupka RW. A research agenda for bipolar disorder developed from a patient’s perspective. J Affect Disord. 2018;239:11–17. https://doi.org/10.1016/j.jad.2018.05.061 .
Article PubMed Google Scholar
MacQueen GM, Young LT, Joffe RT. A review of psychosocial outcome in patients with bipolar disorder. Acta Psychiatr Scand. 2001;103(3):163–70.
Malmström E, Hörberg N, Kouros I, Haglund K, Ramklint M. Young patients’ views about provided psychiatric care. Nord J Psychiatry. 2016;70(7):521–7.
MaxQDA [Internet]. Available from: https://www.maxqda.com/ . Accessed 2 Aug 2018.
Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51(7):1087–110.
Michalak EE, Hole R, Livingston JD, Murray G, Parikh SV, Lapsley S, et al. Improving care and wellness in bipolar disorder: origins, evolution and future directions of a collaborative knowledge exchange network. Int J Ment Health Syst. 2012;6:16.
Mills I, Frost J, Cooper C, Moles DR, Kay E. Patient-centred care in general dental practice—a systematic review of the literature. BMC Oral Health. 2014;14(1):64.
Misak CJ. Narrative evidence and evidence-based medicine. J Eval Clin Pract. 2010;16(2):392–7.
Neogi R, Chakrabarti S, Grover S. Health-care needs of remitted patients with bipolar disorder: a comparison with schizophrenia. World J Psychiatry. 2016;6(4):431–41.
Nestsiarovich A, Hurwitz NG, Nelson SJ, Crisanti AS, Kerner B, Kuntz MJ, et al. Systemic challenges in bipolar disorder management: a patient-centered approach. Bipolar Disord. 2017;19(8):676–88.
Netwerk Kwaliteitsontwikkeling GGZ. Zorgstandaard Bipolaire stoornissen. 2017;1–54.
Newnham EA, Page AC. Bridging the gap between best evidence and best practice in mental health. Clin Psychol Rev. 2010;30(1):127–42.
Pittens C, Noordegraaf A, van Veen S, Broerse J. The involvement of gynaecological patients in the development of a clinical guideline for resumption of (work) activities in the Netherlands. Health Expect. 2013;18:1397–412.
Rusner M, Carlsson G, Brunt D, Nyström M. Extra dimensions in all aspects of life—the meaning of life with bipolar disorder. Int J Qual Stud Health Well-being. 2009;4(3):159–69.
Rycroft-Malone J, Seers K, Titchen A, Harvey G, Kitson A, McCormack B. What counts as evidence in evidence-based practice? J Adv Nurs. 2004;47(1):81–90.
Sackett D, Rosenberg W, Gray J, Haynes R, Richardson W. Evidence based medicine: what it is and what it isn’t. Br Med J. 1996;312(7023):71–2.
Scholl I, Zill JM, Härter M, Dirmaier J. An integrative model of patient-centeredness—a systematic review and concept analysis. PLoS ONE. 2014;9(9):e107828.
Schrevel SJC. Surrounded by controversy: perspectives of adults with ADHD and health professionals on mental healthcare. Amsterdam: VU University; 2015.
Sidani S, Fox M. Patient-centered care: clarification of its specific elements to facilitate interprofessional care. J Interprof Care. 2014;28(2):134–41.
Skelly N, Schnittger RI, Butterly L, Frorath C, Morgan C, McLoughlin DM, et al. Quality of care in psychosis and bipolar disorder from the service user perspective. Qual Health Res. 2013;23(12):1672–85.
Stange KC. The problem of fragmentation and the need for integrative solutions. Ann Fam Med. 2009;7(2):100–3.
Strejilevich SA, Martino DJ, Murru A, Teitelbaum J, Fassi G, Marengo E, et al. Mood instability and functional recovery in bipolar disorders. Acta Psychiatr Scand. 2013;128(3):194–202.
Tait L. Encouraging user involvement in mental health services. Adv Psychiatr Treat. 2005;11(3):168–75.
Teunissen T, Visse M, De Boer P, Abma TA. Patient issues in health research and quality of care: an inventory and data synthesis. Health Expect. 2011;16:308–22.
van der Stel. Het begrip herstel in de psychische gezondheidzorg, Leiden; 2015. p. 1–3.
Van Der Voort TYG, Van Meijel B, Hoogendoorn AW, Goossens PJJ, Beekman ATF, Kupka RW. Collaborative care for patients with bipolar disorder: effects on functioning and quality of life. J Affect Disord. 2015;179:14–22.
Yasuyama T, Ohi K, Shimada T, Uehara T, Kawasaki Y. Differences in social functioning among patients with major psychiatric disorders: interpersonal communication is impaired in patients with schizophrenia and correlates with an increase in schizotypal traits. Psychiatry Res. 2017;249:30–4.
Download references
Authors’ contributions
EFM designed the study, contributed to the data collection, managed the analysis and wrote the first draft of the manuscript. BJR designed the study and contributed to the data collection, data analysis, and writing of the manuscript. JFGB contributed to the study design and critical revision of the manuscript. EJR contributed to the study conception and critical revision of the manuscript. RWK contributed to the study design, acquisition of data, and critical revision of the manuscript. All authors contributed to the final manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
The authors received no financial support for the research.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and affiliations.
Athena Institute, Faculty of Earth and Life Sciences, VU University Amsterdam, Boelelaan 1085, 1081HV, Amsterdam, Netherlands
Eva F. Maassen, Barbara J. Regeer & Joske F. G. Bunders
Altrecht Institute for Mental Health Care, Nieuwe Houtenseweg 12, 3524 SH, Utrecht, Netherlands
Eva F. Maassen, Eline J. Regeer & Ralph W. Kupka
Amsterdam Public Health Research Institute, Amsterdam UMC, Vrije Universiteit Amsterdam, Psychiatry, De Boelelaan 1117, Amsterdam, Netherlands
Ralph W. Kupka
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Eva F. Maassen .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
Cite this article.
Maassen, E.F., Regeer, B.J., Regeer, E.J. et al. The challenges of living with bipolar disorder: a qualitative study of the implications for health care and research. Int J Bipolar Disord 6 , 23 (2018). https://doi.org/10.1186/s40345-018-0131-y
Download citation
Received : 06 June 2018
Accepted : 22 August 2018
Published : 06 November 2018
DOI : https://doi.org/10.1186/s40345-018-0131-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- General Healthcare
- Personal Recovery
- Focus Group Discussions
- Professional-patient Interaction

Understanding Bipolar Disorder: A Comprehensive Guide to Causes, Symptoms, and Treatment
B ipolar disorder is a complex mental health condition that affects millions of people worldwide.It is characterized by extreme shifts in mood , energy levels, and behavior. There are several types of bipolar disorder, including Bipolar I, Bipolar II, and Cyclothymic Disorder. Bipolar I is characterized by manic episodes that can last for several days or weeks, while Bipolar II involves hypomanic episodes and depressive episodes. Cyclothymic Disorder is a milder form of bipolar disorder with less severe mood swings.
The impact of bipolar disorder on daily functioning cannot be understated. The extreme highs and lows experienced by individuals with bipolar disorder can disrupt relationships, work, and overall quality of life.It is estimated that approximately 7 million adults in the United States are affected by bipolar disorder . However, with proper diagnosis, treatment, and support, individuals with bipolar disorder can lead fulfilling lives.
Causes and Risk Factors of Bipolar Disorder
The exact causes of bipolar disorder are not yet fully understood, but research suggests that it is likely a combination of genetic, neurochemical, and environmental factors.Studies have shown that there is a higher prevalence of bipolar disorder among individuals who have a family history of the condition, indicating a genetic component. Neurochemical imbalances, particularly involving neurotransmitters like serotonin, dopamine, and norepinephrine, have also been implicated in the development of bipolar disorder. Additionally, certain environmental factors, such as stressful life events or substance abuse, can trigger or exacerbate symptoms in individuals who are genetically predisposed to the condition.
For example, a study conducted by the National Institute of Mental Health found that individuals with a family history of bipolar disorder were more likely to develop the condition themselves, suggesting a genetic link . Another study published in the Journal of Affective Disorders found that stressful life events, such as the loss of a loved one or financial difficulties, were associated with an increased risk of bipolar disorder.
Symptoms of Bipolar Disorder
Bipolar disorder is characterized by two main types of episodes: manic episodes and depressive episodes. During a manic episode, individuals may experience a heightened sense of euphoria, extreme energy levels, racing thoughts, and impulsive behavior. They may engage in risky activities, such as excessive spending or substance abuse, and have a decreased need for sleep. On the other hand, depressive episodes are characterized by feelings of sadness, hopelessness, loss of interest in activities, fatigue, and changes in appetite and sleep patterns.
In addition to these main symptoms, individuals with bipolar disorder may also experience difficulty concentrating, irritability, and feelings of worthlessness or guilt. It is important to note that the severity and duration of these episodes can vary greatly from person to person.
For instance, during a manic episode, an individual may engage in impulsive and reckless behavior, such as excessive gambling or reckless driving. This behavior can have serious consequences, such as financial loss or legal issues. During a depressive episode, individuals may struggle with feelings of hopelessness and have difficulty performing everyday tasks, such as getting out of bed or going to work.
Diagnosis and Misdiagnosis of Bipolar Disorder
Diagnosing bipolar disorder can be challenging, as the symptoms can overlap with other mental health conditions, such as depression or anxiety disorders. Additionally, individuals with bipolar disorder may not recognize or acknowledge their symptoms, making it difficult for them to seek help. The diagnostic process typically involves a thorough psychiatric evaluation, which includes a detailed assessment of symptoms, medical history, and family history.
In order to meet the diagnostic criteria for bipolar disorder, an individual must have experienced at least one manic or hypomanic episode, along with depressive episodes. However, the frequency and duration of these episodes can vary. It is crucial for healthcare professionals to accurately diagnose bipolar disorder, as misdiagnosis can lead to ineffective treatment and worsening of symptoms.
To further complicate matters, individuals with bipolar disorder may also experience comorbid conditions, such as anxiety disorders or substance use disorders. It is estimated that over 50% of individuals with bipolar I and II also experience anxiety and engage in substance use. Therefore, a comprehensive evaluation is necessary to identify and address all co-occurring conditions.
Treatment Options for Bipolar Disorder
Effective treatment for bipolar disorder often involves a combination of medication, psychotherapy, and lifestyle changes. Medications such as mood stabilizers, anticonvulsants, antipsychotics, and antidepressants are commonly prescribed to manage symptoms and stabilize mood. These medications work by regulating the levels of neurotransmitters in the brain and reducing the severity of mood swings.
Psychotherapy, such as cognitive-behavioral therapy (CBT), family-focused therapy (FFT), and interpersonal and social rhythm therapy (IPSRT), can be highly beneficial for individuals with bipolar disorder. These therapies help individuals develop coping skills, manage stress, and maintain healthy relationships. They can also provide support and education for family members, who play a crucial role in the recovery process.
In addition to medication and therapy, lifestyle changes can also play a significant role in managing bipolar disorder. Maintaining a consistent sleep schedule, following a healthy diet, and engaging in regular exercise can help stabilize mood and improve overall well-being. It is important for individuals with bipolar disorder to establish a routine and practice self-care to minimize the risk of triggering manic or depressive episodes.
For example, a study published in the Journal of Clinical Psychiatry found that individuals who engaged in regular exercise experienced a reduction in depressive symptoms and improved overall mood. Another study published in the journal Bipolar Disorders found that individuals who followed a Mediterranean-style diet, rich in fruits, vegetables, whole grains, and lean proteins, had a lower risk of developing bipolar disorder.
Living with Bipolar Disorder
Living with bipolar disorder can be challenging, but with the right support and self-management strategies, individuals can lead fulfilling lives. It is important for individuals with bipolar disorder to develop a strong support network, which may include family, friends, and support groups. These individuals can provide emotional support, understanding, and encouragement throughout the recovery process.
Self-management strategies are also crucial for individuals with bipolar disorder. Keeping a mood journal, for example, can help individuals identify triggers and patterns in their mood swings. This information can be invaluable for healthcare professionals in developing an effective treatment plan. It is also important for individuals to practice stress management techniques, such as meditation or deep breathing exercises, to reduce the risk of triggering episodes.
It is worth noting that bipolar disorder is not solely a negative experience. Many individuals with bipolar disorder exhibit positive attributes, such as creativity, resilience, and entrepreneurial traits. For example, numerous artists, musicians, and writers have attributed their success to their ability to channel their mood swings into their creative work. While living with bipolar disorder can be challenging, it is important to recognize and embrace these positive aspects.
In conclusion, bipolar disorder is a complex mental health condition that affects millions of people worldwide. It is characterized by extreme shifts in mood, energy levels, and behavior. While the exact causes of bipolar disorder are not yet fully understood, research suggests that it is likely a combination of genetic, neurochemical, and environmental factors. Diagnosing bipolar disorder can be challenging, and misdiagnosis is not uncommon. However, with proper diagnosis, treatment, and support, individuals with bipolar disorder can lead fulfilling lives. It is important for individuals, families, and society as a whole to provide appropriate support and reduce the stigma surrounding mental health. Encouraging individuals with bipolar disorder to seek appropriate treatment, build a support network, and educate loved ones about the condition is essential. With proper treatment, support, and self-management strategies, individuals with bipolar disorder can lead fulfilling lives.
The post Understanding Bipolar Disorder: A Comprehensive Guide to Causes, Symptoms, and Treatment appeared first on Things That Make People Go Aww .


IMAGES
VIDEO
COMMENTS
Bipolar disorder is a broad diagnostic construct associated with significant phenotypic and genetic heterogeneity challenging progress in clinical practice and discovery research. Prospective studies of well-c... Anne Duffy and Paul Grof. International Journal of Bipolar Disorders 2024 12 :12.
Background. Bipolar disorder (BD) is a major mood disorder characterized by recurrent episodes of depression and (hypo)mania (Goodwin and Jamison 2007).According to the Diagnostic and Statistical Manual 5 (DSM-5), the two main subtypes are BD-I (manic episodes, often combined with depression) and BD-II (hypomanic episodes, combined with depression) (APA 2014).
Introduction. Bipolar disorder (BD) is a chronic illness associated with severely debilitating symptoms that can have profound effects on both patients and their caregivers (Miller, 2006).BD typically begins in adolescence or early adulthood and can have life‐long adverse effects on the patient's mental and physical health, educational and occupational functioning, and interpersonal ...
Bipolar disorders are a complex group of severe and chronic disorders that includes bipolar I disorder, defined by the presence of a syndromal, manic episode, and bipolar II disorder, defined by the presence of a syndromal, hypomanic episode and a major depressive episode. Bipolar disorders substantially reduce psychosocial functioning and are ...
Introduction. Bipolar spectrum disorders are a major public health problem, with estimates of lifetime prevalence in the general population of the United States at 3.9 percent, 1 with a range from 1.5 to 6.0 percent. 2 Bipolar disorder is also associated with significant mortality risk, with approximately 25 percent of patients attempting suicide and 11 percent of patients completing. 3 ...
Bipolar disorders (BDs) are recurrent and sometimes chronic disorders of mood that affect around 2% of the world's population and encompass a spectrum between severe elevated and excitable mood states (mania) to the dysphoria, low energy, and despondency of depressive episodes. The illness commonly starts in young adults and is a leading cause of disability and premature mortality. The ...
According to the DSM-5, symptoms must be present for at least 1 week for a diagnosis of a manic episode to be made, or 2 weeks for diagnosis of a depressive episode. However, those durations are ...
Abstract. Bipolar disorder is a severe, complicated, and often misunderstood disorder that can have serious impacts on a person's quality of life, sense of self-worth, and overall health. This ...
60 n engl j med 383;1 nejm.org July 2, 2020 The new england journal of medicine tion deficit-hyperactivity disorder (in 10 to 20%). When these additional problems are present, they increase the ...
Cosgrove VE, Kelsoe JR, Suppes T. Toward a valid animal model of bipolar disorder: how the research domain criteria help bridge the clinical-basic science divide. Biol Psychiatry. 2016;79:62-70.
Overview of bipolar disorder. Bipolar disorder is a chronic and complex mood disorder that is characterized by an admixture of manic (bipolar mania), hypomanic and depressive (bipolar depression) episodes, with significant subsyndromal symptoms that commonly present between major mood episodes Citation 1.Ranked among the leading causes of worldwide disability Citation 2, bipolar I disorder has ...
Bipolar I disorder is defined by the presence of a syndromal, manic episode, and has an estimated global lifetime prevalence of 0·6-1·0%. 1. Bipolar II disorder is defined by the presence of a syndromal, hypomanic episode and a major depressive episode, and has an estimated global lifetime prevalence of 0·4-1·1%. 1.
A shared pathway connects schizophrenia and bipolar disorder. Human and animal studies reveal a neurobiological pathway that connects polygenic risks and behavioural changes that are shared ...
Bipolar disorder (BD) is a severe psychiatric illness with an increasing prevalence worldwide. Although the pathological mechanism of and pharmacological interventions for BD have been extensively investigated in preclinical and clinical studies, a scientometric analysis of the developmental trends, interdisciplinary frontiers, and research hotspots in this field has not yet been conducted.
This issue of the Journal also presents original research articles that address topics related to the treatment of bipolar disorder, the use of a new transcranial magnetic stimulation (TMS) strategy for treatment of refractory depression, and the effects of gender-affirming interventions on the treatment of mood and anxiety disorders in ...
Bipolar disorder is a common psychiatric disorder with a massive psychological and social burden. Research indicates that treatment adherence is not good in these patients. The families' knowledge about the disorder is fundamental for managing their patients' disorder. The purpose of the present study was to investigate the knowledge of the family members of a sample of Iranian patients ...
Bipolar disorder is a recurrent disorder that affects more than 1% of the world population and usually has its onset during youth. Its chronic course is associated with high rates of morbidity and mortality, making bipolar disorder one of the main causes of disability among young and working-age people. The implementation of early intervention strategies may help to change the outcome of the ...
Our operating expenses are covered by separate foundation grants. The Brain & Behavior Research Foundation is a 501 (c) (3) nonprofit organization, our Tax ID # is 31-1020010. The Brain & Behavior Research Foundation has awarded more than $39 million to Bipolar Disorder Research since 1987.
Bipolar disorder, also known as bipolar affective disorder, is one of the top 10 leading causes of disability worldwide. Bipolar disorder is characterized by chronically occurring episodes of mania or hypomania alternating with depression and is often misdiagnosed initially. Treatment involves pharmacotherapy and psychosocial interventions, but ...
Research paper. Impact of bipolar disorder on health-related quality of life and work productivity: Estimates from the national health and wellness survey in Japan ... Bipolar disorder (BD) manifests as both manic and depressive episodes that is recurrent in an individual's life following onset, usually in early adulthood.
Conceptualization of bipolar disorders continues to evolve as the field learns more; for example, changes were made to the DSM-5 diagnostic criteria for BD such that Criteria A for both mania and hypomania now include increased energy as well as elevated or irritable mood (see Table 1). Thus, BD II is now recognized as a disorder of energy as well as mood.
Research in psychology and medicine has linked mental health disorders, and particularly bipolar disorder (BD), to employment in creative professions. Little is known, however, about the ...
Cognitive deficits play an important role in Bipolar Disorder (BPD). The Cognitive Problems and Strategies Assessment (CPSA) is a measure that evaluates the patient's perception of cognitive difficulties, and the spontaneous use of compensatory strategies and could thus have potential utility for clinical practice in patients with BPD.
The sole emphasis on hypomania ignores other important hallmarks of bipolar disorder including an early age at illness onset, periodicity, poor response to antidepressants, and family history of bipolar disorder. Moreover, the use of neuroleptics and/or benzodiazepine may have prevented or attenuated the expression of hypomania.
Research in psychology and medicine has linked mental health disorders, and particularly bipolar disorder (BD), to employment in creative professions. Little is known, however, about the mechanisms for this link, which could be due to biology (primarily through a person's genes) or environmental (through socioeconomic status). Using administrative data on mental health diagnoses and ...
The Bipolar Disorder Biobank collects the following data about each participant: Bipolar diagnosis and history. Personal background. Environment. Family history. What steps are required to become a collaborator? Contact our senior program coordinator if you are interested in collaborating with us.
Relax: Activities like yoga or meditation may help ease anxiety and help with symptoms.; Stay active: Regular exercise improves sleep and helps with stress, among other benefits.; Dietary changes: Poor diet is associated with an increased risk for bipolar disorder and a reduced risk of co-occurring conditions.; Avoid substances: Drinking alcohol, smoking tobacco, or using recreational drugs ...
Introduction. Bipolar affective disorder (bipolar) is a multicomponent illness involving episodes of severe mood disturbance, neuropsychological deficits, immunological and physiological changes, and disturbances in functioning. 1 It is one of the leading causes of disability worldwide 2 and is associated with high rates of premature mortality from both suicide and medical comorbidities. 3,4
Bipolar disorder (BD) is a major mood disorder characterized by recurrent episodes of depression and (hypo)mania (Goodwin and Jamison 2007).According to the Diagnostic and Statistical Manual 5 (DSM-5), the two main subtypes are BD-I (manic episodes, often combined with depression) and BD-II (hypomanic episodes, combined with depression) (APA 2014).
The exact causes of bipolar disorder are not yet fully understood, but research suggests that it is likely a combination of genetic, neurochemical, and environmental factors.Studies have shown ...